Abstract
Background
Approaches to surgical treatment to cubital tunnel syndrome include simple decompression, decompression with medial epicondylectomy, and decompression with anterior transposition of the ulnar nerve. Transposition of the ulnar nerve involves decompression and transposition of the nerve anteriorly to a subcutaneous, intramuscular, or submuscular position. However, transposing the ulnar nerve to subcutaneous plane renders it more susceptible to external trauma. Hence, this technique article introduces the use of a modified fascial sling.
Methodology
The modified fascial sling technique for anterior transposition of the ulnar nerve involves careful dissection to identify the ulnar nerve, decompression of the nerve, then transposition of the ulnar nerve anterior to the medial epicondyle. An AlloWrap (Stryker, Kalamazoo, MI, USA) is first wrapped around the ulnar nerve, followed by wrapping a fascial sling fashioned from the flexor carpi ulnaris fascia. A prospective case series for this surgical technique was conducted. Wilcoxon signed-rank test compared preoperative and postoperative qDASH-9 scores, an abbreviated questionnaire to assess functional limitations of the upper limb.
Results
Five patients were included in this study, with a mean duration of follow-up of 530.4 days. The mean QuickDASH-9 functional disability score was 36.5 ± 25.1 preoperatively and 20.6 ± 12.8 postoperatively, demonstrating statistically significant improvement (P = .008).
Conclusion
The modified fascial sling technique for anterior transposition of the ulnar nerve was developed to address the complications of perineural adhesions after transposition causing tethering of the ulnar nerve. At the same time, the fascial sling prevents posterior subluxation of the ulnar nerve back to its original location, thereby reducing the risk of recurrent symptoms.
Keywords: AlloWrap, Cubital tunnel syndrome, Fascial sling, Questionnaire, Surgical techniques, Ulnar nerve transposition
Cubital tunnel syndrome results from chronic compression or repeated trauma to the ulnar nerve, most commonly occurring within the cubital tunnel, although compression at other sites can occur. Diagnosis is often made based on signs and symptoms and confirmed electrodiagnostically via nerve conduction study and electromyography to identify abnormal ulnar nerve conduction across the elbow.
The ulnar nerve originates from the medial cord of the brachial plexus, entering the posterior compartment of the arm deep to the arcade of Struthers. It then enters the cubital tunnel, bounded laterally by the olecranon, medially by the medial epicondyle, superficially by the Osborne ligament, with the floor formed by the joint capsule and posterior band of the medial collateral ligament of the elbow. The ulnar nerve then passes between the two heads of the flexor carpi ulnaris to enter the forearm.
Cubital tunnel syndrome patients typically present with paresthesia and/or radiating pain along the medial forearm to the palmar and dorsal aspects of the hand and ulnar one and a half fingers. In severe cases, they may have weakness of wrist flexion, flexion of the distal interphalangeal joints of the ring and little fingers, and/or finger abduction and adduction. On examination, there may be wasting of the hypothenar eminence, mild clawing of the little and ring finger, positive Froment’s sign (adductor pollicis muscle weakness), Wartenberg sign (third palmar interosseous muscle weakness), reproduction of sensory symptoms on elbow flexion, and Tinel’s sign along the course of the ulnar nerve.
Compression is often the principal mechanism resulting in cubital tunnel syndrome. Possible sites of compression include the arcade of Struthers, cubital tunnel, Osborne’s ligament, and fascia of the flexor carpi ulnaris. Elbow flexion exacerbates structural restriction by changing the shape of the cubital tunnel from an oval to an ellipse, thereby narrowing the canal by 55% and increasing intraneural pressure.2,22 Elbow movement also results in further stretching and sliding of the ulnar nerve within the cubital tunnel, thereby causing nerve irritation. Presence of other structural pathologies, such as osteophytes, soft tissue masses, snapping medial border of the triceps, or synovitis at the elbow joint, may contribute to a narrower cubital tunnel. Previous injuries to the ulnar nerve or cubitus valgus may also cause tethering of the nerve, putting it at risk of traction injuries.
Nonsurgical treatment includes elbow splinting,3 lifestyle modifications, physiotherapy, analgesia, and corticosteroid injections. In the context of severe symptoms and signs or failure of conservative treatment, surgical intervention may be considered. This article will provide a broad overview of existing surgical techniques and introduce the modified fascial sling technique for ulnar nerve transposition, which has been practiced in our institution.
