Abstract
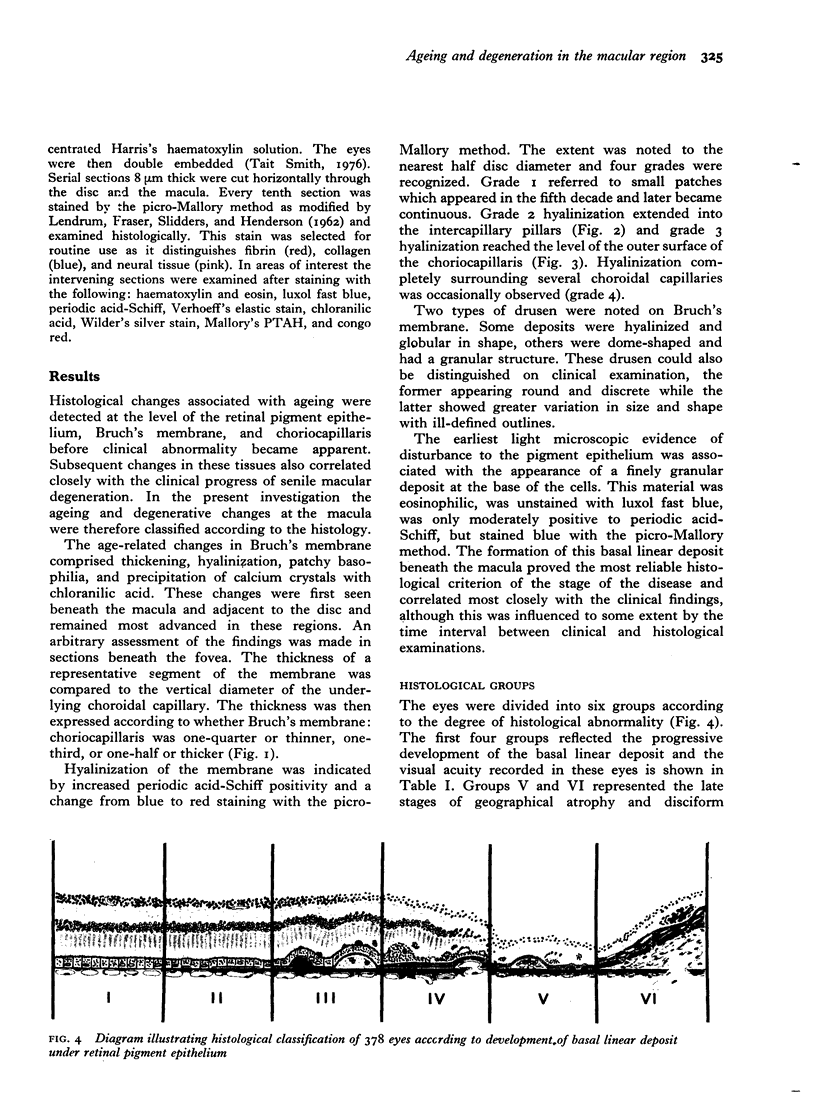
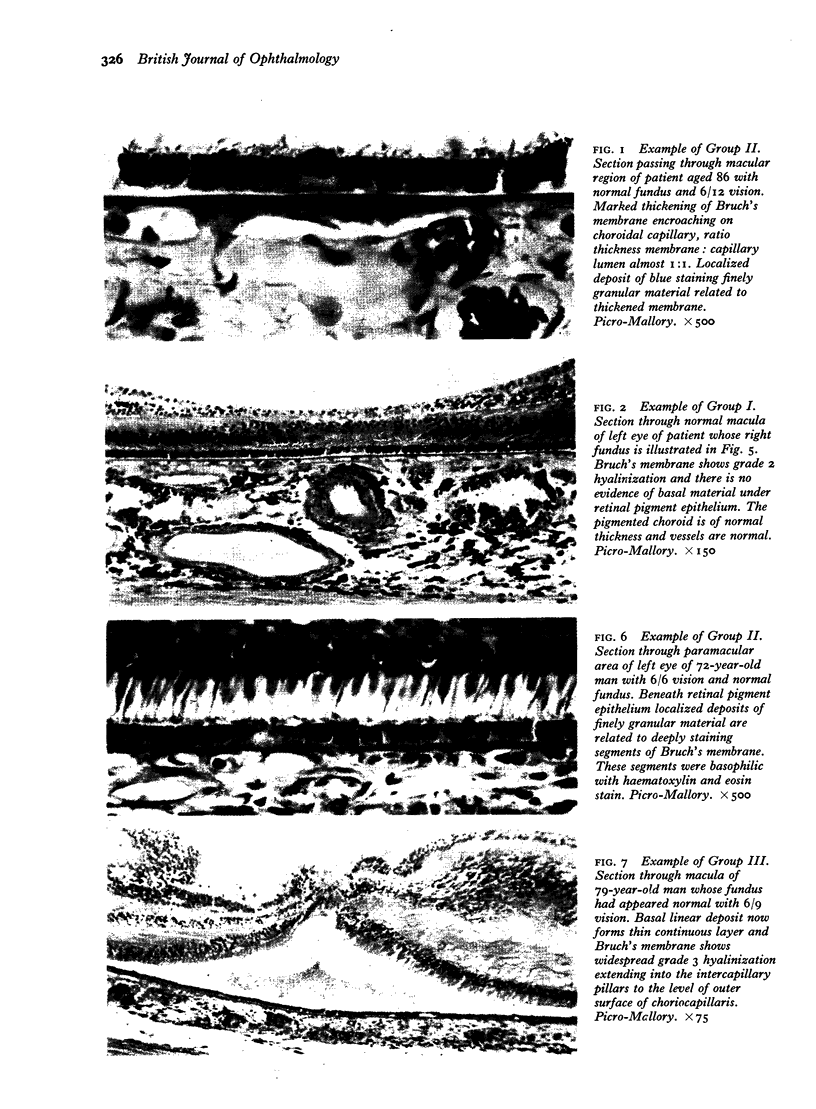
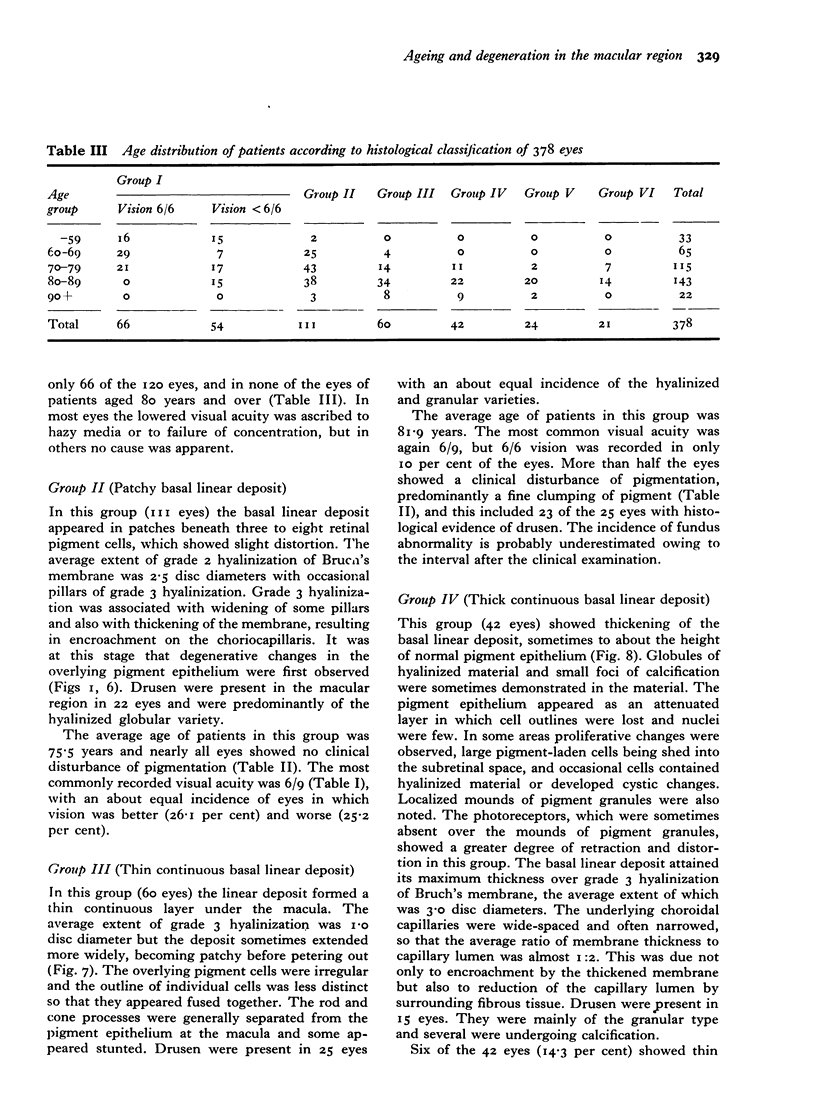
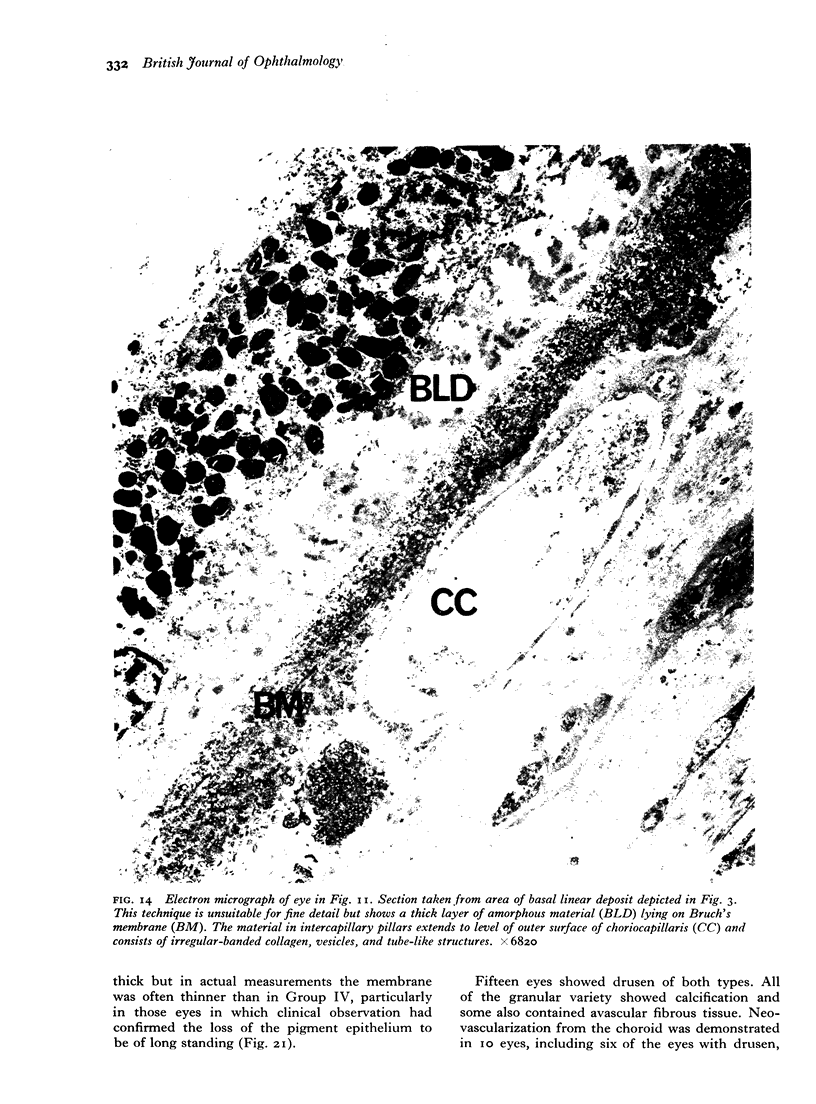
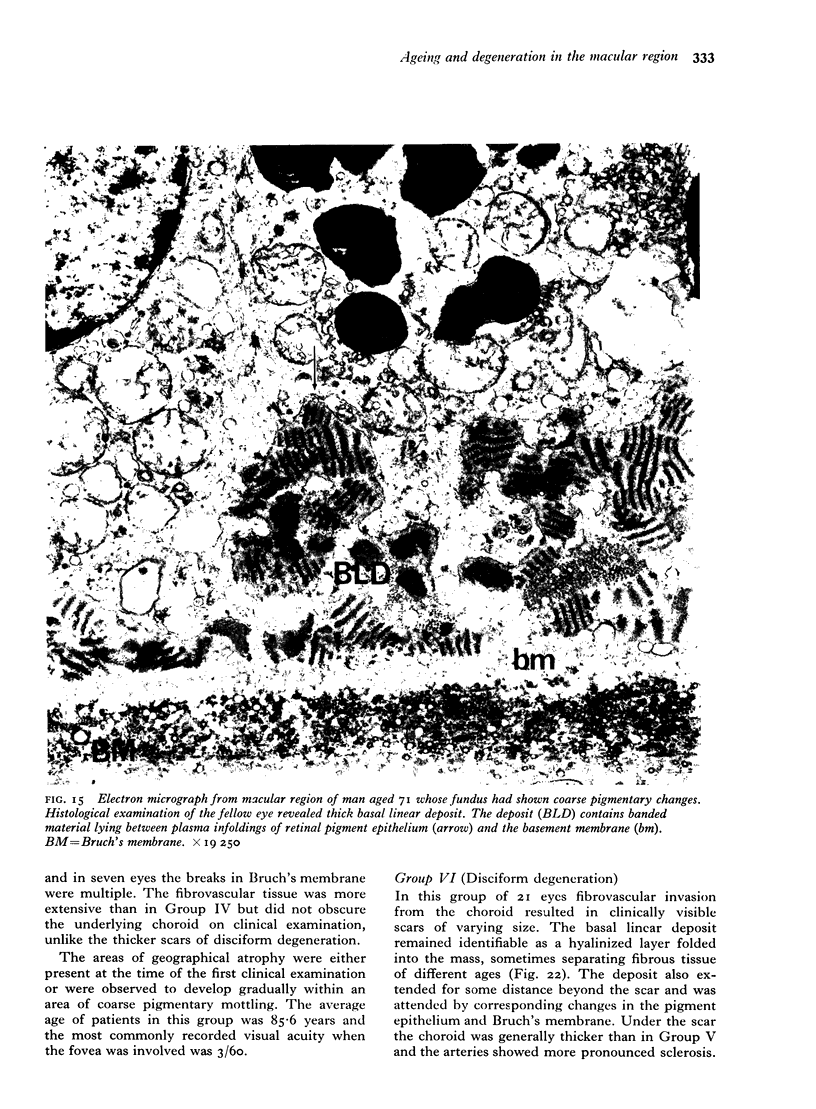
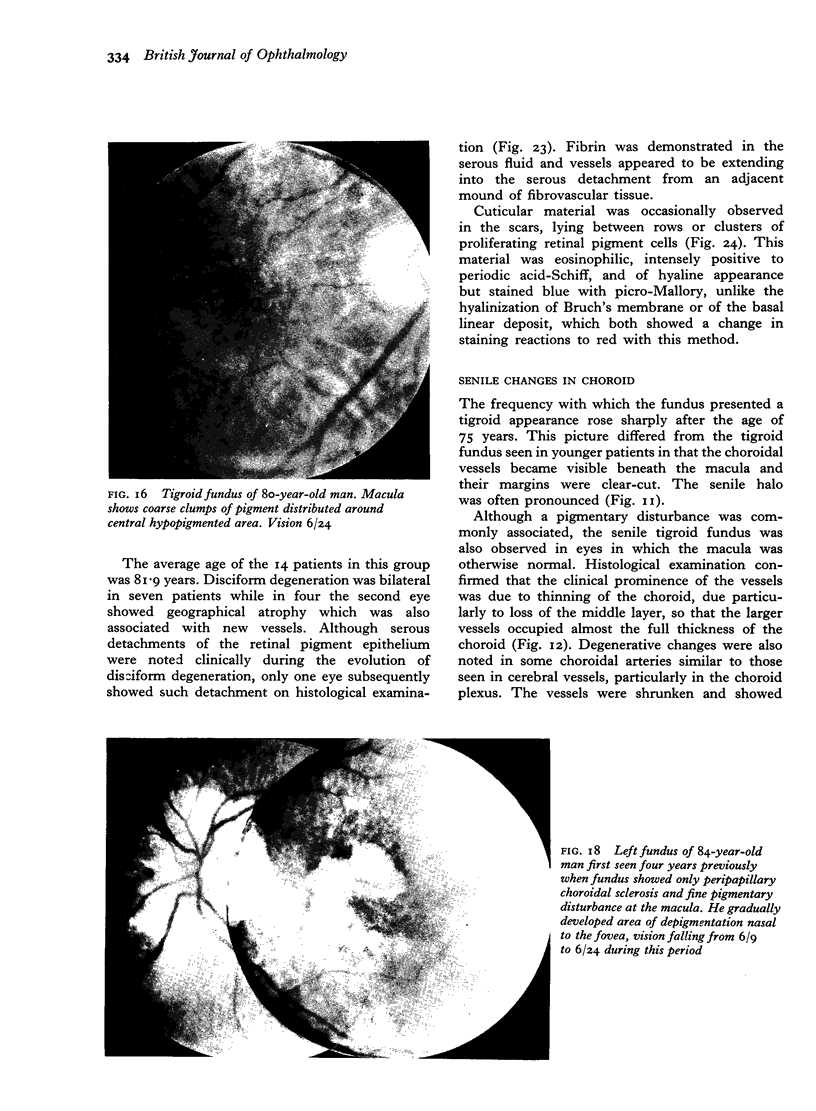
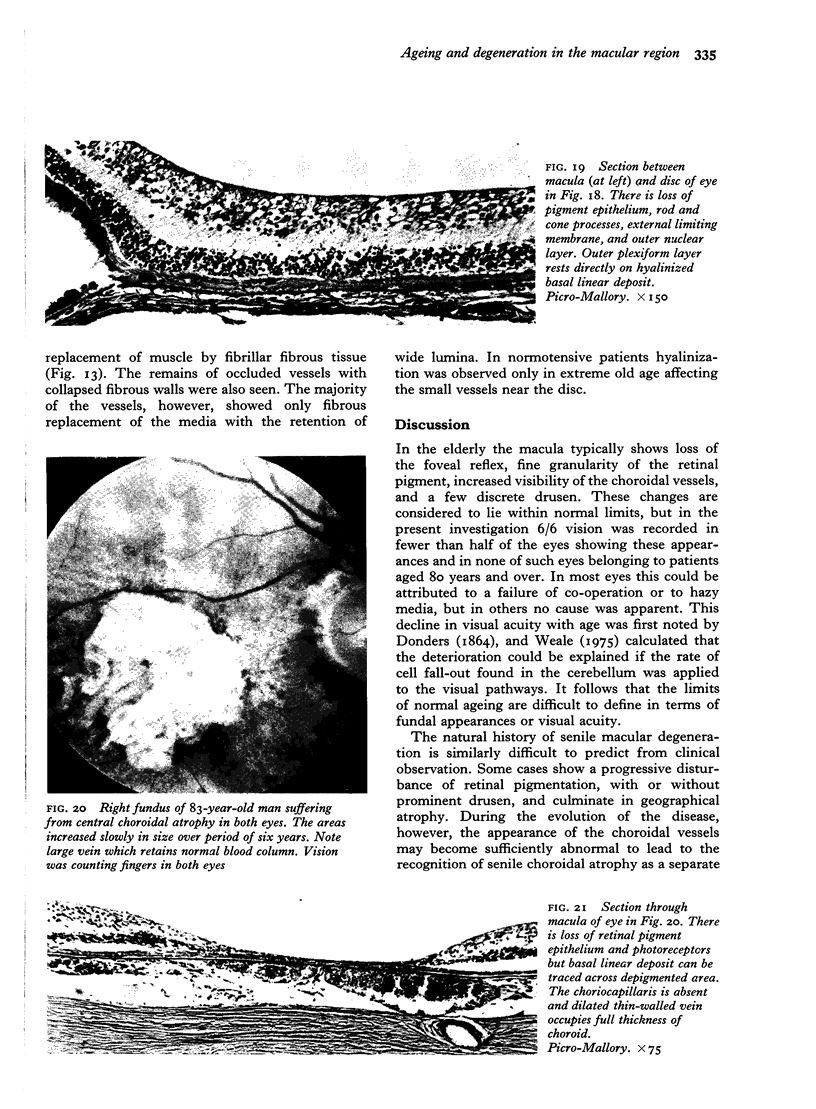
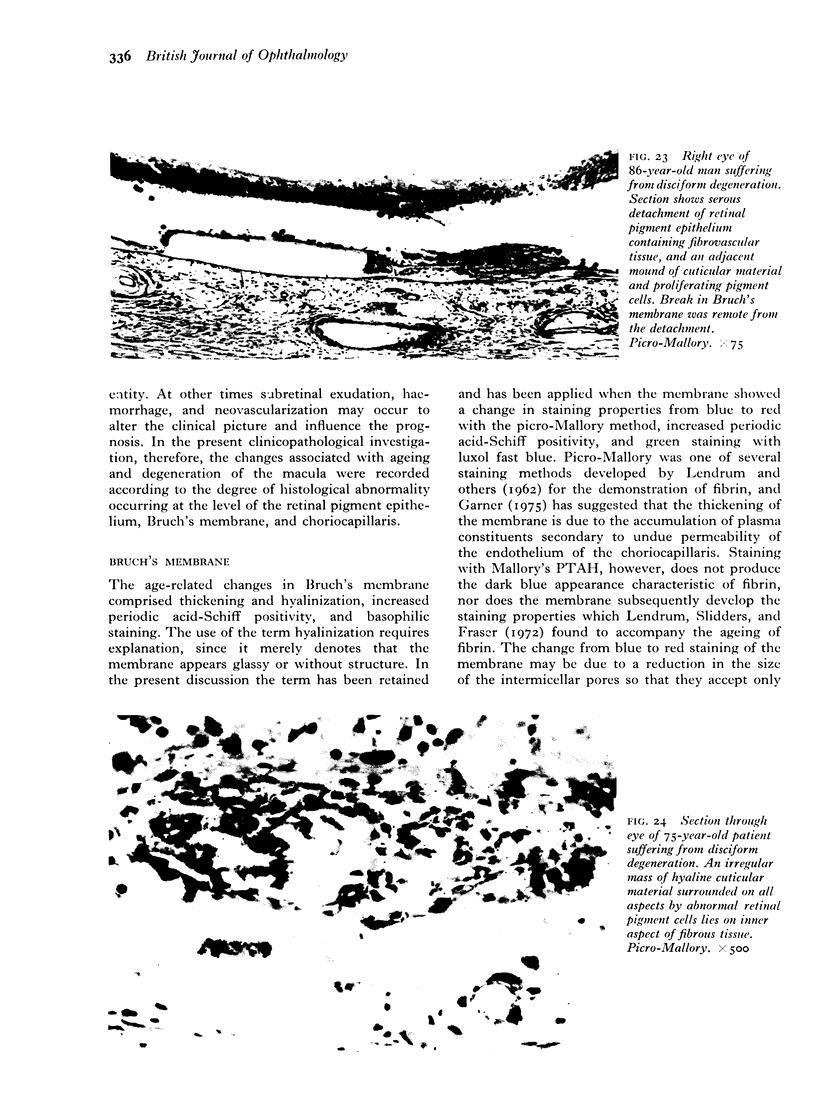
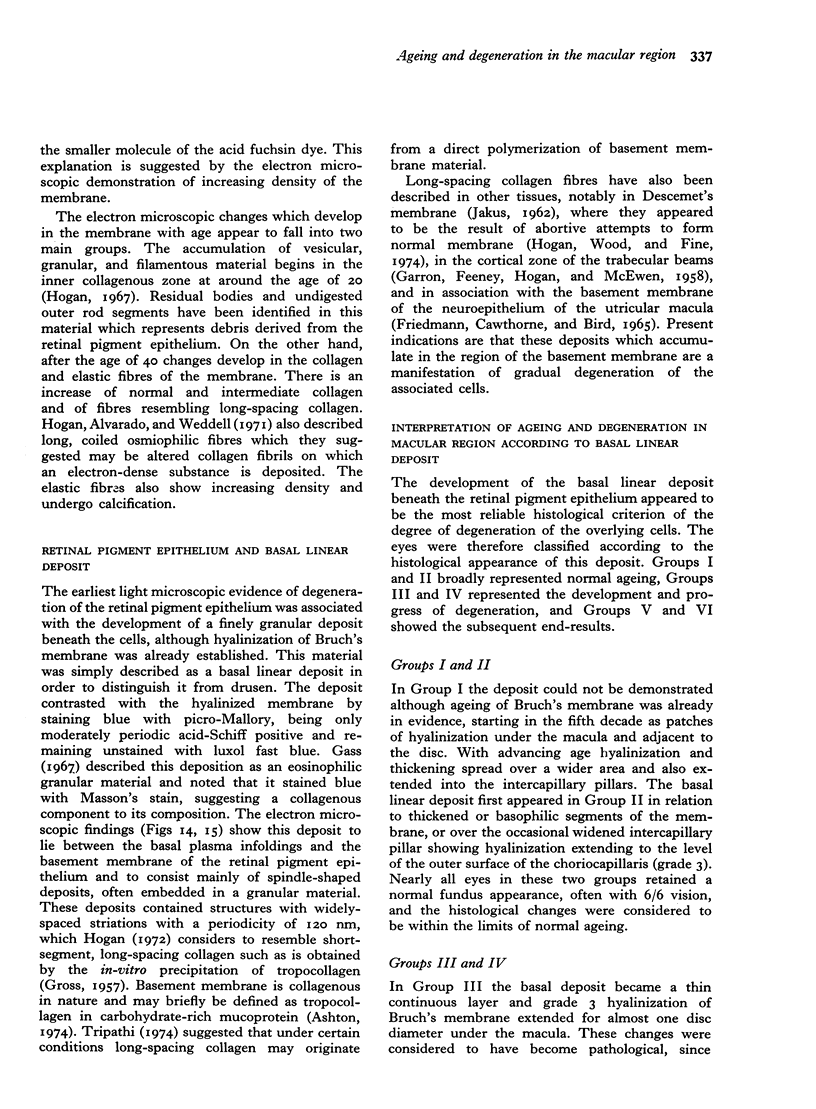
Clinical and pathological examination was performed on 378 eyes from 216 patients aged 43 to 97 years. This series represented eyes in which the fundi were normal or showed various manifestations of senile macular degeneration. The eyes were divided into six groups according to the histological appearance of a linear deposit at the base of the retinal pigment