Highlights
-
•
COVID19 vaccine uptake among people who inject drugs (PWID) is low.
-
•
We identified older age and housing stability as predictors of vaccine uptake.
-
•
The social barriers to vaccination for PWID extend beyond existing models of vaccine hesitancy.
-
•
Barriers include competing demands for survival, government mistrust, and the need for accessible, accurate information.
Keywords: COVID-19, People Who Inject Drugs, Vaccination, Vaccine deliberation, Substance use, Health behaviors, Mixed-methods
Abstract
The objectives of this study were to 1) identify vaccination rates among PWID in Oregon at a time when vaccines were easily accessible, 2) quantitatively identify convergence with demographic correlates of vaccination willingness and uptake to promote generalizability, and 3) explore the factors PWID were considering when deciding whether or not to receive the COVID-19 vaccine. We conducted a mixed-methods study design including 260 quantitative surveys and 41 in-depth qualitative interviews with PWID, conducted July - September 2021 at syringe services programs in Lane County, Oregon. Among the 260 survey respondents, 37.3% indicated that they had received a COVID-19 vaccine by October 1, 2021. In the same period, an estimated 70.1% of the total Lane County population had completed their COVID-19 vaccinations (not including booster rounds). We explored alignment with the WHO’s 3C model of vaccine hesitancy and identified, instead, five common factors as key motivators for vaccine decisions: confidence, convenience, concern, communication, and community implications among PWID. Interviews with PWID describe systemic barriers which prevented them from accessing healthcare resources. We highlight that our proposed 5C model may more accurately depict how PWID navigate vaccine decisions by incorporating the ways that social inequities, infrastructural barriers, and community values influence an individual’s vaccine deliberation.
1. Introduction
During the second year of the COVID-19 pandemic (2021), vaccination was the primary public health intervention used to reduce morbidity. People who inject drugs (PWID) were a priority population for vaccination as they experience structural, social, and health disparities putting them at greater risk for communicable disease (Biancarelli et al., 2019, Braun and Clarke, 2006, Campbell et al., 2007, Centers for Disease Control and Prevention, 2018). Problematically, efforts fell short; PWID in the United States were over represented in the number of COVID-19 cases, breakthrough infections, and deaths (Abadie et al., 2018, Abadie et al., 2021). The World Health Organization's (WHO) ‘3Cs’ 2014 model seeks to describe how individuals make vaccine decisions (Aiken et al., 1991) including: 1) confidence — an individual’s level of trust or distrust in the people providing the vaccine or the vaccine itself; 2) convenience — how easily an individual can get vaccinated, and 3) complacency — an individual’s desire to seek out a vaccine. Even before the COVID-19 pandemic, psychology and public health experts argued that the 3C model excluded important social contextual factors, such as the presence of racism, misinformation, and collective responsibility (Biancarelli et al., 2019, Braun and Clarke, 2006). Given these critiques, this 3C model may not fully characterize the experiences of marginalized populations such as PWID. Our goal was to use a mixed-methods approach to center the voices of PWID and identify whether there was a need for improvements to the WHO's model to better represent the COVID-19 decision making process for this population. The self-identified motivations and barriers affecting COVID-19 vaccination among PWID have not previously been identified though qualitative work.
Prior literature on COVID-19 vaccine uptake, deliberation, and hesitancy has used quantitative data to describe vaccine deliberation among PWID. Even when vaccines were widely available in the United States, many PWID struggled to access vaccine services, were concerned about the vaccine's safety and efficacy, and often did not have accurate knowledge of the benefits and risks associated with vaccination (Campbell et al., 2007, Centers for Disease Control and Prevention, 2018, Cioffi et al., 2022a, Cioffi et al., 2022b, Cohen et al., 2013). Research at the United States-Mexico border in 2020–2021 indicated that approximately one third of PWID were unwilling or unsure of whether to receive the COVID-19 vaccine. Being unwilling or unsure about vaccination was associated with greater exposure to social media, disinformation, and the presence of co-morbidities; it was also inversely associated with food security and high perceived threat of COVID-19 (Cioffi et al., 2022b). Exposure to false information and lack of health insurance were associated with lower vaccine uptake, whereas past influenza vaccination, HIV positivity, SARS-CoV-2 previous positivity, older age, knowing more vaccinated people, and recent incarceration were associated with higher COVID-19 vaccination rates (Cioffi et al., 2022a). Past research has identified convenience as a key barrier to vaccination for PWID in urban areas (Corcorran et al., 2023). A potentially unique feature of vaccination efforts in Oregon was the health authorities' flexibility in administering vaccinations in community locations, in partnership with syringe services programs (SSP).
2. Present study
Our goal was to understand vaccine deliberation among PWID and understand barriers that might still exist for PWID. We used a mixed-methods framework to identify convergence with past literature on vaccine deliberation among PWID and understand their experiences using in depth qualitative interviews. The primary research goals were to: 1) identify vaccination rates among PWID in Oregon at a time when vaccines were easily accessible at SSP; 2) quantitatively identify convergence with demographic correlates of vaccination willingness and uptake to promote generalizability; and 3) qualitatively explore the motivators and barriers of PWID when deciding whether to receive a COVID-19 vaccine.
