Abstract
Background
The goal of this study was to estimate the short-term (∼2 years) healthcare costs of failed primary arthroscopic rotator cuff repair (RCR) in the United States.
Methods
A review of current literature was performed to estimate the number of RCR performed in the United States in the year 2022 and the rate of progression of these patients to lose repair continuity, reach clinical failure, and progress to nonoperative intervention and revision procedures. A review of the current literature was performed to estimate the costs incurred by these failures over the ensuing 2-year postoperative time period.
Results
The direct and indirect healthcare costs of structural and clinical failure of primary RCR performed in 2022 are estimated to reach $438,892,670 in the short-term postoperative period. The majority of the costs come from the estimated $229,390,898 in nonoperative management that these patients undergo after they reach clinical failure.
Conclusion
The short-term healthcare costs of failed arthroscopic RCR performed in the United States in 2022 are predicted to be $438,892,670. Although RCR improves quality of life, pain, function, and is cost-effective, there remains great potential for reducing the economic burden of failed RCR repairs on the US society. Investments into research aimed to improve RCR healing rates are warranted.
Clinical Relevance
Although RCR improves quality of life, pain, function, and is cost-effective, this study provides evidence that there remains great potential for reducing the economic burden of failed RCR repairs on the US society. Investments into research aimed to improve RCR healing rates are warranted.
Keywords: Rotator cuff repair, Healthcare costs, Economics, Reoperation, Failure, Complications, Arthroscopy
Rotator cuff repair (RCR) is one of the most commonly performed orthopedic surgeries in the United States, and the incidence is predicted to steadily increase.10 The surge in RCR procedure volume is due in part to an increased prevalence of rotator cuff tears secondary to an aging population that has higher rates of rotator cuff disease.40 The total cost for RCR is not trivial.28
Even with the high costs associated with surgery, economic analyses of primary RCR indicate that operative treatment decreases the societal burden of rotator cuff disease more effectively than nonoperative management.30 The subjective and functional improvements demonstrated by studies of patients who underwent RCR encourage patients and surgeons to proceed with surgical management following rotator cuff disease diagnosis and exhausting conservative treatment options.2,12,38
Despite the positive functional outcomes and favorable societal economics of RCR surgery, multiple studies document postoperative failure of tendon-to-bone healing (ie, structural failure), with averages between 20% and 40% and wide ranges from 8%-94%.3,6,7,14,23,25,27,32,33,48 The heterogeneity of tear characteristics and repair techniques used in different studies is likely a critical driver of the variable results. Risk factors for primary RCR failure are both patient-specific and surgeon-related, with the latter being more modifiable.9,13,34,45 Structural RCR failure typically occurs within 1 year of the index surgery8,11 and is associated with suboptimal functional outcomes,49 which results in increased healthcare expenditures related to additional nonoperative treatment and/or revision surgery.15 Downstream healthcare expenditures accumulate as revision surgery is associated with higher failure rates, inferior clinical outcomes, and higher associated surgical costs compared to primary procedures.16,20
To date, there is little literature evaluating the economic impact of the relatively high failure rate of RCR. The goal of our study was to estimate the relative short-term healthcare costs (estimated as approximately 2 years) of failed primary arthroscopic RCR in the United States.
Materials and methods
This is an economic impact analysis of failed primary arthroscopic RCR performed in the United States in 2022 based on a review of the literature. Specifically, the data used for this economic analysis were obtained from the US Census Bureau and published, peer-reviewed literature.46
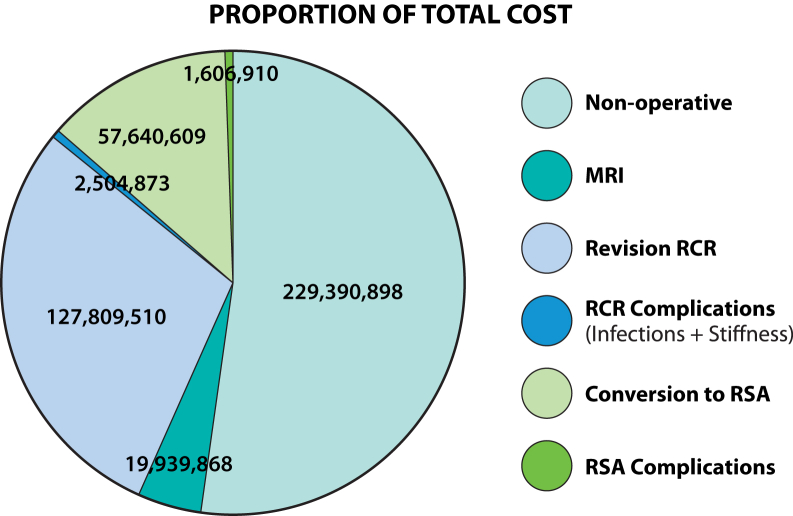
Incidence data
Colvin et al reported that the arthroscopic RCR incidence in the United States increased from 8/100,000 to 58/100,000 people, which represents an 11.5% annual increase between 1996 and 2006.10 Using these data, the incidence of arthroscopic RCR in the United States in 2022 was projected to reach 331/100,000 people with a national estimated demand of 1,119,734 primary RCR surgeries in 202244 (See Supplementary Appendix A for more detail).
