Abstract
Background
Acromioclavicular (AC) joint separation is a common cause of shoulder injury among athletes. High-grade injuries may require operative fixation, and comprehensive return-to-play guidelines have not yet been established. The purpose of this study was to summarize criteria for return to play after operative management of AC joint separation.
Methods
A systematic review of the literature was performed from January 1999 to April 2020 to evaluate clinical evidence regarding criteria for return to play after operative management of isolated AC joint separation.
Results
Sixty-three studies with at least 1 explicitly stated return-to-play criterion were identified out of an initial database search of 1253 published articles. Eight separate categories of return-to-play criteria were identified, the most common of which was time from surgery (95.2%). Return-to-play timelines ranged from 2 to 12 months, the most common timeline being 6 months (37.8%). Only 4 (6.3%) studies used conditional criteria to guide return to play, which included range of motion, strength, clinical stability, radiographic stability, functional assessment, safety assessment, and hardware removal.
Conclusion
Most published studies use only time-based criteria for return to play after surgery for AC joint separation, and only a small number of studies use additional subjective or objective criteria. While this systematic review helps provide a foundation for developing a comprehensive return-to-play checklist, further investigation is needed to establish safe and effective guidelines that will enable athletes to safely return to sport and minimize the recurrence of injury.
Keywords: Acromioclavicular joint, AC joint, AC joint separation, AC joint repair, Return to play criteria, Shoulder
Acromioclavicular (AC) joint separations are among the most common shoulder injuries encountered in clinical practice and account for nearly half of all shoulder injuries sustained by contact sport athletes.78 The Rockwood classification is the most commonly used system to aid with diagnosis and guide treatment of AC joint separations.57 Lower grade injuries (Rockwood Types I and II) are typically managed nonoperatively, while surgeons have generally favored operative treatment for higher grade injuries (Rockwood Types IV – VI), although recent evidence suggests that nonoperative management may not be inferior to operative treatment for certain high-grade injuries.11,15,30 Treatment of Rockwood Type III injuries remains controversial, although a trial of nonoperative management is favored in most cases.63,67
Various operative and nonoperative treatment regimens have been described to manage separation of the AC joint with the goal of improving shoulder function in both athletes and nonathletes.3,15 For athletes, the ability to return to athletic competition is an important goal. Two recent systematic reviews reported high rates of return to play (>90%) after various techniques of surgical treatment of AC joint injuries.28,71 However, despite the high incidence of AC joint injuries and the numerous methods of treatment used, there is no consensus among surgeons regarding when athletes may safely return to competition, particularly among contact and overhead athletes.
The purpose of this study is to systematically review existing literature to identify and describe criteria used to guide return to play after operative management of AC joint separations. We hypothesize that most surgeons use time-based criteria rather than functional criteria to guide return to play.
Methods
Search strategy
We performed a systematic review of Level I to IV studies that provided criteria for return to play after operative management of AC joint separation using the PubMed, EMBASE, and Cochrane databases from January 1999 to April 2020. January 1999 was selected as 20 years before the inception of this investigation to include modern operative techniques of managing AC joint separations. The database search included various combinations of the following search terms: acromioclavicular, AC joint, dislocation, separation, disruption, surgery, surgical, reconstruction, repair, stabilization, and outcome.
Inclusion/exclusion criteria
To be included, studies were required to (1) be written in the English language, (2) be conducted on a population of patients with a mean age of 18 years or higher, (3) include patients who underwent operative treatment for acute or chronic AC joint separations, and (4) include patients with a minimum of 12 months of follow-up. Studies lacking explicit return-to-play criteria, review articles, case reports, biochemanical or cadaveric studies, and technical notes that reported cohorts of less than 5 patients were excluded. Studies in which greater than 10% of patients had concomitant injuries to the ipsilateral extremity or in which greater than 10% of patients underwent secondary management after failure of previous surgical treatment for AC joint separation were also excluded. Studies evaluating patients with chronic AC joint separation not previously treated surgically and patients who failed previous nonoperative treatment were included.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed throughout this review.42 The initial screening of titles, abstracts, and manuscripts was completed by a team including a resident-physician, medical student, and orthopedic sports-medicine fellow (T.D., R.J.G., P.T.O.). Any disagreements were resolved by consensus between reviewers, and other questions regarding further inclusion or exclusion were directed toward the senior authors (M.G.C. and S.B.C.). The references of all studies satisfying inclusion criteria were manually reviewed to screen for any records not obtained during the database search.
Return-to-play criteria
We used the definition return to play as a general term referring to a return to full, unrestricted sporting activity after operative management of AC joint separations. Given the abundance of terms used to describe these criteria in the literature, we treated the following terms as equivalent unless the authors specified any additional surgeon-imposed restrictions on their patients: return to play, return to sport, return to athletics. In addition, given the desire to focus on athletes, any study that did not explicitly mention play, sport, or athletics (ie, instead mentioning only return to heavy lifting, work, unrestricted activity) was excluded from this analysis.
Patient demographics, outcomes, and surgical techniques
From each study satisfying the inclusion criteria, the primary data evaluated were criteria relating to return to sporting activity. Further abstraction included data regarding authors, year of publication, study level of evidence, classification of injuries (Rockwood, Tossy, and so on), average age of patient cohorts, sex distribution, level of athletics, types of sport played, rates of return to sport, changes in frequency, intensity, or level of athletic activity, and rehabilitation protocols. Because of the variability of study designs and the heterogeneity in the reporting of results, a comprehensive meta-analysis was not performed. Surgical techniques appearing in the studies were recorded, making note of the use of arthroscopy, the method of stabilization of the coracoclavicular and AC joints, and the use of grafts, sutures, and other materials.
Quality assessment of literature methodology
A modified version of the Coleman Methodology Score (CMS) was used to assess the methodological quality of included publications.13 The CMS evaluates 10 separate criteria to yield a final score ranging from 0 to 100, with 100 being the highest methodological quality. Scores ranging from 85 to 100 are considered excellent, from 70 to 84 are good, from 55 to 69 are fair, and less than 55 are considered poor. When assessing diagnostic certainty of injury classifications, we considered any article that mentioned specific Rockwood classifications of subjects as having sufficient diagnostic certainty, regardless of whether the authors explicitly mentioned the use of radiographs or a focused physical examination for diagnosis. However, any study in which the authors explicitly stated that diagnoses were made without radiographs or a focused physical examination was considered to have insufficient diagnostic certainty, as per CMS criteria.
Results
Study design
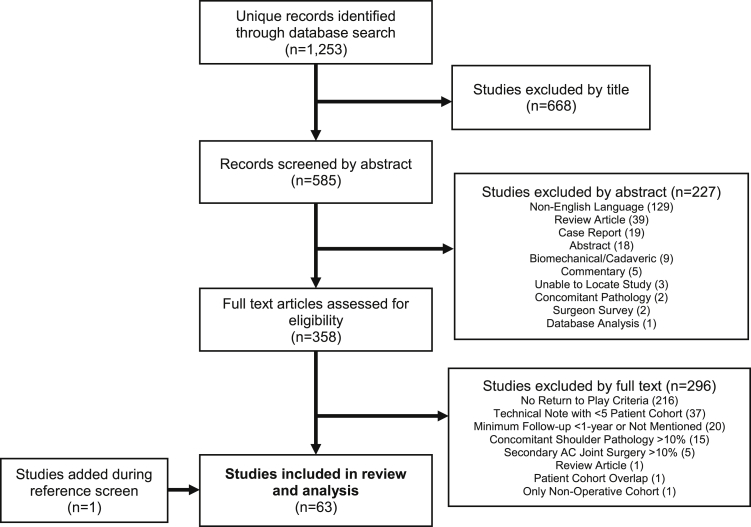
The initial database search yielded 1253 unique published articles. Ultimately, 63 studies that satisfied all inclusion criteria were identified and included in the analysis. Detailed results of the literature review are described in the PRISMA diagram (Fig. 1). Regarding level of evidence for included studies, 2 studies were Level I, 3 studies were Level II, 4 studies were Level III, and 54 studies were Level IV.81
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) diagram of search strategy.