Common surgical techniques
The surgical technique is influenced by the underlying pathology and site of compression. Broadly, approaches to surgical treatment include simple decompression, decompression with medial epicondylectomy, and decompression with anterior transposition of the ulnar nerve.
Simple decompression of the cubital tunnel, which can be done open or endoscopically, involves making an incision overlying the ulnar nerve to divide the constricting fascia and Osborne’s ligament, thereby relieving the compressive forces. Advantages include no devascularization of the ulnar nerve, shorter operative time, and avoiding scarring, kinking, and compression at secondary sites that are associated with nerve transposition. The smaller skin incision also has a faster healing and is more aesthetically appealing. In patients who have more severe symptoms, simple decompression, via either open or endoscopic methods, may be insufficient.
Classic medial epicondylectomy was first described by King and Morgan in 1950.12 Simple decompression is performed, followed by exposure of the medial epicondyle and detachment of the common flexor origin. The medial epicondyle is osteotomized from the metaphyseal-diaphyseal junction to the distal supracondylar ridge, with the remaining bony edge smoothened. The common flexor origin is then repaired to the periosteum. Compared to simple decompression, medial epicondylectomy allows the ulnar nerve to subluxate anteriorly, thus relieving prior pressure and traction on the ulnar nerve within the cubital tunnel, yet preserving the gliding tissues surrounding the nerve and the ulnar nerve blood supply. In a study by Hicks et al, patients who had simple decompression and medial epicondylectomy had a statistically significant reduction in strain of the ulnar nerve postoperatively, as compared to no significant reduction in strain for patients who had a simple decompression with no medial epicondylectomy.9 However, complications of medial epicondylectomy include medial instability of the elbow due to detachment of the anteromedial collateral ligament, valgus elbow instability if >40% of the medial epicondyle is removed, loss of the protective prominence of the medial epicondyle, postoperative pain, ulnar nerve subluxation over the remnant medial epicondyle, and weakness related to partial detachment of the common flexor origin of the forearm.17 Hence, a modification, first reported by Le Viet in 1991,13 was introduced, whereby a frontal partial medial epicondylectomy is utilized to preserve the protective function of the medial epicondyle for the ulnar nerve. With this technique, no cases of ulnar nerve injury or subluxation, medial elbow instability, or weakness of the flexor muscles of the forearm were observed at six months’ follow-up.17
Transposition of the ulnar nerve involves decompression and transposition of the nerve anteriorly to a subcutaneous, intramuscular, or submuscular position. The first successful anterior transposition was reported by Curtis in 1898.5 A human cadaveric study by Gelberman et al7 found traction of the ulnar nerve during flexion of the elbow to be a major contributor to increased intraneural pressures. Hence, advocates of transposition argue that simple decompression is insufficient to address dynamic compression of the ulnar nerve during elbow movement. However, it has been argued that transposition requires extensive dissection of the ulnar nerve, and thus puts the ulnar nerve vascularity at risk.16
Transposing the ulnar nerve to the subcutaneous plane places the nerve superficial to the common flexor origin, rendering it more susceptible to external trauma, especially in patients with minimal subcutaneous tissue. The nerve is also predisposed to subluxation to its prior position. This can be mitigated by a fascial sling,4 which is the technique that will be described in this study, or a vascularized adipose flap.21 For intramuscular transposition, a channel is cut in the flexor pronator muscles to accommodate the ulnar nerve intramuscularly. However, there is a significant risk of scarring and recurrence of ulnar nerve compression. Lastly, submuscular transposition, first described by Learmonth in 1942,14 entails placing the ulnar nerve deep into the common flexor muscle group after dividing the common flexor origin, adjacent to the median nerve.
Materials and methods
A retrospective case series was conducted. All patients who underwent cubital tunnel release with ulnar nerve transposition using the fascial sling technique from November 2018 to January 2022 by the authors were included. A nerve conduction study was performed to confirm the diagnosis. Ultrasound and/or magnetic resonance imaging were used to evaluate for any underlying pathology.
