Abstract
Background
Surgical management of massive irreparable rotator cuff tears remains controversial. Arthroscopic debridement (AD) has shown promising results especially in the population older than 65 years; however, there is no consensus on the benefits of various AD procedures. The aim of this systematic review was to evaluate the functional midterm to long-term outcomes in patients treated with AD in combination with subacromial decompression, biceps tenotomy, tuberoplasty, or bursectomy, without repair of the rotator cuff tear.
Methods
A comprehensive search was performed in PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Cochrane databases for studies reporting clinical outcomes of AD of massive rotator cuff tears. Quality was determined using the Methodological Index for Nonrandomized Studies (MINORS) criteria by two independent reviewers. Pooled frequency-weighted means and standard deviations were calculated for patient-reported outcomes.
Results
Sixteen articles containing 643 patients and 662 shoulders met the eligibility criteria. The mean age at the time of surgery was 65.9 ± 4.4 years with a mean follow-up period of 46.5 ± 27.3 months. There was notable clinically significant improvement across all patient-reported outcome scores postoperatively: Constant 70.4 ± 8.9 (P value = .06), University of California, Los Angeles ultrasonography 26.7 ± 5.2 (P value = .001), American Shoulder and Elbow Surgeons score 71.7 ± 2.1 (P value = .12), Disabilities of the Arm, Shoulder, and Hand score 35.3, and visual analog score 1.7 ± 0.9. Forty-nine patients (7%) required reoperation, which most commonly was a reverse total shoulder arthroplasty for the development of rotator cuff arthropathy.
Conclusion
Arthroscopic debridement with a combination of subacromial decompression, tuberoplasty, subacromial bursectomy, and biceps tenotomy, for treatment of massive irreparable rotator cuff tears, produces good functional outcomes and improvement in pain at mid to long term follow up for the low-demand population greater than 65 years of age looking for pain relief over substantial increase in function.
Keywords: Shoulder arthroscopy, Irreparable rotator cuff tear, Tuberoplasty, Subacromial decompression, Biceps tenotomy, Arthroscopic debridement, Massive rotator cuff tear
Surgical management of massive irreparable rotator cuff tears (iRCTs) remains controversial. Massive rotator cuff tears have been described as those > 5 cm, involving 2 or more tendons, with >3 cm of exposure of the humeral head, and a tear with a perimeter > 9 cm.12,25,56 To define an iRCT, we must acknowledge the likelihood that a primary rotator cuff repair will fail and then recognize the features that lead to increased rates of failure. Failure can be defined as the need for reoperation, structural failure of the repair, lack of restoration of motion or strength, or poor patient-reported outcomes, including persistent pain. Intrinsic factors associated with increased failure rate can be chronicity, loss of acromiohumeral distance, advanced muscle atrophy, fatty infiltration of the rotator cuff musculature, tear retraction beyond the level of the glenoid, and development of glenohumeral degeneration.18,26,27,32,37,40 Extrinsic factors include preoperative range of motion (ROM), smoking, diabetes, advanced age, patient expectations/compliance, and previous failed rotator cuff repair.3,5,9,40,42,48,55,65 Traditionally, the spectrum of operative treatment for iRCT has included complete repair (CR), partial repair (PR), and tendon transfers and reverse shoulder arthroplasty, all with varying results7,8,21,22,23,31,35; but with a notable risk for failure and incomplete pain relief.23,54 Recently, subacromial balloon implantation and superior capsular reconstruction (SCR) have emerged as potential options; but long-term results are lacking for some of the new procedures.10,17,44,64 When patients fail nonoperative management, arthroscopic debridement (AD)—with a combination of subacromial decompression, tuberoplasty/acromioplasty, and/or biceps tenotomy/tenodesis—can be a surgical option of lower risk than more technically demanding procedures, with the inherent risk of device implantation. The utility of AD in the settings of iRCTs may be beneficial as the biceps and labrum can contribute to rotator cuff pain, as well as the lack of need for aggressive postoperative rehabilitation to restore baseline function.5 The aim of this systematic review was to evaluate the functional midterm to long-term outcomes in patients treated with AD without repair of massive iRCTs.
Methods
This systematic review was performed following Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines.44
Search strategy
A comprehensive search was performed in the PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medline Ebschohost, OVID, and Cochrane databases from database inception to April 11, 2020, for studies reporting clinical outcomes of AD of massive rotator cuff tears. Medical Subject Headings and Emtree terms were used in combinations which included “subacromial decompression”, “arthroscopic débridement”, “tuberoplasty”, subacromial bursectomy”, and “biceps tenotomy” paired with “massive rotator cuff tear” and “irreparable rotator cuff tear”.
Assessment of study qualification
Inclusion criteria consisted of English language journal, human subjects, nonreview articles, and measurable outcomes including ROM, patient-reported outcomes, and follow-up duration of at least 12 months. Exclusion criteria included case reports, review articles, technique guides, or literature published in a non-English language.
Screening of study eligibility
Three authors performed the primary search (M.S., M.B., A.O.), and two independently reviewed the references of the qualifying studies and selected the appropriate studies based on the inclusion criteria (A.S.J. and J.M.M). Any articles disputed between reviewers were included and underwent full-text review. After the full-text review, consensus was obtained regarding a study’s eligibility. Quality was assessed using the Methodological Index for Nonrandomized Studies (MINORS) criteria by the two independent reviewers (J.M.M. and A.S.J.).63
Data collection and outcomes
The following data were collected from the studies that met the inclusion criteria: primary author, year of publication, levels of evidence included, mean patient age, mean follow-up period, procedure(s) performed, patient-reported outcomes, secondary outcomes if applicable, ROM, rehabilitation protocol, complications, and subsequent procedures performed. The following outcome scores were collected: Constant score; University of California, Los Angeles ultrasonography (UCLA) score; American Shoulder and Elbow Surgeons (ASES) score; Disabilities of the Arm, Shoulder, and Hand (DASH) score; visual analog score (VAS) for pain. Reported complications and reoperation including the type of secondary procedure were also analyzed.
