Abstract
Sternoclavicular joint pathology can be an uncommon cause of pain and discomfort around the neck and shoulder region. Typically, patients localize their pain deep to the joint and experience referred pain to the ipsilateral neck and shoulder; however, it often presents as a diffuse nonspecific pain. Given the paucity of this pathology and atypical presentation, the use of injections can be helpful to confirm the diagnosis of sternoclavicular arthropathy. Currently, most injections are done via computed tomography. Although this method is accurate, it exposes patients to radiation and burdens the patient with the requirement of multiple appointments. This case series outlines the use of ultrasound-guided sternoclavicular joint injections conducted in the clinic. The patients in this series underwent an ultrasound-guided injection in the affected sternoclavicular joint, which confirmed the diagnosis, and they were subsequently treated with resection arthroplasty. The use of ultrasound-guided injections of the sternoclavicular joint is a safe and accurate alternative diagnostic method, which saves the patient from harmful radiation and additional appointments. Limitations and efficacy may vary depending on skill and comfort level of the operator.
Keywords: Sternoclavicular, Ultrasound, Resection arthroplasty, Guided injection
The sternoclavicular joint is a diarthrodial synovial joint between the medial clavicle and the sternum. At the sternoclavicular joint, the clavicle has 35° of upward elevation, 35° of translation in the anterior to posterior plane, and 50° of rotation around the longitudinal axis.19 The clavicle connects the axial skeleton to the upper extremity; in the kinetic chain, it is a transition point at which the energy from the lower body and axial skeleton transmits to the distal upper extremity. Pathology of the sternoclavicular joint is an uncommon cause of pain around the shoulder and neck. It is an inherently unstable joint; less than half of the sternal facet of the clavicle articulates with the reciprocal notch of the sternum.22 Sternoclavicular joint arthropathy can be caused by trauma, infection, degermation, neurologic deficit, or some combination thereof.22 Patients with sternoclavicular joint arthropathy typically present with a deep localized pain over the joint that can refer to the ipsilateral anterior neck or shoulder; often it presents as a diffuse nonspecific pain.10
Given the rarity, and at times nonspecific presentation of sternoclavicular joint arthropathy, injections can be helpful to confirm the diagnosis.15,22,25 Most commonly, computed tomography (CT) is used for image-guided injection of the sternoclavicular joint. Although accurate, there are several negative effects of CT: it exposes the patient to radiation, including the especially radiosensitive thyroid gland,23 and it requires the additional resource of a radiologist, thereby increasing cost and delaying diagnosis.8,9,15,21
Ultrasonography has been used to assess the shoulder joint anatomy and pathology.4,7,17 It is commonly used to assess the rotator cuff but has also been used for image-guided injections into the acromioclavicular joint1,6,11 and the long head of the biceps tendon sheath.2 The use of ultrasound has also been described as a tool for image-guided injections into the sternoclavicular joint;17 however, there are no studies that describe the clinical efficacy of ultrasound-guided sternoclavicular injections. The aim of this case series is to discuss our results using ultrasound-guided sternoclavicular joint injections in the clinic to diagnose and treat sternoclavicular pathology.
Patient 1
An active 70-year-old female presented to the Orthopedic Clinic with a 6-month history of right shoulder and neck pain. She denied any history of trauma or injury but reported that her pain ranged from a 3/10 to 10/10 on the visual analog scale (VAS). She endorsed an active lifestyle including frequent bowling and caring for an adult son with developmental delays. Her pain was increased with the use of her right upper extremity, including performing her activities of daily living. She reported her Single Assessment Numeric Evaluation (SANE) score of her right shoulder as 60%. She denied pain at rest, but did endorse night pain. Prior treatments had been limited to non-steroidal anti-inflammatory drugs, which did provide moderate but temporary symptomatic relief.
On physical examination, there were no overlying skin changes, but she had tenderness to palpation over the right sternoclavicular joint. She was able to actively flex and abduct her right shoulder to 90⁰, but this resulted in pain at the sternoclavicular joint, which she rated as 6/10. There was no evidence of sternoclavicular joint instability to include clicking or popping of the joint.