Quality assessment
The average CMS was 64.8 ± 9.5, which indicates fair methodological quality (Supplemental Table S1). CMS scores ranged from 29 to 85.38,50,66 Principle methodological strengths among this cohort of studies include a description of postoperative rehabilitation, in which every study described a rehabilitation protocol to some extent, and a description of surgical technique, which received a score of 9.5 ± 1.5 (out of 10). Notable methodological limitations include type of study and overall study size, with these metrics receiving scores of 2.2 ± 4.7 and 2.4 ± 2.6 out of 15 and 10, respectively. Most studies were retrospective cohort studies or case reports (80.1%) with small cohorts. Only 8 studies (12.7%) included cohorts of greater than 50 patients, while 31 studies (49.2%) included cohorts of less than 30 patients.
Patient and study demographics
The 63 studies included 1939 patients. The mean age of subjects in individual studies ranged from 25.0 to 50.1 years, with an overall weighted mean age of 36.5 years. Of the 61 studies that reported sex distribution, 85.1% of patients were male. Patient follow-up ranged from 12 months to 106.3 months, with a weighted average follow-up duration of 33.9 months for the 58 studies that reported the mean follow-up time. Individual study data and demographic information for patients of included studies are detailed in Table I.
Table I.
Individual study data including injury classification, demographic data, and return-to-play criteria.
| First author, yr | Injury classification∗ (no.) | Primary stabilization method(s) | Level of evidence | No. of patients | Mean age in years | Mean follow-up in months (minimum) | No. of RTP criteria† | RTP criteria† |
|---|---|---|---|---|---|---|---|---|
| Abat, 20181 | 3/3/14 | Arth CC suture button | IV | 20 | 36.1 | 25.4 (18.5) | 1 | Time |
| Barth, 20152 | 10/6/8 | Arth CC suture button, Weaver-Dunn, combined Weaver-Dunn and CC reconstruction with soft-tissue graft, combined suture button and CC reconstruction with soft-tissue graft, CC reconstruction with LARS artificial ligament | IV | 24 | 41 | 12 (12) | 1 | Time |
| Beris, 20134 | 8/4/0 | Open CC suture button | IV | 12 | 27.5 | 18.25 (12) | 1 | Time |
| Boutsiadis, 20165 | 0/1/4 | Arth combined Waver-Dunn with suture button and AC and CC reconstruction with palmaris autograft | IV | 5 | 37 | 18 (18) | 1 | Time |
| Breuer, 20196 | 8/11/32 | Open CC suture button and AC suture reconstruction | IV | 51 | 43‡ | 55 (29)‡ | 1 | Time |
| Cano-Martinez, 20167 | 0/0/33 | Open CC suture button | IV | 33 | 25 | 25 (14) | 1 | Time |
| Cardone, 20028 | 6/0/0 | Open CC suture fixation | IV | 6 | 26.7 | 44.8 (31) | 1 | Time |
| Carkci, 20209 | 14/0/22 | Arth CC suture button | IV | 36 | 30.6 | 31.4 (24) | 1 | Time |
| Carrera, 201310 | 7/3/11 | Open CC suture anchor repair and clavicular pinning | IV | 21 | 35 | 18 (13) | 1 | Time |
| Cho, 201612 | 4/12/20 | Open CC suture button with AC K-wire stabilization or clavicular pinning | IV | 36 | 40.8 | 56.7 (24) | 1 | Time |
| Dal Molin, 201716 | 0/3/17 | Open CC screw with CC suture fixation | IV | 20 | 34.8 | 45 (24) | 1 | Time |
| De Carli, 201517 | 30/0/0 | Open CC suture button | IV | 30 | 29.2 | 42 (24) | 1 | Time |
| Dimakopoulos, 200618 | 24/0/10 | Open CC suture fixation | IV | 34 | 33.5 | 33.2 (18) | 1 | Time |
| El Shewy, 201119 | RW IV-V† | Open CC suture fixation | IV | 21 | 31.8 | 92.4 (72) | 1 | Clinical AC joint stability; radiographic AC joint stability |
| Gangary, 201620 | 6/2/3 | Arth CC suture button | IV | 11 | 34.2 | 12 (12) | 1 | Time |
| Garofalo, 201721 | 0/0/32 | Open semitendinosus autograft reconstruction of CC and AC | IV | 32 | 28 | 30 (24) | 1 | Time |
| Gomez-Vieira, 200923 | 2/5/3 | Arth CC suture button | IV | 10 | 34 | 15 (12) | 1 | Time |
| Greiner, 200924 | 5/1/44 | Open CC suture fixation | IV | 50 | 35.3 | 70 (30) | 1 | Time |
| Hashiguchi, 201825 | 8/0/4 | Arth CC reconstruction with Leeds-Keio artificial ligament and AC K-wire stabilization | IV | 12 | 40.8 | 106.3 (62) | 3 | Time; ROM; strength |
| Hou, 201426 | 1/1/18 1 RW VI |
Open semitendinosus allograft reconstruction of CC, combined semitendinosus allograft with suture button | IV | 21 | 39.4 | 15.5 (12) | 1 | Time |
| Katsenis, 201527 | 0/29/21 | Open CC suture button | IV | 50 | 35.5 | 42 (36) | 1 | Time |
| Kocaoglu, 201729 | 25/4/2 1 RW VI |
Open CC suture button with modified Weaver-Dunn; CC reconstruction with palmaris longus autograft and suture button | III | 32 | 39.7 | 44.9 (29) | 1 | Time |
| Kurtoglu, 202031 | 12/0/13 | Open CC suture button | IV | 25 | 30.7 | 18.6 (12) | 1 | Time |
| Läuderman, 201132 | 6/12/19 | Open CC suture fixation with AC joint suture reconstruction | IV | 37 | 33.6 | 54 (24) | 1 | Time |
| Lee, 201934 | 12/0/15 | Arth CC all suture anchor repair | IV | 27 | 35.2 | N/M (24) | 1 | Time |
| Leidel, 200935 | 70/0/0 | Open AC K-wire stabilization | IV | 70 | 37 | 48 (24) | 1 | Time |
| Li, 201336 | 0/7/3 | Arth CC suture button with AC suture anchor fixation | IV | 10 | 46.4 | 33.6 (24) | 1 | Time |
| Liu, 201537 | 7/0/5 | Arth CC suture button | IV | 12 | 48 | 24 (18) | 1 | Time |
| Lu, 201638 | 66/11/3 | Open CC suture button | II | 80 | 33.9 | 25.4 (12) | 1 | Time |
| Metzlaff, 201641 | RW III-V† | Open hook plate; CC suture button | III | 44 | 37.6‡ | 32 (24)‡ | 1 | Time |
| Motta, 201243 | 38/11/2 | Open CC reconstruction with LARS artificial ligament | III | 51 | 36 | 60 (24) | 1 | Time |
| Muccioli, 201640 | 23/5/15 | Open CC reconstruction with LARS artificial ligament | II | 43 | 29‡ | 28.2 (24) | 2 | Strength; functional assessment; safety assessment |
| Müeller, 201846 | 12/6/43 | Open hook plate; Arth CC suture button | I | 61 | 36.1 | N/M (24) | 1 | Time |
| Muench, 201945 | 20/0/23 | Open CC and AC reconstruction with semitendinosus or peroneus longus allograft | IV | 43 | 43.4 | 40.8 (24) | 1 | Time |
| Murena, 201347 | 34/0/0 | Open CC screw fixation; Arth CC screw fixation; Arth CC suture button | IV | 34 | 41.8 | 82.7 (50.4) | 1 | Time |
| Murray, 201848 | 18/11/0 | Open CC suture button | I | 29 | 31 | 12 (12) | 1 | Time |
| Natera-Cisneros, 201550 | N/M | Arth CC suture button plus AC suture reconstruction | IV | 9 | N/M | N/M (12) | 1 | Time |
| Natera-Cisneros, 201749 | 5/0/6 | Open hook plate | IV | 11 | 41 | 32.5 (24) | 1 | Time |
