Abstract
Background
Dual contraception is an essential approach to mitigating the heightened risks of unintended pregnancies and sexually transmitted infections faced by female sex workers (FSWs). We determined the prevalence and factors associated with dual contraceptive use among FSWs in Northern Uganda.
Methods
A cross-sectional study was conducted in Gulu city, Uganda between February, and March 2023. Purposively selected FSWs aged 18 years or older who provided verbal informed consent were enrolled in the study. A sample size of 374 was estimated. Data on sociodemographic and reproductive health characteristics were collected using an interviewer-administered semi-structured questionnaire. Current dual contraception was defined the as concurrent use of a barrier and any other modern contraceptive methods within the last 3 months. Continuous variables were summarized using mean and standard deviation and categorical variables were summarized using frequencies and percentages. Modified Poisson regression analysis was used to determine factors associated with dual contraceptive use.
Results
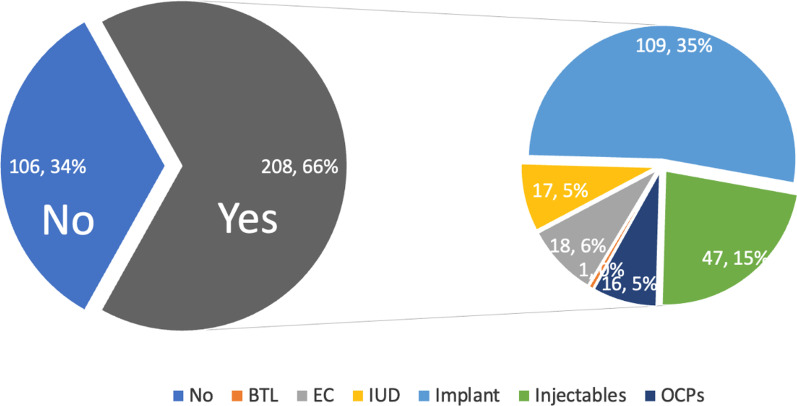
We enrolled 314 FSWs, with a mean age of 28.8 ± 6.4 years. About 13.8% (n = 41) were living with HIV. In total, 66.2% (95%CI 60.8–71.3) of the participants (n = 208) reported current dual contraceptive use. The most common modern contraceptive method used was the implants (52.4%, n = 109), followed by injectable contraceptives (22.6.0%, n = 47), and bilateral tubal ligation (0.5%, n = 1) was the least utilized. Having had at least one previous pregnancy was positively associated with dual contraceptive use (adjusted PR: 1.87, 95%CI 1.40–2.51, p < 0.001).
Conclusions
A high proportion of FSWs in Gulu city were currently using dual contraceptives. Interventions are needed to facilitate the use of dual contraception, particularly among FSWs without a history of previous pregnancies.
Keywords: Female sex workers, Dual contraceptive, Condoms, Implants
Introduction
Dual contraception (use of condom plus another modern contraceptive method) is an effective means of preventing sexually transmitted infections (STIs) including HIV and unintended pregnancies [1]. However, an earlier study among female sex workers (FSWs) in Uganda showed that only 45% of FSWs in Gulu district used dual contraception [2]. This prevalence is below the national estimate of 58% utilization of dual contraceptives among FSWs in Uganda [3]. From literature, several factors have been implicated in the low utilization of dual contraceptives among FSWs including myths and misconceptions associated with contraceptives, alcohol and substance abuse, low level or education, exploitation and, stigma and discrimination among FSWs [4–6]. In addition, rush of sexual negotiations with clients [7], having a non-emotional partner, lack of social support, rate, substance abuse, and young age [8] also contribute to low use of dual contraception among FSWs. If unattended to, the low use of dual contraception [2, 9] puts FSWs at greater risk of STIs, unwanted pregnancies [3, 10], induced abortion and its complications [11].
In sub-Saharan Africa, the risk of HIV infection is 12-folds higher among FSWs than it is in the general population [12]. In Uganda, the prevalence of HIV among sex workers is currently estimated at about 31.3% compared to the 6.3% in the general population [13]. In the bid to achieve the sustainable development goal (SDG) indicator 3.7.1 on contraceptive use, the Uganda Ministry of Health and development partners have greatly increased the availability of free modern contraceptives. Thus, more resources have been allocated to increase access to condoms for HIV prevention despite its high contraceptive failure rates (17%) compared to other modern conceptive methods [14].