3. Methods
The study followed a convergent mixed-methods design rooted in grounded-theory and transformative theoretical frameworks (Creswell and Poth, 2016). Quantitative survey results (N = 260) informed findings from qualitative interviews (N = 41) with PWID. Surveys focused on PWID's self-reported vaccination status, sociodemographic characteristics, and motivations for accepting, delaying, or refusing COVID-19 vaccinations. In-depth, in-person interviews allowed PWID to share their experiences and perceptions of COVID-19 vaccines.
3.1. Setting, recruitment, and inclusion/exclusion criteria
Participants aged 18 and older were recruited from 5 SSP sites between July 1 and September 30, 2021. The SSP sites were operated by HIV Alliance, a harm reduction organization in Lane County, Oregon and a key provider of COVID-19 resources, testing, and vaccines for PWID. HIV Alliance expanded their normal program focus during the pandemic because of National Institutes of Health Rapid Acceleration of Diagnostics for Underserved Populations funding through contracts awarded from the University of Oregon. Written consent was obtained prior to participation in the survey and interview. The University of Oregon Institutional Review Board reviewed and approved this project (approval number: 11162020.013).
3.2. Procedures
Quantitative data (N = 260) were drawn from a larger SARS-CoV-2 study testing initiative at SSP in Oregon (National Institutes of Health Rapid Acceleration of Diagnostics for Underserved Populations initiative; NIH Award Number R01DA037628, PI Stormshak). SSP clients who received COVID-19 testing were invited to participate in a 10–15-minute survey reporting demographic information, vaccination status, and vaccine sentiments. After consenting and participating, individuals received a $10 gift card.
Participants were selected for interviews using purposeful sampling to improve the likelihood of representation of women, transgender people, and Black, Indigenous, Latinx, and other people of color who are not the majority of SSP clients. Clients were asked if they would be willing to participate in a 45 min, in-person interview focused on their experiences during the COVID-19 pandemic and share their thoughts on COVID-19 testing and vaccines. Participants received a $20 gift card for participating. Forty-two semi-structured interviews were conducted at 5 HIV Alliance SSP locations in Lane County after the authors agreed thematic saturation had been achieved. One participant withdrew from the study at the end of their interview; thus, forty-one interviews were included in the final qualitative analysis.
3.3. Quantitative measures
Demographic information collected from participants included age, racial/ethnic identity, gender identity, education level, housing status, job status, self-reported COVID-19 vaccination status, and approximate annual income. Participants also reported on their likelihood of receiving a vaccine on a scale ranging from definitely not (1) to very likely (5). Participants who received a vaccine prior to the survey completion did not complete this item and were coded as very likely (5) for analysis. Clients who responded prefer not to answer or don’t know were excluded from analysis. Sample characteristics are reported descriptively in Table 1 and are presented as a valid percentage for categorical variables or means and standard deviations for continuous variables. (Table 1).
Table 1.
Participant Demographic Characteristics among Syringe Services Program Participants in Oregon from July-September 2021Responding to their History of COVID-19 Vaccination in July-September of 2021.
| Variable | Valid n | M (SD) or % |
|---|---|---|
| Age | 260 | 43.0 (12.8) |
| Gender Non-binary Woman Man OtherPrefer not to answer |
260 | 33 64 12 |
| Transgender | 260 | <1 |
| Hispanic | 260 | 7 |
| Race Native Hawaiian or Pacific Islander White Indigenous Black or African American Middle Eastern/North African Asian More than one race OtherPrefer not to answer |
260 | 78 9 2 <1 1 1 43 |
| Educational background Have never gone to school 5th grade or less 6th to 8th grade 9th to 12th grade High school graduate or GED completed Some college level / technical / vocational Bachelor’s degreeOther advanced degree |
259 | 1 2 14 37 36 52 |
| Housing status Unhoused Temporary housing Permanent housingPrefer not to answer / Don’t know |
260 | 15 137 |
| Employment status Working now Temporarily laid off, sick or maternity leave Looking for work, unemployed Retired Disabled, permanently or temporarily Student OtherPrefer not to answer / Don’t know |
260 | 3 42 5 24 1 716 |
| Health insurance status NoneOregon Health Plan (Medicaid) Medicare Tricare VA Insurance PrivateDon’t know / Prefer not to answer |
260 | 78 10 1 3 16 |
| Income Less than $15,000 $15,000 - $19,999 $20,000 - $24,999 $25,000 - $29,999$30,000 or more |
215 | 5 3 36 |
| Received COVID-19 vaccine No YesDon’t know / Prefer not to answer |
260 | 374 |
Note. The total sample included 260 participants. Vaccine willingness scores were available for 238 participants. Among subjects with willingness scores, rates of missing data on predictor variables ranged from 0% to 16% for income.