Age, gender, hand dominance, details regarding presentation, operation, and follow-up were collected from hospital medical records. Telephone interviews were conducted in May 2022 using the QuickDASH-9 questionnaire (Table I; DASH = disabilities of the arm, shoulder and hand).6 The QuickDASH-9 questionnaire was chosen in view of its feasibility and practicality in administrating a 9-item questionnaire over the telephone, its unidimensional structure, high correlation with the original DASH questionnaire, high reliability, internal consistency, and responsiveness.6 A score of 0 represented no functional disability, while 99 represented the greatest possible functional impairment. A preoperative qDASH score was also taken preoperatively. Improvement of symptoms postoperatively was assessed.
Table I.
QuickDASH-9 questionnaire.6
| No difficulty | Mild difficulty | Moderate difficulty | Severe difficulty | Unable | |
|---|---|---|---|---|---|
| 1. Open a tight or new jar. | 0 | 1 | 2 | 3 | 4 |
| 2. Do heavy household chores (e.g., wash walls, floors). | 0 | 1 | 2 | 3 | 4 |
| 3. Carry a shopping bag or briefcase. | 0 | 1 | 2 | 3 | 4 |
| 4. Wash your back. | 0 | 1 | 2 | 3 | 4 |
| 5. Use a knife to cut food. | 0 | 1 | 2 | 3 | 4 |
| 6. Recreational activities in which you take some force or impact through your arm, shoulder, or hand (e.g., golf, hammering, tennis, etc.) | 0 | 1 | 2 | 3 | 4 |
| Not at all |
Slightly |
Moderately |
Quite a bit |
Extremely |
|
| 7. During the past week, to what extent has your arm, shoulder, or hand problem interfered with your normal social activities with family, friends, neighbors or groups? | 0 | 1 | 2 | 3 | 4 |
| Not at all |
Slightly limited |
Moderately limited |
Very limited |
Unable |
|
| 8. During the past week, were you limited in your work or other regular daily activities as a result of your arm, shoulder, or hand problem? | 0 | 1 | 2 | 3 | 4 |
| None |
Mild |
Moderate |
Severe |
Extreme |
|
| 9. Arm, shoulder, or hand pain. | 0 | 1 | 2 | 3 | 4 |
This questionnaire asks about your symptoms as well as your ability to perform certain activities. Please answer every question, based on your condition in the last week, by circling the appropriate number. If you did not have the opportunity to perform an activity in the past week, please make your best estimate of which response would be the most accurate. It doesn’t matter which hand or arm you use to perform the activity; please answer based on your ability regardless of how you perform the task.
Rate your ability to do the following activities in the last week by circling the number below the appropriate response.
A QuickDASH-9 score may not be calculated if there is greater than 1 missing item.
QuickDASH-9 score = (sum × 1.1) × 5/2, a missing response is added as the average of the remaining.
Statistical analysis was performed using Statistical Product and Service Solutions Version 22.0. Wilcoxon signed-rank test compared preoperative and postoperative qDASH-9 scores, with P value <.05 taken to be statistically significant.
Modified fascial sling surgical technique
Cubital tunnel release with anterior transposition of the ulnar nerve using the fascial sling technique is performed under general anesthesia with the patient in a supine position. We shall now describe a modification of the fascial sling technique with the use of an AlloWrap (Stryker, Kalamazoo, MI, USA), with the aim of diminishing postoperative perineural scarring. The operated upper limb is placed on a Mayo table with the arm externally rotated, shoulder abducted at 90°, and elbow partially flexed to allow ease of access to the ulnar nerve.
