Abstract
We identified patient and healthcare system factors related to receipt of screening results and attendance to colposcopy among patients with positive screening results in a cervical cancer screening program in Mexico City, Mexico. We analyzed data from 1,351 patients with high-risk human papillomavirus (HPV)-positive results from two screening demonstration studies conducted between 2017 and 2018. Factors associated with receipt of screening results and with adherence to a colposcopy appointment were identified using multivariable logistic regression. Participants had a median age of 40 years (IQR = 32–48), 60% had less than high school education, and 74% had a previous Pap screening in the last 5 years. Fifty-five percent of participants retrieved their screening results at the healthcare facility (HCF) without any reminder. Providing an email address for contact information, attending a HCF with family medicine, and receiving care from experienced nurses were associated with greater adherence to obtaining screening test results. Fifty-seven percent of participants attended their first scheduled colposcopy appointment. Providing a phone number improved adherence to colposcopy, whereas longer travel times between the HCF and the colposcopy clinic was associated with a decrease in colposcopy adherence. Having a Pap test in the last 5 years was positively associated with better compliance with both outcomes. Securing contact information may help to overcome barriers to future follow-up. Additional research is necessary on strategies for obtaining screening test results and scheduling appointments, which may help address barriers to access, such as limited staff availability, distance from the clinic, and travel costs.
Keywords: Barriers, Facilitating factors, Cervical cancer, Colposcopy, Abnormal screening results, Mexico
1. Introduction
Screening is a key tool for cervical cancer (CC) prevention (Schiffman et al., 2007 Sep 8). Effective screening includes not only the screening test itself but also prompt diagnosis and treatment, if necessary, following abnormal screening results (World Health Organization, 2013). Colposcopic evaluation is a key component of a successful screening program, providing diagnostic confirmation of abnormal screening results (Burness et al., 2020). Current Mexican guidelines call for patients with abnormal cytology results to be referred to colposcopy clinics for diagnostic confirmation and treatment of precursor lesions or cancer care. A robust colposcopy program also facilitates treatment when precancer is detected.
In Mexico, a national CC screening program has existed since the 1970s (Juárez-Vergara and Meza-Banda, 1986). Nonetheless, it has had a limited impact on cancer incidence and mortality (Nacional, 2011, Palacio-Mejía et al., 2009). Significant previous efforts have focused on improving screening, most recently with the introduction of high-risk human papillomavirus (hrHPV) testing (Hurtado-Salgado et al., 2018). However, without high rates of completion over the entire screening and treatment cascade, improved hrHPV test sensitivity will not lead to a significant reduction in CC incidence and mortality. Inadequate colposcopy follow-up is a primary gap in Mexico’s CC prevention program (Lazcano-Ponce et al., 2014, Secretaría de, 2007, Secretaría de, 2019). According to the country's Ministry of Health, only 62.3% of patients with a positive screening result followed up for colposcopy (Secretaría de, 2019).
Colposcopy follow-up rates may depend on individual, family, health system, and community/structural factors (Bosgraaf et al., 2013 Dec, Eggleston et al., 2007, Pritham et al., 2014, Swancutt et al., 2008 Jan, Yabroff et al., 2000 Oct, Zapka et al., 2010, Percac-Lima et al., 2010 Nov). A synthesis of reviews of studies published between 1980 and 2008 highlights non-patient-level factors associated with improved colposcopy adherence, such as an urban setting, greater social support, or favorable perceived social norms (Zapka et al., 2010). Most studies conducted in the United States reported the effects of patient individual characteristics and structural factors on colposcopy follow-up (Carrillo et al., 2021 Jan 6, Hui et al., 2014 Oct, Brooks et al., 2002 Jan, Miller et al., 2017 Jul). Data are scarce regarding colposcopy adherence in Latin American and other low- and middle-income countries (LMICs). Recently, a Brazilian study of patients with positive hrHPV test results showed that younger age and having a negative cytology result were associated with lower colposcopy adherence. In addition, the study found that patients at clinics that provided both screening test and colposcopy services were more likely to attend colposcopy compared to those whose clinics needed to make external referrals for colposcopy (Buss et al., 2021 Jan).
It is important to understand how factors at different contextual levels influence adequate colposcopy follow-up care for abnormal CC screens in Mexico (Torres-Ibarra et al., 2016 Apr, Salmerón et al., 2016 Apr). Identifying barriers and facilitators to colposcopy adherence can inform interventions to improve it.
2. Methods
2.1. Population
Our study population comprised women participating in the Forwarding Research for Improved Detection and Access for CC Screening and Triage (FRIDA) Study and the FASTER-Tlalpan Study (HPV-FASTER is a concept that offers HPV vaccination and screening to patients aged up to 45–50 years) (Bosch et al., 2016 Feb), both previously described (Torres-Ibarra et al., 2016 Apr, Salmerón et al., 2016 Apr). Briefly, these studies aimed to assess different triage strategies for hrHPV-based CC screening as well as a combined prevention strategy including HPV vaccination and hrHPV testing. Both studies were conducted in primary healthcare facilities (HCFs) in Mexico City's Tlalpan Jurisdiction in 2017–2018. Tlalpan is one of the 16 municipalities in Mexico City, with a total population of 699,928 inhabitants, 22% of them ranked in a high and very high degree of marginalization. Indeed, Tlalpan is the second municipality in Mexico City with the greatest inequality and concentrates 4 of the 10 localities with<1,000 inhabitants with a higher degree of social backwardness. The main economic activities are trade and the provision of services. Regarding the health care provision, Tlalpan has 23 Health Centers, all of them under the responsibility of the Mexico City Ministry of Health (de Desarrollo, 2016). In this study we worked with 8 primary health centers (see Appendix for more details about the healthcare facilities). One colposcopy clinic provided medical attention to all participants. The colposcopy clinic was located 3 to 9 miles by car from the various Tlalpan Jurisdiction healthcare centers included in this study. However, almost all users of public health services do not own a car and depend on public transportation. It means that women from the most distant healthcare center of our study must take two separate buses and spend about 1 h and 46 min to reach the colposcopy clinic. (Appendix. Table A1) It is important to note that Tlalpan has an underdeveloped road system, which means that in addition to long transfer times, people -particularly those from more marginalized areas- face insufficient coverage and poor-quality public transportation, restricting users’ mobility needs (Gobierno, 2023).
2.2. Study procedures
Research nurses recruited women aged 25 to 64 years at health facilities during routine medical care visits. During the recruitment visit, all consenting participants (n = 7,103) underwent screening procedures. A pelvic examination was performed to obtain a cervical sample for hrHPV testing. Nurses also administered a questionnaire on sociodemographic, sexual, and reproductive characteristics. At the end of the visit, each participant received a card with a date for when the hrHPV results would be available.
