The scapula serves as the transition point for energy from the lower body and core through the scapulothoracic articulation to the distal upper extremity. Abnormal motion and asynchrony of the scapulothoracic articulation can disrupt this kinetic chain and lead to pain and dysfunction of the shoulder.
Of the potential causes of abnormal motion of the scapulothoracic joint, the pectoralis minor is often underappreciated (Table I). Because it inserts on the medial aspect of the coracoid process, shortening and contracture of the pectoralis minor can lead to an obligate internal rotation and anterior tilt of the scapula. These changes to scapular positioning can disrupt scapular control and lead to abnormal scapulohumeral and scapulothoracic kinematics. Athletes who participate in repetitive overhead activities, such as weightlifters, baseball players, volleyball players, and tennis players, are at risk of developing a shortened pectoralis minor that can lead to scapular dyskinesia.7,11
Table I.
Causes of abnormal scapulothoracic motion.
| Primary | Associated |
|---|---|
Neurologic scapular winging
|
Acromioclavicular joint arthrosis Acromioclavicular joint instability/separation clavicle fracture External shoulder impingement Glenohumeral instability Pectoralis minor contracture/shortening Scapular fracture malunion Superior labral tear |
Altered kinematics from pectoralis minor contracture can lead to concomitant shoulder pathologies. Shortening of the pectoralis minor can lead to scapula protraction.1,3,6,8,11 This altered scapula positioning decreases the acromial humeral space, especially during forward flexion and internal rotation, thereby causing external shoulder impingement. Furthermore, the shortened pectoralis minor causes a resultant lengthening of its antagonist muscle group, the lower trapezius.1,3 This lengthening results in weakness of the shoulder girdle and increases abnormal stress on the glenohumeral joint,6,8 which can lead to rotator cuff disease, labral tears, and acromioclavicular arthropathy.5,7
Nonoperative treatments of pectoralis minor contracture are focused on stretching and mobilization. Strengthening and stabilizing scapulothoracic dynamics help improve shoulder kinematics.7,8,10 Bordstad et al described 3 stretches to facilitate lengthening of the pectoralis minor and mobilization of the anterior shoulder.2 Several studies have demonstrated that lengthening the pectoralis minor tendon can clinically improve scapular mobility and control.3,8,10 For patients who fail conservative nonoperative treatments, however, surgical interventions are indicated and have been found to be successful.9
Surgical technique
When a patient is being treated for shoulder impingement syndrome or glenohumeral instability, a pectoralis minor release may be necessary. This surgical technique provides a safe approach to arthroscopically release the pectoralis minor from the medial border of the coracoid in the beach chair position (Video).
Positioning
The patient is positioned in the standard beach chair position, and the operative extremity is prepped and draped in the standard fashion. The operative extremity is positioned in neutral rotation, adduction, and 15 degrees of flexion.
Step 1: portal placement
The standard posterior viewing portal into the glenohumeral joint is established, and the anterior triangle of the shoulder is identified. Using needle localization, a superolateral-anterior portal is established within the rotator interval (Fig. 1), and a cannula is placed. This modified anterior portal is placed so that there is sufficient space to palpate the coracoid, partially release the rotator interval, and dissect the lateral border of the conjoint tendon.
Figure 1.
Anterior triangle of the shoulder. RI, rotator interval; SS, subscapularis; LHB, long head of biceps tendon.
Step 2: partial rotator interval release
Using a radiofrequency ablation (RFA) device, the posterolateral portion of the coracoid can be palpated through the rotator interval. It can generally be palpated at the center of the anterior triangle of the shoulder. Once identified, the RFA is used to ablate the inferolateral coracoid. By following the coracoid laterally, the superolateral attachment of the conjoint tendon at the coracoid tip can be identified (Fig. 2).
