Shoulder instability is a common orthopedic condition, especially among younger active individuals. The overall incidence in the United States has been cited as 0.8 per 1000 person-years.8 Although dislocations of the shoulder can occur as isolated injuries, there are many examples in the literature that demonstrate other injuries that may be present in conjunction with a dislocation event. One reported case series by Plachel et al described a phenomenon known as the “triple dislocation fracture,” in which they described fractures of the glenoid rim, greater tuberosity, and coracoid process associated with dislocations of the shoulder.15 Often these injuries can be overlooked at the time of injury because of limited imaging and pain that can be easily ascribed to the dislocation event, preventing further investigation.9,12 The importance of recognizing a coracoid fracture at the time of initial injury can have important implications on whether to allow early mobilization of a stable shoulder or dictate possible surgical interventions needed for patients at risk of further shoulder instability.2,19
Garcia-Elias and Salo described a patient who sustained a shoulder dislocation and was placed in a sling and lost to follow-up until 7 weeks later when persistent pain and further imaging demonstrated a coracoid fracture.9 After 3 more weeks of immobilization, the fracture fragment showed no signs of healing and went on to require surgical intervention.9
Lal et al presented a patient with multiple dislocation events who underwent an open Bankart procedure.13 Although both radiographs and magnetic resonance imaging (MRI) were read as negative before the procedure, a coracoid fracture was found intraoperatively and required fixation. A retrospective review of the imaging was completed, and some deformity of the coracoid was noted on initial imaging that may have been evidence of a fractured coracoid.13
Coracoid fractures and shoulder dislocations
Coracoid fractures themselves are relatively uncommon injuries and account for approximately 1% of all fractures, 3% to 13% of all scapular fractures, and 5% of fractures about the shoulder.4,18 The mechanism of these fractures can include avulsion injuries, fatigue fractures, direct contact injuries, and glenohumeral dislocation events.1,12,13 There have been various proposed methods of injury to the coracoid after a shoulder dislocation. One is direct traction of the coracobrachialis and short head of biceps tendon which attaches to the coracoid cause enough force to cause a fracture of the coracoid.12,18 The other mechanism is that a direct traumatic blow from the dislocated humeral head leads to acute fracture of the coracoid.9,13,18 An important consideration in evaluating the coracoid fracture is its relationship with the coracoclavicular ligaments. According to the Ogawa classification, fractures that occur posterior to the insertion of the coracoclavicular ligaments are classified as type I, and those anterior to the insertion are type II14 (Fig. 1). In a case series by Eyres et al, they included a more specific classification system that divides coracoid fractures into type I through type V, including a modifier, A or B, to denote the presence or absence of injury to the clavicle or ligamentous attachments to the scapula6 (Fig. 1). The location and size of the coracoid fracture have important indications on the method of treatment and possible surgical interventions to address shoulder instability.
Figure 1.
Classification system of coracoid fractures by Ogawa et al14 and Eyres et al.5 (Top) Ogawa type I and type II. (C-CL is the attachment of the coracoclavicular ligament.) (Bottom) Eyres classification; type I: tip or epiphyseal fracture, type II: mid-process, type III: basal fracture, type IV: superior body of scapula involved, type V: fracture extension into glenoid.
We encountered three cases in which patients who had anterior shoulder dislocations with associated coracoid fractures each presented with a similar defect in the anterior-superior glenoid that we propose may be a pathognomonic sign that a coracoid fracture is present and should be further investigated if this pattern of bone loss is seen.
Case 1
A 16-year-old male fell while playing ice hockey and sustained an anterior shoulder dislocation that was reduced by the athletic trainer on the ice. The patient stated that he hit his elbow on the ice driving his shoulder superiorly. He was placed in a sling by the emergency department and sent for follow-up with orthopedic surgery. Radiographs obtained on initial presentation demonstrated a displaced, Ogawa type II coracoid fracture (Fig. 2). A computed tomography (CT) (Fig. 3) and MRI scan (Fig. 4) were then obtained which showed anterior bone loss with a small bony Bankart and edema around the base of the coracoid. Arthroscopic evaluation confirmed the anterior-superior glenoid bone loss (Fig. 5). This patient went on to have a successful arthroscopic Latarjet performed using the fractured coracoid to complete the bony portion of the procedure.3
Figure 2.