Patients returning to the health center received their hrHPV screening result and counseling from a nurse. For those who did not return, research staff attempted to contact them, to ask them to retutn to their health center. The current analysis includes 1,351 participants who had a positive hrHPV screening result. All women found positive for hrHPV infection were invited to colposcopy evaluation, regardless of the triage results. Nurses explained the need for and usefulness of colposcopy to identify possible lesions and treat them in a timely manner. Along with the result sheet, the nurse provided a sheet with the appointment date for colposcopy.
Patients who attended the colposcopy clinic on the scheduled date received the colposcopy exam and, if indicated, treatment. If a patient missed the appointment, a research staff member phoned to reschedule, offering flexible scheduling options. These studies were approved by the institutional review board of Mexico’s National Institute of Public Health.
2.3. Outcome assessment
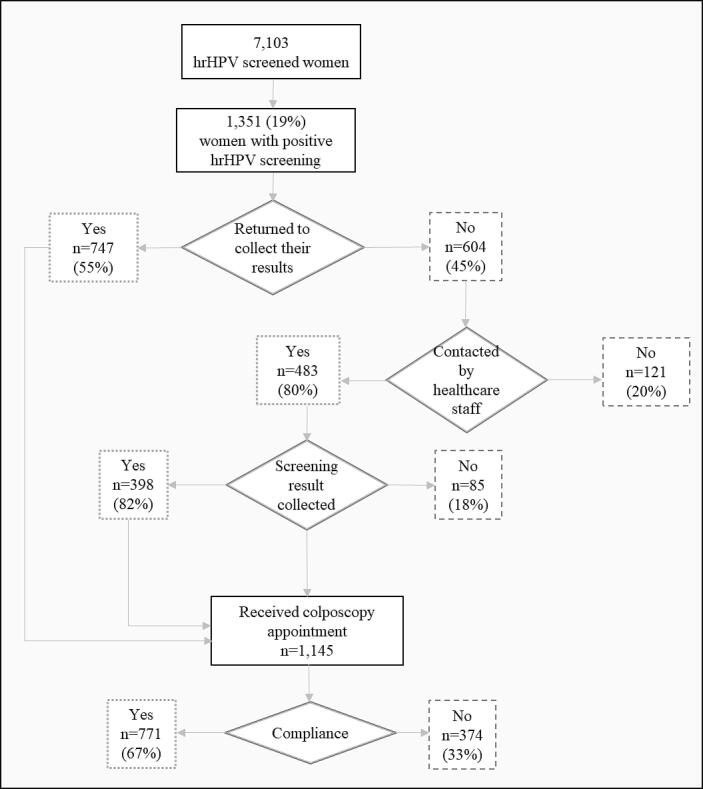
We explored factors associated with adherence to colposcopy as a main outcome. Participants were considered adherent if they attended the first scheduled appointment for colposcopy (Fig. 1). In addition, we examined factors associated with adherence to obtaining screening tests results, defined as returning to the healthcare center to retrieve their initial screening result and their referral to colposcopy, if indicated.
Fig. 1.
Flowchart of colposcopy follow-up after abnormal screening, FRIDA and FASTER-Tlalpan Study, Mexico City.
2.4. Potential predictors
We examined potential barriers and facilitators to colposcopy follow-up based on previously reported factors in other contexts, for example after an abnormal Pap test in developed countries (Bosgraaf et al., 2013 Dec, Eggleston et al., 2007, Pritham et al., 2014, Swancutt et al., 2008 Jan, Yabroff et al., 2000 Oct, Zapka et al., 2010, Percac-Lima et al., 2010 Nov). We included patient’s age (25 to 35 years, 36 to 50 years, and over 50 years), education (primary school or less, secondary school, high school, and university), and employment status (paid vs unpaid work). The variables of providing a cell phone number, a home phone number, and an email address were assessed to evaluate their availability as patient communication methods.
Age at sexual debut was based on the question “How old were you when you had your first sexual intercourse?” We classified responses into the categories of < 18 years and ≥ 18 years. Eighteen is the age of legal adulthood in Mexico. Number of lifetime sexual partners was categorized into < 5 partners and ≥ 5 partners. Gravidity was the total number of times a participant has been pregnant, calculated as the sum of deliveries, caesarean sections, and abortions, and dichotomized as nulligravida or gravida. Based on Mexican screening guidelines, we categorized self-reported previous Pap screening history as never, ≥5 years ago, and < 5 years ago. A participant was defined as having previous treatment for any kind of cervical lesion based on self-report.
To explore characteristics of the HCF of potential relevance to study outcomes, we classified facilities as follows: a) public HCF without family medicine, which were the smallest facilities, operated by a general practitioner and a nurse; b) HCF outside of the public health service system without family medicine, one operated by municipal services and the other by a private university in Mexico City; c) public HCF with family medicine, which are the biggest facilities offering primary healthcare services and which include clinical laboratories and the ability to perform x-ray studies. We treated the three categories as an ordinal scale that assumed increasing quality of care, more health resources, and staff with more training.
We also investigated whether improving the physical infrastructure of the rooms where cervical screening was performed was associated with our outcomes. That included the installation of bathrooms; sinks inside or near the examination rooms; and the presence of gynecological tables, examination rooms, basic equipment, and supplies for the colposcopy clinic.
Travel time between the healthcare center and the colposcopy clinic was estimated as the mean time in minutes required to travel from one to the other. Nursing staff experience was defined as the number of years of service in CC screening programs, including sample collection and counseling related to screening results. In Mexico, nursing students in the last year of the university career must carry out an internship working in clinical practice, mostly in public health services. It is known that the smallest and more distant healthcare facilities are under the responsibility of intern healthcare staff (physicians and nurses). In our study, two types of nurses participated in the cervical cancer screening program: nursing students and registered nurses, the latter of whom had extensive professional experience working with cancer screening programs and even some of them in research projects. Since it has been reported that communication skills -which are key for counselling- are lacking for nursing students (Gardiner and Sheen, 2016 May); (Arranz et al., 2005 Feb) we classified the nursing staff experience as more experienced; otherwise, they were considered less experienced.
2.5. Data analysis
Demographic characteristics, smoking status, and sexual and reproductive health history were presented using summary statistics, with median and interquartile range (IQR) for continuous variables and frequencies and percentages (%) for categorical variables.
Univariate and multivariable logistic regression analyses were performed to identify factors associated with the outcomes. For these analyses, we excluded 12 observations that had missing information in any of the variables included in the analyses, except for the Not applicable category for the variable previous treatment for cervical lesions.
Variables with p-values < 0.20 in the univariate analysis were included in multivariable logistic regression models (Maldonado and Greenland, 1993 Dec 1). For analysis, age, education, smoking status, number of lifetime sexual partners, previous Pap screening, and type of HCF were treated as ordinal variables. We calculated p-values for trend (Wald statistic) with these variables treated as continuous in the models. A two-sided p-value of 0.05 was used to determine statistical significance. Stata 14 software (Stata Corp, Texas, USA) was used for the analysis.