Radiographs of the shoulder and clavicle did not demonstrate any osseous abnormalities. However, a magnetic resonance imaging of the chest was consistent with a subluxated and arthritic right sternoclavicular joint.
To confirm the primary differential diagnosis of right sternoclavicular joint arthrosis as the source of her pain and assess for possible benefit from operative intervention, an ultrasound-guided sternoclavicular joint injection was performed in clinic. After the injection, she endorsed 100% pain relief and improved pain-free (0/10) range of motion about the right shoulder. She was subsequently scheduled for a right sternoclavicular joint resection.
At the time of surgery, she was found to have severe sternoclavicular joint arthritis with large osteophyte formation on the medial clavicle. A 5-mm resection of the medial clavicle was performed (as described by Pingsmann et al).16 Postoperatively, the patient was instructed to remain in a sling for 6 weeks, allowing only passive ROM with physical therapy.
By 4 months postoperative time, her pain at the sternoclavicular joint had completely resolved, she was no longer requiring a sling or pain medications, and she endorsed overall satisfaction with the procedure. Her right shoulder ROM improved to 130⁰ of flexion, 90⁰ of abduction, 20⁰ of external rotation, and internal rotation to the lumbar spine. She reported a SANE score to the right shoulder of 100%.
At 1 year postoperatively, her pain over the right sternoclavicular joint remained resolved. Her right shoulder ROM continued to improve to 160⁰ of flexion, 90⁰ of abduction, and 30⁰ of external rotation, and her SANE score remained 100%.
Patient 2
A 39-year-old, otherwise-healthy male initially presented to the Sports Medicine Clinic with a 2-month history of progressive pain predominately localized to the right sternoclavicular joint, which was associated with a clicking and popping sensation. He did not recall a specific traumatic event associated with the onset of symptoms but believed he injured it while lifting weights in the gym. With increased levels of activity, he also endorsed tension and pain to the right neck and trapezius. His symptoms were exacerbated by walking/running, weight lifting, and working on his computer. The pain was bothersome both during periods of rest and at night.
A family medicine sports physician elected to perform a corticosteroid injection into the right sternoclavicular joint without image guidance, which resulted in no pain relief. After a referral to physical therapy and 4 weeks of treatment, he was subsequently referred to the orthopedic clinic.
At the time of his presentation to the orthopedic clinic, his pain was rated 5/10 on the VAS. He endorsed only minimal benefit from physical therapy and reported a SANE score of 50% for his right sternoclavicular joint.
On physical examination, he did not have tenderness to palpation over the right sternoclavicular joint and there were no overlying skin changes. However, with glenohumeral range of motion, there was crepitus and audible popping at the sternoclavicular joint. He endorsed pain rated 7/10 at the sternoclavicular joint with ROM of the shoulder, but he had full ROM without mechanical block. He also had full ROM about his neck, which was nontender over the trapezius and sternocleidomastoid muscles. When turning his head, he endorsed pain over the right sternoclavicular joint.
Radiographs of the right shoulder and clavicle were unremarkable.
To confirm the suspected diagnosis of sternoclavicular arthrosis and disk tear, an ultrasound-guided sternoclavicular joint injection was performed in clinic. The patient noted immediate and near-complete pain relief. After the injection, with shoulder ROM, he stated that he had 1/10 pain over the sternoclavicular joint. Given the confirmatory injection, he was counselled and prepared for a right sternoclavicular joint resection.
Surgical findings were consistent with sternoclavicular arthritis and a torn disk. The torn disk was resected, as was 5-mm of the medial clavicle. Postoperatively, he was allowed ROM as tolerated, but kept non-weight-bearing to the right upper extremity for 6 weeks. His recovery was complicated by a small wound dehiscence that resolved with local wound care.
At 4 months postoperative time, he stated that the painful clicking had completely resolved, he had minimal tightness when turning his head, and there was some tenderness over the surgical scar. Otherwise, he had returned back to his normal weight lifting and his SANE score was 90%.
