Abstract
In the United States, HIV infection disproportionately affects young gay, bisexual, and other men who have sex with men, aged 13–24 years (collectively referred to as YMSM), specifically black YMSM. Knowledge of HIV status is the first step for timely and essential prevention and treatment services. Because YMSM are disproportionately affected by HIV, the number of CDC-funded HIV testing events, overall and newly diagnosed HIV positivity, and linkage to HIV medical care among YMSM in non-health care settings were examined from 61 health department jurisdictions. Differences by age and race/ethnicity were analyzed. Additionally, trends in number of HIV testing events and newly diagnosed HIV positivity were examined from 2011 to 2015. In 2015, 42,184 testing events were conducted among YMSM in non-health care settings; this represents only 6% of tests in non-health care settings. Overall and newly diagnosed HIV positivity was 2.8% and 2.1%, respectively, with black/African–American YMSM being disproportionately affected (5.6% for overall; 4% for newly diagnosed); 71% of YMSM were linked within 90 days. The newly diagnosed HIV positivity among YMSM decreased from 2.8% in 2011 to 2.4% in 2015, and the number of newly diagnosed YMSM also decreased. Further targeted testing efforts among YMSM are needed to identify undiagnosed YMSM, specifically black YMSM.
Keywords: HIV, testing, diagnoses, young men who have sex with men, linkage
Introduction
In the United States, gay, bisexual, and other men who have sex with men (referred to as MSM) account for approximately 2% of the population but accounted for 63% of all new HIV infections in 2010 (Centers for Disease Control and Prevention, 2012; Purcell et al., 2012). Young MSM (YMSM), aged 13–24 years, are disproportionately affected by HIV, specifically black YMSM. From 2005 to 2014, HIV diagnoses increased 22% and 24% among black and Hispanic/Latino YMSM, respectively. However, diagnoses from 2010 to 2014 have stabilized among black and white YMSM, while increases continue among Hispanic/Latino YMSM (Centers for Disease Control and Prevention, 2016b). Because YMSM are at disproportionate risk, it is recommended that HIV testing and prevention efforts be expanded for YMSM (Holtgrave, 2015).
Persons unaware of their HIV infection do not receive timely HIV medical care or prevention services and may engage in behaviors that can result in HIV transmission. Therefore, knowledge of status and linkage to care for HIV-positive persons are essential prevention strategies. A previous paper on CDC-funded testing found that in 2013, newly diagnosed HIV positivity was 2.4% among MSM in non-health care settings (Seth, Wang, Collins, & Belcher, 2015). However, YMSM were not specifically examined. Because YMSM are disproportionately affected by HIV, this paper describes number of CDC-funded HIV testing events (i.e. HIV testing), HIV positivity, and linkage among YMSM tested in non-health care settings in 2015. Differences in HIV positivity and newly diagnosed HIV positivity by age and race/ethnicity are analyzed. Finally, trends in HIV testing and newly diagnosed HIV positivity from 2011 to 2015 are examined.
Methods
Data source
CDC funds 61 health department jurisdictions, which include the 50 states, District of Columbia, Puerto Rico, US Virgin Islands, and 8 directly funded city/county health departments, to provide HIV testing and other prevention activities. De-identified data are submitted to CDC bi-annually via a secure, online CDC-supported National HIV Monitoring and Evaluation (NHM&E) system. This effort is considered a program evaluation activity by CDC; therefore, IRB approval was not required. The Office of Management and Budget approved this activity.
Measures
Demographics and setting
Data on age, race/ethnicity, and test setting were examined. Only data on white, black, and Hispanic/Latino YMSM are presented; other racial/ethnic groups were not examined due to small sample size. Also, only data from non-health care settings are presented. For target populations (e.g. MSM, defined as male-to-male sexual contact during the past 12 months), CDC requires data for all HIV testing events in non-health care settings but only for HIV-positive testing events in health care settings. A non-health care setting does not provide both medical diagnostic and treatment services (e.g. community settings).
HIV testing events
HIV testing events included all NHM&E HIV testing records for which a test result was reported. A single testing event could include multiple tests administered to the same person in order to make a final determination of the test result.