| Parnes, 201552 | 0/0/12 | Arth CC and AC reconstruction with semitendinosus autograft or allograft | IV | 12 | 25 | 30.4 (24) | 1 | Time |
| Porschke, 201753 | 0/0/55 | Open CC suture button | IV | 55 | 42 | 24 (18) | 1 | Time |
| Porschke, 201954 | 5/0/49 | Open CC suture button | IV | 54 | 41.5 | 23 (18) | 1 | Time |
| Ranne, 202055 | 29/0/29 | Arth CC reconstruction with semitendinosus autograft | IV | 58 | 36.4 | N/M (24) | 1 | Time |
| Saccomanno, 201458 | 8/4/6 | Open CC and AC reconstruction with semitendinosus autograft | IV | 18 | 27.5 | 26.4 (24) | 1 | Time |
| Saier, 201659 | 0/0/42 | Arth CC suture button | IV | 42 | 34.5 | 31.3 (24) | 1 | Time |
| Sandmann, 201260 | 9/9/15 | Open CC suture fixation and AC suture reconstruction | IV | 33 | 39 | 32 (24) | 1 | Time |
| Seo, 201961 | N/M | Arth CC suture button | III | 32 | 50.1 | 13.7 (12) | 1 | Time |
| Shin, 200962 | 0/0/29 | Open CC suture anchor with CA ligament transfer | IV | 29 | 39.7 | 27.8 (24) | 1 | Time |
| Steinbacher, 201464 | 19/0/0 | Open clavicular hook plate | IV | 19 | 29 | 50.4 (22.8) | 1 | Time |
| Struhl, 201565 | 19/2/14 | Open CC suture button with CC repair or CA ligament transfer | IV | 35 | 42.4 | 62.4 (27) | 1 | Time |
| Sun, 201966 | 46/23/11 | Open CC suture button | II | 80 | 35.4 | 34.5 (12) | 1 | Time |
| Tiefenboeck, 201769 | 13/4/2, 3 RW II | Open CC screw with AC K-wire stabilization | IV | 22 | 41 | 93.6 (24) | 1 | Time |
| Tiefenboeck, 201868 | 30/14/3 | Open CC reconstruction with LARS artificial ligament | IV | 47 | 37 | 89 (25) | 1 | Time |
| Triantafyllopoulos, 201770 | 0/0/10 | Open CC and AC reconstruction with JewelACL artificial ligament | IV | 10 | 33 | 48 (24) | 1 | Time |
| Vitali, 201572 | 29/6/2 | Open CC reconstruction with GORE PROPATEN vascular graft and AC K-wire stabilization | IV | 37 | 34.4 | N/M (24) | 1 | Time |
| Vulliet, 201773 | 21/0/19 | Arth CC suture button | IV | 40 | 38.2 | 26.1 (12) | 1 | Time |
| Wang, 200876 | 0/0/13 | Open CC suture fixation with AC pin stabilization | IV | 13 | 28.3 | 55.2 (23) | 1 | Time |
| Wang, 201477 | 18/0/3 | Open clavicular hook plate with coracoid process transfer to clavicle | IV | 21 | 41.6 | 33 (26) | 1 | Hardware removal |
| Wang, 201574 | 0/0/0, 12 Tossy III | Open clavicular hook plate plus with AC and CC trapezius muscle flap | IV | 12 | 36.1 | 22.83 (16) | 1 | Time |
| Wang, 201875 | 6/2/8 | Open clavicular hook plate; AC and CC reconstruction with flexor profundus tendon allograft | IV | 16 | 45.2 | 30.3 (24) | 1 | Time |
| Wolf, 200480 | RW III-V† | Arth suture fixation with clavicular and coracoid tunnel liner screws | IV | 21 | N/M | 24 (12) | 1 | Time |
| Xue, 201882 | 0/0/25 | Open CC suture button | IV | 25 | 43 | 34 (24) | 1 | Time |
| Ye, 201483 | 14/2/26 | Open CC titanium cables | IV | 42 | 36 | 42 (34) | 1 | Time |
| Yoo, 201184 | 3/0/10 | Arth CC reconstruction with semitendinosus autograft | IV | 13 | 28.4 | 17 (12) | 1 | Time |
RTP, return to play; RW, Rockwood; N/M, not mentioned; Arth, arthroscopic; CC, coracoclavicular; AC, acromioclavicular; ROM, range of motion; LARS, Ligament Augmentation and Reconstruction System; CA, coracoacromial ligament.
Injury classification documented as Rockwood III/IV/V unless otherwise mentioned.
Median number.
Number of each classification not specified.
All but 3 studies explicitly mentioned whether patients were treated for acute or chronic AC joint separations.1,26,80 Forty-seven studies evaluated patients who were treated for only acute injuries, 9 studies evaluated patients with only chronic injuries, and 4 studies included patients with both acute and chronic injuries. Sixty-one studies reported the classifications of AC joint separations. The most common injury classification groupings included cohorts with Rockwood Types III/IV/V injuries (38.1%), Rockwood Types III/V injuries (19.0%), and Rockwood Type V injuries alone (14.3%). Additional combinations of injury classifications are demonstrated in Table II. Two studies did not specify the type of AC joint injury: One study50 treated patients with acute “unstable ACJ injuries,” and another study61 treated patients with “acute AC dislocation.” Two studies mentioned the type of Rockwood injuries included but did not specify the number of subjects in each group.19,80
Table II.
Combinations of AC joint injury classifications included among the cohort of 63 studies.
| Injury classifications | Studies, n (%) |
|---|---|
| RW III/IV/V | 24 (38.1) |
| RW III/IV | 2 (3.2) |
| RW IV/V | 5 (7.9) |
| RW III/V | 12 (19.0) |
| RW II/III/IV/V | 1 (1.6) |
| RW III/IV/V/VI | 2 (3.2) |
| RW III | 5 (7.9) |
| RW V | 9 (14.3) |
| Tossy III | 1 (1.6) |
| N/M | 2 (3.2) |
RW, Rockwood; N/M, not mentioned.
Return-to-play criteria
All 63 studies reported at least 1 explicit criterion for return to play, and 60 studies (95.2%) reported only a single return-to-play criterion (Table III). A total of 8 separate criteria were reported: (1) time from surgery, (2) shoulder range of motion, (3) strength, (4) clinical stability of the AC joint, (5) radiographic stability of AC joint, (6) functional assessment, (7) safety assessment, and (8) hardware removal. Time from surgery was the most frequently cited criterion guiding return to play (95.2%) and was the sole criterion in 59 of the 63 studies (Table III).
Table III.
Combinations of criteria for return to play after operative management of AC joint separation in the cohort of 63 studies.
| Combinations of criteria for return to play | Studies, n (%) |
|---|---|
| Time | 59 (93.7) |
| Time, range of motion, strength | 1 (1.6) |
| Clinical stability, radiographic stability | 1 (1.6) |
| Strength, functional assessment, safety assessment | 1 (1.6) |
| Hardware removal | 1 (1.6) |
The most frequently cited timeframe from surgery to return to sport was 6 months in 23 studies, followed by 3 months in 18 studies (Table IV). Return-to-play timelines ranged from 2 months to 12 months after surgery. In addition to the explicit return-to-play criteria, all 63 studies did describe some form of postoperative rehabilitation, although no studies used completion of a rehabilitation program as a criterion for return to sport. Immobilization and range of motion guidelines were the most commonly reported rehabilitation points of interest (95.2% and 93.7%, respectively), followed by strengthening exercises (44.4%) and arm elevation restrictions (36.5%).
