Abstract
Current rotator cuff repair rehabilitation protocols focus on multiple areas, including protecting the healing tissue, optimizing range of motion and strength, and returning the individual to labor demanding and sport-specific tasks. Post-operative rehabilitation timelines with consideration of the tear size remain variable among practitioners. Prognostic factors, healing rates, range of motion timeline, exercise progressions, and guidance on return to sport and work activity are the many factors that can help guide rotator cuff repair rehabilitation and ultimately may reduce failure rates and improve outcomes. The purpose of this narrative review is to outline the multi-factorial nature of rotator cuff pathology and guide treatment based on a multitude of factors.
Keywords: Rotator cuff tear, rotator cuff repair, physical therapy, surgery, rehabilitation, orthopedics, overhead athlete
Current rotator cuff repair rehabilitation protocols focus on the following various benchmarks: (1) protect the healing tissue, (2) restore functional range of motion (ROM) and strength, and (3) return the patient to sport-specific and labor-demanding tasks. The postoperative rehabilitation timeline regarding the ROM goals, strength progressions, and return to sport and work activity with consideration of the healing rotator cuff repair remains variable among practitioners. There is also variation among patients owing to tear size, tissue quality, and compliance. Failure rates within the literature body are shown to be greater than 50% at a 12-month follow-up.27 The purpose of this review is to explore the evidence that suggests consideration and appreciation of a rotator cuff repair's multifactorial nature is imperative for a successful outcome; this includes reducing the rate of failure and optimizing return to function.
Classification
Rotator cuff tears (RCTs) are defined as partial- or full-thickness tears. Ellman7 has classified a partial-thickness RCT as articular, bursal, or intratendinous and is further defined by size: grade 1, partial thickness with <3 mm in depth7; grade 2, partial thickness with 3 mm-6 mm in depth7; and grade 3, >6 mm in depth, thereby affecting >50% of the tendon thickness.7 Full-thickness RCTs are defined by size: small tears, 0 cm-1 cm; medium tears, 1 cm-3 cm; large tears 3 cm-5 cm; and massive tears, >5 cm.
Epidemiology
An RCT is a common musculoskeletal injury that results from trauma or age-related degenerative changes.40 Yamamoto et al40 examined more than 600 people, greater than 1200 shoulders, and found full-thickness tears in 20.7%, and the prevalence increased with age. Of the studied population who had symptoms, 36% had a full-thickness tear, and of those who did not have symptoms, 17% had a full-thickness tear.40 Increased likelihood of having an RCT was associated with the following risk factors: being male, increased age, manual labor, dominant arm, and history of trauma.40 Clinical symptoms associated with an RCT are a positive impingement sign, weakness in abduction and external rotation, and decreased forward elevation.40
Prognostic factors
Chung et al3 examined possible prognostic factors affecting rotator cuff healing after a full-thickness rotator cuff repair. The authors found a 22.8% failure rate, 62 of 272 patients, within their patient population.3 Contributing factors were lower bone mineral density, older age, being female, larger tear size, fatty infiltration, diabetes mellitus, and acromiohumeral distance.3 A large randomized control trial determined that age and tear size are the risk factors for failed repair as well.27 Regardless of age, there is an inverse relationship between the tear size and the healing rate. Therefore, as the tear size increased, the healing rate decreased.27 The decrease in healing rate was most evident when comparing small and medium to large and massive full-thickness tears.27 After controlling for tear size, the authors also found increasing age to impact tendon healing negatively.27 The failure rate within the studied population was 56% at 12 months.27
A systematic literature review by Fermont et al8 found five studies to conclude that increasing age negatively impacted healing rates. The odds of having a tendon defect after surgery were 1.15 times greater for every one-year increase in age.8 One of the studies within the systematic review found those with a healed tendon were an average of ten years younger.8 Those who were younger than 50-55 years of age were more likely to have a successful recovery.8
The systematic review by Lambers Heerspink et al13 found two medium-quality studies to show no significant impact on smokers' functional outcomes. There was also medium-quality evidence to show no significant impact on healing rates in smokers.13 These findings were not the case when examining the tendon-to-bone healing in rat models.10 The nicotine group compared with the saline group showed a decrease in tendon-to-bone healing.10 Nicotine decreased maximum force and maximum stress, suggesting a remodeling delay of the repaired tendon.10 The mechanical properties did increase in both groups; however, the nicotine group was slower.10 The nicotine group also demonstrated prolonged inflammation and a delay in cellular proliferation.10 Santiago-Torres et al30 also found smoking to affect rotator cuff repair outcomes negatively in their systematic review. One of four studies within their review examined the effects of smoking on rotator cuff healing via magnetic resonance imaging and found inferior tendon-to-bone healing at the 16-month follow-up.30 Two of the four studies found a negative association of tendon healing, and the last of the four studies found no effect; these three studies did use ultrasonography to examine healing rates.30