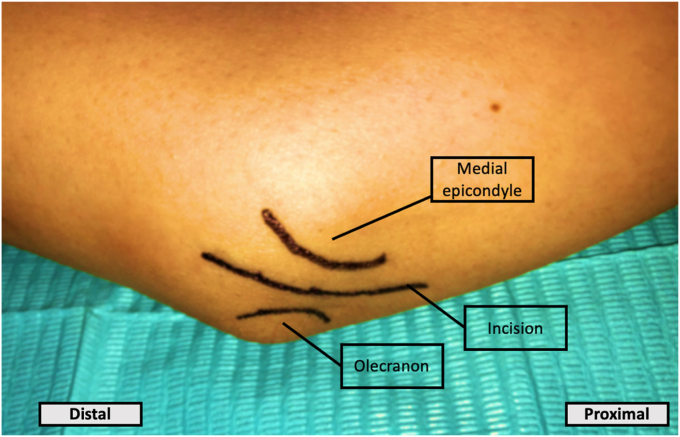
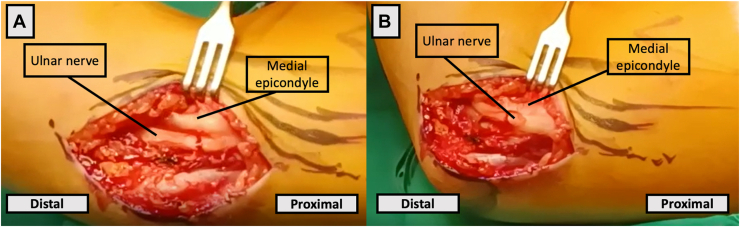
The olecranon and medial epicondyle, anatomic landmarks for the cubital tunnel, are marked out on the skin (Fig. 1). A 5-centimeter curvilinear longitudinal incision over the cubital tunnel is made. Osborne’s ligament is identified through blunt dissection and is carefully divided to expose the ulnar nerve. Throughout the dissection process, the medial brachial cutaneous nerve and medial antebrachial cutaneous nerve need to be protected to avoid inadvertent transection resulting in the development of painful neuromas. Subluxation of the ulnar nerve is confirmed intraoperatively under direct visualization when flexing and extending the elbow (Fig. 2).
Figure 1.
Skin marking on the right elbow illustrating important landmarks (medial epicondyle and olecranon) and the surgical incision.
Figure 2.
(A) The ulnar nerve is identified posterior to the medial epicondyle of the humerus. (B) Subluxation of the ulnar nerve is observed during flexion of the elbow.
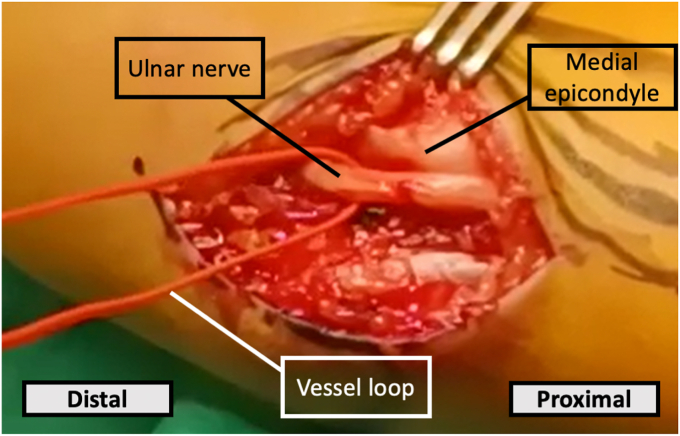
Identification of the ulnar nerve is assisted by placing it within a vessel loop to avoid inadvertent injury to the nerve (Fig. 3).
Figure 3.
Vessel loop placed around the ulnar nerve to aid identification.
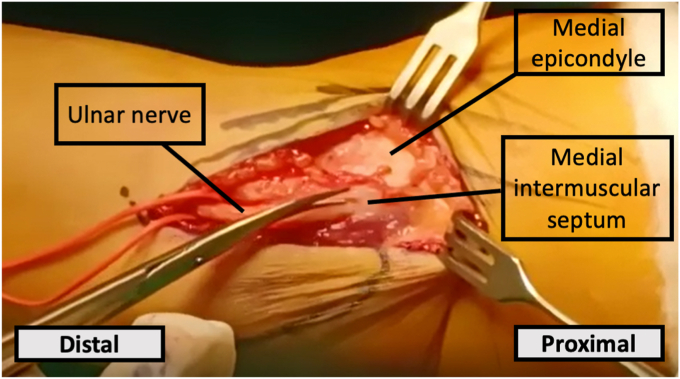
Dissection continues proximally to the arcade of Struthers, freeing the ulnar nerve from the medial intermuscular septum under direct visualization (Fig. 4). Distally, careful dissection continues until the fascia of the flexor carpi ulnaris is identified.
Figure 4.
Proximal dissection with division of the medial intermuscular septum.
