Compression or tension on the ulnar nerve about the elbow may cause neuropathy known as cubital tunnel syndrome (CuTS). It is the second most common upper extremity neuropathy with an incidence of 24.7 cases per 100,000 persons per year.18,26,28,31 Common sites of compression include Osborne’s ligament, the 2 heads of the flexor carpi ulnaris (FCU), and the arcade of Struthers.20,26 Aside from these muscular and ligamentous structures, the ulnar nerve encounters several vascular structures including the superior ulnar collateral and posterior ulnar recurrent arteries.3,32 Along with these arterial structures, there have been scarce reports of ulnar nerve compression by anomalous venous structures.1,5 This study describes 2 cases of a cubital tunnel venous anomaly that may be a site of ulnar nerve compression not yet reported in literature. Although it is difficult to conclude the primary source of compression, these cases highlight the potential utility of diagnostic ultrasound (US) for the preoperative evaluation of such vascular anomalies.
Both patients were informed and consented for the inclusion and publication of this case report.
Case 1
The patient is a 40-year-old right-hand–dominant male with past medical history significant for hypertension, obesity, and gastric bypass surgery. He presented with a 4-month history of radiating pain from left elbow to hand with associated motor and sensory loss. His symptoms worsened at night and with activity. Of note, since the patient’s bariatric surgery 1 year prior to presentation, he had significant weight loss from approximately 450-285 pounds and was participating in regular exercise that exacerbated his symptoms. Despite conservative management that included several months of regular oral anti-inflammatory medication, night splinting, and activity modification, the patient continued to complain of worsening symptoms.
On physical examination, the patient had full range of motion of the fingers, wrist, and elbow. He had normal sensation to light touch in all nerve distributions without evidence of hypothenar or intrinsic wasting. The patient was tender to palpation of the posteromedial aspect of the elbow with a positive Tinel’s sign at the cubital tunnel. In addition, he had a positive elbow flexion test and resisted supination caused ulnar nerve dysesthesia and pain at the elbow radiating into the hand.
Anterior-posterior and lateral radiographs were unremarkable without arthritis or misalignment. Magnetic resonance imaging showed evidence of mild triceps tendinosis with enhanced T2 signal as well as mild edema adjacent to the common flexor origin. Electromyography (EMG) demonstrated evidence of mild ulnar neuropathy.
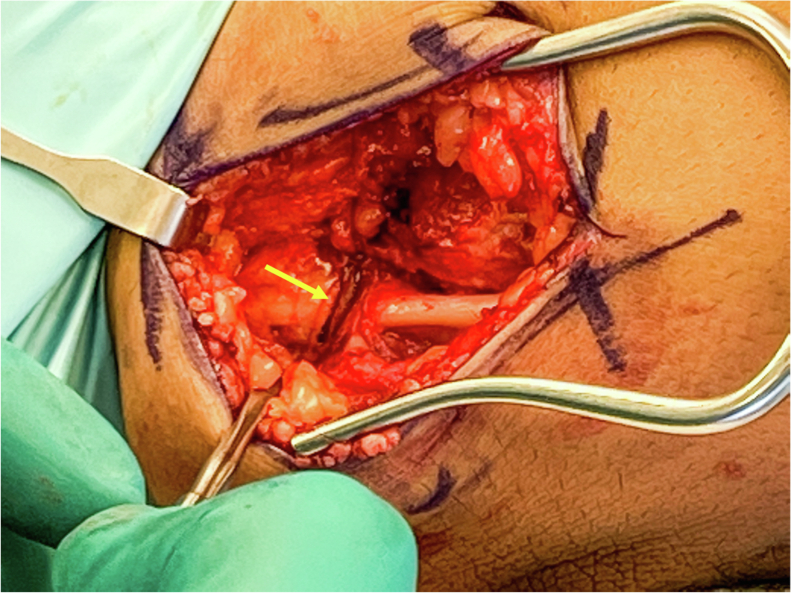
Given ongoing symptoms, the patient elected to proceed with an open left cubital tunnel release with possible anterior subcutaneous transposition. The patient received a brachial plexus block and was placed under general anesthesia. A 4-cm longitudinal incision was made posterior to the medial epicondyle, revealing the fascia overlying the cubital tunnel. Care was taken to cauterize veins when necessary and the medial antebrachial cutaneous nerve was identified and preserved. Starting adjacent to the medial epicondyle and progressing proximally, the fascia overlying the ulnar nerve was carefully released using tenotomy scissors. The anconeus epitrochlearis muscle (AEM) was identified surrounding the ulnar nerve and was resected. In addition, there was a venous vascular leash traversing perpendicular over the ulnar nerve from anterior to posterior. Additionally, there was a significant hourglass deformity due to compression at this vessel-nerve junction (Fig. 1). The venous complex was carefully dissected off the nerve, cauterized with bipolar, and divided to allow for release of the ulnar nerve. Proximal decompression was achieved by releasing fascia of the medial intermuscular septum and the arcade of Struthers approximately 8 cm from the medial epicondyle. Using tenotomy scissors, the distal fascia overlying the ulnar nerve was released from the cubital tunnel until the leading edge of the FCU fascia. With the ulnar nerve carefully protected, the superficial FCU fascia, FCU muscle, and deep fascia were released 4 cm distally until complete decompression of the ulnar nerve was achieved. Subluxation of the ulnar nerve over the medial epicondyle was observed with full flexion and extension of the elbow, indicating the need for a subcutaneous transposition of the nerve. The ulnar nerve was secured over the flexor pronator mass under a subcutaneous flap such that it could freely move in full flexion and extension. The wound was thoroughly irrigated with normal saline and closed in layers. Xeroform was placed over incision with a soft dressing secured over the elbow with an Ace bandage.
