Abstract
Background
Reverse shoulder arthroplasty (RSA) was developed in the late twentieth century to provide a stable arthroplasty option for patients with rotator cuff deficiency arthropathy. Since its inception, there have been changes in materials, design, and positioning. One of the persistent clinical issues has been difficulty with internal rotation (IR) and the associated difficulty with behind the back activities. Implant design, positioning, and the available soft tissues may influence IR after RSA. The purpose of this systematic review is to assess factors that impact IR following RSA.
Methods
The literature search, based on PRISMA guidelines, used 4 databases: Pubmed, Embase, Web of Science, and Cochrane Central Register of Controlled Trials. We included clinical trials that compared different implantation and design modifications and assessed IR.
Results
Of the 617 articles identified in the initial search, 46 satisfied the inclusion criteria. The articles explored multiple factors of RSA and their effects on IR, including humeral and glenoid components and muscle function and integrity. Among humeral factors affecting rotation, there was a broad consensus that: IR decreases as retroversion increases, humeral neck-shaft angle less than 155° improves IR, lateralized humeral offset does not improve IR, and shallow cups improve IR. Insert thickness was not associated with a reproducible effect. Of the studies evaluating the effect of glenoid components, there was majority agreement that glenosphere lateralization improved IR, and there were mixed results regarding the effects of glenosphere size and tilt. Others included one study in each: glenoid overhang, retroversion, and baseplate. One study found an association between teres minor insufficiency and improved IR, with mixed results in the presence of fatty infiltration in both teres minor and subscapularis. Most studies noted subscapularis repair had no effect on IR.
Conclusion
Prosthetic variables affecting IR are not widely studied. Based on the existing literature, evidence is conflicting. More research needs to be undertaken to gain a greater understanding regarding which factors can be modified to improve IR in RSA patients.
Keywords: Reverse total shoulder arthroplasty, Internal rotation, Shoulder replacement, Shoulder motion, Postoperative outcomes, Range of motion
In 1985, Grammont et al17 developed a novel reverse shoulder arthroplasty (RSA) prosthesis, utilizing a hemisphere on the glenoid and a socket in the proximal humerus. Originally used for the treatment of rotator cuff arthropathy, its clinical indications have been expanded to include proximal humeral fractures in the elderly, neoplasms, refractory glenohumeral instability, irreparable rotator cuff tears, and pseudoparalysis.15,48
The original Grammont style of RSA includes a humeral inclination of 155° with a medialized center of rotation.8 However, in the long term, this medialization often resulted in scapular notching, and limited improvement of internal and external rotation.3,42 This limitation can be quite disabling as it poses potential issues with fundamental activities of daily living such as perineal care.12
The purpose of this study was to review the current literature on RSA implantation factors that influence shoulder internal rotation (IR) after RSA. Very few papers focus solely on the effect of RSA on IR. This review will provide a synthesis of the current literature for the numerous factors affecting IR in RSA.
Materials and methods
The literature search was conducted from June 5, 2020 to July 15, 2020, following PRISMA guidelines. Studies not published in English were excluded. Four databases were used: Pubmed, Embase, Web of Science, and Cochrane Central Register of Controlled Trials. We utilized search terms “reverse shoulder arthroplasty OR reverse total shoulder OR reverse shoulder prosthesis” in the title AND “internal rotation” in the abstract to find articles in the time period ending at July 15, 2020. No contact was made with study authors to identify additional studies due to the desire to find and use data already published in journals.
The inclusion criteria included comparison of different adjustments made to both prosthesis design and/or implantation technique. This included alterations to both the glenoid and humeral components and tendon repairs. Additionally, mention of shoulder IR measurement needed to be included. This included terms such as hand to back pocket, toileting ability, or patient’s ability to reach the highest vertebrae. Exclusion criteria included systematic reviews, studies focusing on revision surgery, animal studies, comparative surgical procedures, novel surgical methods for a specific pathology, internal and external rotation mentioned as a single data point, and conference abstracts. The articles had to have compared experimental variables as it relates to IR (eg, how 2 different implant designs impacted IR).
