Abstract
Hypothesis/Background
Value-based healthcare delivery models are becoming increasingly common and are driving cost effectiveness initiatives. Rotator cuff repair (RCR) is a commonly performed procedure with some variations on the specific surgical technique. The purpose of this study was to perform a comprehensive analysis of the cost, complications, and readmission rates of 3 categories of RCR techniques (open [oRCR], combined arthroscopically assisted and mini-open [CRCR], and all arthroscopic [ARCR]) at a high-volume institution.
Methods
All RCR procedures performed by 2 fellowship-trained shoulder surgeons at a single institution between 2012 and 2017 were retrospectively identified. These consisted of oRCR, CRCR, and ARCR repair techniques. One surgeon performed oRCR and CRCR, and the second surgeon performed ARCR. A cost analysis was designed to include a period of 60 days preoperatively, the index surgical hospitalization, and 90 days postoperatively, including costs of any readmission or reoperation.
Results
The cohort consisted of 95 oRCR, 233 CRCR, and 287 ARCR. Median standardized costs were as follows: preoperative evaluation $486.03; index surgical hospitalization oRCR $9,343.10, CRCR $10,057.20, and ARCR $10,330.60; and postoperative care $875.02. Preoperative and postoperative costs did not vary based on the type of RCR performed. However, significant differences were observed among index surgical costs (P = .0008). The highest standardized cost for hospitalization for both the CRCR group and the ARCR group was related to the cost of the operating room and the implants. The 90-day complication, reoperation, and readmission rates were 1.1%, 1.1%, and 2.1% in the open group; 0.8%, 0.8%, and 1.7% in the combination group; 0%, 0%, and 1.7% in the all arthroscopic group, respectively. There were no significant differences among the 3 surgical procedures with respect to complication (P = .26), reoperation (P = .26), and readmission rates (P = .96).
Discussion/Conclusions
In this investigation, the median standardized costs for RCR inclusive of 60-day workup and 90-day postoperative care were $10,704.15, $11,418.25, and $11,691.65 for oRCR, CRCR (average added cost $714.10), and ARCR (added cost $987.50), respectively. The group complication, reoperation, and readmission rate were 0.5%, 0.5%, and 1.8% with no significant differences between the varying techniques, respectively. This retrospective cost analysis and complication profile may serve as a useful reference as surgeons consider engaging in bundled payment for RCR. As value based initiatives continue to progress, implant cost may serve as an actionable area for cost reduction.
Keywords: Cost, Bundled payment, Rotator cuff, Readmission, Complication
Rotator cuff (RC) tears remain one of the most common musculoskeletal conditions, with RC repair (RCR) as a frequently performed orthopedic procedure. Over the past decade, recent reports have demonstrated substantial increases in RCRs with up to a 2-fold growth.7,25 In the United States, more than 250,000 RCRs are performed annually,2,17,19 and in many practices, traditional open approaches have evolved toward more minimally invasive techniques, such as mini-open RCR (mRCR) and all-arthroscopic RCR (aRCR).2,13 Although each surgical approach has demonstrable advantages and disadvantages,7,18 studies have generally validated comparable clinical outcomes and complication profiles among techniques.11,14,23 Despite this, rotator cuff pathology persists as the leading cause of shoulder related disability in orthopedics30 with an associated economic burden accounting for an estimate of $1.2 to 1.6 billion in annual US health care expenditures.5,7,19
In the current era of growing value-based reimbursement models, cost effectiveness initiatives have become a major focus in American economic and health policy.4,22 Bundled payment reimbursement, a key component of value-based models, was formally introduced in 2010 as part of the Patient Protection and Affordable Care Act.15 Since inception, bundled payment programs have become prevalent in hip and knee arthroplasty with evidence demonstrating decreased cost per replacement episode without any associated increase in complication rates.3,27 Although this is not yet widely implemented in the shoulder, certain interest from government and private payers in the near future can be expected.
One essential component of risk-based reimbursement is a clear understanding of the various costs of each element of care, the frequency, and reasons for complications, readmissions, and reoperations.15 With respect to RCRs, previous investigations have evaluated the cost and outcomes of open, mRCR, and aRCR procedures, with general evidence supporting similar complication profiles and increased cost for all-arthroscopic techniques.6,12,20 Moreover, studies have been performed that individually analyzed direct costs of aRCRs,9,22 complications and reoperations within 30 days,2,28 readmissions,2,28 and costs of postoperative physical therapy after RCR.1
Regardless, there continues to be limited data that address all the essential elements in risk-based reimbursement (cost, complications, reoperations, and readmissions) in RCR procedures. Therefore, the purpose of this study was to analyze the cost, 90-day complications, reoperations, and readmission rates of 3 categories of RCR techniques (open [oRCR], combined arthroscopically assisted and mini-open, and all arthroscopic) over a 5-year span at a high-volume institution. We hypothesized that there would be no significant difference among the 90-day complications, reoperations, and readmissions. However, we expected an increase in cost with more minimally invasive techniques, with the all arthroscopic procedures being the most expensive.