3. Results
In total, 1,351 participants tested positive for hrHPV, with a median age of 40 years (IQR = 32–48). Characteristics of the study population are summarized in Table 1. The majority had a high school education or less (85%), did not have paid work (53%), and were never smokers (56%). Fifty-five percent of our participants reported starting sexual activity at 18 years or older. Most reported having previous experience in the screening program, with only 11% reported never having had a previous Pap.
Table 1.
Characteristics of participants with abnormal screens and of provider/healthcare system, by adherence to cervical cancer screening recommendations (n = 1,351).
|
Returned to the healthcare center to retrieve screening results |
Adherence to recommended colposcopy |
||||
|---|---|---|---|---|---|
| No | Yes | No | Yes | ||
| % (n) | 45% (6 0 4) | 55% (7 4 7) | 43% (5 8 0) | 57% (7 7 1) | |
| Age (years) | |||||
| 25–35 | 37.5% (5 0 6) | 38.9% | 36.3% | 40.0% | 35.5% |
| 36–50 | 44.3% (5 9 9) | 43.7% | 44.8% | 45.3% | 43.6% |
| >50 | 18.2% (2 4 6) | 17.4% | 18.9% | 14.7% | 20.9% |
| Education | |||||
| Primary school or less | 21.9% (2 9 5) | 23.1% | 20.9% | 21.0% | 22.5% |
| Secondary school | 36.6% (4 9 4) | 36.7% | 36.5% | 38.1% | 35.5% |
| High school | 26.3% (3 5 5) | 27.0% | 25.7% | 26.6% | 26.1% |
| University | 15.3% (2 0 6) | 13.3% | 16.9% | 14.3% | 16.0% |
| Paid work | 47.3% (6 3 8) | 46.0% | 48.4% | 47.2% | 47.4% |
| Smoking status | |||||
| Current | 26.7% (3 6 1) | 26.0% | 27.30% | 26.7% | 26.7% |
| Former | 17.4% (2 3 5) | 18.4% | 16.60% | 19.3% | 16.0% |
| Never | 55.9% (7 5 5) | 55.6% | 56.10% | 54.0% | 57.3% |
| Age at sexual debut | |||||
| ≥18 years | 54.9% (7 4 2) | 52.3% | 57.0% | 51.6% | 57.5% |
| Living with a partner | 55.2% (7 4 2) | 53.5% | 56.50% | 53.7% | 56.3% |
| Median number of lifetime sexual partners (IQR) | 3 (2–4) | (2–4) | (2–4) | (2–4) | (2–4) |
| ≥5 | 20.1% (2 7 1) | 19.9% | 20.20% | 21.6% | 19.0% |
| Gravida | 91.6% (1237) | 92.5% | 90.8% | 91.2% | 91.8% |
| Previous Pap screening | |||||
| Never | 11.3% (1 5 3) | 12.7% | 10.2% | 13.8% | 9.5% |
| ≥5 years | 14.2% (1 9 2) | 15.9% | 12.9% | 16.9% | 12.2% |
| <5 years | 74.4% (1005) | 71.4% | 76.9% | 69.3% | 78.3% |
| Previous treatment for cervical lesions | |||||
| No | 75.4% (1019) | 74.2% | 76.40% | 74.5% | 76.1% |
| Yes | 13.3% (1 8 0) | 12.9% | 13.70% | 12.1% | 14.3% |
| Not applicable1 | 11.3% (1 5 2) | 12.9% | 9.90% | 13.4% | 9.6% |
| Provided cell phone number | 90.9% (1228) | 89.7% | 91.80% | 91.6% | 90.4% |
| Provided house phone number | 62.3% (8 4 1) | 60.6% | 63.60% | 58.1% | 65.4% |
| Provided email address | 31.8% (4 2 9) | 27.5% | 35.20% | 32.9% | 30.9% |
| Type of primary HCF | |||||
| Public HCF without family medicine | 27.1% (3 6 6) | 33.9% | 21.6% | 30.3% | 24.6% |
| External HCF (without family medicine) | 26.4% (3 5 6) | 25.7% | 26.9% | 25.9% | 26.7% |
| Public HCF w/ family medicine | 46.6% (6 2 9) | 40.4% | 51.5% | 43.8% | 48.6% |
| Improvements in physical infrastructure2 | 50.8% (6 8 6) | 46.9% | 53.9% | 47.2% | 53.4% |
| Mean travel time (minutes) between HCF and colposcopy clinic (SD) | 79.1 (32.6) | NA | NA | 83.4 (33.2) | 75.9 (31.7) |
| Travel time between HCF and colposcopy clinic (hours) | |||||
| <1 | 17.8% (2 4 1) | NA | NA | 15.7% | 19.5% |
| 1 to < 2 | 52.6% (7 1 1) | NA | NA | 49.5% | 55.0% |
| ≥2 | 29.5% (3 9 9) | NA | NA | 34.8% | 25.6% |
| Nurses' experience3 | |||||
| Less experience | 13% (1 7 5) | 18.0% | 8.8% | 15.2% | 11.3% |
Abbreviations: IQR, Interquartile range; HCF, healthcare facility.
Women who had never had a CC screening and hence had no prior treatment were included in the not applicable category.
Improvements in physical infrastructure means improving the place where the pelvic sample was collected. These improvements included the installation of a bathroom inside the rooms, the presence of a sink inside or near the rooms, and the presence of examination tables or basic supplies at the colposcopy clinic.
Nurses' experience was measured as the number of years of nursing staff experience in cervical cancer screening programs (including sample collection and counseling on screening results). Nursing students were classified as less experienced.
3.1. Compliance to returning to the clinic to obtain screening test results
Among participants with positive hrHPV results, 55% retrieved their results at the primary care center without any reminder (Table 1). Age distribution was similar among those who retrieved and did not retrieve their screening results, and of these groups, 35% and 28%, respectively, had provided an email address.
Seventeen percent of participants who received their screening results had completed a university degree compared to 13% among those who did not receive their results. Among participants who retrieved their results, 52% were screened at a HCF with a family medicine and 8% were screened by less experienced nurses. Among participants who did not retrieve their results, 40.4% were screened in HCFs with family medicine and 19% were screened by less experienced nurses.
We examined the associations of client-, provider-, and HCF factors with obtaining screening tests results. In multivariable analysis (Table 2), compared with patients who had never been screened, those who had had a Pap test in the past 5 years had a 36% higher likelihood of adhering to their appointment for results delivery (Odds Ratio [OR] 1.36; 95% Confidence Interval [CI] 0.96–1.94; p-value for trend = 0.03). Providing a contact email address was also associated with higher adherence (OR 1.35; 95% CI 1.03–1.77). Facilities with more resources, such as those with family medicine (OR 1.54) or those outside the public health service system (OR 1.44) were significantly associated with higher odds of returning for screening results. By contrast, participants receiving care from nurses with less experience were 46% less likely to return for their screening results compared to those who received care from nurses with more experience (95% CI 0.37–0.77). Importantly, participants' sociodemographic and other personal characteristics were not significantly associated with this outcome. Rather, the determinants related to implementation.
