Abstract
Introduction: Yoga is focused attention by breath and mantra. This forms the basis for a scientific investigation of its effect on various physiological functions such as intraocular pressure (IOP).
Objective: To evaluate the effect of asanas in Yoga on the IOP of practicing individuals.
Methods:A prospective, observational study was performed on 107 volunteers practising the asanas such as Sun salutation exercise (Surya Namaskar), Skull shining breath (Kapalabhati Pranayama), Downward facing dog (Adho Mukha Svanasana), Standing forward bend (Uttanasana), Legs up the wall pose (Viparita Karani), Alternate breathing technique (Anulom Vilom), Deep meditation (Dhyana), Bellows breath (Bhastrika Pranayama), Yoga head stand (Shirshasana) and control of breathing exercise (Pranayama) each for five minutes/day (40-60 minutes) for at least five days in a week for 12 weeks. The IOP measurement was performed for each asana (before and after) at baseline and every four weeks. The primary outcome was the change in IOP. Statistical analyses were performed using Statistical Package for Social Sciences version 23.0. A p-value of less than 0.05 was considered statistically significant.
Results:The mean age of the participants was 42.64±7 years, and the male to female ratio was 1.2:1. Skull shinning breath, Sun salutation, Downward facing dog, Standing forward bend, Legs up the wall pose, Deep meditation and alternate breathing techniques showed a significant mean reduction in IOP at baseline, followed by every four weeks, till week 12, while Yoga head stand, Bellows breath and control of breath led to a significant increase in IOP.
Conclusion:Yoga head stand, Bellows breath and control of breathing technique worsen IOP transiently.
Keywords:YOGA, intraocular pressure, Skull shining breath.
INTRODUCTION
Yoga is a set of exercises (movements and poses) vital for health promotion, disease prevention, and rehabilitation (1). Although Yoga is a practice of uniting the mind, body and spirit, it has become a trend to promote physical and mental well-being (2). Traditionally, Yoga is advised for ethical lifestyle and spiritual practice; presently, it is limited to physical postures (asanas), breathing techniques [control of breathing technique (Pranayama)], and meditation (dhyana) (3). Across the globe, these physically-oriented Yoga forms are gaining popularity as adjunct therapeutic practices. There is a dramatic shift in the practice of Yoga from maintaining good health to attaining good health. About half of those who practice Yoga started practising explicitly to improve their health (4). Yoga is focused attention by breath, mantra, and sound. Approximately 30 million people worldwide practice Yoga regularly (5). This forms the basis for a scientific investigation of its effect on various physiological functions, such as intraocular pressure (IOP).
Intraocular pressure increases in a body position other than standing or seated (6). A slight variation in IOP can be detected while changing posture from sitting to the head-down position (7). Many Yoga exercises lower IOP to different degrees after aerobic and isometric exercise protocols of varying duration and intensity. In some studies, a significant reduction in IOP occurs in less than five minutes after beginning the exercise protocol (8).
Yoga induces relaxation and introspection through the arousal of alpha-frontal EEG activity. It lowers the heart rate, respiratory rate, and blood pressure. Stress has now become an integral component of the modern lifestyle. There is a direct correlation between plasma cortisol levels and IOP rise. So, Yoga helps in keeping stress and cortisol levels under control. The recent emergence of Yogic exercises as a most important and potentially modifiable risk factor in glaucoma is exciting, as most other factors cannot be modified or controlled by the patient. Moderate intensity exercise appears to be safe and likely to be beneficial for most people.
Many studies are proving that Yoga and Meditation lower IOP, increase cerebral and ocular blood flow, increase parasympathetic activity and decrease the sympathetic activity of the autonomic nervous system, decrease oxidative stress, decrease Interleukin-6 (IL-6) and Tumor Necrosis Factor-alpha (TNF-α) levels and decrease glutamate levels in the brain.
Yoga is also known to up-regulate gene expression that initiates neuroprotection, decrease age-related central nervous system (CNS) atrophy and brain aging, decrease stress and hence improving the quality of life, downregulate transforming growth factor-beta (TGF-β) in the trabecular meshwork and blood thus enhancing aqueous outflow and increase night-time plasma melatonin levels (9).