Henn et al14 completed a prospective study that found individuals who filed a claim through a workman's compensation and had a rotator cuff repair were at risk of poorer outcomes than those who did not file a claim, even after controlling for confounding factors. Studying the confounding variables allowed the authors to understand better if the adverse outcomes were related to workmen's compensation or related to the individual.14 Although individual factors did play a role in outcomes, the authors concluded that a workman's compensation claims have a negative impact on rotator cuff repair outcomes.14 One crucial aspect to consider is that preoperative education, which includes expectations of treatment, has improved outcomes in those who have filed a workman's compensation claim,14 including preoperative education improved pain levels and general health status.14 The authors admit that a limitation within their study is not able to account for every confounding factor.14
Outcomes
In a systematic review completed by Strauss et al,33 the authors concluded there is “no high-level evidence to support a specific treatment algorithm for partial-thickness rotator cuff pathology.” However, what is generally supported is tears >50% show good outcomes with surgical management focusing on tendon repair.33 Partial-thickness tears <50% treated surgically have shown excellent outcomes with debridement of the tendon with or without an acromioplasty.33
Piper et al25 completed a systematic review comparing operative vs. nonoperative management of a full-thickness RCT, which included three randomized control trials. Both values for Constant scores (sum of four subscores – pain, activities of daily living, ROM, and strength) and visual analog scale scores for pain did not meet the clinically significant difference in the surgical group.25 However, with the comparison between groups, the operative group was slightly favored regarding Constant and visual analog scale scores.25
Kukkonen et al19 performed a randomized control trial comparing different treatment modalities of symptomatic nontraumatic supraspinatus tears with a two-year follow-up. Three different treatment groups with ages of individuals ranging from 55 to 81 years were studied: (1) physical therapy only, (2) acromioplasty and physical therapy, and (3) rotator cuff repair, acromioplasty, and physical therapy.19 Magnetic resonance imaging findings of groups one, two, and three of the mean sagittal size of the isolated supraspinatus tear at baseline were 9.6 mm, 9.1 mm, and 8.4 mm, respectively.19 At the two-year follow-up, those who did not have surgery did have a slight increase in tear size, ranging from 1 mm to 2 mm.19 The authors concluded there was no significant or clinically important difference in outcomes among the three groups at the two-year follow-up in patients older than 55 years of age.19
In the systematic review by Strauss et al,33 the outcomes of different arthroscopic repairs regarding tear types were reviewed. Four studies compared postoperative outcomes between bursal and articular partial-thickness tears.33 Two studies found no difference, one study found better outcomes of bursal lesions, and the fourth study found a higher failure rate with a bursal-sided lesion.33 With subacromial decompression and debridement, Park et al23 found a significantly higher pain reduction at six months with bursal-sided lesions than with articular surface lesions. However, there was no difference at the one- and two-year follow-up.23 Kamath et al18 found a 22% failure rate of bursal-sided tears vs. a 9% failure rate of articular-sided tears. With this information, Strauss et al33 concluded that bursal-sided lesions and repairs were “fare worse” than those on the articular side.
A recent study by Jeong et al,17 which analyzed data from 2006 to 2012, compared healing rates and outcomes of a single-row repair vs. double-row transosseous equivalent repair. The pattern in their results was that partial-thickness, small full-thickness, and medium full-thickness tears demonstrated what the authors would consider healed in >90% of the magnetic resonance imaging follow-up in both surgical techniques used.17 In the single-row large full-thickness tear group, only 70% were considered healed, whereas in the transosseous equivalent large full-thickness tear group, >90% were considered healed.17 The transosseous equivalent group also had less retear rate compared with the single-row repair group.17 In both groups, the pattern seemed to be the more extensive the tear, the higher the postoperative failure rate.17
A recent meta-analysis found surgical intervention for a nontraumatic full-thickness RCT to be a favorable intervention if conservative management failed.12 These findings were based on the shoulder-specific quality of life at the one-year follow-up after surgery.12 A recent retrospective study found early surgical repair of traumatic full-thickness tears, specifically massive tears, to regain full function of the shoulder and resolve pseudoparesis; pseudoparesis is defined as “<90 degrees of active, painless elevation with full [passive] ROM.”32 These outcomes are regardless of age.32 There was a small percentage of retears, but these individuals continued to have nearly full function of their shoulder, and pseudoparesis was not present.32 Figure 1 presents a general guideline for the management of tendinopathy and RCTs.34 Individual factors should be considered within the decision-making process.