Materials and methods
Patient selection
After institutional review board approval, a retrospective review was performed collecting all primary RCRs performed by 2 fellowship-trained orthopedic surgeons between January 2012 and December 2017 at a single institution. A total of 707 consecutive patients ≥ 18 years of age who were diagnosed with a partial or complete RC tear and indicated for RCR were initially identified. To avoid cost miscalculation between preoperative and postoperative services on patients receiving RCRs within a short period, the second case of every pair (n = 25) performed within 1 year was removed from the analysis. Patients were then excluded if they refused to sign Minnesota Research Authorization forms (n = 49) or sustained concomitant procedures (n = 18) other than subacromial decompression, biceps tenodesis or tenotomy, or labrum débridement. After exclusions, we analyzed a final sample of 615 patients: 95 open RCR (oRCR), 233 combined arthroscopically-assisted and mini-open RCR (cRCR), and 287 all-arthroscopic RCR (aRCR) (Fig. 1). Demographics and patient characteristics are detailed in Table I.
Figure 1.
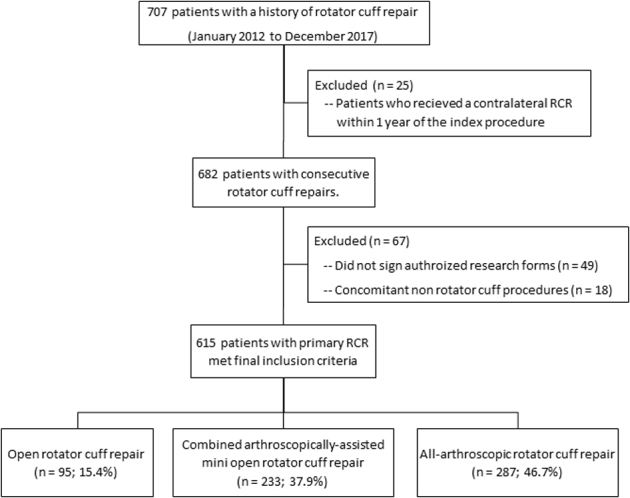
Flow chart of patients included for analysis.
Table I.
Patient demographics and clinical characteristics of rotator cuff repairs.
| Variables | Open repair, n = 95 | Combined mini-open and arthroscopic repair, n = 233 | Arthroscopic repair, n = 287 | Total repairs, n = 615 | P value |
|---|---|---|---|---|---|
| Age (yr ± SD) | 61.1 ± 8.3 | 59 ± 9.2 | 62 ± 9.1 | 60.8 ± 9.1 | <.001 |
| Sex | .37 | ||||
| Male | 63 (66.3%) | 135 (57.9%) | 174 (60.6%) | 372 (60.5%) | |
| Female | 32 (33.7%) | 98 (42.1%) | 113 (39.4%) | 243 (39.5%) | |
| Body mass index (kg/m2) | 31.2 ± 6.1 | 31.3 ± 7 | 31.1 ± 7.3 | 31.2 ± 7 | .95 |
| BMI category | .19 | ||||
| <25 | 12 (13%) | 36 (15.9%) | 56 (21.1%) | 104 (17.8%) | |
| 25-30 | 31 (33.7%) | 68 (30.1%) | 64 (24.2%) | 163 (28%) | |
| >30 | 49 (53.3%) | 122 (54.0%) | 145 (54.7%) | 316 (54.2%) | |
| ASA | .15 | ||||
| 1 | 3 (3.3%) | 18 (9.1%) | 19 (8.5%) | 40 (7.8%) | |
| 2 | 67 (73.6%) | 136 (68.7%) | 137 (6.1%) | 340 (66.3%) | |
| 3 | 19 (20.9%) | 42 (21.2%) | 66 (29.5%) | 127 (24.8%) | |
| 4 | 2 (2.2%) | 2 (1%) | 2 (0.9%) | 6 (1.2%) | |
| Yr of surgery | < .001 | ||||
| 2012 | 29 (30.5%) | 41 (17.6%) | 11 (3.8%) | 81 (13.2%) | |
| 2013 | 35 (36.8%) | 39 (16.7%) | 30 (10.5%) | 104 (16.9%) | |
| 2014 | 16 (16.8%) | 36 (15.5%) | 40 (13.9%) | 92 (15%) | |
| 2015 | 8 (8.4%) | 24 (10.3%) | 88 (30.7%) | 120 (19.5%) | |
| 2016 | 2 (2.1%) | 43 (18.5%) | 61 (21.3%) | 106 (17.2%) | |
| 2017 | 5 (5.3%) | 50 (21.5%) | 57 (19.7%) | 112 (18.2%) | |
| Laterality | .23 | ||||
| Right | 50 (52.6%) | 136 (58.4%) | 179 (62.4%) | 365 (59.3%) | |
| Left | 45 (47.4%) | 97 (41.6%) | 108 (37.6%) | 250 (40.7%) | |
| Anchors (mean ± SD) | 0 | 2.1 ± 1.2 | 3.5 ± 1.4 | 2.4 ± 1.7 | <.001 |
| Biceps procedures | .002 | ||||
| None | 53 (55.8%) | 136 (58.3%) | 159 (55.4%) | 339 (55.1%) | |
| Tenotomy | 8 (8.4%) | 47 (20.1%) | 65 (22.7%) | 120 (19.5%) | |
| Tenodesis | 34 (35.8%) | 50 (21.4%) | 63 (21.9%) | 147 (23.9%) | |
| Surgeon | <.001 | ||||
| Surgeon 1 | 94 (98.9%) | 3 (1.3%) | 186 (64.8%) | 283 (46%) | |
| Surgeon 2 | 1 (1.1%) | 230 (98.7%) | 101 (35.2%) | 332 (54%) | |
| Operative time (min ± SD) | 52.01 (21.8) | 61.3 (14.9) | 74.0 (25.3) | 61.5 (22.6) | <.001 |
| Length of stay (d ± SD) | 1.2 (0.6) | 1.2 (0.8) | 0.5 (0.7) | 1.0 (0.7) | <.001 |
BMI, body mass index; ASA, American Society of Anesthesiologists; SD, standard deviation.
Bolded P values represent the differences across all the columns.
Surgical techniques