The patients were informed and consented to the submission of their clinical data for publication in the form of a case report.
Injection technique
Preinjection assessment
Gather all necessary supplies and equipment (Table I). Before the injection, perform provocative maneuvers that illicit pain at the suspected sternoclavicular joint. Such maneuvers may include axial compression of the joint with scapular protraction and cross body adduction, grind with manual translation of the medial clavicle or provocative exercises such as push-ups. Often, patients complain of pain with contraction of the sternocleidomastoid (looking to the contralateral shoulder). For the provocative maneuver, collect the VAS (Table II).
Table I.
Equipment.
| Linear high-frequency ultrasound probe (6-13Hz) |
| Local anesthetic (1% lidocaine [1 cc], 0.25% marcaine/bupivacaine [1 cc]) |
| 40 mg Kenalog (1 cc) |
| Syringe (3 cc-5 cc) |
| Needle (20-22 gauge), 1-1.5 inch |
Table II.
Pearls and pitfalls.
| Pearls | Pitfalls |
|---|---|
| Before injection, perform a provocative maneuver which elicits pain/discomfort, record the VAS; repeat the same maneuver after injection. | Use a 20- to 22-gauge hypodermic needle, if the needle is too small, it can deflect off the thick and arthritic capsule |
| Position the patient supine and place the ultrasound monitor on the contralateral side next to the patient’s head | Do not use a spinal needle, use a 1- to 1¼-inch needle to avoid inadvertent injection into the mediastinum |
| When positioning and draping, prepare both sternoclavicular joints | Do not use curvilinear ultrasound probe, use a small linear high-frequency probe (6-13Hz) |
Positioning
Provide the patient with a gown that will allow full exposure of the medial clavicle, manubrium, upper sternum, and neck, and position the patient in the supine position with the patient looking to the contralateral side. Position the screen of the ultrasound on the contralateral side, adjacent to the patient’s head.
Procedure
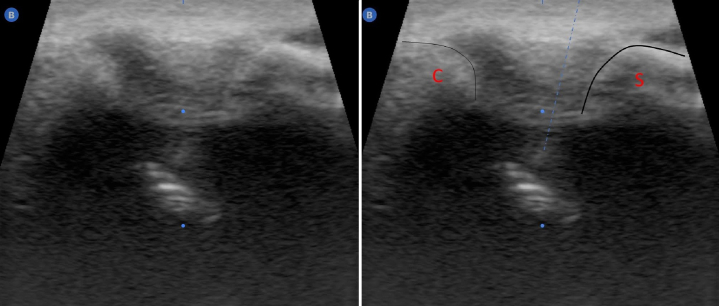
Position the high-frequency linear transducer in the short axis of the sternoclavicular joint (Fig. 1). Often the medial clavicle is more pronounced than the sternum. Scan the transducer proximally and distally along the short axis of the joint to localize the midpoint (Fig. 2). Wipe the excess ultrasound transmission gel and prep the injection site 2 cm distal to the transducer. Two centimeters distal and in-line with the center of the transducer, insert the 21-gauge needle at 45° to the horizontal skin plane. Visualize the pathway of the needle, advance pass the anterior capsule, and stop at the center of the joint (Fig. 3). Inject 2-3 mL of the solution; there should be minimal resistance when injecting the joint.
Figure 1.
Injection technique insert the needle 45° to the skin, along the short axis of the probe.
Figure 2.
Ultrasound case 1 S: sternum; C: medical clavicle; cap: superior sternoclavicular capsule.
Figure 3.
Ultrasound case 2 S: sternum; C: medical clavicle; dashed line: trajectory of the needle.
Postinjection assessment
After waiting 5 minutes, perform a postinjection assessment. Perform the same maneuvers as the preinjection assessment, and record the VAS. A successful injection can be confirmed with a greater than 3-point decrease12 in the VAS provocative examination.