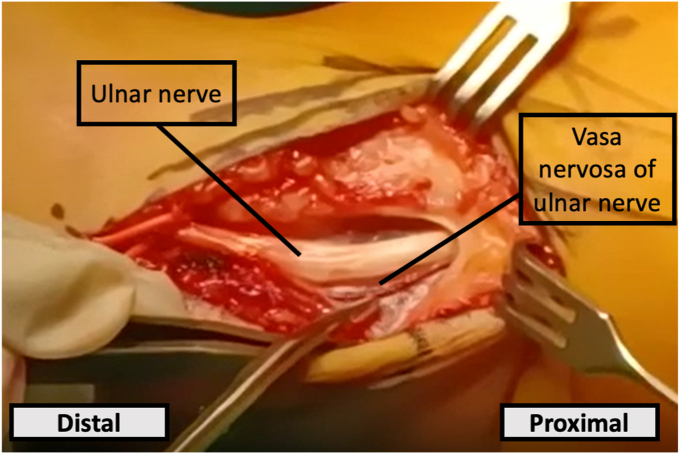
The ulnar nerve is transposed anterior to the medial epicondyle after adequate freeing of the nerve. Care should be taken to preserve the entire longitudinal blood supply of the ulnar nerve (Fig. 5).
Figure 5.
Vasa nervosa of the ulnar is identified and care is taken to preserve it.
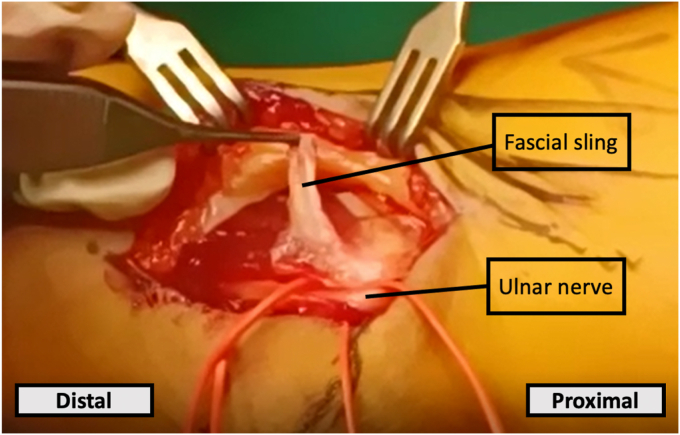
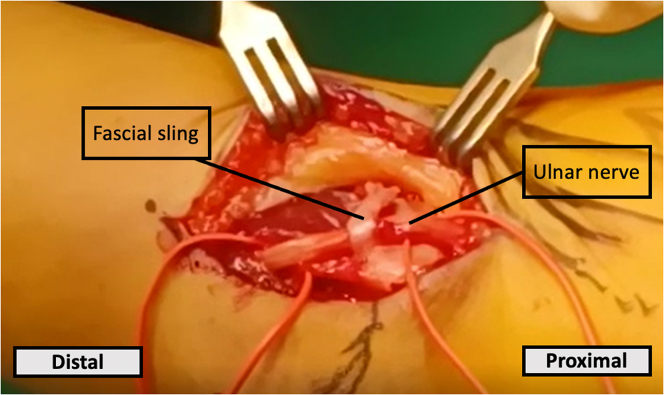
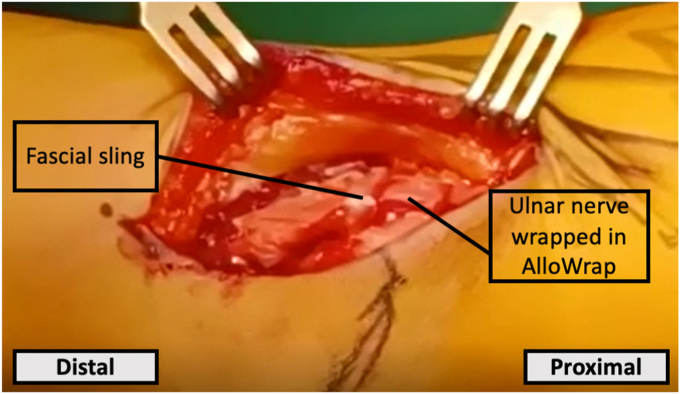
An approximately 1x2cm fascial sling is fashioned from the flexor carpi ulnaris fascia (Fig. 6). Existing fascial sling techniques entail wrapping the fascial sling directly around the ulnar nerve (Fig. 7).8,15
Figure 6.
Creation of fascial sling.
Figure 7.
Traditional application of the fascial sling by wrapping it around the ulnar nerve.