Results
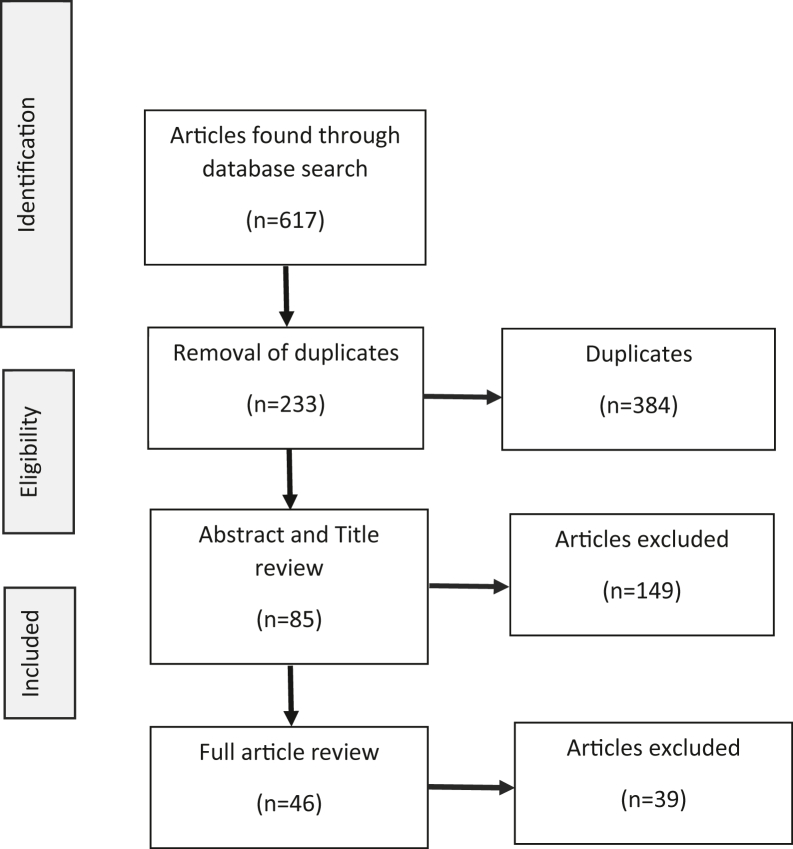
The search terms yielded 617 articles. Once the inclusion and exclusion criteria were applied, 46 articles remained to be used in the systematic review (Fig. 1).
Figure 1.
Process of article recruitment for systematic review.
Humeral components
Retroversion
From the literature search, 4 humeral component variables were studied to determine their effects on IR (Table I). These included retroversion, humeral neck-shaft angle, humeral offset, and cup depth. In terms of retroversion, an overwhelming majority of studies that examined this variable found that IR decreases as retroversion increases.5,19,22,25,26,35,37,41 Of the examined studies, only 1 mentioned that retroversion had no significant difference in IR.7
Table I.
Humeral components and their effect on IR.
| Humeral component changed | Change to IR | Study, yr | Study type |
|---|---|---|---|
| Retroversion | Inverse relationship | Berhouet (2013)5 | Cadaver |
| Gulotta (2012)19 | 3D model | ||
| Jeon (2016)22 | Retrospective | ||
| Kim (2019)25 | 3D model | ||
| Kontaxis (2017)26 | 3D model | ||
| Oh (2020)35 | Retrospective | ||
| Rhee (2015)37 | Retrospective | ||
| Stephenson (2011)41 | Cadaver | ||
| No difference | Boer (2017)7 | Retrospective | |
| Humeral neck-shaft angle | 155 more stable IR | Oh (2014)36 | Cadaver |
| Below 155 improved IR | Keener(2018)24 | Retrospective | |
| Rol (2019)39 | Prospective | ||
| Virani (2013)46 | 3D model | ||
| Werner (2017)49 | 3D model | ||
| Offset | Lateralization no change | Henninger (2014)21 | Biomechanical |
| Kalouche (2009)23 | Retrospective | ||
| Rojas (2019)38 | Retrospective | ||
| Tashjian (2015)43 | Biomechanical | ||
| Verdano (2018)45 | Retrospective | ||
| Virani (2013)46 | 3D model | ||
| Lateralization increases IR | Berhouet (2015)6 | Biomechanical | |
| Posterior offset no change | Chan (2017)11 | Biomechanical | |
| Cup depth | IR improved when shallow | Krämer (2016)27 | Cadaver |
IR, internal rotation; 3D, 3-dimensional.