Statistical analysis
Outcome measures were pooled, and frequency-weighted means and standard deviations were calculated where applicable. The frequency-weighted mean represents the mean from each individual study weighted by the number of patients in that study. Statistical significance of the patient-reported outcome scores was determined using a t-test consisting of the frequency-weighted means. The frequency-weighted standard deviation is determined based on the frequency-weighted mean.
Results
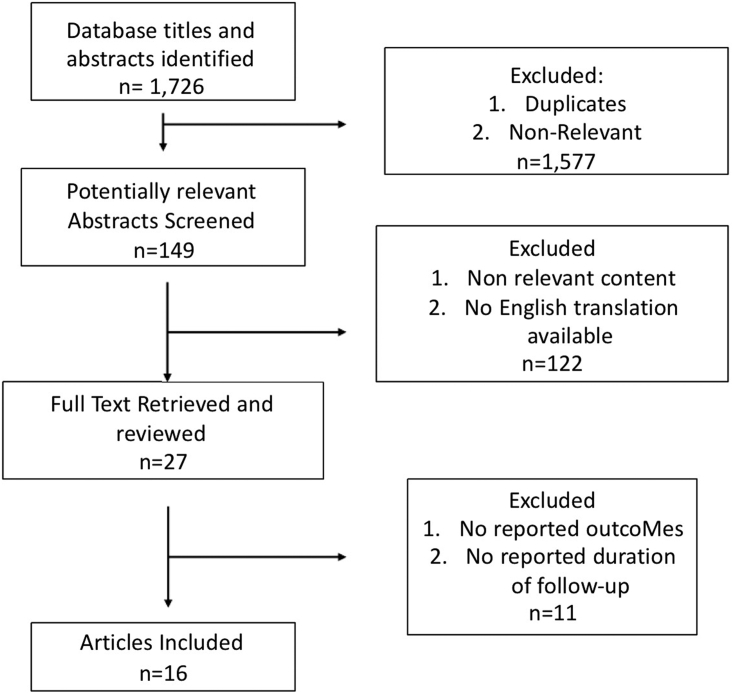
The initial search resulted in 1726 articles. After the removal of duplicates and title and abstract screening, 27 articles were reviewed in full. Ultimately, 16 articles met the inclusion criteria (Fig. 1).4,6,29,30,38,41,45,46,49,52,58,59,61,67, 68, 69 Overall, 16 articles containing 643 patients and 662 shoulders met the eligibility criteria (Table I). Of the 16 articles included, 13 were retrospective case series (level IV)6,29,30,38,41,45,49,58,59,61,67, 68, 69; comparative studies in 2 prospective cohorts (level II)4,46; and comparative studies in 1 retrospective cohort (Level III).58 The mean MINORS score was 11.9 (range, 9-14), out of a maximum of 16. The mean age at the time of surgery was 65.9 ± 4.4 years, with a mean follow-up period of 46.5 ± 27.3 months.
Figure 1.
The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram demonstrating systematic review of literature for extensive arthroscopic debridement of massive irreparable rotator cuff tears.
Table I.
Summary of studies.
| Author, yr | Level of evidence | Number of patients | Mean age, yr | Mean follow-up, mo | MINORS score |
|---|---|---|---|---|---|
| Burkhart et al, 19916 | IV | 8 | 65 | 17.6 | 11 of 16 |
| Walch et al, 200569 | IV | 291 | 64.3 | 57 | 12 of 16 |
| Liem et al, 200845 | IV | 31 | 70.7 | 47 | 12 of 16 |
| Veado et al, 201567 | IV | 22 | 69 | 27 | 11 of 16 |
| Pander et al, 201858 | III | 39 | 75.6 | 78 | 11 of 16 |
| Park et al, 201659 | IV | 16 | 64 | 98 | 12 of 16 |
| Berth et al, 20104 | II | 21 | 64.3 | 24.7 | 18 of 24 |
| Melillo et al, 199749 | IV | 27 | 60 | 89.9 | 9 of 16 |
| Lee et al, 201141 | IV | 32 | 62.4 | 40 | 13 of 16 |
| Verhelst et al, 201068 | IV | 31 | 69.6 | 38 | 12 of 16 |
| Scheibel et al, 200461 | IV | 22 | 69 | 40 | 13 of 16 |
| Ho et al, 202030 | IV | 26 | 60 | 98 | 13 of 16 |
| Mirzaee et al, 201952 | IV | 12 | 65 | 18 | 12 of 16 |
| Maillot et al, 201846 | II | 9 | 59.3 | 37.9 | 13 of 16 |
| Heuberer et al, 201629 | IV | 23 | 66.5 | 45 | 11 of 16 |
| Klinger et al, 200538 | IV | 33 | 69 | 31 | 14 of 16 |
| Total | 643 | 65.8 | 46.4 | 12.3 |
MINORS, Methodological Index for Nonrandomized Studies.
Functional and patient-reported outcomes
Frequency-weighted patient-reported outcome scores are detailed in Table II. There was notable improvement in all mean patient-reported outcome scores across the included studies. Eleven studies reported outcomes based on the Constant score with a preoperative frequency-weighted mean of 40.6, which improved postoperatively to 70.4, P value = .06. The minimal clinical important difference (MCID) for the Constant score is 10.4,70 and our study patients had almost a threefold improvement; however, this was not a statistically significant difference.
Table II.
Preoperative and postoperative patient-reported outcomes.
| Constant score, 11 studies, n = 567 |
UCLA score, 6 studies, n = 117 |
ASES score, 2 studies, n = 57 |
DASH score, 1 study, n = 21 |
VAS score, 7 studies, n = 149 |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Preop | Postop | Preop | Postop | Preop | Postop | Preop | Postop | Preop | Postop | |
| Frequency-weighted mean | 46 | 70.4 | 13.5 | 26.7 | 30.4 | 71.7 | 69.5 | 35.3 | 6.8 | 1.7 |
| Range | 34.4-65.9 | 50.4-90.6 | 9.2-16.8 | 19-33.9 | 24-38 | 69.8-74 | - | - | 4.5-9 | 0.6-2.9 |
UCLA, University of California Los Angeles; ASES, American Shoulder and Elbow Surgeons; DASH, Disabilities of the Arm, Shoulder, Hand; VAS, visual analog scale.
