Abstract
Using the 2021 Occupational Employment and Wage Statistics (OEWS) dataset, we calculate the ratio of direct care workers relative to the population of older adults (ages 65+) across rural and urban areas in the US. We find that there are, on average, 32.9 home health aides per 1000 older adults (age 65+) in rural areas and 50.4 home health aides per 1000 older adults in urban areas. There are, on average, 20.9 nursing assistants per 1000 older adults in rural areas and 25.3 nursing assistants per 1000 older adults in urban areas. There is substantial regional variation. Greater investment needs to be made in improving wages and job quality for direct care workers to attract workers to these critical occupations, especially in rural areas where the need for direct care is greater.
Keywords: home and community based care and services, long-term services & supports, nursing homes, policy, population aging
The crisis of COVID-19 in long-term care services and supports (LTSS) has brought attention to significant challenges in staffing long-term care organizations (Barnett & Grabowski, 2020; Grabowski & Mor, 2020; McGarry et al., 2020). While the COVID-19 crisis has been acute, shortages and turnover of direct care workers in LTSS have been a chronic problem for many years, and staffing shortages and instability are expected to worsen as the population ages (Scales, 2020; Spetz et al., 2019; Stone, 2017). Direct care workers are an essential part of supporting an aging rural population, particularly as more individuals favor aging in place over nursing homes and require in-home assistance with activities of daily living (Poo & Berger, 2022). This study aims to examine the number of LTSS direct care workers, including home health workers and nursing assistants, in the US, with a focus on differences in the number of direct care workers in rural and urban areas relative to the older adult population. In our study, we seek to answer two primary research questions:
Research question 1: How does the ratio of direct care workers relative to the older adult population (age 65+) in rural areas compare to the ratio in urban areas?
Research question 2: Is there regional variation in the ratio of direct care workers relative to the older adult population (age 65+) in rural areas compare to the ratio in urban areas?
Below we describe the need for direct care workers in rural areas and factors that may contribute to differences in the supply of direct care workers across rural and urban areas.
The need for LTSS for adults in rural areas.
There are 46.2 million adults aged 65 and older living in the United States, with 10.6 million adults living in rural areas as designated by the US Census Bureau. Rural areas have older populations on average as compared to urban areas, and the proportion of adults aged 65 and older living in rural areas is growing at a faster rate compared to urban areas (Smith & Trevelyan, 2019). Additionally, rural older adults are in poorer health and are more likely to have a disability, compared to urban adults (Anderson et al., 2015; Garcia et al., 2017; Johnson et al., 2007; Tuttle et al., 2020). The older population in rural areas and higher level of disability may contribute to a greater need for LTSS—and a greater need for direct care workers in rural areas.
Access to LTSS in rural areas is not well-understood. Rural residents face a number of nonmedical barriers to nursing home care, including financial issues, transportation, and nursing home availability and infrastructure (Henning-Smith et al., 2018). However, rural residents have a higher rate of nursing home utilization as compared to urban older adults, which may indicate that there is a lack of access to home and community based services (HCBS), including home health care or home care services (Henning-Smith et al., 2021). Research has also documented that rural families provide a higher rate of informal family caregiving, which may reflect a lack of access to formal caregiving services or a preference for informal family-based care in rural areas (Sterling et al., 2022).
Policies such as the Balancing Incentive Program have attempted to move funds away from nursing homes and more toward HCBS (Karon et al., 2019). However, research indicates that in rural areas, HCBS infrastructure may not be able to meet demand for services when nursing homes close (Tyler & Fennell, 2017). Shifts in funding, along with consumer preferences for aging-in-place, are leading to growing demand for HCBS services in rural areas and a growing need for home health aides (Karlin, 2018; Watts et al., 2020, 2021).
The direct care workforce in rural areas.
Access to both nursing and HCBS for rural older adults depends on having a robust direct care workforce, as direct care workers provide most of the hands-on care in LTSS. Unfortunately, there is substantial evidence that a shortage of direct care workers is already occurring in LTSS (Graham, 2017, 2022; Ochieng et al., 2022; Stone, 2017), and rural LTSS organizations may especially be struggling to recruit and retain direct care workers. A report from the WWAMI Rural Health Research Center states that rural home health care agencies from all four US Census regions reported difficulty in recruiting and retaining home health care aides and personal care assistants, due to being unable to pay a reasonable wage compared to urban agencies—the burden of additional travel time for staff was also cited as a rural-specific occupational challenge (Skillman et al., 2016). A recent qualitative analysis conducted interviews with key stakeholders including Medicaid administrators, service agency manager and patient advocates from 14 states found that key factors limiting rural HCBS access included greater health care staffing shortages in rural compared to urban areas (Siconolfi et al., 2019).
This study will expand on the information available through the Bureau of Labor Statistics on the direct care workforce by focusing on direct care workers relative to the population of adults in rural areas as compared to urban areas (US Bureau of Labor Statistics, 2019a; 2019b). Research suggests that local labor market variation is very important in planning for population health care utilization and workforce supply (Finkelstein et al., 2016; Fisher & Skinner, 2013). The ratio of licensed health care practitioners relative to the population is routinely tracked and monitored; for example, we know that there are 2.6 physicians per 1000 people in US, with substantial variation in this ratio across rural and urban areas, and there are 17.6 nurses per 1000 people in the US (Shanosky et al., 2020). However, there has been limited research on ratios of home health aides and nursing assistants relative to the populations they are serving, particularly differences in rural and urban areas.
Causes of rural and urban differences in the supply of LTSS direct care workers.
