Abstract
The incidence of reverse shoulder arthroplasty (RSA) has increased since the Food and Drug Administration approved its use in the United States in 2004. With the current RSA implants available for surgeon use within the United States of America, each design, regardless of humeral inlay vs. onlay, distalizes the shoulder’s center of rotation. This new center of rotation purposely increases tension to the deltoid, which is the main working muscle in RSA, but also retensions the adjacent tendons. Some patients after RSA experience continued anterior shoulder discomfort that limits their active range of motion and overall patient satisfaction. It has been isolated with physical examination that there is tenderness to palpation at the coracoid process and throughout the conjoint tendon. We have completed conjoint tendon lengthening procedures on this subset of patients with excellent clinical results. This article describes the technique for patients who underwent conjoint tendon lengthening after RSA for recalcitrant anterior shoulder pain.
Keywords: Reverse shoulder arthroplasty, Conjoint tendon lengthening, Anterior shoulder pain, Soft tissue lengthening, Postoperative pain, Conjoint tendonitis
The incidence of reverse shoulder arthroplasty (RSA) has increased since the Food and Drug Administration approved its use in the United States in 2004. What was once used to only treat pseudoparalysis from cuff tear arthropathy is now being used to treat proximal humerus fractures, glenoid deformity in the setting of glenohumeral arthritis, massive cuff tears that are irreparable, and salvage option for failed hemi or total shoulder arthroplasty along with oncologic cases.4,6 As with all types of reconstructive joint implants, there is constantly a demand to improve both implant design and surgical technique.
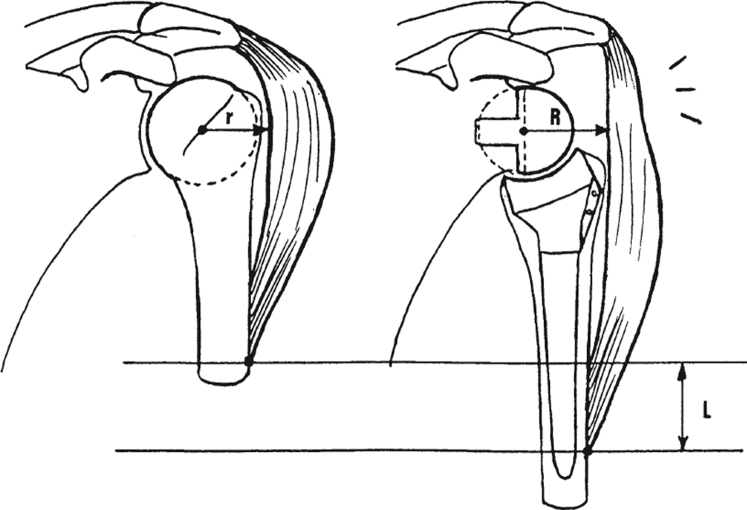
With the current RSA implants available for surgeon use within the United States of America, each design, regardless of humeral inlay vs. onlay, distalizes and medializes the shoulder’s center of rotation (Fig. 1). This new center of rotation purposely increases tension to the deltoid, which is the main working muscle in RSA, but also retensions the adjacent tendons.5,8 Previous studies have reported on coracoid fracture status after RSA.1,5,8 Anakwenze et al believed that these rare coracoid fractures occurred because of increased tension on the conjoint tendon along with decreased bone mineral density within the coracoid as a person ages; therefore, checking the conjoint tendon tension while trialing should be completed before placement of final implants. However, it is unclear in the current literature how the remaining tendons of the rotator cuff or conjoint tendon adapt to the new length tension in the setting of RSA. Our results with RSA are similar to the published literature with respect to functional outcomes and patient-related satisfaction.2,3 However, a subset of patients experience continued anterior shoulder discomfort that limits their active range of motion and overall patient satisfaction. In these patients, physical examination demonstrates tenderness to palpation at the coracoid process and throughout the conjoint tendon. If the pain over the conjoint tendon persists beyond six months postoperatively, we have indicated these patients for elective lengthening of the conjoint tendon. Although tendon lengthening in the orthopedic patient is not a novel idea, that is, partial lengthening of the Achilles tendon and sternocleidomastoid muscle, it has yet to be reported in the shoulder status after RSA. Tashjian et al recently described complete release of the conjoint tendon from the coracoid with improved patient satisfaction scores for the persistent anterior shoulder after RSA without obvious adverse effect to the implant or to implant instability.9 However, no publication at this time describes a conjoint tendon lengthening in this setting which we consider superior to complete release. This article describes our technique for patients who underwent conjoint tendon lengthening after RSA for recalcitrant anterior shoulder pain.