Axillary view showing displacement of coracoid fracture, bony Bankart lesion, and loss of anterior glenoid contour.3
Figure 3.

Three-dimensional reconstruction from computed tomography demonstrating anterior-superior bone loss as well as fracture of coracoid base.3
Figure 4.

Sagittal magnetic resonance image showing edema surrounding coracoid base fracture.
Figure 5.
Arthroscopic view demonstrating anterior-superior and inferior bone loss of glenoid.3
Case 2
A 16-year-old male presented to the emergency department after experiencing a seizure and was found to have an anteriorly dislocated left shoulder. Postreduction imaging demonstrated satisfactory reduction of the shoulder but also a displaced coracoid fracture (Fig. 6, Fig. 7). A CT scan was obtained and confirmed a displaced, Ogawa type II coracoid fracture (Fig. 8). CT imaging of the shoulder was also noted to have a small defect on the anterior-superior glenoid. An MRI was obtained and identified a Hill-Sachs lesion of the humeral head and a labral tear with associated anterior labral periosteal sleeve avulsion lesion (Fig. 9). In light of the patient's coracoid fracture and high likelihood of repeat seizure and possible dislocation, the decision was made for the patient to undergo an open Latarjet procedure, also using the fractured coracoid piece as the anterior bone block. During the initial arthroscopic evaluation before converting to an open Latarjet, the glenoid bone defect was once again seen (Fig. 10).
Figure 6.

Anterio-posterior shoulder demonstrating successful reduction and displaced coracoid fracture.
Figure 7.

Scapular Y demonstrating displaced coracoid fracture.
Figure 8.

Three-dimensional reconstruction demonstrating anterior-superior bone loss of the glenoid.
Figure 9.

Sagittal magnetic resonance image demonstrating displaced coracoid fracture with anterior-superior glenoid bone loss.
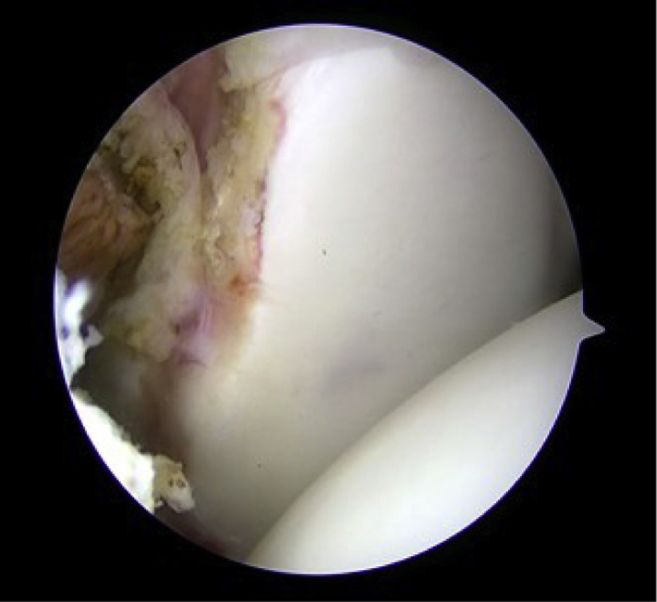
Figure 10.
Arthroscopic images demonstrating anterior-superior glenoid bone loss.
Case 3
A 38-year-old male with a known traumatic brain injury and seizure disorder presented to the orthopedic clinic with a chief complaint of right shoulder pain. Imaging demonstrated a right anterior shoulder dislocation with a displaced coracoid fracture (Fig. 11; Fig. 12). Patient was a poor historian, and his family believed the dislocation possibly occurred 4 days before presentation. He was sent to the emergency department for reduction and told to follow-up with the shoulder specialist. Upon return back to the clinic, he was found to have a persistent anterior-inferior, locked shoulder dislocation. A CT shoulder reconstruction demonstrated a defect in the anterior-superior potion of the glenoid, a large, engaging Hill-Sachs lesion, and a small displaced, Ogawa type II coracoid fracture (Fig. 13; Fig. 14). The patient went on to have open allograft reconstruction of the humeral head and glenoid (Fig. 15), as well as open reduction internal fixation of the coracoid fracture (Fig. 16). A talar head allograft was used to match the curvature of the humeral head, and distal tibial allograft was used to augment the anterior-superior glenoid bone defect.