There are many reasons why the supply of LTSS direct care workers may be lower in rural areas as compared to urban areas. First, wages and job benefits are typically higher in urban areas (Skillman et al., 2016). This may draw workers who live in rural areas to either migrate to urban areas or commute for their jobs, which has been shown in past research (Dahal et al., 2020). Second, there may not be a robust long-term care infrastructure in rural areas for employing direct care workers. If home health or home care agencies do not exist in rural areas, we would not expect to find a large number of direct care workers (McAuley et al., 2008; Tyler & Fennell, 2017). Further, families in rural areas may be more likely to provide family caregiving rather than rely on paid caregivers (Sterling et al., 2022). Third, population demographics in rural areas may restrict the direct care workforce; as noted earlier, the rural population is older than urban areas, which means that there are fewer younger workers to fill direct care jobs (Smith & Trevelyan, 2019).
Variation in the direct care workforce across regions in the US.
Recent research has also highlighted substantial differences in the supply of the LTSS workforce across US states and regions, and this extends to rural and urban areas in US regions. For example, a recent study by Chapman et al. (2022) found that the ratio of personal care aides relative to the number of adults with a self-care disability was lower in rural areas in the Southeast and in the Midwest, and higher on the Pacific Coast, in some parts of the Northeast, and in the Mid-North Central region. State-wide and regional LTSS policies underlie the supply and demand for direct care workers in rural and urban areas (Friedman et al., 2021). For example, states use Medicaid 1915(c) HCBS Waivers differently, which may lead to a different distribution of institutional and HCBS care—and a different distribution of home health aides and nursing assistants (Watts et al., 2020, 2021). A recent study by Friedman et al. (2021) showed significant variation across states and regions in increasing numbers of home care workers and decreasing numbers of nursing home workers. Some states have placed more of an emphasis on HCBS, like Washington, and would have a larger number of home health aides, while other states, like Louisiana, depend more heavily on skilled nursing homes to provide care and would have a larger number of certified nursing assistants (Wenzlow et al., 2013).
The goal of this paper is to describe rural and urban differences in the supply of direct care workers relative to the older adult population. We also explore differences in the supply of direct care workers across rural and urban areas in the different Census regions of the US because, as described above, past research has demonstrated substantial regional variation (Chapman et al., 2022; Friedman et al., 2021). Our study contributes to ongoing and necessary research that demonstrates variation in the supply of direct care workforce needed to care for older rural adults in institutional and home-based settings.
Methods
Data
The data used in the study are the 2021 Occupational Employment and Wage Statistics (OEWS) data available through the Bureau of Labor Statistics. The OEWS program collects data on wage and salary workers in nonfarm establishments in order to produce employment and wage estimates for about 800 occupations. The OEWS program surveys approximately 180,000 to 200,000 establishments per panel (every 6 months), taking 3 years to fully collect the sample of 1.1 million establishments, and covers all full-time and part-time age and salary workers in nonfarm industries. Importantly, the OEWS does not include direct care workers that are employed privately by families (not through an agency or organization).
The OEWS program produces these occupational estimates for the nation as a whole, by state, and by metropolitan or nonmetropolitan area. The metropolitan and nonmetropolitan areas designated within the OEWS are defined by the BLS and include clusters of counties. The BLS definitions of metropolitan and nonmetropolitan areas can be found here: https://www.bls.gov/oes/current/msa_def.htm. In this paper, we refer to metropolitan and nonmetropolitan areas as urban and rural areas, respectively; because of the sampling design of the OEWS Survey, finer gradations of rural beyond nonmetropolitan were not possible but this rural/urban distinction in the OEWS has been used in past research (Richardson et al., 2010). The counties that are included “nonmetropolitan areas” in the OEWS align with counties that are designated as rural by the Health Resources and Services Administration (Health Resources and Services Administration, 2010). Further, since home health and nursing homes often serve broad areas, especially in rural areas, bigger measures of geography may be appropriate. Finally, we also use the 2020–2021 Area Health Resource File (AHRF) to estimate the size of the older adult populations (age 65+), which we describe below in the measurement section.
Measurement
We have two primary variables in our analyses in this paper: the number of direct care workers in rural and urban areas, and the older adult population (age 65+) in these areas. First, we identify direct care occupations as either home health aides or nursing assistants in the OEWS based on US Census occupational codes. The full Census code labels are “home health and personal care aides” and “nursing assistants, orderlies, and psychiatric aides,” and which we abbreviate to home health aides and nursing assistants. We only use the occupation codes for identifying workers; we did not use the industry codes to further specify where workers are located. Because the occupational category includes both “personal care aides” and “home health aides,” we know that workers are in agencies that are providing both medical and nonmedical home care, but we do not have information on whether the agency that employs direct care workers is funded by Medicare, Medicaid, or private-pay patients in the OEWS. Because the OEWS includes data collected from employers, it reflects where workers are employed, not where they live. This is an important contribution to the literature, as workers often commute to more populated areas to for their jobs (Dahal et al., 2020).
Second, we estimate the size of the adult population that is age 65 or older in urban and rural areas. The ARHF includes estimates of the 2020 older adult populations (age 65+) from the American Community Survey administered by the US Census Bureau by county; we added the county populations within each metropolitan and nonmetropolitan area together to measure the older adult populations (age 65+) for the larger metropolitan and nonmetropolitan areas defined and used by the OEWS dataset.