Coding
When performing an ultrasound-guided sternoclavicular joint injection, the in-office procedure can be coded as an “arthrocentesis, aspiration and/or injection, intermediate joint or bursa (eg, temporomandibular, acromioclavicular, wrist, elbow or ankle, olecranon bursa); with ultrasound guidance, with permanent recording and reporting” (CPT: 20606).
Discussion
Osteoarthritis of the sternoclavicular joint is an uncommon condition that can result in persistent pain; sternoclavicular joint arthropathy can be caused by trauma, infection, degermation, neurologic deficit, or some combination thereof.22 Although available, radiographic imaging of the sternoclavicular joint (posterior anterior, anterior oblique, lateral sternal, and serendipity) are of limited value owing to the overlapping shadows from ribs, spine, and mediastinal structures. Considering the low incidence, atypical presentation, and limitations of plain radiographs, a diagnostic injection is helpful to confirm diagnosis. When there is a concern for sternoclavicular arthritis and pathology, patients are often sent for a CT-guided injection into the sternoclavicular joint.15,18 However, CT exposes the patient to radiation, including the especially radiosensitive thyroid gland.23
When properly performed, ultrasound-guided aspirations and injections are safe and efficacious.2,4,6,11,20 Dave et al retrospectively reviewed their 18 years of experience with 128 ultrasound-guided procedures on American football players; they found that these techniques are safe and effective in improving injury outcomes.4 Unlike fluoroscopy, roentgenogram, and CT, ultrasound does not subject the patient to harmful radiation. Ultrasound-guided shoulder injections are highly accurate and have been found to be 87.6% successful in the biceps sheath2 and 96% successful in the acromioclavicular joint.6 Ultrasound is a valuable tool that can be performed in an office setting. Patients have also reported greater comfort with ultrasound-guided injection than with fluoroscopic guidence.20 In addition, performing the procedure in-office allows the patient and surgeon to diagnose the condition with a high degree of certainty, treat the condition with a corticosteroid injection, and provide appropriate disposition. It provides value to the patient because it avoids the need for additional consultations (CT-guided injection with radiologist), avoids radiation exposure, and eliminates the need for follow-up with the orthopedic surgeon to confirm the diagnosis.
Nonoperative therapy is the treatment modality of choice for sternoclavicular arthritis.13 For those patients who fail nonoperative treatment, resection arthroplasty of the sternoclavicular joint has been found to be a successful surgical option.5,14,16,19
In our case series, both patients were accurately diagnosed with sternoclavicular joint arthropathy using the ultrasound. Their VASs before diagnosis were 6 and 7, and their VASs after the injection improved to 0 and 1, respectively. Given the positive results, we were able to confidently take the patients to the operating room and perform a resection arthroplasty of the sternoclavicular joint.
Resection arthroplasty of the sternoclavicular joint is a successful procedure in the treatment of sternoclavicular arthropathy.3,16,19 Rockwood et al first described resection arthroplasty as a treatment option for the painful sternoclavicular joint. In his series of 15 patients, those patients who underwent the resection and had preservation of the costoclavicular ligament have excellent clinical results.19
Postoperatively, the patients in our case series had significant improvements in their SANE score (the minimal clinically important difference for SANE is 15%24), both improving by 40%.
There are limitations to this case series. Given the low incidence of sternoclavicular joint arthropathy, only two patients are included in this case series. Also, ultrasound skill and comfort are surgeon dependent. In our department, ultrasound is frequently utilized for guided injections into the long-head of the biceps sheath, acromioclavicular joint, and tendon sheaths of the hand and wrist; therefore, our level of skill and comfort may be greater than that of the novice ultrasonographer.
Conclusion
Ultrasound-guided injections to the sternoclavicular joint provide a safe and accurate alternative to the CT-guided injection while saving the patient from harmful radiation and additional appointments.
Disclaimers
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Patient consent: Obtained.
Footnotes
The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Army, Department of Defense, or the U.S. Government.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. According to the Department of Clinical Investigations Institutional Review Board at Tripler Army Medical Center, Case Reports/Series are IRB exempt.