Figure 1.
Treatment algorithm for rotator cuff pathology. Information was derived from the study by Tashjian.34
Early vs. delayed rehabilitation
Based on the available literature and the variability of treatment protocols, there does not seem to be a specific consensus on early vs. delayed motion or less vs. more aggressive rehabilitation. As per the systematic review by Thomson et al,37 there is no consensus on when to initiate an early or delayed rehabilitation program. Based on their systematic review, large and massive tears may benefit from a less-aggressive program, whereas small and medium tears may benefit from a more-aggressive program.37 Saltzman et al29 completed a systematic review of meta-analysis on an early vs. delayed ROM postoperative rotator cuff repair. The authors concluded that early motion rehabilitation demonstrated improved outcomes compared with delayed rehabilitation; however, there is a risk of retear with early motion, specifically in those with larger tear sizes.29 A subgroup analysis completed by the authors found early motion rehabilitation with individuals who had a massive preoperative tear and that they were at a higher risk of retear.29
Galatz et al9 performed a rat study to determine the effects of supraspinatus paralysis/immobilization, paralysis/nonimmobilization, and nonparalysis/immobilization. Their results demonstrated that the nonparalysis/immobilization had a higher scar volume and cross-sectional area of the repair.9 At seven and 14 days after surgery, all groups demonstrated poor tendon-bone interface.9 By day 21, tendon healing was presented more organized in both the paralysis/immobilization and nonparalysis/immobilization groups.9 In addition, the structural properties, ultimate load, and stiffness of the tendon demonstrated more improvement at days 21 and 56 in the nonparalysis/immobilization group.9 Therefore, a low-level controlled force is recommended to optimize the healing of the repaired tendon.9 This rat study suggests that early protective passive ROM and sling use will protect the repair and potentially facilitate tendon healing.
Hsu et al15 compared outcomes between tear size and an early vs. delayed ROM protocol. Based on the articles reviewed, small- to medium-sized tears may benefit from early mobilization to improve function at earlier time points without increasing the risk of retear in patients without prognostic factors that would negatively impact healing or retear rates.15 A conservative program may be more appropriate with the following prognostic factors: poor tissue quality, being older, a more sedentary lifestyle, and individuals with systemic diseases.15 Taking into consideration the repair is mechanically delicate in the early phases, it has been shown that repetitive stresses and overload to the tendon complex can cause potential repair site failure or gap formation.15 However, complete removal of the load may understimulate the repair site.15 The authors concluded that “early passive ROM does not risk failure of the repair unless the protocol is too aggressive.”15
Exercise prescription
Within the literature, there is no consensus defining safe and unsafe exercise prescription as the individual progresses through rehabilitation. Based on the prospective study by Long et al20 and the systematic review by Edwards et al,6 muscle activation levels have been categorized into various levels based on maximal voluntary isometric contraction (MVIC). The range of the levels are low, 0%-20% MVIC; moderate, 21%-40% MVIC; high 41%-60% MVIC; and very high, >60% MVIC.6,20 Long et al20 biomechanically calculated a threshold of 15% MVIC as the maximum load for a newly repaired rotator cuff. Edwards et al6 performed a systematic review of biomechanical studies comparing levels of MVIC and categorized them within each of the levels defined. These exercise progressions for a supraspinatus tendon repair are presented in Appendix A and Figure 2. These studies suggest that introducing exercises based on MVIC is more appropriate to reduce stress and overload of the repaired tendon.6,20
Figure 2.