HIV positivity
HIV positivity is defined as the proportion of YMSM who were tested and received an HIV-positive result during the current testing event. Newly diagnosed YMSM included those who tested HIV positive during the current testing event but were not previously reported to the health department’s HIV surveillance system (37 grantees matched more than 80% of their records against surveillance data). Self-report data were used for grantees that did not or were unable to verify prior test result due to specific policies within their jurisdiction.
Linkage to HIV medical care
Linkage was defined as attendance at first medical appointment within 90 days and was examined for all newly diagnosed YMSM. Grantees collect these data in various ways, including self-report, medical records, surveillance, or program data.
Data analysis plan
Descriptive statistics examined 2015 HIV testing, overall and newly diagnosed HIV positivity, and linkage among YMSM by age and race/ethnicity. Log binominal regression analysis assessed differences across demographic characteristics. Finally, estimated annual percent change (EAPC) analyses examined trends in HIV testing and newly diagnosed HIV positivity from 2011 to 2015.
Results
HIV testing events
In 2015, 703,374 CDC-funded HIV testing events were conducted in non-health care settings. Of those, 153,378 (21.8%) were among MSM, and 42,184 (6.0%) were among YMSM. The largest percentage of testing events conducted in non-health care settings was among heterosexuals (44.7%). The majority of testing events among YMSM were among those aged 18–24 years (96.9%). Of testing events among YMSM, 30.7% were among white, 30.2% among black, and 28.7% among Hispanic/Latino YMSM (Table 1).
Table 1.
CDC-funded HIV testing and linkage to HIV medical care among YMSM, aged 13–24 years, in non-health care settings, 2015.
| Demographic characteristics | HIV testing eventsa | HIV-positive YMSM | Newly diagnosed HIV-positive YMSMb | Linkage to HIV medical care within 90 daysc | ||
|---|---|---|---|---|---|---|
| N (column %) | N (row %) | PR (95% CI) | N (row %) | PR (95% CI) | N (row %) | |
| Age groupsd | ||||||
| 13–17 years | 1325 (3.1) | 23 (1.7) | 0.49 (0.33−0.75) | 18 (1.3) | 0.52 (0.3−0.84) | 13 (72.2) |
| 18–24 years | 40,859 (96.9) | 1168 (2.9) | Referent | 865 (2.1) | Referent | 614 (71.0) |
| Race/ethnicity | ||||||
| White | 12,955 (30.7) | 175 (1.4) | 0.24 (0.20−0.28) | 133 (1.0) | 0.25 (0.21−0.31) | 101 (75.9) |
| Black/African-American | 12,737 (30.2) | 707 (5.6) | Referent | 511 (4.0) | Referent | 343 (67.1) |
| Hispanic/Latino | 12,091 (28.7) | 253 (2.1) | 0.37 (0.32−0.43) | 196 (1.6) | 0.40 (0.34−0.47) | 154 (78.6) |
| Total (all MSM 13–24 years)d | 42,184 | 1191 (2.8) | 883 (2.1) | 627 (71.0) | ||
HIV testing events were defined as tests for which a test result was reported.
YMSM who tested HIV-positive but did not report a previous positive test result and/or who had not been reported to a state’s surveillance system were categorized as newly diagnosed HIV-positive persons.
The denominator for the percentages for linkage is newly diagnosed HIV-positive YMSM.
Includes YMSM of all racial/ethnic backgrounds.
Overall HIV positivity
In 2015, 1191 (2.8%) YMSM tested HIV positive in non-health care settings. YMSM aged 18–24 years had a significantly higher HIV positivity percentage (2.9%) than YMSM aged 13–17 years (1.7%). Additionally, black YMSM had a significantly higher positivity percentage (5.6%) than Hispanic/Latino (2.1%) and white (1.4%) YMSM (Table 1).
Newly diagnosed HIV positivity
In 2015, 883 (2.1%) YMSM were newly diagnosed in non-health care settings, which was 74.1% of YMSM who tested positive. YMSM aged 18–24 years (2.1%) had a significantly higher percentage of new diagnoses than YMSM aged 13–17 years (1.3%). Additionally, black YMSM had a significantly higher percentage of new diagnoses (4.0%) than Hispanic/Latino (1.6%) and white (1.0%) YMSM (Table 1).