All 3 techniques were performed under general anesthesia with the use of standard beach-chair position and disposable shoulder drapes. As per institutional protocol, each patient received a 1 shot single scalene nerve block, and all RC foot prints were prepared with the use of a motorized burr. In the oRCR technique, an anterolateral deltoid-splitting approach was used. Rotator cuff tears were repaired using transosseous non-absorbabe sutures. As such, no suture anchors were used. The long head of the biceps tendon (LHBT) was intact and unremarkable in 53 (55.8%) cases. Concomitant biceps tenotomy or tenodesis was performed in 8 (8.4%) and 34 (35.8%) of cases, respectively. LHBT tenodesis was performed using soft tissue or bone tunnels with suture fixation.
In the cRCR cases, a two-portal technique was created for diagnostic arthroscopy and analysis of the tear pattern. Then, a 1- to 2-cm anterolateral deltoid-splitting approach was used for repair. Tears were fixed with a combination of nonabsorbable suture and suture anchors. The mean number of suture anchors used was 2.1 ± 1.2 anchors. The LHBT was intact and unremarkable in 136 (58.3%) cases. Concomitant biceps tenotomy or tenodesis was performed in 47 (20.1%) and 50 (21.4%) of cases, respectively. LHBT tenodesis was performed using soft tissue or bone tunnels with suture fixation.
In the aRCR cases, 3 or more portals were used for diagnostic arthroscopy, tear pattern analysis, and fixation. Tears were fixed primarily with the use of knotless suture anchors. Single- or double-row repairs were performed based on tear pattern and surgeon preference. The mean number of suture anchors used was 3.5 ± 1.4 anchors. The LHBT was intact and unremarkable in 159 (55.4%) cases. Concomitant biceps tenotomy or tenodesis was performed in 65 (22.7%) and 63 (21.9%) cases, respectively. LHBT tenodesis was performed using a mini-open approach with bone tunnels with suture fixation until June 2016 when the primary surgeon transitioned to performing arthroscopic fixation with the use of suture from the rotator cuff anchors.
Standardized cost analysis
Cost analysis in this investigation was designed similarly to the previously published article from this institution.15 Generally, this consisted of a period of 60 days preoperatively, the index surgical hospitalization, and 90 days postoperatively. As standardized costs reported in this study only included services provided by our health system, modeling was performed for the 60 days before and 90 days after surgery accurately representing the clinical practice of the 2 senior surgeons (J.S.S, J.W.S) participating in the study. This helped account for the possibility of missing services owing to the nature of our practice as a high-volume tertiary referral center and portion of our patients who travel more than 6 hours for evaluations.
The 60-day preoperative period included a consultation, referral for medical clearance, standard shoulder radiographs, and magnetic resonance imaging of the shoulder all within 2 months preceding surgery. With respect to the index surgical hospitalization, services from admission through discharge were included in the analysis and categorized by uniform billing revenue codes: Current Procedural Terminology fourth edition, procedure codes, and internal charge master codes. The 90-day postoperative period consisted of 1 follow-up evaluation in the clinic and physical therapy services. Physical therapy consisted of 1 consultation followed by 12 additional therapy sessions. Progression to a home therapy is encouraged at our institution and thus limits the need for further therapy sessions.