Failure of primary RCR was defined as tendon discontinuity (ie, failure of tendon-to-bone healing) on advanced postoperative imaging. Based on previous literature, it is assumed that the RCR radiological failure rate would not change after the first postoperative year.17,24,33 It was assumed that if an RCR is in continuity at 1-year postoperatively, it will remain in continuity for the duration of the short-term postoperative period24 (See Supplementary Appendix B for more detail).
Based on the data reported by Sobhy et al, it was assumed that the overall retear rate (loss of structural integrity on advanced imaging) for modern repair techniques is 26.0%44 (See Supplementary Appendix C for more detail). Thus, it is calculated that 291,355 (26.0% of 1,119,734) primary RCRs performed in 2022 would not have tendon-to-bone continuity at 1 year following surgery.
Data reported by Kim et al and Namdari et al were averaged to estimate that 38.5% of primary arthroscopic RCR that structurally fail will also fail clinically21,37 (See Supplementary Appendix D for more detail). Thus, it is calculated that 112,172 (38.5% of 291,355) of primary RCR patients in 2022 will experience symptomatic tendon discontinuity in their first postoperative year.
Cost data
It is assumed that the 112,172 failed RCR patients would undergo 6 weeks of nonoperative management in an attempt to improve their shoulder symptoms. The estimated cost of nonoperative management of rotator cuff disease in 2022 was $2045 per patient30 (See Supplementary Appendix E for more detail). Thus, the short-term, total national healthcare expenditure for the initial nonoperative management of failed symptomatic primary RCRs performed in 2022 was estimated to be $229,390,898.
Patients who remain symptomatic following failed RCR may elect 1 of 3 management pathways in the short-term: (1) decline additional treatment, (2) proceed with revision RCR, or (3) proceed with reverse shoulder arthroplasty (RSA). Based on recent peer-reviewed published literature, the average rate of revision surgery (revision RCR or revision to RSA) in patients with structural and clinical failure of their index RCR was 8.1% (Namdari et al, 2 of 28; Shim et al, 4 of 44).37,41 Thus, 9348 (8.3% of 112,172) of primary RCR performed in 2022 are estimated to have failed and underwent subsequent revision RCR or RSA. Furthermore, all patients who underwent a revision operation were assumed to undergo shoulder magnetic resonance imaging (MRI) prior to this surgical intervention. Based on the study by Westermann et al, the average cost of a shoulder MRI is predicted to be $2134 per patient after adjusting for 9% inflation rate from 2017 to 2022.47 Thus, it is calculated that the cost of MRIs for these patients who failed primary RCR both structurally and clinically and elected to proceed with revision surgery cost $19,939,868.
Revision RCR
It is assumed that the vast majority of patients aged less than 65 years who failed their primary RCR and remained significantly symptomatic after an attempt at nonoperative management would be offered and choose to pursue revision RCR rather than RSA. Based on 2022 US Census data, 80% of the US population is under the age of 65 years.46 Based on those US Census population metrics, the mathematical extrapolations indicate that 7474 (80% of 9343) of patients who underwent primary RCR in 2022 will undergo revision RCR by the end of 2024.46 The estimated revision RCR surgery costs $17,098 per patient, which was also based on the 13.5% inflation adjusted primary RCR costs reported by Mather et al.30 Therefore, national economic burden of the estimated 7474 patients undergoing revision RCRs by the end of 2024 to treat failed primary RCR performed in 2022 following subsequent failed nonoperative management equates to $127,809,510.
