Abstract
Background
Most studies on minimally invasive pancreatoduodenectomy (MIPD) combine patients with pancreatic and periampullary cancers even though there is substantial heterogeneity between these tumors. Therefore, this study aimed to evaluate the role of MIPD compared to open pancreatoduodenectomy (OPD) in patients with non-pancreatic periampullary cancer (NPPC).
Methods
A systematic review of Pubmed, Embase, and Cochrane databases was performed by two independent reviewers to identify studies comparing MIPD and OPD for NPPC (ampullary, distal cholangio, and duodenal adenocarcinoma) (01/2015–12/2021). Individual patient data were required from all identified studies. Primary outcomes were (90-day) mortality, and major morbidity (Clavien-Dindo 3a-5). Secondary outcomes were postoperative pancreatic fistula (POPF), delayed gastric emptying (DGE), postpancreatectomy hemorrhage (PPH), blood-loss, length of hospital stay (LOS), and overall survival (OS).
Results
Overall, 16 studies with 1949 patients were included, combining 928 patients with ampullary, 526 with distal cholangio, and 461 with duodenal cancer. In total, 902 (46.3%) patients underwent MIPD, and 1047 (53.7%) patients underwent OPD. The rates of 90-day mortality, major morbidity, POPF, DGE, PPH, blood-loss, and length of hospital stay did not differ between MIPD and OPD. Operation time was 67 min longer in the MIPD group (P = 0.009). A decrease in DFS for ampullary (HR 2.27, P = 0.019) and distal cholangio (HR 1.84, P = 0.025) cancer, as well as a decrease in OS for distal cholangio (HR 1.71, P = 0.045) and duodenal cancer (HR 4.59, P < 0.001) was found in the MIPD group.
Conclusions
This individual patient data meta-analysis of MIPD versus OPD in patients with NPPC suggests that MIPD is not inferior in terms of short-term morbidity and mortality. Several major limitations in long-term data highlight a research gap that should be studied in prospective maintained international registries or randomized studies for ampullary, distal cholangio, and duodenum cancer separately.
Protocol registration
PROSPERO (CRD42021277495) on the 25th of October 2021.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00423-023-03047-4.
Keywords: Minimally invasive surgery, Minimally invasive pancreatoduodenectomy, Ampulla of Vater carcinoma, Duodenal adenocarcinoma, Distal cholangiocarcinoma, Individual patient data meta-analysis
Introduction
Periampullary cancer is a widely used term to define a heterogeneous group of neoplasms in the pancreatic head, the ampulla of Vater, distal bile duct, and duodenum [1, 2]. Pancreatic ductal adenocarcinoma (PDAC) is the most frequently diagnosed periampullary cancer and also has the worst prognosis with 5-year overall survival of 5–22% after surgical resection [3–6]. The remaining periampullary tumors are commonly classified into a single category of non-pancreatic periampullary cancer (NPPC) [7]. Despite anatomic similarities, there are fundamental and biological differences between the NPPCs [8–12]. The distinct origin is associated with a variety of reported 5-year survival, ranging between 30 to 70% for ampullary [13–16] cancer, 18 to 40% for distal cholangiocarcinoma [17–20], and 46 to 71% for duodenal cancer [21–24].
After diagnosis with resectable NPPC (ampullary, distal cholangio, or duodenal cancer), the only curative treatment is a pancreatoduodenectomy. In the last decade, minimally invasive pancreatoduodenectomy (MIPD) has been widely implemented, both for PDAC and NPPC [25], and a shift is taking place from traditional open pancreatoduodenectomy (OPD) towards MIPD [26–28]. Some studies have demonstrated potential peri- and postoperative benefits of the MIPD when compared to the traditional OPD, including shorter hospital stay, decreased intraoperative blood-loss, and lower rates of wound infections [29–33]. However, despite the fundamental heterogeneity of the various NPPCs, the majority of the studies on MIPD assessed periampullary lesions as one single entity (Fig. A1, Appendix). This can lead to important disharmony in the compared groups and hence, inaccurate treatment strategies in clinical practice.
The primary aim of the present study was to compare the mortality and major morbidity after MIPD and OPD in patients with NPPC and its subgroups using individual patient-level data from published studies, identified by a systematic literature review. By collecting all relevant evidence on the topic, this study can assist in determining the best surgical strategy and potentially guide clinical decision making in the treatment of ampullary, distal cholangio, and duodenum cancer.
Methods
Design
This study was designed as a systematic review and individual patient data meta-analysis (IPDMA). This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (PRISMA-IPD [34]) and Assessing the Methodological Quality of Systematic Reviews (AMSTAR [35]) guidelines. The protocol was developed before the start of the reviewing process registered in the online openly available PROSPERO registry.
Study identification, search strategy, and selection criteria
All comparative studies (retrospective cohort, prospective cohort, and randomized controlled trial) comparing MIPD with OPD for periampullary tumors were identified using Pubmed, Embase (via Ovid), and Cochrane databases. The keywords “minimally invasive,” “laparoscopic,” “robotic,” “open,” “pancreatoduodenectomy,” and synonyms were used to identify all relevant studies from January 2015 until December 2021 (full search available in the Appendix). Following exclusion of duplicates, two authors (BAU and DHL) independently reviewed the titles, abstracts, and full texts of studies identified by the literature search. Studies reporting a comparison of minimally invasive and open pylorus-resecting or -preserving pancreatoduodenectomy in human subjects for periampullary cancers including ampullary, distal cholangio, duodenal cancer, and written in English were included. Excluded were (1) studies with a non-comparative cohort design (e.g., review articles, case reports, technical procedure reports, pilot trials), (2) studies evaluating different types of pancreatic surgery (e.g., distal/total pancreatectomy), or (3) studies selectively focusing on PDAC or benign indications (e.g., chronic pancreatitis or benign tumors). The search was extended with a manual evaluation of relevant references used in the included articles. Conflicts or concerns were resolved by discussion between the two reviewers and a third reviewer (MAH). After reaching consensus of the included studies, all corresponding authors or principal investigators were contacted with the study protocol describing the objectives and procedures of this IPDMA, and the database used for the selected study was requested.
Inclusion criteria
From the received databases, only the cases with ampullary, distal cholangio, and duodenal cancers (NPPCs) operated with pylorus-preserving pancreatoduodenectomy (Whipple’s procedure) or pylorus-resecting pancreatoduodenectomy were included for analyses. Patients with PDAC, benign neoplasms, hybrid procedures, cases with missing primary outcomes, or operated with other surgical techniques (e.g., total pancreatectomy, duodenum sparing pancreatectomy, ampullectomy) were excluded from final analyses.
Outcomes
The primary outcomes were 90-day mortality and postoperative major morbidity, defined as Clavien-Dindo 3a-5 [36]. Secondary outcomes were operation time (minutes), perioperative estimated blood-loss (ml), postoperative incidence of postoperative pancreatic fistula (POPF), delayed gastric emptying (DGE), postpancreatectomy hemorrhage (PPH), wound infections, and the length of hospital stay (days). Oncological outcomes included R1 resections, disease-free survival (DFS), and overall survival (OS). The 3-year survival and recurrence were reported in the percentage of the patients “at risk” 36 months after surgery.
Subgroup analyses
Using subgroup analyses, MIPD and OPD were compared for ampullary, distal cholangio, and duodenal cancer separately. Other subgroup analyses we considered to be relevant were (1) young versus elderly patients, since perioperative blood-loss and complication rates are known to be higher in elderly patients [37], (2) pylorus-resecting versus pylorus-preserving pancreatoduodenectomy, since pylorus-preserving pancreatoduodenectomy is known to be associated with higher rates of DGE [38], and (3) outcomes between Western (European-USA) centers and Eastern (Asian-Pacific) centers because in Asia–Pacific centers, it is common practice to discharge a patient to their pre-surgical living situation. In European centers, it is more common to discharge a patient to a temporary stay in a rehabilitation center, and in American centers, there is a well-organized home-nursing system in place which could offer postoperative care at home. Since patients must be in a better state of recovery before returning to their previous living situation, the length of hospital stays in different continents could correlate with a different stage of rehabilitation. Additionally, patient population in Asian-Pacific centers are known to have a lower BMI that could be a predictive factor for postoperative complications or survival [39].