Figure 1.
Case 1: Intraoperative view of a vascular complex (yellow arrow) traversing perpendicular over the exposed ulnar nerve overlying the cubital tunnel.
The patient was instructed to limit weight-bearing with a sling and given light duty at work for approximately 2 weeks. At his 2-week follow-up, he had full range of motion at the elbow, sensation, and motor function in all nerve distributions. He endorsed complete resolution of his ulnar neuropathic symptoms with mild soreness around the incision site. To date, he has no return of symptoms or complications.
Case 2
The patient is a 64-year-old male who presents with 3 months of right hand numbness, tingling, and vague radiating pain of the ulnar-sided digits. His symptoms are most severe at the small finger and worsen at night while sleeping with flexed elbows. He denies radiating electrical type pain sensations from the neck or proximal forearm. The patient complains of hand weakness and has noticed atrophy of the first dorsal interosseous muscle. Despite night splinting, the patient’s condition gradually worsened from intermittent symptoms to constant numbness, tingling, and pain.
On physical examination, the patient had full range of motion at his finger, wrist, and elbow. Sensation was intact to light touch in all nerve distributions including ulnar and dorsal sensory branch of the ulnar nerve. He had moderate intrinsic muscle atrophy and decreased intrinsic strength. The patient had a positive elbow flexion compression test, positive Tinel’s over the cubital tunnel, and negative Tinel’s test over Guyon’s canal. He did not exhibit ulnar nerve subluxation with active or passive elbow range of motion.
The patient obtained an EMG that demonstrated severe CuTS with associated chronic denervation of the ulnar innervated muscles. Of note, the patient had a prior cervical spine MRI that demonstrated a mass at the level of C1 that protruded into the anterior aspect of the spinal canal. There was visible impingement of the cervical spinal cord at the junction of cervical spine and brainstem. He was advised to be re-evaluated by neurosurgery before pursuing surgical decompression of the ulnar nerve.
Given the patient’s history, physical examination and EMG findings, the patient elected to proceed with an open cubital tunnel release with possible anterior transposition of the ulnar nerve. The patient was placed under general anesthesia and the operation proceeded in similar fashion to Case 1 described previously. Notably, the patient did not have an AEM but did have a tight venous vascular leash overlying the ulnar nerve. It traversed perpendicular to the ulnar nerve just proximal to the medial epicondyle (Fig. 2). The vascular structure was tied with zero silk suture and divided with bipolar electrocautery. The remainder of the case was performed in standard fashion as described in Case 1. No ulnar nerve subluxation was observed with passive elbow range of motion and therefore no anterior transposition was performed.
Figure 2.
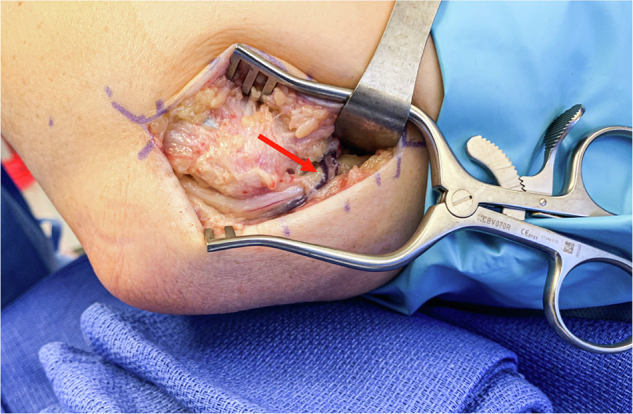
Case 2: Intraoperative view of a vascular complex ( ) wrapping superficially across the exposed ulnar nerve in the cubital tunnel.
