Abstract
Background
The ulnar collateral ligament (UCL) of the elbow is subject to repetitive stress in overhead throwing athletes. This can lead to morphologic changes at the bony attachments of the UCL and hypertrophy of the sublime tubercle. The purpose of this case series is to describe the surgical details and clinical outcomes of a series of competitive baseball pitchers with hypertrophic sublime tubercles who underwent UCL reconstruction (UCLR).
Methods
All baseball pitchers who were treated for UCL injuries with significant hypertrophy of the sublime tubercle on preoperative imaging were included in the series. Clinical history, preoperative imaging, intraoperative findings during UCLR, and postoperative outcomes measured with the Conway scale were described.
Results
Ten players (average age of 22.9 years [range 13-39]) were included (average follow-up 20.4 months [range 3-38 months]). Five patients also had symptoms of ulnar nerve compression, with 4 requiring transposition at the time of ULCR and 1 at 3 months postoperatively. Bony hypertrophy of the sublime tubercle was confirmed intraoperatively in all cases and excised before UCLR with the docking technique. Of the 7 patients with at least 12-month follow-up postoperatively, 6 had excellent outcomes, and 1 had a fair outcome.
Conclusion
Although UCLR in the setting of hypertrophic sublime tubercle can be more complex than typical UCLR, excellent outcomes are achievable with preoperative recognition and surgical planning.
Keywords: Ulnar collateral ligament, UCL, Sublime tubercle, Baseball pitcher, Ulnar collateral ligament reconstruction
Injury to the elbow ulnar collateral ligament (UCL) is a debilitating and potentially career-ending condition in elite throwing athletes.22 The anterior bundle of the UCL is the major ligamentous restraint against valgus stress of the elbow through a large arc of elbow motion and is subject to significant loads during the late cocking and early acceleration phases of throwing.11,12,23 Over the past 2 decades, there has been a significant increase in the number of UCL reconstructions (UCLRs) performed in Major League Baseball pitchers, with 25% of these pitchers having had previous UCLR.3
Furthermore, with increasing rates of youth and adolescent participation in sports, 15- to 19-year-old athletes now account for most UCLRs across all age groups.10 As athletes begin throwing from a younger age, repetitive microtrauma to the UCL, along with its bony attachments, are cumulative over years. This may lead to adaptive changes in local anatomy, particularly in the skeletally immature patient. Depending on the age and sex of the athlete, the medial epicondyle may not completely fuse until age 17 years in boys, and repetitive forces to the medial elbow likely affect the process of chondro-osseous transformation.21 Among adult elite overhead athletes, significant hypertrophy of the medial epicondyle has been described relative to controls.16
Hypertrophy of the UCL insertion at the ulnar sublime tubercle has not been well described in elite throwing athletes. It may develop in a similar fashion to hypertrophy of the medial epicondyle, or it may represent a distal avulsion of the ligament resulting in a nonunited bony fragment. Depending on the extent of hypertrophy, which likely exists along a spectrum with ossification of the distal UCL, ligament reconstruction in these patients requires preoperative recognition and planning, as the altered anatomy can be disorienting. Failure to consider sublime tubercle hypertrophy may result in nonanatomic reconstructions. The purpose of this case series was to describe 10 cases of significant sublime tubercle hypertrophy in baseball pitchers undergoing UCLR and to discuss pertinent intraoperative findings and techniques.
Materials and methods
This retrospective case series review was approved by our institutional review board (#2017-0083). Inclusion criteria were UCL injury requiring surgical reconstruction with concomitant sublime tubercle hypertrophy. Ten patients who had surgery between 2015 and 2021 were included in this series. All UCLRs were performed using the docking technique.1,2,24 All patients had preoperative examination findings consistent with UCL insufficiency, including pain with valgus stress and a positive moving valgus stress test. If the patient had preoperative ulnar nerve symptoms (including numbness of the ring and small fingers, wasting of the hand intrinsics, etc.), an anterior subcutaneous ulnar nerve transposition was also performed. Preoperative X-ray and magnetic resonance imaging were obtained on each patient to evaluate the extent of sublime tubercle hypertrophy (Figs. 1 and 2). Arthroscopic débridement of posteromedial osteophytes was carried out concomitantly with ligament reconstruction if preoperative examination and imaging studies were consistent with posteromedial impingement. One patient also presented with findings consistent with pronator syndrome; therefore, open median nerve decompression was performed at the time of UCLR.