Table IV.
Summary of return-to-play timelines after operative management of AC joint separation among the 60 studies that cited return-to-play timelines.
| Return-to-play timeline | Studies, n (%) |
|---|---|
| 2 mo | 1 (1.7) |
| 3 mo | 18 (30.0) |
| 4 mo | 5 (8.3) |
| 4-5 mo | 2 (3.3) |
| 5 mo | 2 (3.3) |
| 4-6 mo | 5 (8.3) |
| 5-6 mo | 1 (1.7) |
| 6 mo | 23 (38.3) |
| 6-8 mo | 1 (1.7) |
| 10 mo | 1 (1.7) |
| 12 mo | 1 (1.7) |
Sport participation and return to sport outcomes
Twenty-three studies (36.5%) reported the number of athletes included, representing a total of 594 athletes. An additional 281 athletes were inferred from 24 other studies (38.0%) based on a sports-related mechanism of injury, but these studies did not explicitly mention the total number of athletes among their patient cohorts. Sixteen studies (25.4%) did not mention the number of athletes either explicitly or in their mechanism of injury. Twenty-four studies (38.0%) reported the sports in which patients participated before injury. Among the 36 sports represented, the most frequently reported types of athletes were cyclists in 15 studies (23.8%), soccer players in 10 studies (15.9%), basketball players in 6 studies (9.5%), and skiers or snowboarders in 5 (7.9%) studies. The level of sports in which patients participated was explicitly referenced in 9 studies, accounting for 231 patients. Among these were 38 professional athletes (16.5%), 7 semi-professional athletes (3.0%), 21 nonprofessional athletes (9.1%), 20 competitive athletes (8.7%), and 145 recreational athletes (62.8%).
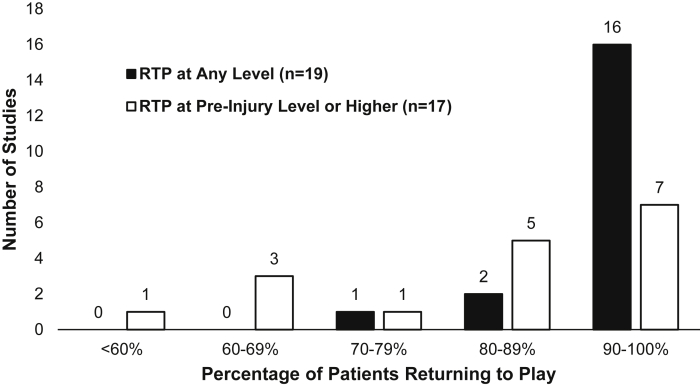
The rate of return to play was reported in 19 studies (Fig. 2). Among these, 94.2% of athletes returned to some level of athletics regardless of whether athletes regained their preinjury level of performance (range 72.4% to 100%). Seventeen studies specifically reported that patients returned to their preinjury level of performance or higher at a rate of 81.1% (range 50% to 100%). Nine studies described changes in the level of sports participation after treatment compared with the preinjury level.
Figure 2.
Rates of return to play after operative management of AC joint separation reported in the literature.
Surgical techniques
Fifty-two of the 63 studies (82.5%) used a single surgical technique. Nine studies (14.3%) reported on 2 surgical techniques while 2 studies (3.2%) included 3 or more techniques. Twenty-one studies (33.3%) reported the use of an arthroscopic-assisted technique. In all, 11 primary modes of stabilization, 9 of which involved reconstructing or repairing the coracoclavicular ligaments and 2 involved AC stabilization primarily, were identified, and 5 methods of auxiliary AC joint stabilization or augmentation were also identified and used in 27 studies (42.9%) (Table V). Twenty-six combinations of surgical techniques were identified, with the most commonly reported being suture button constructs without additional AC stabilization (18 studies, 28.6%). In looking at primary stabilization methods regardless of the utilization of auxiliary AC stabilization, the most frequently used surgical technique involved suture button constructs (28 studies, 44.4%), followed by suture constructs, soft-tissue graft constructs, artificial graft constructs (8 studies each, 12.7%), and hook plate stabilization (7 studies, 11.1%). The most frequently used auxiliary AC stabilization techniques involved soft-tissue graft reconstruction and suture repair (8 studies each, 12.7%). Fifteen techniques included combined coracoclavicular and AC joint stabilization, with the most frequently used being soft-tissue graft reconstruction of both joints (5 studies, 7.9%). With regard to distal clavicle excision, a Weaver-Dunn-type procedure was used in 4 studies (6.3%), and 7 studies (11.1%) used techniques that always, or sometimes, required a distal clavicle excision. A free soft-tissue graft was used in 11 studies (17.5%), while the coracoclavicular ligaments were repaired in 8 studies (12.7%). See Table V for further information.
Table V.
Number of studies using various surgical techniques.∗
| Technique | Studies | Technique | Studies |
|---|---|---|---|
| Primary stabilization method | Number of techniques described | ||
| Suture button construct | 28 | 1 | 52 |
| Suture-only construct | 8 | 2 | 9 |
| Soft-tissue graft reconstruction | 8 | ≥3 | 2 |
| Synthetic graft | 8 | ||
| Clavicular hook plate | 7 | Open surgical approach | 44 |
| Suture anchor | 4 | Arthroscopic assistance | 21 |
| Weaver-Dunn procedure | 2 | ||
| Combined soft-tissue graft and suture button | 3 | Use of distal clavicle excision | |
| Coracoclavicular screw | 3 | No | 58 |
| Combined Weaver-Dunn and soft-tissue graft augmentation | 2 | Yes/Sometimes | 7 |
| Acromioclavicular pinning | 1 | Weaver-Dunn | 3 |
| Auxiliary acromioclavicular stabilization | Free soft-tissue graft utilization | ||
| None | 37 | None | 55 |
| Reconstruction with soft-tissue graft | 8 | Autograft | 6 |
| Suture repair | 8 | Allograft | 3 |
| Pinning | 7 | Both or unclear source | 2 |
| Suture reconstruction | 6 | ||
| Reconstruction with artificial graft | 1 | No coracoclavicular ligaments repair | 58 |
| Coracoclavicular ligaments repaired | 9 |
Owing to several studies describing multiple techniques, values exceed the overall number of included studies.
Discussion
The results of this systematic review suggest that, despite the high incidence of AC joint injuries among athletes, return-to-play criteria remain insufficiently defined. Currently, no comprehensive guidelines for rehabilitation and return to sport have been recognized.
Return-to-play rates after management of AC joint separations are consistently high. Two recent systematic reviews evaluating return to sport outcomes after surgical treatment demonstrate return-to-play rates greater than 90%, which are consistent with our results.28,71 Despite these high rates of return to play, the rates of reinjury and loss of reduction are not insignificant. While the incidence of reduction loss is largely dependent on variations in hardware implantation and surgical technique, several case series have demonstrated loss of reduction rates as high as 15% to 80%.14,39,79 Premature progression through rehabilitation as well as patient noncompliance with postoperative activity limitations also contribute to loss of reduction and other complications that impede return to optimal athletic performance. For this reason, comprehensive criteria guiding progression through rehabilitation and return to sporting activities must be established.