3.4. Quantitative analysis plan
We conducted multiple linear and logistic regression analyses to examine demographic correlates of self-reported vaccine status (frequency of participants who endorsed vaccination for COVID-19) and vaccination willingness, respectively. Standardized regression coefficients (βs) and odds ratios (ORs) were reported as measures of effect size. Regression models were estimated for all demographic variables, including age, race (non-White versus White), gender (female versus male), education level (at least high school diploma or GED versus below), unstable housing status (unhoused or temporary housing versus permanent housing), employment status (unemployed versus employed), and annual income (at least $l5k versus below $15 k). These variables were selected for analysis to examine how demographic characteristics related to marginalization in healthcare (gender and race) and social determinants of health (housing status, job status, and income) affected vaccine willingness and uptake. Each predictor variable was assessed individually to observe its unadjusted correlation with an individual’s vaccine willingness and uptake. Next, all predictors that were significant at the α = 0.05 level were included in the adjusted regression models. Summary statistics that calculated the frequency of responses to certain questions were used to compare themes identified in qualitative data. All data analysis was conducted using SAS version 9.4 We assessed whether there was evidence of multicollinearity in adjusted regression models, as evidenced by tolerance values greater than 0.1 and variance inflation values less than 10 (Des Jarlais et al., 2022, Dhakal, 2022).
3.5. Qualitative analysis plan
All interviews were audio recorded, transcribed, and coded using NVivo (Eskola et al., 2014) using inductive deduction thematic analysis (Koslik et al., 2020). Initial themes were drawn from existing models for vaccine deliberation, and a draft codebook was created (Marshall et al., 2015). The draft codebook was reviewed by an independent researcher familiar with the project, and the finalized codebook was used for all analysis. Analyses were complemented by ethnographic notes and memos written shortly after each interview, which helped contextualize client responses.
4. Results
4.1. Vaccine uptake
Among the 260 HIV Alliance clients surveyed in Lane County, 37% (n = 97) indicated they had received a COVID-19 vaccine, 58% (n = 151) indicated they had not been vaccinated, and 4% (n = 12) did not answer. According to the Oregon Health Authority, as of September 31, 2021, the rate of complete vaccination (completing a full vaccine series of either one or two doses) for Lane County residents was 70.1%, and 74.8%. of the population had received at least one dose (Milaney et al., 2020).
4.2. Demographic correlates of vaccine uptake
We used logistic regression to examine associations between demographic characteristics and vaccine uptake (Table 2). In unadjusted analyses, vaccine uptake was significantly associated with age (OR [95% CI] = 1.04 [1.02, 1.06], p =.0004), education (OR = 1.84 [1.10, 3.09], p =.0207), and unstable housing (OR = 0.27 [0.14, 0.52], p =.0001). Older participants, those with more education, and those in stable housing had greater odds of vaccine uptake. In adjusted analyses, age (OR [95% CI] = 1.03 [1.01, 1.05], p =.0070) and unstable housing (OR [95% CI] = 0.29 [0.15, 0.59], p =.0006) were predictors of vaccine uptake. Education did not have a statistically significant association with vaccine uptake. There was no evidence of multicollinearity in the adjusted model.
Table 2.
Results of Logistic Regression of Vaccine Uptake Status (Dependent Variable) on Demographic Characteristics (Predictor) among Syringe Services Program Participants in Oregon from July-September 2021.
| Predictor | Unadjusted Results |
Adjusted Results |
|||
|---|---|---|---|---|---|
| n | OR[95% CI] | p-value | OR[95% CI] | p-value | |
| Age | 248 | 1.04[1.02, 1.06] | 0.0004 | 1.03[1.01, 1.05] | 0.0070 |
| Non-White | 248 | 1.31[0.60, 2.85] | 0.5030 | ||
| Female | 248 | 0.82[0.48, 1.41] | 0.4712 | ||
| Education (High school degree or more) | 247 | 1.84[1.10, 3.09] | 0.0207 | 1.66[0.95, 2.88] | 0.0738 |
| Unstable housing (Unhoused or temporary housing) | 248 | 0.27[0.14, 0.52] | 0.0001 | 0.29[0.15, 0.59] | 0.0006 |
| Unemployed | 248 | 0.85[0.51, 1.42] | 0.5275 | ||
| Annual income (at least $15 k) | 213 | 0.61[0.30, 1.25] | 0.1774 | ||
Note. OR = odds ratio. Unadjusted results are based on separate logistic regression models for each predictor. n = number of participants with data for each predictor variable and vaccination status. Adjusted results are based on a model with age, education, and unstable housing as simultaneous predictors, and included 247 participants with complete data.
4.3. Demographic correlates of vaccine willingness
We found no significant associations between demographic characteristics and vaccine willingness among people who had not yet been vaccinated (Table 3).
Table 3.
Unadjusted Results of Regressing Vaccine Willingness (Dependent Variable) on Demographic Characteristics (Predictor) among Syringe Services Program Participants in Oregon from July-September 2021.
| Predictor | n | β | p-value |
|---|---|---|---|
| Age | 135 | -0.15 | 0.0781 |
| Non-White | 135 | -0.02 | 0.8067 |
| Female | 135 | 0.07 | 0.4193 |
| Education (High school degree or more) | 135 | 0.11 | 0.2213 |
| Unstable housing (Unhoused or temporary housing) | 135 | 0.04 | 0.6228 |
| Unemployed | 135 | 0.03 | 0.7253 |
| Annual income (at least $15 k) | 115 | 0.04 | 0.7027 |
Note. β = standardized regression coefficient. Results are based on separate regression models for each predictor. n = number of participants with data for each predictor variable and vaccine willingness ratings.