Figure 1.
Schematic showing distalization and medialization of the Center of rotation in an RSA. This results in lengthening of the arm, deltoid, and adjacent soft tissues. RSA, reverse shoulder arthroplasty.
Materials and Methods
There were seven patients who previously underwent an RSA from August 2017 to July 2019 and continued to have anterior shoulder pain over the coracoid process and conjoint tendon for a minimum of six months despite the standard rehab protocol. These patients were indicated for lengthening of the conjoint tendon. The specific population of those who were indicated included patients who underwent RSA for cuff tear arthropathy, chronic irreparable rotator cuff with glenohumeral arthrosis, and failed anatomic total shoulder arthroplasty. Three of the patients within this cohort were referred from outside community surgeons for recalcitrant anterior shoulder pain after both Grammont-style and lateralized RSA.
These procedures were performed in the outpatient setting. The patients were placed under general anesthesia and are positioned in the beach chair position. The proximal portion of the deltopectoral incision is used. A medial full-thickness skin flap is developed to identify the deltopectoral interval. Blunt dissection is then carried down to the conjoint tendon. The conjoint tendon is isolated, and the tension within the proximal aspect of the tendon is palpated.
A three-incision lengthening of the conjoint tendon is performed via 3 partial tenotomies in separate areas of the proximal tendon while sparing the underlying muscle (Figure 2, Figure 3). A Schnidt tonsil clamp is placed across one-third of the width and only under the tendonous portion of the conjoint tendon. Electrocautery is then used to complete the partial tenotomy over the Schnidt tonsil clamp. This lengthening is performed within the proximal 6 cm of the conjoint tendon, which keeps the tenotomy on average proximal to the musculocutaneous nerve. Gentle palpation is performed to ensure that the tendon is no longer under excessive tension. Typically, there is minimal to no bleeding at the tenotomy sites. The wound was then closed in a standard layered fashion. Patients were placed in a shoulder immobilizer for the 24 hours after surgery. There are no postoperative restrictions, and patients were encouraged to use the arm as tolerated. The technique Video of the procedure has also been included for reference.
Figure 2.
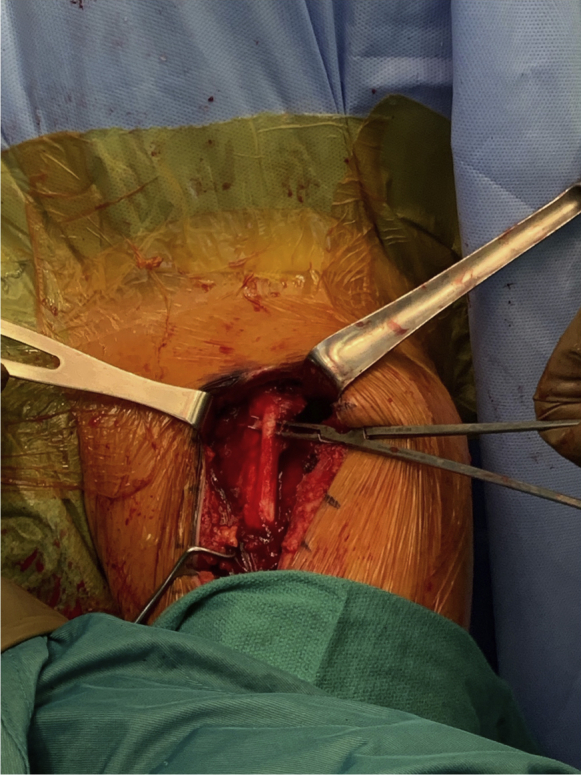
The coracoid process and conjoint tendon of a Left shoulder that has previously undergone RSA are exposed. A Schnidt clamp isolating the lateral portion of the conjoint tendon to be released with the first of three partial tenotomies. RSA, reverse shoulder arthroplasty.