Figure 1.
Representative preoperative anterior-posterior radiographs of the elbow showing hypertrophy of the sublime tubercle for patient 1 (A), patient 2 (B), patient 5 (C), patient 6 (D), patient 7 (E), and patient 9 (F).
Figure 2.
Preoperative coronal gradient-echo magnetic resonance images for patient 2, showing complete UCL rupture with hypertrophy of the sublime tubercle. UCL, ulnar collateral ligament.
Postoperative outcomes were assessed with the Conway scale.5 Excellent outcomes were defined as return to play at the previous level of competition for at least 1 year after surgery. A good result was defined as return to play at a lower level or the ability to throw daily batting practice for at least 1 year after surgery. A fair result was defined as return to play at a recreational level. Finally, a poor outcome was defined as inability to return to throwing. Patient symptoms and physical examination were used to detect any cases of recurrent elbow instability.
Surgical technique
All patients underwent UCLR using the docking technique with either palmaris or hamstring autograft. The technique was similar to previous docking techniques that have been previously published with the addition of careful removal of the hypertrophic bone at the sublime tubercle. After dissection through the flexor carpi ulnaris, the native UCL is identified at the medial epicondyle. The amount and quality of native ligament tissue remaining can be variable based on the chronicity of the injury and how large the hypertrophic bone at the sublime tubercle is (Fig. 3). If any native ligament tissue remains, this can be followed distally to identify the excess bone that needs to be removed at the sublime tubercle. If the tissue is degenerated or no longer there, excess bone should be removed to be confluent with the surrounding ulna. Tissue surrounding the excess bone is removed to define the extent of hypertrophy. This can be accomplished using an osteotome positioned from distal to proximal on the deep aspect of the bony prominence. The surgeon should remove enough bone to restore the native sublime tubercle anatomy. Care should be taken to ensure that the underlying bone of the native sublime tubercle is not compromised, as this may prevent the surgeon from forming an adequate bony bridge between the ulnar tunnels. After bony resection (Fig. 4), the docking technique is performed as has been previously described (Fig. 5). Postoperative protocol is also the same as has been published in previous techniques.
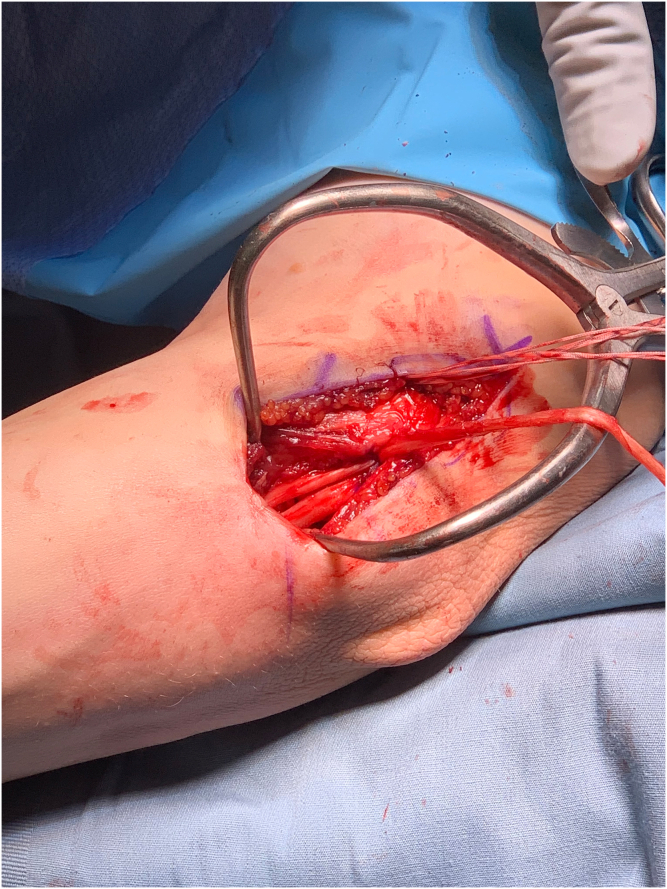
Figure 3.