Throughout this paper, we present ratios of home health aides and nursing assistants across US major census regions including: New England (1), Middle Atlantic (2), East North Central (3), West North Central (4), South Atlantic (5), East South Central (6), West South Central (7), Mountain (8), and Pacific (9). We have chosen to focus on regional differences because
Analyses
Our primary analyses in this paper included calculating the ratios of home health aides and nursing assistants relative to the population of adults (ages 65+) across urban and rural areas in the US. We calculated the ratios by dividing the number of home health aides or nursing assistants in metropolitan or nonmetropolitan areas available in the OEWS by the number of older adults (age 65+) in metropolitan or nonmetropolitan areas. These ratios can be easily updated for future research when new OEWS data and population data released. We then used descriptive statistics and data visualization by US Census region to present our findings. For the data visualization, we built scatter plots to show the ratio differences in metropolitan and nonmetropolitan areas. We built our scatter plots using Python Pandas and Matplotlib libraries. The home health aide ratios and nursing assistant ratios were plotted on the y-axis separately against US Census region on the x-axis. A full dataset of the number of home health aides, nursing assistants, older adult population (age 65+), and calculated ratios of home health aides and nursing assistants by metropolitan and nonmetropolitan area is included in the Supplemental Appendix. The Supplemental Appendix also includes county and township data so that readers can see how counties and townships are assigned to metropolitan and nonmetropolitan areas.
Findings
We find that there are, on average, 32.8 home health aides per 1000 older adults (age 65+) in rural areas and 50.4 home health aides per 1000 older adults in urban areas (shown in Table 1). These findings indicate that the average ratio of home health aides relative to the older adult population in urban areas is about 34.7% larger than the ratio in rural areas. There are, on average, 20.9 nursing assistants per 1000 older adults in rural areas and 25.3 nursing assistants per 1000 older adults in urban areas. The average ratio of nursing assistants in urban areas is 17.4% times larger than the ratio in rural areas.
Table 1.
Ratios of Direct Care Workers Relative to The Older Adult Population in Rural and Urban Areas.
| Rural areas | Urban Areas | |
|---|---|---|
| Home health aides per 1000 older adults | 32.8 (n = 133) | 50.4 (n = 395) |
| Nursing assistants per 1000 older adults | 20.9 (n = 134) | 25.3 (n = 389) |
Source: OEWS and AHRF
Note. The units of measurement (n) are metropolitan and nonmetropolitan areas defined by the Bureau of Labor Statistics.
In Table 2, we describe regional variation across US Census regions for home health aides and nursing assistants. For each region, we list the average ratio of home health aides per 1000 older adults and nursing assistants per 1000 older adults in rural and urban areas, along with the sample size for each area. We find that rural areas have lower average ratios of both home health aides and nursing assistants across all regions.
Table 2.
Ratios of Direct Care Workers Relative to The Older Adult Population in Rural and Urban Areas by US Census Region.
| Home Health aides | Nursing assistants | ||||
|---|---|---|---|---|---|
| New England | Rural | 14.2 | (n = 9) | 10.2 | (n = 9) |
| Urban | 26.6 | (n = 21) | 13.1 | (n = 21) | |
| Middle Atlantic | Rural | 55.7 | (n = 6) | 18.3 | (n = 6) |
| Urban | 60.9 | (n = 34) | 26.7 | (n = 35) | |
| East North Central | Rural | 30.2 | (n = 19) | 22.2 | (n = 19) |
| Urban | 47.2 | (n = 58) | 27.7 | (n = 57) | |
| West North Central | Rural | 40.9 | (n = 20) | 33.5 | (n = 20) |
| Urban | 61.1 | (n = 33) | 45.1 | (n = 33) | |
| South Atlantic | Rural | 26.2 | (n = 20) | 19.5 | (n = 20) |
| Urban | 27.4 | (n = 83) | 24.7 | (n = 83) | |
| East South Central | Rural | 22.0 | (n = 16) | 21.0 | (n = 16) |
| Urban | 31.9 | (n = 29) | 25.6 | (n = 29) | |
| West South Central | Rural | 43.3 | (n = 17) | 22.8 | (n = 17) |
| Urban | 77.4 | (n = 43) | 25.3 | (n = 42) | |
| Mountain | Rural | 34.4 | (n = 16) | 17.3 | (n = 16) |
| Urban | 53.0 | (n = 37) | 23.0 | (n = 37) | |
| Pacific | Rural | 38.4 | (n = 5) | 11.4 | (n = 10) |
| Urban | 80.4 | (n = 49) | 17.3 | (n = 48) | |
Source: 2021 OEWS and AHRF
Note. The units of measurement (n) are metropolitan and nonmetropolitan areas defined by the Bureau of Labor Statistics.
Home health aides
In Figure 1, we present a scatterplot of the ratios of home health aides per 1000 older adults for rural and urban areas, distributed by US Census region. The scatterplot demonstrates that rural areas have substantially lower ratios compared to urban areas, and this is consistent across the regional distribution. There is also significant regional variation in the ratio of home health aides to the older adult population. Ratios of home health aides to older adults in both rural and urban areas are the lowest in New England, the South Atlantic, and the East South Central regions. The largest disparities between rural and urban areas in the ratio of home health aides to older adults, on average, are found in the West South Central region and the Pacific regions (also see Table 2), although notably the sample size of rural areas in the Pacific region is small (n = 5 rural areas).
Figure 1.