Joint efforts from The AIDS Support Organization (TASO) and Reproductive Health Uganda (RHU) have significantly improved access to sexual and reproductive health and rights services among FSWs in Gulu City. However, despite integrating HIV and Sexual and reproductive health services for FSWs across the country, more effort to enhance the use of dual contraception among FSWs is needed as current use is still below average [3]. This study, therefore, aimed to determine the prevalence and associated factors with dual contraceptive use among FSWs of reproductive age in a fast-growing urban city in Northern Uganda.
Methods
Study area
Gulu city is a fast growing, mainly urban city in Northern Uganda, with an estimated population of 150,000 inhabitants. It is located about 350 kms from Kampala, the capital city of Uganda. The study was conducted in several hotspots within Gulu, city which has an estimated 1300 FSWs. A total of 15 hotspots across the city constituted the study sites. Participants were recruited from different locations within Gulu City, where FSWs were known to congregate, including bars, nightclubs, brothels, and streets in pece, layibi and laroo divisions. A vast majority of the FSWs in Gulu and surrounding districts live and work in Gulu city [15]. There are over 20 governmental and non-governmental health facilities and organizations that work closely with FSWs in Gulu city, including Gulu Regional Referral Hospital, The AIDS Support Organization (TASO)—Gulu Branch, Reproductive Health Uganda, the Voice of Community Empowerment, and others.
Study design and period
Between February, and March 2023, we conducted a community-based cross-sectional study among eligible FSWs in Gulu city, Northern Uganda. This report is written in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for cross-sectional studies [16].
Population
The source population were FSWs of reproductive age engaged in sex work within Gulu city. To be eligible for the study, participants had to be 18 years or older and within the reproductive age bracket (15–49 years), cisgender female, provided written informed consent to participate in the study and currently working and identifying as a sex worker. HIV status was verified from the most recent HIV testing results less than 3 months old. We excluded transgender women.
Sample size estimation
The sample size of 374 was calculated using the modified Kish-Leslie formula (1965) for a single population, with the prevalence of dual contraception estimated at 58% from a previous study [8], type 1 error of 5% (1.96) and 95% confidence. Consecutive sampling was used to recruit the participants in the study.
Data collection tool and procedures
Enrolment was conducted by engaging peer leaders of a hotspot who knew most of the FSWs who operate within his/her area. Two research assistants (MA and FGL) had previous and ongoing engagements with FSWs in Gulu through the Voice of Community Empowerment, which provides advocacy for FSWs and other vulnerable populations in Gulu. Additional respondents were enrolled through snowballing, where after interviewing the participants, they were requested to identify and refer their colleagues to the research team.
Data were collected through face-to-face interviews in a private space within the place of sex work across the hotspots using a pre-tested semi-structured questionnaire. The questionnaire was developed in English and translated into the local language, Acholi. The questionnaire collected information on socio-demographic characteristics, sexual behaviour, condom use, contraceptive use, and depression. The data collection process was supervised by FB and GM.
Operational definition
Dual contraceptive user was defined as a FSW who concurrently use a barrier (male or female condoms) regularly and any other modern (pills, injections, intrauterine devices) contraceptive methods.
Depression over the past 2 weeks was assessed using the Patient Health Questionnaire-2 (PHQ-2), with a cutoff score of 3 used to define depressed mood [17].
Condom use was defined as regularly if a FSW uses it most of the time or “sometimes” if the use was occasional and “never” if the participants never used it in the past 3 months.
Statistical analysis
Data were cleaned and exported into STATA version 14.0, StataCorp LLC, College Station, Texas, USA for analysis. Normally distributed continuous variables were summarized using mean and standard deviation and categorical variables were summarized using proportions and percentages. The proportion FSWs with dual contraceptive use was summarized as a proportion with its 95% confidence interval. For the regression analysis, the outcome variable of dual contraceptive use was dichotomized as 1 “yes” 0 “no”. Since the outcome was common (the proportion of dual contraceptive use was > 10%), modified Poisson regression was used to determine factors associated with dual contraception and measure of association was the prevalence ratio. We conducted bivariate analysis and variables with p < 0.20 were considered for multivariate analysis. In the multivariate analysis, we used manual backward elimination method until all the variables in the model had p value ≤ 0.05. We assessed for interaction by forming product terms and performed a chunk test. We assessed for confounding by considering a percentage change of > 10% in the crude and adjusted prevalence ratios. The goodness of fit of the model was assessed using Hosmer–Lemeshow goodness of fit test. Variables with p values < 0.05 were considered statistically significant.