References
- 1.Borbas P., Kraus T., Clement H., Grechenig S., Weinberg A.M., Heidari N. The influence of ultrasound guidance in the rate of success of acromioclavicular joint injection: an experimental study on human cadavers. J Shoulder Elbow Surg. 2012;21:1694–1697. doi: 10.1016/j.jse.2011.11.036. [DOI] [PubMed] [Google Scholar]
- 2.Chang K.V., Wu W.T. The Biceps Long-Head Tendon: An Overlooked Pain Origin for Ultrasound-Guided Injection. J Ultrasound Med. 2020;39:409–410. doi: 10.1002/jum.15109. [DOI] [PubMed] [Google Scholar]
- 3.Chun J.M., Kim J.S., Jung H.J., Park J.B., Song J.S., Park S.S., et al. Resection arthroplasty for septic arthritis of the sternoclavicular joint. J Shoulder Elbow Surg. 2012;21:361–366. doi: 10.1016/j.jse.2011.05.020. [DOI] [PubMed] [Google Scholar]
- 4.Dave R.B., Stevens K.J., Shivaram G.M., McAdams T.R., Dillingham M.F., Beaulieu C.F. Ultrasound-guided musculoskeletal interventions in American football: 18 years of experience. AJR Am J Roentgenol. 2014;203:W674–W683. doi: 10.2214/AJR.14.12678. [DOI] [PubMed] [Google Scholar]
- 5.Dekker T.J., Lacheta L., Goldenberg B.T., Horan M.P., Pogorzelski J., Millett P.J. Minimum 5-Year Outcomes and Return to Sports After Resection Arthroplasty for the Treatment of Sternoclavicular Osteoarthritis. Am J Sports Med. 2020;48:715–722. doi: 10.1177/0363546519897892. [DOI] [PubMed] [Google Scholar]
- 6.Edelson G., Saffuri H., Obid E., Lipovsky E., Ben-David D. Successful injection of the acromioclavicular joint with use of ultrasound: anatomy, technique, and follow-up. J Shoulder Elbow Surg. 2014;23:e243–e250. doi: 10.1016/j.jse.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 7.Ferri M., Finlay K., Popowich T., Jurriaans E., Friedman L. Sonographic examination of the acromioclavicular and sternoclavicular joints. J Clin Ultrasound. 2005;33:345–355. doi: 10.1002/jcu.20153. [DOI] [PubMed] [Google Scholar]
- 8.Galla R., Basava V., Conermann T., Kabazie A.J. Sternoclavicular steroid injection for treatment of pain in a patient with Osteitis condensans of the clavicle. Pain Physician. 2009;12:987–990. [PubMed] [Google Scholar]
- 9.Golder W., Karberg K., Sieper J. Fluoroscopy-guided application of corticosteroids for local control of manubriosternal joint pain in patients with spondyloarthropathies. Clin Rheumatol. 2004;23:481–484. doi: 10.1007/s10067-004-0912-9. [DOI] [PubMed] [Google Scholar]
- 10.Hassett G., Barnsley L. Pain referral from the sternoclavicular joint: a study in normal volunteers. Rheumatology (Oxford) 2001;40:859–862. doi: 10.1093/rheumatology/40.8.859. [DOI] [PubMed] [Google Scholar]
- 11.Jung E., Kye Y.C., Park C., Lee J., Park J.R., Lee K.H., et al. Ultrasound-guided analgesic injection for acromioclavicular joint - For better safety. Am J Emerg Med. 2020;38:1038. doi: 10.1016/j.ajem.2019.11.009. [DOI] [PubMed] [Google Scholar]
- 12.Lee J.S., Hobden E., Stiell I.G., Wells G.A. Clinically important change in the visual analog scale after adequate pain control. Acad Emerg Med. 2003;10:1128–1130. doi: 10.1111/j.1553-2712.2003.tb00586.x. [DOI] [PubMed] [Google Scholar]
- 13.Martetschlager F., Warth R.J., Millett P.J. Instability and degenerative arthritis of the sternoclavicular joint: a current concepts review. Am J Sports Med. 2014;42:999–1007. doi: 10.1177/0363546513498990. [DOI] [PubMed] [Google Scholar]