This exercise progression timeline is for a supraspinatus rotator cuff repair that was a small-to-medium complete tear. Refer to Appendix B for precautions, weight restrictions, range of motion timeline, and goals. These exercise progressions serve solely as a guideline, which is based on the available literature and is not an exhaustive list. Information was derived from the study by Edwards et al.6
Sonnabend et al31 completed an observational histologic study of primate models to examine the healing process after a rotator cuff repair. In this study, the authors found the rotator cuff heals by reestablishing Sharpey's fibers, which bind the healing tendon to the bone.31 Although the repair appeared healed at eight weeks macroscopically, the Sharpey's fibers did not appear in any considerable number before the 12th week.31 At week 15, the bone-tendon junction was almost considered mature.31 According to Gerber et al,11 the rotator cuff repair strength in sheep is probably <30% of normal at six weeks and not more than 50% of normal at 12 weeks. The authors concluded that mechanical strength of the scar that bridged the gap between the tendon and the bone was near-full strength at six months.11 This histologic study suggests that excessive tendon loading should be avoided for 12 weeks owing to the time it takes for the tendon-to-bone healing to occur.11,31
Overhead athletes
Return-to-play statistics after a rotator cuff repair has varied within the literature. Payne et al24 evaluated 29 overhead throwers with an atraumatic partial-thickness RCT treated with debridement and subacromial decompression. Only 45% of the overhead athletes returned to preinjury sports.24 A more recent study by Reynolds et al28 found that 76% of the overhead athletes who underwent debridement of a small partial-thickness RCT returned to some level of professional pitching. Ide et al16 evaluated six overhead athletes who underwent a partial-thickness repair; two athletes returned to their prior level of play, three athletes returned to a lower level of play, and one athlete did not return. Regarding full-thickness rotator cuff repairs in these athletes, the statistics are less promising for return to play. Of the 16 professional baseball players, repairs evaluated by Mazoué and Andrews,21 only one pitcher and one position player were able to return to professional baseball at a mean follow-up of 66 months.
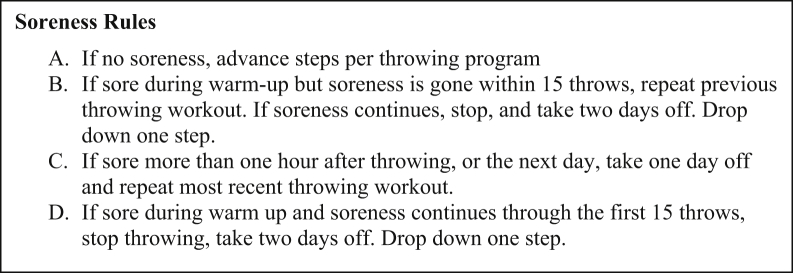
A return-to-throwing program is recommended to guide the athlete to minimize the risk of reinjury.38 Thorsness et al38 developed an interval throwing program that gradually increases volume and distance but not both variables simultaneously. The 12-step throwing program and transition to position-specific and pitching program are found in Appendix C and Figure 3, Figure 4, Figure 5.1,2,4,5,38,39 Thorsness et al38 recommend supervision during this program to ensure sound throwing mechanics and monitor fatigue; both can potentially increase the reinjury risk. This program also allows each athlete to progress at their respective pace by following soreness rules developed by the authors.38 These soreness rules are included in Appendix C and Figure 3.38 During this program, it is imperative to continue a guided individualized exercise program for each athlete.38
Figure 3.
Soreness rules. Information was derived from the study by Thorsness et al.38
Figure 4.
Return-to-throwing program. Perform each step 2 to 3 times with at least 1-day rest between sessions. Follow soreness rules in Figure 3. At the completion of step 12, transition to position or pitching-specific program. Position players are recommended to start at 50% and gradually increase to 100% play. Information was derived from the study by Thorsness et al.38
Figure 5.