Ethical consideration
The study received ethical approval from the Gulu University Research Ethics Committee (approval number: GUREC-2022-414). Verbal informed consent was obtained from all participants before the start of the study. Participants were informed of their right to withdraw from the study at any time and that their participation was voluntary. All data collected was kept confidential and anonymous. The ethical principles outlined in the Declaration of Helsinki were all adhered to. Study participants who required specific sexual and reproductive health services were counselled and referred to the appropriate health facility.
Results
Participants
Of the 374 anticipated participants, 314 (response rate 84%) were eligible and were enrolled into the study.
Sociodemographic characteristics
Overall, 314 FSWs with a mean age of 28.8 ± 6.4 years were included in the final analysis. More than half of the participants were below the age of 29 (58.3%, n = 183). In terms of education, slightly over half of the participants had received secondary or tertiary education (51.3%, n = 161). Most participants resided in rural areas (93.3%, n = 293), were single (81.8%), and Christians (92.6%), while only a small proportion identified as Muslim (7.4%). About two-third (67.2%, n = 211) had been pregnant between 1 and 4 times, and 9.5% had been pregnant more than four times. In terms of abortion, 39.2% (n = 123) had had between 1 and 4 abortions.
When it comes to income, 40.5% (n = 127) of participants reported sex work as their major source of income. In terms of mental health, most participants reported symptoms of depression (90.1%, n = 283). In terms of awareness of HIV status, most participants were aware of their status (94.9%, n = 298). Of those who were aware, 13.8% (n = 41) were living with HIV. Regarding alcohol consumption, 80.7% (n = 250) of participants reported consuming alcohol sometimes, while 16.8% (n = 52) reported consuming alcohol always. In terms of age at first sexual encounter, slightly over half of the participants had their first sexual encounter before the age of 17 (55.2%, n = 158). Table 1 summarizes the baseline characteristics of the study participants.
Table 1.
Sociodemographic and reproductive health characteristics of female sex workers in Gulu city, Uganda
| Variable | Category | Frequency (N = 314) | Percent (%) |
|---|---|---|---|
| Age (years) mean (SD) | 28.8 (6.4) | ||
| Age (years) | < 29 | 183 | 58.3 |
| > 28 | 131 | 41.7 | |
| Education | None/Primary | 153 | 48.7 |
| Secondary/tertiary | 161 | 51.3 | |
| Residence | Urban | 21 | 6.7 |
| Rural | 293 | 93.3 | |
| Marital status | Married | 57 | 18.2 |
| Single | 257 | 81.8 | |
| Religion | Moslem | 23 | 7.4 |
| Christian | 286 | 92.6 | |
| Number of pregnancies | None | 73 | 23.3 |
| 1–4 | 211 | 67.2 | |
| > 4 | 30 | 9.5 | |
| Number of abortions | None | 167 | 53.2 |
| 1–4 | 123 | 39.2 | |
| > 4 | 24 | 7.6 | |
| Number of unplanned pregnancy n = 305 | None | 166 | 54.4 |
| 1–3 | 118 | 38.7 | |
| > 3 | 21 | 6.9 | |
| Number of conceptions during sex work n = 305 | None | 193 | 63.3 |
| 1–3 | 100 | 32.8 | |
| > 3 | 12 | 3.9 | |
| Number of unplanned pregnancies during sex work n = 307 | None | 187 | 60.9 |
| 1–4 | 108 | 35.2 | |
| > 4 | 12 | 3.9 | |
| Sex work as major source of income | No | 187 | 59.6 |
| Yes | 127 | 40.5 | |
| Depression | No | 31 | 9.9 |
| Yes | 283 | 90.1 | |
| Awareness of HIV status | No | 16 | 5.1 |
| Yes | 298 | 94.9 | |
| HIV status n = 298 | Negative | 257 | 86.2 |
| Positive | 41 | 13.8 | |
| Alcohol consumption n = 310 | Always | 52 | 16.8 |
| Never | 8 | 2.6 | |
| Sometimes | 250 | 80.7 | |
| Age at first sexual encounter n = 286 | < 17 | 158 | 55.2 |
| > 16 | 128 | 44.8 |
Reproductive characteristics
Regarding unplanned pregnancy and sex work, 38.7% (n = 118) had experienced between 1 and 3 unplanned pregnancies, and 6.9% (n = 21) had experienced more than 3. In terms of conception during sex work, 32.8% (n = 100) had conceived between 1 and 3 times, and 3.9% (n = 12) had conceived more than 3 times. Of those who had experienced unplanned pregnancies during sex work, 35.2% (n = 108) had experienced between 1 and 4 unplanned pregnancies, and 3.9% (n = 12) had experienced more than 4.