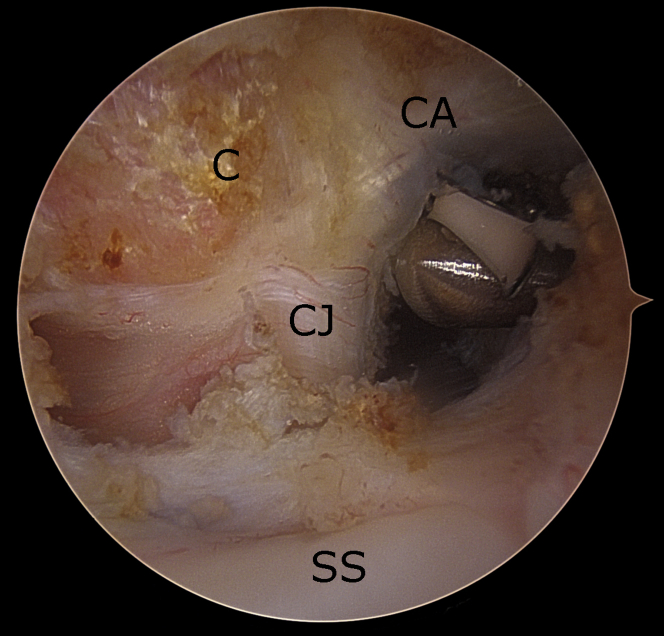
Figure 2.
Partial rotator interval release. C, coracoid; CA, coracoacromial ligament; CJ, conjoint tendon; SS, subscapularis.
Step 3: identification of conjoint tendon and coracoacromial ligament
The lateral aspect of the rotator interval is sufficiently released to expose the lateral border of the conjoint tendon. Once this is delineated, the lateral border of the conjoint tendon is traced superiorly to the superolateral aspect of the coracoid, where the coracoacromial (CA) ligament attaches. The RFA is used to release 2 mm of the anterior attachment of the CA ligament on the lateral coracoid. This small partial release of the anterior attachment of the CA ligament will guide the surgeon to identify the tip of the coracoid clearly and safely. The bursal surface of the conjoint tendon is then bluntly débrided, starting from the tip of the coracoid and working inferiorly; this generally does not require ablation. If the anterior deltoid is crowding the conjoint tendon, increased flexion of the shoulder can increase the space between the conjoint tendon and anterior deltoid.
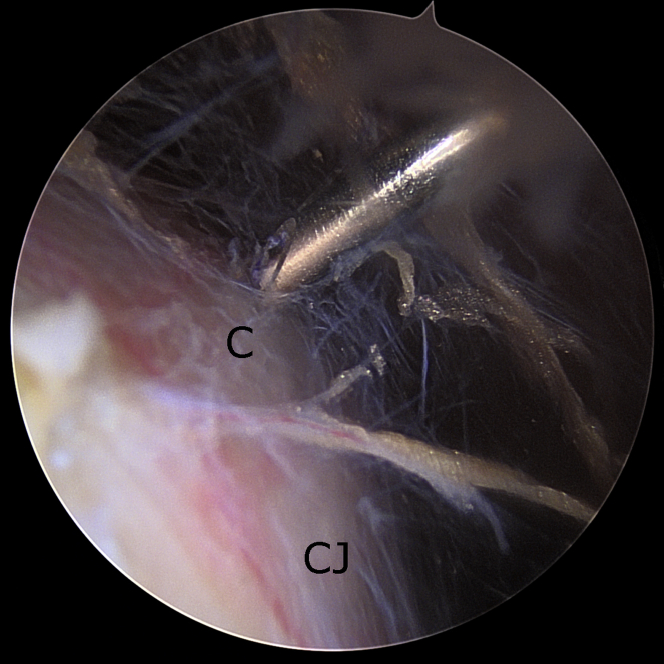
Step 4: accessory mid-coracoid portal
Once the coracoid tip and bursal side of the conjoint tendon is adequately débrided, a switching stick is placed in the modified anterior portal, and the camera is then introduced (Fig. 3). From the anterior viewing portal, the subscapularis can be viewed inferiorly, the CA ligament superiorly, both the articular and bursal surfaces of the conjoint tendon anteriorly, and the coracoid tip.
Figure 3.
Establish anterolateral viewing portal. SS, subscapularis.
The coracoid tip is viewed and palpated. The accessory mid-coracoid portal is then placed with needle localization (Fig. 4). The ideal location for this mid-coracoid portal is slightly superior to the coracoid tip and in line with the medial border of the coracoid. A cannula can be used in this portal to facilitate instrument passage.
Figure 4.
View from anterolateral portal. C, coracoid tip; CJ, conjoint tendon.
Step 5: coracoid exposure
The RFA is placed in the mid-coracoid portal and used to bluntly expose the superior aspect of the coracoid. Exposure needs to be taken all the way to the coracoclavicular (CC) ligaments, which attach at the genu of the coracoid. From this view, the entire superior aspect of the coracoid can be exposed.