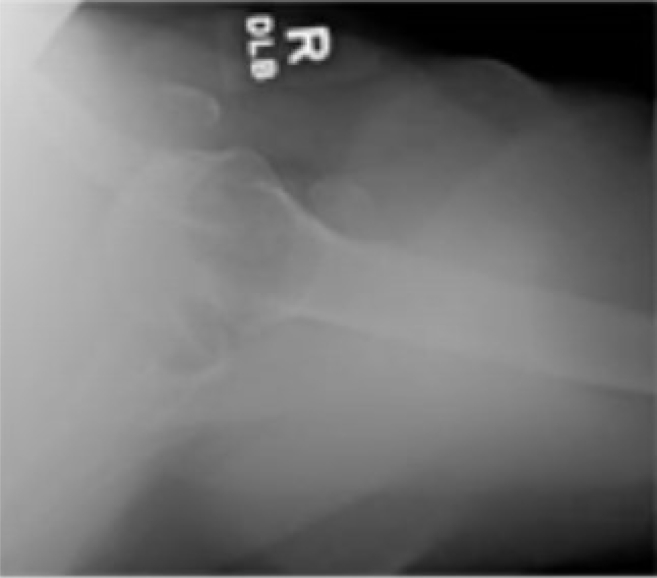
Figure 11.
Anterio-posterior shoulder demonstrating anterior inferior shoulder dislocation.
Figure 12.
Axillary view demonstrating anterior shoulder dislocation with associated coracoid fracture.
Figure 13.
Sagittal computed tomography scan demonstrating large Hill-Sachs lesion as well as anterior-superior glenoid bone loss.
Figure 14.
Computed tomography shoulder reconstruction demonstrating anterior-superior glenoid bone loss with associated coracoid fracture.
Figure 15.
Open distal tibial allograft augmentation of glenoid bone defect.
Figure 16.
Open reduction and internal fixation of coracoid fracture.
Discussion
Pain often is a limiting factor in the quality of imaging obtained acutely after a dislocation event. However, without proper imaging, associated injuries including coracoid fractures may be missed.2,13,19 The coracoid itself is best visualized on axillary view, anteroposterior cephalic tilt view, Stryker notch view, and Goldberg views (Fig. 17, A and B).1,10,19
Figure 17.
(A) Axillary view of shoulder with no obvious fracture. (B) Goldberg view of shoulder with 20° cephalad angulation and 20° posterior oblique positioning demonstrating a transverse fracture at the base of the coracoid ( ) as well as fracture of the acromion (
) as well as fracture of the acromion ( ).8
).8
For case 2, no dedicated shoulder imaging was obtained before reduction by the emergency department. Initial imaging was limited to an anterio-posterior chest radiograph (Fig. 18) which demonstrated the anterior dislocation but did not diagnose the acute coracoid fracture. It was not until the postreduction imaging was obtained (Figs. 6 and 7) that the displaced coracoid fracture was appreciated. However, a retrospective review of the anterio-posterior chest radiograph (Fig. 19) did confirm the fracture of the coracoid despite being missed on initial examination by the emergency department.
Figure 18.

Anterio-posterior chest x-ray of case 2, demonstrating anterior dislocation of humeral head, with missed fracture of the coracoid.
Figure 19.
Enhanced imaging of anterio-posterior chest demonstrating acute, displaced coracoid fracture (arrow).
It is our hypothesis that the coracoid fractures in these cases occurred from a direct blow by the humeral head traveling anteriorly and superiorly.9,13 As evidence to support this theory, we believe the anterior-superior bone loss seen on the 3D reconstruction CTs (Figs. 3, 8, 14) is likely pathognomonic and shows the path the humeral head travels toward the coracoid. The 3D reconstructions along with the intraoperative photos in all cases (Figs. 5, 10 and 15) demonstrate similar bone loss in the anterior-superior glenoid, once again supporting the evidence that the humeral head causes trauma to the anterior-superior portion of the glenoid on its pathway to making contact with the coracoid.
Although rare, coracoid fractures after anterior shoulder dislocations have been reported before in the literature. Verma et al presented a case report in 2016 of a patient who suffered multiple shoulder dislocations, and on preoperative CT scan, a coracoid fracture was seen as well as glenoid bony deficiency, that were initially missed on plain radiographs.5 However, they do not comment on the specific location of the bony deficiency of the glenoid. Based off our findings, we hypothesize that the deficit would likely be in the anterior-superior region, similar to the cases we present.