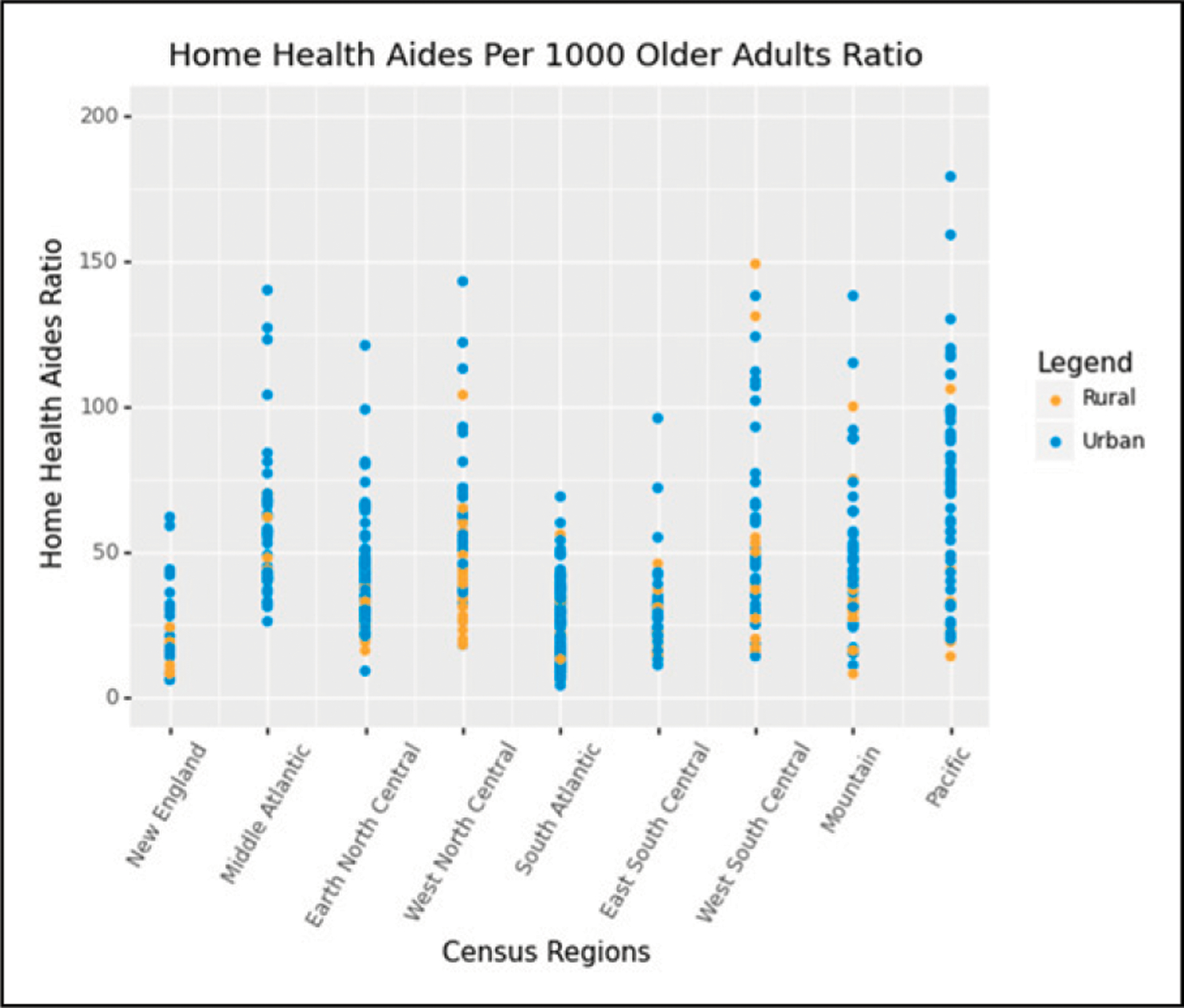
Ratios of home health aides per 1000 older adult (age 65+). Source: 2021 OEWS and AHRF.
Note. The units of measurement (n) are metropolitan and nonmetropolitan areas defined by the Bureau of Labor Statistics.
Nursing assistants
In Figure 2, we present a scatterplot of the ratios of nursing assistants per 1000 older adults for rural and urban areas, distributed by US Census region. The scatterplot demonstrates that rural areas have lower ratios compared to urban areas, and this is also consistent across the regional distribution. Ratios of nursing assistants to older adults in both rural and urban areas are the lowest in New England and the Pacific. In general, ratios of nursing assistants relative to the older adult population are far more consistent across regions than the home health aide workforce (described above), but the West North Central does stand out as having higher ratios of nursing assistants to older adults in both rural and urban areas.
Figure 2.