Contraceptive use and methods mix
In total, 66.2% (95%CI 60.8–71.3) of the participants (208 out of 314) reported using dual contraception. Condom use in the last month was reported by 95.9% (n = 301 out of 314) of the participants, and 85.4% (n = 268) reported using a condom during their last sexual encounter. The frequency of condom use was reported as always by 21.7% (n = 68), sometimes by 76.4% (n = 240), and never by 1.9% (n = 6).
Among the participants, 208 reported using modern contraceptives. The most common method was the implants (52.4%, n = 109), followed by injectable contraceptives (22.6%, n = 47), and bilateral tubal ligation (0.5%, n = 1) was the least utilized, Fig. 1, Table 2.
Fig. 1.
Pie-of-pie chart showing contraceptive methods used by female sex workers in Gulu city, Uganda. BTL bilateral tubal ligation, EC emergency pills, OCPs oral contraceptive pills
Table 2.
Contraceptive use among female sex workers in Gulu city, Uganda
| Variable | Category | Frequency (N = 314) | Percent (%) |
|---|---|---|---|
| Dual contraception | No | 106 | 33.8 |
| Yes | 208 | 66.2 | |
| Condom use in the last month | No | 13 | 4.1 |
| Yes | 301 | 95.9 | |
| Condom use during last sexual encounter | No | 46 | 14.6 |
| Yes | 268 | 85.4 | |
| Frequency of condom use | Always | 68 | 21.7 |
| Never | 6 | 1.9 | |
| Sometimes | 240 | 76.4 | |
| Modern contraceptives n = 208 | Bilateral tubal ligation | 1 | 0.5 |
| Emergency pills | 18 | 8.7 | |
| Intrauterine device | 17 | 8.2 | |
| Implants | 109 | 52.4 | |
| Injectables | 47 | 22.6 | |
| Oral pills | 16 | 7.7 |
Factors associated with dual contraceptive use among female sex workers in Gulu city, Uganda
In the bivariable analysis, age (p < 0.001), ever had pregnancy (p < 0.001), ever had unplanned pregnancy (p = 0.032), and ever had unplanned pregnancy during sex work (p = 0.038) were significant.
In the multivariate analysis, ever had a pregnancy (adjusted PR: 1.87, 95%CI 1.40–2.51, p < 0.001) was significantly associated with dual contraceptive use. Participants who had ever had a pregnancy were 1.87 times likely to use dual contraception. Other demographic and reproductive factors, including education, residence, marital status, religion, ever had abortions, and history of abortion, were not significantly associated with the use of dual contraception (Table 3).
Table 3.