Definitions
NPPC is defined as adenocarcinoma arising from the ampulla of Vater, distal bile duct, and periampullary duodenum (second segment), extracted from postoperative pathology report. ASA classification was defined following American Society of Anesthesiologists (ASA) classification [40]. TNM staging was according to the 7th and 8th editions of the American Joint Committee on Cancer (AJCC) [41, 42]. Since N2 stage is only introduced in the 8th edition, the N2 tumors in the 8th edition would have been N1 in the 7th edition. Therefore, N-stage is classified in N0 and N1-2. POPF, DGE, and PPH were defined as ISGPS grade B and C [43–45]. An R1 resection margin is defined as < 1 mm according to the definition of the Royal College of Pathologists [46]. All converted cases were included in the minimally invasive group following the intention to treat principle.
Statistical analyses
Normally distributed variables are reported as means with standard deviation (SD). Non-normally distributed variables are reported as medians with interquartile ranges (IQR). Categorical variables are presented as frequencies and proportions. Categorical data were compared by means of the chi square test, whereas numerical data were compared by the Student t-test for normally distributed data and non-normally distributed data by its non-parametric equivalent the Mann–Whitney U test. Standardized mean differences (SMD) were used to assess balance. An SMD below 0.2 is deemed as optimal balance [47, 48]. The meta-analysis was performed using R (version 3.6.1; the R Foundation for Statistical Computing, Vienna, Austria). Statistical significance was set at P < 0.05, with 95% confidence intervals (CI) shown for all results. A “2-stage” approach was adopted for the IPDMA, as recommended; the IPD within studies generated summary measures, which were combined using standard meta-analytical methods. The fixed-effects model was adopted if heterogeneity was not statistically significant. The random-effects model was used when statistical heterogeneity was identified. The mean difference (MD) in continuous variables was compared using the inverse variance method, and categorical dichotomous variables were assessed using risk differences (RDs) by the inverse variance method. OS was assessed using the hazard ratio (HR) which was calculated using the Cox proportional hazard model. Heterogeneity was assessed using Cochran’s Q test, the observed values of I2 were used to represent the severity of heterogeneity and were interpreted using thresholds that were previously recommended (0–40%: likely minimal; 30–60%: likely moderate; 50–90%: likely substantial; and 75–100%: likely considerable), along with the strength of evidence [49]. Funnel plots were used to explore the presence of publication bias visually, and their symmetry was evaluated by the Egger’s test [50].
Results
Systematic review
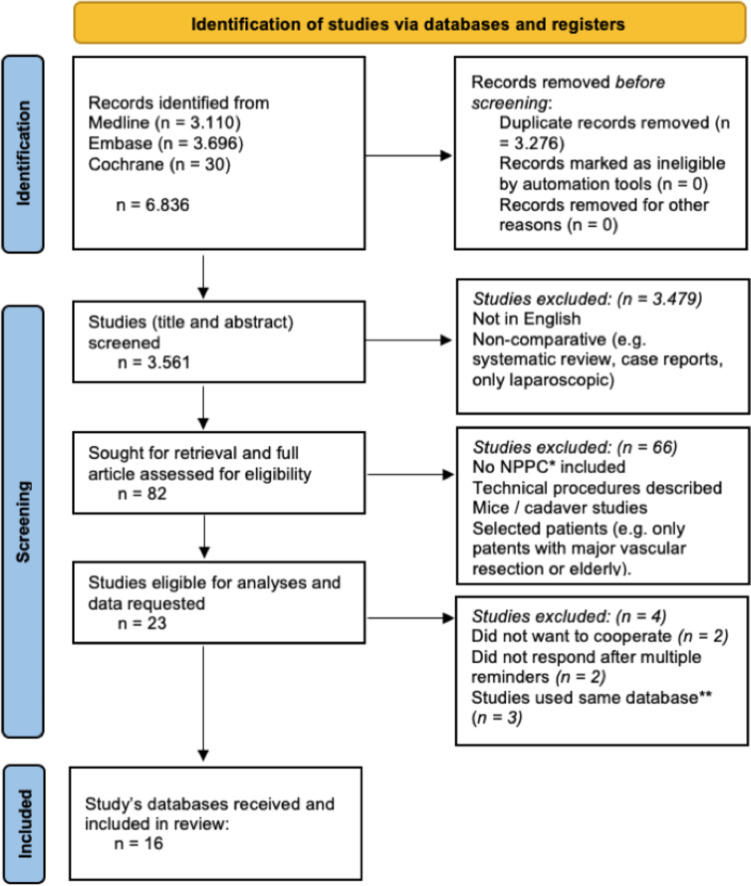
Of the 3530 screened studies, 23 compared MIPD versus OPD with included NPPC and matched the selection criteria (Fig. 1). Subsequently, the corresponding or senior authors were invited to share the database of their study. When multiple studies were based on the same database, the most complete database of the most recent study was requested [51–53]. Requested databases of four studies were not retrieved [54–57].
Fig. 1.
Flowchart systematic web search; *NPPC, non-pancreatic periampullary cancer; **when multiple studies used the same database, the complete database of the most recent study was requested
Study and patient characteristics
In total, 16 studies, of which four randomized controlled trials and 12 retrospective cohort studies, were included [29, 33, 51, 52, 58–69]. Included number of patients with NPPC varied between 14 [60] and 436 [29] per study (Table 1). One study [51] focused on ampullary cancer in specific, while the remaining 15 studies included all NPPCs. Most studies were conducted in South Korea, China, and the Netherlands (World map, Fig. A2, Appendix). No conflicts of interests were identified in the included studies.
Table 1.
Characteristics of the included studies
| Study | Country | Study design | No. of patients | Indication | ||||
|---|---|---|---|---|---|---|---|---|
| Total | MIPD | OPD | MIPD | OPD | P-value | |||
| Hakeem et al. 2014 [58] | UK | RCS | 24 | 12 | 12 | AAC, 9 (38%) | AAC, 9 (38%) | 1.000 |
| DCC, 3 (13%) | DCC, 3 (13%) | |||||||
| DAC, 0 (0%) | DAC, 0 (0%) | |||||||
| Low et al. 2020 [52] | Singapore | RCS | 14 | 5 | 9 | AAC, 4 (33%) | AAC, 4 (33%) | 0.598 |
| DCC, 2 (17%) | DCC, 1 (8%) | |||||||
| DAC, 1 (8%) | DAC, 0 (0%) | |||||||
| van Hilst et al. 2019 [59] | Netherlands | RCT | 38 | 20 | 18 | AAC, 12 (32%) | AAC, 6 (16%) | 0.254 |
| DCC, 5 (13%) | DCC, 8 (21%) | |||||||
| DAC, 3 (8%) | DAC, 4 (11%) | |||||||
| Poves et al. 2017 [60] | Spain | RCT | 14 | 11 | 3 | AAC, 5 (36%) | AAC, 1 (7%) | 0.707 |
| DCC, 6 (43%) | DCC, 2 (14%) | |||||||
| DAC, 0 (0%) | DAC, 0 (0%) | |||||||
| Mazzola et al. 2021 [61] | Italy | RCS | 27 | 16 | 11 | AAC, 11 (41%) | AAC, 6 (22%) | 0.424 |
| DCC, 5 (19%) | DCC, 4 (15%) | |||||||
| DAC, 0 (0%) | DAC, 1 (4%) | |||||||
| Palanivelu et al. 2019 [62] | India | RCT | 53 | 29 | 24 | AAC, 15 (28%) | AAC, 11 (21%) | 0.582 |
| DCC, 4 (8%) | DCC, 6 (11%) | |||||||
| DAC, 10 (19%) | DAC, 7 (13%) | |||||||
| Shin et al. 2019 [63] | South Korea | RCS | 80 | 40 | 39 | AAC, 19 (24%) | AAC, 17 (22%) | 0.127 |
| DCC, 19 (24%) | DCC, 20 (25%) | |||||||
| DAC, 4 (5%) | DAC, 0 (0%) | |||||||
| Yoo et al. 2020 [77] | South Korea | RCS | 359 | 76 | 282 | AAC, 76 (21%) | AAC, 282 (79%) | 0.604 |
| DCC, 0 | DCC, 0 | |||||||
| DAC, 0 | DAC, 0 | |||||||
| Klompmaker et al. 2018 [64] | Netherlands | RCS | 308 | 266 | 42 | AAC, 131 (43%) | AAC, 25 (8%) | P = 0.463 |
| DCC, 89 (29%) | DCC, 11 (4%) | |||||||