The Yogic poses associated with a rise in IOP may be explained by the hydrostatic increase in the pressure of episcleral veins and orbital veins into which aqueous humour is eventually drained and the pressures of which directly influence the IOP according to the Goldmann equation, Po = (F/C) + Pv, where Po is the IOP in mm Hg, F is the rate of aqueous formation, C is the facility of outflow and Pv is the episcleral venous pressure (10). But only a few of these studies show which Yogic postures are beneficial and which postures need to be avoided by ocular hypertensives and glaucoma patients. This led us to the inception of this study to determine which Yogic postures were effective in lowering IOP and which asanas should be avoided by the ocular hypertensive population. To the best of our knowledge, this is the first study highlighting the effect of 10 Yogic asanas on intraocular pressure with a long-term follow-up.
MATERIALS AND METHODS
This is a prospective observational study with a cohort of 107 subjects tested at a renowned yoga facility in the tier 2 city of Western Rajasthan in India. The study was performed by a team of ophthalmologists in a tertiary eye care institute of national importance. It was initiated on the 9th of August 2018 and concluded within 18 months. Healthy individuals above 18 years of age and of either gender practising regular Yoga were recruited for the study. People with known ophthalmic diseases, pediatric patients, and patients with systemic comorbidities such as uncontrolled diabetes, uncontrolled hypertension, severe cardiac disease, renal, liver, and pulmonary diseases were excluded from the study. Participants were enrolled only after they provided written informed consent.
In contrast, 48 participants performed all ten asanas (including Shirshashna and Bhastrika Pranayama) for five minutes each, with a gap of 5–10 minutes between each asana. One experienced Yoga instructor monitored the Yoga exercises. Participants performed Shirshashna at the end of the Yoga session. After recruitment, each participant underwent baseline ophthalmic investigations such as Snellen's visual acuity for distance and near vision and pin-hole vision, detailed anterior segment evaluation, including cornea, pupil, lens, and anterior chamber depth by A-scan, undilated and dilated fundus evaluation by +90 D lens.
We measured the IOP of both eyes of the participants for each pose. The IOP was measured immediately at the start of the pose and just after its completion in a seated position. All IOP readings were taken using I-Care tonometer. The IOP of each participant was measured at a four-week interval for a total period of 12 weeks.
Ethics approval and consent to participate
The study was approved by the Institutional Ethics Committee of All India Institute of Medical Sciences (AIIMS), Jodhpur, India. It was undertaken according to the World Medical Association's Declaration of Helsinki of 1975, as revised in 2000, and ICMR GCP guidelines. Voluntary, written, informed consent was obtained from all enrolled study participants (Institutional Ethics Committee Certificate reference number AIIMS/IEC/2016/224).
Statistical analysis
Statistical analyses were performed using SPSS version 23.0 (SPSS, Inc., Chicago, IL). The paired Student t-test was used to compare pre- and postfor each asana at baseline and week 12. In addition, the t-test for two independent samples was used to compare baseline and week 12 groups. A P-value less than 0.05 was considered statistically significant.
RESULTS
Subjects had a mean age of 42.64±7 years and most of them (55.1%) were males. None of the study participants had a significant family history of glaucoma. The summary of baseline characteristics of intraocular pressure recorded in all Yoga performing subjects (Table 1).