Step 6: identification and release of the pectoralis minor
The pectoralis minor attaches to the superomedial border of the coracoid (Fig. 5). The safe zone for pectoralis minor release is the CC ligament posteriorly and tip of the coracoid anteriorly. Care must be taken to not release posterior to the CC ligament, as this is where the suprascapular nerve crosses under the suprascapular ligament. Anteriorly, the musculocutaneous nerve innervates the coracobrachialis approximately 3 cm distal to the tip of the coracoid.
Figure 5.
Pectoralis minor. C, coracoid tip; PM PB, pectoralis minor posterior border.
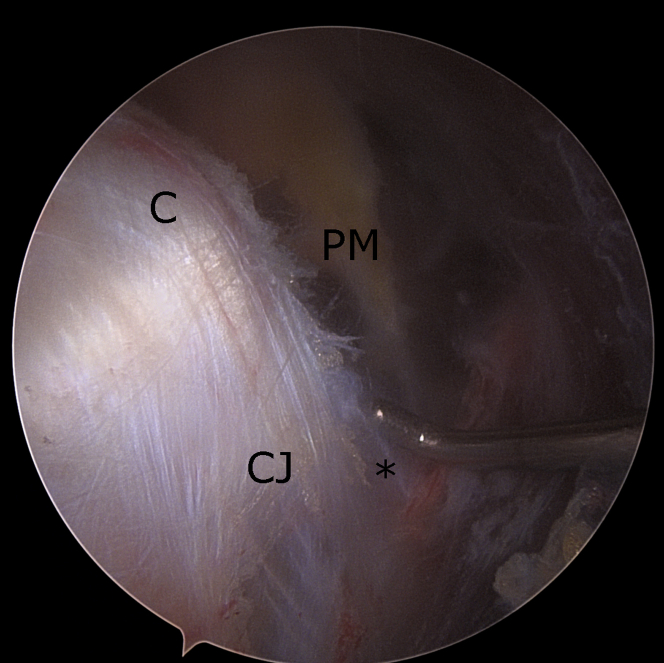
Using the RFA, the superomedial border of the coracoid is palpated, and the tendon of the pectoralis minor is ablated directly off the bone. As the tendon is released, it will retract medially (Fig. 6). By ablating directly off the bone, the surgeon can safely avoid injury to the brachial plexus. Anteriorly at the tip of the coracoid, the pectoralis minor will have a confluence of tissue connecting to the conjoint tendon (Fig. 7). Given the close proximity of the musculocutaneous nerve, this confluent tissue should be bluntly released.
Figure 6.
Pectoralis minor release. PM, pectoralis minor tendon edge.
Figure 7.
Supracoracoid space. C, coracoid tip; CJ, conjoint tendon; PM, pectoralis minor tendon edge; ∗confluence of tissue between pectoralis minor and conjoint tendon.
Postoperative rehabilitation
When the primary procedure is isolated release of the pectoralis minor tendon, the patient can undergo the range of motion and activity as tolerated. Physical therapy needs to be initiated immediately and focused on scapular retraction, external rotation, posterior scapular tilt, and downward rotation: strengthening of the rhomboid minor and rhomboid major will increase external rotation; strengthening of the lower trapezius and serratus anterior will increase posterior tilt; and stretching and lengthening of the upper trapezius and strengthening of levator scapulae and lower trapezius will increase downward rotation.
Typically, the arthroscopic pectoralis minor release will serve as an adjunct to a primary procedure (eg, rotator cuff repair, labral repair). In such situations, the postoperative rehabilitation should be directed by the needs of the primary procedure.
Discussion
By disrupting the synchrony of the periscapular musculature, a tight pectoralis minor can mimic scapular winging. Furthermore, it can lead to increased shoulder impingement syndrome and glenohumeral instability.
In most situations, a contracted pectoralis minor can be successfully treated with nonoperative management. Provencher et al published a series of 46 patients with isolated pectoralis minor tightness.9 The majority of these patients improved with nonoperative management. However, 6 patients required open surgical release of their pectoralis minor. At final follow-up, all patients, both operative and nonoperative, significantly improved in their American Shoulder Elbow Surgeons score, Single Assessment Numeric Evaluation score, and Visual Analog Scale pain scale.
A tight pectoralis minor often has concomitant pathology, such as shoulder impingement syndrome, rotator cuff tear, glenohumeral instability, acromioclavicular instability, or scapular winging.6 As such, an arthroscopic technique to release the pectoralis minor can allow the surgeon to address concomitant pathology.