cells. Groups I and II were considered to represent normal ageing, Groups III and IV the progressive development of senile macular degeneration and Groups V and VI the end-results. Group I showed no basal linear deposit. Thickening and hyalinization of Bruch's membrane was noted as early as the fifth decade. Group II showed patchy development of the basal linear deposit in relation to thickened or basophilic segments of Bruch's membrane, or over intercapillary hyalinization extending to the level of the outer surface of the choriocapillaris. Almost all eyes in these two groups retained a normal fundus appearance but visual acuity declined with age even in the absence of other causes. In Group III the basal deposit formed a thin continuous layer associated with moderate degeneration of the retinal pigment epithelium. More than half the eyes had developed a clinical disturbance of pigmentation and in most vision was reduced. Group IV was characterized by thickening of the deposit and more pronounced disturbance of the pigment epithelium. Clinically most eyes showed coarse pigmentary changes and vision was in the order of 6/24. 14-3 per cent of eyes in this group showed early neovascularization from the choroid. In Group V the pigment epithelium disappeared to produce circumscribed areas of depigmentation. The basal linear deposit could be traced throughout the depigmented area in most eyes. Thin fibrovascular sheets were found beneath the pigment epithelium in 41-7 per cent of eyes. Group VI represented disciform degeneration. The basal linear deposit could often be demonstrated as a disrupted hyalinized layer incorporated into the scar. Disciform degeneration was an alternative end-result to geographical atrophy. In each group the clinical and histological findings may be modified by the presence of drusen or by atrophy of the choroid. The basal linear deposit consisted of banded fibres embedded in granular material lying between the plasma infoldings and the basement membrane of the retinal pigment epithelium. This deposit seems to be a manifestation of gradual failure of the pigment epithelium and proved to be the most suitable criterion by which to study the natural history of senile macular degeneration.
