Abstract
Background:
The Affordable Care Act (ACA)-dependent coverage Provision (the Provision), implemented in 2010, extended family insurance coverage to adult children until age 26.
Objectives:
To examine the impact of the ACA Provision on insurance coverage and care among women with a recent live birth.
Research Design, Subjects, and Outcome Measures:
We conducted a difference-in-difference analysis to assess the effect of the Provision using data from the Pregnancy Risk Assessment Monitoring System among 22,599 women aged 19–25 (treatment group) and 22,361 women aged 27–31 years (control group). Outcomes include insurance coverage in the month before and during pregnancy, and at delivery, and receipt of timely prenatal care, a postpartum check-up, and postpartum contraceptive use.
Results:
Compared with the control group, the Provision was associated with a 4.7-percentage point decrease in being uninsured and a 5.9-percentage point increase in private insurance coverage in the month before pregnancy, and a 5.4-percentage point increase in private insurance coverage and a 5.9-percentage point decrease in Medicaid coverage during pregnancy, with similar changes in insurance coverage at delivery. Findings demonstrated a 3.6-percentage point increase in receipt of timely prenatal care, and no change in receipt of a postpartum check-up or postpartum contraceptive use.
Conclusions:
Among women with a recent live birth, the Provision was associated with a decreased likelihood of being uninsured and increased private insurance coverage in the month before pregnancy, a shift from Medicaid to private insurance coverage during pregnancy and at delivery, and an increased likelihood of receiving timely prenatal care.
Keywords: affordable care act, health insurance, dependent coverage, pregnancy, PRAMS
The Affordable Care Act (ACA)-dependent care Provision (hereafter referred to as the Provision) made dependent coverage available to adult children until age 26 and became effective September 23, 2010.1,2 Studies have shown that the Provision improved insurance coverage, access to care, and self-reported health status among young adults.3-7 Although 39% of US births occur among women aged 25 years or younger,8 few studies have examined the effect of the Provision among childbearing women; of those that did, only insurance status at delivery was examined.9,10 State Medicaid expansions enacted during the 1980s lowered income eligibility during pregnancy and ensured that the majority of pregnant women had insurance coverage at time of delivery.8,11,12 However, many women are not covered until after they are pregnant, and this coverage ends after 60 days postpartum.12
Insurance coverage before pregnancy may help improve uptake of preventive services, such as timely prenatal care and interpregnancy care, which can improve pregnancy and infant outcomes.11,13-16 Studies have shown that women without prepregnancy insurance coverage are less likely to receive prenatal care early compared with women with insurance;11,13 that women with private insurance are more likely to receive postpartum care than women with Medicaid;14 and uninsured women at risk for unintended pregnancy are less likely to use contraception.15 A study found that state Medicaid expansions for low-income mothers improved insurance coverage before and during pregnancy and receipt of early prenatal care. By using birth certificate data, 2 recent studies found that the Provision was associated with increased private insurance coverage at delivery, receipt of early prenatal care, and a reduction in preterm births.9,12
Using data from the Pregnancy Risk Assessment Monitoring System (PRAMS), this study builds upon previous studies9,10 by examining the association of the Provision with insurance coverage before and during pregnancy, and at delivery, in addition to early prenatal care, postpartum visits, and postpartum contraceptive use.
METHODS
Data
We examined data from 2009 to 2013 from PRAMS. PRAMS is a state (or jurisdiction), population-based, surveillance system conducted by the Centers for Disease Control and Prevention and State Health Departments to monitor maternal behaviors and experiences that occur before, during, and shortly after pregnancy among women with a recent live birth.17 The PRAMS sample is randomly drawn from birth certificate records, and women are contacted 2–6 months after delivery. Self-reported survey data are linked to birth certificate data and weighted to be state representative.17
Study Population
We restricted analyses to 16 states that had 5 years of data available from 2009 to 2013, met response rate thresholds for data release for all 5 years, and approved the data release of maternal age as a continuous variable (Appendix 1, Supplemental Digital Content 1, http://links.lww.com/MLR/B665). The study population consisted of 44,990 women, including 22,599 women aged 19–25 years (treatment group) and 22,361 women aged 27–31 years (control group). We excluded 26-year-old women, as in previous studies,6,9 because they could belong to either group depending on their birth date and their plan’s coverage period for that year.