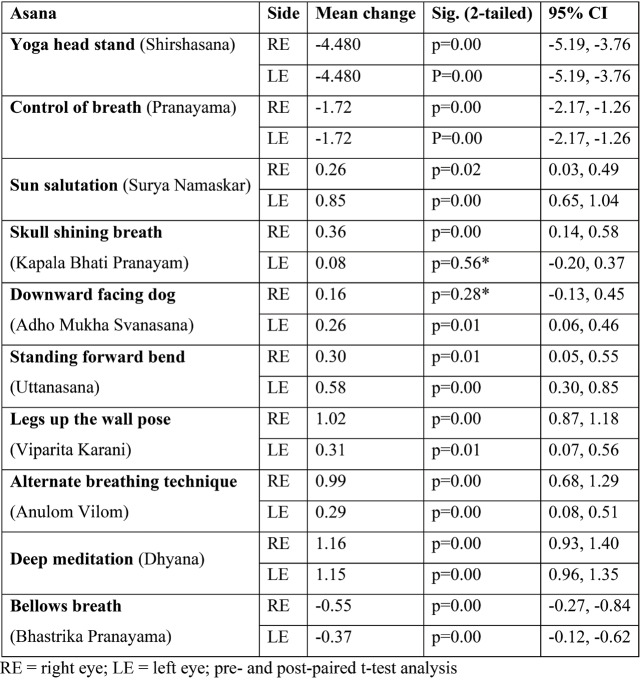
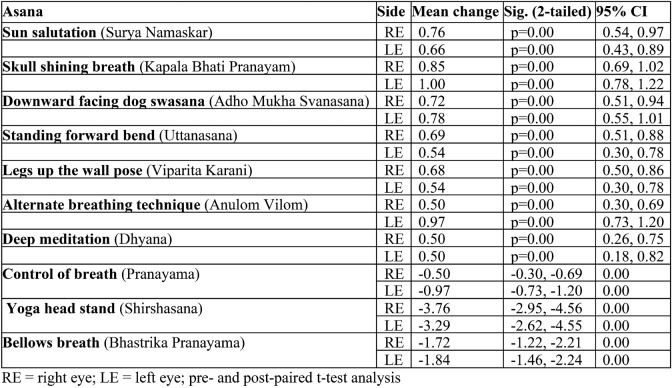
In our study, after performing Skull shining breath (Kapala Bhati Pranayam), the mean change (decrease) in IOP was 0.36 mm Hg in the right eye (RE) and 0.08 mm Hg in the left eye (LE) at baseline versus 0.36 mm Hg (RE) and 0.27 mm Hg (LE) at 12 weeks.
Evaluating for Alternate breathing technique (Anulom Vilom) showed that the mean change (decrease) in IOP was 0.99 mm Hg (RE) and 0.29 mm Hg (LE) at baseline versus 0.59 mm Hg (RE) and 0.43 mm Hg (LE) at 12 weeks.
A similar result was found for Sun salutations exercise (Surya Namaskar): the mean change (decrease) in IOP was 0.26 mm Hg (RE) and 0.26 mm Hg (LE) at baseline versus 0.46 mm Hg (RE) and 0.20 mm Hg (LE) at 12 weeks.
Considering Standing forward bend (Uttanasana), the mean change (decrease) in IOP was 0.30 mm Hg (RE) and 0.58 mm Hg (LE) at baseline versus 0.66 mm Hg (RE) and 0.73 mm Hg (LE) at 12 weeks.
For Downward facing dog (Adho Mukha Svanasana), the mean change (decrease) in IOP was 0.16 mm Hg (RE) and 0.26 mm Hg (LE) at baseline versus 0.46 mm Hg (RE) and 0.20 mm Hg (LE) at 12 weeks.
Considering Legs up the wall pose (Viparita Karani), the mean change (decrease) in IOP was 1.02 mm Hg (RE) and 0.32 mm Hg (LE) at baseline versus 0.69 mm Hg (RE) and 0.84 mm Hg (LE) at 12 weeks.
A similar result was found for Deep meditation (Dhyana): the mean change (decrease) in IOP was 1.16 mm Hg (RE) and 1.15 mm Hg (LE) at baseline versus 0.44 mm Hg (RE) and 0.42 mm Hg (LE) at 12 weeks.
On the contrary, Yoga head stand (Shirshasana) significantly raised the IOP, with the mean change being 4.34 mm Hg (RE) and 4.29 mm Hg (LE) at baseline versus 3.76 mm Hg (RE) and 3.291 mm Hg (LE) at 12 weeks.
Likewise, while practising Bellows breath (Bhastrika Pranayama), the mean change (increase) in IOP was 1.69 mm Hg (RE) and 1.88 mm Hg (LE) at baseline versus 1.72 mm Hg (RE) and 1.84 mm Hg (LE) at 12 weeks (Tables 2 and 3).