All standardized costs were obtained from our institutional cost data warehouse, which uses a widely accepted health service research methodology. Medicare reimbursement was assigned to all professionally build services. Appropriate Medicare cost report cost-to-charge ratios were multiplied by the charges for all hospital billed services, and all resulting costs were adjusted to 2017 dollars with the gross domestic product implicit price deflator.31
Ninety-day outcomes (complications, reoperations, readmissions)
All patient concerns and complications were directly addressed with the surgical team and documented within the electronic medical record. In addition, subsequent emergency department and in-patient service encounters were captured in our electronic medical record and subjected to a detailed review. From this, an individual review was performed to identify any related complications, reoperations, or readmissions from the index surgical hospitalization.
Statistical analysis
Descriptive statistics were performed for various patient demographic and clinical characteristics. Cost analysis also included descriptive statistics: mean, median, and standard deviation. However, given that healthcare cost data are generally skewed, the median cost was emphasized. A generalized linear modeling regression with gamma distribution for cost and logarithmic link was performed and then used to assess the average marginal affective different protectors on the average index cost. All statistical tests were 2 sided, and a P value less than .05 was considered statistically significant.
Results
Cohort demographics
The final cohort consisted of 615 patients who were identified as undergoing RCRs at our institution between January 2012 and December 2017. A total of 95 were with oRCR, 233 cRCR, and 287 aRCR. The mean age was 60.8 ± 9.1 years, with the oldest patients receiving aRCR at 62 ± 9.1 (P = .0007) years. There was an overall male predominance (60.5%) to all RCR recipients. In addition, a majority of our patients had a body mass index > 30 (54.2%) with a group average of 31.2 ± 7. The median American Society of Anesthesiologists score was 2.2 with 66.3% of patients at an American Society of Anesthesiologists score of 2. Operative time was significantly different across all 3 groups with oRCR at 52.01 ± 21.8 minutes, cRCR 61.3 ± 14.9 minutes, and aRCR at 74.0 ± 25.3 (P < .001). In all 3 groups, the biceps was most commonly intact at the time of surgery with no concomitant procedure performed (oRCR = 55.8%, cRCR = 58.3%, aRCR = 55.4%, P = .21). Discharge disposition with respect to mean and median of the 3 groups was 1.2 and 1 day in the oRCR, 1.2 and 1 day in the cRCR, and 0.5 and 0 days in the aRCR, respectively (P < .001).
Cost
In this cohort, the modeled standardized cost for our 60-day preoperative evaluation was $496.69 (Table II). The median standardized cost for the index surgical hospitalization by procedure was as follows: oRCR $9,343.10, cRCR $10,057.20, and aRCR $10,330.60 (Table III). The modeled standardized cost for our 90-day postoperative care was $875.02 (Table IV). In the oRCR group, the highest standardized cost for the index hospitalization was related to the cost of the operating room (40.4%), followed by the hospital room (19%), implant (9.1%), and recovery (7.8%) costs. In the cRCR group, the highest standardized cost for the index hospitalization was related to the cost of the operating room (36.4%), followed by the implant (21.2%), hospital room (12.1%), and supplies (10.9%) costs. In the aRCR group, the highest standardized cost for the index hospitalization was related to the cost of the operating room (31.6%), followed by the implant (28.7%), supplies (12.3%), and hospital room (6.5%) costs (Table V).
Table II.
Modeled preoperative costs of RCRs.
| CPT4 code | Service description | Cost, US $ |
|---|---|---|
| 99214 | Office or other outpatient visit for the evaluation and management of an established patient, which requires at least 2 of these 3 key components: A detailed history; A detailed examination; Medical decision making of moderate complexity. Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient's and/or family's needs. Usually, the presenting problem(s) are of moderate to high severity. Typically, 25 minutes are spent face-to-face with the patient and/or family. (This is the most frequent E and M code) | 108.74 |
| 73030 | Radiologic examination, shoulder; complete, minimum of 2 views | 29.43 |
| 73221 | Magnetic resonance (eg, proton) imaging, any joint of upper extremity | 240.45 |
| 36415 | Collection of venous blood by venipuncture | 2.87 |
| 86900 | Blood group typing (ABO) | 75.04 |
| 86850 | Antibody screen, RBC, each serum technique | 5.25 |
| 82565 | Blood creatinine level | 7.03 |
| 85025 | Blood count; complete (CBC), automated (Hgb, Hct, RBC, WBC and platelet count) and automated differential WBC count | 10.66 |
| 93000 | Electrocardiogram, routine ECG with at least 12 leads; with interpretation and report. | 17.22 |
| 496.69 |
RCR, rotator cuff repair.