Unfortunately, some of these revision RCR patients will have acute postoperative complications, such as infection and stiffness. The estimated national healthcare costs to manage just these 2 potential acute postoperative complications in 194 (2.6% of 7474) patients who underwent revision RCR after failed primary RCR performed in 2022 are $2,504,87330 (See Supplementary Appendix F for more detail). As the study herein focuses on short-term costs, it should be noted that we do not account for the predicted 11.1% patients who undergo revision RCR that may undergo a rerevision RCR surgery at an average 31 months after index procedure.34
Reverse shoulder arthroplasty
It was assumed that the vast majority of patients aged more than 65 years who failed their primary RCR and remained significantly symptomatic after an attempt at nonoperative management would be offered and would choose to pursue RSA rather than revision RCR.36 In 2022, the US Census Bureau reports that 20% of the US population is more than the age of 65 years.46 We computed that 1869 (20% of 9344) of patients who underwent primary RCR in 2022 would undergo RSA to treat their persistent or recurrent shoulder symptoms. The cost of RSA in 2022 was estimated to be $30,34019 (See Supplementary Appendix G for more detail). Therefore, the national economic burden of the estimated 1869 patients undergoing RSA by the end of 2024 to treat failed primary RCR performed in 2022 following subsequent failed nonoperative management equates to $57,640,609.
It is also important to consider the costs of potential acute complications after RSA surgery. It is estimated that approximately 45 (2.4% of 1869) patients will undergo a two-stage procedure for infection of RSAs performed after failed RCR at a cost of $42,470 per episode1,4 (See Supplementary Appendix H for more detail). Based on this computation, we project that the 2022 national periprosthetic joint infection costs stemming from RSA for failed RCR is $1,606,910. Furthermore, this current analysis focuses on short-term costs, and it does not account for patients who have RSA for irreparable cuff tears who may fail after the first year (which has been reported to be as high as 13%).39
This analysis does not account for any associated costs related to patients who elected to accept a poor clinical outcome by declining further treatment after failure of their primary RCR. In addition, it is assumed that patients who have clinical failure after revision RCR and/or RSA would not undergo a third level of surgical management within the short-term window of this financial analysis.
Results
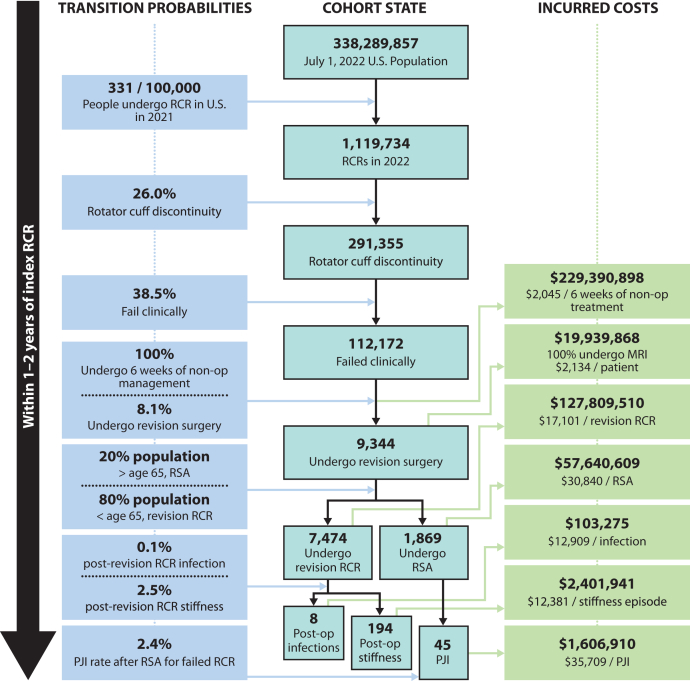
The majority of the short-term healthcare costs stemming from structural failure of primary arthroscopic RCR in the United States in 2022 come from the estimated $229,390,898 in nonoperative management that these patients undergo after they reach clinical failure (Fig. 1). The sources of the remaining economic burden are portrayed in Fig. 2.
Figure 1.
Portrays how the transition probabilities over the short-term postoperative period following RCR affect the residual patient cohort and demonstrate the estimated economic burden associated with each step of the model associated with costs. MRI, magnetic resonance imaging; RCR, rotator cuff repair; RSA, reverse shoulder arthroplasty.
Figure 2.
A pie graph depicting the proportion of healthcare costs from various expected expenditures stemming from structural failure of primary arthroscopic RCR performed in 2022. RCR, rotator cuff repair; RSA, reverse shoulder arthroplasty; MRI, magnetic resonance imaging; PJI, periprosthetic joint infection.