4.4. Vaccine deliberation themes
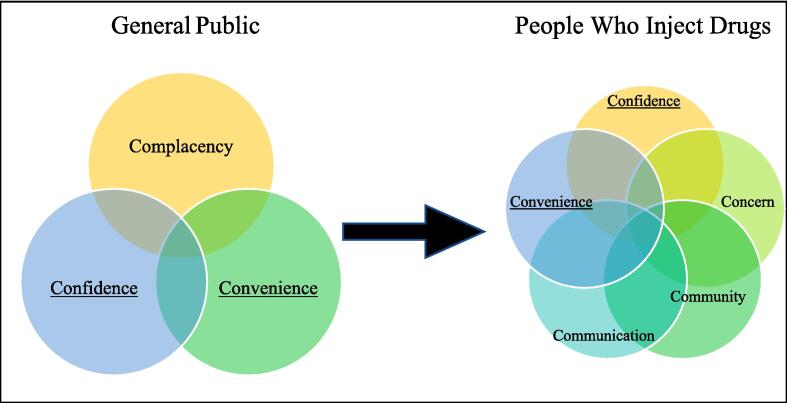
Five themes emerged from the interviews that characterized PWID vaccine deliberation: confidence, convenience, concern, communication, and community implications. (Fig. 1, Table 4). Two themes, confidence and convenience, matched those presented in the WHO's 3C model. We chose to modify the WHO's third C, complacency, with the more value-neutral term, concern. Two new Cs emerged from our research and were added: community and communication.
Fig. 1.
Comparison of WHO’s 3C Model and Proposed 5C Model WHO’s 3C Model (left) and Proposed 5C Model (right). Underlined categories represent common themes in both models.
Table 4.
Factors Affecting Vaccine Willingness and Vaccine Uptake according to WHO’s 3C Model and the Revised Model based on Qualitative Interviews and Surveys collected from Syringe Services Program Participants in Oregon from July-September 2021.
| WHO 3Cs11 | Hardin, et al. (current study) 5Cs | |
|---|---|---|
| 1 | Confidence an individual’s level of mis/trust in the vaccine, or the people providing it |
Confidence an individual’s level of mis/trust in the vaccine, or the people providing it |
| 2 | Convenience how easily an individual can get vaccinated |
Convenience how easily an individual can get vaccinated |
| 3 | Complacency an individual’s desire to seek out a vaccine |
Concern an individual’s perceived risk of a vaccine-preventable disease relative to other known risks to their health (food insecurity, violence, chronic health issues, etc.) * a challenge to “complacency” which implies carelessness or laziness |
| 4 | Communication the sources and methods a person uses to learn new information about vaccines |
|
| 5 | Community Implications how positive community-based systems of reliance, mutual support, and caretaking affect an individual's willingness to be vaccinated |
4.5. Confidence
Confidence refers to an individual’s level of trust in the vaccine and those responsible for vaccine development and distribution. In surveys, 38% (n = 58) of participants indicated that confidence-related barriers dissuaded them from accepting a COVID-19 vaccine by marking I’m concerned about side effects from the vaccine, or I don’t think vaccines work very well. Among participants who were interviewed, most explained that distrust in government, healthcare services, and the vaccine were influential in their decision-making. Participants were specifically concerned about government involvement and vaccine development, citing concerns that the government wanted to get rid of unhoused individuals and did not care or wanted to harm people who were unhoused.
“It’s just a way for the government to… I don’t know. It’s a way to round people up, the homeless and stuff, and do something with them. So, it would be the smart thing to do to instead control the population because we have too many fucking people in this world. And they’re gonna take out the weak and the old and the homeless.” (Unvaccinated person, age 52).
“I've heard about people getting sick. Lots of complications with [the vaccine] that had me scared. The rumors say that lots of people are getting sick and having complications from it.” (Unvaccinated person, age 46).
“I think they put chips in people [via the vaccine].” (Unvaccinated person, age 63).
During the interviews, although there was negative perception of government actors, the perception of healthcare providers was more positive, specifically regarding community-based health organizations like HIV Alliance that cater specifically to unhoused individuals.
“Just like asking them two ladies up there, they were very helpful. Explaining what was, what is, what's going on. I can't remember the questions I had but you know, when I started off, I was kind of in the dark and other than the stuff I partially heard on the news, I didn't know what to believe. And they just pretty much laid out what's going on, you know how it's doing.” (Unvaccinated person, age 60).
4.6. Convenience
Convenience refers to how easily individuals can access the vaccine itself, and vaccine resources. The quantitative study did not ask about convenience-related vaccine deliberation motivators. In the interviews, people who were vaccinated noted that convenience was a determining factor in their vaccine decision. For those who were not vaccinated, they cited competing demands such as limited time, energy, or money. As stated within the Concern theme, clients have competing priorities sometimes make it hard to access vaccines. Clients indicated that having vaccine services co-located with other priority resources like SSP or shelters alleviates some barriers to access.