Six studies evaluated outcomes based on the UCLA score with a preoperative frequency-weighted mean of 13.5 improving to 26.7, significantly above the MCID of 3.5 points.70 This was a statistically significant difference with a P value = .001.
Two studies used the ASES score with a preoperative mean of 30.4 improving to 71.7 and a total difference of 41.3 which is well above the MCID of 15.2 points for this outcome measurement.47 This change, however, was not statistically significant with a P value = .12; however, there were only two studies using this outcome score. Finally, 1 study reported outcomes based on the DASH score with an improvement of 35.2 points (69.5 to 35.3), again above the reported MCID average of 13 points.39
Patient satisfaction was reported in 13 studies (n=587). Postoperative satisfaction was reported based on percentage, categorical ranking, or a 5-point VAS scale. Seven studies (n=165) used categorial rankings of very satisfied/excellent, satisfied/good, neutral, and dissatisfied/unhappy, with 80% of patients having satisfied/good outcomes or above. Five studies (n = 390) reported satisfaction in percentage, with 84.5% of patients being satisfied or very satisfied with their outcomes. One study (n = 32) reported satisfaction on a 5-point VAS scale with 5 being the most satisfied with a range of 0.8-4.5.
Rehab protocol
Across the 16 studies included, there were a variety of rehab protocols. Two major postoperative pathways were used: Eight studies opted for active ROM and activity as tolerated immediately, while the other 8 studies began with passive ROM and gradual return to activities. For the gradual return protocol, patients began passive ROM on average on postoperative day 1, including passive, passive-assisted, and pendulum exercises. Active ROM typically began around the 4-week mark. Most studies limited strengthening exercises until 6 weeks postoperatively.
Range of motion
The frequency-weighted mean preoperative and postoperative forward flexion, abduction, and internal and external rotation were calculated where applicable. Results are shown in Table III.
Table III.
Frequency-weighted mean preoperatively and postoperatively for range of motion.
| Forward flexion, 11 studies, n = 504 |
Abduction, 6 studies, n = 132 |
External rotation, 4 studies, n = 431 |
Internal rotation, 3 studies, n = 360 |
|||||
|---|---|---|---|---|---|---|---|---|
| Preop | Postop | Preop | Postop | Preop | Postop | Preop | Postop | |
| Frequency-weighted mean (degrees) | 122.1 | 157.7 | 103.1 | 138 | 44.4 | 40.2 | T12 | T10 |
| Range | 91.1-170 | 122-170 | 86.4-125 | 103.5-160 | 20-52.5 | 36.2-68.1 | - | - |
Complications
There were 14 studies that discussed complications associated with AD of iRCTs. No intraoperative complications were noted, but 24 patients had postoperative complications, which are detailed in Table IV. The overall mean pooled complication rate was 4.1%.
Table IV.
Complications related to extensive arthroscopic debridement.
| Author, year | No. of patients | Complication |
|---|---|---|
| Burkhart et al, 19916 | 1 | Rupture of the long head of the biceps |
| Walch et al, 200569 | 19 | Superficial wound infection (1) Postoperative stiffness (15) Traumatic anterior shoulder dislocation (3) |
| Liem et al, 200845 | NR | |
| Veado et al, 201567 | NR | |
| Pander et al, 201858 | NR | |
| Park et al, 201659 | NR | |
| Berth et al, 20104 | 1 | Glenohumeral arthritis |
| Melillo et al, 199749 | N/A | |
| Lee et al, 201141 | N/A | |
| Verhelst et al, 201068 | 1 | Continued pain > clinical failure |
| Scheibel et al, 200461 | 1 | Postop hematoma |
| Ho et al, 202030 | 1 | Draining portal sites |
| Mirzaee et al, 201952 | NR | |
| Maillot et al, 201846 | NR | |
| Heuberer et al, 201629 | NR | |
| Klinger et al, 200538 | NR |
NR, none reported; N/A, complications not discussed.
Subsequent procedures
Forty-nine patients (7%) required reoperation, which most commonly was a reverse total shoulder arthroplasty (rTSA) for the development of progressive rotator cuff arthropathy (n = 19). Other procedures included 17 rotator cuff repairs, 10 hemiarthroplasties for glenohumeral arthritis, 1 arthroscopic irrigation and débridement for infection, 1 distal clavicle excision for persistent acromioclavicular joint pain, and 1 manipulation under anesthesia for postoperative stiffness at 3 months postoperatively. Of the 17 patients who underwent subsequent rotator cuff repairs, 1 was due to a traumatic subscapularis tear after a dislocation event, 2 initially elected against repair based off of compliance to postoperative rehabilitation protocols at the time of their study procedure but later had repair,65 and 14 were initially randomized into a debridement group as part of their original study participation, eventually undergoing repair at a later date.46
Discussion
The iRCTs remain a challenging pathology for both the treating surgeon and patients.67 The results of this study demonstrate that AD procedures for iRCTs lead to good improvement in midterm to long-term function and patient-reported outcomes. Of the 16 included studies, all showed clinically significant improvement in patient-reported outcomes (ASES, Constant, UCLA, DASH), pain (VAS), and ROM. Across the included studies, AD appeared to be a safe and reproducible procedure with a relatively low risk of complication (4.1%). The most commonly performed subsequent procedure was rTSA (7%) for progressive rotator cuff arthropathy. In further scrutiny of the included studies, positive prognostic factors influencing improvement in pain/outcomes including normal preoperative ROM, posterior and anterior rotator cuff (RC) strength/integrity, and minimal glenohumeral osteoarthritis were identified; however, a detailed analysis could not be performed. Several theories have been proposed to explain the observed improvements in patients with massive iRCTs undergoing AD. Burkhart et al described force coupling through which balance between the deltoid and the inferior rotator cuff created a fulcrum at the glenohumeral joint that can maintain equilibrium at all angles of humeral rotation in the coronal plane.6 This potentially explains why patients are able to maintain near-normal ROM in the settings of massive iRCTs, but this can vary depending on involvement of posterior or anterior cuff tendons.16 The included studies showed populations older than 65 years had significant satisfaction with AD, possibly due to pain relief having greater importance than gains of shoulder motion or function. It is important to understand this and discuss patients’ expectations and goals preoperatively to better strategize the appropriate treatments for maximum benefit.