The patient positioned is supine on the operating table and with the right upper extremity on a hand table and the medial elbow shown. After incision, subcutaneous dissection, and FCU muscle split, the underlying native UCL is exposed (A). After removal of the tissue on the hypertrophic sublime tubercle, the excess bone can be visualized clearly (B). FCU, flexor carpi ulnaris; UCL, ulnar collateral ligament.
Figure 4.
Excess bone is removed from the sublime tubercle (A), which leaves a space where the native UCL typically is (B). UCL, ulnar collateral ligament.
Figure 5.
Standard docking technique using hamstring autograft was performed.
Results
Ten patients met inclusion criteria and were included in the series (Table I). Hypertrophy of the sublime tubercle was demonstrated with preoperative radiographs and magnetic resonance imaging in all patients (Figs. 1 and 2). The mean age was 22.9 ± 7.7 years (range 13-39) at the time of surgery. All patients were baseball pitchers, with 4 in minor league professional baseball, 1 collegiate athlete, 3 high school pitchers, 1 former professional who injured his UCL while playing baseball recreationally, and 1 high-level recreational pitcher.
Table I.
Patients with hypertrophic sublime tubercle who underwent UCL reconstruction.
| Patient number | Age | Level | Concurrent procedures | Graft | Follow-up (mo) | Outcome | Conway outcome scale |
|---|---|---|---|---|---|---|---|
| 1 | 25 | Minor leagues | Palmaris longus autograft | 28 | Playing recreationally | Fair | |
| 2 | 18 | Minor leagues | Elbow arthroscopy, posterior trochlear débridement | Palmaris longus autograft | 34 | Pitching professionally in minor leagues | Excellent |
| 3 | 24 | Minor leagues | Elbow arthroscopy, posteromedial osteophyte débridement, ulnar nerve transposition | Palmaris longus autograft | 15 | Returned to minor leagues | Excellent |
| 4 | 26 | Minor leagues | Gracilis autograft | 26 | Returned to pitching in minor league baseball | Excellent | |
| 5 | 13 | High school | Palmaris longus autograft | 26 | Returned to pitching at previous level | Excellent | |
| 6 | 30 | Former professional, injured playing recreationally | Ulnar nerve transposition | Semitendinosus autograft | 38 | Returned to playing recreationally | Excellent |
| 7 | 18 | High school | Elbow arthroscopy, open median nerve decompression for pronator syndrome | Palmaris longus autograft | 15 | Reoperation at 3 mo postop for lysis of adhesions/manipulation under anesthesia, ulnar nerve transposition, returned to previous level of competition | Excellent |
| 8 | 20 | College | Elbow arthroscopy and débridement, ulnar nerve transposition | Gracilis autograft | 11 | Returned to throwing | Pending |
| 9 | 16 | High school, national teams | Ulnar nerve transposition | Palmaris longus autograft | 9 | Throwing 105 feet with no symptoms, progressing with physical therapy with plan for fall baseball, able to return to play but not as pitcher | Pending |
| 10 | 39 | Recreational | Gracilis autograft | 6 | Started throwing progression with no symptoms | Pending |
Four patients underwent concomitant elbow arthroscopy with intra-articular débridement. Five patients had symptoms consistent with ulnar neuropathy, with 4 patients undergoing ulnar nerve transposition at the time of UCLR, and 1 (patient 7) needing a second surgery at 3 months after UCLR for ulnar nerve transposition, manipulation under anesthesia, and lysis of adhesions. Of note, patient 7 also presented preoperatively with symptoms consistent with pronator syndrome and underwent open median nerve decompression at the time of initial UCLR. In 6 of the 10 cases, palmaris longus autograft was used to reconstruct the UCL with the docking technique. In 2 cases, after the resection of the hypertrophied sublime tubercle, a particularly large void was noted and addressed with either doubling over the palmaris longus graft (patient 1) or using a larger semitendinosus autograft (patient 6). Gracilis autograft was used for the remaining 3 patients.