“They’ve got the vaccine right there. So that’s helpful, they come to you. Makes it a lot easier.” (Unvaccinated person, age 57).
“[Answering why they chose to vaccinate] Because some guy was passing 'em out. Like I said, like, like hard life, it's one thing where if I got it. I got it. If I didn't, I didn't. I didn't think I'd live to see 21. And so now it's like every day above ground is a beautiful day. I sort of just take it as it comes.” (Vaccinated person, age 42)
4.7. Concern (not Complacency)
Concern is our recommended modification of the WHO's complacency. We offer the new term to challenge the idea that vaccine-hesitant people are intentionally complacent in remaining unvaccinated. Concern is a more neutral term, referring to an individual’s concern about the perceived risk of a vaccine-preventable disease relative to other potential risks to their health (such as food insecurity, housing insecurity, chronic health issues, etc.). This clarifies that while vaccination is important for mitigating the impacts of deadly diseases for PWID, people may have other competing concerns that constrain their ability to get vaccinated.
“I just don’t have the time for it. Just trying to stay alive is a full-time job. Especially when they make you move locations every 3–7 days.” (Unvaccinated person, age 46).
“Just being preoccupied, you know?… Just like daily activities… finding meals or a place to sleep. I can’t afford to just veer off my path to come get it.” (Unvaccinated person, age 35).
“I've had a crazy life. I was really abused when I was a kid and you know, I moved so much. I mean, now with any kind of worries from the virus, I'm over it. I didn't think I'd live to see 20.” (Unvaccinated person, age 42).
There was significant variation in how participants assessed their own personal risk about the severity of a COVID-19 infection. In surveys, 21% (n = 32) marked that they would get vaccinated due to concern that they would get really sick from COVID-19, while 16% (n = 24) marked that they would not get vaccinated because they were not concerned about getting really sick. Among interviewees, some expressed mixed sentiments: while they were not concerned about getting COVID-19 or having severe health side effects, they also understood there was risk in not getting vaccinated.
“It could be argued that my defenses are down. But I don't worry about getting it. There are two choices, the choice to worry about it and a choice to not worry about it. It's a false dichotomy, I suppose, there's a million choices in between, but I just choose to not worry about it.” (Unvaccinated person, age 66).
“I've really never heard of a homeless person getting [COVID-19] at all because we're not inside breathing the same air as everybody else. That's why I was never worried about it.” (Vaccinated person, age 42).
4.8. Communication
Communication refers to the flows of information about COVID-19 and the vaccine: what information is communicated, how, and by whom. This is an addition to the WHO's model and responds to the large number of respondents who commented on a perceived “lack” of information. Forty-four percent (n = 67) of the 151 survey respondents explained that they would not get a COVID-19 vaccine because they didn’t know enough about how the vaccine worked. Most people who stated they didn’t have enough information expressed that they wanted to learn more about the vaccine but did not have access to trustworthy information. Vaccinated interviewees expressed confidence in their ability to access reliable information through HIV Alliance.
“If people want information, [HIV Alliance] has tons of information about [COVID-19] too. Which I think is good for us homeless people because we don't -- a lot of us don't have the internet to get information.” (Vaccinated person, age 43).
Interviewees referenced misinformation, such as conspiracy theories, related to the vaccines. While most clients did not present these theories as truths, unverifiable claims about the dangers of the vaccine made some clients hesitant to receive a vaccine.
“[Others are] convinced that the government is making sure that everybody who has taken the vaccine now has some sort of I don't know, “X” on their back or something like that so that they can get rid of all the people that have had the vaccine to lower the population of the Earth. I don't agree with most of it, but it's scary. And you never know nowadays. You don't know. That could be the absolute truth.” (Vaccinated person, age 49).
4.9. Community implications
Community Implications is another addition to the WHO's model and characterizes PWID’s desires to protect others in their community, to act for the larger good, and to be vaccinated as a way of protecting others that they lived with or near, such as family members, housemates, or other PWID. Forty-nine percent (n = 74) of unvaccinated survey respondents indicated that community responsibility was a primary reason for considering a COVID-19 vaccine. Of those 74 respondents, 78% (n = 58) marked I want to keep my family safe, 51% (n = 38) marked I want to keep my community safe, and 30% (n = 22) marked both responses. Interviewees discussed how it was their moral responsibility to protect those around them.I think it was socially responsible I also have some health issues, and some people in my community that have compromised immune systems. I just think it's unconscionable not to take the precaution if you can. (Vaccinated person, age 47).
“Because I live in a community and I'd rather have it to protect, you know, take precautions.” (Vaccinated person, age 57).
“Definitely the only reason that I want to get it is because of my peers. I love the community. I don't want to be a burden to them by any means.” (Unvaccinated person, age 35)
“I just think it's unconscionable not to take the precaution [and get vaccinated] if you can.” (Vaccinated person, age 48).