| DAC, 46 (15%) | DAC, 6 (2%) | |||||||
| Kim et al. 2021 [33] | South Korea | RCS | 178 | 45 | 133 | AAC, 22 (12%) | AAC, 66 (37%) | 0.939 |
| DCC, 20 (11%) | DCC, 60 (34%) | |||||||
| DAC, 3 (2%) | DAC, 7 (4%) | |||||||
| Bencini et al. 2020 [65] | Italy | RCS | 45 | 23 | 22 | AAC, 17 (38%) | AAC, 6 (13%) | 0.007 |
| DCC, 5 (11%) | DCC, 14 (31%) | |||||||
| DAC, 1 (2%) | DAC, 2 (4%) | |||||||
| Deichmann et al. 2016 [66] | Germany | RCS | 31 | 14 | 17 | AAC, 7 (23%) | AAC, 9 (29%) | 0.950 |
| DCC, 4 (13%) | DCC, 4 (13%) | |||||||
| DAC, 3 (10%) | DAC, 4 (13%) | |||||||
| Choi et al. 2020 [67] | South Korea | RCS | 118 | 69 | 49 | AAC, 31 (26%) | AAC, 9 (8%) | 0.010 |
| DCC, 34 (29%) | DCC, (37 (31%) | |||||||
| DAC, 4 (3%) | DAC, 3 (3%) | |||||||
| Delitto et al. 2014 [68] | USA | RCS | 52 | 24 | 28 | AAC, 13 (25%) | AAC, 17 (33%) | 0.483 |
| DCC, 10 (19%) | DCC, 8 (15%) | |||||||
| DAC, 1 (2%) | DAC, 3 (6%) | |||||||
| Wang et al. 2021 [69] | China | RCT | 173 | 100 | 73 | AAC, 16 (9%) | AAC, 13 (8%) | 0.907 |
| DCC, 40 (23%) | DCC, 27 (16%) | |||||||
| DAC, 44 (25%) | DAC, 33 (19%) | |||||||
| Dang et al. 2021 [29] | China | RCS | 436 | 148 | 288 | AAC, 24 (6%) | AAC, 51 (12%) | 0.324 |
| DCC, 34 (8%) | DCC, 49 (11%) | |||||||
| DAC, 90 (21%) | DAC, 188 (43%) | |||||||
Bold values indicate a significance level <0.05
Abbreviations: MIPD minimally invasive pancreatoduodenectomy, OPD open pancreatoduodenectomy, RCS retrospective cohort study, RCT randomized controlled trial, AAC ampullary adenocarcinoma, DCC distal cholangiocarcinoma, DAC duodenal adenocarcinoma
The meta-analyses included a total of 1949 patients with resected NPPC, consisting of 902 MIPD and 1047 OPD. Within the MIPD cohort, 146 patients after Robotic PD were included. Patient demographics, surgical details, and tumor characteristics are demonstrated in Table 2, and elaborate baseline characteristics per NPPC subgroup can be found in the Appendix (Table A1). Age and BMI were higher in the MIPD group (65 versus 63 years and 23.2 versus 22.9kg/m2, Table 2) and there were less patients with ampullary cancer in the MIPD group (46 versus 51%; P = 0.016, Table 2) and more patients with distal cholangiocarcinoma in the MIPD group (31 versus 24%; P < 0.001; Table 2). In the MIPD group, more patients with distal cholangio and duodenal cancer had a higher T-stage (P = 0.009 and P = 0.047 respectively), while the tumor size of only distal cholangiocarcinoma was larger in the OPD group (median 20 versus 25mm; P = 0.001, Table 2). Other baseline characteristics (sex, ASA, NPPC subgroup, N-stage, adjuvant chemotherapy, and R1 resection) did not differ significantly between the MIPD and OPD group based on P-value and standardized mean differences (Table 2) [47].
Table 2.
Baseline characteristics of all included patients
| Total (1949) | MIPD (902, 46.3%) | OPD (1047, 53.7%) | P-value | SMD | |
|---|---|---|---|---|---|
| Age, yrs, median (IQR) | 64 (56–71) | 65 (57–72) | 63 (55–71) | 0.015 | |
| Male, n (%) | 1131 (58) | 507 (56.2) | 624 (59.6) | 0.130 | 0.016 |
| ASA, mean (SD) | 2.1 (0.5) | 2.1 (0.6) | 2.1 (0.5) | 0.395 | 0.037 |
| BMI, median kg/m2 (IQR) | 23.4 (3.4) | 23.2 (21.0–25.6) | 22.9 (21.0–25.1) | 0.032 | |
| NPPC subtype | 0.003 | 0.136 | |||
| AAC, n (%) | 928 (49) | 403 (46) | 525 (51) | 0.016 | 0.110 |
| DCC, n (%) | 526 (28) | 276 (31) | 250 (24) | < 0.001 | 0.151 |
| DAC, n (%) | 461 (24) | 207 (23) | 254 (25) | 0.500 | 0.031 |
| Tumor size, median (IQR) | 15 (20–30) | 20 (15–28) | 21 (15–30) | 0.038 | |
| AAC, median (IQR) | 20 (13–25) | 20 (15–26) | 0.185 | ||
| DCC, median (IQR) | 20 (16–28) | 25 (20–34) | 0.001 | ||
| DAC, median (IQR) | 20.5 (16.8–35) | 20 (16–30) | 0.156 | ||
| T-stage tumor, total, n (%) |
T1-2: 635 (56) T3-4: 509 (45) |
T1-2: 259 (50) T3-4: 257 (50) |
T1-2: 376 (60) T3-4: 252 (40) |
< 0.001 | 0.231 |
| AAC, n (%) |
T1-2: 189 (60) T3-4: 125 (40) |
T1-2: 288 (64) T3-4: 161 (36) |
0.267 | 0.082 | |
| DCC, n (%) |
T1-2: 61 (38) T3-4: 100 (62) |
T1-2: 72 (53) T3-4: 64 (47) |
0.009 | 0.307 | |
| DAC, n (%) |
T1-2: 3 (12) T3-4: 22 (88) |
T1-2: 9 (36) T3-4: 16 (64) |
0.047 | 0.580 | |
| N-stage 1–2, n (%) |
N0: 627 (60) N1-2: 418 (40) |
N0: 343 (61) N1-2: 219 (39) |
N0: 377 (59) N1-2: 262 (41) |
0.480 | 0.041 |
| Adjuvant Chemotherapy, n (%) | 412 (41) | 179 (43) | 233 (40) | 0.470 | 0.046 |
| R1 resection margin, n (%) | 142 (8) | 67 (8) | 75 (7) | 0.659 | 0.020 |
| Lymph nodes resected, median (IQR) | 14 (10–19) | 13 (10–19) | 14 (11–20) | < 0.001 | |
| AAC, median (IQR) | 14 (10–19) | 15 (10–21) | 0.113 | ||
| DCC, median (IQR) | 13 (9–19) | 15 (11–20) | 0.037 | ||
| DAC, median (IQR) | 13 (10–16) | 14 (12–17) | 0.019 | ||
| PA-positive lymph nodes, median (IQR) | 0 (0–2) | 0 (0–2) | 0 (0–2) | 0.926 | |
| Lymph node ratio | 0.00 (0.00–0.10) | 0.00 (0.00–0.11) | 0.00 (0.00–0.10) | 0.759 |
Bold values indicate a significance level <0.05
Abbreviations: SD standard deviation, n count, AC adenocarcinoma, OPD open pancreatoduodenectomy, MIPD minimally invasive pancreatoduodenectomy, SMD standardized mean difference (not applicable for median and IQR), AAC ampullary adenocarcinoma, DCC distal cholangiocarcinoma, DAC duodenal adenocarcinoma, T-stage tumor: differentiated in T1 and T2 versus T3 and T4 groups (elaborate T-stage distribution in the Appendix table A1), following AJCC 7th and 8th edition
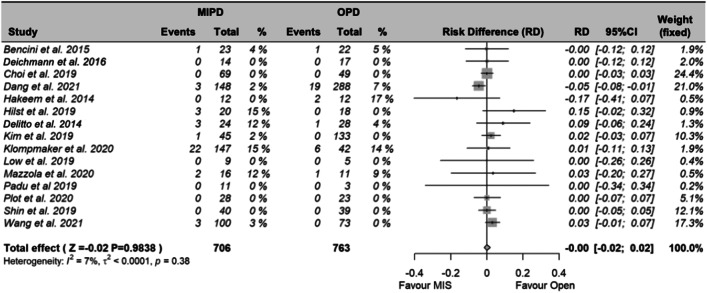
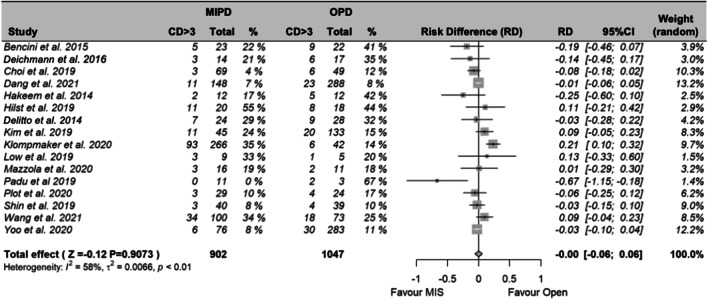
Primary outcomes: 90-day mortality and major morbidity
Overall, 15 studies reported on 90-day mortality, and 16 studies reported on major morbidity. Meta-analysis showed no difference in 90-day mortality (RD -0.01; 95% CI − 1.69–1.66%; P = 0.984; Fig. 2) and major morbidity (RD − 0.04%; 95% CI -6.4–5.7; P = 0.907; Fig. 3) between MIPD and OPD, respectively. More detailed analyses are shown in the Appendix (Fig. A2-A4).