In this systematic review, we identified 8 unique criteria for return to play after operative management of AC joint dislocations. These criteria can aid the creation of a checklist for return to play after AC joint stabilization surgery. As hypothesized, time from surgery was by far the most commonly reported criterion guiding return to play. Several studies reported other subjective or objective conditional criteria. However, only 1 study cited a functional return-to-play criterion associated with a specific measurement,43 and none of the included studies described a well-defined series of criteria to guide return to play. In addition to explicit return-to-play criteria, we also analyzed rehabilitation protocols to determine which general factors surgeons favored during postoperative rehabilitation. Immobilization (95.2%) and range of motion guidelines (93.7%) were the most commonly cited rehabilitation points of interest, although adequate shoulder motion was explicitly cited as a return-to-play criterion in only one study analyzed in this review.25
In several instances, it was apparent that authors were cognizant of the demands that certain activities might place on the surgical repair. One study imposed restrictions on patients from specifically returning to competitive football matches, rather than athletics in general.8 Two studies provided multiple tiers of return-to-play guidance with 2 different time points, both of which permitted athletes to return to “noncontact sports” at an earlier time point (3 or 4 months, respectively) and then removed all restrictions at 6 months.16,54 All three of these studies were included in this analysis, and we considered the 6-month time point for both studies with a tiered return-to-play protocol.
Few studies used metrics other than time-based criteria to guide return to play. Only 1 study19 used a radiographic return-to-play criterion, and no studies applied a validated scoring assessment to guide return to play. While infrequently used in the context of guiding return to play, these assessments can be considered for use in developing return-to-play guidelines; however, their utility for this purpose is not immediately clear.
In establishing comprehensive return-to-play guidelines, consideration may need to be given to the surgical technique because of the large number of techniques currently being used. Certain techniques involve implantation of hardware, such as AC hook plates, which need to be removed before a patient can return to unrestricted sporting activity.33 Furthermore, the effects of other surgical factors (ie, open vs. arthroscopic procedures, autograft vs. allografts vs. other techniques) remain uncertain as they pertain to establishing return-to-play guidelines.
Lower grade AC joint injuries are generally treated nonoperatively.44,51 In 1997, Gladstone et al22 described a 4-phase rehabilitation protocol, which includes an immobilization period, a range of motion and strengthening period, a functional participation period, and a sports-specific training period. Despite this, return to play after nonoperative treatment of AC joint injuries is rarely the subject of investigation. While this systematic review did not formally assess criteria for return to play after nonoperative treatment of AC joint separations, we identified 4 studies with nonoperative patient cohorts that would have otherwise satisfied inclusion criteria for this review. Among these was one study that focused exclusively on nonoperative patients and three comparative studies of which patients in the operative cohort were included in this analysis. Two of these nonoperative cohorts based their return-to-play guidelines exclusively on time-based criteria,48,56 while the remaining two studies each used a specific subjective criterion: when patients were “asymptomatic” and when patients “felt able” to return to their athletics.8,49
The main limitations of this investigation concern the inherent variability in the reporting of return-to-play criteria and the overall heterogeneity of study characteristics regarding surgical technique and treatment acuity. We only included studies that explicitly mentioned return to athletic activity and excluded studies that may have ultimately contained athletes who returned to sport. Similarly, authors may have provided their patients with return-to-play guidelines, such as completing a rehabilitation program, without explicitly reporting them in their final manuscripts. Owing to advancement in surgical techniques, we included only studies from the last 20 years, which may have limited our ability to identify additional criteria for return to play.
Conclusion
This systematic review revealed that criteria for return to play after operative management of AC joint separations remain insufficiently defined. Most published articles report exclusively time-based criteria, and no studies in this review offered detailed functional return-to-play guidelines. The results of this systematic review provide a foundation for developing a comprehensive return-to-play checklist. Further investigation is needed to establish specific and effective guidelines that will enable athletes to safely return to sport and minimize the recurrence of injury after operative management of AC joint separation.
Disclaimers
Funding: No funding was disclosed by the authors.
Conflicts of interest: Dr. D'Amore reports educational support from Liberty Surgical Inc. and Medical Device Business Services Inc., all of which are not relevant to the submitted work.
Dr. Otlans reports receiving educational support from Liberty Surgical Inc., which is not relevant to the submitted work.
Dr. Cohen reports receiving research support funding from Arthrex, United States and Major League Baseball, United States; personal fees from CONMED Linvatec, Slack Inc., and Zimmer; and is a board/committee member of the American Orthopaedic Society for Sports Medicine and International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine, all of which are not relevant to the submitted work.
Dr. Ciccotti reports receiving grants from DJO LLC, personal fees from Liberty Surgical Inc., and is a board/committee member of the American Orthopaedic Society for Sports Medicine, the Major League Baseball Team Physicians Association, and the Orthopaedic Learning Center, all of which are not relevant to the submitted work.
The other authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this systematic review.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.xrrt.2021.11.005.
Supplementary Data
References
- 1.Abat F., Gich I., Natera L., Besalduch M., Sarasquete J. Clinical factors that affect perceived quality of life in arthroscopic reconstruction for acromioclavicular joint dislocation. Rev Esp Cir Ortopédica Traumatol Engl Ed. 2018;62:121–126. doi: 10.1016/j.recote.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 2.Barth J., Duparc F., Baverel L., Bahurel J., Toussaint B., Bertiaux S., et al. Prognostic factors to succeed in surgical treatment of chronic acromioclavicular dislocations. Orthop Traumatol Surg Res. 2015;101:S305–S311. doi: 10.1016/j.otsr.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 3.Beitzel K., Cote M.P., Apostolakos J., Solovyova O., Judson C.H., Ziegler C.G., et al. Current concepts in the treatment of acromioclavicular joint dislocations. Arthrosc J Arthrosc Relat Surg. 2013;29:387–397. doi: 10.1016/j.arthro.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 4.Beris A., Lykissas M., Kostas-Agnantis I., Vekris M., Mitsionis G., Korompilias A. Management of acute acromioclavicular joint dislocation with a double-button fixation system. Injury. 2013;44:288–292. doi: 10.1016/j.injury.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 5.Boutsiadis A., Baverel L., Lenoir H., Delsol P., Barth J. Arthroscopic-assisted acromioclavicular and coracoclavicular ligaments reconstruction for chronic acromioclavicular dislocations: surgical technique. Tech Hand Up Extrem Surg. 2016;20:172–178. doi: 10.1097/BTH.0000000000000142. [DOI] [PubMed] [Google Scholar]