Identifying associated injuries that may occur in conjunction with a shoulder instability event is important in creating appropriate and individualized treatment plans for the patient and their needs. In the same way, accurately assessing the presence and extent of labral, capsular, Bankart, or Hill-Sachs lesions can dictate your operative vs. nonoperative planning11,16; being able to recognize and diagnose a coracoid fracture is equally vital to appropriately manage shoulder dislocations.15
Similar to a Segond fracture in the knee being associated with an anterior cruciate ligament injury,4,7,17 we believe the bone loss pattern seen on the anterior-superior glenoid after an anterior dislocation is likely pathognomonic for a fracture of the coracoid process. A missed coracoid fracture may lead to persistent pain after a shoulder dislocation due to delayed healing from lack of appropriate immobilization.9 In case 1 and case 2, the coracoid fracture was identified and used to address future instability events via an arthroscopic and open Latarjet, respectively.3 This allowed the patients to both be protected from future instability and avoid possible pain from non-union of the coracoid if left untreated. In case 3, the coracoid fractured was felt to be too small to perform a successful Latarjet, and instead open augmentation with distal tibial allograft was used to address the glenoid bone loss. However, the coracoid fracture in case 3 was treated with open reduction and internal fixation with a single partially threaded screw.
Of note, some controversy exists in regard to how to properly manage traumatic shoulder dislocations in patients with history of seizures. In 2 of the 3 cases we present, the instability events were preceded by a seizure. Traditionally, in the setting of seizure, it has been taught that posterior shoulder dislocations are more common.5 However, in a study by Buhler and Geber, in 26 patients with epilepsy, the incidence of anterior and posterior dislocation was each 50%.5 Repeat seizures can lead to recurrent instability and potential failures of treatment. Ersen et al looked at 11 patients with epilepsy and 54 without who underwent Latarjet procedures.5 They found the functional results were similar between the two groups. However, the redislocation rate in the epilepsy group was 9% vs. 1.8% in the nonepileptic group. Despite medical treatment, seizures can be uncontrolled in up to 30% of patients with epilepsy.5 It is important to have an open discussion with patients about the risk and benefits of undergoing Latarjet or other bony stabilizing procedures in the setting of shoulder instability brought about by seizures.
Conclusion
In the setting of acute anterior shoulder dislocations, one should have a high index of suspicion for an associated coracoid fracture if anterior-superior glenoid bone loss is noted on CT imaging. Subsequently, if no CT is obtained or available and anterior-superior bone loss is noted during an arthroscopic or open procedure, a coracoid fracture should be ruled out with advanced imaging. Missed coracoid fractures can be a cause of persistent shoulder pain even after successful reduction of an anterior shoulder dislocation. Understanding that the pattern of anterior-superior glenoid bone loss may be pathognomonic for a coracoid fracture can help guide clinicians in the acute and long-term management of anterior shoulder dislocations.
Disclaimers
Funding: No funding was disclosed by the author(s).
Conflicts of interest: Dr. Bishai is a paid consultant for Arthrex, Johnson and Johnson, Smith and Nephew, Stryker, Anika Therapeutics, Pacira, Trice Medical, Zimmer Biomet, BD, and Xiros North America. None of these relationships are potential conflicts of interest with this article. The other authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Patient consent: Obtained.
Footnotes
Institutional review board approval was not required for this case report.