Factors associated with dual contraceptive use among female sex workers in Gulu city, Uganda
| Variable | Category | Dual Contraception | Crude PR | 95% CI | p value | |
|---|---|---|---|---|---|---|
| Yes (N = 208) | No (N = 106) | |||||
| Age (years) | < 29 | 106 (57.9) | 77 (42.1) | 1 | ||
| > 28 | 102 (77.9) | 29 (22.1 | 1.34 | 1.15, 1.57 | < 0.001 | |
| Education | None/Primary | 105 (68.6) | 48 (31.4) | 1 | ||
| Secondary/tertiary | 103 (64.0) | 58 (36.0) | 0.92 | 0.80, 1.09 | 0.384 | |
| Residence | Urban | 15 (71.4) | 6 (28.6) | 1 | ||
| Rural | 193 (65.9) | 100 (34.1) | 0.92 | 0.69, 1.22 | 0.575 | |
| Marital status | Married | 34 (59.7) | 23 (40.4) | 1 | ||
| Single | 174 (67.7) | 83 (32.3) | 1.14 | 0.90, 1.43 | 0.28 | |
| Religion | Moslem | 11 (47.8) | 12 (52.2) | 1 | ||
| Christian | 194 (67.8) | 92 (32.2) | 1.42 | 0.92, 2.19 | 0.115 | |
| Ever had a pregnancy | No | 29 (39.7) | 44 (60.3) | 1 | ||
| Yes | 179 (74.3) | 62 (25.7) | 1.87 | 1.40, 2.51 | < 0.001 | |
| Ever had an induced abortion | No | 105 (62.9) | 62 (37.1) | 1 | ||
| Yes | 103 (70.1) | 44 (29.9) | 1.11 | 0.95, 1.30 | 0.178 | |
| Ever had a pregnancy during sex work, n = 305 | No | 124 (64.2) | 69 (35.8) | 1 | ||
| Yes | 82 (73.2) | 30 (26.8) | 1.34 | 0.98, 1.33 | 0.096 | |
| Unplanned pregnancies during sex work, n = 307 | No | 118 (63.1) | 69 (36.9) | 1 | ||
| Yes | 89 (74.2) | 31 (25.8) | 1.18 | 1.01, 1.37 | 0.038 | |
| Sex work as major source of income | No | 120 (64.2) | 67 (35.8) | 1 | ||
| Yes | 88 (69.3) | 39 (30.7) | 1.08 | 0.92, 1.26 | 0.341 | |
| Depression | No | 19 (61.3) | 12 (38.7) | 1 | ||
| Yes | 189 (66.8) | 94 (33.2) | 1.09 | 0.81, 1.46 | 0.565 | |
| HIV status n = 298 | Negative | 174 (67.7) | 83 (32.3) | 1 | ||
| Positive | 27 (65.9) | 14 (34.2 | 0.97 | 0.77, 1.23 | 0.818 | |
| Alcohol consumption n = 310 | Always | 38 (73.1) | 14 (26.9) | 1 | ||
| Never | 4 (50.0) | 4 (50.0) | 0.68 | 0.34, 1.40 | 0.297 | |
| Sometimes | 162 (64.8) | 88 (35.2) | 0.89 | 0.73, 1.07 | 0.212 | |
| Age at first sexual encounter n = 286 | < 17 | 106 (67.1) | 52 (32.9) | 1 | ||
| > 16 | 87 (68.0) | 41 (32.0) | 1.01 | 0.86, 1.19 | 0.875 | |
Discussion
Dual contraception plays a pivotal role in the prevention of unintended pregnancies and STIs, including HIV among FSWs who are at heightened risk of these conditions due to the nature of their activities [18]. In this study, we aimed to determine the prevalence and associated factors with dual contraceptive use among FSWs in Gulu City, Northern Uganda. In this mainly urban setting in Northern Uganda, we found that almost 2 in 3 of the FSWs reported using dual contraception. In this study, the prevalence of HIV among FSWs was 13.8%, which is higher than in the general women population in Uganda at 6.3% [13]. Condom use in the last month was reported by 95.9%. However, the frequency of condom use was reported as always by only 22% and sometimes by majority (76.4%). The most commonly modern contraceptive method was the implants (51.5%) and injectable contraceptives (23.0%).
The prevalence of dual contractive use of about 67% in our study is comparable though slightly higher than findings from an earlier study conducted in the four regions of Uganda in 2017, where the prevalence of dual contraception among FSWs was estimated at 58.0% [3]. On the contrary, lower prevalence of dual contraceptives use were registered among FSWs in a more recent study in Northern Uganda (45%), Kenya (38%), Zambia (18.3%), Russia (12%), Switzerland (8%) and Tanzania (5.7–6%) [2, 9, 19–23]. The difference in the prevalence could be due to the joint efforts from TASO-Uganda and RHU in Gulu city, where evening mobile clinics are held to extend sexual and reproductive health services to FSWs to bridge the gap between FSWs and the health system. In addition, availability of condoms in the sex work places has been shown to increase use as FSWs can then negotiate for safe sex with clients [20].