As this review includes multiple modalities of treatment in AD, several included studies investigated the utility of biceps tenotomy and/or acromioplasty/tuberoplasty separately in affecting outcomes in massive iRCTs. Overall, biceps tenotomy showed favorable improvement in outcome and pain scores. Factors contributing to this were suspected biceps pathology contributing to rotator cuff pain. Walch et al observed pain relief in the setting of spontaneous long head of the biceps ruptures in patients with massive iRCTs when being managed nonoperatively.69 With arthroscopic biceps tenotomy in the same patient population, they noted similar improvement in pain and secondary improvement in ROM. It was noted in these studies involving biceps tenotomy that there were decreases in the acromiohumeral intervals, likely owing to the long head of the biceps acting as a secondary humeral head depressor.38,63 Interestingly, patients still experienced improvement in pain and measured outcomes with observed superior humeral head migration.38,63
Studies evaluating acromioplasty/tuberoplasty demonstrated similar results in the population older than 65 years with improved results in strength, pain, and ROM with mean follow-up of 18-98 months.30,34,41,52,59,61,68 Rotator cuff tear size, chronicity, and aggressive acromial pattern were predictors of poor results seen across these studies.41,61,41,68 A loss of acromiohumeral distance as well as continued progression of arthropathy was noted; however, these changes did not seem to influence the improvements observed.
Four comparison studies between AD versus partial rotator cuff repair and/or complete rotator cuff repair were included. Berth et al demonstrated improvement in Constant and DASH scores in both PR and AD groups.4 The final analysis showed slightly better functional outcomes at 24 months in follow-up, favoring PR over AD (P < .01), even though ultrasonography displayed failure of repair in 52% of patients. Melillo et al demonstrated improvement in UCLA scores with both open rotator cuff repair with Neer acromioplasty and AD at short- to mid-term range follow-up (2-4 years); however, the AD group showed worsening pain and functional scores leading to 87% of the AD group needing subsequent procedures in long-term follow-up.49 Maillot et al demonstrated initial improvement in Constant and VAS scores when comparing CR, repair with xenograft patch augmentation, and AD in the short-term follow-up period.46 However, Constant scores did not continue to improve in the AD group at 12 and 24 months of follow-up as was shown with the CR/patch augmentation groups. Heuberer et al demonstrated significant improvement in Constant, VAS, and qDASH scores for AD, PR, and CR at median follow-up of 42 months with similar satisfaction scores (AD 87%; PR 86%; CR 91%).29 Rerupture rates of PR and CR in the setting of massive iRCT have been shown to range from 42% to 94%.4,11,23,29,36,48 Interestingly, patients with intact repairs and repair reruptures still demonstrated significant improvement in functional outcomes and pain scores at short- to midterm follow-up vists.23,29,46 While comparing patient-reported outcome measures with arthroscopic partial/complete rotator cuff repair, constant scores demonstrated a mean improvement in AD of 25 points, with arthroscopic partial/complete rotator cuff repair improving 27-52,4,29,46,49,69 both exceeding the Constant MCID of 10.4.70
Latissimus dorsi transfer (LDT) is a treatment option for iRCTs described in relatively young patients without glenohumeral osteoarthritis or subscapularis insufficiency and minimal teres minor fatty infiltration.1,13,31,43,53,57 LDT has been reported to show good pain relief, function, and strength with good or excellent results in 74% of patients at a mean of 9-10 years.20,24,54 However, progression of glenohumeral arthritis in approximately one-third of patients as well as high rates of tendon rupture have been reported.1,24,33,60 These patients would also require a long rehabilitation process and compliance to postoperative restrictions, which may limit the population that LDT may benefit. Comparison of Constant/ASES scores of this study to those of other studies showed similar score improvements between AD and LDT (AD constant 25, LDT constant 26-28; AD ASES 41.4, LDT 40.1).20,54 This review, however, found no studies showing a direct comparison of outcomes between AD and LDT or other tendon transfer options (lower trapezius, pectoralis major, combination transfers) in the setting of massive iRCT; therefore, further investigation is warranted.
Other alternative procedures in iRCTs include placing static restraints superior to the humeral head to maintain native a glenohumeral relationship and improve shoulder biomechanics. The use of a subacromial balloon spacer has been proposed as a minimally invasive palliative procedure that seeks to prevent humeral head elevation, thereby centering the humeral head in the glenoid and improving the ability of the deltoid to actively elevate the arm. Senekovic et al reported maintained functional improvements at a mean follow-up of 5 years, even though the balloon is designed to degrade 2-12 months after implantation.62 Other limited studies showed favorable short-term outcomes with recognition that further prospective randomized or comparative studies are warranted to ascertain clinical outcomes of subacromial balloon spacers in the management of massive and iRCTs.20,64 A comparison of Constant scores of this study to those of other studies showed a slight improvement in subacromial balloon spacer over AD (AD 25; subacromial balloon spacer 27.7-35.5).62,64 However, this review included no studies directly comparing outcomes of AD versus subacromial balloon spacer implantation in iRCT, and further studies will be necessary to evaluate these palliative treatments.
SCR is another emerging technique in the treatment of iRCTs in which autograft fascia lata or acellular dermal allograft is anchored to recreate a static superior capsule and prevent superior humeral migration. Early results have shown success rates averaging 84% and marked improvement in postoperative ROM, VAS, and ASES scores for iRCTs in younger patients (age < 65 years) with low-grade RC arthropathy (Hamada grade 1-2) at 12-34 months in follow-up.15,50,51 Other studies have demonstrated SCR graft retear rates from 36% to 55% on MRI at 1-year postoperative follow-ups; however, graft thickness, postoperative acromiohumeral distance, and remnant posterior rotator cuff tissue integrity must be considered.15,42 SCR is a technically challenging procedure that requires prolonged surgical time, a substantial rehabilitation period, and strict adherence to postoperative ROM and weight-bearing restrictions. Comparison of ASES scores of this study to those of other studies showed a similar improvement in AD to SCR (AD 41.4; SCR 30-55).19 Our review contains no studies directly comparing outcomes of AD versus SCR in iRCT treatment, and further research must be performed to assess this.