Full text
PDF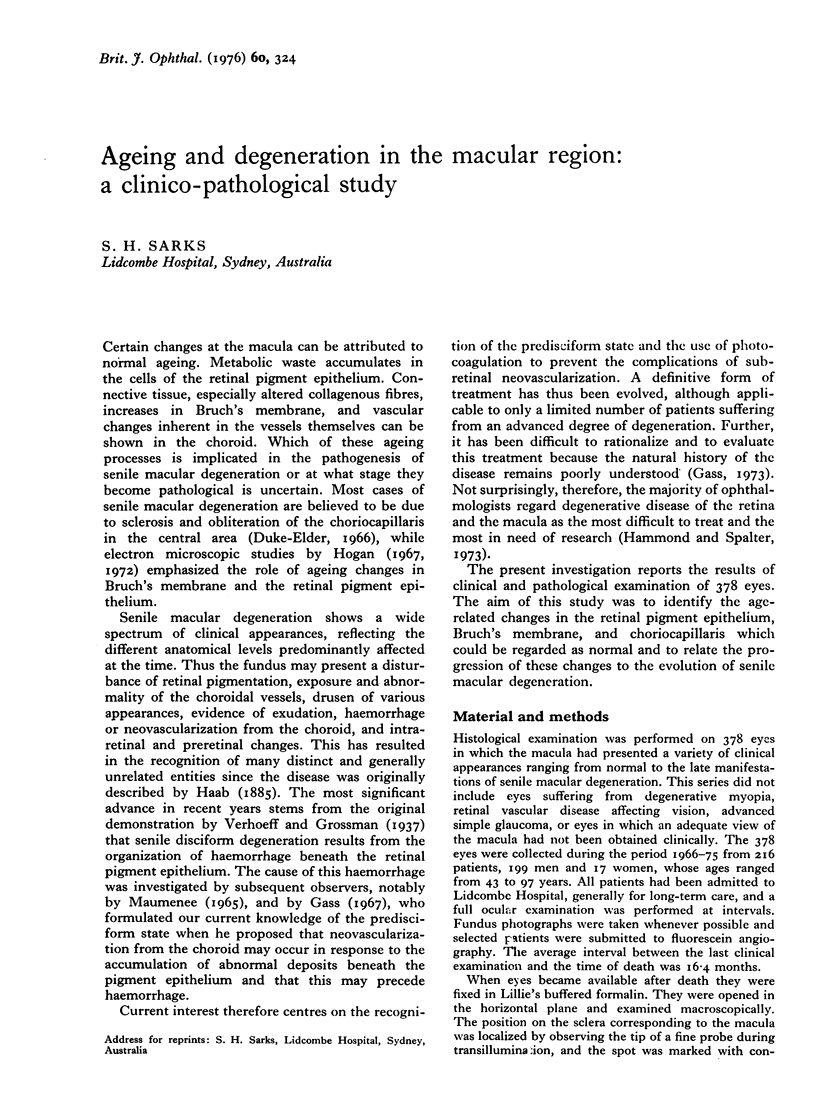
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ASHTON N., SORSBY A. Fundus dystrophy with unusual features; a histological study. Br J Ophthalmol. 1951 Dec;35(12):751–764. doi: 10.1136/bjo.35.12.751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashton N. Vascular basement membrane changes in diabetic retinopathy. Montgomery lecture, 1973. Br J Ophthalmol. 1974 Apr;58(4):344–366. doi: 10.1136/bjo.58.4.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair C. J. Geographic atrophy of the retinal pigment epithelium. A manifestation of senile macular degeneration. Arch Ophthalmol. 1975 Jan;93(1):19–25. doi: 10.1001/archopht.1975.01010020023003. [DOI] [PubMed] [Google Scholar]