Overall, the direct and indirect healthcare costs of structural and clinical failure of primary RCR performed in 2022 are estimated to reach $438,892,670 in the short postoperative period of approximately 2 years (Fig. 2).
Discussion
This study found that the indirect and direct healthcare costs of failed primary RCR performed in the United States in the year 2022 will total nearly $440 million in the ensuing short-term postoperative period. The majority (52%) of this economic burden is incurred from attempted nonoperative management of these RCRs that have structural and clinical failure.
RCR has repeatedly been shown to provide greater improvement in pain and outcome scores compared to nonoperative management.26,35,39 Specifically, a randomized control trial by Moosmayer et al found that patients who underwent RCR have significantly better Constant Scores, American Shoulder and Elbow Surgeons score, pain-free abduction, and pain reduction at 12 months postoperatively compared to patients who were treated with conservative management.35 Furthermore, Heerspink et al found that disability and pain scores were significantly better in patients who underwent RCR compared to nonoperative management at 1 year postoperatively.26 Not only has RCR been shown to improve the function and quality of life for patients, there has also been shown to be a tremendous financial benefit to RCR. Mather et al demonstrated that RCR can greatly reduce the economic burden of this disease; specifically, RCRs performed each year in the United States save approximately $3.44 billion to our economy over the patients’ lifetimes.30 Despite these tremendous clinical and financial benefits of RCR, published literature reports structural failure of RCR to occur between 20% and 40% of the time (with ranges reported from 8%-94%).3,6,7,14,23,25,27,32,33 Sobhy et al pointed out the significant potential for improving the economic impact of this surgery due to its high structural failure rate of 26.0%.44 The analysis herein may be used by governing bodies and policy makers to justify further funding, research, and development into improving rotator cuff healing and therefore improving RCR outcomes. For example, based on the computational model developed in this study, for every 5% improvement in the rate of successful structural healing of primary RCR repairs in the United States per year, the short-term, downstream annual healthcare costs of structural failure would decrease by more than $84 million ($84,33,7562).
Although RCR with structural failure can still be associated with improved clinical outcomes, optimal outcomes are experienced by patients with an intact repair.26,49 In their systematic review of the peer-reviewed literature, Slabough et al reported that patients with healed rotator cuffs after RCR, based on radiologic evaluation, had statistically improved patient-reported outcomes and improved forward elevation motion and shoulder strength as compared to patients with nonhealed rotator cuffs.42 Cummins et al showed that nonhealed repairs most commonly failed via the tendon pulling through the sutures, suggesting that achieving tendon-to-bone healing rather than relying on the suture to maintain the integrity is imperative.11 Optimizing the biomechanical strength of the repair constructs,43 improving the apposition of the tendon to the original footprint,31 identifying patient risk factors for poor tendon-to-bone healing,18 augmentation with biologic patches,5 and idealizing postoperative therapy protocols are all primary goals of researchers and clinicians who are attempting to improve rotator cuff tendon-to-bone healing.
In addition to identifying that an improvement in the structural healing rates of primary RCR can substantially decrease the downstream economic burden of failure, this study also provides evidence that significant healthcare savings could potentially be obtained by optimizing the nonoperative management of patients with structural and clinical failure following primary RCR. Many patients will not respond favorably to nonoperative management, including physical therapy, after failed RCR. A recent 2020 study by Shim et al suggests that 51.9% of RCR patients presenting with substantial symptoms and tendon discontinuity following primary surgery will remain moderately to severely symptomatic following the initial nonoperative management.41 The study by Shim et al also provides evidence that patients with rotator cuff tendon discontinuity on postoperative MRI at 6 months that were larger than their index tear were more likely to have persistent, severe symptoms (pain visual analog scale > 3) after nonoperative management.41 Additionally, Kim et al identified that younger age, worker’s compensation claim, and lower education level were all patients’ factors that were associated with poorer outcomes after structural failure of RCR.22 Namdari et al performed a retrospective analysis of patients with structural failure of their RCR and found that patients who reported “labor-intensive occupations” represented a defined cohort at high risk for poor outcomes.37 Most recently, another study by Kim et al stratified patients with structural RCR failure based on satisfaction scores at final follow-up. They found that those with poor satisfaction scores after retear were more likely to be female, active smokers, and had retears that were equal or larger in size to their index tear.21 The aforementioned data can be used to identify symptomatic retears that are at risk for failing costly nonoperative management and for tailoring treatment toward those at risk.