The mean follow-up was 20.4 months (range 3-38; Table I). Three patients (8, 9, and 10) were less than 12 months removed from UCLR; thus, their final outcomes on the Conway scale were undetermined at the time of writing. Of the remaining 7 patients, 6 were able to return to pitching at or above their previous level and thus achieved excellent outcomes on the Conway scale. Patient 1 was unable to return to his previous level of play (minor league professional baseball) and had a fair outcome on the Conway scale. No patients complained of residual symptoms or had findings of instability on examination postoperatively. There were no cases of recurrent sublime tubercle hypertrophy on postoperative X-rays.
Discussion
In this case series of 10 baseball pitchers undergoing UCLR in the setting of significant sublime tubercle hypertrophy, outcomes demonstrated that with appropriate preoperative recognition and planning, a high rate of return to sport was achievable.
The elbow UCL experiences repetitive microtrauma during baseball pitching,11,23,26 and for professional baseball pitchers, this is a chronic process that has been ongoing for a number of years. Given trends toward increasing youth participation in high-level sports in recent years, the incidence of elbow UCL injury requiring surgical reconstruction among 15- to 19-year-olds is increasing at a rate of 9.12% per year,10 with overall favorable outcomes after UCLR in adolescent athletes.14 Concurrently over the past 2 decades, there has been a significant increase in the number of UCLR performed in Major League Baseball pitchers, from one reconstruction in 1986 to 32 in 2012.9,17
As with musculoskeletal structures elsewhere in the body, repetitive valgus loads in the elbow have the potential to lead to remodeling of bony anatomy, especially in developing athletes. In a computed tomography study of elite overhead athletes compared with control patients, Makhni et al showed that the medial epicondyles in elite athletes were significantly larger than those found in controls.16 Using quantitative geometric analysis, they found the medial epicondyle to be larger in total volume as well as anterior-posterior thickness, lending support to the theory that chronic repetitive stresses at the elbow can result in bony hypertrophy.16 In adolescent boys, the medial epicondyle ossification center may not be fused until up to age 17 years, and these patients may be especially susceptible to alterations in bony morphology due to repetitive throwing.21
This process of adaptive hypertrophy is less established at the sublime tubercle, with only a few small case series published in the literature. Although there is no ossification center at the sublime tubercle, repetitive traction on the developing periosteum and/or healed avulsion fractures may result in a hypertrophic sublime tubercle. In a retrospective radiographic review of 42 patients with heterotopic calcification of the UCL, Mulligan et al reported 2 cases of confluent ossification of the distal UCL, similar in appearance to the cases presented in this series. In their series, a positive association was found between heterotopic calcification in any location within the UCL with partial or complete tears of the UCL.18 Salvo et al presented a case series of acute avulsion fractures of the sublime tubercle in 8 overhead throwing athletes. Two of the 8 patients demonstrated healing of their avulsion fracture with nonoperative management, whereas the other 6 had residual medial elbow pain limiting their performance and underwent either UCL repair or reconstruction. They report that all patients were able to return to their previous level of activity following treatment (Salvo 2002). Glajchen et al report a case series of 3 college baseball players who had calcific densities adjacent to the sublime tubercle. Two of these 3 athletes underwent UCL reconstruction without any follow-up presented in this series (Glajchen 1998). Therefore, these injuries may represent nonunited avulsion fractures or hypertrophic calcification from repetitive valgus loads across the UCL.