Neck-shaft angle
For the humeral neck-shaft angle, 1 article mentioned IR of the shoulder was more stable at 155°.35 However, 4 articles found IR improved at shaft angles below 155°.24,39,46,51 The difference between 145° and 135° was unclear.24,51 Two studies did not find a difference between 145° and 155°.4,31
Humeral offset
There were 8 studies that examined the changes humeral offset has on IR. IR was not influenced by humeral lateralization in 6 studies.21,23,38,43,45,46 Of the 2 articles that disputed this, one found posterior offset increased IR,6 while another found lateralization increased IR.11
Humeral cup depth
Of the 46 studies, only one mentioned the effects of cup depth on IR, noting IR improved with a shallow cup.27
Glenoid components
In terms of glenosphere implantation and design, 7 different aspects were investigated in the articles that specifically evaluated the effects on IR (Table II). This included lateralization, diameter, overhang, retroversion, tilt, baseplate position/ design, and insert thickness.
Table II.
Glenoid components and their effect on IR.
| Changes to glenoid component | Change to IR | Study, yr | Study type |
|---|---|---|---|
| Lateralization | Improves IR | Berhouet (2013)5 | Cadaver |
| Keener (2018)24 | Retrospective | ||
| Krämer (2016)27 | Cadaver | ||
| Lädermann (2020)28 | 3D model | ||
| Li (2013)30 | 3D model | ||
| Terrier (2013)44 | 3D model | ||
| Werner (2018)50 | 3D model | ||
| BIO-RSA not better than tRSA | Athwal (2015)2 | Prospective | |
| Collin (2018)14 | Retrospective | ||
| Greiner (2015)18 | Prospective | ||
| NS effect | Langhor (2015)29 | Cadaver | |
| Merolla (2019)33 | Retrospective | ||
| Rojas (2019)38 | Retrospective | ||
| Diameter | 42 mm increases IR | Berhouet (2013)5 | Cadaver |
| Virani (2013)46 | 3D model | ||
| No difference | Müller (2018)34 | Retrospective | |
| Inverse relationship | Langhor (2015) | Cadaver | |
| Terrier (2013)44 | 3D model | ||
| Overhang | Improved | Rol (2019)39 | Prospective |
| Retroversion | Greater retroversion greater IR | Keener (2018)24 | Retrospective |
| Tilt | Inferior tilt, improved IR | Li (2013)30 | 3D model |
| Decreased IR | Werner (2018)50 | 3D model | |
| Baseplate | NS between 25-29mm | Chae (2014)10 | Biomechanical |
| Insert thickness | Reduces when over 6mm | Tashjian (2015)43 | Biomechanical |
| Increases releative to IR | Henninger (2012)20 | Biomechanical | |
| No difference with high or low constraints | Abdulla (2017)1 | Cadaver |
IR, internal rotation; 3D, 3-dimensional; RSA, reverse shoulder arthroplasty; tRSA, traditional reverse shoulder arthroplasty.
Lateralization
Of studies examining lateralization, 7 of 13 found that lateralization of the glenosphere improved IR.5,24,27,28,30,44,50 Of the 6 whose results did not agree with the majority, 3 looked specifically at boney increase-offset RSA (BIO-RSA), which increases glenosphere lateralization through the use of a bone graft. These studies found BIO-RSA did not improve IR when compared to standard RSA.2,14,27 The other 3 articles found lateralization of the glenosphere had no significant effect on active IR.29,32,38
Glenosphere diameter
In terms of glenosphere diameter, 2 studies found a diameter of 42 mm increased IR.45,46 One study found no difference34; however, others found that an increased diameter decreased passive IR.29,44 Terrier et al44 found a 36 mm and 42 mm diameter glenosphere made it difficult for the completion of hand to back-pocket motion as a measurement of IR, with a 42 mm offering a slight improvement.
Inferior overhang
Only 1 study examined the effects of overhang changes in improvements to IR. This study found that IR improved in patients with at least 6 mm of overhang.39
Glenosphere version
Similar to overhang, glenosphere retroversion also had only 1 investigation. The study conducted by Keener et al24 in 2018 found that a greater glenosphere retroversion resulted in greater IR. Two articles reported the impact of glenosphere on IR. Li et al30 in 2013 found inferior tilt improved IR. Meanwhile, Werner et al50 in 2018 found inferior tilt of the glenosphere decreased IR. Chae et al10 in 2014 found that a baseplate of 25-29 mm had similar IR.