- 6.Breuer R., Unterrainer A., Komjati M., Tiefenboeck T.M., Trieb K., Pirkl C. Minimally invasive AC joint reconstruction system (MINAR®) in modified triple-button technique for the treatment of acute AC joint dislocation. J Clin Med. 2019;8:1683. doi: 10.3390/jcm8101683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cano-Martínez J.A., Nicolás-Serrano G., Bento-Gerard J., Picazo-Marín F., Andrés-Grau J. Acute high-grade acromioclavicular dislocations treated with triple button device (MINAR): preliminary results. Injury. 2016;47:2512–2519. doi: 10.1016/j.injury.2016.09.029. [DOI] [PubMed] [Google Scholar]
- 8.Cardone D., Brown J.N., Roberts S.N.J., Saies A.D., Hayes M.G. Grade III acromioclavicular joint injury in Australian Rules Football. J Sci Med Sport. 2002;5:143–148. doi: 10.1016/S1440-2440(02)80035-4. [DOI] [PubMed] [Google Scholar]
- 9.Çarkçı E., Polat A.E., Gürpınar T. The frequency of reduction loss after arthroscopic fixation of acute acromioclavicular dislocations using a double-button device, and its effect on clinical and radiological results. J Orthop Surg. 2020;15:136. doi: 10.1186/s13018-020-01674-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carrera EdF., Pierami R., Sugawara M.J., Nicolao F.A., Netto N.A., Matsumoto M.H. Evaluation of the surgical treatment of acromioclavicular joint dislocation with a new option for temporary fixation of the acromioclavicular joint. Tech Shoulder Elb Surg. 2013;14:99–103. [Google Scholar]
- 11.Chang N., Furey A., Kurdin A. Operative versus nonoperative management of acute high-grade acromioclavicular dislocations: a systematic review and meta-analysis. J Orthop Trauma. 2018;32:1–9. doi: 10.1097/BOT.0000000000001004. [DOI] [PubMed] [Google Scholar]
- 12.Cho C.-H., Kim B.-S., Kwon D.-H. Importance of additional temporary pin fixation combined coracoclavicular augmentation using a suture button device for acute acromioclavicular joint dislocation. Arch Orthop Trauma Surg. 2016;136:763–770. doi: 10.1007/s00402-016-2437-5. [DOI] [PubMed] [Google Scholar]
- 13.Coleman B.D., Khan K.M., Maffulli N., Cook J.L., Wark J.D. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Scand J Med Sci Sports. 2000;10:2–11. doi: 10.1034/j.1600-0838.2000.010001002.x. [DOI] [PubMed] [Google Scholar]
- 14.Cook J.B., Shaha J.S., Rowles D.J., Bottoni C.R., Shaha S.H., Tokish J.M. Early failures with single clavicular transosseous coracoclavicular ligament reconstruction. J Shoulder Elbow Surg. 2012;21:1746–1752. doi: 10.1016/j.jse.2012.01.018. [DOI] [PubMed] [Google Scholar]
- 15.Cote M.P., Wojcik K.E., Gomlinski G., Mazzocca A.D. Rehabilitation of acromioclavicular joint separations: operative and nonoperative considerations. Clin Sports Med. 2010;29:213–228. doi: 10.1016/j.csm.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 16.Dal Molin F., Feder M.G., Gaibor G.R.G. Quadruple repair technique for acromioclavicular dislocation. Tech Shoulder Elb Surg. 2017;18:65–71. doi: 10.1097/BTE.0000000000000093. [DOI] [Google Scholar]
- 17.De Carli A., Lanzetti R., Ciompi A., Lupariello D., Rota P., Ferretti A. Acromioclavicular third degree dislocation: surgical treatment in acute cases. J Orthop Surg. 2015;10:13. doi: 10.1186/s13018-014-0150-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dimakopoulos P., Panagopoulos A., Syggelos S.A., Panagiotopoulos E., Lambiris E. Double-loop suture repair for acute acromioclavicular joint disruption. Am J Sports Med. 2006;34:1112–1119. doi: 10.1177/0363546505284187. [DOI] [PubMed] [Google Scholar]
- 19.El Shewy M.T., El Azizi H. Suture repair using loop technique in cases of acute complete acromioclavicular joint dislocation. J Orthop Traumatol. 2011;12:29–35. doi: 10.1007/s10195-011-0130-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gangary S.K., Meena S. Arthroscopic stabilization of acute acromioclavicular joint dislocation with tightrope AC system: a tale of failures. J Arthrosc Joint Surg. 2016;3:13–16. doi: 10.1016/j.jajs.2015.11.003. [DOI] [Google Scholar]
- 21.Garofalo R., Ceccarelli E., Castagna A., Calvisi V., Flanagin B., Conti M., et al. Open capsular and ligament reconstruction with semitendinosus hamstring autograft successfully controls superior and posterior translation for type V acromioclavicular joint dislocation. Knee Surg Sports Traumatol Arthrosc. 2017;25:1989–1994. doi: 10.1007/s00167-017-4509-7. [DOI] [PubMed] [Google Scholar]
- 22.Gladstone J.N., Wilk K.E., Andrews J.R. Nonoperative treatment of acromioclavicular joint injuries. Oper Tech Sports Med. 1997 Apr;5:78–87. [Google Scholar]
- 23.GÓmez Vieira L.A., Visco A., Daneu Fernandes L.F., GÓmez Cordero N.G. Arthroscopic treatment of acromioclavicular joint dislocation by tight rope technique (Arthrex®) Rev Bras Ortop Engl Ed. 2009;44:52–56. doi: 10.1016/S2255-4971(15)30049-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Greiner S., Braunsdorf J., Perka C., Herrmann S., Scheffler S. Mid to long-term results of open acromioclavicular-joint reconstruction using polydioxansulfate cerclage augmentation. Arch Orthop Trauma Surg. 2009;129:735–740. doi: 10.1007/s00402-008-0688-5. [DOI] [PubMed] [Google Scholar]
- 25.Hashiguchi H., Iwashita S., Abe K., Sonoki K., Yoneda M., Takai S. Arthroscopic coracoclavicular ligament reconstruction for acromioclavicular joint dislocation. J Nippon Med Sch. 2018;85:166–171. doi: 10.1272/jnms.JNMS.2018_85-24. [DOI] [PubMed] [Google Scholar]
- 26.Hou Z., Graham J., Zhang Y., Strohecker K., Feldmann D., Bowen T.R., et al. Comparison of single and two-tunnel techniques during open treatment of acromioclavicular joint disruption. BMC Surg. 2014;14:53. doi: 10.1186/1471-2482-14-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Katsenis D.L., Stamoulis D., Begkas D., Tsamados S. Minimally invasive reconstruction of acute type IV and type V acromioclavicular separations. Orthopedics. 2015;38:e324–e330. doi: 10.3928/01477447-20150402-62. [DOI] [PubMed] [Google Scholar]
- 28.Kay J., Memon M., Alolabi B. Return to sport and clinical outcomes after surgical management of acromioclavicular joint dislocation: a systematic review. Arthrosc J Arthrosc Relat Surg. 2018;34:2910–2924.e1. doi: 10.1016/j.arthro.2018.04.027. [DOI] [PubMed] [Google Scholar]
- 29.Kocaoglu B., Ulku T.K., Gereli A., Karahan M., Türkmen M. Palmaris longus tendon graft versus modified Weaver-Dunn procedure via dynamic button system for acromioclavicular joint reconstruction in chronic cases. J Shoulder Elbow Surg. 2017;26:1546–1552. doi: 10.1016/j.jse.2017.01.024. [DOI] [PubMed] [Google Scholar]
- 30.Krul K.P., Cook J.B., Ku J., Cage J.M., Bottoni C.R., Tokish J.M. Successful conservative therapy in Rockwood type V acromioclavicular dislocations. Orthop J Sports Med. 2020;3 doi: 10.1177/2325967115S00017. [DOI] [Google Scholar]