Fig. 2.
Meta-analysis of 90-day mortality between MIPD and OPD. Abbreviations: MIPD, minimally invasive pancreatoduodenectomy; OPD, open pancreatoduodenectomy; RD, risk difference; 95% CI, confidence interval
Fig. 3.
Meta-analysis of major morbidity (Clavien-Dindo 3a – 5) between MIPD and OPD. Abbreviations: CD > 3, Clavien-Dindo 3a-5; MD, mean difference; SD, standard deviation; 95% CI, confidence interval
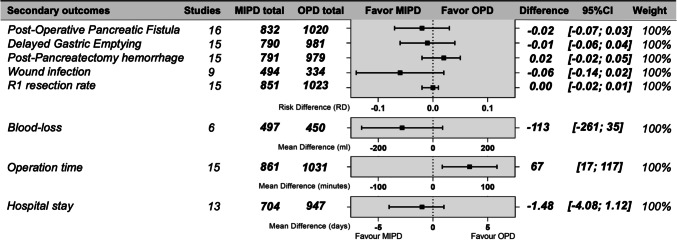
Secondary outcomes: perioperative
Six studies reported on blood-loss. Median blood-loss for MIPD was 200 ml (IQR 100–300 ml) compared to median of 300 ml (IQR 200–500 ml) for OPD. The MD was − 113 ml for the MIPD cohort (95% CI − 261–35 ml; P = 0.135; Fig. 4). In total, 15 studies reported on operative time. The operation time for MIPD was on average 383 min versus 336 min for OPD with a MD of + 67 min (95% CI 17–117 m; P = 0.009; Fig. 4) in the MIPD group. More detailed analyses are shown in the Appendix (Fig. A5-A6).
Fig. 4.
Summary of the meta-analysis with the risk difference or mean difference of the included studies combined. Displayed ranges correlate with the 95% confidence interval. Operation time significance, P = 0.009. Abbreviations: MIPD, minimally invasive pancreatoduodenectomy; OPD, open pancreatoduodenectomy; POPF, postoperative pancreatic fistula; DGE, delayed gastric emptying; PPH, postpancreatectomy hemorrhage; WI, wound infections; R1, resection margin < 1 mm
Secondary outcomes: postoperative
All studies reported on postoperative complications [29, 33, 51, 52, 58–64, 66–69]. The incidence rate of the following complications did not differ between MIPD and OPD: POPF (RD − 1.7; 95% CI − 6.8–3.5%; P = 0.524; Fig. 4), DGE (RD − 1.0; 95% CI − 5.6–3.6%; P = 0.678; Fig. 4), PPH (RD 1.7%; 95% CI − 2.0–5.3%; P = 0.369; Fig. 4), and wound infections (RD − 6.0%; 95% CI − 13.6–1.6%; P = 0.120; Fig. 4). MIPD was not associated with a significantly shorter hospital stay (MD − 1.5 days; 95% CI − 4.1–1.1 days, P = 0.266; Fig. 4). Fifteen studies reported the R0/R1 resection rate [29, 33, 51, 52, 58–64, 66–69]. The R1 resection rate did not differ significantly between MIPD and OPD with a RD of − 0.4% for MIPD (95% CI − 2.1–1.3%; P = 0.624; Fig. 4). More detailed analyses are shown in the Appendix (Appendix, Fig. A7-A12).
Subgroup analyses
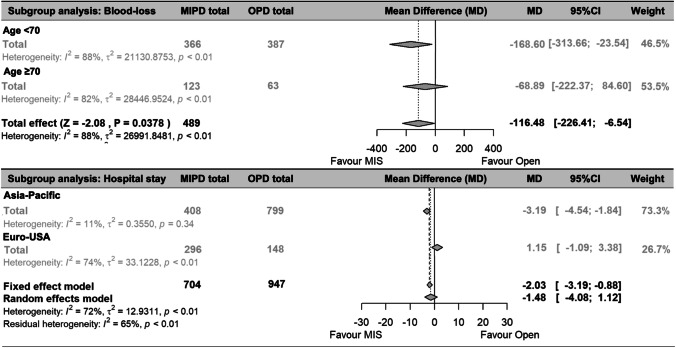
The main subgroup analysis was to compare MIPD and OPD for the three NPPCs separately. The 90-day mortality and major morbidity were comparable between MIPD and OPD for ampullary, distal cholangio, and duodenal cancer. Due to the differences in perioperative blood-loss and the use of oral anticoagulant drugs, subgroup analysis for age was performed and showed that MIPD is associated with significantly less blood-loss for the patients below 70 years old (MD − 169 ml; 95% CI − 314 to − 24 ml; P = 0.023; Fig. 5). For the patients with an age above 70, the measured reduction in blood-loss (− 69 ml) was not significant (95% CI − 222–84 ml, Fig. 5). Also, due to differences in postoperative care, geographic location of the center is analyzed for its influence on the length of hospital stay. In Eastern centers, MIPD was associated with a significant reduction in hospital stay of 3.2 days (95% CI − 4.7 to − 1.7 days, P < 0.001; Fig. 5) compared to OPD. Furthermore, subgroup analyses between pylorus-preserving and pylorus-resecting pancreatoduodenectomy, between Western and Eastern centers, and between young and elderly patients did not result in significant differences in 90-day mortality and major morbidity (Appendix, Fig A3 and A4). In addition, there are no significant differences found in 90-day mortality, major mortality, or POPF when compared OPD with laparoscopic PD or robotic PD separately (appendix, Fig A14).
Fig. 5.
Subgroup analysis Blood-loss (in cc) and Hospital stay (in days). Abbreviations: MIPD, minimally invasive pancreatoduodenectomy; OPD, open pancreatoduodenectomy; MIS, minimally invasive surgery; MD, mean difference; 95% CI, confidence interval
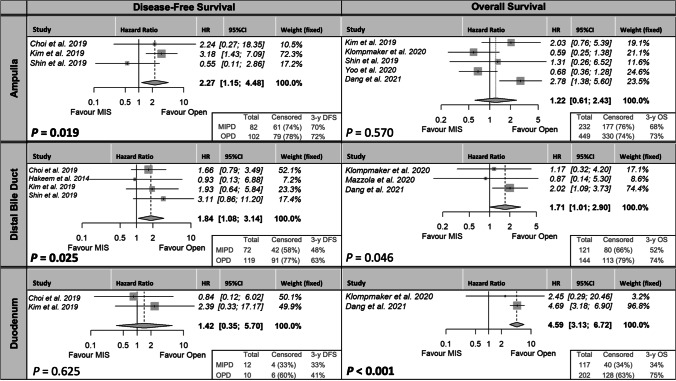
Disease-free and overall survival
Four studies reported on DFS [33, 58, 63, 67], and five studies reported on OS [29, 33, 51, 63, 64]. DFS was longer in the OPD group for ampullary (3-year DFS 70 versus 72%; HR 2.27; 95% CI 1.15–4.48; P = 0.019; Fig. 6) and distal cholangio (3-year DFS 48 versus 63%; HR 1.84; 95% CI 1.08–3.14; P = 0.025; Fig. 6), but not for duodenal cancer (3-year DFS 33 versus 41%; HR 1.42; 95% CI 0.35–5.70; P = 0.625; Fig. 6). The number of patients included for analyses was limited, and there were less patients in the MIPD group for ampullary (82 versus 102), distal cholangio (72 versus 119), but not for duodenal (10 versus 12) cancer. Also, there were less patients censored in the MIPD group for ampullary (74 versus 78%), distal cholangio (58 versus 77%), and duodenal (33 versus 60%). The OS was longer in the OPD group for distal cholangio (3-year OS 52 versus 74%; HR 1.17; 95% CI 1.01–2.90; P = 0.046; Fig. 6) and duodenal cancer (3-year OS 34 versus 75%; HR 4.59; 95% CI 3.13–6.72; P = < 0.001; Fig. 6), but not for ampullary cancer (3-year OS 68 versus 73%; HR 1.22; 95% CI 0.61–2.43; P = 0.570; Fig. 6). For the OS analyses as well, there were less patients in the MIPD group for ampullary (232 versus 449), distal cholangio (121 versus 144), and for duodenal (117 versus 202) cancer. Also, there were less patients censored in the MIPD group for distal cholangio (66% versus 79%) and duodenal (34 versus 63%) cancer. Only for ampullary cancer, the number of censored patients was comparable (76 versus 74%).