Table 2.
Association of participant and provider/healthcare system characteristics with returning to the clinic to retrieve screening test results (n = 1,339).
|
Univariate Model |
Multivariable Model |
|||
|---|---|---|---|---|
| OR (95% CI) | p-value1 | OR (95% CI) | p-value2 | |
| Age (years) | ||||
| 25–35 | 1.0 (Reference) | 0.39 | ||
| 36–50 | 1.09 (0.86–1.38) | |||
| >50 | 1.13 (0.83–1.54) | |||
| Education | ||||
| Primary school or less | 1.0 (Reference) | 0.12 | 1.0 (Reference) | 0.94 |
| Secondary school | 1.14 (0.85–1.52) | 1.13 (0.83–1.52) | ||
| High school | 1.07 (0.78–1.45) | 0.91 (0.64–1.28) | ||
| University | 1.43 (1.00–2.06) | 1.07 (0.71–1.62) | ||
| Paid work | 1.12 (0.90–1.39) | 0.31 | ||
| Smoking status | ||||
| Current | 1.0 (Reference) | 0.84 | ||
| Former | 0.91 (0.65–1.26) | |||
| Never | 0.97 (0.75–1.25) | |||
| Age at sexual debut | ||||
| ≥18 years | 1.19 (0.96–1.48) | 0.11 | 1.11 (0.88–1.39) | 0.37 |
| Living with a partner | 1.14 (0.92–1.41) | 0.25 | ||
| Number of lifetime sexual partners | ||||
| 0–1 | 1.0 (Reference) | 0.69 | ||
| 2 | 1.17 (0.86–1.59) | |||
| 3–4 | 0.94 (0.70–1.27) | |||
| 5–9 | 1.21 (0.84–1.74) | |||
| 10 and more | 0.74 (0.43–1.27) | |||
| Number of pregnancies | 0.96 (0.90–1.03) | 0.24 | ||
| Previous Pap screening | ||||
| Never | 1.0 (Reference) | 0.03 | 1.0 (Reference) | 0.03 |
| ≥5 years | 1.01 (0.66–1.55) | 1.02 (0.65–1.58) | ||
| <5 years | 1.36 (0.96–1.91) | 1.36 (0.96–1.94) | ||
| Previous treatment for cervical lesions | 1.04 (0.75–1.43) | 0.82 | ||
| Provided cell phone number | 1.29 (0.89–1.87) | 0.18 | 1.13 (0.76–1.67) | 0.54 |
| Provided house phone number | 1.15 (0.92–1.43) | 0.23 | ||
| Provided email address | 1.44 (1.14–1.81) | <0.01 | 1.35 (1.03–1.77) | 0.03 |
| Type of primary HCF | ||||
| Public HCF without family medicine | 1.0 (Reference) | <0.01 | 1.0 (Reference) | <0.01 |
| External HCF (without family medicine) | 1.65 (1.23–2.21) | 1.44 (1.03–2.01) | ||
| Public HCF w/ family medicine | 2.01 (1.54–2.61) | 1.54 (1.07–2.21) | ||
| Improvements in physical infrastructure3 | 1.33 (1.07–1.65) | 0.01 | 1.23 (0.86–1.77) | 0.25 |
| Nurses’ experience4 | ||||
| Less experience | 0.44 (0.32–0.61) | <0.001 | 0.54 (0.37–0.77) | <0.01 |
Abbreviations: OR, Odds Ratio; CI, Confidence Interval; HCF, healthcare facility.
p-value is the trend test p-value for all variables except the binary ones.
Bold p-values represent variables with statistical significance p < 0.2 in the univariate analysis, which were included in multivariable logistic regression.
Bold values represent statistically significant associations (p < 0.05).
Improvements in physical infrastructure means improving the place where the pelvic sample was collected. These improvements included the installation of a bathroom inside the rooms, the presence of a sink inside or near the rooms, and the presence of examination tables or basic supplies at the colposcopy clinic.
Nurses' experience was measured as the number of years of nursing staff experience in cervical cancer screening programs (including sample collection and counseling on screening results). Nursing students were classified as less experienced.
3.2. Adherence to colposcopy appointment
Forty-four percent of participants who attended their scheduled colposcopy appointment were 36 to 50 years old. Forty-two percent who attended colposcopy, and 41% of women who did not attend, had a high school degree or higher. Among those who attended colposcopy, 78% had had a Pap screening in the last five years, while 9.5% had never been screened. Among those who did not attend colposcopy, 69.3% and 13.8% had a Pap within five years and never had one, respectively.
In multivariable analysis (Table 3), participants who had had a Pap test within the past 5 years had 59% higher odds of attending their colposcopy appointment compared to those who had never had a Pap test (95% CI 1.10–2.29). Also, those who provided a home phone number had a 27% higher likelihood of attending a colposcopy appointment compared to those who did not have a phone or declined to provide a number (95% CI 1.01–1.59). For every minute increase in estimated travel time between the HCF and colposcopy clinic, the odds of adherence to the colposcopy appointment decreased (OR 0.68; 95% CI 0.49–0.94). Sociodemographic characteristics, provision of an email address, and other personal factors were not independently associated with this outcome.
Table 3.
Association of participant and provider/healthcare system characteristics with adherence to colposcopy (n = 1,339).