- 31.Kurtoglu A., Sukur E., Cicekli O., Daldal I., Kochai A., Sen Z., et al. Does the ZipTight effective to maintain reduction after the treatment of acute acromioclavicular joint dislocation? Medicine (Baltimore) 2020;99:e19387. doi: 10.1097/MD.0000000000019387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lädermann A., Grosclaude M., Lübbeke A., Christofilopoulos P., Stern R., Rod T., et al. Acromioclavicular and coracoclavicular cerclage reconstruction for acute acromioclavicular joint dislocations. J Shoulder Elbow Surg. 2011;20:401–408. doi: 10.1016/j.jse.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 33.Lee S., Bedi A. Shoulder acromioclavicular joint reconstruction options and outcomes. Curr Rev Musculoskelet Med. 2016;9:368–377. doi: 10.1007/s12178-016-9361-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee S.-J., Yoo Y.-S., Kim Y.-S., Jang S.-W., Kim J., Kim S.-J., et al. Arthroscopic coracoclavicular fixation using multiple low-profile devices in acute acromioclavicular joint dislocation. Arthrosc J Arthrosc Relat Surg. 2019;35:14–21. doi: 10.1016/j.arthro.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 35.Leidel B.A., Braunstein V., Kirchhoff C., Pilotto S., Mutschler W., Biberthaler P. Consistency of long-term outcome of acute Rockwood grade III acromioclavicular joint separations after K-wire transfixation. J Trauma Inj Infect Crit Care. 2009;66:1666–1671. doi: 10.1097/TA.0b013e31818c1455. [DOI] [PubMed] [Google Scholar]
- 36.Li H., Wang C., Wang J., Wu K., Hang D. Restoration of horizontal stability in complete acromioclavicular joint separations: surgical technique and preliminary results. Eur J Med Res. 2013;18:42. doi: 10.1186/2047-783X-18-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu X., Huangfu X., Zhao J. Arthroscopic treatment of acute acromioclavicular joint dislocation by coracoclavicular ligament augmentation. Knee Surg Sports Traumatol Arthrosc. 2015;23:1460–1466. doi: 10.1007/s00167-013-2800-9. [DOI] [PubMed] [Google Scholar]
- 38.Lu D., Wang T., Chen H., Sun L.-J. A comparison of double Endobutton and triple Endobutton techniques for acute acromioclavicular joint dislocation. Orthop Traumatol Surg Res. 2016;102:891–895. doi: 10.1016/j.otsr.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 39.Ma R., Smith P.A., Smith M.J., Sherman S.L., Flood D., Li X. Managing and recognizing complications after treatment of acromioclavicular joint repair or reconstruction. Curr Rev Musculoskelet Med. 2015;8:75–82. doi: 10.1007/s12178-014-9255-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marcheggiani Muccioli G.M., Manning C., Wright P., Grassi A., Zaffagnini S., Funk L. Acromioclavicular joint reconstruction with the LARS ligament in professional versus non-professional athletes. Knee Surg Sports Traumatol Arthrosc. 2016;24:1961–1967. doi: 10.1007/s00167-014-3231-y. [DOI] [PubMed] [Google Scholar]
- 41.Metzlaff S., Rosslenbroich S., Forkel P.H., Schliemann B., Arshad H., Raschke M., et al. Surgical treatment of acute acromioclavicular joint dislocations: hook plate versus minimally invasive reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24:1972–1978. doi: 10.1007/s00167-014-3294-9. [DOI] [PubMed] [Google Scholar]
- 42.Moher D., Liberati A., Tetzlaff J., Altman D.G., The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Motta P., Bruno L., Maderni A., Tosco P., Mariotti U. Acromioclavicular motion after surgical reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20:1012–1018. doi: 10.1007/s00167-011-1627-5. [DOI] [PubMed] [Google Scholar]
- 44.Mouhsine E., Garofalo R., Crevoisier X., Farron A. Grade I and II acromioclavicular dislocations: results of conservative treatment. J Shoulder Elbow Surg. 2003;12:599–602. doi: 10.1016/S1058-2746(03)00215-5. [DOI] [PubMed] [Google Scholar]
- 45.Muench L.N., Kia C., Jerliu A., Murphy M., Berthold D.P., Cote M.P., et al. Functional and radiographic outcomes after anatomic coracoclavicular ligament reconstruction for type III/V acromioclavicular joint injuries. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119884539. 232596711988453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Müller D., Reinig Y., Hoffmann R., Blank M., Welsch F., Schweigkofler U., et al. Return to sport after acute acromioclavicular stabilization: a randomized control of double-suture-button system versus clavicular hook plate compared to uninjured shoulder sport athletes. Knee Surg Sports Traumatol Arthrosc. 2018;26:3832–3847. doi: 10.1007/s00167-018-5044-x. [DOI] [PubMed] [Google Scholar]
- 47.Murena L., Canton G., Vulcano E., Cherubino P. Scapular dyskinesis and SICK scapula syndrome following surgical treatment of type III acute acromioclavicular dislocations. Knee Surg Sports Traumatol Arthrosc. 2013;21:1146–1150. doi: 10.1007/s00167-012-1959-9. [DOI] [PubMed] [Google Scholar]
- 48.Murray I.R., Robinson P.G., Goudie E.B., Duckworth A.D., Clark K., Robinson C.M. Open reduction and tunneled suspensory device fixation compared with nonoperative treatment for type-III and type-IV acromioclavicular joint dislocations: the ACORN prospective, randomized controlled trial. J Bone Joint Surg. 2018;100:1912–1918. doi: 10.2106/JBJS.18.00412. [DOI] [PubMed] [Google Scholar]
- 49.Natera-Cisneros L., Sarasquete Reiriz J. Acute high-grade acromioclavicular joint injuries: quality of life comparison between patients managed operatively with a hook plate versus patients managed non-operatively. Eur J Orthop Surg Traumatol. 2017;27:341–350. doi: 10.1007/s00590-016-1862-z. [DOI] [PubMed] [Google Scholar]
- 50.Natera-Cisneros L., Sarasquete Reiriz J., Besalduch M., Petrica A., Escolà A., Rodriguez J., et al. Horizontal and vertical stabilization of acute unstable acromioclavicular joint injuries arthroscopy-assisted. Arthrosc Tech. 2015;4:e721–e729. doi: 10.1016/j.eats.2015.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pallis M., Cameron K.L., Svoboda S.J., Owens B.D. Epidemiology of acromioclavicular joint injury in young athletes. Am J Sports Med. 2012;40:2072–2077. doi: 10.1177/0363546512450162. [DOI] [PubMed] [Google Scholar]
- 52.Parnes N., Friedman D., Phillips C., Carey P. Outcome after arthroscopic reconstruction of the coracoclavicular ligaments using a double-bundle coracoid cerclage technique. Arthrosc J Arthrosc Relat Surg. 2015;31:1933–1940. doi: 10.1016/j.arthro.2015.03.037. [DOI] [PubMed] [Google Scholar]
- 53.Porschke F., Schnetzke M., Aytac S., Studier-Fischer S., Gruetzner P.A., Guehring T. Sports activity after anatomic acromioclavicular joint stabilisation with flip-button technique. Knee Surg Sports Traumatol Arthrosc. 2017;25:1995–2003. doi: 10.1007/s00167-016-4287-7. [DOI] [PubMed] [Google Scholar]
- 54.Porschke F., Schnetzke M., Studier-Fischer S., Gruetzner P.A., Guehring T. Return to work after acromioclavicular joint stabilization: a retrospective case control study. J Orthop Surg. 2019;14:45. doi: 10.1186/s13018-019-1071-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ranne J.O., Kainonen T.U., Lehtinen J.T., Kanto K.J., Vastamäki H.A., Kukkonen M.K., et al. Arthroscopic coracoclavicular ligament reconstruction of chronic acromioclavicular dislocations using autogenous semitendinosus graft: a two-year follow-up study of 58 patients. Arthrosc Sports Med Rehabil. 2020;2:e7–e15. doi: 10.1016/j.asmr.2019.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rasmont Q., Delloye C., Van Isacker T. Is conservative treatment still defensible in grade III acromioclavicular dislocation? Are there predictive factors of poor outcome? Acta Orthop Belg. 2015;81:107–114. [PubMed] [Google Scholar]