Return-to-pitching program. Perform each step 1 to 2 times with at least 1-day rest between sessions. Follow soreness rules in Figure 3. Information was derived from the study by Thorsness et al.38
Limitations
There are limitations within this narrative review and proposed rehabilitation guidelines. This narrative review's primary focus was supraspinatus tendon pathology, which is the most torn rotator cuff tendon.22 This review and the recommended protocols based on tear size assume that there is only a supraspinatus tendon repair. If the labrum, subscapularis, and biceps are surgically involved, other precautions should be in place. Second, there is high variability within the research on the surgical technique used to repair the rotator cuff and interobserver differences in the measurement of tear sizes.17,23,25,33 Third, patient compliance is difficult to measure and can affect research outcomes. A patientless compliant with a recommended rehabilitation program may be at risk for failed repair or a poor outcome. Fourth, there is minimal consensus on the ROM goal timeline regarding early vs. delayed mobilization and appropriate exercise progression.6,9,25,26,29,33,35, 36, 37 What is supported within the literature is the older the individual, the larger the tear, and the poorer the tissue quality, rehabilitation should be less aggressive to optimize tendon healing.3,15,26,29,33 Muscle activation levels are measured on healthy participants, and this information does not consider muscle activity on a recently repaired rotator cuff tendon; therefore, compensatory patterns after surgery may increase or decrease muscle activity.6,20 Finally, many biological and structural studies on the rotator cuff repair and failure loads are performed with nonhuman animals.9, 10, 11
Conclusion
Outcomes and failure rates of rotator cuff repair vary significantly, and the best evidence should be considered to make operative and postoperative decisions. As per the RCT size, the following outlined exercise prescription and protocols are general guidelines for rehabilitation (see Appendices). The individual should be progressed based on their clinical presentation using such recommendations as a guideline. Before starting a rehabilitation program, it is helpful for all involved practitioners and the patient to be informed of the extent of the RCT, which includes tendon involvement, tear size, tissue quality, and concomitant shoulder pathology. In conclusion, this narrative review outlines the multifactorial nature of rotator cuff pathology, treatment, and respective rehabilitation.
Disclaimers
Funding: No funding was disclosed by the author(s).
Conflicts of interest: The authors, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this review article.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.xrrt.2021.04.009.
Supplementary data
References
- 1.Burkhart S., Morgan C., Kibler W. The disabled throwing shoulder: spectrum of pathology part I: pathoanatomy and biomechanics. Arthroscopy. 2003;19:404–420. doi: 10.1053/jars.2003.50128. [DOI] [PubMed] [Google Scholar]
- 2.Camp C., Sinatro A., Spiker A., Werner B., Altchek D., Coleman S., et al. Decreased shoulder external rotation and flexion are greater predictors of injury than internal rotation deficits: analysis of 132 pitcher-seasons in professional baseball. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117s00221. [DOI] [PubMed] [Google Scholar]
- 3.Chung S., Oh J., Gong H., Kim J., Kim S. Factors affecting rotator cuff healing after arthroscopic repair. Am J Sports Med. 2011;39:2099–2107. doi: 10.1177/0363546511415659. [DOI] [PubMed] [Google Scholar]
- 4.Conway J. Arthroscopic repair of partial-thickness rotator cuff tears and SLAP lesions in professional baseball players. Orthop Clin North Am. 2001;32:443–456. doi: 10.1016/s0030-5898(05)70213-3. [DOI] [PubMed] [Google Scholar]
- 5.Cools A., Johansson F., Borms D., Maenhout A. Prevention of shoulder injuries in overhead athletes: a science-based approach. Braz J Phys Ther. 2015;19:331–339. doi: 10.1590/bjpt-rbf.2014.0109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Edwards P., Ebert J., Littlewood C., Ackland T., Wang A. A systematic review of electromyography studies in normal shoulders to inform postoperative rehabilitation following rotator cuff repair. J Orthop Sports Phys Ther. 2017;47:931–944. doi: 10.2519/jospt.2017.7271. [DOI] [PubMed] [Google Scholar]