Although this study was limited to healthcare costs associated with structural failure of RCR, it should be recognized that this model does not account for patients who will undergo primary RCR in 2022, experience structural failure, experience clinical failure, and decide not to undergo revision surgery (ie, live impaired). It has been shown that surgical management of rotator cuff syndrome results in an average improvement of 0.62 quality adjusted life years and estimated lifetime societal savings of $13,771 per patient.30 Further studies should be performed to assess the societal economic burden (missed workdays, disability, etc.) associated with RCR patients per year that may live with suboptimal outcomes after failure.
This study has several limitations. First, this study is based on a review of current literature; therefore, it relies on the accuracy of previously published content. Second, the transition rates extrapolated from available literature only allow for short-term cost analysis. For example, our analysis does not account for costly, suboptimal survivorship of RSA performed after failed RCR.29,39 It is intuitive that costs from failed RCR will continue to accrue through mid-term and long-term follow-up, but attempting a cost-analysis past the short-term follow-up relies more on expert opinion for transition rates and was considered to be less accurate. Next, we were unable to identify costs associated with the large number of patients who failed RCR and were predicted to live with persistent suboptimal outcomes, living in a suboptimal life state that may have costs associated with missed workdays and lower quality of life. Finally, it should be noted that this study does not account for patients who clinically fail RCR but have no evidence of repair failure on imaging (ie, failures in continuity). It is important to note that all of these limitations increase the risk for this study to underestimate the short-term costs of failed RCR.
Conclusion
The short-term healthcare costs of failed arthroscopic RCR performed in the United States in 2022 are predicted to be $438,892,670. Thus, the accumulated cost of short-term failures through 2026 is predicted to supersede $2 billion. Although RCR improves quality of life, pain, function, and is cost-effective, there remains great potential for reducing the economic burden of failed RCR repairs on the US society. Investments into research aimed to improve RCR healing rates are warranted.
Disclaimers
Funding: No funding was disclosed by the authors.
Conflicts of interest: Susan Marie Odum is a paid consultant for AAOS and Stryker and board or committee member of AAOS, Lumbar Spine Research Society, and PrideOrtho. Nady Hamid is a paid consultant for Stryker. Shadley Schiffern is a paid consultant for Medacta. Patrick M. Connor is a paid consultant for Lima, past-president and executive board member of NFL Physicians Society, and past chairman of the board of OrthoCarolina Research Institute. The other authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this literature review.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.xrrt.2023.03.008
Supplementary data
References
- 1.Baghdadi Y.M.K., Maradit-Kremers H., Dennison T., Ransom J.E., Sperling J.W., Cofield R.H., et al. The hospital cost of two-stage reimplantation for deep infection after shoulder arthroplasty. JSES Open Access. 2017;1:15–18. doi: 10.1016/j.jses.2017.02.001. 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhatia S., Greenspoon J.A., Horan M.P., Warth R.J., Millett P.J. Two-year outcomes after arthroscopic rotator cuff repair in recreational athletes older than 70 years. Am J Sports Med. 2015;43:1737–1742. doi: 10.1177/0363546515577623. [DOI] [PubMed] [Google Scholar]
- 3.Boileau P., Brassart N., Watkinson D.J., Carles M., Hatzidakis A.M., Krishnan S.G. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87:1229–1240. doi: 10.2106/JBJS.D.02035. [DOI] [PubMed] [Google Scholar]