Finally, rTSA has been increasingly used for iRCTs with and without glenohumeral osteoarthritis. Current recommendations indicate rTSA in patients with intermediate- to advanced-stage rotator cuff arthropathy (Hamada grade 3 or greater), anterosuperior escape, severe pseudoparalysis, and/or those older than 65 years demonstrating reliable pain relief and improved function in long-term outcomes.2,14 However, Hartzler et al found an association between poor outcomes at a minimum of 2 years in follow-up in patients who underwent rTSA for iRCT without arthritis and age < 60 years, high preoperative function, and neurologic dysfunction.28 Ernstbrunner et al reported a series of rTSA for patients younger than 60 years with a mean follow-up period of 11.7 years, finding subjective and functional improvement but with 39% complication rate and 9% failure rate.22 Also, rTSA can be an extensive and technically complex surgery associated with relatively high complication rates and limited salvage options, especially among younger patients with high-demand jobs and activities. Comparison of Constant scores of this study to those of other studies showed a similar improvement in AD to rTSA (AD 25; rTSA 28.3-32).2,66 Our review contains no studies directly comparing outcomes of AD versus rTSA in iRCTs.
As AD does not directly address the underlying problem of the ruptured RC tendons, functional improvements cannot be expected to match outcomes after rotator cuff repair, reconstructive techniques, or rTSA. Given the improvement in functional outcomes and pain scores at midterm follow-up demonstrated in this review, AD remains an effective treatment modality for the population older than 65 years who seek pain relief and have lower functional demands. Overall improvement in patient-reported outcomes, ROM, and patient satisfaction can be expected. However, there is still a need to determine which procedure is best for optimizing outcomes.
Limitations
Weaknesses of this study include those inherent to any systematic review. Each individual study characteristics such as its retrospective design, limited case series, short-term follow-up, and so on can translate into limitations of this review. The lack of randomization and controls for bias, confounding factors, or chance could have influenced results. In addition, as we elected to group multiple modalities of treatment under one entity (AD), we cannot comment on which of these modalities ranks superior to one another as no studies available provided data in direct comparison analysis. As such, our study is simply an observational review of mostly observational studies, but it does provide an overview of the literature available. Weaknesses inherent to the individual studies are not improved by aggregating them. Furthermore, although we used a systematic methodology that we believe to be reproducible, it is possible that different search terms and different search engines would have provided additional studies that would have met our inclusion criteria. Only two studies provided a breakdown of the patient-reported outcomes based on the patient's age. The authors recognize that further delineation of outcomes based on age would provide further insight as to what population age group potentially would receive the most benefit with AD.
Conclusion
AD in combination with at least one of the following procedures—subacromial decompression, tuberoplasty, subacromial bursectomy, and/or biceps tenotomy—for the treatment of massive iRCTs, produces good functional outcomes and improvement in pain at midterm to long-term follow-up for the low-demand population older than 65 years looking for pain relief over substantial increase in function.
Disclaimers
Funding: There was no external funding for this study.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
The investigation was performed at the Department of Orthopaedic Surgery, Franciscan Heath-Olympia Fields, Olympia Fields, IL, USA.
Institutional review board approval was not required for this systematic review.
References
- 1.Aoki M., Okamura K., Fukushima S., Takahashi T., Ogino T. Transfer of latissimus dorsi for irreparable rotator-cuff tears. J Bone Joint Surg Br. 1996;78:761–766. [PubMed] [Google Scholar]
- 2.Bacle G., Nové-Josserand L., Garaud P., Walch G. Long-term outcomes of reverse total shoulder arthroplasty: a follow-up of a previous study. J Bone Joint Surg Am. 2017;99:454–461. doi: 10.2106/JBJS.16.00223. [DOI] [PubMed] [Google Scholar]
- 3.Beason D.P., Tucker J.J., Lee C.S., Edelstein L., Abboud J.A., Soslowsky L.J. Rat rotator cuff tendon-to-bone healing properties are adversely affected by hypercholesterolemia. J Shoulder Elbow Surg. 2014;23:867–872. doi: 10.1016/j.jse.2013.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berth A., Neumann W., Awiszus F., Pap G. Massive rotator cuff tears: functional outcome after débridement or arthroscopic partial repair. J Orthop Traumatol. 2010;11:13–20. doi: 10.1007/s10195-010-0084-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boileau P., Brassart N., Watkinson D.J., Carles M., Hatzidakis A.M., Krishnan S.G. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87:1229–1240. doi: 10.2106/JBJS.D.02035. [DOI] [PubMed] [Google Scholar]
- 6.Burkhart S.S. Arthroscopic treatment of massive rotator cuff tears. Clinical results and biomechanical rationale. Clin Orthop Relat Res. 1991;267:45–56. [PubMed] [Google Scholar]