- 57.Rockwood C.A. In: Fractures in Adults. Rockwood C.A., Green D.P., editors. JB Lippincott; Philadelphia: 1984. Injuries to the acromioclavicular joint; pp. 860–910. [Google Scholar]
- 58.Saccomanno M.F., Fodale M., Capasso L., Cazzato G., Milano G. Reconstruction of the coracoclavicular and acromioclavicular ligaments with semitendinosus tendon graft: a pilot study. Joints. 2020;2:6–14. [PMC free article] [PubMed] [Google Scholar]
- 59.Saier T., Plath J.E., Beitzel K., Minzlaff P., Feucht J.M., Reuter S., et al. Return-to-activity after anatomical reconstruction of acute high-grade acromioclavicular separation. BMC Musculoskelet Disord. 2016;17:145. doi: 10.1186/s12891-016-0989-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sandmann G.H., Martetschläger F., Mey L., Kraus T.M., Buchholz A., Ahrens P., et al. Reconstruction of displaced acromio-clavicular joint dislocations using a triple suture-cerclage: description of a safe and efficient surgical technique. Patient Saf Surg. 2012;6:25. doi: 10.1186/1754-9493-6-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Seo J.-B., Lee D.-H., Kim K.-B., Yoo J.-S. Coracoid clavicular tunnel angle is related with loss of reduction in a single-tunnel coracoclavicular fixation using a dog bone button in acute acromioclavicular joint dislocation. Knee Surg Sports Traumatol Arthrosc. 2019;27:3835–3843. doi: 10.1007/s00167-019-05731-9. [DOI] [PubMed] [Google Scholar]
- 62.Shin S.-J., Yun Y.-H., Yoo J.D. Coracoclavicular ligament reconstruction for acromioclavicular dislocation using 2 suture anchors and coracoacromial ligament transfer. Am J Sports Med. 2009;37:346–351. doi: 10.1177/0363546508324968. [DOI] [PubMed] [Google Scholar]
- 63.Smith T.O., Chester R., Pearse E.O., Hing C.B. Operative versus non-operative management following Rockwood grade III acromioclavicular separation: a meta-analysis of the current evidence base. J Orthop Traumatol. 2011;12:19–27. doi: 10.1007/s10195-011-0127-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Steinbacher G., Sallent A., Seijas R., Boffa J.M., Espinosa W., Cugat R. Clavicular hook plate for grade-III acromioclavicular dislocation. J Orthop Surg. 2014;22:329–332. doi: 10.1177/230949901402200312. [DOI] [PubMed] [Google Scholar]
- 65.Struhl S., Wolfson T.S. Continuous Loop Double Endobutton Reconstruction for Acromioclavicular Joint Dislocation. Am J Sports Med. 2015;43:2437–2444. doi: 10.1177/0363546515596409. [DOI] [PubMed] [Google Scholar]
- 66.Sun L.-J., Lu D., Ma Y.-F., Yu B. Minimally invasive procedure of acute acromioclavicular joint dislocation: one suture-button device versus two suture-button devices. Acta Orthop Belg. 2019;85:54–62. [PubMed] [Google Scholar]
- 67.Tamaoki M.J.S., Lenza M., Matsunaga F.T., Belloti J.C., Matsumoto M.H., Faloppa F. Surgical versus conservative interventions for treating acromioclavicular dislocation of the shoulder in adults. Cochrane Database Sys Rev. 2019;10:1465–1858. doi: 10.1002/14651858.CD007429.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tiefenboeck T.M., Boesmueller S., Popp D., Payr S., Joestl J., Binder H., et al. The use of the LARS system in the treatment of AC joint instability – Long-term results after a mean of 7.4 years. Orthop Traumatol Surg Res. 2018;104:749–754. doi: 10.1016/j.otsr.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 69.Tiefenboeck T.M., Popp D., Boesmueller S., Payr S., Joestl J., Komjati M., et al. Acromioclavicular joint dislocation treated with Bosworth screw and additional K-wiring: results after 7.8 years – still an adequate procedure? BMC Musculoskelet Disord. 2017;18:339. doi: 10.1186/s12891-017-1692-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Triantafyllopoulos I.K., Lampropoulou-Adamidou K., Schizas N.P., Karadimas E.V. Surgical treatment of acute type V acromioclavicular joint dislocations in professional athletes: an anatomic ligament reconstruction with synthetic implant augmentation. J Shoulder Elbow Surg. 2017;26:e369–e375. doi: 10.1016/j.jse.2017.05.032. [DOI] [PubMed] [Google Scholar]
- 71.Verstift D.E., Welsink C.L., Spaans A.J., van den Bekerom M.P.J. Return to sport after surgical treatment for high-grade (Rockwood III–VI) acromioclavicular dislocation. Knee Surg Sports Traumatol Arthrosc. 2019;27:3803–3812. doi: 10.1007/s00167-019-05528-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Vitali M., Pedretti A., Naim Rodriguez N., Franceschi A., Fraschini G. Vascular graft employment in the surgical treatment of acute and chronic acromio-clavicular dislocation. Eur J Orthop Surg Traumatol. 2015;25:1205–1211. doi: 10.1007/s00590-015-1672-8. [DOI] [PubMed] [Google Scholar]
- 73.Vulliet P., Le Hanneur M., Cladiere V., Loriaut P., Boyer P. A comparison between two double-button endoscopically assisted surgical techniques for the treatment acute acromioclavicular dislocations. Musculoskelet Surg. 2018;102:73–79. doi: 10.1007/s12306-017-0501-0. [DOI] [PubMed] [Google Scholar]
- 74.Wang C., Huang S., Wang Y., Sun X., Zhu T., Li Q., et al. Complete acromioclavicular joint dislocation treated with reconstructed ligament by trapezius muscle fascia and observation of fascial metaplasia. Open Med. 2020;10:370–376. doi: 10.1515/med-2015-0055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wang G., Xie R., Mao T., Xing S. Treatment of AC dislocation by reconstructing CC and AC ligaments with allogenic tendons compared with hook plates. J Orthop Surg. 2018;13:175. doi: 10.1186/s13018-018-0879-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wang S.-J., Wong C.-S. Transacromial extra-articular knowles pin fixation treatment of acute type V acromioclavicular joint injuries. J Trauma Inj Infect Crit Care. 2008;65:424–429. doi: 10.1097/TA.0b013e318068ddd3. [DOI] [PubMed] [Google Scholar]
- 77.Wang Y., Zhang J. Acromioclavicular joint reconstruction by coracoid process transfer augmented with hook plate. Injury. 2014;45:949–954. doi: 10.1016/j.injury.2013.12.013. [DOI] [PubMed] [Google Scholar]
- 78.Warth R.J., Martetschläger F., Gaskill T.R., Millett P.J. Acromioclavicular joint separations. Curr Rev Musculoskelet Med. 2013;6:71–78. doi: 10.1007/s12178-012-9144-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Weinstein D.M., McCann P.D., Mcllveen S.J., Flatow E.L., Bigliani L.U. Surgical treatment of complete acromioclavicular dislocations. Am J Sports Med. 1995;23:324–331. doi: 10.1177/036354659502300313. [DOI] [PubMed] [Google Scholar]
- 80.Wolf E.M., Fragomen A.T. Arthroscopic reconstruction of the coracoclavicular ligaments for acromioclavicular joint separations. Oper Tech Sports Med. 2004;12:49–55. doi: 10.1053/j.otsm.2004.04.008. [DOI] [Google Scholar]
- 81.Wright J., Swiontkowski M., Heckman J. Introducing Levels of Evidence to the Journal. J Bone Joint Surg. 2003;85:1–3. [PubMed] [Google Scholar]
- 82.Xue C., Song L.-J., Zhang H., Tang G.-L., Li X., Fang J.-H. Truly anatomic coracoclavicular ligament reconstruction with 2 Endobutton devices for acute Rockwood type V acromioclavicular joint dislocations. J Shoulder Elbow Surg. 2018;27:e196–e202. doi: 10.1016/j.jse.2017.12.015. [DOI] [PubMed] [Google Scholar]
- 83.Ye T., Ouyang Y., Chen A. Multistrand titanium cable for the coracoclavicular stabilization of acute acromioclavicular joint dislocation. Acta Orthop Belg. 2014;80:5. [PubMed] [Google Scholar]
- 84.Yoo Y.-S., Seo Y.-J., Noh K.-C., Patro B.P., Kim D.-Y. Arthroscopically assisted anatomical coracoclavicular ligament reconstruction using tendon graft. Int Orthop. 2011;35:1025–1030. doi: 10.1007/s00264-010-1124-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.