Outcome Variables
Primary outcomes were primary insurance coverage (private, Medicaid, and uninsured) in the month before pregnancy, during pregnancy (insurance coverage for prenatal care), and at delivery (see Table 1 for detailed definition).
TABLE 1.
Characteristics of the Treatment Group and the Control Group Before and After Implementation of the ACA-dependent Coverage Provision, Pregnancy Risk Assessment Monitoring System, 2009–2013†
| 19–25-y-old Women (Treatment Group) | 27–31-y-old Women (Control Group) | |||||
|---|---|---|---|---|---|---|
| Characteristics (%) | Pre-Provision (N = 12,219)& |
Post-Provision (N = 10,380) |
P | Pre-Provision (N = 11,510)& |
Post-Provision (N = 10,851) |
P |
| Race or ethnicity | ||||||
| Non-Hispanic white | 58.1 (56.7–59.6) | 58.7 (57.1–60.2) | 68.3 (67–69.6) | 68.7 (67.4–69.9) | ||
| Non-Hispanic black | 18.8 (17.5–20.1) | 17.3 (16–18.6) | 10.5 (9.5–11.5) | 10.4 (9.5–11.4) | ||
| Hispanic | 17 (16–18.1) | 17.1 (16–18.2) | 13.3 (12.4–14.3) | 12.1 (11.2–13) | ||
| Asian/Alaska native | 1.5 (1.3–1.7) | 1.3 (1–1.5) | * | 0.8 (0.6–1) | 0.6 (0.5–0.8) | * |
| Other | 4.5 (4–5.1) | 5.6 (5–6.2) | ** | 7.1 (6.4–7.7) | 8.2 (7.5–8.9) | ** |
| Educational level | ||||||
| High school and under | 20 (18.8–21.2) | 17.3 (16.1–18.5) | * | 10.1 (9.2–11.1) | 8.3 (7.5–9.1) | ** |
| High school | 39.3 (37.9–40.8) | 37.2 (35.7–38.7) | *** | 19.1 (18–20.2) | 16.8 (15.7–17.9) | |
| College and post college | 40.6 (39.2-42) | 45.5 (44–47) | 70.8 (69.5–72.1) | 74.9 (73.6–76.1) | ||
| Married | 40.7 (39.3–42) | 40.6 (39.1–42) | 77.6 (76.4–78.9) | 76 (74.7–77.2) | ||
| Multiple births | 54 (52.6–55.5) | 54.6 (53.1–56.2) | *** | 35.9 (34.6–37.1) | 37.4 (36.1–38.7) | |
| Birth in a state with previous mandate | 83.3 (82.6–83.9) | 86.1 (85.4–86.9) | 86.8 (86.2–87.4) | 88.6 (88–89.2) | ||
| Pregnancy intended‡ | 41.6 (40.2–43) | 40.9 (39.4–42.4) | *** | 69 (67.7–70.3) | 65.3 (63.9–66.6) | |
| State unemployment rate | 8.8 (8.8–8.8) | 7.4 (7.4–7.5) | *** | 8.8 (8.7-8.8) | 7.4 (7.4-7.4) | |
| State per capita income($) | 38703 (38595-38,810) | 43329 (43,205–43,453) | 39336 (39,233–39,439) | 43960 (43,850–44,070) | ||
All the results were weighted accounting for the complex survey design of PRAMS.
The following states were included in the analysis: Colorado, Delaware, Georgia, Illinois, Maryland, Maine, Minnesota, Missouri, Nebraska, Oklahoma, Oregon, Pennsylvania, Utah, Vermont, Washington, and Wyoming.
Pregnancy intention was assessed using the following question, “Thinking back to just before you got pregnant with your new baby, how did you feel about becoming pregnant?” Women who answered that they wanted their pregnancy “sooner” or “then” were classified as having an intended pregnancy, and those who answered “later,” “did not want at any time in the future,” or “I wasn’t sure what I wanted” were classified as having an unintended pregnancy.