Linkage to HIV medical care
Seventy-one percent of newly diagnosed YMSM were linked within 90 days. Linkage by age group was 72.2% and 71.0% for YMSM aged 13–17 and 18–24 years, respectively. By race/ethnicity, linkage ranged from 67.1% (blacks) to 78.6% (Hispanics/Latinos) (Table 1).
HIV testing and HIV positivity from 2011 to 2014
From 2011 to 2015, the number of HIV testing events among YMSM significantly increased by an EAPC of 3.1% (95% CI: 2.8, 3.4). However, the percentage of newly diagnosed YMSM significantly decreased by an EAPC of 4.9% (95% CI: 3.1, 6.7) from 2011 to 2015 (Figure 1).
Figure 1.
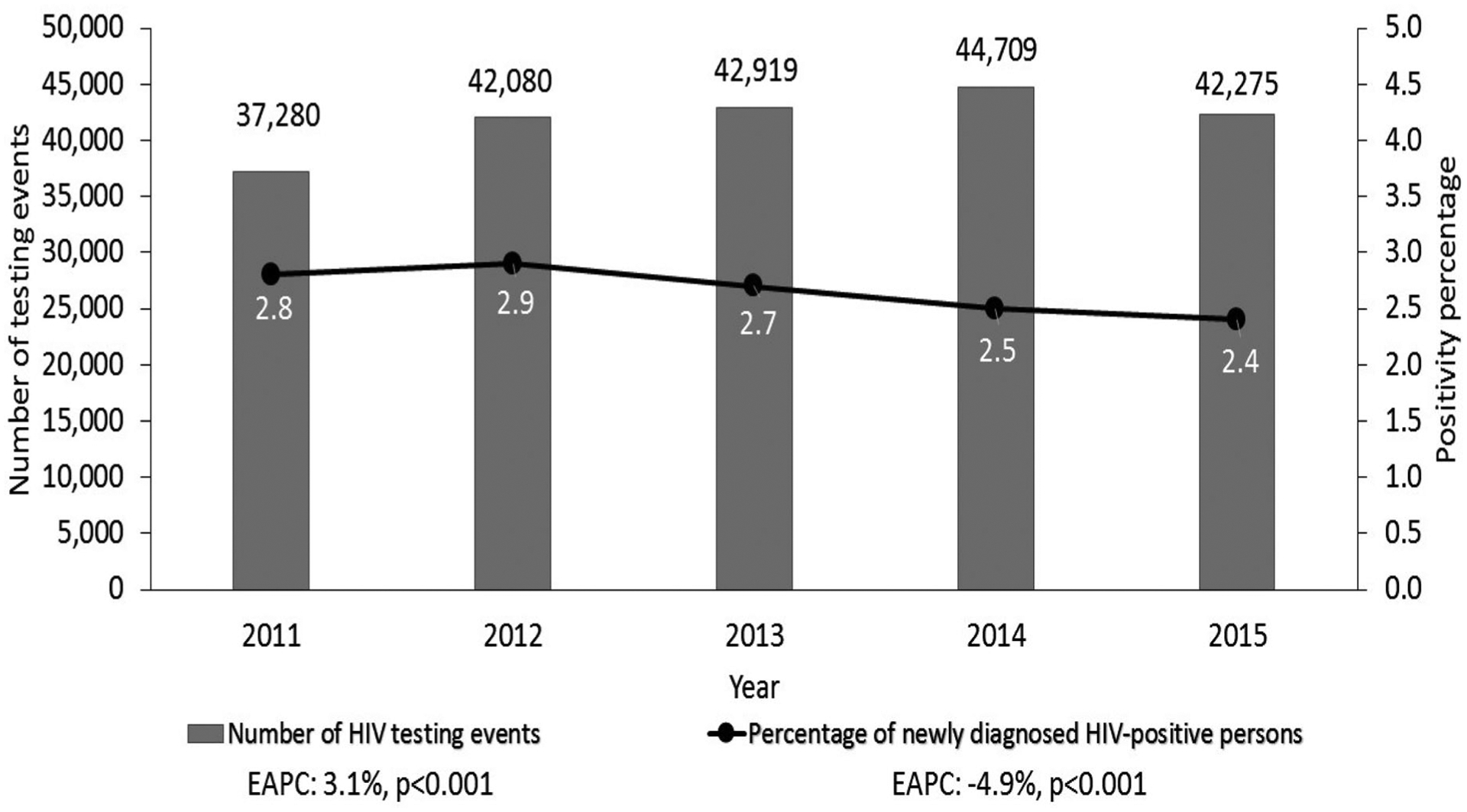
HIV testing events and percentages of HIV positivity and newly diagnosed YMSM, aged 13–24 years, in non-health care settings, 2011–2015.