- 7.Burkhart S.S., Nottage W.M., Ogilvie-Harris D.J., Kohn H.S., Pachelli A. Partial repair of irreparable rotator cuff tears. Arthroscopy. 1994;10:363–370. doi: 10.1016/s0749-8063(05)80186-0. [DOI] [PubMed] [Google Scholar]
- 8.Burnier M., Elhassan B.T., Sanchez-Sotelo J. Surgical management of irreparable rotator cuff tears: what works, what does not, and what is coming. J Bone Joint Surg Am. 2019;101:1603–1612. doi: 10.2106/JBJS.18.01392. [DOI] [PubMed] [Google Scholar]
- 9.Carbone S., Gumina S., Arceri V., Campagna V., Fagnani C., Postacchini F. The impact of preoperative smoking habit on rotator cuff tear: cigarette smoking influences rotator cuff tear sizes. J Shoulder Elbow Surg. 2012;21:56–60. doi: 10.1016/j.jse.2011.01.039. [DOI] [PubMed] [Google Scholar]
- 10.Catapano M., de Sa D., Ekhtiari S., Lin A., Bedi A., Lesniak B.P. Arthroscopic superior capsular reconstruction for massive, irreparable rotator cuff tears: a systematic review of modern literature. Arthroscopy. 2019;35:1243–1253. doi: 10.1016/j.arthro.2018.09.033. [DOI] [PubMed] [Google Scholar]
- 11.Choi S., Kim M.K., Kim G.M., Roh Y.H., Hwang I.K., Kang H. Factors associated with clinical and structural outcomes after arthroscopic rotator cuff repair with a suture bridge technique in medium, large, and massive tears. J Shoulder Elbow Surg. 2014;23:1675–1681. doi: 10.1016/j.jse.2014.02.021. [DOI] [PubMed] [Google Scholar]
- 12.Cofield R.H. Rotator cuff disease of the shoulder. J Bone Joint Surg Am. 1985;67:974–979. [PubMed] [Google Scholar]
- 13.Costouros J.G., Espinosa N., Schmid M.R., Gerber C. Teres minor integrity predicts outcome of latissimus dorsi tendon transfer for irreparable rotator cuff tears. J Shoulder Elbow Surg. 2007;16:727–734. doi: 10.1016/j.jse.2007.02.128. [DOI] [PubMed] [Google Scholar]
- 14.Cvetanovich G.L., Waterman B.R., Verma N.N., Romeo A.A. Management of the Irreparable Rotator Cuff Tear. J Am Acad Orthop Surg. 2019;27:909–917. doi: 10.5435/JAAOS-D-18-00199. [DOI] [PubMed] [Google Scholar]
- 15.Denard P.J., Brady P.C., Adams C.R., Tokish J.M., Burkhart S.S. Preliminary results of arthroscopic superior capsule reconstruction with dermal allograft. Arthroscopy. 2018;34:93–99. doi: 10.1016/j.arthro.2017.08.265. [DOI] [PubMed] [Google Scholar]
- 16.DePalma A.F., Callery G., Bennett G.A. Variational anatomy and degenerative lesions of the shoulder joint. Instr Course Lect. 1949;6:255. [Google Scholar]
- 17.Deranlot J., Herisson O., Nourissat G., Zbili D., Werthel J.D., Vigan M., Bruchou F. Arthroscopic subacromial spacer implantation in patients with massive irreparable rotator cuff tears: clinical and radiographic results of 39 retrospectives cases. Arthroscopy. 2017;33:1639–1644. doi: 10.1016/j.arthro.2017.03.029. Erratum in: Arthroscopy. 2018 Feb;34(2):647. [DOI] [PubMed] [Google Scholar]
- 18.Dwyer T., Razmjou H., Henry P., Gosselin-Fournier S., Holtby R. Association between pre-operative magnetic resonance imaging and reparability of large and massive rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2015;23:415–422. doi: 10.1007/s00167-013-2745-z. [DOI] [PubMed] [Google Scholar]
- 19.Ekhtiari S., Adili A.F., Memon M., et al. Sources, quality, and reported outcomes of superior capsular reconstruction: a systematic review. Curr Rev Musculoskelet Med. 2019;12:173–180. doi: 10.1007/s12178-019-09551-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.El-Azab H.M., Rott O., Irlenbusch U. Long-term follow-up after latissimus dorsi transfer for irreparable posterosuperior rotator cuff tears. J Bone Joint Surg Am. 2015;97:462–469. doi: 10.2106/JBJS.M.00235. [DOI] [PubMed] [Google Scholar]
- 21.Elhassan B.T., Wagner E.R., Werthel J.D. Outcome of lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tear. J Shoulder Elbow Surg. 2016;25:1346–1353. doi: 10.1016/j.jse.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 22.Ernstbrunner L., Suter A., Catanzaro S., Rahm S., Gerber C. Reverse total shoulder arthroplasty for massive, irreparable rotator cuff tears before the age of 60 years: long-term results. J Bone Joint Surg Am. 2017;99:1721–1729. doi: 10.2106/JBJS.17.00095. [DOI] [PubMed] [Google Scholar]
- 23.Galatz L.M., Ball C.M., Teefey S.A., Middleton W.D., Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86:219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Gerber C. Latissimus dorsi transfer for the treatment of irreparable tears of the rotator cuff. Clin Orthop Relat Res. 1992:152–160. [PubMed] [Google Scholar]
- 25.Gerber C., Fuchs B., Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82:505–515. doi: 10.2106/00004623-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Goutallier D., Le Guilloux P., Postel J.M., Radier C., Bernageau J., Zilber S. Acromio humeral distance less than six millimeter: its meaning in full-thickness rotator cuff tear. Orthop Traumatol Surg Res. 2011;97:246–251. doi: 10.1016/j.otsr.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 27.Goutallier D., Postel J.M., Bernageau J., Lavau L., Voisin M.C. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994:78–83. [PubMed] [Google Scholar]
- 28.Hartzler R.U., Steen B.M., Hussey M.M., Cusick M.C., Cottrell B.J., Clark R.E., et al. Reverse shoulder arthroplasty for massive rotator cuff tear: risk factors for poor functional improvement. J Shoulder Elbow Surg. 2015;24:1698–1706. doi: 10.1016/j.jse.2015.04.015. [DOI] [PubMed] [Google Scholar]
- 29.Heuberer P.R., Kölblinger R., Buchleitner S., Pauzenberger L., Laky B., Auffarth A., et al. Arthroscopic management of massive rotator cuff tears: an evaluation of débridement, complete, and partial repair with and without force couple restoration. Knee Surg Sports Traumatol Arthrosc. 2015 doi: 10.1007/s00167-015-3739-9. 6;24:3828-3837. [DOI] [PubMed] [Google Scholar]