ACA indicates Affordable Care Act; PRAMS, Pregnancy Risk Assessment Monitoring System.
P < 0.001, comparison between the treatment and control groups in the pre-Provision period except for state unemployment rate.
P < 0.05.
P < 0.01.
P < 0.001, comparison for pre- and post-Provision period within the treatment and control groups.
Secondary outcomes included whether women received timely prenatal care (defined as initiation within the first trimester), a postpartum check-up after delivery, and used any contraception postpartum, as indicators of recommended prenatal and postpartum preventive services.18-20
Statistical Analysis
We applied a difference-in-difference (DD) model to examine the change in outcomes before and after the Provision in the treatment compared with the control group.21 We calculated last menstrual period to represent the index date for the policy indicator (before versus after the Provision) by subtracting the gestational age from the delivery date. We retained this policy variable for all outcomes. Additional sensitivity analyses were conducted by using delivery date as the index date. We intentionally excluded observations from women whose last menstrual period was from March 1 to December 31, 2010, as the “wash-out” period to exclude the ambiguity during the implementation period of the Provision as in the previous studies.6,9
Multivariate ordinary least squares regression5,6 was used to calculate the DD estimates, controlling for maternal race or ethnicity, education level, marital status, number of previous live births, whether the pregnancy was unintended (mistimed, unwanted, or unsure), whether the delivery occurred in a state mandated to expand family coverage to young adults,22 temporal trends, and a state fixed effect. We did not control for family household income given 30% of data were missing and the potential measurement error as noted in a previous study.5 However, we did conduct 2 sensitivity analyses, one using imputed income and another including only observations without missing income.
We conducted subgroup analyses by marital status, education, race or ethnicity, pregnancy intention, and previous state mandate status as these factors may respond to the Provision differently.5-7 Lastly, we conducted placebo tests to assess whether the effects detected in the DD model were attributable to chance, tested the prepolicy parallel trend assumption by creating an interaction term between treatment group and time trend indicator using data from the prepolicy period, and further limited the age of the treatment group to 23–25 years and the control group to 27–29 years to control for different labor market changes among different age groups, as suggested in a previous study.6 All analyses were conducted in SAS version 9.4 and accounted for the complex survey design of PRAMS.
RESULTS
Study Population
The characteristics of women in the treatment and comparison groups before versus after passage of the Provision were generally similar, although there were some statistically significant differences (Table 1). Before the Provision, the treatment group had a higher proportion of women who were non-Hispanic black, Hispanic, less educated, unmarried, and had multiple births, and more unintended pregnancies than the control group.
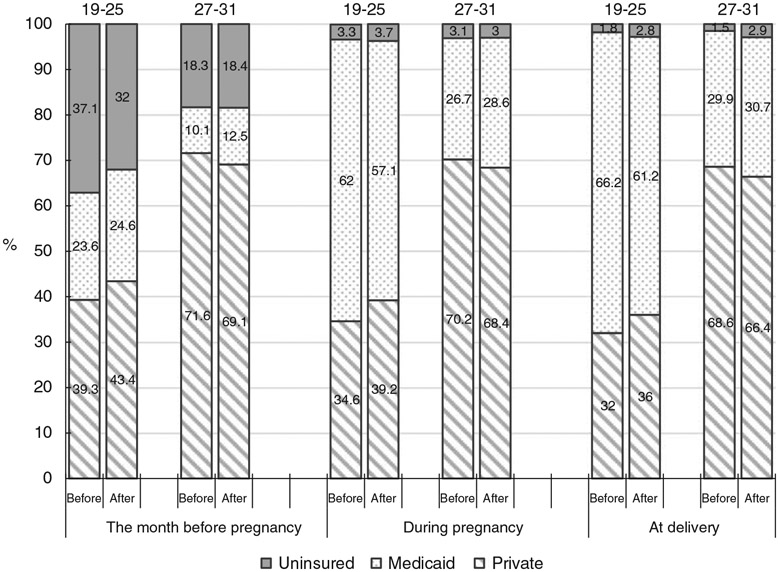
Insurance Coverage
Before the Provision, the rate of being uninsured and type of coverage differed between the treatment and control groups (Fig. 1). In the month before pregnancy, compared with the control group, a higher percentage of women in the treatment group were uninsured (37.1% vs. 18.3%), whereas a lower percentage had private insurance coverage (39.3% vs. 71.6%). During pregnancy and at delivery, the uninsured rates in both groups were <4%, although the treatment group had a lower percentage with private insurance coverage (34.6% vs. 70.2% during pregnancy and 32.0% vs. 68.6% at delivery). The hypothesis on the pre-Provision parallel trends in the treatment and control groups could not be rejected at 0.05 level (most P-values > 0.40) for all outcomes examined (Appendix Table 2, Supplemental Digital Content 3, http://links.lww.com/MLR/B667), thus supporting the appropriateness of the control group.