It is important to recognize hypertrophy of the sublime tubercle in the preoperative imaging work-up of athletes indicated for surgery. The surgeon must restore the native morphology of the sublime tubercle at the time of surgery by adequately removing the excess bone while not compromising the integrity of the ligament insertion site. Alterations in the bony morphology and fixation points of the reconstructed ligament may have significant effects on ligament isometry and tension during maximal load. It is also important to assess bone quality when excising the hypertrophied bone, as the remaining bony bed of the ligamentous footprint may be more cancellous in nature. In cases of insufficient bone quality after hypertrophic sublime tubercle excision, the use of interference screw fixation on the ulna with docking of the graft on the humeral side (the DANE TJ technique) or docking the graft on the ulna and securing the sutures over a bony bridge (double docking technique) may be considered.6,8 In addition, after the resection of the hypertrophied sublime tubercle, a large bony or soft tissue void may be encountered. This may potentially be addressed with the use of a larger graft, such as semitendinosus, or doubling over the palmaris longus graft if there is adequate length.
With modern surgical techniques, excellent outcomes can be achieved in up to 90% of primary UCLRs.25 When counseling patients regarding prognosis and expected postoperative outcomes, however, it is important to recognize that certain cohorts are at increased risk of inferior outcomes. Revision reconstruction,7,15 the presence of posteromedial chondromalacia,19 and combined flexor-pronator mass and UCL injuries20 have all been associated with worse outcomes after UCLR. Although outcomes in this series were mostly excellent at intermediate-term follow-up, patients with hypertrophic sublime tubercles may be another cohort with poorer prognoses, and further studies in this area are warranted.
When evaluating a throwing athlete with medial elbow pain, it is also important to carefully examine other medial elbow structures. Ulnar nerve irritation often presents solely as medial elbow pain without neurologic findings and can be mistaken for ligamentous injury.4,13 Ulnar nerve compression is often a dynamic phenomenon in pitchers, as pressure in the cubital tunnel can significantly increase during the pitching motion. Although not documented in the literature, a hypertrophic sublime tubercle could potentially further compress the ulnar nerve in the cubital tunnel, so ulnar nerve transposition may be indicated at the time of UCLR in these patients.
This case series is limited by its small sample size and lack of long-term functional outcomes. Nevertheless, this is a rare entity even among competitive baseball pitchers, and further studies quantitatively examining the morphology of the sublime tubercle in elite throwing athletes are warranted.
Conclusion
In this series of 10 baseball pitchers with hypertrophic sublime tubercles who underwent UCLR and had short-term follow-up of at least 12 months, 6 of the 7 patients had excellent outcomes and were able to return to their previous level of pitching, whereas one patient had a fair outcome. UCLR in patients with hypertrophic sublime tubercles are complex cases that require adequate preoperative radiographic work-up, careful assessment of any concomitant pathology, and surgical planning, with the ability to alter the surgical technique based on intraoperative findings.
Disclaimers:
Funding: No funding was disclosed by the authors.
Conflicts of interest: Michael C. Fu is a consultant at Stryker and serves as an editorial board member of Arthroscopy Journal and HSS Journal. Joshua S. Dines has received royalties from Conmed, Arthrex, and Livatec; is a consultant at and on speakers bureau of Arthrex; and he holds ownership of ViewFi. Brandon J. Erickson is a board or committee member of AAOS, American Orthopaedic Society for Sports Medicine, American Shoulder and Elbow Surgeons; is a paid consultant for Arthrex, Inc; has received research support from DePuy, A Johnson & Johnson Company, Linvatec, Smith & Nephew, and Stryker; and is on editorial or governing board of PLOS One. Dean N. Papaliodis is a consultant at DePuy/Mitek. David Altchek is a consultant at Stryker and Arthrex. The other authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
The Hospital for Special Surgery Institutional Review Board approved this study (#2017-0083).