Table III.
Index surgical costs of rotator cuff repairs by procedure type.
| Procedure | Standardized cost, US $ |
||||||
|---|---|---|---|---|---|---|---|
| Minimum | Lower quartile | Median | Upper quartile | Maximum | Mean | SD | |
| Open RCR n = 95 | 6,613 | 8,624 | 9,343 | 10,268 | 18,140 | 9,748 | 1,749 |
| Combined n = 233 | 7,002 | 9,150 | 10,057 | 11,410 | 36,873 | 10,625 | 2,757 |
| Arthroscopic RCR n = 287 | 6,891 | 9,012 | 10,331 | 10,268 | 18,428 | 10,396 | 1,839 |
RCR, rotator cuff repair.
Table IV.
Modeled postoperative costs of RCRs.
| CPT4 code | Service description | Cost, US $ |
|---|---|---|
| 99499 | Evaluation and management service | 0.00 |
| 97001 | Physical therapy consultation evaluation | 82.54 |
| Physical therapy return visits (12 sessions) | 792.48 | |
| 875.02 |
RCR, rotator cuff repair.
Table V.
Index surgical hospitalization costs by service.
| Service | Mean % of index cost |
||
|---|---|---|---|
| Open RCR n = 95 | Combined n = 233 | Arthroscopic RCR n = 287 | |
| Implant | 9.1% | 21.2% | 28.7% |
| Operating room | 40.4% | 36.4% | 31.6% |
| Hospital room | 19.0% | 12.1% | 6.5% |
| Supplies | 6.4% | 10.9% | 12.3% |
| Pharmacy | 6.6% | 5.1% | 4.7% |
| Recovery | 7.8% | 5.1% | 6.2% |
| Anesthesia | 5.9% | 6.2% | 6.2% |
| Other | 4.7% | 3.1% | 3.8% |
RCR, rotator cuff repair.
Ninety-day outcomes (complications, reoperations, readmissions)
In the 90-day postoperative period, there were a total of 3 complications, 3 reoperations, and 8 readmissions in 8 patients. Across each group, there were no differences in the 90-day complication (P = .26), reoperation (P = .26), and readmission rates (P = .73) and were 1.1%, 1.1%, and 2.1% in the oRCR; 0.8%, 0.8%, and 1.3% cRCR; 0%, 0%, and 1% in the aRCR, respectively. Shoulder-related causes of readmission which also led to reoperations included a wound dehiscence (n=1) in the oRCR and superficial wound infection (n = 1) and deltoid avulsion (n = 1) in the cRCR. Medical complications such as pulmonary embolus (n = 3), deep vein thrombosis (n = 2; upper extremity = 1 and lower extremity = 1), ischemic colitis, narcotic overdose, and metabolic imbalance accounted for the 8 other readmissions.
Discussion
RCRs remain a relevant orthopedic challenge with an economic burden eclipsing more than $1.0 billion in annual US healthcare expenditures.5,7,19 With an associated rapid rise in RCRs,7,25 cost containment and value-based reimbursement models will continue to be a major focus for healthcare systems, payers, and surgeons. In addition, patient perception of the value of RCRs continues to be much higher than actual surgeon reimbursement.21,29 In this investigation, the median standardized costs for RCRs inclusive of 60-day workup and 90-day postoperative care were $10,704.15, $11,418.25, and $11,691.65 for oRCR, cRCR (average added cost $714.1), and aRCR (added cost $987.5), respectively. Moreover, there were no significant differences between the 90-day complication, reoperation, and readmission rate with a low overall group rate of 0.5%, 0.5%, and 1.3%, respectively.
Although current literature reflects an interest in health economics within orthopedics, few studies have investigated the costs incurred by patients undergoing all 3 repair techniques. In 2010, Churchill et al6 used an ambulatory surgery database from New York to analyze mRCR and aRCR across various-volume surgical centers. They found that the mRCR technique was significantly less expensive and required less operative time. Furthermore, regardless of the repair technique, high-volume centers were the most cost efficient. Hui et al12 performed a similar study of a tertiary hospital in Singapore comparing hospitalization costs of standard mini-open repair and arthroscopic repair, demonstrating significantly less cost with mini-open repairs with most of the differences arising from the cost of implants and consumables.
The findings in this study reinforce those from previous investigations that mRCRs cost significantly less and required less time than arthroscopic repairs6,12 with our investigation including cost reduction when compared with cRCR and aRCR as well. In the mini-open group, operating room (40.4%) and hospital room services (19%) accounted for more than half of the index hospitalization cost, with the implant cost accounting only for 9.1%. The lower implant cost with oRCR was as expected owing to the use of nonabsorbable sutures passed through the greater tuberosity as opposed to suture anchors.