FIGURE 1.
Insurance coverage and type the month before pregnancy, during pregnancy, and at delivery, among women aged 19–25 and 27–31 years, before and after the Affordable Care Act provision was enacted.
After the Provision, in the month before pregnancy, among the treatment group, there was a decline in the rate of being uninsured concomitant with an increase in private insurance coverage. Conversely, among the control group, the uninsured rate did not change (Fig. 1). During pregnancy, the percentage of women with private insurance coverage increased, and the percentage of Medicaid coverage decreased among the treatment group, whereas a change in the opposite direction was observed in the control group. Changes in insurance coverage at delivery were similar to the pattern observed during pregnancy (Fig. 1).
Adjusted DD estimates (Table 2) show that after the Provision was implemented, in the treatment group, there was a decrease in the probability being uninsured (−4.7 percentage points, P < 0.001) and increase in the probability of having private insurance (+5.9 percentage points, P < 0.001) in the month before pregnancy relative to the control group. During pregnancy there was an increase with private insurance coverage in the treatment group (+5.4 percentage points, P < 0.001) and decrease in Medicaid coverage (−5.9 percentage points, P < 0.001), relative to the control group. DD estimates for coverage at delivery were similar to those during pregnancy.
TABLE 2.
Estimated Change Before and After Implementation of the ACA-dependent Coverage Provision in the Treatment Group and Control Group, Pregnancy Risk Assessment Monitoring System, 2009–2013
| Outcome Measure (Percentage Points) |
19–25-y-old Unadjusted Difference (95% CI) |
27–31-y-old Unadjusted Difference (95% CI) |
Unadjusted DD Estimate (95% CI) |
Adjusted DD Estimate (95% CI) |
|---|---|---|---|---|
| Insurance coverage the month before pregnancy | ||||
| Medicaid | 1 (−0.9 to 2.8) | 2.4 (1.1 to 3.7)*** | −1.4 (−3.7 to 0.8) | −1.1 (−3.5 to 1.2) |
| Private insurance | 4.2 (2.1–6.2)*** | −2.5 (−4.3 to −0.6)** | 6.6 (3.8–9.4)*** | 5.9 (4–7.8)*** |
| No insurance | −5.1 (−7.2 to −3.1)*** | 0.1 (−1.5 to 1.7) | −5.2 (−7.8 to −2.6)*** | −4.7 (−7.4 to −2.1)*** |
| Insurance coverage during pregnancy | ||||
| Medicaid | −4.9 (−7 to −2.9)*** | 1.9 (0.1 to 3.7)* | −6.8 (−9.6 to −4.1)*** | −5.9 (−8.9 to −2.8)*** |
| Private insurance | 4.5 (2.5 to 6.5)*** | −1.8 (−3.7 to 0.1) | 6.3 (3.5–9.1)*** | 5.4 (3.2–7.6)*** |
| No insurance | 0.4 (−0.4 to 1.3) | −0.1 (−0.9 to 0.7) | 0.5 (−0.7 to 1.7) | 0.5 (−0.9 to 1.8) |
| Insurance coverage at delivery | ||||
| Medicaid | −5 (−7 to −3)*** | 0.8 (−1 to 2.7) | −5.9 (−8.6 to −3.1) | −4.9 (−7.7 to −2)*** |
| Private insurance | 4 (2–6)*** | −2.2 (−4.1 to −0.3)* | 6.2 (3.4–8.9)*** | 5.2 (2.5–7.9)*** |
| No insurance | 1 (0.3–1.7)** | 1.3 (0.7–2)*** | −0.3 (−1.3 to 0.6) | −0.3 (−1.1 to 0.4) |
| Prenatal and postpartum care | ||||
| Receiving timely prenatal care | 5.3 (3.5–7.1)*** | 1.2 (0–2.5) | 4.1 (1.9–6.2)*** | 3.6 (1.4–5.9)** |
| Receiving postpartum check-up | 0.2 (−1.9 to 2.2) | 0.6 (−1.1 to 2.2) | −0.4 (−3 to 2.2) | −0.8 (−2.9 to 1.3) |
| Use of any postpartum contraception | −2.8 (−4.3 to −1.3)*** | −2.7 (−4.1 to −1.3)*** | −0.1 (−2.2 to 2) | −0.1 (−2 to 1.7) |
Equation: Yit = β0+β1×treatment group indicator+β2×postpolicy indicator+β3×treatment group indicator×postpolicy indicator+β×Xs. β3 is the adjusted DD estimate. Xs are the covariant matrix.