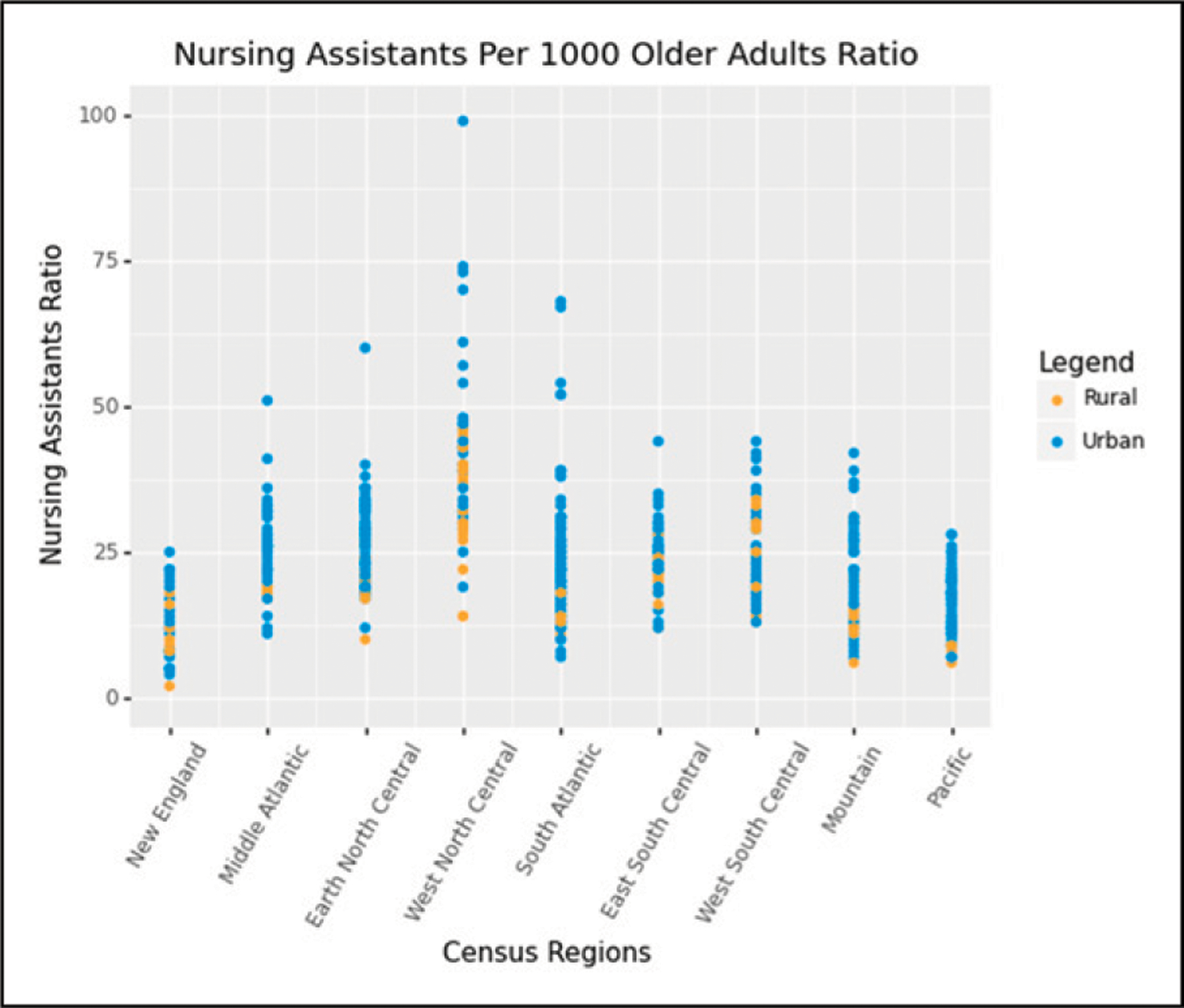
Ratios of nursing assistants per 1000 older adult (age 65+). Source: 2021 OEWS and AHRF.
Note. The units of measurement (n) are metropolitan and nonmetropolitan areas defined by the Bureau of Labor Statistics.
Discussion
The goal of this study was to measure the ratio of the direct care workforce relative to the older adult population in rural and urban areas. Past research has long demonstrated that rural areas have a larger proportion of older adults compared to urban areas (Smith & Trevelyan, 2019), but little research has aimed to document how many home health aides and nursing assistants are located in geographic areas to care for older adults who may need LTSS. The provision of LTSS in rural areas depends on a robust supply of direct care workers, so measuring the ratio of direct care workers relative to the older adult population in rural and urban areas is an important step in assessing where there may be an insufficient supply of direct care workers and LTSS.
Our findings indicate that the ratio of home health aides and nursing assistants in rural areas relative to the older adult population is far lower than in urban areas. The ratio of home health aides per 1000 older adults in rural areas is a third smaller than the ratio in urban areas, and the ratio of nursing assistants per 1000 older adults in rural areas is 17% lower than the average ratio in urban areas. As outlined in our conceptual model, these disparities between rural and urban areas are likely due to many factors, including a lower level of available younger workers to fill direct care positions, lower wages and overall job quality in rural areas, and a lack of long-term care infrastructure to support a direct care workforce. Future research is needed to directly measure the causes of the low ratio of direct care workers relative to the older adult population in rural areas in order to better understand the supply and demand dynamics of this critical workforce.
We also found substantial regional variation in the ratio of home health aides and nursing assistants relative to the older adult population in both rural and urban areas. While we do not directly measure the causes of the regional variation in these ratios, we can provide some potential explanations. For example, New England has consistently lower ratios of home health aides and nursing assistants relative to the older adult population as compared to other regions of the country. New England has among the oldest states in the county, including Maine, Vermont, New Hampshire, Rhode Island, and Connecticut, and it is likely that population demographics are driving their direct workforce supply (Federal Reserve Bank of Boston, 2019).
We also find that the South Atlantic and the East South Central regions have very low ratios of home health aides relative to their older adult populations. A major source of funding of HCBS is Medicaid 1915(c) HCBS Waivers, which have waiting lists in many states. Many of the states with the longest waiting lists are located in the South Atlantic and the East South Central regions, including Florida, South Carolina, Virginia, North Carolina, Kentucky, Maryland, and Georgia (KFF, 2020). These waiting lists indicate that the funding for home care is not adequate in these states to meet demand and that greater funding would lead to greater utilization and a corresponding increase in the home health workforce. HCBS is a complex web of services with many sources of funding, including both Medicare home health care and Medicaid HCBS, but the waiting lists in the South Atlantic and East South Central regions indicate that there is much more capacity for HCBS these regions, which is also reflected in the workforce ratios.
Distribution of long-term care funding is changing to meet the desire for adults to age in place, with large shifts from traditional nursing home services toward HCBS settings; medicaid expenditures on home health services grew by over 6.5% per year since 2011, but Medicaid expenditures on nursing home services increased at just 3.0% per year (He & Gokhale, 2022). Census numbers in skilled nursing units have also declined, and hundreds of units have closed (Flinn, 2020). However, the impact of the shift from nursing home care to HCBS on the direct care workforce is not well-understood. For example, home health aide jobs typically have lower compensation and nonstandard hours as compared to direct care worker jobs in institutional settings (Scales, 2020); consequently, the shift toward HCBS may reduce retention of the direct care workforce. Reduced retention among the direct care workforce and growing demand for HCBS may contribute to shortage “hotspots” of home health aides in local labor markets, making it difficult for older adults—and especially older adults in rural are—to obtain HCBS.