Fig. 6.
Disease-free survival (left) and overall survival (right). Abbreviations: MIPD, minimally invasive pancreatoduodenectomy; OPD, open pancreatoduodenectomy; HR, hazard ratio for MIPD compared to OPD; 95% CI, confidence interval; 3-y DFS, 3-year disease-free survival in percentage
Publication bias
Funnel plots were created for each outcome and assessed for symmetry. There was no asymmetry found in the funnel plots for the primary outcomes of 90-day mortality and major morbidity, suggesting no or limited publication bias (Appendix Fig. A15). Also, the funnel plots for POPF, DGE, PPH, hospital stay, blood-loss, operation time, or R1 resections were symmetrical. However, only the funnel plot for the wound infections is significantly different from zero (Egger’s test: P = 0.018).
Discussion
This first IPDMA on minimally invasive versus open pancreatoduodenectomy for NPPC (ampullary, distal cholangio, and duodenal cancer) found that MIPD is associated with comparable 90-day mortality, major morbidity, and postoperative complications compared to OPD. Subgroup analyses show that MIPD was associated with a shorter hospital stay in Eastern centers, and MIPD was associated with less blood-loss in patients below the age of 70. Moreover, operating time was 67 min longer in the MIPD group. Since there is a lack of data on the impact of MIPD for NPPC in terms of long-term survival, conclusions derived from the existing literature are inaccurate.
Various studies suggested comparable short-term short-term mortality and major morbidity between MIPD and OPD [70]. This study as well shows comparable 90-day mortality and major morbidity after MIPD compared to OPD for NPPC collectively but also for ampullary, distal cholangio, and duodenal cancer separately. Furthermore, minimally invasive surgery is considered to be associated with less trauma and less physical stress for the patient. Therefore, it is believed that the application of MIPD has a potential to reduce major complications. Some studies reported a shorter hospital stay, fewer wound infections, and less blood-loss after MIPD [31, 62, 71, 72]. In this study, postoperative complications are found to be comparable between MIPD and OPD for all NPPCs collectively and for ampullary, distal cholangio, and duodenal cancer separately.
In the current literature, subgroup analyses in the comparison of MIPD and OPD are marginally addressed. The NPPC subgroup was not predicted to influence short-term complications, which this meta-analysis did not contradict by demonstrating similar short-term outcomes for ampullary, distal cholangio, and duodenal cancer. Adequate patient selection, such as defining high-risk groups, is key in improving outcomes in pancreatic surgery. Elderly patients are often classified as high-risk group due to a lack of research selectively focusing on elderly patients [37]. Therefore, some surgeons remain reluctant to adopt the minimally invasive approach in this population [63]. Upon this topic, this study performed subgroup analyses for patients with an age above and below 70 and found similar short-term survival and perioperative outcomes within a large number of patients. Notably, MIPD resulted in significantly lower blood-loss than OPD among patients under 70 years old, while the blood-loss rates were comparable for patients aged 70 years and above. It is known that elderly patients generally have more perioperative blood-loss during general surgery [37] and more frequently use oral anticoagulant drugs. A well-known benefit of minimally invasive surgery is a reduction in blood-loss, which may be less prominent in elderly patients or those on anticoagulant medications. Nonetheless, the results of this study indicate that MIPD can be offered safely to patients over the age of 70 in terms of mortality and postoperative complications, comparable to OPD when performed by an experienced surgeon. Furthermore, subgroup analyses of the geographic location of the performing center were applied in the evaluation of hospital stay. This subgroup analysis was required considering that hospital stay can be longer in Eastern centers due to the goal of discharging the patients to their previous living situation instead of the option for a temporary rehabilitation clinic or intensive medical home care. Indeed, our cohort showed a longer hospital stay in Eastern centers as well for MIPD and OPD. In addition, some studies suggested a decreased length of hospital stay for MIPD [29, 33] which is supported by this study for patients in Eastern centers. The difference in length of hospital stay between MIPD and OPD in Western centers was not significant. A potential explanation could be that the benefit of MIPD (less surgical trauma and stress, early mobilization) plays an essential factor in a later phase of the rehabilitation of the patients when some of the Western patients already have been discharged to a rehabilitation clinic or medical home care. Therefore, the benefit of the MIPD on the length of hospital stay will be greater in centers who keep patients admitted until further rehabilitation. This insinuates that the improvements in Western centers should result in shorter stay in rehabilitation centers and should be measured in time to functional recovery or time to return to previous living situation to find the true effect of MIPD on postoperative recovery, which should be confirmed in future studies.
Due to differences in biological behavior of the NPPC subgroups, long-term results are essential. Survival and recurrence rates for MIPD versus OPD for all periampullary tumors are reported to be comparable by multiple studies [32, 33, 57, 66–68, 73] or even improved by the minimally invasive approach for DFS [67, 73] or OS [66]. However, literature on long-term oncological outcomes for patients with resected NPPC is scarce, and when DFS or OS are analyzed, either the number of patients or the follow-up period was limited [29, 33, 57, 61, 64]. In addition, long-term outcomes were only assessed for patient cohorts combining all periampullary tumors or cohorts selectively including patients with PDAC while no studies assessed long-term outcomes for ampullary, distal cholangio, or duodenal cancer separately. Therefore, it is unclear if the outcomes for a patient with NPPC can be extrapolated from the current literature. This is the first study that performed a meta-analysis for all NPPCs separately. Surprisingly, in this study, the MIPD group showed a decrease in DFS for ampullary and distal cholangio cancer, as well as a decrease in OS for distal cholangio and duodenal cancer compared to the OPD group. However, these results are insufficient for permanent conclusions since there are potential explanations for impaired outcomes of MIPD in the databases of the available studies. First, the survival and recurrence data of only 4 studies were available in which both the follow-up period and number of patients included were limited in these studies [58]. One study reported exclusively on 30- and 90-day survival [33], the OS for duodenal cancer is 97% based on one study [29], and the DFS of duodenal cancer is only based on 22 patients. Second, more cases were censored in the OPD group that potentially underestimated the number of events (death or recurrence) in this group. Third, there were differences in important predictive variables in the baseline characteristics [12, 74, 75]. The MIPD group has a substantial higher T-stage, BMI, and age. Nonetheless, it was not possible to propensity score the groups or to correct for risk factors associated with survival and recurrence. Nonetheless, the majority of studies comparing MIPD and OPD that reported the inclusion of ampullary, distal cholangio, or duodenal cancers were included in this review. Therefore, these findings based on widely varied, limited in number and follow-up, marginally comparable data of only a few studies indicate an essential research gap for MIPD long-term outcomes in NPPC subgroups.
Some limitations of the current study should be addressed. First, MIPD requires a long learning curve [76], so very early cases may reduce the treatment effect. Therefore, in this meta-analysis, studies before 2015 were excluded to prevent all studies were conducted after 2015 in order to lower potential bias resulting from the learning curve. Yet, it was challenging to assess if the analyzed databases did not include patients in the early phase of the learning curve. Most studies sought to minimize the effect of the learning curve by including only patients operated by one [29, 52, 58, 60, 61, 66, 68] or two [62] experienced MIPD surgeon(s) with a surpassed learning curve. Studies who included patients operated by different surgeons required an annual volume of > 10 MIPDs [64] or a personal experience of the surgeon of > 20 MIPDs [59], > 30 MIPDs [33], or even > 104 MIPDs [69], and two of the included studies did not report how they prevented the results from the bias of the learning curve [63, 77]. Therefore, it is likely to assume that the included OPD patients in this study were in general operated in a further phase of the surgeon learning curve compared to the MIPD cases which resulted in a disadvantage for MIPD in the analyses. Second, the retrospective aspect of most included studies in surgical techniques introduces the risk of selection bias. Different surgeons prefer different techniques based on their experience. The large numbers of included patients in this review and the inclusion of both randomized controlled trials and cohort studies will minimalize this bias. However, it remains practically impossible to exclude selection in the retrospective setting. Third, the data is collected in multiple centers. Therefore, it was difficult to validate the data on their individual quality. Only events and complications reported by the providing center could be included, resulting in a potential underestimation of the exact number of complications. All received databases were validated with other centers. Studies with deviating data and results were asked to review the database again. Fourth, the international multicontinental design resulted in a collection of centers with sociocultural differences in their healthcare systems. It is possible that this results in differences in postoperative treatment protocols and could have affected the results. Fifth, there was a variation found in R1 resection rate among the included studies. This can be due to either the absence of clear definitions in the studies included or the lack of standardized pathology reporting for the resection margins. In order to ensure oncological safety, future studies should use a uniform definition and implement standardized pathological examinations. Sixth, this study comparing MIPD and OPD did not specifically explore the impact of periampullary tumor differences on surgical outcomes; future research should investigate this aspect to improve understanding of the factors influencing variations in outcomes.