In contrast, both the cRCR and aRCR had the operating room (cRCR = 36.4%, aRCR = 31.6%) and implant (cRCR = 21.2%, aRCR = 28.7%) as the major elements accounting for cost. Notably, the implant cost was variable across the 3 groups with aRCR (28.7%) representing the highest proportion of index costs compared with cRCR (21.2%) and oRCR (9.1%). In addition, implant cost had a higher proportion of index hospitalization costs than all the supplies across all 3 groups (oRCR 9.1% vs. 6.4%, cRCR 21.2% vs. 10.9%, aRCR 28.7% vs 12.3%). Implants and consumables have been previously described as key items leading to majority of cost differences between mini-open and arthroscopic techniques.12 We observed relatively stable supply costs, but did note varying implant costs across the 3 groups with higher proportions in arthroscopic techniques. This is further supported with the increasing use of mean number of suture anchors with arthroscopic techniques (oRCR = 0 vs. cRCR = 2.1 ± 1.2 vs. aRCR = 3.5 ± 1.4; P < .001). As value-based initiatives continue to progress, implant cost may serve as an actionable area for cost reduction.
RCRs and the different techniques have been described as low-morbidity procedures. Complication rates have been described in the literature with variability between 0.7% and 14%.10,13,18,26,28 In our investigation, our group complication rate of 0.5% was on par with the low end of described short-term complications. Traditionally, oRCRs have demonstrated an increased risk for longer hospital stay, surgical site infection, and return to operating room compared with arthroscopic techniques.2,8,28 Likewise, we observed that techniques with an open component did sustain complications similar to those described in the literature (superficial wound, wound dehiscence, and deltoid avulsion) and did lead to reoperation. However, we observed no differences among the various repair techniques overall (1.1% in oRCR, 0.8% cRCR, and 0% in the aRCR; P = .26). This is supported by more recent data by Liu et al,18 a randomized clinical trial demonstrating similar complication rates between mRCR and aRCR. Of note, the authors did also report that aRCR was associated with less pain, lower DASH scores, and higher CMS scores in the early recovery period suggestive of better earlier recovery with arthroscopic techniques.18
Currently, RCRs have transitioned to becoming largely outpatient procedures. Our institution manages oRCR and cRCR as planned 1 night in hospital stays and aRCR as outpatient procedures. This was observed in this investigation with both oRCR and cRCR with mean length of stay around 1.2 days (median = 1) and aRCR with a mean of 0.5 days (median = 0). With respect to cost, this translated to hospital room services holding the highest proportion in the oRCR (19%) group followed by cRCR (12.1%), with the lowest proportion in the aRCR group (6.5%). It is important to note that even with this discharge disposition with oRCR and cRCR having longer length of stays, both were still cheaper than aRCR. Unplanned readmissions in this study within the first 90 days were 1.3% and were largely medically related. This is comparable with the readmission rates in the literature range of 0.8-1.55%.16,24,28
The present study had several limitations including those specific to a retrospective, single-center referral center. Our study is representative of the clinical practice of the senior authors who perform 100 to 150 rotator cuff repairs annually with standardized perioperative protocols and close to 40 years of combined shoulder experience. As such the cost results of this investigation are largely specific to this practice type and would not be as applicable to general practices initially. As such, we attempted to make these results more generalizable by modeling the 60-day preoperative and 90-day postoperative costs to properly capture those costs which would have been missed by our patients receiving outside evaluations by their referring provider. However, there are still specific elements unique to the present study (single follow-up visit in the 90-day global period) that would need to be considered when comparing various practice setting. Next, the standardized cost methodology used is helpful for understanding our institutional cost components. However, it is an imperfect tool which is not easily translated to particular payer’s (government or private) or provider’s costs or able to capture services incurred at other facilities. In addition, the standardized costs reported in this study are not directly applicable to bundled payment formulation by Accountable Care Organizations.
Conclusions
With the current focus on value-based care and standardized preoperative and postoperative protocols, the median standardized costs for RCRs inclusive of 60-day workup and 90-day postoperative care were $10,704.15, $11,418.25, and $11,691.65 for oRCR, cRCR (average added cost $714.1), and aRCR (added cost $987.5), respectively. The group complication, reoperation, and readmission rate were 0.5%, 0.5%, and 1.8% with no significant differences between the varying techniques, respectively. This retrospective cost analysis and complication profile may serve as a useful reference for surgeons and healthcare systems in providing high-quality patient care and attempting to decrease the economic burden of rotator cuff repairs. As bundled payment initiatives continue to increase significantly, this study further highlights that implant cost may serve as an actionable area for cost reduction. Furthermore, this may be used as a care based economic model in the creation of bundled payment packages.
Conflicts of interest
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Funding
No funding was disclosed by the author(s).