Note: Number of newly diagnosed YMSM were 1058 in 2011, 1198 in 2012, 1136 in 2013, 1116 in 2014, and 997 in 2015. Prior to 2014, HIV testing events were defined as records having data on test technology or a test result. In the 2015 data, HIV testing events are defined as records having data on test result. The old definition was used for trends to have a consistent definition of HIV testing events across all years.
Discussion
In 2015, MSM accounted for 21.9% of CDC-funded HIV testing events in non-health care settings, and YMSM accounted for only 6%. Among YMSM tested in non-health care settings, those aged 18–24 years represented the majority of testing events (96.9%) and had a higher overall and newly diagnosed HIV positivity than those aged 13–17 years. Additionally, black YMSM had higher overall and newly diagnosed HIV positivity than other racial/ethnic groups. When examining 2014 HIV surveillance data (Centers for Disease Control and Prevention, 2015), 11% of all new diagnoses among YMSM appear to be diagnosed through CDC-funded testing in non-health care settings. In 2014, an overall HIV positivity of 0.9% and newly diagnosed HIV positivity of 0.4% among CDC-funded grantees was reported in all settings (Centers for Disease Control and Prevention, 2016a). Current findings revealed an overall and newly diagnosed positivity of 2.8% and 2.1%, respectively, among YMSM in non-health care settings. These percentages were even higher among black YMSM (5.6% and 4%, respectively).
According to trends, the number and percentage of newly diagnosed YMSM has been decreasing in CDC-funded testing programs. This is consistent with decreasing trends in surveillance data, which could indicate decreasing incidence and/or frequent testing (Centers for Disease Control and Prevention, 2016b). One goal of the National HIV/AIDS Strategy (NHAS) (White House Office of National AIDS Policy, 2015) is to reduce disparities in the rate of new diagnoses by at least 15% among MSM and black YMSM. Additionally, although linkage percentages have been increasing since 2012 (Centers for Disease Control and Prevention, 2014, 2016a), improvements are needed to increase linkage. The current linkage percentages fall far below the goals set by NHAS (White House Office of National AIDS Policy, 2010, 2015) of having 85% of newly diagnosed persons linked to HIV medical care within 90 days by 2015 and within 30 days by 2020.
There are limitations. Data are limited to CDC-funded HIV testing events in non-health care settings (~30%). Data to define MSM are only required for all persons tested in non-health care settings. The true number of CDC-funded testing events and HIV positivity among YMSM cannot be determined; thus, findings may not be generalizable. Because of client privacy protections, non-health care settings are not always able to determine if an HIV-positive client was linked, resulting in missing data. Trend analyses do not take into account demographic changes in the population over time. Finally, some new diagnoses were based on self-report for health departments unable to verify from surveillance, which may result in socially desirable responses.
YMSM are at higher risk for HIV infection in the United States. Targeted testing efforts are needed to identify undiagnosed YMSM in non-health care settings, as only 6% of all CDC-funded tests being conducted in these settings are among YMSM. Although HIV testing has increased among MSM, improvements are needed to meet CDC recommendations, specifically annual testing among sexually active MSM (Cooley et al., 2014). However, in addition to targeted testing approaches to ensure knowledge of status, it is necessary to improve linkage to HIV medical care, other essential prevention services, and retention in care. Programs should also be aware of any existing barriers and challenges that may impact success along each step of the continuum of care in order to ensure early initiation of treatment and retention to care for better health outcomes (Balaji, Bowles, Le, Paz-Bailey, & Oster, 2013; Oster et al., 2014; Sifakis et al., 2007).