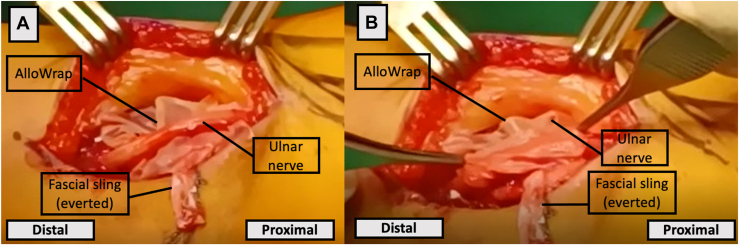
In our technique, we utilize the AlloWrap, a human amniotic membrane designed to provide a biologic barrier following surgical repair.1 It contains bioactive proteins that support wound healing. It aims to reduce friction between the ulnar nerve and fascial sling and minimize scarring at the transposition site, which can predispose to symptom recurrence. We apply the Allowrap loosely around the ulnar nerve (Fig. 8). The fascial sling is loosely placed over the Allowrap and secured with an absorbable suture (Fig. 9). After irrigating the wound, closure is done in layers with absorbable sutures. Adequate padded dressing is placed over the surgical site, with the upper limb placed in an arm sling. Postoperatively, patients underwent sessions by the physiotherapist and occupational therapist for nerve gliding exercises.
Figure 8.
(A) The fascial sling is everted. (B) AlloWrap is applied loosely around the ulnar nerve.
Figure 9.
The fascial sling is secured around the transposed ulnar nerve.
Results
Six patients were approached to be included in this study, whereby one patient declined to be included. The mean age was 54.4 years (range, 26-83 years). All were of Chinese ethnicity, with only one male patient. Ulnar nerve transposition was performed on the dominant arm in 80% of patients. Preoperatively, 20% presented with pain (visual analog scale [VAS] 6/10), 80% with paresthesia, 40% with hypoesthesia, and 80% with subjective weakness (Table II). On examination, 40% had muscle wasting of the hypothenar eminence and/or interossei, and 60% with Tinel’s sign positive over the cubital tunnel. All patients underwent ultrasound evaluation preoperatively, and 20% with additional magnetic resonance imaging evaluation. The mean preoperative QuickDASH-9 functional disability score was 36.5 ± 25.1.
Table II.
Comparison of preoperative vs. postoperative symptoms and signs.
| Symptom/sign | Presence of symptoms preoperatively (n = 5) | Improvement in symptoms postoperatively (n = 5) | P value |
|---|---|---|---|
| Pain | 1 | 1 | - |
| Paresthesia | 4 | 4 | - |
| Hypoesthesia | 2 | 2 | - |
| Subjective weakness | 4 | 4 | - |
| QuickDASH-9 score | 36.5 ± 25.1 | 20.6 ± 12.8 | .008 |
The mean duration of follow-up was 530.4 days (Table III). The patient who experienced pain preoperatively had persistent pain postoperatively, but with a reduction of VAS from a preoperative score of 6/10 to a postoperative score of 1/10. There was improvement in postoperative paresthesia, hypoesthesia, and subjective weakness in all the patients. Patients who were working preoperatively returned to work after an average of 83.3 days. None of the patients regretted undergoing surgery. The patients’ postoperative functional disability scored at 20.6 ± 12.8 on the QuickDASH-9, demonstrating statistically significant improvement (P = .008).
Table III.
Patient-specific data collected.
| Patient number | Nature of surgery | Duration of follow-up (days) | Time taken for return to work (days) | Preoperative qDASH-9 | Postoperative qDASH-9 |
|---|---|---|---|---|---|
| Patient 1 | Right cubital tunnel decompression and ulnar nerve transposition | 1274 | 68 | 9.3 | 3.1 |
| Patient 2 | Right cubital tunnel decompression and ulnar nerve transposition | 528 | NA (retired) | 55.7 | 27.8 |
| Patient 3 | Right cubital tunnel decompression, ulnar nerve transposition, arthroscopic capsular release, and removal of loose bodies | 451 | 60 | 11.0 | 11.0 |
| Patient 4 | Left cubital tunnel decompression and ulnar nerve transposition | 274 | 125 | 43.3 | 27.8 |
| Patient 5 | Right cubital tunnel decompression and ulnar nerve transposition | 125 | 80 | 63.3 | 33.0 |
| Mean ± SD | 530.4 ± 444.2 | 83.3 ± 29.0 | 36.5 ± 25.1 | 20.6 ± 12.8 |
SD, standard deviation.