Finally, studies on insert thickness yielded variable results. One study stated that thickness over 6 mm reduced passive IR,43 while another found that increased insert thickness resulted in an increase relative IR.20 This study used spacers to increase thickness. Abdulla et al1 in 2017 reported when placed with shallow or deep cup inserts, there was an insignificant change in IR compared to the standard but a significant difference between the high and low constraints.
Soft tissue envelope
Two muscles showed a relationship to IR: teres minor and subscapularis (Table III). IR improved when teres minor function was absent.39 Additionally, 2 studies found contradictory results regarding whether fatty infiltrate of the teres minor improved IR.32,40 Regarding the subscapularis, the majority of studies found subscapularis repair had no effect on IR,9,13,35,38,47 while 1 study noted an effect.16 Additionally, results were contradictory regarding the effect of fatty infiltration on IR.32,51
Table III.
Muscle status effects on IR.
| Muscle | Changes to muscle | Change to IR | Study, yr | Study type |
|---|---|---|---|---|
| Teres minor | Repair | Dec IR | Rol (2019)39 | Prospective |
| Fatty | Less, better IR | Simovitch (2007)40 | Prospective | |
| infiltrate | NS | Merolla (2020)32 | Retrospective | |
| Subscapularis | Repair | No effect | Bonnevialle (2020)9 | Retrospective |
| Clark (2012)13 | Retrospective | |||
| Oh (2020)35 | Retrospective | |||
| Rojas (2019)38 | Retrospective | |||
| Vourazeris (2017)47 | Retrospective | |||
| Improved IR | Friedman (2017)16 | Database analysis | ||
| Fatty | NS | Merolla (2020)32 | Retrospective | |
| Infiltrate | Wiater (2015)51 | Prospective |
IR, internal rotation.
Discussion
Since the advent of the reverse total shoulder arthroplasty procedure decreased IR and behind the back movement has emerged as a common patient complaint. We sought to analyze the existing literature for factors affecting IR.
Of the component changes found, only 4 categories had a strong consensus of studies in agreement. The inverse relationship between humeral retroversion and IR had 8 out of 9 studies with similar results. These studies included experiments on cadavers, 3-dimensional models, and retrospective clinicals. Berhouet et al6 found that instead of an increase in IR when retroversion increases, there is an increase in external rotation. Additionally, for the humeral neck-shaft angle, 4 out of 5 studies agreed that an angle below 155° improved IR.24,39,46,49 The angles compared in these studies included 135°, 145°, and 155°. Both Keener et al24 and Werner et al49 did not find a significant difference between 135° and 145°. Although Mellano et al31 disagreed with the majority, his disagreement could have been due to the fact that the study was focused on comparing medialized and lateralized center of rotation rather than the humeral neck-shaft angle as a single entity. The offset of the humeral component does not affect IR, while the lateralization of the glenosphere improves IR. The final category that had majority of the studies in agreement was the lack of effect on IR when the subscapularis was repaired.
Unfortunately, biomechanical studies noting improved IR by changing a single variable do not always translate to real-world clinical improvement in IR. This is most likely due to a variety of variables that act synergistically and are difficult to model. We are currently working on the development of a better computer model to more closely replicate in vivo conditions.
While there is literature pertaining to the aforementioned categories, this does not hold true for other aspects of RSA components that might influence IR. There is little or no literature on cup depth, glenoid overhang, glenoid retroversion, and glenoid baseplate size. Therefore, conclusions on their effects on IR cannot be made. This lack of investigation could be due to the relative newness of the procedure. Evaluation of glenoid diameter, tilt, insert thickness, and fatty infiltrate of the teres minor yielded contradictory results in the limited literature available. These differences could also be due to the variation in another component of an RSA between the studies, resulting in lack of control between studies. For example, in the assessment of glenoid tilt, the 2 available studies used different degrees of humeral retroversion, one used the patient’s natural retroversion,50 while the other kept a 20° constant.30 The different results observed may be due to the change in retroversion not the glenoid tilt.