- 4.Bois A.J., Knight P., Alhojailan K., Bohsali K.I. Clinical outcomes and complications of reverse shoulder arthroplasty used for failed prior shoulder surgery: a systematic review and meta-analysis. JSES Int. 2020;4:156–168. doi: 10.1016/j.jses.2019.10.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chalmers P.N., Tashjian R.Z. Patch augmentation in rotator cuff repair. Curr Rev Musculoskelet Med. 2020;13:561–571. doi: 10.1007/s12178-020-09658-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cho N.S., Lee B.G., Rhee Y.G. Arthroscopic rotator cuff repair using a suture bridge technique: is the repair integrity actually maintained? Am J Seports Med. 2011;39:2108–2116. doi: 10.1177/0363546510397171. [DOI] [PubMed] [Google Scholar]
- 7.Cho N.S., Yi J.W., Lee B.G., Rhee Y.G. Retear patterns after arthroscopic rotator cuff repair: single-row versus suture bridge technique. Am J Sports Med. 2010 Apr;38:664–671. doi: 10.1177/0363546509350081. [DOI] [PubMed] [Google Scholar]
- 8.Chona D.V., Lakomkin N., Lott A., Workman A.D., Henry A.C., Kuntz A.F., et al. The timing of retears after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2017;26:2054–2059. doi: 10.1016/j.jse.2017.07.015. [DOI] [PubMed] [Google Scholar]
- 9.Chung S.W., Oh J.H., Gong H.S., Kim J.Y., Kim S.H. Factors affecting rotator cuff healing after arthroscopic repair: osteoporosis as one of the independent risk factors. Am J Sports Med. 2011;39:2099–2107. doi: 10.1177/0363546511415659. [DOI] [PubMed] [Google Scholar]
- 10.Colvin A.C., Egorova N., Harrison A.K., Moskowitz A., Flatow E.L. National trends in rotator cuff repair. J Bone Joint Surg Am. 2012;94:227–233. doi: 10.2106/JBJS.J.00739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cummins C.A., Murrell G.A. Mode of failure for rotator cuff repair with suture anchors identified at revision surgery. J Shoulder Elbow Surg. 2003;12:128–133. doi: 10.1067/mse.2003.21. [DOI] [PubMed] [Google Scholar]
- 12.DeFranco M.J., Bershadsky B., Ciccone J., Yum J.K., Iannotti J.P. Functional outcome of arthroscopic rotator cuff repairs: a correlation of anatomic and clinical results. J Shoulder Elbow Surg. 2007;16:759–765. doi: 10.1016/j.jse.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 13.Duquin T.R., Buyea C., Bisson L.J. Which method of rotator cuff repair leads to the highest rate of structural healing? A systematic review. Am J Sports Med. 2010;38:835–841. doi: 10.1177/0363546509359679. [DOI] [PubMed] [Google Scholar]
- 14.Galatz L.M., Ball C.M., Teefey S.A., Middleton W.D., Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86-A:219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Heuberer P.R., Smolen D., Pauzenberger L., Plachel F., Salem S., Laky B., et al. Longitudinal long-term magnetic resonance imaging and clinical follow-up after single-row arthroscopic rotator cuff repair: clinical superiority of structural tendon integrity. Am J Sports Med. 2017;45:1283–1288. doi: 10.1177/0363546517689873. [DOI] [PubMed] [Google Scholar]
- 16.Higgins L. Cost-effectiveness of rotator cuff repair. Read at Arthroscopy Association of North America Annual Meeting; 2013 April 25-27. San Antonio, Texas. Paper #SS-28. 10.1016/j.arthro.2013.03.035. [DOI]
- 17.Iannotti J.P., Deutsch A., Green A., Rudicel S., Christensen J., Marraffino S., et al. Time to failure after rotator cuff repair: a prospective imaging study. J Bone Joint Surg Am. 2013;95:965–971. doi: 10.2106/JBJS.L.00708. [DOI] [PubMed] [Google Scholar]
- 18.Jensen A.R., Taylor A.J., Sanchez-Sotelo J. Factors influencing the reparability and healing rates of rotator cuff tears. Curr Rev Musculoskelet Med. 2020;13:572–583. doi: 10.1007/s12178-020-09660-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kang J.R., Sin A.T., Cheung E.V. Treatment of massive irreparable rotator cuff tears: a cost-effectiveness analysis. Orthopedics. 2017;40(1):e65–e76. doi: 10.3928/01477447-20160926-06. [DOI] [PubMed] [Google Scholar]
- 20.Keener J.D., Wei A.S., Kim H.M., Paxton E.S., Teefey S.A., Galatz L.M., et al. Revision arthroscopic rotator cuff repair: repair integrity and clinical outcome. J Bone Joint Surg Am. 2010;92:590–598. doi: 10.2106/JBJS.I.00267. [DOI] [PubMed] [Google Scholar]