5. Discussion
Our study found lower COVID-19 vaccination rates among PWID, some confirmation of prior literature on demographic correlates of vaccine willingness and uptake and identified expanded structural considerations for engaging PWID in vaccination from our qualitative interviews. This paper contributes to the discussions on vaccine uptake and health equity by centering the self-identified barriers and concerns of PWID, offering their quotes to begin to remediate historic patterns of exclusion, stigmatization, discrimination, and violence. We offered a modification of the WHO's popular 3C model of vaccine decision making, suggesting that a 5C framework better represents the vaccine decision making process of PWID.
Vaccination rates among PWID were 30% compared to approximately 71% in the same region in the general population. Strathdee and colleagues found similar rates of vaccination among PWID from their sample around a similar timeframe (Cioffi et al., 2022a). Importantly, this marks a substantial increase from our study conducted several months prior to these interviews in 2021 when vaccines were not easily accessible to PWID and only approximately 10% of PWID were vaccinated (Campbell et al., 2007). While the Oregon Health Authority had been providing vaccines during the study timeframe in collaboration with HIV Alliance, having a government employee provide vaccination may have been a deterrent to uptake considering the persistent theme in the qualitative data of government mistrust. Future work should consider whether vaccine administration by an employee of a trusted non-profit improves uptake. It may have also taken time to build trust and report and vaccine rates among PWID following more stable presence of vaccines on site at SSP. Our findings align with previous studies that indicate older age and greater stability (in this case, housing stability) are associated with higher levels of vaccine uptake (Cioffi et al., 2022a). There were no associations between vaccine willingness and any of our demographic variables. Our data suggest those who were older and stably housed were more motivated to seek out vaccination. More information is needed to determine which individuals were willing to be vaccinated but had not yet done so.
Framing our inquiry around an expansion of the WHO’s 3C model of vaccine hesitancy, our mixed-methods work shows that this framework does not fully capture the breadth of considerations that went into PWIDs’ decisions to accept, delay, or refuse vaccination. This research proposed a new understanding of vaccine deliberation that considered individual and community influences for PWID vaccine deliberation through 5C’s— confidence, convenience, concern, communication, and community implications. This study also reflects the association between stigmatization and health disparities which have been well-document related to substance use (Muncan et al., 2020, Office of the United Nations High Commissioner for Human Rights, 2022). Fear stemming this stigmatization has led PWID to worry that agencies that are supposed to help them may instead be seeking to harm them which deters PWID from accessing available healthcare services (Rochester and Graboyes, 2022, Saldana, 2015). PWID have higher morbidity and mortality rates from respiratory and autoimmune diseases, including chronic obstructive pulmonary disease, HIV/AIDS, and hepatitis C (Oregon Health Authority, 2020, Piltch-Loeb et al., 2021, Razai et al., 2021), making them acutely at greater risk for COVID-19, however, a lack of centering the needs of PWID tailored for convenience, confidence, and communication during the pandemic likely led to low uptake COVID-19 vaccination identified in our study and others (Campbell et al., 2007). In particular, the notion of fear of government supports the idea posited by Razai and colleagues that discriminatory ideology in healthcare can manifest as reduced motivation to receive vaccines (Biancarelli et al., 2019).
The themes identified through client interviews largely align with existing research that has found that reducing physical and social barriers to vaccination increases vaccine uptake for PWID (Strathdee et al., 2023). Improving the convenience of vaccination through SSP may have a promising impact on vaccine uptake particularly when paired with reliable information (Corcorran et al., 2023, Strathdee et al., 2019). Related to communication and community, we find that the sources and methods of communication people use to learn new information about vaccines and vaccine-preventable diseases affect their perception of vaccines (United Nations Programme on HIV/AIDS, March 13, 2019). Additionally, due to the dehumanization that PWID frequently experience, many of HIV Alliance’s clients described reliance on other community members as systems of mutual support and caretaking (Valasek et al., 2022).
6. Limitations
Our study has limitations. Our data may not be generalizable to the characteristics of all PWID. The sample of PWID included in our study were approximately 71% Non-Hispanic White which may be less diverse than PWID in other areas of the United States. Additionally, our statistical reduction to categorize “Non-White” and “Women” reduces our ability to detect nuanced intersectional experiences. Additionally, all participants were clients of HIV Alliance. While conducting research at HIV Alliance SSP locations fostered greater trust among PWID, individuals receiving services at HIV Alliance may have greater comfort accessing health services compared to PWID who do not engage in SSP.
Qualitative coding was done independently by one person, which may have biased our results. However, the coder did present all codes and themes to multiple co-authors for feedback, and there were weekly reviews during the coding process. Finally, the quantitative surveys only asked if clients had received a COVID-19 vaccine before but did not clarify whether clients were fully or partially vaccinated. Thus, clients who received a first dose but were hesitant to receive a second cannot be distinguished from clients who were fully vaccinated.