Despite the ensured availability of condoms, most FSWs still report inconsistent use of condoms as was reported in other publications, where consistent condom use was as low as 16% [22]. This is attributed to factors such as being HIV positive, alcohol and substance use, clients’ indifference towards sex with condoms as well as mutual agreement between FSW and client to have condomless sex at an extra fee [24, 25]. As such, the risky behaviour increases odds of contracting HIV as evidenced by the high prevalence of HIV (13.8%) among FSWs in this study. Even more, FSWs who tested positive for HIV were less likely to use any condoms, propagating spread of HIV. As evidenced by the reduced uptake of contraceptive in FSW population with HIV in this study [22]. FSWs may be hard pressed to provide services in remote or unsafe occupational environments. The stigma and lack of protection place FSWs at increased risk of violence from clients, and because rushed negotiations, they are not able to screen clients properly or to negotiate the use of condoms in the sexual encounter [18, 26, 27]. Further studies are recommended to qualitative evaluate the barriers and facilitators of condom use among FSWs in Gulu City.
In our study, we found that over 70% of FSWs using modern contraceptives were using implants or injectable methods. Recent studies have shown that implants and injectables, which are long acting reversible contraceptives (LARCs), are the most preferred modern contraceptive methods especially for FSWs with future fertility desires due to their perceived effectiveness in prevention of unintended pregnancies and limited interference in the FSWs’ day-to-day activities [11, 28]. LARCs offer a reliable and convenient option for contraception, which is particularly important for FSWs who may face barriers to accessing healthcare services regularly.
We also observed that participants who had ever had a pregnancy were almost twofold more likely to use dual contraception, which is consistent with preliminary literature suggesting a similar association [2]. This finding suggests that pregnancy experience may play a role in shaping contraceptive decision-making among FSWs by increasing their awareness of the potential consequences of unprotected sex, such as the risk of unplanned pregnancies. Furthermore, the involvement of healthcare providers in providing education and counselling about the benefits of dual contraception during or after pregnancy may further influence their decision-making process regarding dual contraception [2].
In addition, women are more likely to use dual contraception if they are aware of dual contraception, have used non-barrier contraceptives as well as having disclosed their HIV status to their sexual partner given that they are HIV positive [29]. Whereas, having rush sexual negotiations owing to police presence and fear of side effects from modern contraceptive methods are negatively associated with dual contraceptive use [2].
Our study was not without limitations. Our study relied on self-reported contraceptive use and the information provided by the FSWs may have been influenced by recall bias and desire for social acceptance. Some studies have noted a trade off in women who adopt non-barrier modern contraception abandon condoms [30, 31]. However, our study provides further insights into contraceptive use among FSWs and sets a stage for further interventional studies.
Conclusions
In this study, we found that about two-thirds of FSWs used dual contraception indicating a positive trend towards safer sexual practices. We found a positive association between previous pregnancy and dual contraception use, suggesting that FSWs who have experienced pregnancy prioritize the use of multiple contraceptive methods for enhanced protection against unplanned pregnancies and STIs.
Recommendations
FSWs in Gulu city should be targeted for continued support for dual contraception among other sexual and reproductive health services through peer support networks and community-based interventions that address barriers to dual contraceptive use and promote its benefits. We also recommend development of targeted educational programs that emphasize and provide comprehensive information on dual protection, tailored to the specific needs of FSWs without history of pregnancy in Gulu city. Findings from this study should be utilized to guide the Ministry of Health in formulating evidence-based policies aimed at improving the uptake of dual contraception among FSWs to effectively prevent unintended pregnancies and improve the overall sexual and reproductive health outcomes for FSWs in Uganda.
Acknowledgements
We would like to acknowledge the study participants.
Author contributions
FB conceptualised the study. All authors made substantial contributions to the design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This study was supported through a seed Grant from the Centre for International Reproductive Health Training at the University of Michigan (CIRHT-UM), the United State of America. The funder had no role in the design and conduction of this study.
Availability of data and materials
All relevant data are within the manuscript and its supporting information files. Data are available upon reasonable request from the first author.
Declarations
Ethics approval and consent to participate
The study received ethical approval from the Gulu University Research Ethics Committee (approval number: GUREC-2022-414). Informed consent was obtained from all participants before the start of the study. Participants were informed of their right to withdraw from the study at any time and that their participation was voluntary. All data collected was kept confidential and anonymous. The ethical principles outlined in the Declaration of Helsinki were all adhered to.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO. Sexually transmitted infections (STIs) World Health Organisation; 2022.