Pregnant women who reported that they were enrolled in Medicaid or selected a state-named Medicaid program were categorized in the Medicaid group. Pregnant women who reported private insurance coverage alone or in combination with any other kind of insurance, (eg, TRICARE or other military insurance) were included with the private insurance group. Pregnant women who reported having no insurance or exclusively reporting Indian Health Services were included in the uninsured group similar to the classification used by the National Health Interview Survey.
ACA indicates Affordable Care Act; CI, confidence interval; DD, difference-in-difference.
P < 0.05.
P < 0.01.
P < 0.001.
Prenatal Care
Receipt of timely prenatal care increased in the treatment group by 5.3 percentage points from 76.6% during the pre-Provision period to 81.9% during the post-Provision period (P < 0.001), but did not change significantly in the control group (from 88.6% to 89.8%, P = 0.07) (Table 2). Relative to the control group, there was a 3.6 percentage point (adjusted P < 0.001) increase in probability of receiving timely prenatal care for the treatment group after the implementation of the Provision (Table 2).
Postpartum Services
Most women in the treatment (89.4%) and control groups (92.8%) received postpartum check-ups during the pre-Provision period. There was no significant change in either group in the post-Provision period compared with the pre-Provision period. Likewise, 87.0% of women in the treatment group and 86.7% of women in the control group were reported to be using contraception postpartum during the pre-Provision period, and the rate decreased during the post-Provision period in both groups. The DD estimates for both outcomes were close to 0 and not statistically significant (Table 2).
Subgroup Analysis
The DD estimates did not differ by status of previous state mandates and pregnancy intention (data not shown). DD estimates among those who were non-Hispanic white and had at least some college education generally mirrored the main analysis, whereas no changes in outcomes were observed among women who were Hispanic or with less than a high school education. Among unmarried women, the Provision was associated with significant decreases in Medicaid coverage and increases in private insurance both before and during pregnancy, but was only associated with a reduction in the likelihood of being uninsured before pregnancy among married women (Appendix Table 1, Supplemental Digital Content 2, http://links.lww.com/MLR/B666).
Sensitivity Analyses
Placebo tests were negative across all outcomes (Appendix Table 2, Supplemental Digital Content 3, http://links.lww.com/MLR/B667). In general, results of sensitivity analyses were similar to the base-case analysis (Appendix Table 3, Supplemental Digital Content 4, http://links.lww.com/MLR/B668).
CONCLUSIONS
In this analysis of women with recent live births in 16 US states, after the Provision was enacted in 2010, we found that, among those aged 19–25 years, there was a decrease in being uninsured, an increase in having private insurance coverage in the month before pregnancy, a shift from Medicaid to private insurance during pregnancy, and an increase in receipt of timely prenatal care, as compared to those aged 27–31 years who were not affected by the Provision. The findings shed light on the effectiveness of insurance expansion policies to improve insurance coverage and receipt of preventive care services among women with a recent live birth.