This paper has a number of limitations. First and foremost, it is only a descriptive study, and we do not directly measure causes of the differences in ratios of home health aides and nursing assistants relative to the older adult population. The potential causes that we provide in our theoretical model and discussion are post-hoc explanations that need to be directly measured and tested in future research. Second, the direct care workforce serves a much broader population than just older adults, including disabled children and adults who need care. While we think that measuring the ratio of direct care workers relative to the older adult population is a good proxy for need of LTSS and direct care services, understanding the health needs of the broader populations within local labor markets, states, and regions may provide a better context and estimate of the direct care workforce needed to meet the care needs of a population. Further, we are not able to measure the number of adults with limitations in daily activities, which would better reflect demand for HCBS.
Policy implications
Given the demonstrated need for a robust and well-trained direct care workforce to help care for the aging rural population in the US (Galewitz, 2021; Poo & Berger, 2022; Siconolfi et al., 2019), it is vital that policymakers and employers improve infrastructure around HCBS and LTSS through targeted investment in the direct care workforce. One example of a LTSS policy that has been specifically targeted at rural areas is Medicare rural add-on payments to home health agencies serving rural counties, which is intended to strengthen the home health infrastructure in rural areas. Policies like this may increase the size of the rural HCBS workforce (Mroz et al., 2020).
Many states have implemented programs across both rural and urban areas which strive to make the direct care workforce more robust. Some states have utilized wage pass-throughs, which are an additional allocation of funds provided through Medicaid reimbursement for the express purpose of increasing compensation for direct care workers (Baughman & Smith, 2010; Spetz et al., 2019; U.S. Department of Health and Human Services State & Institute for the Future of Aging Services, 2015). Programs that provide free CNA training, job placement, and a retention bonus for workers such as Wisconsin’s WisCaregivers program can remove financial barriers which prevent qualified individuals from becoming direct care workers (WisCaregiver Career Program, 2017). Other states, such as Colorado and North Carolina, have used American Rescue Plan Funds to increase hourly wages or provide hazard pay for direct care workers, and Colorado is working to make this wage increase permanent (North Carolina Department of Health and Human Services, Division of Health Benefits, 2017). In addition to increasing direct care worker wages, it is important to improve critical employment benefits such as health insurance and paid time off. Virginia implemented the Paid Sick Leave for Home Health Workers Act in 2021, which provides paid time off for direct care workers to seek medical treatment for themselves or their families (Article 2.1: Paid Sick Leave, 2021).
Conclusion
The LTSS direct care workforce is in a state of crisis (Campbell et al., 2021; Stone & Wiener, 2016), and this crisis is especially acute in rural areas. This paper demonstrates that rural residents in particular are at risk of lacking access to HCBS because of an insufficient number of home health aides. Most older adults report that they would like to age in place, or receive care in their home as they need more assistance with tasks of daily living (Poo & Berger, 2022). However, older adults in rural areas may struggle to gain access to HCBS if there are not additional supports and policies are put into place to recruit and retain the rural direct care workforce.
Supplementary Material
What this paper adds
This is the first paper to measure the ratio of direct care workers relative to the older adult population in rural and urban areas.
We find that the ratios of home health aides and nursing assistants in rural areas are much lower than in urban areas.
There is substantial regional variation in the ratio of home health aides, indicating that HCBS may be difficult for rural older adults to access in many areas.
Applications of study findings
This study extends past research by demonstrating substantial differences in the capacity of the direct care workforce in rural and urban areas.
These disparities are likely due to many factors, including a lower level of available younger workers to fill direct care positions, lower wages and overall job quality in rural areas, and a lack of long-term care infrastructure to support a direct care workforce.
Future research is needed to directly measure the causes of the low ratio of direct care workers relative to the older adult population in rural areas in order to better understand the supply and demand dynamics of this critical workforce.
Acknowledgments
The authors would like to thank David Van Riper and Jonathan Schroeder.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Support for this study was provided by the Federal Office of Rural Health Policy, Health Resources and Services Administration, Cooperative Agreement U1CRH03717-13-00. The information, conclusions, and opinions expressed are those of the authors, and no endorsement by FORHP, HRSA, or HHS is intended or should be inferred. Additional support was provided by the National Institute on Aging (Grant No. P30AG066613 to Phyllis Moen).
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Review Board Statement
This study is not considered to be human subjects research and was exempted from review by the University of Minnesota Institutional Review Board.
Supplemental Material
Supplemental material for this article is available online.