) wrapping superficially across the exposed ulnar nerve in the cubital tunnel.
Discussion
As the ulnar nerve travels from its origin at the brachial plexus, it crosses several anatomical structures that can compress and cause subsequent sensory and motor symptoms. In the upper arm, the ulnar nerve initially travels in the anterior compartment and lays posteromedial to the brachial artery.4 Approximately 8 cm proximal to the medial epicondyle, it traverses posteriorly through the medial intermuscular septum and arcade of Struthers.23 This thickening of the deep investing fascia of the arm is a known source of ulnar compression neuropathy; however, its presence is variable.24,28 Lying posterior to the medial intermuscular septum, the ulnar nerve continues its descent to the medial epicondyle, where just proximal may lie the anomalous AEM.12,23 The AEM travels from the medial epicondyle to the olecranon, covering and rarely causing ulnar nerve compression. The more commonly described Osborne ligament is a fibrous tunnel formed from the flexor pronator aponeurosis that often results in ulnar nerve entrapment due to the significant decrease in cubital tunnel volume with deep elbow flexion.7,8 However, inconsistent anatomical terms create discrepancies among cadaveric studies regarding its presence.7,8,10,27
A review of the literature revealed a scarcity of ulnar nerve compression by anatomic and pathologic anomalies other than those described above. Such rare sources of CuTS include intraneural hemangiomas,13 hemangiomas of antebrachial flexor muscles,21 intramuscular venous malformations19 and intraneural ganglion cysts.16 In addition, there have only been 2 case reports of CuTS of venous origin. Abe et al1 reports a case of acute CuTS due to venous thrombosis of the posterior ulnar recurrent vein that was successfully treated with surgical resection of the mass. Finally, Draghi et al5 reports the presence of an accessory vein located along the ulnar nerve that caused CuTS. Given the accessory vein’s location along the ulnar nerve, the patient was managed conservatively with clinical follow-up and repeat imaging.
We presented 2 cases of vascular anomalies in the cubital tunnel that may be sites of ulnar nerve compression. In both cases, we encountered an anomalous venous complex that ran superficial and perpendicular to the ulnar nerve, creating a vascular leash. We believe this venous structure to be the superior ulnar collateral venous complex given its directionality as it traversed from anterior to posterior about the medial epicondyle. However, many anatomic variants of upper extremity veins are reported as their anatomy is less consistent compared to their arterial counterparts.2,9,14,15 Although we cannot be certain that this venous complex was the primary cause of ulnar nerve compression, its presence coinciding with an associated hourglass nerve deformation and clinical improvement after surgical release of the structure supports that it may have at least contributed to the patient’s symptoms. Neuropathy associated with similar cases of venous compression has been described as causes of sciatica22 and trigeminal neuralgia.33
Diagnostic US has recently gained popularity as an effective tool for diagnosing CuTS in addition to a thorough history, physical examination, and nerve conduction studies.11,30 Normal peripheral nerves are visualized on US as a tubular structure with a fascicular appearance, whereas an injured nerve may appear focally enlarged with decreased echogenicity.6 In addition to aiding the diagnosis of an injured nerve, US can often detect anomalous structures such as cysts and neurofibromas.29,25 Furthermore, US is particularly useful for accurate visualization of vascular structures while using the color doppler setting.17 In light of the present vascular anomalies, diagnostic US may be particularly helpful in diagnosing these structures as potential sites of ulnar nerve compression preoperatively.
Conclusion
A vascular anomaly within the cubital tunnel is a rare but potential cause of ulnar nerve compression and subsequent functional impairment. Diagnostic US has shown its utility in detecting anomalous structures in the cubital tunnel, highlighting its potential use as a routine preoperative evaluative tool for ulnar nerve compression. Surgical release of these vascular anomalies along with other common sites of ulnar nerve compression provided long-lasting relief without complication.
Disclaimers:
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Patient consent: Obtained.
Footnotes
Institutional Review Board approval was not required for this case report.