|
Univariate Model |
Multivariable Model |
|||
|---|---|---|---|---|
| OR (95% CI) | p-value1 | OR (95% CI) | p-value2 | |
| Age (years) | ||||
| 25–35 | 1.0 (Reference) | 0.01 | 1.0 (Reference) | 0.27 |
| 36–50 | 1.09 (0.86–1.38) | 0.95 (0.74–1.22) | ||
| >50 | 1.60 (1.17–2.20) | 1.29 (0.93–1.81) | ||
| Education | ||||
| Primary school or less | 1.0 (Reference) | 0.75 | ||
| Secondary school | 0.88 (0.66–1.19) | |||
| High school | 0.92 (0.67–1.26) | |||
| University | 1.06 (0.74–1.53) | |||
| Paid work | 1.01 (0.81–1.25) | 0.94 | ||
| Smoking status | ||||
| Current | 1.0 (Reference) | 0.22 | ||
| Former | 0.83 (0.59–1.15) | |||
| Never | 1.07 (0.83–1.38) | |||
| Age at sexual debut | ||||
| ≥18 years | 1.29 (1.03–1.6) | 0.02 | 1.18 (0.94–1.48) | 0.15 |
| Living with a partner | 1.11 (0.89–1.38) | |||
| Number of lifetime sexual partners | ||||
| 0–1 | 1.0 (Reference) | 0.47 | ||
| 2 | 1.12 (0.82–1.53) | |||
| 3–4 | 1.11 (0.82–1.49) | |||
| 5–9 | 1.00 (0.69–1.43) | |||
| 10 and more | 0.70 (0.41–1.20) | |||
| Number of pregnancies | 0.99 (0.93–1.06) | 0.76 | ||
| Previous Pap screening | ||||
| Never | 1.0 (Reference) | <0.001 | 1.0 (Reference) | 0.003 |
| ≥5 years | 1.08 (0.71–1.66) | 1.05 (0.67–1.63) | ||
| <5 years | 1.68 (1.19–2.37) | 1.59 (1.10–2.29) | ||
| Previous treatment for cervical lesions | 1.19 (0.86–1.64) | 0.30 | ||
| Provided cell phone number | 0.89 (0.61–1.3) | 0.53 | ||
| Provided house phone number | 1.35 (1.08–1.68) | 0.01 | 1.27 (1.01–1.59) | 0.04 |
| Provided email address | 0.92 (0.73–1.16) | 0.50 | ||
| Type of primary HCF | ||||
| Public HCF without family medicine | 1.0 (Reference) | 0.03 | 1.0 (Reference) | 0.53 |
| External HCF (without family medicine) | 1.28 (0.95–1.72) | 0.68 (0.37–1.24) | ||
| Public Health w/ family medicine | 1.35 (1.04–1.75) | 0.87 (0.60–1.26) | ||
| Improvements in physical infrastructure3 | 1.26 (1.02–1.57) | 0.03 | 1.12 (0.73–1.70) | 0.61 |
| Travel time (minutes) between HCF and colposcopy clinic | 0.99 (0.98–0.99) | <0.001 | 0.68 (0.49–0.94) | 0.01 |
| Nurses' experience4 | ||||
| Less experience | 0.72 (0.52–0.99) | 0.04 | 0.84 (0.58–1.21) | 0.34 |
Abbreviations: OR, Odds Ratio; CI, Confidence Interval; HCF, healthcare facility.
p-value is the trend test p-value for all variables except the binary ones.
Bold p-values represent variables with statistical significance p < 0.2 in the univariate analysis, which were included in multivariable logistic regression.
Bold values represent statistically significant associations (p < 0.05).
Improvements in physical infrastructure means improving the place where the pelvic sample was collected. These improvements included the installation of a bathroom inside the rooms, the presence of a sink inside or near the rooms, and the presence of examination tables or basic supplies at the colposcopy clinic.
Nurses' experience was measured as the number of years of nursing staff experience in cervical cancer screening programs (including sample collection and counseling on screening results). Nursing students were classified as less experienced.
4. Discussion
Understanding factors associated with adherence to follow-up after positive screens is important for implementing an effective CC screening program. Our study found that, along with individual patient characteristics, factors at other levels (i.e., provider and health system) may act as barriers or facilitators to successful adherence to CC screening follow-up recommendations in a public hrHPV-based CC screening program in Mexico City. We found that having a history of recent CC screening, providing a personal email address as contact information, and being screened in HCFs with greater physical and human resources favored the return of patients to collect their screening results. By contrast, being served by less experienced nurses decreased the likelihood of patients retrieving their results. Our study provides information about factors associated with the first scheduled colposcopy appointment, documenting that having had a previous screening in the last 5 years, providing a house phone number as contact information, and a shorter estimated travel time between the HCF and the colposcopy clinic each increases the likelihood of patients to attend their colposcopy appointment.
Interestingly, our study corroborates that having had prior experience with the CC screening process facilitates adherence to the screening cascade. Participants who had been screened in the last 5 years were more likely to retrieve their results and to attend colposcopy, which can reflect greater familiarity with the procedures and therefore less fear of the unknown. This result agrees with a previous study in women referred for colposcopy in three hospitals in Mexico documenting that first-time visitors report less intention to return to colposcopy as compared to those who had prior visits (de la Campa et al., 2005). Thus, efforts to persuade people to accept CC screening, and follow-up, must include strategies to ensure understanding of all activities and the importance of complying with them (Peterson et al., 2016 Dec). In the case of colorectal cancer (CRC) screening follow up, previous experience with CRC screening predicts adherence to follow-up after an abnormal result (Lo et al., 2015 Feb, Kim et al., 2020 Jan 18). When patients have a more positive initial medical visit, they tend to better recall information and are more likely to adhere to recommendations (Falvo and Tippy, 1988 Jun).
Providing contact information was also significantly associated with a better adherence to both outcomes of our study. In routine practice, nurses and health workers have to reach patients with an abnormal screening result. National guidelines suggest making only one attempt. Previous research has suggested that personalized appointment reminders by telephone, email, or letter, directed counseling by telephone or in-person visits, or registered invitational letters with an allocated appointment time (Khanna and Phillips, 2001), especially in low-income settings, are effective strategies to enhance colposcopy adherence. However, these strategies are not possible if providers lack patients' contact information. It is necessary to strengthen the collecting of contact information, including phone numbers and email addresses, in primary HCFs.
Our results indicate that returning to the clinic to obtain screening test results was also determined by the provider and the health system characteristics. At the provider level, being screened by nurses with more experience in CC favored this activity, which highlights the importance of providers’ abilities to improve CC screening. Paul et al. documented that, in Uganda and Peru, fear of learning the result or fear of positive diagnosis are barriers to screening (Paul et al., 2013). Although we cannot assume that additional years of experience necessarily correspond to better counseling, it has been documented that training on improving communication with patients can improve screening completion (Khanna and Phillips, 2001, Ferreira et al., 2005 Mar 1, Fox et al., 2009 May, Kwan et al., 2012 Jan). Previous research has shown that lack of information and poor understanding of the screening process is one of the main reasons women do not complete screening (Percac-Lima et al., 2010 Nov).
Regarding the healthcare system level, we found that HCF characteristics influence the likelihood that patients will return for screening results. As mentioned earlier, HCFs with family medicine offer a range of medical services, including family physicians, mental health providers, dentists, nutritionists, and laboratories. Thus, patients may return to these facilities for a reason other than screening and take advantage of the visit to collect their results. Additionally, HCFs with family practice physicians emphasize preventive medicine, promoting education for disease prevention. Conversely, other types of HCFs may have only one general practitioner and a nurse and tend to mostly deal with acute conditions. These providers may be overworked and have fewer appointments to offer. A recent study in Mexico City found that healthcare providers' perception of overwork were a barrier to CRC screening (Unger-Saldaña et al., 2020). Another hypothesis is that smaller HCFs are in less populated communities, where it is more likely that people know each other. Previous research has found that women with a positive HPV result can fear stigma and discrimination and experience feelings of shame (Hudon et al., 2011).
Around the organization of the provision of health services, patient-centered care is an approach of great interest. In family medicine, this approach can improve access to care and patient involvement in health promotion and prevention (Zarychanski et al., 2007).