One of the greatest limitations of this study is that many of the papers included are single variable studies utilizing different types of modeling. In reality, multiple variables likely interact to affect IR as well as other aspects of outcome. The development of better biomechanical and simulated computer models that more closely replicate in vivo conditions will help improve our understanding of how to improve IR as well as other aspects of outcome.
Conclusion
In our literature review, we found numerous RSA design and technique factors that had variable outcomes on IR. A majority of studies agree that humeral retroversion causes decreased IR, neck-shaft angle below 155° improves IR, lateralization of the humerus has no change on IR, lateralization of the glenosphere improves IR, and subscapularis repair has no effect on IR. Given the relative paucity of studies as well as the contradictory nature of some of the findings, the impact of prosthetic placement and design on IR merits further investigation.
Disclaimers:
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this review article.
References
- 1.Abdulla I., Langohr G.L., Giles J.W., Johnson J.A., Athwal G.S. The effect of humeral polyethylene insert constraint on reverse shoulder arthroplasty biomechanics. Shoulder Elbow. 2018;10:25–31. doi: 10.1177/2F1758573217701065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Athwal G.S., MacDermid J.C., Reddy K.M., Marsh J.P., Faber K.J., Drosdowech D. Does bony increased-offset reverse shoulder arthroplasty decrease scapular notching? J Shoulder Elbow Surg. 2015;24:468–473. doi: 10.1016/j.jse.2014.08.015. [DOI] [PubMed] [Google Scholar]
- 3.Barco R., Savvidou O.D., Sperling J.W., Sanchez-Sotelo J., Cofield R.H. Complications in reverse shoulder arthroplasty. EFORT Open Rev. 2016;1:72–80. doi: 10.1302/2058-5241.1.160003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beltrame A., Di Benedetto P., Cicuto C., Cainero V., Gisonni R., Causero A. Onlay versus Inlay humeral steam in Reverse Shoulder Arthroplasty (RSA): clinical and biomechanical study. Acta Biomed. 2019;90:54–63. doi: 10.23750/abm.v90i12-S.8983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berhouet J., Garaud P., Favard L. Influence of glenoid component design and humeral component retroversion on internal and external rotation in reverse shoulder arthroplasty: a cadaver study. Orthop Traumatol Surg Res. 2013;99:887–894. doi: 10.1016/j.otsr.2013.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Berhouet J., Kontaxis A., Gulotta L.V., Craig E., Warren R., Dines J., et al. Effects of the humeral tray component positioning for onlay reverse shoulder arthroplasty design: a biomechanical analysis. J Shoulder Elbow Surg. 2015;24:569–577. doi: 10.1016/j.jse.2014.09.022. [DOI] [PubMed] [Google Scholar]
- 7.de Boer F.A., van Kampen P.M., Huijsmans P.E. Is there any influence of humeral component retroversion on range of motion and clinical outcome in reverse shoulder arthroplasty? A clinical study. Musculoskelet Surg. 2017;101:85–89. doi: 10.1007/s12306-016-0443-y. [DOI] [PubMed] [Google Scholar]
- 8.Boileau P., Watkinson D.J., Hatzidakis A.M., Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005;14:S147–S161. doi: 10.1016/j.jse.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 9.Bonnevialle N., Ohl X., Clavert P., Favard L., Frégeac A., Obert L., et al. Should the supraspinatus tendon be excised in the case of reverse shoulder arthroplasty for fracture? Eur J Orthop Surg Traumatol. 2020;30:231–235. doi: 10.1007/s00590-019-02572-7. [DOI] [PubMed] [Google Scholar]