- 14.Panzica M., Zeichen J., Hankemeier S., Gaulke R., Krettek C., Jagodzinski M. Long-term outcome after joint reconstruction or medial resection arthroplasty for anterior SCJ instability. Arch Orthop Trauma Surg. 2010;130:657–665. doi: 10.1007/s00402-009-0911-z. [DOI] [PubMed] [Google Scholar]
- 15.Peterson C.K., Saupe N., Buck F., Pfirrmann C.W., Zanetti M., Hodler J. CT-guided sternoclavicular joint injections: description of the procedure, reliability of imaging diagnosis, and short-term patient responses. AJR Am J Roentgenol. 2010;195:W435–W439. doi: 10.2214/AJR.10.4501. [DOI] [PubMed] [Google Scholar]
- 16.Pingsmann A., Patsalis T., Michiels I. Resection arthroplasty of the sternoclavicular joint for the treatment of primary degenerative sternoclavicular arthritis. J Bone Joint Surg Br. 2002;84:513–517. doi: 10.1302/0301-620x.84b4.12601. [DOI] [PubMed] [Google Scholar]
- 17.Pourcho A.M., Sellon J.L., Smith J. Sonographically guided sternoclavicular joint injection: description of technique and validation. J Ultrasound Med. 2015;34:325–331. doi: 10.7863/ultra.34.2.325. [DOI] [PubMed] [Google Scholar]
- 18.Robinson C.M., Jenkins P.J., Markham P.E., Beggs I. Disorders of the sternoclavicular joint. J Bone Joint Surg Br. 2008;90:685–696. doi: 10.1302/0301-620X.90B6.20391. [DOI] [PubMed] [Google Scholar]
- 19.Rockwood C.A., Jr., Groh G.I., Wirth M.A., Grassi F.A. Resection arthroplasty of the sternoclavicular joint. J Bone Joint Surg Am. 1997;79:387–393. doi: 10.2106/00004623-199703000-00011. [DOI] [PubMed] [Google Scholar]
- 20.Rutten M.J., Collins J.M., Maresch B.J., Smeets J.H., Janssen C.M., Kiemeney L.A., et al. Glenohumeral joint injection: a comparative study of ultrasound and fluoroscopically guided techniques before MR arthrography. Eur Radiol. 2009;19:722–730. doi: 10.1007/s00330-008-1200-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sencan S., Guler E., Cuce I., Erol K. Fluoroscopy-guided intra-articular steroid injection for sternoclavicular joint arthritis secondary to limited cutaneous systemic sclerosis: a case report. Korean J Pain. 2017;30:59–61. doi: 10.3344/kjp.2017.30.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sewell M.D., Al-Hadithy N., Le Leu A., Lambert S.M. Instability of the sternoclavicular joint: current concepts in classification, treatment and outcomes. Bone Joint J. 2013;95-B:721–731. doi: 10.1302/0301-620X.95B6.31064. [DOI] [PubMed] [Google Scholar]
- 23.Sinnott B., Ron E., Schneider A.B. Exposing the thyroid to radiation: a review of its current extent, risks, and implications. Endocr Rev. 2010;31:756–773. doi: 10.1210/er.2010-0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thigpen C.A., Shanley E., Momaya A.M., Kissenberth M.J., Tolan S.J., Tokish J.M., et al. Validity and Responsiveness of the Single Alpha-numeric Evaluation for Shoulder Patients. Am J Sports Med. 2018;46:3480–3485. doi: 10.1177/0363546518807924. [DOI] [PubMed] [Google Scholar]
- 25.Weinberg A.M., Pichler W., Grechenig S., Tesch N.P., Heidari N., Grechenig W. Frequency of successful intra-articular puncture of the sternoclavicular joint: a cadaver study. Scand J Rheumatol. 2009;38:396–398. doi: 10.1080/03009740902953856. [DOI] [PubMed] [Google Scholar]