- 21.Kim D.M., Jeon I.H., Yang H.S., Shin M.J., Park J.H., Kholinne E., et al. Poor prognostic factors in patients with rotator cuff retear. Orthop J Sports Med. 2021;9 doi: 10.1177/2325967121992154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim H.M., Caldwell J.M., Buza J.A., Fink L.A., Ahmad C.S., LU Bigliani, et al. Factors affecting satisfaction and shoulder function in patients with a recurrent rotator cuff tear. J Bone Joint Surg Am. 2014;96:106–112. doi: 10.2106/JBJS.L.01649. [DOI] [PubMed] [Google Scholar]
- 23.Kim K.C., Shin H.D., Cha S.M., Park J.Y. Comparisons of retear patterns for 3 arthroscopic rotator cuff repair methods. Am J Sports Med. 2014;42:558–565. doi: 10.1177/0363546514521577. [DOI] [PubMed] [Google Scholar]
- 24.Koh K.H., Laddha M.S., Lim T.K., Park J.H., Yoo J.C. Serial structural and functional assessments of rotator cuff repairs: do they differ at 6 and 19 months postoperatively? J Shoulder Elbow Surg. 2012;21:859–866. doi: 10.1016/j.jse.2011.05.027. [DOI] [PubMed] [Google Scholar]
- 25.Lafosse L., Brzoska R., Toussaint B., Gobezie R. The outcome and structural integrity of arthroscopic rotator cuff repair with use of the double-row suture anchor technique. Surgical technique. J Bone Joint Surg Am. 2008;90:275–286. doi: 10.2106/JBJS.F.00305. [DOI] [PubMed] [Google Scholar]
- 26.Lambers Heerspink F.O., van Raay J.J., Koorevaar R.C., van Eerden P.J., Westerbeek R.E., van 't Riet E., et al. Comparing surgical repair with conservative treatment for degenerative rotator cuff tears: a randomized controlled trial. J Shoulder Elbow Surg. 2015;24:1274–1281. doi: 10.1016/j.jse.2015.05.040. [DOI] [PubMed] [Google Scholar]
- 27.Lee Y.S., Jeong J.Y., Park C.D., Kang S.G., Yoo J.C. Evaluation of the risk factors for a rotator cuff retear after repair surgery. Am J Sports Med. 2017;45:1755–1761. doi: 10.1177/0363546517695234. [DOI] [PubMed] [Google Scholar]
- 28.Li L., Bokshan S.L., Ready L.V., Owens B.D. The primary cost drivers of arthroscopic rotator cuff repair surgery: a cost-minimization analysis of 40,618 cases. J Shoulder Elbow Surg. 2019;28:1977–1982. doi: 10.1016/j.jse.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 29.Makhni E.C., Swart E., Steinhaus M.E., Mather R.C., 3rd, Levine W.N., Bach B.R., Jr., et al. Cost-effectiveness of reverse total shoulder arthroplasty versus arthroscopic rotator cuff repair for symptomatic large and massive rotator cuff tears. Arthroscopy. 2016;32:1771–1780. doi: 10.1016/j.arthro.2016.01.063. [DOI] [PubMed] [Google Scholar]
- 30.Mather R.C., 3rd, Koenig L., Acevedo D., Dall T.M., Gallo P., Romeo A., et al. The societal and economic value of rotator cuff repair. J Bone Joint Surg Am. 2013;95:1993–2000. doi: 10.2106/JBJS.L.01495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meier S.W., Meier J.D. Rotator cuff repair: the effect of double-row fixation on three-dimensional repair site. J Shoulder Elbow Surg. 2006;15:691–696. doi: 10.1016/j.jse.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 32.Mihata T., Watanabe C., Fukunishi K., Ohue M., Tsujimura T., Fujiwara K., et al. Functional and structural outcomes of single-row versus double-row versus combined double-row and suture-bridge repair for rotator cuff tears. Am J Sports Med. 2011;39:2091–2098. doi: 10.1177/0363546511415660. [DOI] [PubMed] [Google Scholar]
- 33.Miller B.S., Downie B.K., Kohen R.B., Kijek T., Lesniak B., Jacobson J.A., et al. When do rotator cuff repairs fail? Serial ultrasound examination after arthroscopic repair of large and massive rotator cuff tears. Am J Sports Med. 2011;39:2064–2070. doi: 10.1177/0363546511413372. [DOI] [PubMed] [Google Scholar]