References
- 1.Abe Y., Saito M. A case report of acute cubital tunnel syndrome caused by venous thrombosis. Hand Surg. 2015;20:137–139. doi: 10.1142/S0218810415720016. [DOI] [PubMed] [Google Scholar]
- 2.Adanır S.S., Orhan M. A thick anastomotic vein between cephalic and lateral radial veins: clinical significance of an unusual variation. Cureus. 2021;13 doi: 10.7759/cureus.16629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bailey D.N., Ishwarkumar S., De Gama B.Z., Pillay P. The ulnar nerve in the cubital tunnel: a foetal study. Folia Morphol. 2022;81:31–36. doi: 10.5603/FM.A2020.0150. [DOI] [PubMed] [Google Scholar]
- 4.Bailey C.S., Rasoulinejad P., Taylor D., Sequeira K., Miller T., Watson J., et al. Surgery versus conservative care for persistent sciatica lasting 4 to 12 months. N Engl J Med. 2020;382:1093–1102. doi: 10.1056/nejmoa1912658. [DOI] [PubMed] [Google Scholar]
- 5.Draghi F., Bortolotto C. Importance of the ultrasound in cubital tunnel syndrome. Surg Radiol Anat. 2016;38:265–268. doi: 10.1007/s00276-015-1534-4. [DOI] [PubMed] [Google Scholar]
- 6.Gallardo E., Noto Y.I., Simon N.G. Ultrasound parameterrs other than the direct measurement of ulnar nerve size for diagnosing cubital tunnel syndrome: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2019;86:1114–1130. doi: 10.1136/JNNP-2014-309599. [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez M.H., Lotfi P., Bendre A., Mandelbroyt Y., Lieska N. The ulnar nerve at the elbow and its local branching: an anatomic study. J Hand Surg Br. 2001;26:142–144. doi: 10.1054/JHSB.2000.0532. [DOI] [PubMed] [Google Scholar]
- 8.Granger A., Sardi J.P., Iwanaga J., Wilson T., Yang L., Loukas M., et al. Osborne’s ligament: a review of its history, anatomy, and surgical importance. Cureus. 2017;9 doi: 10.7759/cureus.1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Husarik D.B., Saupe N., Pfirrmann C.W.A., Jost B., Hodler J., Zanetti M. Elbow nerves: MR findings in 60 asymptomatic subjects - normal anatomy, variants, and pitfalls. Radiology. 2009;252:148–156. doi: 10.1148/RADIOL.2521081614. [DOI] [PubMed] [Google Scholar]
- 10.Karatas A., Apaydin N., Uz A., Tubbs S.R., Loukas M., Gezen F. Regional anatomic structures of the elbow that may potentially compress the ulnar nerve. J Shoulder Elbow Surg. 2009;18:627–631. doi: 10.1016/j.jse.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Kerasnoudis A., Tsivgoulis G. Nerve ultrasound in peripheral neuropathies: a review. J Neuroimaging. 2015;25:528–538. doi: 10.1111/jon.12261. [DOI] [PubMed] [Google Scholar]
- 12.Kim N., Stehr R., Matloub H.S., Sanger J.R. Anconeus epitrochlearis muscle associated with cubital tunnel syndrome: a case series. Hand (N Y) 2019;14:477–482. doi: 10.1177/1558944718762566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kline S.C., Moore J.R. Intraneural hemangioma: a case report of acute cubital tunnel syndrome. J Hand Surg Am. 1992;17:305–307. doi: 10.1016/0363-5023(92)90411-h. [DOI] [PubMed] [Google Scholar]
- 14.Kusztal M., Weyde W., Letachowicz K., Gołebiowski T., Letachowicz W. Anatomical vascular variations and practical implications for access creation on the upper limb. J Vasc Access. 2014;15:70–75. doi: 10.5301/jva.5000257. [DOI] [PubMed] [Google Scholar]
- 15.Lee H.S., Song Y.R., Kim J.K., Choi S.R., Joo N., Kim H.J., et al. Anatomical variants of upper arm veins on preoperative mapping venography for hemodialysis access in Korean adults. J Vasc Access. 2019;20:270–275. doi: 10.1177/1129729818803870. [DOI] [PubMed] [Google Scholar]