The family physician is the main point of access to preventive services such as immunization and cancer screening in many settings. In Canada, contact with a family physician has been linked to a higher probability of being screened for CRC (Gerend et al., 2017 Feb). In CC screening, in a previous study in the US, most of the women who ever had a Pap test were typically attended by an obstetrician/gynecologist, followed by a family physician, followed by a nurse practitioner. However, guideline recommendation of extending screening interval after an abnormal Pap smear was less likely to be accepted among patients whose Pap was typically performed by an obstetrician/gynecologist or nurse practitioner compared with a family medicine physician (Marcus et al., 1992 Mar).
Access to HCFs is a key determinant for participation in preventive programs. In this study, longer travel times between the primary HCF and the colposcopy clinic reduced the likelihood of attending the colposcopy appointment. This result is similar to that reported by Percac-Lima et al., who studied U.S. Latina women referred to colposcopy after abnormal Pap results (Percac-Lima et al., 2010 Nov). In that study, transportation was a barrier to colposcopy follow-up for a quarter of the participants, and new patients experienced more challenging transportation issues. Patients who live further away from the clinic usually must take more than one bus to get there, which also increases transportation expenses. Cost associated with travel has been recognized as a barrier to attending screening (Percac-Lima et al., 2010 Nov). Since women of low socioeconomic status are the main users of this public program, resolving these access issues should be prioritized to increase adherence to the cancer care continuum. A previous paper found that transportation incentives improve adherence to abnormal smear Pap follow-up among patients who are socioeconomically disadvantaged (Marcus et al., 1992 Mar).
We acknowledge limitations of our study. Data for this analysis comes from information collected in two demonstrative studies aimed to evaluate screening algorithms. Thus, some variables of interest already reported in the literature were not measured, while other measured variables had to serve as proxies for the variables of interest. For instance, we assumed years of nurseś experience was a proxy for the quality of counseling. Despite these limitations, our findings help clarify individual and environmental factors associated with colposcopy follow-up for abnormal CC screens in an urban Mexican population. In fact, a strength of this study is that we were able to analyze the characteristics associated with colposcopy within the CC screening program administered by the Ministry of Health that provides free-of-charge screening services. Although we were not able to address emotional, cultural, or socioeconomic barriers as did some other studies (Eggleston et al., 2007, Pritham et al., 2014, Swancutt et al., 2008 Jan), we included factors beyond the individual level and assessed the impact of some provider- and facility-level characteristics.
5. Conclusions
Adherence to screening and colposcopy protocols for CC depends strongly on factors other than just individual patient level characteristics. Factors associated with follow-up after positive screening included patient’s prior experience with the CC screening, the availability of patient contact information, attendance at a primary HCF with family medicine, and attendance by experienced nurses. Locating colposcopy centers in central places could facilitate access and thus help to increase colposcopy follow-up rates. To our knowledge, no previous studies have examined and/or addressed the factors associated with colposcopy follow-up in Mexican women. We believe our findings help to fill this knowledge gap and illuminate the barriers women face in accessing colposcopy care. By identifying some of the factors that limit colposcopy follow-up among Mexican patients, our results can be used to help build successful strategies adapted to our context.
Funding
This work was supported by the National Council of Science and Technology of Mexico (CONACyT) https://www.conacyt.gob.mx/- FON.INST./261/2016/2016 grant number [274836], by the National Institutes of Health (NIH) grant DP1ES025459 and 1R21CA267900-01A1, and by the Global Health Spark Award from the Yale Institute for Global Health (YIGH).
CRediT authorship contribution statement
Leith León-Maldonado: Conceptualization, Methodology, Investigation, Writing – original draft, Project administration. Raúl U. Hernández-Ramírez: Conceptualization, Methodology, Formal analysis, Writing – review & editing. Leticia Torres-Ibarra: Methodology, Validation, Formal analysis, Writing – original draft, Writing – review & editing. Donna Spiegelman: Methodology, Writing – review & editing, Supervision. Sangini S. Sheth: Methodology, Writing – review & editing. Eduardo Lazcano: Project administration, Funding acquisition, Writing – review & editing. José D. Cadena-Fiscal: Investigation, Resources, Writing – review & editing. Jorge Salmerón: Conceptualization, Methodology, Writing – review & editing, Supervision, Project administration, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would like to thank the healthcare center’s personnel from Tlalpan Jurisdiction of Mexico City for their support of this project. We thank the participants in this study. We also thank local healthcare center’s staff for their work, in particular María de los Ángeles López, Eira Huerta, and Silvia Cardoso.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2023.102347.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
Data will be made available on request.
References
- Arranz P., Ulla S.M., Ramos J.L., Del Rincón C., López-Fando T. Evaluation of a counseling training program for nursing staff. Patient Educ. Couns. 2005 Feb;56(2):233–239. doi: 10.1016/j.pec.2004.02.017. [DOI] [PubMed] [Google Scholar]
- Bosch F.X., Robles C., Díaz M., Arbyn M., Baussano I., Clavel C., Ronco G., Dillner J., Lehtinen M., Petry K.U., Poljak M., Kjaer S.K., Meijer C.J., Garland S.M., Salmerón J., Castellsagué X., Bruni L., de Sanjosé S., Cuzick J. HPV-FASTER: broadening the scope for prevention of HPV-related cancer. Nat. Rev. Clin. Oncol. 2016 Feb;13(2):119–132. doi: 10.1038/nrclinonc.2015.146. [DOI] [PubMed] [Google Scholar]
- Bosgraaf R.P., de Jager W.C., Servaes P., Prins J.B., Massuger L.F., Bekkers R.L. Qualitative insights into the psychological stress before and during colposcopy: a focus group study. J. Psychosom. Obstet. Gynaecol. 2013 Dec;34(4):150–156. doi: 10.3109/0167482X.2013.849688. [DOI] [PubMed] [Google Scholar]
- Brooks S.E., Gordon N.J., Keller S.J., Thomas S.K., Chen T.T., Moses G. Association of knowledge, anxiety, and fear with adherence to follow up for colposcopy. J. Low. Genit. Tract Dis. 2002 Jan;6(1):17–22. doi: 10.1046/j.1526-0976.2002.61004.x. [DOI] [PubMed] [Google Scholar]
- Burness JV, Schroeder JM, Warren JB. Cervical Colposcopy: Indications and Risk Assessment. Am Fam Physician. 2020 Jul 1;102(1):39-48. PMID: 32603071. Review. Available at: https://www.aafp.org/pubs/afp/issues/2020/0701/p39.html. [PubMed]
- Buss L.F., Levi J.E., Longatto-Filho A., Cohen D.D., Cury L., Martins T.R., Fuza L.M., Villa L.L., Eluf-Neto J. Attendance for diagnostic colposcopy among high-risk human papillomavirus positive women in a Brazilian feasibility study. Int. J. Gynaecol. Obstet. 2021 Jan;152(1):72–77. doi: 10.1002/ijgo.13362. [DOI] [PubMed] [Google Scholar]
- Carrillo T., Montealegre J.R., Bracamontes C.G., Scheurer M.E., Follen M., Mulla Z.D. Predictors of timely diagnostic follow-up after an abnormal Pap test among Hispanic women seeking care in El Paso, Texas. BMC Womens Health. 2021 Jan 6;21(1):11. doi: 10.1186/s12905-020-01161-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Programa de Desarrollo de la Delegación Tlalpan 2015-2018. Mexico City, 2016. [accessed June 20, 2023]. Available at: http://repositorio.tlalpan.gob.mx:8080/DGC/7a_LTAIPRC_Art_121_Fr_VII/2016/Tr1/Programa_Delegacional.pdf.