- 30.Ho J.C., Kane L., Stone M.A., Romeo A.A., Abboud J.A., Namdari S. Arthroscopic débridement of irreparable rotator cuff tears: predictors of failure and success. J Shoulder Elbow Surg. 2020;29:e118–e123. doi: 10.1016/j.jse.2019.08.010. [DOI] [PubMed] [Google Scholar]
- 31.Iannotti J.P., Hennigan S., Herzog R., Kella S., Kelley M., Leggin B., et al. Latissimus dorsi tendon transfer for irreparable posterosuperior rotator cuff tears. Factors affecting outcome. J Bone Joint Surg Am. 2006;88:342–348. doi: 10.2106/JBJS.D.02996. [DOI] [PubMed] [Google Scholar]
- 32.Jeong H.Y., Kim H.J., Jeon Y.S., Rhee Y.G. Factors predictive of healing in large rotator cuff tears: is it possible to predict retear preoperatively? Am J Sports Med. 2018;46:1693–1700. doi: 10.1177/0363546518762386. [DOI] [PubMed] [Google Scholar]
- 33.Kany J., Grimberg J., Amaravathi R.S., Sekaran P., Scorpie D., Werthel J.D. Arthroscopically-assisted latissimus dorsi transfer for irreparable rotator cuff insufficiency: modes of failure and clinical correlation. Arthroscopy. 2018;34:1139–1150. doi: 10.1016/j.arthro.2017.10.052. [DOI] [PubMed] [Google Scholar]
- 34.Kempf J.F., Gleyze P., Bonnomet F., Walch G., Mole D., Frank A., et al. A multicenter study of 210 rotator cuff tears treated by arthroscopic acromioplasty. Arthroscopy. 1999;15:56–66. doi: 10.1053/ar.1999.v15.015005. [DOI] [PubMed] [Google Scholar]
- 35.Khair M.M., Gulotta L.V. Treatment of irreparable rotator cuff tears. Curr Rev Musculoskelet Med. 2011;4:208–213. doi: 10.1007/s12178-011-9098-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim J.R., Cho Y.S., Ryu K.J., Kim J.H. Clinical and radiographic outcomes after arthroscopic repair of massive rotator cuff tears using a suture bridge technique: assessment of repair integrity on magnetic resonance imaging. Am J Sports Med. 2012;40:786–793. doi: 10.1177/0363546511434546. [DOI] [PubMed] [Google Scholar]
- 37.Kim J.Y., Park J.S., Rhee Y.G. Can preoperative magnetic resonance imaging predict the reparability of massive rotator cuff tears? Am J Sports Med. 2017;45:1654–1663. doi: 10.1177/0363546517694160. [DOI] [PubMed] [Google Scholar]
- 38.Klinger H.M., Steckel H., Ernstberger T., Baums M.H. Arthroscopic débridement of massive rotator cuff tears: negative prognostic factors. Arch Orthop Trauma Surg. 2005;125:261–266. doi: 10.1007/s00402-004-0738-6. [DOI] [PubMed] [Google Scholar]
- 39.Koorevaar R.C.T., Kleinlugtenbelt Y.V., Landman E.B.M., van 't Riet E., Bulstra S.K. Psychological symptoms and the MCID of the DASH score in shoulder surgery. J Orthop Surg Res. 2018;13:246. doi: 10.1186/s13018-018-0949-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Le B.T., Wu X.L., Lam P.H., Murrell G.A. Factors predicting rotator cuff retears: an analysis of 1000 consecutive rotator cuff repairs. Am J Sports Med. 2014;42:1134–1142. doi: 10.1177/0363546514525336. [DOI] [PubMed] [Google Scholar]
- 41.Lee B.G., Cho N.S., Rhee Y.G. Results of arthroscopic decompression and tuberoplasty for irreparable massive rotator cuff tears. Arthroscopy. 2011;27:1341–1350. doi: 10.1016/j.arthro.2011.06.016. [DOI] [PubMed] [Google Scholar]
- 42.Lee S.J., Min Y.K. Can inadequate acromiohumeral distance improvement and poor posterior remnant tissue be the predictive factors of re-tear? Preliminary outcomes of arthroscopic superior capsular reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26:2205–2213. doi: 10.1007/s00167-018-4912-8. [DOI] [PubMed] [Google Scholar]
- 43.Lehmann L.J., Mauerman E., Strube T., Laibacher K., Scharf H.P. Modified minimally invasive latissimus dorsi transfer in the treatment of massive rotator cuff tears: a two-year follow-up of 26 consecutive patients. Int Orthop. 2010;34:377–383. doi: 10.1007/s00264-009-0782-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P., et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 45.Liem D., Lengers N., Dedy N., Poetzl W., Steinbeck J., Marquardt B. Arthroscopic débridement of massive irreparable rotator cuff tears. Arthroscopy. 2008;24:743–748. doi: 10.1016/j.arthro.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 46.Maillot C., Harly E., Demezon H., Le Huec J.C. Surgical repair of large-to-massive rotator cuff tears seems to be a better option than patch augmentation or débridement and biceps tenotomy: a prospective comparative study. J Shoulder Elbow Surg. 2018;27:1545–1552. doi: 10.1016/j.jse.2018.05.023. [DOI] [PubMed] [Google Scholar]
- 47.Malavolta E.A., Yamamoto G.J., Bussius D.T., Assunção J.H., Andrade-Silva F.B., Gracitelli M.E.C., et al. Establishing minimal clinically important difference for the UCLA and ASES scores after rotator cuff repair. Orthop Traumatol Surg Res. 2021:102894. doi: 10.1016/j.otsr.2021.102894. [DOI] [PubMed] [Google Scholar]
- 48.Maman E., Yehuda C., Pritsch T., Morag G., Brosh T., Sharfman Z., et al. Detrimental effect of repeated and single subacromial corticosteroid injections on the intact and injured rotator cuff: a biomechanical and imaging study in rats. Am J Sports Med. 2016;44:177–182. doi: 10.1177/0363546515591266. [DOI] [PubMed] [Google Scholar]
- 49.Melillo A.S., Savoie F.H., Field L.D. Massive rotator cuff tears: débridement versus repair. Orthop Clin North Am. 1997;28:117–124. doi: 10.1016/s0030-5898(05)70269-8. [DOI] [PubMed] [Google Scholar]