Footnotes
Mayo Institutional Review Board approved this study (IRB # 19-005380).
References
- 1.Arshi A., Kabir N., Cohen J.R., Lord E.L., Wang J.C., McAllister D.R., et al. Utilization and Costs of Postoperative Physical Therapy After Rotator Cuff Repair: A Comparison of Privately Insured and Medicare Patients. Arthroscopy. 2015;31:2392–2399.e2391. doi: 10.1016/j.arthro.2015.06.018. [DOI] [PubMed] [Google Scholar]
- 2.Baker D.K., Perez J.L., Watson S.L., McGwin G., Brabston D.W., Hudson P.W., et al. Arthroscopic Versus Open Rotator Cuff Repair: Which Has a Better Complication and 30-Day Readmission Profile? Arthroscopy. 2017;33:1764–1769. doi: 10.1016/j.arthro.2017.04.019. [DOI] [PubMed] [Google Scholar]
- 3.Barnett M.L., Wilcock A., McWilliams J.M., Epstein A.M., Joynt Maddox K.E., et al. Two-Year Evaluation of Mandatory Bundled Payments for Joint Replacement. N Engl J Med. 2019;380:252–262. doi: 10.1056/NEJMsa1809010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Branning G., Vater M. Healthcare Spending: Plenty of Blame to Go Around. Am Health Drug Benefits. 2016;9:445–447. [PMC free article] [PubMed] [Google Scholar]
- 5.Chalmers P.N., Granger E., Nelson R., Yoo M., Tashjian R.Z. Factors Affecting Cost, Outcomes, and Tendon Healing After Arthroscopic Rotator Cuff Repair. Arthroscopy. 2018;34:1393–1400. doi: 10.1016/j.arthro.2017.11.015. [DOI] [PubMed] [Google Scholar]
- 6.Churchill R.S., Ghorai J.K. Total cost and operating room time comparison of rotator cuff repair techniques at low, intermediate, and high volume centers: mini-open versus all-arthroscopic. J Shoulder Elbow Surg. 2010;19:716–721. doi: 10.1016/j.jse.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 7.Colvin A.C., Egorova N., Harrison A.K., Moskowitz A., Flatow E.L. National trends in rotator cuff repair. J Bone Joint Surg. 2012;94A:227–233. doi: 10.2106/JBJS.J.00739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Day M., Westermann R., Duchman K., Gao Y., Pugely A., Bollier M., et al. Comparison of Short-term Complications After Rotator Cuff Repair: Open Versus Arthroscopic. Arthroscopy. 2018;34:1130–1136. doi: 10.1016/j.arthro.2017.10.027. [DOI] [PubMed] [Google Scholar]
- 9.Grobet C., Audigé L., Eichler K., Meier F., Brunner B., Wieser S., et al. Cost-Utility Analysis of Arthroscopic Rotator Cuff Repair: A Prospective Health Economic Study Using Real-World Data. Arthroscopy Sports Med Rehabil. 2020;2:e193–e205. doi: 10.1016/j.asmr.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heyer J.H., Kuang X., Amdur R.L., Pandarinath R. Identifiable risk factors for thirty-day complications following arthroscopic rotator cuff repair. Phys Sportsmed. 2018;46:56–60. doi: 10.1080/00913847.2018.1388732. [DOI] [PubMed] [Google Scholar]
- 11.Huang R., Wang S., Wang Y., Qin X., Sun Y. Systematic Review of All-Arthroscopic Versus Mini-Open Repair of Rotator Cuff Tears: A Meta-Analysis. Sci Rep. 2016;6:22857. doi: 10.1038/srep22857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hui Y.J., Teo A.Q., Sharma S., Tan B.H., Kumar V.P. Immediate costs of mini-open versus arthroscopic rotator cuff repair in an Asian population. J Orthopaedic Surg. 2017;25 doi: 10.1177/2309499016684496. 2309499016684496. [DOI] [PubMed] [Google Scholar]
- 13.Jensen A.R., Cha P.S., Devana S.K., Ishmael C., Di Pauli von Treuheim T., D'Oro A., et al. Evaluation of the Trends, Concomitant Procedures, and Complications With Open and Arthroscopic Rotator Cuff Repairs in the Medicare Population. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117731310. 2325967117731310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ji X., Bi C., Wang F., Wang Q. Arthroscopic versus mini-open rotator cuff repair: an up-to-date meta-analysis of randomized controlled trials. Arthroscopy. 2015;31:118–124. doi: 10.1016/j.arthro.2014.08.017. [DOI] [PubMed] [Google Scholar]
- 15.Kennon J.C., Songy C.E., Marigi E., Visscher S.L., Larson D.R., Borah B.J., et al. Cost analysis and complication profile of primary shoulder arthroplasty at a high-volume institution. J Shoulder Elbow Surg. 2020;29:1337–1345. doi: 10.1016/j.jse.2019.12.008. [DOI] [PubMed] [Google Scholar]