References
- 1.Bowers A.L., Dines J.S., Dines D.M., Altchek D.W. Elbow medial ulnar collateral ligament reconstruction: clinical relevance and the docking technique. J Shoulder Elbow Surg. 2010;19:110–117. doi: 10.1016/j.jse.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 2.Camp C.L., Dines J.S., Voleti P.B., James E.W., Altchek D.W. Ulnar collateral ligament reconstruction of the elbow: the docking technique. Arthrosc Tech. 2016;5:e519–e523. doi: 10.1016/j.eats.2016.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Conte S.A., Fleisig G.S., Dines J.S., Wilk K.E., Aune K.T., Patterson-Flynn N., et al. Prevalence of ulnar collateral ligament surgery in professional baseball players. Am J Sports Med. 2015;43:1764–1769. doi: 10.1177/0363546515580792. [DOI] [PubMed] [Google Scholar]
- 4.Conti M.S., Camp C.L., Elattrache N.S., Altchek D.W., Dines J.S. Treatment of the ulnar nerve for overhead throwing athletes undergoing ulnar collateral ligament reconstruction. World J Orthopedics. 2016;7:650–656. doi: 10.5312/wjo.v7.i10.650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Conway J.E., Jobe F.W., Glousman R.E., Pink M. Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am Vol. 1992;74:67–83. [PubMed] [Google Scholar]
- 6.Dines J.S., ElAttrache N.S., Conway J.E., Smith W., Ahmad C.S. Clinical outcomes of the DANE TJ technique to treat ulnar collateral ligament insufficiency of the elbow. Am J Sports Med. 2007;35:2039–2044. doi: 10.1177/0363546507305802. [DOI] [PubMed] [Google Scholar]
- 7.Dines J.S., Yocum L.A., Frank J.B., ElAttrache N.S., Gambardella R.A., Jobe F.W. Revision surgery for failed elbow medial collateral ligament reconstruction. Am J Sports Med. 2008;36:1061–1065. doi: 10.1177/0363546508314796. [DOI] [PubMed] [Google Scholar]
- 8.Erickson B.J., Bach B.R., Jr., Cohen M.S., Bush-Joseph C.A., Cole B.J., Verma N.N., et al. Ulnar Collateral Ligament Reconstruction: The Rush Experience. Orthopaedic J Sports Med. 2016;4 doi: 10.1177/2325967115626876. 2325967115626876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Erickson B.J., Gupta A.K., Harris J.D., Bush-Joseph C., Bach B.R., Abrams G.D., et al. Rate of return to pitching and performance after Tommy John surgery in Major League Baseball pitchers. Am J Sports Med. 2014;42:536–543. doi: 10.1177/0363546513510890. [DOI] [PubMed] [Google Scholar]
- 10.Erickson B.J., Nwachukwu B.U., Rosas S., Schairer W.W., McCormick F.M., Bach B.R., Jr., et al. Trends in Medial Ulnar Collateral Ligament Reconstruction in the United States: A Retrospective Review of a Large Private-Payer Database From 2007 to 2011. Am J Sports Med. 2015;43:1770–1774. doi: 10.1177/0363546515580304. [DOI] [PubMed] [Google Scholar]
- 11.Fleisig G.S., Andrews J.R., Dillman C.J., Escamilla R.F. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23:233–239. doi: 10.1177/036354659502300218. [DOI] [PubMed] [Google Scholar]
- 12.Floris S., Olsen B.S., Dalstra M., Sojbjerg J.O., Sneppen O. The medial collateral ligament of the elbow joint: anatomy and kinematics. J Shoulder Elbow Surg. 1998;7:345–351. doi: 10.1016/s1058-2746(98)90021-0. [DOI] [PubMed] [Google Scholar]
- 13.Hyman J., Breazeale N.M., Altchek D.W. Valgus instability of the elbow in athletes. Clin Sports Med. 2001;20:25–45. doi: 10.1016/s0278-5919(05)70245-3. viii. [DOI] [PubMed] [Google Scholar]