- 10.Chae S.W., Kim S.Y., Lee H., Yon J.R., Lee J., Han S.H. Effect of baseplate size on primary glenoid stability and impingement-free range of motion in reverse shoulder arthroplasty. BMC Musculoskelet Disord. 2014;15:417. doi: 10.1186/1471-2474-15-417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chan K., Langohr G.D.G., Mahaffy M., Johnson J.A., Athwal G.S. Does humeral component lateralization in reverse shoulder arthroplasty affect rotator cuff torque? Evaluation in a cadaver model. Clin Orthop Relat Res. 2017;475:2564–2571. doi: 10.1007/s11999-017-5413-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen A.L., Bain E.B., Horan M.P., Hawkins R.J. Determinants of patient satisfaction with outcome after shoulder arthroplasty. J Shoulder Elbow Surg. 2007;16:25–30. doi: 10.1016/j.jse.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 13.Clark J.C., Ritchie J., Song F.S., Kissenberth M.J., Tolan S.J., Hart N.D., et al. Complication rates, dislocation, pain, and postoperative range of motion after reverse shoulder arthroplasty in patients with and without repair of the subscapularis. J Shoulder Elbow Surg. 2012;21:36–41. doi: 10.1016/j.jse.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 14.Collin P., Liu X., Denard P.J., Gain S., Nowak A., Lädermann A. Standard versus bony increased-offset reverse shoulder arthroplasty: a retrospective comparative cohort study. J Shoulder Elbow Surg. 2018;27:59–64. doi: 10.1016/j.jse.2017.07.020. [DOI] [PubMed] [Google Scholar]
- 15.Flatow E.L., Harrison A.K. A history of reverse total shoulder arthroplasty. Clin Orthop Relat Res. 2011;469:2432–2439. doi: 10.1007/s11999-010-1733-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Friedman R.J., Flurin P.H., Wright T.W., Zuckerman J.D., Roche C.P. Comparison of reverse total shoulder arthroplasty outcomes with and without subscapularis repair. J Shoulder Elbow Surg. 2017;26:662–668. doi: 10.1016/j.jse.2016.09.027. [DOI] [PubMed] [Google Scholar]
- 17.Grammont P.M., Trouilloud P., Laffay J.P., Deries X. Étude et réalisation d’une nouvelle prothèse d’épaule. Rhumatologie. 1987;39:17–22. [Google Scholar]
- 18.Greiner S., Schmidt C., Herrmann S., Pauly S., Perka C. Clinical performance of lateralized versus non-lateralized reverse shoulder arthroplasty: a prospective randomized study. J Shoulder Elbow Surg. 2015;24:1397–1404. doi: 10.1016/j.jse.2015.05.041. [DOI] [PubMed] [Google Scholar]
- 19.Gulotta L.V., Choi D., Marinello P., Knutson Z., Lipman J., Wright T., et al. Humeral component retroversion in reverse total shoulder arthroplasty: a biomechanical study. J Shoulder Elbow Surg. 2012;21:1121–1127. doi: 10.1016/j.jse.2011.07.027. [DOI] [PubMed] [Google Scholar]
- 20.Henninger H.B., Barg A., Anderson A.E., Bachus K.N., Tashjian R.Z., Burks R.T. Effect of deltoid tension and humeral version in reverse total shoulder arthroplasty: a biomechanical study. J Shoulder Elbow Surg. 2012;21:483. doi: 10.1016/j.jse.2011.01.040. [DOI] [PubMed] [Google Scholar]
- 21.Henninger H.B., King F.K., Tashjian R.Z., Burks R.T. Biomechanical comparison of reverse total shoulder arthroplasty systems in soft tissue-constrained shoulders. J Shoulder Elbow Surg. 2014;23:e108–e117. doi: 10.1016/j.jse.2013.08.008. [DOI] [PubMed] [Google Scholar]
- 22.Jeon B.K., Panchal K.A., Ji J.H., Xin Y.Z., Park S.R., Kim J.H., et al. Combined effect of change in humeral neck-shaft angle and retroversion on shoulder range of motion in reverse total shoulder arthroplasty - A simulation study. Clin Biomech (Bristol, Avon) 2016;31:12–19. doi: 10.1016/j.clinbiomech.2015.06.022. [DOI] [PubMed] [Google Scholar]
- 23.Kalouche I., Sevivas N., Wahegaonker A., Sauzieres P., Katz D., Valenti P. Reverse shoulder arthroplasty: does reduced medialisation improve radiological and clinical results? Acta Orthop Belg. 2009;75:158–166. [PubMed] [Google Scholar]