- 50.Mihata T., Lee T.Q., Fukunishi K., Itami Y., Fujisawa Y., Kawakami T., et al. Return to sports and physical work after arthroscopic superior capsule reconstruction among patients with irreparable rotator cuff tears. Am J Sports Med. 2018;46:1077–1083. doi: 10.1177/0363546517753387. [DOI] [PubMed] [Google Scholar]
- 51.Mihata T., Lee T.Q., Watanabe C., Fukunishi K., Ohue M., Tsujimura T., et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 52.Mirzaee F., Aslani M.A., Zafarani Z., Aslani H. Treatment of massive irreparable rotator cuff tear with arthroscopic subacromial bursectomy, biceps tenotomy, and tuberoplasty. Arch Bone Jt Surg. 2019;7:263–268. No doi. [PMC free article] [PubMed] [Google Scholar]
- 53.Moursy M., Forstner R., Koller H., Resch H., Tauber M. Latissimus dorsi tendon transfer for irreparable rotator cuff tears: a modified technique to improve tendon transfer integrity. J Bone Joint Surg Am. 2009;91:1924–1931. doi: 10.2106/JBJS.H.00515. [DOI] [PubMed] [Google Scholar]
- 54.Namdari S., Voleti P., Baldwin K., Glaser D., Huffman G.R. Latissimus dorsi tendon transfer for irreparable rotator cuff tears: a systematic review. J Bone Joint Surg Am. 2012;94:891–898. doi: 10.2106/JBJS.K.00841. [DOI] [PubMed] [Google Scholar]
- 55.Neyton L., Godenèche A., Nové-Josserand L., Carrillon Y., Cléchet J., Hardy M.B. Arthroscopic suture-bridge repair for small to medium size supraspinatus tear: healing rate and retear pattern. Arthroscopy. 2013;29:10–17. doi: 10.1016/j.arthro.2012.06.020. [DOI] [PubMed] [Google Scholar]
- 56.Nobuhara K., Hata Y., Komai M. Surgical procedure and results of repair of massive tears of the rotator cuff. Clin Orthop Relat Res. 1994:54–59. [PubMed] [Google Scholar]
- 57.Nyffeler R.W., Werner C.M., Sukthankar A., Schmid M.R., Gerber C. Association of a large lateral extension of the acromion with rotator cuff tears. J Bone Joint Surg Am. 2006;88:800–805. doi: 10.2106/JBJS.D.03042. [DOI] [PubMed] [Google Scholar]
- 58.Pander P., Sierevelt I.N., Pecasse G.A.B.M., van Noort A. Irreparable rotator cuff tears: long-term follow-up, five to ten years, of arthroscopic débridement and tenotomy of the long head of the biceps. Int Orthop. 2018;42:2633–2638. doi: 10.1007/s00264-018-3991-y. [DOI] [PubMed] [Google Scholar]
- 59.Park J.G., Cho N.S., Song J.H., Baek J.H., Rhee Y.G. Long-term outcome of tuberoplasty for irreparable massive rotator cuff tears: is tuberoplasty really applicable? J Shoulder Elbow Surg. 2016;25:224–231. doi: 10.1016/j.jse.2015.07.025. [DOI] [PubMed] [Google Scholar]
- 60.Petriccioli D., Bertone C., Marchi G. Recovery of active external rotation and elevation in young active men with irreparable posterosuperior rotator cuff tear using arthroscopically assisted latissimus dorsi transfer. J Shoulder Elbow Surg. 2016;25:e265–e675. doi: 10.1016/j.jse.2015.12.011. [DOI] [PubMed] [Google Scholar]
- 61.Scheibel M., Lichtenberg S., Habermeyer P. Reversed arthroscopic subacromial decompression for massive rotator cuff tears. J Shoulder Elbow Surg. 2004;13:272–278. doi: 10.1016/j.jse.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 62.Senekovic V., Poberaj B., Kovacic L., Mikek M., Adar E., Markovitz E., et al. The biodegradable spacer as a novel treatment modality for massive rotator cuff tears: a prospective study with 5-year follow-up. Arch Orthop Trauma Surg. 2017;137:95–103. doi: 10.1007/s00402-016-2603-9. [DOI] [PubMed] [Google Scholar]
- 63.Slim K., Nini E., Forestier D., Kwiatkowski F., Panis Y., Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 64.Stewart R.K., Kaplin L., Parada S.A., Graves B.R., Verma N.N., Waterman B.R. Outcomes of subacromial balloon spacer implantation for massive and irreparable rotator cuff tears: a systematic review. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119875717. 232596711987571-2325967119875717: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tokish J.M., Alexander T.C., Kissenberth M.J., Hawkins R.J. Pseudoparalysis: a systematic review of term definitions, treatment approaches, and outcomes of management techniques. J Shoulder Elbow Surg. 2017;26:e177–e187. doi: 10.1016/j.jse.2017.02.024. [DOI] [PubMed] [Google Scholar]
- 66.Torrens C., Guirro P., Santana F. The minimal clinically important difference for function and strength in patients undergoing reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25:262–268. doi: 10.1016/j.jse.2015.07.020. [DOI] [PubMed] [Google Scholar]
- 67.Veado M.A., Rodrigues A.U. Functional evaluation of patients who have undergone arthroscopic débridement to treat massive and irreparable tears of the rotator cuff. Rev Bras Ortop. 2015;45:426–431. doi: 10.1016/S2255-4971(15)30431-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Verhelst L., Vandekerckhove P.J., Sergeant G., Liekens K., Van Hoonacker P., Berghs B. Reversed arthroscopic subacromial decompression for symptomatic irreparable rotator cuff tears: mid-term follow-up results in 34 shoulders. J Shoulder Elbow Surg. 2010;19:601–608. doi: 10.1016/j.jse.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 69.Walch G., Edwards T.B., Boulahia A., Nové-Josserand L., Neyton L., Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg. 2005;14:238–246. doi: 10.1016/j.jse.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 70.Xu S., Chen J.Y., Lie H.M.E., Hao Y., Lie D.T.T. Determination of threshold scores for treatment success after arthroscopic rotator cuff repair using oxford, constant, and university of california, los angeles shoulder scores. Arthroscopy. 2019;35:304–311. doi: 10.1016/j.arthro.2018.07.047. [DOI] [PubMed] [Google Scholar]