- 34.Millett P.J., Warth R.J., Dornan G.J., Lee J.T., Spiegl U.J. Clinical and structural outcomes after arthroscopic single-row versus double-row rotator cuff repair: a systematic review and meta-analysis of level I randomized clinical trials. J Shoulder Elbow Surg. 2014;23:586–597. doi: 10.1016/j.jse.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 35.Moosmayer S., Lund G., Seljom U., Svege I., Hennig T., Tariq R., et al. Comparison between surgery and physiotherapy in the treatment of small and medium-sized tears of the rotator cuff: a randomised controlled study of 103 patients with one-year follow-up. J Bone Joint Surg Br. 2010;92:83–91. doi: 10.1302/0301-620X.92B1.22609. [DOI] [PubMed] [Google Scholar]
- 36.Mulieri P., Dunning P., Klein S., Pupello D. Frankle M reverse shoulder arthroplasty for the treatment of irreparable rotator cuff tear without glenohumeral arthritis. J Bone Joint Surg. 2010;92:2544–2556. doi: 10.2106/JBJS.I.00912. [DOI] [PubMed] [Google Scholar]
- 37.Namdari S., Donegan R.P., Chamberlain A.M., Galatz L.M., Yamaguchi K., Keener J.D. Factors affecting outcome after structural failure of repaired rotator cuff tears. J Bone Joint Surg Am. 2014;96:99–105. doi: 10.2106/JBJS.M.00551. [DOI] [PubMed] [Google Scholar]
- 38.Novoa-Boldo A., Gulotta L.V. Expectations following rotator cuff surgery. Curr Rev Musculoskelet Med. 2018;11:162–166. doi: 10.1007/s12178-018-9470-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ramme A.J., Robbins C.B., Patel K.A., Carpenter J.E., Bedi A., Gagnier J.J., et al. Surgical versus nonsurgical management of rotator cuff tears: a matched-pair analysis. J Bone Joint Surg Am. 2019;101:1775–1782. doi: 10.2106/JBJS.18.01473. [DOI] [PubMed] [Google Scholar]
- 40.Sambandam S.N., Khanna V., Gul A., Mounasamy V. Rotator cuff tears: an evidence based approach. World J Orthop. 2015;6:902–918. doi: 10.5312/wjo.v6.i11.902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shim J.W., Lee Y.K., Yoo J.C. Clinical outcomes of nonoperative treatment for rotator cuff retears and analysis of factors that affect outcomes. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120967911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Slabaugh M.A., Nho S.J., Grumet R.C., Wilson J.B., Seroyer S.T., Frank R.M., et al. Does the literature confirm superior clinical results in radiographically healed rotator cuffs after rotator cuff repair? Arthroscopy. 2010;26:393–403. doi: 10.1016/j.arthro.2009.07.023. [DOI] [PubMed] [Google Scholar]
- 43.Smith C.D., Alexander S., Hill A.M., Huijsmans P.E., Bull A.M., Amis A.A., et al. A biomechanical comparison of single and double-row fixation in arthroscopic rotator cuff repair. J Bone Joint Surg Am. 2006;88:2425–2431. doi: 10.2106/JBJS.E.00697. [DOI] [PubMed] [Google Scholar]
- 44.Sobhy M.H., Khater A.H., Hassan M.R., Shazly O.E. Do functional outcomes and cuff integrity correlate after single- versus double-row rotator cuff repair? A systematic review and meta-analysis study. Eur J Orthop Surg Traumatol. 2018;28:593–605. doi: 10.1007/s00590-018-2145-7. [DOI] [PubMed] [Google Scholar]
- 45.Tashjian R.Z., Hollins A.M., Kim H.M., Teefey S.A., Middleton W.D., Steger-May K., et al. Factors affecting healing rates after arthroscopic double-row rotator cuff repair. Am J Sports Med. 2010;38:2435–2442. doi: 10.1177/0363546510382835. [DOI] [PubMed] [Google Scholar]
- 46.United States Census Bureau U.S. and World Population Clock. 2021 https://www.census.gov/popclock/ [Google Scholar]
- 47.Westermann R.W., Schick C., Graves C.M., Duchman K.R., Weinstein S.L. What Does a Shoulder MRI Cost the Consumer? Clin Orthop Relat Res. 2017;475:580–584. doi: 10.1007/s11999-016-5181-936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Piasecki D.P., Verma N.N., Nho S.J., Bhatia S., Boniquit N., Cole B.J., et al. Outcomes after arthroscopic revision rotator cuff repair. Am J Sports Med. 2010;38:40–46. doi: 10.1007/s11999-016-5181-9. Epub 2009 Nov 25. [DOI] [PubMed] [Google Scholar]
- 49.Yang J., Jr., Robbins M., Reilly J., Maerz T., Anderson K. The clinical effect of a rotator cuff retear: a meta-analysis of arthroscopic single-row and double-row repairs. Am J Sports Med. 2017;45:733–741. doi: 10.1177/0363546516652900. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.