- 16.Li P., Lou D., Lu H. The cubital tunnel syndrome caused by intraneural ganglion cyst of the ulnar nerve at the elbow: a case report. BMC Neurol. 2018;18:217. doi: 10.1186/s12883-018-1229-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meola M., Ibeas J., Lasalle G., Petrucci I. Basics for performing a high-quality color Doppler sonography of the vascular access. J Vasc Access. 2021;22:18–31. doi: 10.1177/11297298211018060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mondelli M., Giannini F., Ballerini M., Ginanneschi F., Martorelli E. Incidence of ulnar neuropathy at the elbow in the province of Siena (Italy) J Neurol Sci. 2005;234:5–10. doi: 10.1016/J.JNS.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 19.Muchemwa F.C., Ishihara T., Matsushita S. Intramuscular venous malformation in the upper arm with gross calcifications and compression of the ulnar nerve. Scand J Plast Reconstr Surg Hand Surg. 2007;41:93–95. doi: 10.1080/02844310600699432. [DOI] [PubMed] [Google Scholar]
- 20.O’Driscoll S.W., Horii E., Carmichael S.W., Morrey B.F. The cubital tunnel and ulnar neuropathy. J Bone Joint Surg Br. 1991;73:613–617. doi: 10.1302/0301-620X.73B4.2071645. [DOI] [PubMed] [Google Scholar]
- 21.Ouarab M., Rahmi M., Harfaoui A., Hassoun J., Trafeh M. Ulnar nerve hemangioma associated with hemangioma of the epitrochlean muscles. A case report. Ann Chir Main Memb Super. 1997;16:339–341. doi: 10.1016/s0753-9053(97)80048-8. [DOI] [PubMed] [Google Scholar]
- 22.Pacult M.A., Henderson F.C., Wooster M.D., Varma A.K. Sciatica caused by venous varix compression of the sciatic nerve. World Neurosurg. 2018;117:242–245. doi: 10.1016/j.wneu.2018.06.058. [DOI] [PubMed] [Google Scholar]
- 23.Polatsch D.B., Melone C.P., Beldner S., Incorvaia A. Ulnar nerve anatomy. Hand Clin. 2007;23:283–289. doi: 10.1016/j.hcl.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 24.de Ruiter G.C., de Jonge J.G., Vlak M.H., van Loon-Felter A.E. Ulnar neuropathy caused by muscular arcade of struthers. World Neurosurg. 2020;142:128–130. doi: 10.1016/j.wneu.2020.06.179. [DOI] [PubMed] [Google Scholar]
- 25.Schertz M., Mutschler C., Masmejean E., Silvera J. High-resolution ultrasound in etiological evaluation of ulnar neuropathy at the elbow. Eur J Radiol. 2017;95:111–117. doi: 10.1016/j.ejrad.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 26.Staples J.R., Calfee R. Cubital tunnel syndrome: current concepts. J Am Acad Orthop Surg. 2017;25:e215–e224. doi: 10.5435/JAAOS-D-15-00261. [DOI] [PubMed] [Google Scholar]
- 27.Suwannakhan A., Chaiyamoon A., Yammine K., Yurasakpong L., Janta S., Limpanuparb T., et al. The prevalence of anconeus epitrochlearis muscle and Osborne’s ligament in cubital tunnel syndrome patients and healthy individuals: an anatomical study with meta-analysis. Surgeon. 2021;19:E402–E411. doi: 10.1016/j.surge.2020.12.006. [DOI] [PubMed] [Google Scholar]
- 28.Tubbs R.S., Deep A., Shoja M.M., Mortazavi M.M., Loukas M., Cohen-Gadol A.A. The arcade of Struthers: an anatomical study with potential neurosurgical significance. Surg Neurol Int. 2011;2:184. doi: 10.4103/2152-7806.91139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Van Royen K., Goubau J., Goorens C.K. Value of ultrasound in the management of cubital tunnel syndrome with associated space-occupying lesions. J Hand Surg. 2021;42:195–196. doi: 10.1177/1753193420942701. [DOI] [PubMed] [Google Scholar]
- 30.Wiesler E.R., Chloros G.D., Cartwright M.S., Shin H.W., Walker F.O. Ultrasound in the diagnosis of ulnar neuropathy at the cubital tunnel. J Hand Surg Am. 2006;31:1088–1093. doi: 10.1016/J.JHSA.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 31.Wright T.W., Glowczewskie F., Cowin D., Wheeler D.L. Ulnar nerve excursion and strain at the elbow and wrist associated with upper extremity motion. J Hand Surg Am. 2001;26:655–662. doi: 10.1053/jhsu.2001.26140. [DOI] [PubMed] [Google Scholar]
- 32.Yamaguchi K., Sweet F.A., Bindra R., Morrey B.F., Gelberman R.H. The extraosseous and intraosseous arterial anatomy of the adult elbow. J Bone Joint Surg Am. 1997;79:1653–1662. doi: 10.2106/00004623-199711000-00007. [DOI] [PubMed] [Google Scholar]
- 33.Zhao Y., Zhang X., Yao J., Li H., Jiang Y. Microvascular decompression for trigeminal neuralgia due to venous compression alone. J Craniofac Surg. 2018;29:178–181. doi: 10.1097/SCS.0000000000004174. [DOI] [PubMed] [Google Scholar]