Discussion
Anterior transposition of the ulnar nerve is an effective treatment for cubital tunnel syndrome patients who have failed nonsurgical management. A study by Huang et al demonstrated improvement in VAS and disability score (DASH),10 while a 67-month follow-up study by Stuebe et al found improvement in intrinsic muscle mass and functional outcomes.19 These findings are in keeping with our findings of improved patient symptoms, functional disability score (QuickDASH-9), and no patient regret with regard to undergoing the surgery.
Compared to simple decompression, ulnar nerve transposition entails a larger incision, more extensive dissection and manipulation of the ulnar nerve and surrounding structures. Hence, this puts a patient more at risk of complications such as nerve fibrosis, perineural adhesions, vascular compromise to the nerve, infection, scar sensitivity, posterior subluxation, and damage to surrounding nerves resulting in painful neuromas. However, a meta-analysis by Said et al comparing the outcomes between simple decompression and ulnar nerve transposition found no significant difference between the two methods in terms of eventual clinical outcome scores, and rate of revision surgery.18
Simple decompression is often considered in patients with milder forms of cubital tunnel syndrome and where there is a structural abnormality causing compression that can be removed surgically. On the other hand, anterior transposition is preferred in the context of ulnar nerve subluxation where there is chronic insult to the ulnar nerve from ongoing subluxation.
Clinical failure rates have been reported to be approximately 25% after anterior transposition of the ulnar nerve.20 In a systematic review by Kholinne et al,11 perineural scarring of 79% was found to be the most common intraoperative finding in patients who require revision surgery. Hence, the modified technique of using a fascial sling was developed to address the complications of perineural adhesions after transposition causing tethering of the ulnar nerve. At the same time, it prevents posterior subluxation of the ulnar nerve back to its original location, thereby reducing the risk of recurrent symptoms. However, scarring of the fascial sling and tethering become significant risk factors for symptom recurrence.21 Hence, placement of the AlloWrap aids to reduce scarring and tethering so as to optimize surgical outcomes.
This study describes a modified fascial sling technique with the addition of AlloWrap for anterior transposition of the ulnar nerve. At our institution, a 2 × 2 cm piece of AlloWrap costs US$750, which does increase the cost of the surgery to the patient. However, its use aims to reduce postoperative scarring rates and the need for revision surgery, and future cost-effectiveness analysis is required to analyze if our surgical technique with the AlloWrap results in overall cost savings. We hope that our proposed technique will decrease scarring of the ulnar nerve, but future study with a longer duration of follow-up, larger population size, objective measures for preoperative and postoperative assessment (eg, grip strength, two-point discrimination, and electrophysiological assessment), and comparisons between this modified technique and other techniques without the use of AlloWrap are needed to better assess the effectiveness of this proposed technique.
Disclaimers:
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this technique article.
References
- 1.AlloWrap D.S. 2022. https://www.stryker.com/us/en/trauma-and-extremities/products/allowrap-ds-amniotic-membrane.html Available from:
- 2.Apfelberg D.B., Larson S.J. Dynamic anatomy of the ulnar nerve at the elbow. Plast Reconstr Surg. 1973;51:76–81. [PubMed] [Google Scholar]
- 3.Assmus H., Antoniadis G., Bischoff C. Carpal and cubital tunnel and other, rarer nerve compression syndromes. Dtsch Arztebl Int. 2015;112:14–25. doi: 10.3238/arztebl.2015.0014. quiz 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Catalano L.W., 3rd, Barron O.A. Anterior subcutaneous transposition of the ulnar nerve. Hand Clin. 2007;23:339–344. doi: 10.1016/j.hcl.2007.06.005. vi. [DOI] [PubMed] [Google Scholar]