References
- Anderson TJ, Saman DM, Lipsky MS, & Lutfiyya MN (2015). A cross-sectional study on health differences between rural and non-rural U.S. counties using the County Health Rankings. BMC Health Services Research, 15(1), 441. 10.1186/s12913-015-1053-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Article 2.1: Paid Sick Leave, HB 2137, General Assembly of Virginia, 2021 Special Session I, Code of Virginia (2021). https://lis.virginia.gov/cgi-bin/legp604.exe?212+ful+CHAP0449
- Barnett ML, & Grabowski DC (2020). Nursing homes are ground zero for COVID-19 pandemic. JAMA Health Forum, 1(3), Aticle e200369e200369. 10.1001/jamahealthforum.2020.0369 [DOI] [PubMed] [Google Scholar]
- Baughman RA, & Smith K (2010). The effect of Medicaid wage pass-through programs on the wages of direct care workers. Medical Care, 48(5), 426–432. 10.1097/MLR.0b013e3181d6888a [DOI] [PubMed] [Google Scholar]
- Campbell S, Drake ADR, Espinoza R, & Scales K (2021). Caring for the future: The power and potential of America’s direct care workforce (p. 126). PHI. http://phinational.org/caringforthefuture/
- Chapman SA, Greiman L, Bates T, Wagner LM, Lissau A, Toivanen-Atilla K, & Sage R (2022). Personal care aides: Assessing self-care needs and worker shortages in rural areas. Health Affairs, 41(10), 1403–1412. 10.1377/hlthaff.2022.00483 [DOI] [PubMed] [Google Scholar]
- Dahal A, Skillman S, Patterson D, & Frogner B (2020). What commute patterns can tell us about the supply of allied health workers and registered nurses Center for Health Workforce Studies, Univesity of Washington. https://depts.washington.edu/fammed/chws/wp-content/uploads/sites/5/2020/05/Commute-Patterns-FR-2020.pdf [Google Scholar]
- Federal Reserve Bank of Boston (2019). Aging and declining populations in northern new England: Is there a role for immigration? https://www.bostonfed.org/publications/new-england-public-policy-center-regional-briefs/2019/aging-and-declining-populations-in-northern-new-england.aspx
- Finkelstein A, Gentzkow M, & Williams H (2016). Sources of geographic variation in health care: Evidence from patient migration. The Quarterly Journal of Economics, 131(4), 1681–1726. 10.1093/qje/qjw023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher E, & Skinner J (2013). Making sense of geographic variations. In Health care: The new IOM report | health Affairs 10.1377/hblog20130724.033319/full/ [DOI]
- Flinn B (2020). Nursing home Closures and trends, June 2015–2019. LeadingAge https://leadingage.org/sites/default/files/Nursing%20Home%20Closures%20and%20Trends%202020.pdf
- Friedman EM, Ghosh-Dastidar M, Ruder T, Siconolfi D, & Shih RA (2021). Trends in home care versus nursing home workforce sizes: Are states converging or diverging over time? Health Affairs, 40(12), 1875–1882. 10.1377/hlthaff.2021.00749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galewitz P (2021). June 30). Desperate for home care, seniors often wait months with workers in short supply Kaiser Health News. https://khn.org/news/article/desperate-for-home-care-seniors-often-wait-months-with-workers-in-short-supply/
- Garcia MC, Faul M, Massetti G, Thomas CC, Hong Y, Bauer UE, & Iademarco MF (2017). Reducing potentially excess deaths from the five leading causes of death in the rural United States. MMWR Surveillance Summaries, 66(2), 1–7. 10.15585/mmwr.ss6602a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski DC, & Mor V (2020). Nursing home care in crisis in the wake of COVID-19. JAMA, 324(1), 23–24. 10.1001/jama.2020.8524 [DOI] [PubMed] [Google Scholar]
- Graham J (2017, April 26). Severe shortage of home health workers robs thousands of proper care Kaiser Health News. https://khn.org/news/severe-shortage-of-home-health-workers-robs-thousands-of-proper-care/
- Graham J (2022, February 3). Pandemic-fueled shortages of home health workers strand patients without necessary care Kaiser Health News. https://khn.org/news/article/pandemic-fueled-home-health-care-shortages-strand-patients/
- He Y, & Gokhale J (2022). Projecting medicaid’s long term care expenditures. Penn Wharton Budget Model https://budgetmodel.wharton.upenn.edu/issues/2022/3/9/projecting-medicaids-long-term-care-expenditures
- Health Resources and Services Administration (2010). List of rural counties and designated eligible census tracts in metropolitan counties (p. 86). Health Resources and Services Administration. [Google Scholar]
- Henning-Smith C, Kozhimannil KB, Casey MM, & Prasad S (2018). Beyond clinical complexity: Nonmedical barriers to nursing home care for rural residents. Journal of Aging & Social Policy, 30(2), 109–126. 10.1080/08959420.2018.1430413 [DOI] [PubMed] [Google Scholar]
- Henning-Smith C, Mulcahy J, Lahr M, & Tanem J (2021). Aging in place in rural America: What does it look like and how can it be supported? The University of Minnesota Rural Health Research Center. http://rhrc.umn.edu/project/aging-in-place-in-rural-america-what-does-it-look-like-and-how-can-it-be-supported/
- Johnson RW, Toohey D, & Wiener JM (2007). Meeting the long-term care needs of the baby boomers (p. 61). The Urban Institute. [Google Scholar]
- Karlin NJ (2018). Older adult service usage assessment: Evidence from two rural samples. Activities, Adaptation & Aging, 42(4), 305–327. 10.1080/01924788.2017.1412228 [DOI] [Google Scholar]
- Karon S, Knowles M, Lyda-McDonald B, Thach N, & Wiener J (2019). Final outcome evaluation of the balancing incentive program. Office of the Assistant Secretary for Planning and Evaluation https://aspe.hhs.gov/reports/final-outcome-evaluation-balancing-incentive-program-0
- KFF (2020, February 27). Waiting list enrollment for Medicaid section 1915(c) home and community-based services Waivers KFF. https://www.kff.org/health-reform/state-indicator/waiting-lists-for-hcbs-waivers/ [Google Scholar]