Acknowledgements
The authors would like to acknowledge the Prevention Program Branch at the Centers for Disease Control and Prevention for monitoring of the HIV testing programs. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Balaji AB, Bowles KE, Le BC, Paz-Bailey G, Oster AM, & NHBS Study Group. (2013). High HIV incidence and prevalence and associated factors among young MSM, 2008. AIDS, 27, 269–278. doi: 10.1097/QAD.0b013e32835ad489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2012). Estimated HIV incidence in the United States, 2007–2010. HIV Surveillance Supplemental Report, 17(4). Retrieved from http://www.cdc.gov/hiv/pdf/statistics_hssr_vol_17_no_4.pdf [Google Scholar]
- Centers for Disease Control and Prevention. (2014). CDC-funded HIV testing: United States, Puerto Rico, and the U.S. Virgin Islands, 2012 Retrieved from http://www.cdc.gov/hiv/pdf/2012_HIV_Testing_Report_01-29-15.pdf
- Centers for Disease Control and Prevention. (2015). Diagnosis of HIV infection in the United States and dependent areas, 2014. Retrieved from http://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-us.pdf
- Centers for Disease Control and Prevention. (2016a). CDC-funded HIV testing: United, States, Puerto Rico and the U.S. Virgin Islands, 2014 Retrieved from http://www.cdc.gov/hiv/library/reports/index.html
- Centers for Disease Control and Prevention. (2016b). Trends in U.S. HIV Diagnoses, 2005–2014 Retrieved from http://www.cdc.gov/nchhstp/newsroom/docs/factsheets/hiv-data-trends-fact-sheet-508.pdf
- Cooley LA, Oster AM, Rose CE, Wejnert C, Le BC, Paz-Bailey G, & NHBS Study Group. (2014). Increases in HIV testing among men who have sex with men--National HIV Behavioral Surveillance System, 20 U.S. Metropolitan Statistical Areas, 2008 and 2011. Plos One, 9(9), e104162. doi: 10.1371/journal.pone.0104162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtgrave DR (2015). Achieving and advancing the goals of the national HIV/AIDS strategy for the United States. AIDS and Behavior, 19, 211–213. doi: 10.1007/s10461-014-0903-z [DOI] [PubMed] [Google Scholar]
- Oster AM, Johnson CH, Le BC, Balaji AB, Finlayson TJ, Lansky A, … Paz-Bailey G (2014). Trends in HIV prevalence and HIV testing among young MSM: five United States cities, 1994–2011. AIDS and Behavior, 18 (Suppl. 3), S237–S247. doi: 10.1007/s10461-013-0566-1 [DOI] [PubMed] [Google Scholar]
- Purcell DW, Johnson CH, Lansky A, Prejean J, Stein R, Denning P, … Crepaz N (2012). Estimating the population size of men who have sex with men in the United States to obtain HIV and syphilis rates. The Open AIDS Journal, 6, 98–107. doi: 10.2174/1874613601206010098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seth P, Wang G, Collins NT, & Belcher L (2015). Identifying new positives and linkage to HIV medical care - 23 testing site types, United States, 2013. MMWR Morbidity and Mortality Weekly Report, 64(24), 663–667. [PMC free article] [PubMed] [Google Scholar]
- Sifakis F, Hylton JB, Flynn C, Solomon L, Mackellar DA, Valleroy LA, & Celentano DD (2007). Racial disparities in HIV incidence among young men who have sex with men: The Baltimore Young Men’s Survey. Journal of Acquired Immune Deficiency Syndromes, 46, 343–348. doi: 10.1097/QAI.0b013e31815724cc [DOI] [PubMed] [Google Scholar]
- White House Office of National AIDS Policy. (2010). National HIV/AIDS strategy for the United States. Retrieved from http://www.whitehouse.gov/sites/default/files/uploads/NHAS.pdf
- White House Office of National AIDS Policy. (2015). The National HIV/AIDS Strategy for the United States: Updated to 2020. Retrieved from https://www.aids.gov/federal-resources/national-hiv-aids-strategy/nhas-update.pdf