- 24.Keener J.D., Patterson B.M., Orvets N., Aleem A.W., Chamberlain A.M. Optimizing reverse shoulder arthroplasty component position in the setting of advanced arthritis with posterior glenoid erosion: a computer-enhanced range of motion analysis. J Shoulder Elbow Surg. 2018;27:339–349. doi: 10.1016/j.jse.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 25.Kim S.J., Jang S.W., Jung K.H., Kim Y.S., Lee S.J., Yoo Y.S. Analysis of impingement-free range of motion of the glenohumeral joint after reverse total shoulder arthroplasty using three different implant models. J Orthop Sci. 2019;24:87–94. doi: 10.1016/j.jos.2018.08.016. [DOI] [PubMed] [Google Scholar]
- 26.Kontaxis A., Chen X., Berhouet J., Choi D., Wright T., Dines D.M., et al. Humeral version in reverse shoulder arthroplasty affects impingement in activities of daily living. J Shoulder Elbow Surg. 2017;26:1073–1082. doi: 10.1016/j.jse.2016.11.052. [DOI] [PubMed] [Google Scholar]
- 27.Krämer M., Bäunker A., Wellmann M., Hurschler C., Smith T. Implant impingement during internal rotation after reverse shoulder arthroplasty. the effect of implant configuration and scapula anatomy: a biomechanical study. Clin Biomech (Bristol, Avon) 2016;33:111–116. doi: 10.1016/j.clinbiomech.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 28.Lädermann A., Denard P.J., Collin P., Zbinden O., Chiu J.C., Boileau P., et al. Effect of humeral stem and glenosphere designs on range of motion and muscle length in reverse shoulder arthroplasty. Int Orthop. 2020;44:519–530. doi: 10.1007/s00264-019-04463-2. [DOI] [PubMed] [Google Scholar]
- 29.Langohr G.D., Giles J.W., Athwal G.S., Johnson J.A. The effect of glenosphere diameter in reverse shoulder arthroplasty on muscle force, joint load, and range of motion. J Shoulder Elbow Surg. 2015;24:972–979. doi: 10.1016/j.jse.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 30.Li X., Knutson Z., Choi D., Lobatto D., Lipman J., Craig E.V., et al. Effects of glenosphere positioning on impingement-free internal and external rotation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22:807–813. doi: 10.1016/j.jse.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 31.Mellano C.R., Kupfer N., Thorsness R., Chalmers P.N., Feldheim T.F., O'Donnell P., et al. Functional results of bilateral reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:990–996. doi: 10.1016/j.jse.2016.10.011. [DOI] [PubMed] [Google Scholar]
- 32.Merolla G., De Cupis M., Walch G., De Cupis V., Fabbri E., Franceschi F., et al. Pre-operative factors affecting the indications for anatomical and reverse total shoulder arthroplasty in primary osteoarthritis and outcome comparison in patients aged seventy years and older. Int Orthop. 2020;44:1131–1141. doi: 10.1007/s00264-020-04501-4. [DOI] [PubMed] [Google Scholar]
- 33.Merolla G., Paladini P., Porcellini G. Grammont humeral design versus onlay curved-stem reverse shoulder arthroplasty: comparison of clinical and radiographic outcomes with minimum two-year follow-up. JSES Open Access. 2019;3:247. doi: 10.1016/j.jses.2019.10.056. [DOI] [PubMed] [Google Scholar]
- 34.Müller A.M., Born M., Jung C., Flury M., Kolling C., Schwyzer H.K., et al. Glenosphere size in reverse shoulder arthroplasty: is larger better for external rotation and abduction strength? J Shoulder Elbow Surg. 2018;27:44–52. doi: 10.1016/j.jse.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 35.Oh J.H., Sharma N., Rhee S.M., Park J.H. Do individualized humeral retroversion and subscapularis repair affect the clinical outcomes of reverse total shoulder arthroplasty? J Shoulder Elbow Surg. 2020;29:821–829. doi: 10.1016/j.jse.2019.08.016. [DOI] [PubMed] [Google Scholar]
- 36.Oh J.H., Shin S.J., McGarry M.H., Scott J.H., Heckmann N., Lee T.Q. Biomechanical effects of humeral neck-shaft angle and subscapularis integrity in reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1091–1098. doi: 10.1016/j.jse.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 37.Rhee Y.G., Cho N.S., Moon S.C. Effects of humeral component retroversion on functional outcomes in reverse total shoulder arthroplasty for cuff tear arthropathy. J Shoulder Elbow Surg. 2015;24:1574–1581. doi: 10.1016/j.jse.2015.03.026. [DOI] [PubMed] [Google Scholar]