Hendrix et al described the arthroscopic pectoralis minor release in the lateral position. For surgeons adept in shoulder arthroscopy in the lateral position, the technique guide provides tips and tricks on how to safely perform an arthroscopic pectoralis minor release.4 However, not all surgeons are comfortable performing shoulder arthroscopy in the lateral position.
The technique in this article is performed in the beach chair position. Other than surgeon preference, the primary advantage in the beach chair position is the ability to convert to an open procedure.
When done correctly, the arthroscopic release of the pectoralis minor can be performed very safely. However, there are risks to this procedure. Endoscopic anatomy of the shoulder is unfamiliar to most surgeons and can lead to injury to the brachial plexus. Furthermore, this procedure requires the placement of a mid-coracoid portal, with which most surgeons are unaccustomed. Careful palpation of landmarks, needle localization, and safe arthroscopic practices can decrease iatrogenic risk to the surrounding neurovascular structures.
Conclusion
The key to treating abnormal scapulothoracic motion is recognizing the diagnosis and understanding the cause of the dysfunction. Although rare, a tight pectoralis minor can lead to abnormal scapular motion, which in most situations, can be treated nonoperatively with stretching, mobilization, and scapulothoracic rehabilitation. However, in patients unresponsive to physical therapy and/or with concomitant pathology, arthroscopic pectoralis minor release may be a viable solution. Further clinical studies with long-term follow-up are needed for patients treated with arthroscopic release of the pectoralis minor.
Disclaimers:
Disclosure: The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Army, Department of Defense, or the U.S. Government.
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
According to the Department of Clinical Investigations Institutional Review Board (IRB) at Tripler Army Medical Center, Technique Articles are IRB exempt.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.xrrt.2021.11.006.
Supplementary data
References
- 1.Borstad J.D., Ludewig P.M. The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals. J Orthop Sports Phys Ther. 2005;35:227–238. doi: 10.2519/jospt.2005.35.4.227. [DOI] [PubMed] [Google Scholar]
- 2.Borstad J.D., Ludewig P.M. Comparison of three stretches for the pectoralis minor muscle. J Shoulder Elbow Surg. 2006;15:324–330. doi: 10.1016/j.jse.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 3.Burkhart S.S., Morgan C.D., Kibler W.B. The disabled throwing shoulder: spectrum of pathology part III: the SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19:641–661. doi: 10.1016/s0749-8063(03)00389-x. [DOI] [PubMed] [Google Scholar]
- 4.Hendrix S.T., Hoyle M., Tokish J.M. Arthroscopic pectoralis minor release. Arthrosc Tech. 2018;7:e589–e594. doi: 10.1016/j.eats.2018.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kibler W.B., Kuhn J.E., Wilk K., Sciascia A., Moore S., Laudner K., et al. The disabled throwing shoulder: spectrum of pathology-10-year update. Arthroscopy. 2013;29:141–161.e126. doi: 10.1016/j.arthro.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 6.Kibler W.B., McMullen J. Scapular dyskinesis and its relation to shoulder pain. J Am Acad Orthop Surg. 2003;11:142–151. doi: 10.5435/00124635-200303000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Kibler W.B., Sciascia A. Evaluation and management of scapular dyskinesis in overhead athletes. Curr Rev Musculoskelet Med. 2019;12:515–526. doi: 10.1007/s12178-019-09591-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Panagiotopoulos A.C., Crowther I.M. Scapular dyskinesia, the forgotten culprit of shoulder pain and how to rehabilitate. SICOT J. 2019;5:29. doi: 10.1051/sicotj/2019029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Provencher M.T., Kirby H., McDonald L.S., Golijanin P., Gross D., Campbell K.J., et al. Surgical release of the pectoralis minor tendon for scapular dyskinesia and shoulder pain. Am J Sports Med. 2017;45:173–178. doi: 10.1177/0363546516664720. [DOI] [PubMed] [Google Scholar]
- 10.Saini S.S., Shah S.S., Curtis A.S. Scapular dyskinesis and the kinetic chain: recognizing dysfunction and treating injury in the tennis athlete. Curr Rev Musculoskelet Med. 2020;13:748–756. doi: 10.1007/s12178-020-09672-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yesilyaprak S.S., Yuksel E., Kalkan S. Influence of pectoralis minor and upper trapezius lengths on observable scapular dyskinesis. Phys Ther Sport. 2016;19:7–13. doi: 10.1016/j.ptsp.2015.08.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.