- Madrigal de la Campa Mde L, Lazcano Ponce EC, Infante Castañeda C. Sobreutilización del servicio de colposcopia en México [Overuse of colposcopy service in Mexico]. Ginecol Obstet Mex. 2005 Dec;73(12):637-47. Spanish. [PubMed]
- Eggleston K.S., Coker A.L., Das I.P., Cordray S.T., Luchok K.J. Understanding barriers for adherence to follow-up care for abnormal pap tests. J Womens Health. 2007;16(3):311–330. doi: 10.1089/jwh.2006.0161. [DOI] [PubMed] [Google Scholar]
- Falvo D., Tippy P. Communicating information to patients. Patient satisfaction and adherence as associated with resident skill. J. Fam. Pract. 1988 Jun;26(6):643–647. [PubMed] [Google Scholar]
- Ferreira M.R., Dolan N.C., Fitzgibbon M.L., Davis T.C., Gorby N., Ladewski L., Liu D., Rademaker A.W., Medio F., Schmitt B.P., Bennett C.L. Health care provider-directed intervention to increase colorectal cancer screening among veterans: results of a randomized controlled trial. J. Clin. Oncol. 2005 Mar 1;23(7):1548–1554. doi: 10.1200/JCO.2005.07.049. [DOI] [PubMed] [Google Scholar]
- Fox S.A., Heritage J., Stockdale S.E., Asch S.M., Duan N., Reise S.P. Cancer screening adherence: does physician-patient communication matter? Patient Educ. Couns. 2009 May;75(2):178–184. doi: 10.1016/j.pec.2008.09.010. [DOI] [PubMed] [Google Scholar]
- Gardiner I., Sheen J. Graduate nurse experiences of support: a review. Nurse Educ. Today. 2016 May;40:7–12. doi: 10.1016/j.nedt.2016.01.016. [DOI] [PubMed] [Google Scholar]
- Gerend M.A., Shepherd M.A., Kaltz E.A., Davis W.J., Shepherd J.E. Understanding women's hesitancy to undergo less frequent cervical cancer screening. Prev. Med. 2017 Feb;95:96–102. doi: 10.1016/j.ypmed.2016.11.028. [DOI] [PubMed] [Google Scholar]
- Gobierno de la ciudad de México. Secretaría de Movilidad. Programa integral de Movilidad de la ciudad de México. 2020-2024. Diagnóstico técnico. [accessed June 14, 2023]. Available at: https://semovi.cdmx.gob.mx/storage/app/media/diagnostico-tecnico-de-movilidad-pim.pdf.
- Hudon C., Fortin M., Haggerty J.L., Lambert M., Poitras M.-E. Measuring patients' perceptions of patient-centered care: a systematic review of tools for family medicine. The Annals of Family Medicine. 2011;9(2):155–164. doi: 10.1370/afm.1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hui S.K., Miller S.M., Wen K.Y., Fang Z., Li T., Buzaglo J., Hernandez E. Psychosocial barriers to follow-up adherence after an abnormal cervical cytology test result among low-income, inner-city women. J. Prim. Care Community Health. 2014 Oct;5(4):234–241. doi: 10.1177/2150131914529307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurtado-Salgado E., Ortiz-Panozo E., Salmerón J., Saavedra-Lara N., Kuri-Morales P., Pesqueira-Villegas E., Luna-Gordillo R., Franco E.L., Lazcano-Ponce E. Use of HPV testing in cervical cancer screening services in Mexico, 2008–2018: a nationwide database study. Salud Publica Mex. 2018 Nov-Dic;60(6, nov-dic):722–733. doi: 10.21149/9891. [DOI] [PubMed] [Google Scholar]
- Juárez-Vergara P., Meza-Banda S. Toma de muestras para examen citológico. En: Instituto Mexicano del Seguro Social, Subdirección General Médica. Cáncer cérvicouterino. Histología normal y citología exfoliativa. México: IMSS. 1986 [Google Scholar]
- Khanna N., Phillips M.D. Adherence to care plan in women with abnormal Papanicolaou smears: a review of barriers and interventions. J. Am. Board Fam. Pract. 2001 Mar-Apr;14(2):123–130. [PubMed] [Google Scholar]
- Kim B.C., Kang M., Park E., Shim J.I., Kang S., Lee J., Tchoe H.J., Kong K.A., Kim D.H., Kim Y.J., Choi K.S., Moon C.M. Clinical factors associated with adherence to the follow-up examination after positive fecal occult blood test in national colorectal cancer screening. J. Clin. Med. 2020 Jan 18;9(1):260. doi: 10.3390/jcm9010260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwan T.T., Lo S.S., Tam K.F., Chan K.K., Ngan H.Y. Assessment of knowledge and stigmatizing attitudes related to human papillomavirus among Hong Kong Chinese healthcare providers. Int. J. Gynaecol. Obstet. 2012 Jan;116(1):52–56. doi: 10.1016/j.ijgo.2011.07.035. [DOI] [PubMed] [Google Scholar]
- Lazcano-Ponce E., Lőrincz A.T., Torres L., Salmerón J., Cruz A., Rojas R., Hernández P., Hernández M. Specimen self-collection and HPV DNA screening in a pilot study of 100,242 women. Int. J. Cancer. 2014 Jul 1;135(1):109–116. doi: 10.1002/ijc.28639. [DOI] [PubMed] [Google Scholar]
- Lo S.H., Halloran S., Snowball J., Seaman H., Wardle J., von Wagner C. Colorectal cancer screening uptake over three biennial invitation rounds in the English bowel cancer screening programme. Gut. 2015 Feb;64(2):282–291. doi: 10.1136/gutjnl-2013-306144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maldonado G., Greenland S. Simulation study of confounder-selection strategies. Am. J. Epidemiol. 1993 Dec 1;138(11):923–936. doi: 10.1093/oxfordjournals.aje.a116813. [DOI] [PubMed] [Google Scholar]
- Marcus A.C., Crane L.A., Kaplan C.P., Reading A.E., Savage E., Gunning J., Bernstein G., Berek J.S. Improving adherence to screening follow-up among women with abnormal Pap smears: results from a large clinic-based trial of three intervention strategies. Med. Care. 1992 Mar;30(3):216–230. doi: 10.1097/00005650-199203000-00004. [DOI] [PubMed] [Google Scholar]
- Miller S.M., Tagai E.K., Wen K.Y., Lee M., Hui S.A., Kurtz D., Scarpato J., Hernandez E. Predictors of adherence to follow-up recommendations after an abnormal Pap smear among underserved inner-city women. Patient Educ. Couns. 2017 Jul;100(7):1353–1359. doi: 10.1016/j.pec.2017.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Instituto Nacional de Salud Pública. Evaluación del programa de Prevención y Control del Cáncer Cervical en México, 2008-2011. Problemas y Recomendaciones Cuernavaca: INSP, 2011. [accessed November 27, 2022]. Available at: https://www.insp.mx/images/stories/Centros/cisp/Docs/120412_cneg.pdf.