- 7.Ellman H. Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res. 1990:64–74. [PubMed] [Google Scholar]
- 8.Fermont A., Wolterbeek N., Wessel R., Baeyens J., de Bie R. Prognostic factors for successful recovery after arthroscopic rotator cuff repair: a systematic literature review. J Orthop Sports Phys Ther. 2014;44:153–163. doi: 10.2519/jospt.2014.4832. [DOI] [PubMed] [Google Scholar]
- 9.Galatz L., Charlton N., Das R., Kim H., Havlioglu N., Thomopoulos S. Complete removal of load is detrimental to rotator cuff healing. J Shoulder Elbow Surg. 2009;18:669–675. doi: 10.1016/j.jse.2009.02.016. [DOI] [PubMed] [Google Scholar]
- 10.Galatz L., Silva M., Rothermich S., Zaegel M., Havlioglu N., Thomopoulos S. Nicotine delays tendon-to-bone healing in a rat shoulder model. J Bone Joint Surg Am. 2006;88:2027–2034. doi: 10.2106/JBJS.E.00899. [DOI] [PubMed] [Google Scholar]
- 11.Gerber C., Schneeberger A., Perren S., Nyffeler R. Experimental rotator cuff repair. A preliminary study∗. J Bone Joint Surg. 1999;81:1281–1290. doi: 10.2106/00004623-199909000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Gurnani N., van Deurzen D., van den Bekerom M. Shoulder-specific outcomes 1 year after nontraumatic full-thickness rotator cuff repair: a systematic literature review and meta-analysis. Shoulder Elbow. 2017;9:247–257. doi: 10.1177/1758573217711903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heerspink F.O.L., Dorrestijn O., van Raay J., Diercks R. Specific patient-related prognostic factors for rotator cuff repair: a systematic review. J Shoulder Elbow Surg. 2014;2014:1073–1080. doi: 10.1016/j.jse.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 14.Henn R., Kang L., Tashjian R., Green A. Patients with workers' compensation claims have worse outcomes after rotator cuff repair. J Bone Joint Surg Am. 2008;90:2105–2113. doi: 10.2106/JBJS.F.00260. [DOI] [PubMed] [Google Scholar]
- 15.Hsu J., Horneff J., Gee A., Hsu J., Horneff J., Gee A. Immobilization after rotator cuff repair. Orthop Clin North Am. 2016;47:169–177. doi: 10.1016/j.ocl.2015.08.017. [DOI] [PubMed] [Google Scholar]
- 16.Ide J., Maeda S., Takagi K. Arthroscopic transtendon repair of partial-thickness articular-side tears of the rotator cuff. Am J Sports Med. 2005;33:1672–1679. doi: 10.1177/0363546505277141. [DOI] [PubMed] [Google Scholar]
- 17.Jeong J., Park K., Sundar S., Yoo J. Clinical and radiologic outcome of arthroscopic rotator cuff repair: single-row versus transosseous equivalent repair. J Shoulder Elbow Surg. 2018;27:1021–1029. doi: 10.1016/j.jse.2017.10.040. [DOI] [PubMed] [Google Scholar]
- 18.Kamath G., Galatz L., Keener J., Teefey S., Middleton W., Yamaguchi K. Tendon integrity and functional outcome after arthroscopic repair of high-grade partial-thickness supraspinatus tears. J Bone Joint Surg Am. 2009;91:1055–1062. doi: 10.2106/jbjs.g.00118. [DOI] [PubMed] [Google Scholar]
- 19.Kukkonen J., Joukainen A., Lehtinen J., Mattila K., Tuominen E., Kauko T., et al. Treatment of nontraumatic rotator cuff tears. J Bone Joint Surg. 2015;97:1729–1737. doi: 10.2106/jbjs.n.01051. [DOI] [PubMed] [Google Scholar]
- 20.Long J., Ruberte R., Skendzel J., Jeon J., Hughes R., Miller B., et al. Activation of the shoulder musculature during pendulum exercises and light activities. J Orthop Sports Phys Ther. 2010;40:230–237. doi: 10.2519/jospt.2010.3095. [DOI] [PubMed] [Google Scholar]
- 21.Mazoué C., Andrews J. Repair of full-thickness rotator cuff tears in professional baseball players. Am J Sports Med. 2006;34:182–189. doi: 10.1177/0363546505279916. [DOI] [PubMed] [Google Scholar]
- 22.Opsha O., Malik A., Baltazar R., Primakov D., Beltran S., Miller T., et al. MRI of the rotator cuff and internal derangement. Eur J Radiol. 2008;68:36–56. doi: 10.1016/j.ejrad.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 23.Park J., Yoo M., Kim M. Comparison of surgical outcome between bursal and articular partial thickness rotator cuff tears. Orthopedics. 2003;26:387–390. doi: 10.3928/0147-7447-20030401-16. discussion 390. [DOI] [PubMed] [Google Scholar]