- 38.Rojas J., Bitzer A., Joseph J., Srikumaran U., McFarland E.G. Toileting ability of patients after primary reverse total shoulder arthroplasty. JSES Int. 2019;4:174–181. doi: 10.1016/j.jses.2019.10.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rol M., Favard L., Berhouet J., la Société d’orthopédie de l’Ouest Factors associated with internal rotation outcomes after reverse shoulder arthroplasty. Orthop Traumatol Surg Res. 2019;105:1515–1519. doi: 10.1016/j.otsr.2019.07.024. [DOI] [PubMed] [Google Scholar]
- 40.Simovitch R.W., Helmy N., Zumstein M.A., Gerber C. Impact of fatty infiltration of the teres minor muscle on the outcome of reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2007;89:934–939. doi: 10.2106/jbjs.f.01075. [DOI] [PubMed] [Google Scholar]
- 41.Stephenson D.R., Oh J.H., McGarry M.H., Rick Hatch G.F., 3rd, Lee T.Q. Effect of humeral component version on impingement in reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2011;20:652–658. doi: 10.1016/j.jse.2010.08.020. [DOI] [PubMed] [Google Scholar]
- 42.Stevens C.G., Struk A.M., Wright T.W. The functional impact of bilateral reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1341–1348. doi: 10.1016/j.jse.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 43.Tashjian R.Z., Burks R.T., Zhang Y., Henninger H.B. Reverse total shoulder arthroplasty: a biomechanical evaluation of humeral and glenosphere hardware configuration. J Shoulder Elbow Surg. 2015;24:e68–e77. doi: 10.1016/j.jse.2014.08.017. [DOI] [PubMed] [Google Scholar]
- 44.Terrier A., Scheuber P., Pioletti D.P., Farron A. Activities of daily living with reverse prostheses: importance of scapular compensation for functional mobility of the shoulder. J Shoulder Elbow Surg. 2013;22:948–953. doi: 10.1016/j.jse.2012.09.014. [DOI] [PubMed] [Google Scholar]
- 45.Verdano M.A., Aliani D., Galavotti C., Maroun C., Vaienti E., Ceccarelli F. Grammont versus lateralizing reverse shoulder arthroplasty for proximal humerus fracture: functional and radiographic outcomes. Musculoskelet Surg. 2018;102:57–65. doi: 10.1007/s12306-018-0565-5. [DOI] [PubMed] [Google Scholar]
- 46.Virani N.A., Cabezas A., Gutiérrez S., Santoni B.G., Otto R., Frankle M. Reverse shoulder arthroplasty components and surgical techniques that restore glenohumeral motion. J Shoulder Elbow Surg. 2013;22:179–187. doi: 10.1016/j.jse.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 47.Vourazeris J.D., Wright T.W., Struk A.M., King J.J., Farmer K.W. Primary reverse total shoulder arthroplasty outcomes in patients with subscapularis repair versus tenotomy. J Shoulder Elbow Surg. 2017;26:450–457. doi: 10.1016/j.jse.2016.09.017. [DOI] [PubMed] [Google Scholar]
- 48.Wall B.T., Mottier G., Walch G. Complications and revision of the reverse prosthesis: a multicenter study of 457 cases. J Shoulder Elbow Surg. 2007;16:e55. doi: 10.1016/j.jse.2007.02.058. [DOI] [Google Scholar]
- 49.Werner B.S., Chaoui J., Walch G. The influence of humeral neck shaft angle and glenoid lateralization on range of motion in reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1726–1731. doi: 10.1016/j.jse.2017.03.032. [DOI] [PubMed] [Google Scholar]
- 50.Werner B.S., Chaoui J., Walch G. Glenosphere design affects range of movement and risk of friction-type scapular impingement in reverse shoulder arthroplasty. Bone Joint J. 2018;100-B:1182–1186. doi: 10.1302/0301-620x.100b9.bjj-2018-0264.r1. [DOI] [PubMed] [Google Scholar]
- 51.Wiater B.P., Koueiter D.M., Maerz T., Moravek J.E., Jr., Yonan S., Marcantonio D.R., et al. Preoperative deltoid size and fatty infiltration of the deltoid and rotator cuff correlate to outcomes after reverse total shoulder arthroplasty. Clin Orthop Relat Res. 2015;473:663–673. doi: 10.1007/s11999-014-4047-2. [DOI] [PMC free article] [PubMed] [Google Scholar]