7. Conclusions
There is a need to facilitate strategic efforts to address the concerns and competing priorities that have created barriers for vaccination among PWID. To be effective, these strategies should reflect the sentiments shared in this study to foster safety and trust for PWID, and leverage the relationships of trusted community health organizations to facilitate consistent access to vaccination resources and evidence-based information (Wang et al., 2021, Wang et al., 2022, Wismans et al., 2021). A public health approach to vaccination requires an understanding of the structural factors that may be targeted to improve health outcomes, particularly for underserved community members such as PWID. Our study demonstrates that the experiences of this population that can be leveraged to promote access, build on community strengths, and identify novel vaccination delivery strategies to promote the uptake of vaccination for other infectious diseases.
8. Disclosure of funding and conflicts of interest
The authors do not have any conflicts of interest to report. Research supported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number R01DA037628 and U01DA055982 and NSF CAREER grant award number 1,844,715 (PI: Graboyes). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the National Science Foundation.
CRediT authorship contribution statement
Blake Hardin: Conceptualization, Methodology, Investigation, Formal analysis, Data curation, Writing – original draft, Project administration. Melissa Graboyes: Supervision, Writing – review & editing. Derek Kosty: Data curation, Formal analysis. Camille Cioffi: Supervision, Writing – review & editing, Methodology, Resources, Funding acquisition, Project administration.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Data availability
The authors do not have permission to share data.
References
- Abadie R., Goldenberg S., Welch-Lazoritz M., Fisher C.B., Khudyakov Y.E. Establishing trust in HIV/HCV research among people who inject drugs (PWID): insights from empirical research. PLoS One. 2018;13(12):e0208410. doi: 10.1371/journal.pone.0208410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abadie R., Gelpi-Acosta C., Aquino-Ruiz F., Aponte-Melendez Y. COVID-19 risks among people who inject drugs in Puerto Rico. Int. J. Drug Policy. 2021;93 doi: 10.1016/j.drugpo.2020.102903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken L.S., West S.G., Reno R.R. SAGE; 1991. Multiple Regression: Testing and Interpreting Interactions. [Google Scholar]
- Biancarelli D.L., Biello K.B., Childs E., Drainoni M., Salhaney P., Edeza A., Mimiaga M.J., Saitz R., Bazzi A.R. Strategies used by people who inject drugs to avoid stigma in healthcare settings. Drug Alcohol Depend. 2019;198:80–86. doi: 10.1016/j.drugalcdep.2019.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V., Clarke V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- Campbell J.V., Garfein R.S., Thiede H., Hagan H., Ouellet L.J., Golub E.T., Hudson S.M., Ompad D.C., Weinbaum C. Convenience is the key to hepatitis A and B vaccination uptake among young adult injection drug users. Drug Alcohol Depend. 2007;91:S64–S72. doi: 10.1016/j.drugalcdep.2006.09.022. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Diagnoses of HIV infection in the United States and dependent areas, 2018: Persons who inject drugs. CDC. Published May 6, 2020. Accessed February 15, 20https://www.cdc.gov/hiv/library/reports/hiv-surveillance/vol-31/content/pwid.html.
- Cioffi C.C., Kosty D., Nachbar S., Capron C.G., Mauricio A.M., Tavalire H.F. COVID-19 vaccine deliberation among people who inject drugs. Drug Alcohol Depend Rep. 2022;3 doi: 10.1016/j.dadr.2022.100046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cioffi C.C., Kosty D., Capron C.G., Tavalire H.F., Barnes R.C., Mauricio A.M. Contingency management and SARS-CoV-2 testing among people who inject drugs. Public Health Rep. 2022;137(3):573–579. doi: 10.1177/00333549221074385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J., Cohen P., West S.G., Aiken L.S. Routledge; 2013. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. [Google Scholar]
- Corcorran M.A., Austin E.J., Behrends C.N., Briggs E.S., Frost M.C., Juarez A.M., Frank N.D., Healy E., Prohaska S.M., LaKosky P.A., Kapadia S.N., Perlman D.C., Schackman B.R., Des Jarlais D.C., Williams E.C., Glick S.N. Syringe service program perspectives on barriers, readiness, and programmatic needs to support rollout of the COVID-19 vaccine. J. Addict. Med. 2023;17(1):e36–e41. doi: 10.1097/ADM.0000000000001036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell J.W., Poth C.N. SAGE Publications; 2016. Qualitative Inquiry and Research Design: Choosing Among Five Approaches. [Google Scholar]
- Des Jarlais D.C., Behrends C.N., Corcorran M.A., Glick S.N., Perlman D.C., Kapadia S.N., Lu X., Feelemyer J., LaKosky P., Prohaska S.M., Schackman B.R. Availability of and obstacles to providing COVID-19 vaccinations at syringe services programs in the United States, 2021. Public Health Rep. 2022;137(6):1066–1069. doi: 10.1177/00333549221120241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhakal K. NVivo. J. Med. Libr Assoc. 2022;110:2. doi: 10.5195/jmla.2022.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eskola J., Liang X., Reingold A. SAGE working group. Report of the SAGE Working Group on Vaccine Hesitancy. World Health. Organization. 2014 https://www.asset-scienceinsociety.eu/sites/default/files/sage_working_group_revised_report_vaccine_hesitancy.pdf Accessed June 28, 2023. [Google Scholar]