Within these limitations, the principal strength of the present study is the IPDMA design, which is the first in assessing the surgical approach for NPPC and its subgroups. Due to this approach, this is the first study that could assess the different NPPC subgroups. Also, regardless of the rarity of the NPPC tumors, this IPDMA reached large numbers of patients. This allowed to evaluate subgroups and efficiently assess more subtle differences in subgroups between the minimally invasive and open approach for the selected patients. Moreover, 16 centers delivered their database (some of which are responsible for multiple studies in the field), resulting in a database including practically all of the important studies on the topic and thus a valid representation of all published cases and available evidence to date.
In conclusion, this systematic review and IPDMA suggest a safe implication of MIPD only in the perioperative and postoperative period for patients with NPPC. However, the available long-term data suffer from several major limitations which highlight an essential research gap that should be investigated in prospectively maintained international registries or cohort studies with longer follow-up periods for ampullary, distal cholangio, and duodenum cancer separately.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
Collaborating authors
Abdul Hakeem, Fernando Burdio, Palanisamy Senthilnathan, Patricia Sánchez, Hyeong Seok Kim, Steven J. Hughes, Alessandro Giani.
Abbreviations
- AJCC
American Joint Committee on Cancer
- ASA
American Society of Anesthesiologists
- DFS
Disease-free survival
- DGE
Delayed gastric emptying
- HR
Hazard ratio
- IPDMA
Individual Patient Data Meta-Analysis
- IQR
Inter quartile range
- MD
Mead difference
- MIPD
Minimally invasive pancreatoduodenectomy
- NPPC
Non-pancreatic periampullary cancer
- OPD
Open pancreatoduodenectomy
- OS
Overall survival
- PD
Pancreatoduodenectomy
- PDAC
Pancreatic ductal adenocarcinoma
- POPF
Postoperative pancreatic fistula
- PPH
Postpancreatectomy hemorrhage
- RD
Risk difference
- SD
Standard deviation
- SMD
Standardized mean difference
Authors’ contributions
Study conception and design: Uijterwijk, Lemmers, Kasai, Abu Hilal; acquisition of data: all authors; analysis and interpretation of data: Uijterwijk, Kasai, Lemmers, Abu Hilal; drafting of manuscript: Uijterwijk, Lemmers, Abu Hilal; critical revision: all authors.
Data availability
Data used for this study is not available online. For requests, the corresponding author should be contacted.
Declarations
Conflict of interest
Kelly M. Herremans is supported by the National Human Genome Research Institute (T32 HG0008958). Marc G. Besselink has received grants from Intuitive for the LEARNBOT European robot Whipple training program, the DIPLOMA-2 trial, and the E-MIPS quality registry, from Medtronic for the investigator-initiated DIPLOMA trial and from Ethicon for the PANDORA trial and the E-MIPS quality registry. Bas A. Uijterwijk, Meidai Kasai, Daniel H.L. Lemmers, Palanivelu Chinnusamy, Jony van Hilst, Benedetto Ielpo, Kongyuan Wei, Ki Byung Song, Song C Kim, Sjors Klompmaker, Jin-Young Jang, Kelly M. Herremans, Lapo Bencini, Andrea Coratti, Michele Mazzola, Krishna V. Menon, Brian KP Goh, Renyi Qin, Marc G. Besselink, and Mohammed Abu Hilal have no conflicts of interests or financial ties to disclose.
Footnotes
Renyi Qin, Marc G. Besselink, and Mohammed Abu Hilal are shared senior authors.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
There is no publication history of this paper. The paper is not published before. The paper is currently not under submission or consideration at another journal.
Contributor Information
Bas A. Uijterwijk, Email: basuijterwijk@live.nl
Mohammed Abu Hilal, Email: abuhilal9@gmail.com.
for the International Study Group on non-pancreatic periAmpullary CAncer (ISGACA):
Abdul Hakeem, Fernando Burdio, Palanisamy Senthilnathan, Patricia Sánchez, Hyeong Seok Kim, Steven J. Hughes, and Alessandro Giani
References
- 1.Adsay V, Ohike N, Tajiri T, et al. Ampullary region carcinomas: definition and site specific classification with delineation of four clinicopathologically and prognostically distinct subsets in an analysis of 249 cases. Am J Surg Pathol. 2012;36(11):1592–1608. doi: 10.1097/PAS.0b013e31826399d8. [DOI] [PubMed] [Google Scholar]
- 2.Sarmiento JM, Nagomey DM, Sarr MG, et al. Periampullary cancers: are there differences? Surg Clin North Am. 2001;81(3):543–555. doi: 10.1016/S0039-6109(05)70142-0. [DOI] [PubMed] [Google Scholar]
- 3.Stark AP, Sacks GD, Rochefort MM, et al. Long-term survival in patients with pancreatic ductal adenocarcinoma. Surgery. 2016;159(6):1520–1527. doi: 10.1016/j.surg.2015.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schnelldorfer T, Ware AL, Sarr MG, et al. Long-term survival after pancreatoduodenectomy for pancreatic adenocarcinoma: is cure possible? Ann Surg. 2008;247(3):456–462. doi: 10.1097/SLA.0b013e3181613142. [DOI] [PubMed] [Google Scholar]
- 5.Han SS, Jang JY, Kim SW, et al. Analysis of long-term survivors after surgical resection for pancreatic cancer. Pancreas. 2006;32(3):271–275. doi: 10.1097/01.mpa.0000202953.87740.93. [DOI] [PubMed] [Google Scholar]
- 6.Kure S, Kaneko T, Takeda S, et al. Analysis of long-term survivors after surgical resection for invasive pancreatic cancer. HPB (Oxford) 2005;7(2):129–134. doi: 10.1080/13651820510003744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Erdmann JI, Eskens FA, Vollmer CM, et al. Histological and molecular subclassification of pancreatic and nonpancreatic periampullary cancers: implications for (neo) adjuvant systemic treatment. Ann Surg Oncol. 2015;22(7):2401–2407. doi: 10.1245/s10434-014-4267-4. [DOI] [PubMed] [Google Scholar]
- 8.Moekotte AL, Lof S, Van Roessel S, et al. Histopathologic predictors of survival and recurrence in resected ampullary adenocarcinoma: international multicenter cohort study. Ann Surg. 2020;272(6):1086–1093. doi: 10.1097/SLA.0000000000003177. [DOI] [PubMed] [Google Scholar]
- 9.Hatzaras I, George N, Muscarella P, et al. Predictors of survival in periampullary cancers following pancreaticoduodenectomy. Ann Surg Oncol. 2010;17(4):991–997. doi: 10.1245/s10434-009-0883-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Riall TS, Cameron JL, Lillemoe KD, et al. Resected periampullary adenocarcinoma: 5-year survivors and their 6- to 10-year follow-up. Surgery. 2006;140(5):764–772. doi: 10.1016/j.surg.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 11.Ahn DH, Bekaii-Saab T (2014) Ampullary cancer: an overview. Am Soc Clin Oncol Educ Book 112–5 [DOI] [PMC free article] [PubMed]
- 12.He C, Mao Y, Wang J, et al. Nomograms predict long-term survival for patients with periampullary adenocarcinoma after pancreatoduodenectomy. BMC Cancer. 2018;18(1):327. doi: 10.1186/s12885-018-4240-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Albores-Saavedra J, Schwartz AM, Batich K, et al. Cancers of the ampulla of vater: demographics, morphology, and survival based on 5,625 cases from the SEER program. J Surg Oncol. 2009;100(7):598–605. doi: 10.1002/jso.21374. [DOI] [PubMed] [Google Scholar]
- 14.Winter JM, Cameron JL, Olino K, et al. Clinicopathologic analysis of ampullary neoplasms in 450 patients: implications for surgical strategy and long-term prognosis. J Gastrointest Surg. 2010;14(2):379–387. doi: 10.1007/s11605-009-1080-7. [DOI] [PubMed] [Google Scholar]
- 15.Moekotte AL, van Roessel S, Malleo G, et al. Development and external validation of a prediction model for survival in patients with resected ampullary adenocarcinoma. Eur J Surg Oncol. 2020;46(9):1717–1726. doi: 10.1016/j.ejso.2020.04.011. [DOI] [PubMed] [Google Scholar]