References
- 1.Archik S., Nanda S.N., Tripathi S., Choudhari A., Rajadhyaksha H. An Isolated Displaced Fracture of the Coracoid Process Treated with Open reduction and internal fixation - A Case Report and Review of Literature. J Orthopaedic Case Rep. 2016;6:37–39. doi: 10.13107/jocr.2250-0685.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benchetrit E., Friedman B. Fracture of the coracoid process associated with subglenoid dislocation of the shoulder. A case report. J Bone Joint Surg Am. 1979;61:295–296. [PubMed] [Google Scholar]
- 3.Bishai S.K., Hinz J.A., Ward L.C., Martinez M.M. Management of Traumatic Coracoid Fracture and Anterior Shoulder Instability With a Modified Arthroscopic Latarjet Technique. Arthrosc Tech. 2020;9:e1341–e1348. doi: 10.1016/j.eats.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Daggett M., Busch K., Sonnery-Cottet B. Surgical Dissection of the Anterolateral Ligament. Arthrosc Tech. 2016;5:e185–e188. doi: 10.1016/j.eats.2015.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Erşen A., Bayram S., Birişik F., Atalar A.C., Demirhan M. The effectiveness of the Latarjet procedure for shoulder instability in patients with epilepsy. Orthop Traumatol Surg Res. 2017;103:1277–1282. doi: 10.1016/j.otsr.2017.08.017. [DOI] [PubMed] [Google Scholar]
- 6.Eyres K.S., Brooks A., Stanley D. Fractures of the coracoid process. J Bone Joint Surg Br. 1995;77:425–428. [PubMed] [Google Scholar]
- 7.Flores D.V., Smitaman E., Huang B.K., Resnick D.L. Segond fracture: an MR evaluation of 146 patients with emphasis on the avulsed bone fragment and what attaches to it. Skeletal Radiol. 2016;45:1635–1647. doi: 10.1007/s00256-016-2479-3. [DOI] [PubMed] [Google Scholar]
- 8.Galvin J.W., Ernat J.J., Waterman B.R., Stadecker M.J., Parada S.A. The Epidemiology and Natural History of Anterior Shoulder Instability. Curr Rev Musculoskelet Med. 2017;10:411–424. doi: 10.1007/s12178-017-9432-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garcia-Elias M., Salo J.M. Non-union of a fractured coracoid process after dislocation of the shoulder. A case report. J Bone Joint Surg Br. 1985;67:722–723. doi: 10.1302/0301-620X.67B5.4055868. [DOI] [PubMed] [Google Scholar]
- 10.Goldberg R.P., Vicks B. Oblique angled view for coracoid fractures. Skeletal Radiol. 1983;9:195–197. doi: 10.1007/BF00352554. [DOI] [PubMed] [Google Scholar]
- 11.Hill H.A., Sachs M.D. The grooved defect of the humeral head: A frequently unrecognized complication of dislocations of the shoulder joint. Radiology. 1940;35:690–700. [Google Scholar]
- 12.Kennedy N.I., Ferrari M.B., Godin J.A., Sanchez G., Provencher M.T. Repair of an Isolated Coracoid Fracture With Suture Anchor Fixation. Arthrosc Tech. 2017;6:e1715–e1719. doi: 10.1016/j.eats.2017.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lal H., Bansal P., Sabharwal V.K., Mawia L., Mittal D. Recurrent shoulder dislocations secondary to coracoid process fracture: a case report. J Orthop Surg (Hong Kong) 2012;20:121–125. doi: 10.1177/230949901202000127. [DOI] [PubMed] [Google Scholar]
- 14.Ogawa K., Yoshida A., Takahashi M., Ui M. Fractures of the coracoid process. J Bone Joint Surg Br. 1997;79:17–19. doi: 10.1302/0301-620x.79b1.6912. [DOI] [PubMed] [Google Scholar]
- 15.Plachel F., Schanda J.E., Ortmaier R., Auffarth A., Resch H., Bogner R. The “triple dislocation fracture”: Anterior shoulder dislocation with concomitant fracture of the glenoid rim, greater tuberosity and coracoid process—a series of six cases. J Shoulder Elbow Surg. 2017;26:E278–E285. doi: 10.1016/j.jse.2017.01.022. [DOI] [PubMed] [Google Scholar]
- 16.Provencher M.T., Frank R.M., Leclere L.E., Metzger P.D., Ryu J.J., Bernhardson A., Romeo A.A. The Hill-Sachs lesion: diagnosis, classification, and management. J Am Acad Orthop Surg. 2012;20:242–252. doi: 10.5435/JAAOS-20-04-242. [DOI] [PubMed] [Google Scholar]
- 17.Segond P. Recherches cliniques et expérimentales sur les épanchements sanguins du genou par entorse. Progres Med. 1879;7:297–341. [Google Scholar]
- 18.Verma N., Chahar D., Chawla A., Sreenivasan R., Pankaj A. Recurrent anterior instability of the shoulder associated with coracoid fracture - An unusual presentation. J Clin Orthop Trauma. 2016;7:99–102. doi: 10.1016/j.jcot.2016.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong-Chung J., Quinlan W. Fractured coracoid process preventing closed reduction of anterior dislocation of the shoulder. Injury. 1989;20:296–297. doi: 10.1016/0020-1383(89)90173-3. [DOI] [PubMed] [Google Scholar]