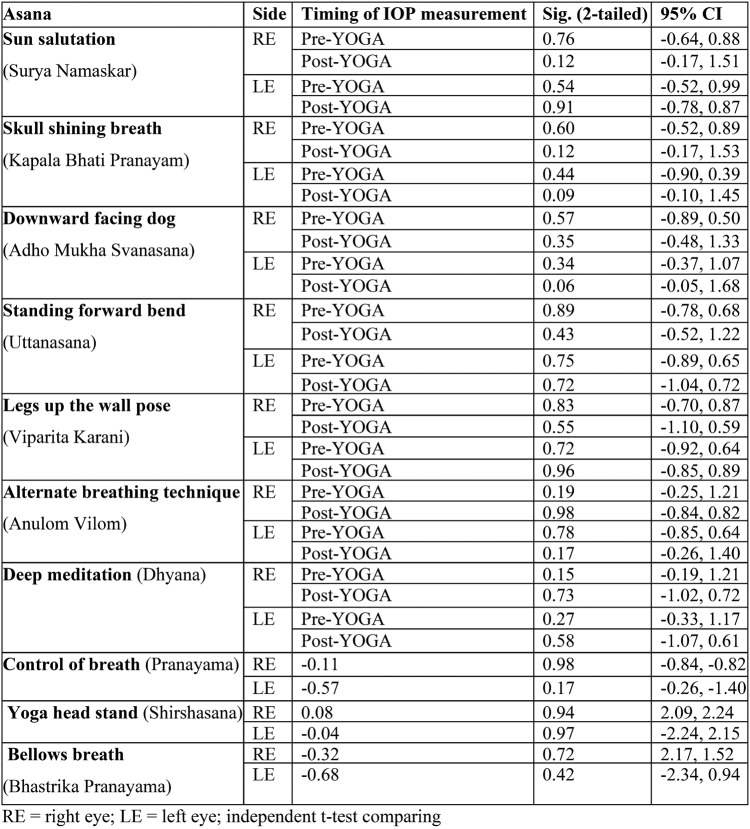
While practising the control of breath technique (Pranayama), the mean change (increase) in IOP was 1.71 mm Hg (RE) and 1.73 mm Hg (LE) at baseline versus -0.11 mm Hg (RE) and -0.57 mm Hg (LE) at 12 weeks. No significant difference was recorded in mean baseline IOP, and to the 12th week, each post asana mean IOP in both eyes (Table 4).
All subjects with IOP rise were referred to an ophthalmologist.
DISCUSSION
The word "Yoga" has come from the Sanskrit root "Yuj," which means to unite, join or yoke and make one concentrate towards a particular task. Regular Yoga practice improves strength, endurance, joint mobility and flexibility, the attitude of togetherness, friendliness, self-discipline, a sense of compassion, and relaxation and promotes well-being. The increasing trend toward a traditional Indian system of exercises (movements and postures/poses) Yoga has many health effects and is now practised for health promotion and disease prevention worldwide. These exercises have excellent health benefits and are free from any adverse effects. However, these exercises may affect many physiological processes, such as IOP. Some Yogic postures increase IOP, and prolonged practice of such postures may affect patients with glaucoma (11). Our study aimed to determine the effect of various Yoga asanas on the IOP of otherwise healthy individuals. The results of this study can be extrapolated to the prevention and control of IOP in glaucoma patients.
Our findings suggest that Yoga head stand (Shirshasana), a downward-facing posture, Bellows breath (Bhastrika Pranayama) and control of breath (Pranayama), which are types of breathing exercises, increase IOP and may cause pressure-related damage to the eye. On assuming a head stand position and the body vertical, IOP begins to rise, which results in a doubling of the IOP, which remains elevated as long as the subject maintains this position (12). Gallardo et al (2006) reported a case of a female patient who was routinely practising Yoga head stand (Shirshasana) for many years and suffered progressive glaucomatous optic neuropathy (13). Similarly, Sankalp et al (2018) and Bertschinger et al (2007) also mentioned a raised IOP and worsening glaucomatous visual field defect (14, 15).
Of note, many Yoga practitioners recommend pranayama as a routine exercise to keep the mind and body in balance. Bellows breath (Bhastrika Pranayama) and control of breath technique (Pranayama) are breathing exercises performed by a large subset of the population which are considered harmless. On the contrary, in our study, it increased IOP. To the best of our knowledge, none of the studies published so far reports the effect of Bellows breath (Bhastrika Pranayama) and control of breath technique (Pranayama) on IOP.
However, our study's astonishing and unique observation was that the IOP worsening was only transient. On a long-term follow-up of 12 weeks, it was observed that the mean IOP from baseline was not significantly raised, suggesting that these asanas do not have a long-term negative impact on IOP. However, this observation needs to be further detailed with the support of more objective tests for glaucoma progression.