- 24.Payne L., Altchek D., Craig E., Warren R. Arthroscopic treatment of partial rotator cuff tears in young athletes. Am J Sports Med. 1997;25:299–305. doi: 10.1177/036354659702500305. [DOI] [PubMed] [Google Scholar]
- 25.Piper C., Hughes A., Ma Y., Wang H., Neviaser A. Operative versus nonoperative treatment for the management of full-thickness rotator cuff tears: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2018;27:572–576. doi: 10.1016/j.jse.2017.09.032. [DOI] [PubMed] [Google Scholar]
- 26.Randelli P., Spennacchio P., Ragone V., Arrigoni P., Casella A., Cabitza P. Complications associated with arthroscopic rotator cuff repair: a literature review. Musculoskelet Surg. 2011;96:9–16. doi: 10.1007/s12306-011-0175-y. [DOI] [PubMed] [Google Scholar]
- 27.Rashid M., Cooper C., Cook J., Cooper D., Dakin S., Snelling S., et al. Increasing age and tear size reduce rotator cuff repair healing rate at 1 year. Acta Orthop. 2017;88:606–611. doi: 10.1080/17453674.2017.1370844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reynolds S., Dugas J., Cain E., McMichael C., Andrews J. Débridement of small partial-thickness rotator cuff tears in elite overhead throwers. Clin Orthop Relat Res. 2008;466:614–621. doi: 10.1007/s11999-007-0107-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saltzman B., Zuke W., Go B., Mascarenhas R., Verma N., Cole B., et al. Does early motion lead to a higher failure rate or better outcomes after arthroscopic rotator cuff repair? A systematic review of overlapping meta-analyses. J Shoulder Elbow Surg. 2017;26:1681–1691. doi: 10.1016/j.jse.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 30.Santiago-Torres J., Flanigan D., Butler R., Bishop J. The effect of smoking on rotator Cuff and glenoid labrum surgery. Am J Sports Med. 2014;43:745–751. doi: 10.1177/0363546514533776. [DOI] [PubMed] [Google Scholar]
- 31.Sonnabend D., Howlett C., Young A. Histological evaluation of repair of the rotator cuff in a primate model. J Bone Joint Surg Br. 2010;92-B:586–594. doi: 10.1302/0301-620x.92b4.22371. [DOI] [PubMed] [Google Scholar]
- 32.Spross C., Behrens G., Dietrich T., Olaf Kim C., Puskas G., Zdravkovic V., et al. Early arthroscopic repair of acute traumatic massive rotator cuff tears leads to reliable reversal of pseudoparesis: clinical and radiographic outcome. Arthroscopy. 2019;35:343–350. doi: 10.1016/j.arthro.2018.08.048. [DOI] [PubMed] [Google Scholar]
- 33.Strauss E., Salata M., Kercher J., Barker J., McGill K., Bach B., et al. The arthroscopic management of partial-thickness rotator cuff tears: a systematic review of the literature. Arthroscopy. 2011;27:568–580. doi: 10.1016/j.arthro.2010.09.019. [DOI] [PubMed] [Google Scholar]
- 34.Tashjian R. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31:589–604. doi: 10.1016/j.csm.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 35.Thigpen C., Shaffer M., Gaunt B., Leggin B., Williams G., Wilcox R. The American Society of Shoulder and Elbow Therapists' consensus statement on rehabilitation following arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2016;25:521–535. doi: 10.1016/j.jse.2015.12.018. [DOI] [PubMed] [Google Scholar]
- 36.Thigpen C., Shaffer M., Kissenberth M. Knowing the speed limit: weighing the benefits and risks of rehabilitation progression after arthroscopic rotator cuff repair. Clin Sports Med. 2015;34:233–246. doi: 10.1016/j.csm.2014.12. [DOI] [PubMed] [Google Scholar]
- 37.Thomson S., Jukes C., Lewis J. Rehabilitation following surgical repair of the rotator cuff: a systematic review. Physiotherapy. 2016;102:20–28. doi: 10.1016/j.physio.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 38.Thorsness R., Alland J., McCulloch C., Romeo A. Return to play after shoulder surgery in throwers. Clin Sports Med. 2016;35:563–575. doi: 10.1016/j.csm.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 39.Wilk K., Macrina L., Fleisig G., Aune K., Porterfield R., Harker P., et al. Deficits in glenohumeral passive range of motion increase risk of elbow injury in professional baseball pitchers. Am J Sports Med. 2014;42:2075–2081. doi: 10.1177/0363546514538391. [DOI] [PubMed] [Google Scholar]
- 40.Yamamoto A., Takagishi K., Osawa T., Yanagawa T., Nakajima D., Shitara H., et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19:116–120. doi: 10.1016/j.jse.2009.04.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.