- 16.Kosinski L.R., Gil J.A., Durand W.M., DeFroda S.F., Owens B.D., Daniels A.H. 30-Day readmission following outpatient rotator cuff repair: an analysis of 18,061 cases. Phys Sportsmed. 2018;46:466–470. doi: 10.1080/00913847.2018.1502571. [DOI] [PubMed] [Google Scholar]
- 17.Li L., Bokshan S.L., Mehta S.R., Owens B.D. Disparities in Cost and Access by Caseload for Arthroscopic Rotator Cuff Repair: An Analysis of 18,616 Cases. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119850503. 2325967119850503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu J., Fan L., Zhu Y., Yu H., Su T., Li G. Comparison of clinical outcomes in all-arthroscopic versus mini-open repair of rotator cuff tears: A randomized clinical trial. Medicine. 2017;96:e6322. doi: 10.1097/MD.0000000000006322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mather R.C., 3rd, Koenig L., Acevedo D., Dall T.M., Gallo P., Romeo A., et al. The societal and economic value of rotator cuff repair. J Bone Joint Surg. 2013;95A:1993–2000. doi: 10.2106/JBJS.L.01495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murphy J., Gray A., Cooper C., Cooper D., Ramsay C., Carr A. Costs, quality of life and cost-effectiveness of arthroscopic and open repair for rotator cuff tears: an economic evaluation alongside the UKUFF trial. Bone Joint J. 2016;98-b:1648–1655. doi: 10.1302/0301-620X.98B12.BJJ-2016-0121.R1. [DOI] [PubMed] [Google Scholar]
- 21.Nagda S., Wiesel B., Abboud J., Salamone A., Sheth N., Foran J., et al. Patient perception of physician reimbursement in elective shoulder surgery. J Shoulder Elbow Surg. 2015;24:106–110. doi: 10.1016/j.jse.2014.06.034. [DOI] [PubMed] [Google Scholar]
- 22.Narvy S.J., Didinger T.C., Lehoang D., Vangsness D.T., Jr., Tibone J.E., Hatch G.F.R., 3rd, et al. Direct Cost Analysis of Outpatient Arthroscopic Rotator Cuff Repair in Medicare and Non-Medicare Populations. Orthop J Sports Med. 2016;4 doi: 10.1177/2325967116668829. 2325967116668829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nazari G., MacDermid J.C., Bryant D., Dewan N., Athwal G.S. Effects of arthroscopic vs. mini-open rotator cuff repair on function, pain & range of motion. A systematic review and meta-analysis. PloS One. 2019;14:e0222953. doi: 10.1371/journal.pone.0222953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Padaki A.S., Boddapati V., Mathew J., Ahmad C.S., Jobin C.M., Levine W.N. The effect of age on short-term postoperative complications following arthroscopic rotator cuff repair. JSES Open Access. 2019;3:194–198. doi: 10.1016/j.jses.2019.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paloneva J., Lepola V., Äärimaa V., Joukainen A., Ylinen J., Mattila V.M. Increasing incidence of rotator cuff repairs--A nationwide registry study in Finland. BMC Musculoskel Disorders. 2015;16:189. doi: 10.1186/s12891-015-0639-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Randelli P., Spennacchio P., Ragone V., Arrigoni P., Casella A., Cabitza P. Complications associated with arthroscopic rotator cuff repair: a literature review. Musculoskelet Surg. 2012;96:9–16. doi: 10.1007/s12306-011-0175-y. [DOI] [PubMed] [Google Scholar]
- 27.Ryan A.M. Medicare Bundled Payment Programs for Joint Replacement: Anatomy of a Successful Payment Reform. J Am Med Assoc. 2018;320:877–879. doi: 10.1001/jama.2018.11787. [DOI] [PubMed] [Google Scholar]
- 28.Schairer W.W., Nwachukwu B.U., Fu M.C., Warren R.F. Risk Factors for Short-term Complications After Rotator Cuff Repair in the United States. Arthroscopy. 2018;34:1158–1163. doi: 10.1016/j.arthro.2017.10.040. [DOI] [PubMed] [Google Scholar]
- 29.Southam B.R., Crawford Z., Grawe B.M. Patient Perceptions of Surgeon Reimbursement for Rotator Cuff Repair. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118795712. 2325967118795712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tashjian R.Z. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31:589–604. doi: 10.1016/j.csm.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 31.Visscher S.L., Naessens J.M., Yawn B.P., Reinalda M.S., Anderson S.S., Borah B.J. Developing a standardized healthcare cost data warehouse. BMC Health Serv Res. 2017;17:396. doi: 10.1186/s12913-017-2327-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