Our study also gave insights that Alternate breathing technique (AnulomVilom), a type of slow nasal breathing exercise, and Skull shining breath (Kapala Bhati Pranayam), which involves forceful breathing through the nose, have a favourable effect (decrease in IOP). Pramanik et al showed that slow pace breathing exercise (respiratory rate 6/min) had the potential to improvise the autonomic nervous system through enhanced activation of the parasympathetic system, which may lead to a favourable effect (decrease in IOP) (16). Also, Pal et al showed that regular practice of slow breathing exercises like Alternate breathing technique (Anulom Vilom) for three months improved autonomic functions, while fast breathing exercises for the same duration did not affect the autonomic functions (17).
Backon et al reported a change in IOP on forced unilateral nostril breathing (FUNB). They found that IOP decreased with the right side FUNB, while the left side FUNB increased the IOP (18). Gosewade et al suggested that simple eye exercises and Kapalbhaati helped improve visual reaction time (19). Dada et al did a study on a Yoga population (one hour per day for 21 days), and the results were very positive. This comprehensive study proved that decreased cortisol levels lower the inflammatory marker (IL-6 and TNF-alpha) levels. The results also showed an up-regulation of 54 genes, down-regulation of 56 genes, lowering IOP by parasympathetic action, increased trabecular meshwork outflow, and increased night-time plasma melatonin levels (20-21).
There was no statistically significant difference between post-asanas IOP measurements at week 12 compared with the baseline value. However, a sudden change in IOP was recorded while performing asanas. Therefore, a long-duration study is needed to confirm the sustained effects.
The strengths of our study include a prospective study with a long-term follow-up, a large sample size compared to previous studies, the inclusion of 10 Yogic asanas, and consideration of both eyes for IOP measurement since glaucoma is primarily bilateral. A significant limitation of the study was that we could not analyze the central corneal thickness compensated IOP, which could give a much more predictive result by removing one of the major confounding factors. We plan to include an additional objective test in future studies.
CONCLUSION
Our study suggests that Sun salutation (Surya Namaskar), Skull shining breath (Kapala Bhati Pranayam), Downward facing dog (Adho Mukha Svanasana), Legs up the wall pose (Viparita Karani), alternate breathing technique (Anulom Vilom), standard forward bending (Uttanasana) and Deep meditation (Dhyana) have a favourable effect (decrease in IOP), while Yoga head stand (Shirshasana), Bellows breath (Bhastrika Pranayama) and control of breath technique (Pranayama) worsen IOP transiently and are more likely to cause pressure-related changes in the eye, although on a long-term follow-up of 12 weeks we did not observe a significant difference in IOP by any of the asanas. It is recommended that healthy individuals practising Yoga head stand (Shirshasana), Bellows breath (Bhastrika Pranayama) and control of breath technique (Pranayama) have a regular check-up of their IOP as these asanas may worsen IOP. Also, as suggested, subjects with ocular hypertension and those with glaucoma can do Yoga in moderation and improve their quality of life.
Conflicts of interest: none declared.
Financial support: none declared.
Acknowledgments: The authors would like to thank Dr. Kanchan Chaudhary, Dr. Sulabh Sahu, Dr. Sujeet Prakash and Dr. Kirandeep Kaur for their technical help for the present article.
TABLE 1.

Baseline demographic characteristics of study participants
TABLE 2.
Effect of various asanas on IOP of both eyes at baseline
TABLE 3.
Effect of various asanas on IOP of both eyes at 12th week
TABLE 4.
Change in mean IOP from baseline to week 12 for each asana in both eyes
Contributor Information
Arvind Kumar MORYA, Cataract, Glaucoma, Refractive, Squint, Pediatric Ophthalmology and Medical Retina Services, All India Institute of Medical Sciences, Bibinagar, Hyderabad, Telangana, India.
Ankur Kumar SHRIVASTAVA, Department of Ophthalmology, All India Institute of Medical Sciences, Raipur, India.
Siddharam S JANTI, All India Institute of Medical Sciences, Bibinagar, Hyderabad, Telangana, India.
Antarvedi TEJASWINI, All India Institute of Medical Sciences, Bibinagar, Telangana, India.
Rajan GUPTA, Rajan Eye Heart & Laser Centre, Tohana Distt. Fatehabad, Haryana, India.
Bharat GURNANI, Consultant Cataract, Cornea, External Disease, Trauma, Ocular Surface and Refractive Surgery, Dr. Om Parkash Eye Institute, Amritsar, Punjab, India.