Previous studies effect of the Provision among pregnant women have only focused on insurance coverage at delivery.9,10 However, studies have shown that insurance coverage status changes for many women around the time of pregnancy,11,12 and both the type and timing of coverage predicted receipt of timely prenatal care. Women with private insurance coverage before pregnancy, or who obtain insurance in the first trimester, were more likely to initiate timely prenatal care.11 Our analysis of PRAMS data found a 4.4 percentage point reduction in the prevalence of being uninsured before pregnancy mirrored by a 5.5 percentage point increase in private insurance; these findings are consistent with previous studies on the Provision among young adults, both in direction and in magnitude.3-5 We found the Provision was positively associated with receiving timely prenatal care overall. We also found a substitution effect between private insurance and Medicaid coverage during pregnancy. The magnitude of the effects on both outcomes was higher in our study compared with previous studies,9,10 which might be caused by the use of a different study population and data source. In subgroup analyses, findings mirrored overall results among non-Hispanic white women and those with at least some college education. Consistent with previous studies,5,9,10 the Provision had larger effects on increasing private insurance coverage among unmarried women than married women.
We did not find an effect of the Provision on the receipt of a postpartum check-up or postpartum contraception use, which might be the result of a ceiling effect. In addition, the postpartum visit is typically covered by insurance at time of delivery, and even before the Provision, the overwhelming majority of women had insurance coverage at delivery.8
This analysis has a few limitations. First, only 16 states were included in the analysis; thus, the findings may not be generalizable nationally. Second, PRAMS data are self-reported and collected several months after delivery, and may be subject to recall bias. However, studies have shown high reliability of PRAMS data for multiple indicators, especially insurance measures.23,24 Lastly, as with any DD approach, other underlying factors, such as competing interventions or different ongoing trends in control groups, may have positively or negatively affected our results. However, we are unaware of other large scale policy changes on insurance coverage for these age groups during the study period, and our data showed that the treatment and control groups had similar trends in insurance coverage before the policy change.
Despite these limitations, using a large, representative sample of women with a recent live birth we found that the ACA-dependent coverage Provision was associated with increases in private insurance coverage before and during pregnancy, and at delivery, and improved timeliness of prenatal care for young women with a recent live birth aged 19–25 years. Future studies could be conducted to estimate the potential effect of the Provision to improve insurance continuity around pregnancy and maternal and infant health outcomes by providing opportunities to manage existing conditions before pregnancy and ensuring early entry into prenatal care.
Supplementary Material
ACKNOWLEDGMENTS
We thank Dr Scott Grosse at the Center for Birth Defects and Developmental Disabilities and Dr Jared Fox at the National Center for Environmental Health for their valuable comments on the manuscript.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention.
Presented at AcademyHealth Annual Research Meeting, June 25–27, 2017, New Orleans, LA and APHA Annual Scientific Meeting, November 4–8, 2017, Atlanta, GA.
The authors declare no conflict of interest.
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website, www.lww-medicalcare.com.
REFERENCES
- 1.National Conference of State Legislatures. Dependent health coverage and age for healthcare benefits. 2016. Available at: http://www.ncsl.org/research/health/dependent-health-coverage-state-implementation.aspx. Accessed April 17, 2018.
- 2.U.S. Department of Health and Human Services. Young adult coverage. 2017. Available at: https://www.hhs.gov/healthcare/about-the-aca/young-adult-coverage/index.html. Accessed April 10, 2018.