- 16.Moekotte AL, Malleo G, van Roessel S, et al. Gemcitabine-based adjuvant chemotherapy in subtypes of ampullary adenocarcinoma: international propensity score-matched cohort study. Br J Surg. 2020;107(9):1171–1182. doi: 10.1002/bjs.11555. [DOI] [PubMed] [Google Scholar]
- 17.Andrianello S, Paiella S, Allegrini V, et al. Pancreaticoduodenectomy for distal cholangiocarcinoma: surgical results, prognostic factors, and long-term follow-up. Langenbecks Arch Surg. 2015;400(5):623–628. doi: 10.1007/s00423-015-1320-0. [DOI] [PubMed] [Google Scholar]
- 18.Tan X, Xiao K, Liu W, et al. Prognostic factors of distal cholangiocarcinoma after curative surgery: a series of 84 cases. Hepatogastroenterology. 2013;60(128):1892–1895. [PubMed] [Google Scholar]
- 19.Kim HJ, Kim CY, Hur YH, et al. Prognostic factors for survival after curative resection of distal cholangiocarcinoma: perineural invasion and lymphovascular invasion. Surg Today. 2014;44(10):1879–1886. doi: 10.1007/s00595-014-0846-z. [DOI] [PubMed] [Google Scholar]
- 20.Belkouz A, Van Roessel S, Strijker M et al (2022) Development and external validation of a prediction model for overall survival after resection of distal cholangiocarcinoma. Br J Cancer 126(9):1280–1288 [DOI] [PMC free article] [PubMed]
- 21.Nakagawa K, Sho M, Okada KI et al (2022) Surgical results of non-ampullary duodenal cancer: a nationwide survey in Japan. J Gastroenterol 1–12 [DOI] [PubMed]
- 22.Li D, Si X, Wan T, et al. Outcomes of surgical resection for primary duodenal adenocarcinoma: a systematic review. Asian J Surg. 2019;42(1):46–52. doi: 10.1016/j.asjsur.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 23.Meijer LL, Alberga AJ, de Bakker JK, et al. Outcomes and treatment options for duodenal adenocarcinoma: a systematic review and meta-analysis. Ann Surg Oncol. 2018;25(9):2681–2692. doi: 10.1245/s10434-018-6567-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Solaini L, Jamieson NB, Metcalfe M, et al. Outcome after surgical resection for duodenal adenocarcinoma in the UK. Br J Surg. 2015;102(6):676–681. doi: 10.1002/bjs.9791. [DOI] [PubMed] [Google Scholar]
- 25.Smeenk HG, Erdmann J, van Dekken H, et al. Long-term survival after radical resection for pancreatic head and ampullary cancer: a potential role for the EGF-R. Dig Surg. 2007;24(1):38–45. doi: 10.1159/000100917. [DOI] [PubMed] [Google Scholar]
- 26.Goh BK, Low TY, Koh YX, et al. Changing trends and outcomes associated with the adoption of minimally invasive pancreatic surgeries: a single institution experience with 150 consecutive procedures in Southeast Asia. J Minim Access Surg. 2020;16(4):404–410. doi: 10.4103/jmas.JMAS_127_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Hilst J, de Rooij T, Abu Hilal M, et al. Worldwide survey on opinions and use of minimally invasive pancreatic resection. HPB (Oxford) 2017;19(3):190–204. doi: 10.1016/j.hpb.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 28.Dokmak S, Fteriche FS, Aussilhou B, et al. The largest European single-center experience: 300 laparoscopic pancreatic resections. J Am Coll Surg. 2017;225(2):226–234 e2. doi: 10.1016/j.jamcollsurg.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 29.Dang C, Wang M, Zhu F, et al. Comparison of laparoscopic and open pancreaticoduodenectomy for the treatment of nonpancreatic periampullary adenocarcinomas: a propensity score matching analysis. Am J Surg. 2021;222(2):377–382. doi: 10.1016/j.amjsurg.2020.12.023. [DOI] [PubMed] [Google Scholar]
- 30.Kamarajah SK, Gujjuri R, Bundred JR, et al. Long-term survival after minimally invasive resection versus open pancreaticoduodenectomy for periampullary cancers: a systematic review, meta-analysis and meta-regression. HPB (Oxford) 2021;23(2):197–205. doi: 10.1016/j.hpb.2020.09.023. [DOI] [PubMed] [Google Scholar]
- 31.Lin D, Yu Z, Chen X, et al. Laparoscopic versus open pancreatoduodenectomy: a meta-analysis of randomized controlled trials. Rev Esp Enferm Dig. 2020;112(1):34–40. doi: 10.17235/reed.2019.6343/2019. [DOI] [PubMed] [Google Scholar]
- 32.Chapman BC, Gleisner A, Ibrahim-Zada I, et al. Laparoscopic pancreaticoduodenectomy: changing the management of ampullary neoplasms. Surg Endosc. 2018;32(2):915–922. doi: 10.1007/s00464-017-5766-8. [DOI] [PubMed] [Google Scholar]
- 33.Kim HS, Kim H, Kwon W, et al. Perioperative and oncologic outcome of robot-assisted minimally invasive (hybrid laparoscopic and robotic) pancreatoduodenectomy: based on pancreatic fistula risk score and cancer/staging matched comparison with open pancreatoduodenectomy. Surg Endosc. 2021;35(4):1675–1681. doi: 10.1007/s00464-020-07551-2. [DOI] [PubMed] [Google Scholar]
- 34.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med. 2021;18(3):e1003583. doi: 10.1371/journal.pmed.1003583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lu C, Lu T, Ge L, et al. Use of AMSTAR-2 in the methodological assessment of systematic reviews: protocol for a methodological study. Ann Transl Med. 2020;8(10):652. doi: 10.21037/atm-20-392a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–196. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 37.Brown CHt, Savage WJ, Masear CG, et al. Odds of transfusion for older adults compared to younger adults undergoing surgery. Anesth Analg. 2014;118(6):1168–78. doi: 10.1213/ANE.0000000000000033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nikfarjam M, Houli N, Tufail F, et al. Reduction in delayed gastric emptying following non-pylorus preserving pancreaticoduodenectomy by addition of a Braun enteroenterostomy. JOP. 2012;13(5):488–496. doi: 10.6092/1590-8577/800. [DOI] [PubMed] [Google Scholar]
- 39.Organization WH (2000) International association for the study of obesity, international obesity taskforce. The Asia-Pacific perspective: redefining obesity and its treatment 15–21
- 40.Ament R. Origin of the ASA classification. Anesthesiology. 1979;51(2):179. doi: 10.1097/00000542-197908000-00023. [DOI] [PubMed] [Google Scholar]
- 41.Amin MB, Greene FL, Edge SB, et al. The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017;67(2):93–99. doi: 10.3322/caac.21388. [DOI] [PubMed] [Google Scholar]
- 42.Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17(6):1471–4. doi: 10.1245/s10434-010-0985-4. [DOI] [PubMed] [Google Scholar]
- 43.Pulvirenti A, Ramera M, Bassi C. Modifications in the International Study Group for Pancreatic Surgery (ISGPS) definition of postoperative pancreatic fistula. Transl Gastroenterol Hepatol. 2017;2:107. doi: 10.21037/tgh.2017.11.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wente MN, Bassi C, Dervenis C, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS) Surgery. 2007;142(5):761–768. doi: 10.1016/j.surg.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 45.Wente MN, Veit JA, Bassi C, et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142(1):20–25. doi: 10.1016/j.surg.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 46.Campbell F, Cairns A, Duthie F, Feakins R (2017) Dataset for the histopathological reporting of carcinomas of the pancreas, ampulla of Vater and common bile duct. R Coll Pathol. https://www.rcpath.org/static/34910231-c106-4629-a2de9e9ae6f87ac1/g091-pancreasdataset-mar17.pdf
- 47.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–3107. doi: 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Andrade C (2020) Mean difference, standardized mean difference (SMD), and their use in meta-analysis: as simple as it gets. J Clin Psychiatry 81(5) [DOI] [PubMed]