Figure 3.
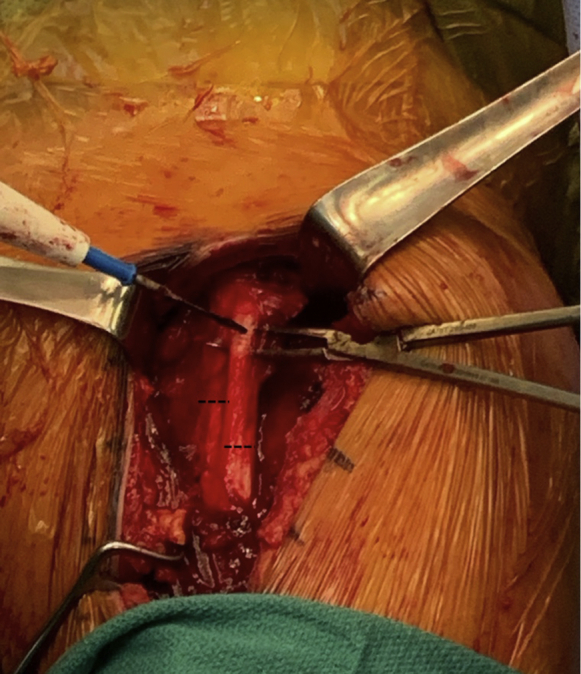
The dashed lines represent the site and extent of the second and third partial tenotomies. Only the tight superficial fascia is released.
Results
Seven patients underwent the procedure between August 2017 and July 2019. After the conjoint lengthening procedure was completed, all patients subjectively reported that the preoperative anterior shoulder pain had resolved within 3 months. Most of the patients regained their range of motion at the 2-week postoperative check. There were no complications within our small cohort. Specifically, there are no cases of musculocutaneous nerve injury, no infections, and no subsequent complete conjoint tendon ruptures. In addition, by performing our Z-lengthening to the conjoint tendon, there were no issues of postoperative instability or functional consequences. These patients were then returned to their standard RSA follow-up schedule. Six of seven patients describe complete or near-complete relief of their anterior shoulder pain at the initial postoperative visit. The seventh patient was improved but not asymptomatic within 2 weeks of surgery.
Discussion
The incidence of RSA in the United States of America has increased since Food and Drug Administration approval in 2004.4,6,7 Extrapolating data from previous nationwide utilization studies have suggested a growth of 12.3% in shoulder arthroplasty (total shoulder arthroplasty and RSA) from 2008 to 2011. This steady increase in shoulder arthroplasty is expected to continue as the active elderly population increases. Unfortunately, it was not until 2010 that the International Classification of Diseases-9 procedure codes were updated to give RSA a unique code (80.88); therefore, we can only have rough estimates as to what the actual increase in RSA is as there are expected delays in populating the national database.6,7
The design of the RSA is predicated on chronically torn and dysfunctional rotator cuff, therefore solely relying on the deltoid muscle. To maximize deltoid function, the glenohumeral center of rotation is distal and medial compared with native anatomy.4,5,8 Although this new center of rotation purposely tensions the deltoid to maximize shoulder function, there are assumed risks which have been published. The risks include, but are not limited to, axillary nerve palsy, brachial plexopathy, deltoid fatigue, acromial stress fracture, coracoid stress fracture, and recalcitrant anterior shoulder pain.1, 2, 3 The senior author has noticed in his practice that there is a subset of patients who complain of recalcitrant anterior shoulder pain along the conjoint tendon to its origin at the coracoid process.