- 2.Erickson M, Goldenberg SM, Ajok M, Muldoon KA, Muzaaya G, Shannon K, et al. Structural determinants of dual contraceptive use among female sex workers in Gulu, northern Uganda. Int J Gynecol Obstet. 2015;131(1):91–95. doi: 10.1016/j.ijgo.2015.04.029. [DOI] [PubMed] [Google Scholar]
- 3.Bukenya JN, Wanyenze RK, Barrett G, Hall J, Makumbi F, Guwatudde D, et al. Contraceptive use, prevalence and predictors of pregnancy planning among female sex workers in Uganda: a cross sectional study. BMC Pregnancy Childbirth. 2019;19:1–11. doi: 10.1186/s12884-019-2260-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peipert JF, Zhao Q, Meints L, Peipert BJ, Redding CA, Allsworth JE. Adherence to dual-method contraceptive use. Contraception. 2011;84(3):252–258. doi: 10.1016/j.contraception.2011.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chacham AS, Diniz SG, Maia MB, Galati AF, Mirim LA. Sexual and reproductive health needs of sex workers: two feminist projects in Brazil. Reprod Health Matters. 2007;15(29):108–118. doi: 10.1016/S0968-8080(07)29292-4. [DOI] [PubMed] [Google Scholar]
- 6.Becker M, Ramanaik S, Halli S, Blanchard JF, Raghavendra T, Bhattacharjee P, et al. The intersection between sex work and reproductive health in Northern Karnataka, India: identifying gaps and opportunities in the context of HIV prevention. AIDS Res Treatment 2012;2012. [DOI] [PMC free article] [PubMed]
- 7.Ochako R, Okal J, Kimetu S, Askew I, Temmerman M. Female sex workers experiences of using contraceptive methods: a qualitative study in Kenya. BMC Women’s Health. 2018;18:1–10. doi: 10.1186/s12905-018-0601-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Selvey LA, Hallett J, McCausland K, Bates J, Donovan B, Lobo R. Declining condom use among sex workers in Western Australia. Front Public Health. 2018;6:342. doi: 10.3389/fpubh.2018.00342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yam EA, Mnisi Z, Mabuza X, Kennedy C, Kerrigan D, Tsui A, et al. Use of dual protection among female sex workers in Swaziland. Int Perspect Sex Reprod Health. 2013;39:69–78. doi: 10.1363/3906913. [DOI] [PubMed] [Google Scholar]
- 10.Zhang X-D, Kennedy E, Temmerman M, Li Y, Zhang W-H, Luchters S, et al. High rates of abortion and low levels of contraceptive use among adolescent female sex workers in Kunming, China: a cross-sectional analysis. Eur J Contracept Reprod Health Care. 2014;19(5):368–378. doi: 10.3109/13625187.2014.927421. [DOI] [PubMed] [Google Scholar]
- 11.Ouma S, Tumwesigye NM, Abbo C, Ndejjo R. Factors associated with the uptake of long-acting reversible contraception among female sex workers in post-conflict Northern Uganda: a cross-sectional study. Reprod Health. 2022;19(1):34. doi: 10.1186/s12978-022-01345-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baral S, Beyrer C, Muessig K, Poteat T, Wirtz AL, Decker MR, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(7):538–549. doi: 10.1016/S1473-3099(12)70066-X. [DOI] [PubMed] [Google Scholar]
- 13.UNAIDS. Geneva: Joint United Nations Programme on HIV/AIDS 2022. Available from: https://www.unaids.org/sites/default/files/media_asset/data-book-2022_en.pdf. [PubMed]
- 14.Kost K, Singh S, Vaughan B, Trussell J, Bankole A. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception. 2008;77(1):10–21. doi: 10.1016/j.contraception.2007.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Apodaca K, Doshi RH, Ogwal M, Kiyingi H, Aluzimbi G, Musinguzi G, et al. Capture-recapture among men who have sex with men and among female sex workers in 11 towns in Uganda. JMIR Public Health Surveill. 2019;5(2):e12316. doi: 10.2196/12316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13(Suppl 1):S31–S34. doi: 10.4103/sja.SJA_543_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Löwe B, Kroenke K, Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2) J Psychosom Res. 2005;58(2):163–171. doi: 10.1016/j.jpsychores.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 18.Scorgie F, Chersich MF, Ntaganira I, Gerbase A, Lule F, Lo YR. Socio-demographic characteristics and behavioral risk factors of female sex workers in sub-saharan Africa: a systematic review. AIDS Behav. 2012;16(4):920–933. doi: 10.1007/s10461-011-9985-z. [DOI] [PubMed] [Google Scholar]