- 3.Kotagal M, Carle AC, Kessler LG, et al. Limited impact on health and access to care for 19- to 25-year-olds following the Patient Protection and Affordable Care Act. JAMA Pediatr. 2014;168:1023–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lau JS, Adams SH, Park MJ, et al. Improvement in preventive care of young adults after the affordable care act: the affordable care act is helping. JAMA Pediatr. 2014;168:1101–1106. [DOI] [PubMed] [Google Scholar]
- 5.Sommers BD, Buchmueller T, Decker SL, et al. The Affordable Care Act has led to significant gains in health insurance and access to care for young adults. Health Aff (Project Hope). 2013;32:165–174. [DOI] [PubMed] [Google Scholar]
- 6.Barbaresco S, Courtemanche CJ, Qi Y. Impacts of the Affordable Care Act dependent coverage provision on health-related outcomes of young adults. J Health Econ. 2015;40:54–68. [DOI] [PubMed] [Google Scholar]
- 7.Cantor JC, Monheit AC, DeLia D, et al. Early impact of the Affordable Care Act on health insurance coverage of young adults. Health Serv Res. 2012;47:1773–1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.D’Angelo DV, Le B, O’Neil ME, et al. Patterns of health insurance coverage around the time of pregnancy among women with live-born infants—Pregnancy Risk Assessment Monitoring System, 29 States, 2009. MMWR Surveill Summ. 2015;64:1–19. [PMC free article] [PubMed] [Google Scholar]
- 9.Akosa Antwi Y, Ma J, Simon K, et al. Dependent coverage under the ACA and Medicaid coverage for Childbirth. N Engl J Med. 2016;374:194–196. [DOI] [PubMed] [Google Scholar]
- 10.Daw JR, Sommers BD. Association of the Affordable Care Act dependent coverage provision with prenatal care use and birth outcomes. JAMA. 2018;319:579–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Egerter S, Braveman P, Marchi K. Timing of insurance coverage and use of prenatal care among low-income women. Am J Public Health. 2002;92: 423–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Daw JR, Hatfield LA, Swartz K, et al. Women In The United States experience high rates of coverage ‘churn’ in months before and after childbirth. Health Aff (Project Hope). 2017;36:598–606. [DOI] [PubMed] [Google Scholar]
- 13.Oberg CN, Lia-Hoagberg B, Hodkinson E, et al. Prenatal care comparisons among privately insured, uninsured, and Medicaid-enrolled women. Public Health Rep. 1990;105:533–535. [PMC free article] [PubMed] [Google Scholar]
- 14.Oberg CN, Lia-Hoagberg B, Skovholt C, et al. Prenatal care use and health insurance status. J Health Care Poor Underserved. 1991;2:270–292. [DOI] [PubMed] [Google Scholar]
- 15.Stulberg DB, Cain L, Hasham Dahlquist I, et al. Pre-pregnancy and early prenatal care are associated with lower risk of ectopic pregnancy complications in the medicaid population: 2004–08. Paediatr Perinat Epidemiol. 2017;31:4–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson K, Posner SF, Biermann J, et al. Recommendations to improve preconception health and health care—United States. A report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR Recommendations Reports. 2006;55:1–23. [PubMed] [Google Scholar]
- 17.Shulman HB, D’Angelo D, Harrison L, et al. The Pregnancy Risk Assessment Monitoring System (PRAMS): Overview of Design and Methodology. AM J Public Health. 2018;108:1305–1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Health Resources and Services Administration (HRSA). Prenatal—first trimester care access. 2011. Available at: https://www.hrsa.gov/sites/default/files/quality/toolbox/pdfs/prenatalfirsttrimestercareaccess.pdf. Accessed October 4, 2018.
- 19.Johnson K, Posner SF, Biermann J, et al. Recommendations to improve preconception health and health care. MMWR Recomm Rep. 2006; 55:1–23. [PubMed] [Google Scholar]
- 20.Gavin L, Moskosky S, Carter M , et al. Providing quality family planning services: recommendations from Centers for Disease Control and Prevention and the US Office of Population Affairs (QFP). MMWR Recomm Rep. 2014;63:1–29. [PubMed] [Google Scholar]
- 21.Craig P, Cooper C, Gunnell D, et al. Using natural experiments to evaluate population health interventions: new Medical Research Council guidance. J Epidemiol Community Health. 2012;66:1182–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blum AB, Kleinman LC, Starfield B, et al. Impact of state laws that extend eligibility for parents’ health insurance coverage to young adults. Pediatrics. 2012;129:426–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahluwalia IB, Helms K, Morrow B. Assessing the validity and reliability of three indicators self-reported on the pregnancy risk assessment monitoring system survey. Public Health Rep. 2013;128:527–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shulman HB, Gilbert BC, Msphbrenda CG, et al. The Pregnancy Risk Assessment Monitoring System (PRAMS): current methods and evaluation of 2001 response rates. Public Health Rep. 2006;121: 74–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.