Most patients within the cohort underwent shoulder replacement with Grammont-style RSA implants (humeral neck-shaft angle ≥150 degrees), which distalizes and medializes the centers of rotation. However, 2 of the patients had a lateralized design, which also medializes and can distally displace the center of rotation depending on placement of the glenosphere. By purposely distalizing the center of rotation to tension the deltoid, the arm length increases along with increased tension to the surrounding soft tissues.8 We have concluded that although most people adjust well to the new soft tissue lengthening and tension, there are a small group of people who experience persistent anterior shoulder pain because of over-tension of the conjoint tendon. Interesting is that although the conjoint tendon is over tensioned, no patients within the cohort presented with a musculocutaneous nerve palsy. In addition, there were no issues of postoperative instability or functional consequences after lengthening of the conjoint joint with our described technique. Although there are a limited number of patients within this case series, the clinical results after tendon lengthening have been successful; therefore, we have changed the way we assess soft tissue tension when trialing and once final implants are placed. We have continued to perform this lengthening when necessary and have a larger cohort of patients in whom it has been performed prospectively.10 When implanting an RSA, if the conjoint tendon is taught to palpation without any suppleness, we now proceed with primary Z-lengthening at the index replacement procedure.
Conclusion
Recalcitrant anterior shoulder pain after RSA does occur. One needs to consider over-tensioning to the conjoint tendon as the reason for anterior shoulder pain if it persists. The described technique has been successful in our patient population. Additional biomechanical studies should be completed to better quantify the tension applied to the conjoint after RSA and compare the tension after the Z-lengthening procedure is completed.
Disclaimers:
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this technique article.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.xrrt.2021.12.005.
Supplementary data
References
- 1.Anakwenze O.A., Kancherla V.K., Carolan G.F., Abboud J. Coracoid fracture after reverse total shoulder arthroplasty: a report of 2 cases. Am J Orthop (Belle Mead NJ) 2015;44:E469–E472. [PubMed] [Google Scholar]
- 2.Black E., Roberts S., Siegal E., Yannopoulos P., Higgins L., Warner J. Failure after reverse total shoulder arthroplasty: what is the success of component revision? J Shoulder Elbow Surg. 2015;24:1908–1914. doi: 10.1016/j.jse.2015.05.029. [DOI] [PubMed] [Google Scholar]
- 3.Boileau P., Melis B., Duperron D., Moineau G., Rumian A., Han Y. Revision surgery of reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22:1359–1370. doi: 10.1016/j.jse.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 4.Drake G.N., O’Connor D.P., Edwards T.B. Indications for reverse total shoulder arthroplasty in rotator cuff disease. Clin Orthop Relat Res. 2010;468:1526–1533. doi: 10.1007/s11999-009-1188-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grammont P.M., Baulot E. The classic: delta shoulder prosthesis for rotator cuff rupture. 1993. Clin Orthop Relat Res. 2011;469:2424. doi: 10.1007/s11999-011-1960-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim S.H., Wise B.L., Zhang Y., Szabo R.M. Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am. 2011;93:2249–2254. doi: 10.2106/JBJS.J.01994. [DOI] [PubMed] [Google Scholar]
- 7.Schairer W.W., Nwachukwu B.U., Lyman S., Craig E.V., Gulotta L.V. National utilization of reverse total shoulder arthroplasty in the United States. J Shoulder Elbow Surg. 2015;24:91–97. doi: 10.1016/j.jse.2014.08.026. [DOI] [PubMed] [Google Scholar]
- 8.Schwartz D.G., Kang S.H., Lynch T.S., Edwards S., Nuber G., Zhang L.Q., et al. The anterior deltoid’s importance in reverse shoulder arthroplasty: a cadaveric biomechanical study. J Shoulder Elbow Surg. 2013;22:357–364. doi: 10.1016/j.jse.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Tashjian R.Z., Frandsen J.J., Christensen G.V., Chalmers P.N. Conjoint tendon release for persistent anterior shoulder pain following reverse total shoulder arthroplasty. JSES Int. 2020;4:975–978. doi: 10.1016/j.jseint.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams R., Gomez G., Huffman G.R. AAOS Orthopaedic Video Theater: San Diego, CA; San Diego, CA: 2021. Conjoint tendon lengthening for alleviation or prevention of anterior shoulder pain after reverse total shoulder arthroplasty. Available at: https://www.aaos.org/videos/video-detail-page/23227__Videos. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.