- Koslik H.J., Joshua J., Cuevas-Mota J., Goba D., Oren E., Alcaraz J.E., Garfein R.S. Prevalence and correlates of obstructive lung disease among people who inject drugs, San Diego, California. Drug Alcohol Depend. 2020;214:108158. doi: 10.1016/j.drugalcdep.2020.108158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall Z., Dechman M.K., Minichiello A., Alcock L., Harris G.E. Peering into the literature: a systematic review of the roles of people who inject drugs in harm reduction initiatives. Drug Alcohol Depend. 2015;151:1–14. doi: 10.1016/j.drugalcdep.2015.03.002. [DOI] [PubMed] [Google Scholar]
- Milaney K., Williams N., Lockerbie S.L., Dutton D.J., Hyshka E. Recognizing and responding to women experiencing homelessness with gendered and trauma-informed care. BMC Public Health. 2020;20(1):397. doi: 10.1186/s12889-020-8353-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muncan B., Walters S.M., Ezell J., Ompad D.C. “They look at us like junkies”: influences of drug use stigma on the healthcare engagement of people who inject drugs in New York City. Harm Reduct. J. 2020;17(1):53. doi: 10.1186/s12954-020-00399-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of the United Nations High Commissioner for Human Rights. Statement by the UN expert on the right to health* on the protection of people who use drugs during the COVID-19 pandemic. OHCHR. Published April 16, 2020. Accessed October 2, 2022. https://www.ohchr.org/en/statements/2020/04/statement-un-expert-right-health-protection-people-who-use-drugs-during-covid-19.
- Oregon Health Authority. Oregon’s COVID-19 Data Dashboards - Table of Contents. Tableau Public. Published October 30, 2020. Accessed April 8, 2022. https://public.tableau.com/app/profile/oregon.health.authority.covid.19/viz/OregonsCOVID-19DataDashboards-TableofContents/TableofContentsStatewide.
- Piltch-Loeb R., Savoia E., Goldberg B., Hughes B., Verhey T., Kayyem J., Miller-Idriss C., Testa M., Gesser-Edelsburg A. Examining the effect of information channel on COVID-19 vaccine acceptance. PLoS One. 2021;16(5):e0251095. doi: 10.1371/journal.pone.0251095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razai M.S., Oakeshott P., Esmail A., Wiysonge C.S., Viswanath K., Mills M.C. COVID-19 vaccine hesitancy: the five Cs to tackle behavioural and sociodemographic factors. J. R. Soc. Med. 2021;114(6):295–298. doi: 10.1177/01410768211018951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rochester E., Graboyes M. Experiences of people who use drugs with naloxone administration: a qualitative study. DrugsEduc. Prev. Policy. 2022;29(1):54–61. doi: 10.1080/09687637.2020.1855116. [DOI] [Google Scholar]
- Saldana J.M. 3rd ed. SAGE Publications; 2015. The Coding Manual for Qualitative Researchers. [Google Scholar]
- Strathdee S.A., Abramovitz D., Vera C.F., Artamonova I., Patterson T.L., Smith D.M., Chaillon A., Bazzi A.R. Predictors of COVID-19 vaccine uptake among people who inject drugs. Vaccine. 2023;41(12):1916–1924. doi: 10.1016/j.vaccine.2023.01.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Abramovitz D, Harvey-Vera A, et al. Correlates of coronavirus disease 2019 (COVID-19) vaccine hesitancy among people who inject drugs in the San Diego-Tijuana border region. Clin Infect Dis. 2022;75(1):e726-e733. doi:10.1093/cid/ciab975. [DOI] [PMC free article] [PubMed]
- United Nations Programme on HIV/AIDS Health, rights and drugs — Harm reduction, decriminalization and zero discrimination for people who use drugs. Published. March 13, 2019. https://www.unaids.org/en/resources/documents/2019/JC2954_UNAIDS_drugs_report_2019 Accessed October 2, 2022. [Google Scholar]
- Valasek C.J., Streuli S.A., Pines H.A., Mittal M.L., Strathdee S.A., Vera C.F., Harvey-Vera A., Bazzi A.R. COVID-19 vaccination acceptability and experiences among people who inject drugs in San Diego County. Prev. Med. Rep. 2022;30:101989. doi: 10.1016/j.pmedr.2022.101989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q.Q., Kaelber D.C., Xu R., Volkow N.D. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol. Psychiatry. 2021;26(1):30–39. doi: 10.1038/s41380-020-00880-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L., Wang Q., Davis P.B., Volkow N.D., Xu R. Increased risk for COVID-19 breakthrough infection in fully vaccinated patients with substance use disorders in the United States between December 2020 and August 2021. World Psychiatry. 2022;21(1):124–132. doi: 10.1002/wps.20921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wismans A., Thurik R., Baptista R., Dejardin M., Janssen F., Franken I., Delcea C. Psychological characteristics and the mediating role of the 5C Model in explaining students’ COVID-19 vaccination intention. PLoS One. 2021;16(8):e0255382. doi: 10.1371/journal.pone.0255382. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors do not have permission to share data.