- Friedmann I., Cawthorne T., Bird E. S. Broad-banded striated bodies in the sensory epithelium of the human macula and in neurinoma. Nature. 1965 Jul 10;207(993):171–174. doi: 10.1038/207171a0. [DOI] [PubMed] [Google Scholar]
- GARRON L. K., FEENEY M. L., HOGAN M. J., McEWEN W. K. Electron microscopic studies of the human eye. I. Preliminary investigations of the trabeculas. Am J Ophthalmol. 1958 Jul;46(1 Pt 2):27–35. doi: 10.1016/0002-9394(58)90031-x. [DOI] [PubMed] [Google Scholar]
- Green W. R., Gass J. D. Senile disciform degeneration of the macula. Retinal arterialization of the fibrous plaque demonstrated clinically and histopathologically. Arch Ophthalmol. 1971 Nov;86(5):487–494. doi: 10.1001/archopht.1971.01000010489001. [DOI] [PubMed] [Google Scholar]
- Hammond E. C., Spalter H. F. Survey of needs in ophthalmic research and development. Am J Ophthalmol. 1973 Sep;76(3):389–396. doi: 10.1016/0002-9394(73)90496-0. [DOI] [PubMed] [Google Scholar]
- Hogan M. J. Bruch's membrane and disease of the macula. Role of elastic tissue and collagen. Trans Ophthalmol Soc U K. 1967;87:113–161. [PubMed] [Google Scholar]
- Hogan M. J., Wood I., Fine M. Fuchs' endothelial dystrophy of the cornea. 29th Sanford Gifford Memorial lecture. Am J Ophthalmol. 1974 Sep;78(3):363–383. doi: 10.1016/0002-9394(74)90224-4. [DOI] [PubMed] [Google Scholar]
- JAKUS M. A. Further observations on the fine structure of the cornea. Invest Ophthalmol. 1962 Apr;1:202–225. [PubMed] [Google Scholar]
- KLIEN B. A. Macular lesions of vascular origin. Am J Ophthalmol. 1951 Sep;34(9):1279–1289. doi: 10.1016/0002-9394(51)91864-8. [DOI] [PubMed] [Google Scholar]
- Lendrum A. C., Slidders W., Fraser D. S. Renal hyalin. A study of amyloidosis and diabetic fibrinous vasculosis with new staining methods. J Clin Pathol. 1972 May;25(5):373–396. doi: 10.1136/jcp.25.5.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tripathi R. C. Fine structure of mesodermal tissues of the human eye. Trans Ophthalmol Soc U K. 1974 Sep;94(3):663–695. [PubMed] [Google Scholar]
- Weale R. A. Senile changes in visual acuity. Trans Ophthalmol Soc U K. 1975 Apr;95(1):36–38. [PubMed] [Google Scholar]