- McAuley WJ, Spector W, & Van Nostrand J (2008). Home health care agency staffing patterns before and after the balanced budget Act of 1997, by rural and urban location. The Journal of Rural Health, 24(1), 12–23. 10.1111/j.1748-0361.2008.00132.x [DOI] [PubMed] [Google Scholar]
- McGarry BE, Porter L, & Grabowski DC (2020). Opinion | Nursing home workers now have the most dangerous jobs in America. They deserve better Washington Post. [Google Scholar]
- Mroz TM, Patterson DG, & Frogner BK (2020). The impact of medicare’s rural add-on payments on supply of home health agencies serving rural counties. Health Affairs, 39(6), 949–957. 10.1377/hlthaff.2019.00952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- North Carolina Department of Health and Human Services, Division of Health Benefits (2017). North Carolina spending plan for the implementation of the American Rescue plan Act of 2021. Section 9817 https://medicaid.ncdhhs.gov/media/9910/open
- Ochieng N, Chidambaram P, & Musumeci M (2022, April 4). Nursing facility staffing shortages during the COVID-19 pandemic KFF. https://www.kff.org/coronavirus-covid-19/issue-brief/nursing-facility-staffing-shortages-during-the-covid-19-pandemic/
- Poo A, & Berger I (2022, March 30). Opinion | many of us want to age at home. But that option is fading fast . The New York Times. https://www.nytimes.com/2022/03/30/opinion/home-care-aides-industry.html
- Richardson I, Slifkin R, Randolph R, & Holmes GM (2010). A rural–urban comparison of allied health professionals’ average hourly wage. Journal of Allied Health, 39(3), 91E–96E. [PubMed] [Google Scholar]
- Scales K (2020). It’s time to care: A detailed profile of America’s direct care workforce—PHI PHI. https://phinational.org/resource/its-time-to-care-a-detailed-profile-of-americas-direct-care-workforce/
- Shanosky N, McDermott D, & Kurani N (2020). How do U.S. healthcare resources compare to other countries? Peterson-KFF Health System Tracker https://www.healthsystemtracker.org/chart-collection/u-s-health-care-resources-compare-countries/
- Siconolfi D, Shih RA, Friedman EM, Kotzias VI, Ahluwalia SC, Phillips JL,& Saliba D (2019). Rural-urban disparities in access to home- and community-based services and supports: Stakeholder perspectives from 14 states. Journal of the American Medical Directors Association, 20(4), 503–508. e1. Scopus 10.1016/j.jamda.2019.01.120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skillman SM, Patterson DG, Couthard C, & Mroz TM (2016). Access to rural home health services: Views from the field (No. 152, p. 19). WWAMI Rural Health Research Center. https://www.ruralhealthresearch.org/publications/1003 [Google Scholar]
- Smith AS, & Trevelyan E (2019). The older population in rural America: 2012–2016. (American Community Survey Reports, p. 21). U.S. Census Bureau. https://www.census.gov/library/publications/2019/acs/acs-41.html
- Spetz J, Stone RI, Chapman SA, & Bryant N (2019). Home and community-based workforce for patients with serious illness requires support to meet growing needs. Health Affairs, 38(6), 902–909. 10.1377/hlthaff.2019.00021 [DOI] [PubMed] [Google Scholar]
- Sterling MR, Cené CW, Ringel JB, Avgar AC, & Kent EE (2022). Rural-urban differences in family and paid caregiving utilization in the United States: Findings from the cornell national social survey. The Journal of Rural Health, 38(4), 689–695. 10.1111/jrh.12664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone RI (2017). Developing a quality direct care workforce: Searching for solutions. Public Policy & Aging Report, 27(3), 96–100. 10.1093/ppar/prx015 [DOI] [Google Scholar]
- Stone RI, & Wiener JM (2016, June 4). Who will care for us? Addressing the long-term care workforce crisis Urban Institute. https://www.urban.org/research/publication/who-will-care-us-addressing-long-term-care-workforce-crisis
- Tuttle C, Tanem J, Lahr M, Schroeder J, Tuttle M, & Henning-Smith C (2020). Rural-urban differences among older adults University of Minnesota Rural Health Research Center. https://rhrc.umn.edu/wp-content/uploads/2020/08/Rural-Urban-Older-Adults_Chartbook_Final_8.25.20.pdf
- Tyler DA, & Fennell ML (2017). Rebalance without the balance: A research note on the availability of community-based services in areas where nursing homes have closed. Research on Aging, 39(5), 597–611. 10.1177/0164027515622244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Bureau of Labor Statistics (2019a). Home health and personal care aides https://www.bls.gov/oes/current/oes311120.htm
- US Bureau of Labor Statistics (2019b). Nursing assistants https://www.bls.gov/oes/current/oes311131.htm
- U.S. Department of Health and Human Services State, & Institute for the Future of Aging Services. (2015, June 13). State wage pass-through legislation: An analysis ASPE. https://aspe.hhs.gov/basic-report/state-wage-pass-through-legislation-analysis [Google Scholar]
- Watts MO, Musumeci M, & Chidambaram P (2021, February 26). State variation in Medicaid LTSS policy choices and implications for upcoming policy debates—issue brief KFF. https://www.kff.org/report-section/state-variation-in-medicaid-ltss-policy-choices-and-implications-for-upcoming-policy-debates-issue-brief/
- Watts MO, Musumeci M, & Chidambaram P (2020). Medicaid home and community-based services enrollment and spending (p. 23). Kaiser Family Foundation. https://collections.nlm.nih.gov/master/borndig/101779106/Issue-Brief-Medicaid-Home-and-Community-Based-Services-Enrollment-and-Spending.pdf
- Wenzlow A, Borck R, Miller D, Doty P, & Drabek J (2013). An investigation of interstate variation in Medicaid long-term care use and expenditures across 40 states in 2006 (p. 86). U.S. Department of Health and Human Services Assistant Secretary for Planning and Evaluation Office of Disability, Aging and Long-Term Care Policy.
- WisCaregiver Career Program. (2017, April 3). Wisconsin Department of Health Services https://www.dhs.wisconsin.gov/caregiver-career/index.htm
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