- 19.Sutherland EG, Alaii J, Tsui S, Luchters S, Okal J, Kingola N, et al. Contraceptive needs of female sex workers in Kenya–a cross-sectional study. Eur J Contracept Reprod Health Care. 2011;16(3):173–182. doi: 10.3109/13625187.2011.564683. [DOI] [PubMed] [Google Scholar]
- 20.Chanda MM, Ortblad KF, Mwale M, Chongo S, Kanchele C, Kamungoma N, et al. Contraceptive use and unplanned pregnancy among female sex workers in Zambia. Contraception. 2017;96(3):196–202. doi: 10.1016/j.contraception.2017.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Decker MR, Yam EA, Wirtz AL, Baral SD, Peryshkina A, Mogilnyi V, et al. Induced abortion, contraceptive use, and dual protection among female sex workers in Moscow. Russia. 2013;120(1):27–31. doi: 10.1016/j.ijgo.2012.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mbita G, Mwanamsangu A, Plotkin M, Casalini C, Shao A, Lija G, et al. Consistent condom use and dual protection among female sex workers: surveillance findings from a large-scale, community-based combination HIV prevention program in Tanzania. AIDS Behav. 2020;24(3):802–811. doi: 10.1007/s10461-019-02642-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beckham SW, Stockton M, Galai N, Davis W, Mwambo J, Likindikoki S, et al. Family planning use and correlates among female sex workers in a community empowerment HIV prevention intervention in Iringa, Tanzania: a case for tailored programming. BMC Public Health. 2021;21(1):1377. doi: 10.1186/s12889-021-11426-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Laušević D, Begić S, Terzić N, Vratnica Z, Čičić A, Mugoša B. Factors associated with inconsistent condom use with clients among female sex workers in Podgorica, Montenegro. Srp Arh Celok Lek. 2016;144(7–8):424–430. doi: 10.2298/SARH1608424L. [DOI] [PubMed] [Google Scholar]
- 25.Decker MR, Park JN, Allen ST, Silberzahn B, Footer K, Huettner S, et al. Inconsistent condom use among female sex workers: partner-specific influences of substance use, violence, and condom coercion. AIDS Behav. 2020;24(3):762–774. doi: 10.1007/s10461-019-02569-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shannon K, Csete J. Violence, condom negotiation, and HIV/STI risk among sex workers. JAMA. 2010;304(5):573–574. doi: 10.1001/jama.2010.1090. [DOI] [PubMed] [Google Scholar]
- 27.Kempner ME. Sex workers: a glimpse into public health perspectives. 2005;33(2):2–3.
- 28.Nyaoke B. P4. 17 Contraceptive preference among female sex workers in the sivet study in nairobi, kenya. BMJ Publishing Group Ltd; 2017.
- 29.Mulongo AM, Lihana RW, Githuku J, Gura Z, Karanja S. Factors associated with uptake of dual contraception among HIV-infected women in Bungoma County, Kenya: a cross-sectional study. Pan Afr Med J. 2017;28(Suppl 1):2. doi: 10.11604/pamj.supp.2017.28.1.9289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ott MA, Adler NE, Millstein SG, Tschann JM, Ellen JM. The trade-off between hormonal contraceptives and condoms among adolescents. Perspect Sex Reprod Health. 2002;34:6–14. doi: 10.2307/3030227. [DOI] [PubMed] [Google Scholar]
- 31.Hoefnagels C, Hospers HJ, Hosman C, Schouten L, Schaalma H. One measure, two motives. Prediction of condom use and interaction between two prevention goals among heterosexual young adults: preventing pregnancy and/or sexually transmitted diseases. Prevent Sci. 2006;7:369–376. doi: 10.1007/s11121-006-0048-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the manuscript and its supporting information files. Data are available upon reasonable request from the first author.