Dharavath VENKATESH, Department of Ophthalmology, All India Institute of Medical Sciences, Bibinagar, Telangana, India.
Rajendra PRASAD, Department of Ophthalmology, RP Eye Institute, New Delhi, India.
References
- 1.Kuntsevich V, Bushell WC, Theise ND. Mechanisms of yogic practices in health, aging, and disease. Mt Sinai J Med. 2010;77:559–569. doi: 10.1002/msj.20214. [DOI] [PubMed] [Google Scholar]
- 4.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1–23. [PubMed] [Google Scholar]
- 5.Tarkkanen A, Leikola J. Pathophysiology Postural variations of the intraocular pressure. Actaophthalmologica. 1967;45:569–575. doi: 10.1111/j.1755-3768.1967.tb06523.x. [DOI] [PubMed] [Google Scholar]
- 6.Wilensky JT. Diurnal variations in intraocular pressure. Trans Am Ophthalmol Soc. 1991;89:757–790. [PMC free article] [PubMed] [Google Scholar]
- 7.Baskaran M, Raman K, Ramani KK, et al. Intraocular pressure changes and ocular biometry during Sirsasana (headstand posture) in yoga practitioners. Ophthalmology. 2006;113:1327–1332. doi: 10.1016/j.ophtha.2006.02.063. [DOI] [PubMed] [Google Scholar]
- 9.Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 10.Jasien JV, Jonas JB, de MoraesCG, et al. Intraocular Pressure Rise in Subjects with and without Glaucoma during Four Common Yoga Positions. PLoS One. 2015;10:0144505. doi: 10.1371/journal.pone.0144505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baskaran C, Volkening LK, Diaz M, et al. A decade of temporal trends in overweight/obesity in youth with type 1 diabetes after the Diabetes Control and Complications Tria. Pediatr Diabetes. 2015;16:263–270. doi: 10.1111/pedi.12166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gallardo MJ, Aggarwal N, Cavanagh HD, et al. Progression of glaucoma associated with the Sirsasana (headstand) yoga posture. Adv Ther. 2006;23:921–925. doi: 10.1007/BF02850214. [DOI] [PubMed] [Google Scholar]
- 14.Bertschinger DR, Mendrinos E, Dosso A. Yoga can be dangerous—glaucomatous visual field defect worsening due to postural yoga. Br J Ophthalmol. 2007;91:1413–1414. doi: 10.1136/bjo.2007.114546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sankalp, Dada T, Yadav RK, Faiq MA. Effect of Yoga-Based Ocular Exercises in Lowering Intraocular Pressure in Glaucoma Patients: An Affirmative Proposition. Int J Yoga. 2018;11:239–241. doi: 10.4103/ijoy.IJOY_55_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pramanik T, Sharma HO, Mishra S, et al. Immediate effect of slow pace bhastrika pranayama on blood pressure and heart rate. J Altern Complement Med. 2009;15:293–295. doi: 10.1089/acm.2008.0440. [DOI] [PubMed] [Google Scholar]
- 17.Pal GK, Velkumary S, Madanmohan. Effect of short-term practice of breathingexercises on autonomic functions in normal human volunteers. Indian J Med Res. 2004;120:115–121. [PubMed] [Google Scholar]
- 18.Backon J, Matamoros N, Ramirez M. A functional vagotomy induced by unilateral forced right nostril breathing decreases intraocular pressure in open and closed-angle glaucoma. Br J Ophthalmol. 1990;74:607–609. doi: 10.1136/bjo.74.10.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gosewade NB, Shende VS, Kashalikar SJ. Effect of Various Eye Exercise Techniques along with Pranayama on Visual Reaction Time: A Case-Control Study. J Clin Diagn Res. 2013;7:1870–1873. doi: 10.7860/JCDR/2013/6324.3338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dada T, Gagrani M. Mindfulness Meditation Can Benefit Glaucoma Patients. J Curr Glaucoma Pract. 2019;13:1–2. doi: 10.5005/jp-journals-10078-1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Udenia H, Mittal S, Agrawal A, et al. Yogic Pranayama and Diaphragmatic Breathing: Adjunct Therapy for Intraocular Pressure in Patients With Primary Open-angle Glaucoma: A Randomized Controlled Trial. J Glaucoma. 2021;30:115–123. doi: 10.1097/IJG.0000000000001697. [DOI] [PubMed] [Google Scholar]