- 14.Jones K.J., Dines J.S., Rebolledo B.J., Weeks K.D., Williams R.J., Dines D.M., et al. Operative management of ulnar collateral ligament insufficiency in adolescent athletes. Am J Sports Med. 2014;42:117–121. doi: 10.1177/0363546513507695. [DOI] [PubMed] [Google Scholar]
- 15.Liu J.N., Garcia G.H., Conte S., ElAttrache N., Altchek D.W., Dines J.S. Outcomes in revision Tommy John surgery in Major League Baseball pitchers. J Shoulder Elbow Surg. 2016;25:90–97. doi: 10.1016/j.jse.2015.08.040. [DOI] [PubMed] [Google Scholar]
- 16.Makhni E.C., Khanna K., Simpson M.T., Redler L.H., Anakwenze O.A., Li R., et al. Medial Epicondyle Morphology in Elite Overhead Athletes: A Closer Look Using 3-Dimensional Computer Simulation. Orthopaedic J Sports Med. 2014;2 doi: 10.1177/2325967113517211. 2325967113517211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Makhni E.C., Lee R.W., Morrow Z.S., Gualtieri A.P., Gorroochurn P., Ahmad C.S. Performance, Return to Competition, and Reinjury After Tommy John Surgery in Major League Baseball Pitchers: A Review of 147 Cases. Am J Sports Med. 2014;42:1323–1332. doi: 10.1177/0363546514528864. [DOI] [PubMed] [Google Scholar]
- 18.Mulligan S.A., Schwartz M.L., Broussard M.F., Andrews J.R. Heterotopic calcification and tears of the ulnar collateral ligament: radiographic and MR imaging findings. AJR Am J Roentgenol. 2000;175:1099–1102. doi: 10.2214/ajr.175.4.1751099. [DOI] [PubMed] [Google Scholar]
- 19.Osbahr D.C., Dines J.S., Rosenbaum A.J., Nguyen J.T., Altchek D.W. Does posteromedial chondromalacia reduce rate of return to play after ulnar collateral ligament reconstruction? Clin Orthopaedics Relat Res. 2012;470:1558–1564. doi: 10.1007/s11999-011-2132-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Osbahr D.C., Swaminathan S.S., Allen A.A., Dines J.S., Coleman S.H., Altchek D.W. Combined flexor-pronator mass and ulnar collateral ligament injuries in the elbows of older baseball players. Am J Sports Med. 2010;38:733–739. doi: 10.1177/0363546509351558. [DOI] [PubMed] [Google Scholar]
- 21.Pappas A.M. Elbow problems associated with baseball during childhood and adolescence. Clin Orthopaedics Relat Res. 1982:30–41. [PubMed] [Google Scholar]
- 22.Petty D.H., Andrews J.R., Fleisig G.S., Cain E.L. Ulnar collateral ligament reconstruction in high school baseball players: clinical results and injury risk factors. Am J Sports Med. 2004;32:1158–1164. doi: 10.1177/0363546503262166. [DOI] [PubMed] [Google Scholar]
- 23.Regan W.D., Korinek S.L., Morrey B.F., An K.N. Biomechanical study of ligaments around the elbow joint. Clin Orthopaedics Relat Res. 1991:170–179. [PubMed] [Google Scholar]
- 24.Smith G.R., Altchek D.W., Pagnani M.J., Keeley J.R. A muscle-splitting approach to the ulnar collateral ligament of the elbow. Neuroanatomy and operative technique. Am J Sports Med. 1996;24:575–580. doi: 10.1177/036354659602400503. [DOI] [PubMed] [Google Scholar]
- 25.Watson J.N., McQueen P., Hutchinson M.R. A systematic review of ulnar collateral ligament reconstruction techniques. Am J Sports Med. 2014;42:2510–2516. doi: 10.1177/0363546513509051. [DOI] [PubMed] [Google Scholar]
- 26.Werner S.L., Fleisig G.S., Dillman C.J., Andrews J.R. Biomechanics of the elbow during baseball pitching. J Orthopaedic Sports Phys Ther. 1993;17:274–278. doi: 10.2519/jospt.1993.17.6.274. [DOI] [PubMed] [Google Scholar]