- 5.Curtis B. Traumatic ulnar neuritis - transplantation of the nerve. J Nerv Ment Dis. 1898;25:480. [Google Scholar]
- 6.Gabel C.P., Yelland M., Melloh M., Burkett B. A modified QuickDASH-9 provides a valid outcome instrument for upper limb function. BMC Musculoskelet Disord. 2009;10:161. doi: 10.1186/1471-2474-10-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gelberman R.H., Yamaguchi K., Hollstien S.B., Winn S.S., Heidenreich F.P., Jr., Bindra R.R., et al. Changes in interstitial pressure and cross-sectional area of the cubital tunnel and of the ulnar nerve with flexion of the elbow. An experimental study in human cadavera. J Bone Joint Surg Am. 1998;80:492–501. doi: 10.2106/00004623-199804000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Han H.H., Kang H.W., Lee J.Y., Jung S.-N. Fascia wrapping technique: a modified method for the treatment of cubital tunnel syndrome. The Scientific World J. 2014;2014 doi: 10.1155/2014/482702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hicks D., Toby E.B. Ulnar nerve strains at the elbow: the effect of in situ decompression and medial epicondylectomy. J Hand Surg Am. 2002;27:1026–1031. doi: 10.1053/jhsu.2002.35870. [DOI] [PubMed] [Google Scholar]
- 10.Huang W., Zhang P.-X., Peng Z., Xue F., Wang T.-B., Jiang B.-G. Anterior subcutaneous transposition of the ulnar nerve improves neurological function in patients with cubital tunnel syndrome. Neural Regen Res. 2015;10:1690–1695. doi: 10.4103/1673-5374.167770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kholinne E., Alsharidah M.M., Almutair O., Aljasser S., Alhothali W., Kwak J.-M., et al. Revision surgery for refractory cubital tunnel syndrome: a systematic review. Orthopaedics Traumatol Surg Res. 2019;105:867–876. doi: 10.1016/j.otsr.2019.03.020. [DOI] [PubMed] [Google Scholar]
- 12.King T., Morgan F. The treatment of traumatic ulnar neuritis. Mobilisation of the ulnar nerve at the elbow by removal of the medial epicondyle and adiacent bone. Aust N Z J Surg. 1950;20:33–42. doi: 10.1111/j.1445-2197.1950.tb03723.x. [DOI] [PubMed] [Google Scholar]
- 13.Le Viet D. Frontal partial epicondylectomy for release of the ulnar nerve in the elbow. Chirurgie. 1991;117:868–873. [PubMed] [Google Scholar]
- 14.Learmonth J. A technique for transplanting the ulnar nerve. Surg Gynecol Obstet. 1942;75:792–793. [Google Scholar]
- 15.Mahadevan D., David H.G. Anterior transposition of the ulnar nerve utilising a fascial sling. Ann R Coll Surg Engl. 2008;90:701. doi: 10.1308/rcsann.2008.90.8.701a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Messina A., Messina J.C. Transposition of the ulnar nerve and its vascular bundle for the entrapment syndrome at the elbow. J Hand Surg Br. 1995;20:638–648. doi: 10.1016/s0266-7681(05)80126-3. [DOI] [PubMed] [Google Scholar]
- 17.Popa M., Dubert T. Treatment of cubital tunnel syndrome by frontal partial medial epicondylectomy. A retrospective series of 55 cases. J Hand Surg Br. 2004;29:563–567. doi: 10.1016/j.jhsb.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 18.Said J., Van Nest D., Foltz C., Ilyas A.M. Ulnar nerve in situ decompression versus transposition for idiopathic cubital tunnel syndrome: an updated meta-analysis. J Hand Microsurg. 2019;11:18–27. doi: 10.1055/s-0038-1670928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stuebe A.M., Novak C.B., Mackinnon S.E. Recovery of ulnar innervated intrinsic muscles following anterior transposition of the ulnar nerve. Can J Plast Surg. 2001;9:25–28. [Google Scholar]
- 20.Tos P., Crosio A., Pugliese P., Adani R., Toia F., Artiaco S. Painful scar neuropathy: principles of diagnosis and treatment. Plast Aesthet Res. 2015;2:156–164. doi: 10.4103/2347-9264.160878. [DOI] [Google Scholar]
- 21.Verveld C.J., Danoff J.R., Lombardi J.M., Rosenwasser M.P. Adipose flap versus fascial sling for anterior subcutaneous transposition of the ulnar nerve. Am J Orthop (Belle Mead NJ) 2016;45:89–94. no doi. [PubMed] [Google Scholar]
- 22.Werner C.O., Ohlin P., Elmqvist D. Pressures recorded in ulnar neuropathy. Acta Orthop Scand. 1985;56:404–406. doi: 10.3109/17453678508994358. [DOI] [PubMed] [Google Scholar]