- 49.Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaborationʼs tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Egger M, Smith GD. Bias in location and selection of studies. BMJ. 1998;316(7124):61–66. doi: 10.1136/bmj.316.7124.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Han SH, Kang CM, Hwang HK, et al. The Yonsei experience of 104 laparoscopic pancreaticoduodenectomies: a propensity score-matched analysis with open pancreaticoduodenectomy. Surg Endosc. 2020;34(4):1658–1664. doi: 10.1007/s00464-019-06942-4. [DOI] [PubMed] [Google Scholar]
- 52.Low TY, Koh YX, Goh BK. First experience with robotic pancreatoduodenectomy in Singapore. Singapore Med J. 2020;61(11):598–604. doi: 10.11622/smedj.2019119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Goh BKP, Low TY, Kam JH, et al. Initial experience with laparoscopic and robotic surgery for the treatment of periampullary tumours: single institution experience with the first 30 consecutive cases. ANZ J Surg. 2019;89(4):E137–E141. doi: 10.1111/ans.15033. [DOI] [PubMed] [Google Scholar]
- 54.Chapman BC, Gajdos C, Hosokawa P, et al. Comparison of laparoscopic to open pancreaticoduodenectomy in elderly patients with pancreatic adenocarcinoma. Surg Endosc. 2018;32(5):2239–2248. doi: 10.1007/s00464-017-5915-0. [DOI] [PubMed] [Google Scholar]
- 55.Meng L-W, Cai Y-Q, Li Y-B et al (2018) Comparison of laparoscopic and open pancreaticoduodenectomy for the treatment of nonpancreatic periampullary adenocarcinomas. Surg Laparosc Endosc Percutan Tech 28(1):56 [DOI] [PMC free article] [PubMed]
- 56.Varley PR, Zenati MS, Klobuka A, et al. Does robotic pancreaticoduodenectomy improve outcomes in patients with high risk morphometric features compared to the open approach. HPB (Oxford) 2019;21(6):695–701. doi: 10.1016/j.hpb.2018.10.016. [DOI] [PubMed] [Google Scholar]
- 57.Conrad C, Basso V, Passot G, et al. Comparable long-term oncologic outcomes of laparoscopic versus open pancreaticoduodenectomy for adenocarcinoma: a propensity score weighting analysis. Surg Endosc. 2017;31(10):3970–3978. doi: 10.1007/s00464-017-5430-3. [DOI] [PubMed] [Google Scholar]
- 58.Hakeem AR, Verbeke CS, Cairns A, et al. A matched-pair analysis of laparoscopic versus open pancreaticoduodenectomy: oncological outcomes using Leeds Pathology Protocol. Hepatobiliary Pancreat Dis Int. 2014;13(4):435–441. doi: 10.1016/S1499-3872(14)60048-5. [DOI] [PubMed] [Google Scholar]
- 59.van Hilst J, de Rooij T, Bosscha K, et al. Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol. 2019;4(3):199–207. doi: 10.1016/S2468-1253(19)30004-4. [DOI] [PubMed] [Google Scholar]
- 60.Poves I, Burdio F, Morato O, et al. Comparison of perioperative outcomes between laparoscopic and open approach for pancreatoduodenectomy: the PADULAP randomized controlled trial. Ann Surg. 2018;268(5):731–739. doi: 10.1097/SLA.0000000000002893. [DOI] [PubMed] [Google Scholar]
- 61.Mazzola M, Giani A, Crippa J, et al. Totally laparoscopic versus open pancreaticoduodenectomy: a propensity score matching analysis of short-term outcomes. Eur J Surg Oncol. 2021;47(3 Pt B):674–680. doi: 10.1016/j.ejso.2020.10.036. [DOI] [PubMed] [Google Scholar]
- 62.Palanivelu C, Senthilnathan P, Sabnis SC, et al. Randomized clinical trial of laparoscopic versus open pancreatoduodenectomy for periampullary tumours. Br J Surg. 2017;104(11):1443–1450. doi: 10.1002/bjs.10662. [DOI] [PubMed] [Google Scholar]
- 63.Shin H, Song KB, Kim YI, et al. Propensity score-matching analysis comparing laparoscopic and open pancreaticoduodenectomy in elderly patients. Sci Rep. 2019;9(1):12961. doi: 10.1038/s41598-019-49455-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Klompmaker S, van Hilst J, Wellner UF, et al. Outcomes after minimally-invasive versus open pancreatoduodenectomy: a Pan-European Propensity Score Matched Study. Ann Surg. 2020;271(2):356–363. doi: 10.1097/SLA.0000000000002850. [DOI] [PubMed] [Google Scholar]
- 65.Bencini L, Tofani F, Paolini C, et al. Single-centre comparison of robotic and open pancreatoduodenectomy: a propensity score-matched study. Surg Endosc. 2020;34(12):5402–5412. doi: 10.1007/s00464-019-07335-3. [DOI] [PubMed] [Google Scholar]
- 66.Deichmann S, Bolm LR, Honselmann KC, et al. Perioperative and long-term oncological results of minimally invasive pancreatoduodenectomy as hybrid technique - a matched pair analysis of 120 cases. Zentralbl Chir. 2018;143(2):155–161. doi: 10.1055/s-0043-124374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Choi M, Hwang HK, Rho SY, et al. Comparing laparoscopic and open pancreaticoduodenectomy in patients with pancreatic head cancer: oncologic outcomes and inflammatory scores. J Hepatobiliary Pancreat Sci. 2020;27(3):124–131. doi: 10.1002/jhbp.697. [DOI] [PubMed] [Google Scholar]
- 68.Delitto D, Luckhurst CM, Black BS, et al. Oncologic and perioperative outcomes following selective application of laparoscopic pancreaticoduodenectomy for periampullary malignancies. J Gastrointest Surg. 2016;20(7):1343–1349. doi: 10.1007/s11605-016-3136-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wang M, Li D, Chen R, et al. Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours: a multicentre, open-label, randomised controlled trial. Lancet Gastroenterol Hepatol. 2021;6(6):438–447. doi: 10.1016/S2468-1253(21)00054-6. [DOI] [PubMed] [Google Scholar]
- 70.Feng Q, Liao W, Xin Z, et al. Laparoscopic pancreaticoduodenectomy versus conventional open approach for patients with pancreatic duct adenocarcinoma: an up-to-date systematic review and meta-analysis. Front Oncol. 2021;11:749140. doi: 10.3389/fonc.2021.749140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Moghadamyeghaneh Z, Sleeman D, Stewart L. Minimal-invasive approach to pancreatoduodenectomy is associated with lower early postoperative morbidity. Am J Surg. 2019;217(4):718–724. doi: 10.1016/j.amjsurg.2018.04.009. [DOI] [PubMed] [Google Scholar]
- 72.Song KB, Kim SC, Hwang DW, et al. Matched case-control analysis comparing laparoscopic and open pylorus-preserving pancreaticoduodenectomy in patients with periampullary tumors. Ann Surg. 2015;262(1):146–155. doi: 10.1097/SLA.0000000000001079. [DOI] [PubMed] [Google Scholar]
- 73.Croome KP, Farnell MB, Que FG, et al. Total laparoscopic pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: oncologic advantages over open approaches? Ann Surg. 2014;260(4):633–8. doi: 10.1097/SLA.0000000000000937. [DOI] [PubMed] [Google Scholar]
- 74.van Roessel S, Strijker M, Steyerberg EW, et al. International validation and update of the Amsterdam model for prediction of survival after pancreatoduodenectomy for pancreatic cancer. Eur J Surg Oncol. 2020;46(5):796–803. doi: 10.1016/j.ejso.2019.12.023. [DOI] [PubMed] [Google Scholar]
- 75.Greenblatt DY, Kelly KJ, Rajamanickam V, et al. Preoperative factors predict perioperative morbidity and mortality after pancreaticoduodenectomy. Ann Surg Oncol. 2011;18(8):2126–2135. doi: 10.1245/s10434-011-1594-6. [DOI] [PubMed] [Google Scholar]
- 76.Tyutyunnik P, Klompmaker S, Lombardo C, et al. Learning curve of three European centers in laparoscopic, hybrid laparoscopic, and robotic pancreatoduodenectomy. Surg Endosc. 2022;36(2):1515–1526. doi: 10.1007/s00464-021-08439-5. [DOI] [PubMed] [Google Scholar]
- 77.Yoo D, Song KB, Lee JW et al (2020) A comparative study of laparoscopic versus open pancreaticoduodenectomy for ampulla of Vater carcinoma. J Clin Med 9(7) [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data used for this study is not available online. For requests, the corresponding author should be contacted.