- Palacio-Mejía LS, Lazcano-Ponce E, Allen-Leigh B, Hernández-Avila M. Diferencias regionales en la mortalidad por cáncer de mama y cérvix en México entre 1979 y 2006 [Regional differences in breast and cervical cancer mortality in Mexico between 1979-2006]. Salud Publica Mex. 2009;51 Suppl 2:s208-19. Spanish. doi: 10.1590/s0036-36342009000800011. [DOI] [PubMed]
- Paul P., Winkler J.L., Bartolini R.M., Penny M.E., Huong T.T., Nga le T., Kumakech E., Mugisha E., Jeronimo J. Screen-and-treat approach to cervical cancer prevention using visual inspection with acetic acid and cryotherapy: experiences, perceptions, and beliefs from demonstration projects in Peru, Uganda, and Vietnam. Oncologist. 2013;18(12):1278–1284. doi: 10.1634/theoncologist.2013-0253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Percac-Lima S., Aldrich L.S., Gamba G.B., Bearse A.M., Atlas S.J. Barriers to follow-up of an abnormal Pap smear in Latina women referred for colposcopy. J. Gen. Intern. Med. 2010 Nov;25(11):1198–1204. doi: 10.1007/s11606-010-1450-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson E.B., Ostroff J.S., DuHamel K.N., D'Agostino T.A., Hernandez M., Canzona M.R., Bylund C.L. Impact of provider-patient communication on cancer screening adherence: A systematic review. Prev. Med. 2016 Dec;93:96–105. doi: 10.1016/j.ypmed.2016.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pritham U.A., Brigdon A., Jones M. Understanding factors related to women's adherence to colposcopy. Nurs. Womens Health. 2014;18(5):402–412. doi: 10.1111/1751-486X.12148. [DOI] [PubMed] [Google Scholar]
- Salmerón J., Torres-Ibarra L., Bosch F.X., Cuzick J., Lörincz A., Wheeler C.M., Castle P.E., Robles C., Lazcano-Ponce E. HPV vaccination impact on a cervical cancer screening program: methods of the FASTER-Tlalpan Study in Mexico. Salud Publica Mex. 2016 Apr;58(2):211–219. doi: 10.21149/spm.v58i2.7790. [DOI] [PubMed] [Google Scholar]
- Schiffman M., Castle P.E., Jeronimo J., Rodriguez A.C., Wacholder S. Human papillomavirus and cervical cancer. Lancet. 2007 Sep 8;370(9590):890–907. doi: 10.1016/S0140-6736(07)61416-0. [DOI] [PubMed] [Google Scholar]
- Secretaría de Salud. Dirección General de Epidemiología. Boletines Históricos Caminando a la Excelencia. Boletines 2007 a 2018 [accessed November 27, 2022]. Available at: https://www.gob.mx/salud/acciones-y-programas/boletines-historicos-caminando-a-la-excelencia.
- Secretaría de Salud. Dirección General de Epidemiología. Boletín Caminando a la Excelencia Cierre 2019 [accessed November 27, 2022]. Available at: https://epidemiologia.salud.gob.mx/gobmx/salud/documentos/bol_camexc/2019/BOLETIN%20CIERRE2019.pdf.
- Swancutt D.R., Greenfield S.M., Wilson S. Women's colposcopy experience and preferences: a mixed methods study. BMC Womens Health. 2008 Jan;14(8):2. doi: 10.1186/1472-6874-8-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres-Ibarra L., Lazcano-Ponce E., Franco E.L., Cuzick J., Hernández-Ávila M., Lorincz A., Rivera B., Ramírez P., Mendiola-Pastrana I., Rudolph S.E., León-Maldonado L., Hernández R., Barrios E., Gravitt P., Moscicki A.B., Schmeler K.M., Flores Y.N., Méndez-Hernández P., Salmerón J. FRIDA Study Group. Triage strategies in cervical cancer detection in Mexico: methods of the FRIDA Study. Salud Publica Mex. 2016 Apr;58(2):197–210. doi: 10.21149/spm.v58i2.7789. [DOI] [PubMed] [Google Scholar]
- Unger-Saldaña K., Saldaña-Tellez M., Potter M.B., et al. Barriers and facilitators for colorectal cancer screening in a low-income urban community in Mexico City. Implement. Sci. Commun. 2020;1:64. doi: 10.1186/s43058-020-00055-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Sexual and reproductive health. Guidelines for screening and treatment of precancerous lesions for cervical cancer prevention WHO guidelines. 2013. [accessed December 12, 2022]. Available at: https://apps.who.int/iris/handle/10665/94830. [PubMed]
- Yabroff K.R., Kerner J.F., Mandelblatt J.S. Effectiveness of interventions to improve follow-up after abnormal cervical cancer screening. Prev. Med. 2000 Oct;31(4):429–439. doi: 10.1006/pmed.2000.0722. [DOI] [PubMed] [Google Scholar]
- Zapka J., Taplin S.H., Price R.A., Cranos C., Yabroff R. Factors in quality care–the case of follow-up to abnormal cancer screening tests–problems in the steps and interfaces of care. J. Natl. Cancer Inst. Monogr. 2010;2010(40):58–71. doi: 10.1093/jncimonographs/lgq009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarychanski R., Chen Y., Bernstein C.N., Hébert P.C. Frequency of colorectal cancer screening and the impact of family physicians on screening behaviour. CMAJ. 2007;177(6):593–597. doi: 10.1503/cmaj.070558. [DOI] [PMC free article] [PubMed] [Google Scholar]
Further reading
- Secretaria de Salud Programa de Acción Específico. Prevención y control del cáncer de la mujer 2013–2018. México: Secretaría de Salud. 2013 Programa sectorial de salud. [Google Scholar]
- Song M, Zhou X, Pazaris M, Spiegelman D. The missing covariate indicator method is nearly valid almost always. Preprint. Posted online October 30, 2021. ArXiv:211100138. doi: 10.48550/arXiv.2111.00138.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.