Highlights
-
•
Prevalence of substance use disorders increased significantly from 2011 to 2019 in young adults.
-
•
Age, gender, race, insurance type, and family income were associated with substance use disorders in young adults.
-
•
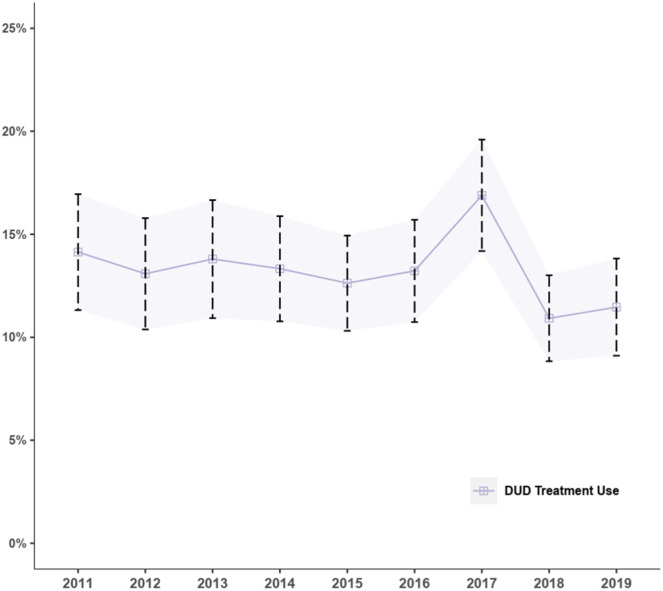
Prevalence of treatment use fluctuated insignificantly over the study period.
-
•
Self-help groups and rehabilitation facilities were most cited treatment facilities.
-
•
Gender, race, insurance type, and family income were associated with treatment use for substance use disorders in young adults.
Keywords: Substance use disorders, Young adults, Treatment use across settings
Abstract
Background
Compared with adults of other age groups, young adults are more likely to have substance use disorders (SUDs) but less likely to receive treatment. Untreated SUDs can lead to lethal consequences, particularly deaths related to drug overdose.
Objectives
This study aimed to examine trends and sociodemographic differences in the prevalence and treatment use of SUDs among US young adults aged 18 to 25 in the National Survey on Drug Use and Health 2011–2019.
Methods
Bivariable logistic regression analyses were conducted to examine annual changes in the prevalence and treatment use of SUDs, and multivariable logistic regression was used to examine sociodemographic differences in SUD prevalence and treatment use in the pooled sample of young adults from 2011 to 2019.
Results
From 2011 to 2019, the overall SUD prevalence increased significantly from 5.4% to 6.2%. Cannabis use disorder was the most common SUD annually. Groups with lower prevalence of SUDs included females, young adults aged 22–25, and Hispanic, Black, and Asian participants. Across the survey years, the prevalence of treatment use fluctuated insignificantly between 10.9% and 16.9% among young adults with SUDs, and most young adults received SUD treatment in self-help groups and residential and outpatient rehabilitation facilities. Compared to White participants, treatment use was lower in Hispanic, Black, Asian participants, as well as young adults of two or more races. Young adults covered by Medicaid/CHIP were more likely to use treatment.
Conclusions
This study revealed an alarming level of unmet treatment need and significant disparities in treatment use among young adults with SUDs. To reduce barriers to treatment utilization, more coordinated efforts that leverage policy and structural changes alongside innovations to engage young adults with SUD care are needed.
1. Background
Young adults aged 18–25 are more likely to initiate or increase substance use than any other age group (Substance Abuse and Mental Health Services Administration, 2019b). Compared to adolescents and adults aged 26 or older, young adults were least likely to perceive a great risk of harm from using drugs (Substance Abuse and Mental Health Services Administration, 2020a), potentially leading to drug initiation and use (Lipari and Jean-Francois, 2016). Previous national studies using data from 2002 to 2014 have examined and reported an overall decreasing trend in the annual prevalence of substance use disorders (SUDs) overall among adolescents aged 12–17 (Han et al., 2017) or adults aged 18 and older (Lipari and Van Horn, 2013); yet, changes in the annual prevalence of specific types of SUDs, e.g., cannabis use disorders, are not well documented (Lipari and Van Horn, 2013). Particularly, to our knowledge, no study has examined time changes in the prevalence of SUDs among young adults for the past decade (Lu et al., 2021; Seitz et al., 2019). Preventing SUDs in young adults is particularly important given that substance use during this developmental stage can have lasting effects on brain development, and can lead to a range of negative health outcomes, such as addiction and mental health problems (Squeglia et al., 2009). Further, studies have identified some sociodemographic factors (e.g., gender, educational level, etc.) related to drug use in adults (Han et al., 2015; Kessler et al., 2001; Martins et al., 2012), such as opioid misuse, but little is known about sociodemographic differences in SUDs among young adults (Gaither et al., 2018; Hadland et al., 2017). Such information is important to identify groups who are at higher risk for SUDs and inform targeted prevention efforts.
Although SUDs are treatable, few people in the U.S. receive any or adequate treatment (American Addiction Centers, 2022). Untreated SUDs have detrimental impact on individuals, families, and communities, including devastating overdose-related consequences. From January 2015 to November 2021, the number of deaths due to drug overdose in the U.S. doubled and reached a peak of more than 100,000 people (Centers for Disease Control and Prevention, 2022). The death rates from both prescription and illicit opioids in the population ages 15–24 increased by 15.4% per year between 2013 and 2015 (Ali et al., 2019). To avoid such lethal consequences, it is crucial to examine the prevalence of treatment use for SUDs among young adults and identify underserved populations to guide further service provision. Depending on the severity level of their disorders, young adults can receive treatment for SUDs in a variety of settings, including specialty facilities, school clinics, primary care, and mental health clinics (Center for Substance Abuse Treatment, 1999). Yet, previous studies primarily focused on evaluating treatment use in specialty facilities (Romo et al., 2018) and residential and outpatient treatment (Stahler et al., 2016), but excluded treatment use in self-help groups and hospital-based inpatient settings. A more comprehensive investigation of young adults’ treatment use for SUDs across settings can shed light on young adults’ preferences for treatment modalities and facilitate refinement of treatment that is acceptable and engaging for this high-risk population.
This study aimed to address these research gaps by examining trends and sociodemographic differences in the prevalence and treatment of SUDs among young adults in the U.S. using data from the 2011–2019 National Survey on Drug Use and Health (NSDUH). Our specific research questions are:
-
1
What is the current prevalence of SUDs among young adults aged 18–25 in the U.S.?
-
2
Has the annual prevalence of SUDs in young adults changed from 2011 to 2019?
-
3
Has the annual proportion of young adults who received treatment for SUDs changed from 2011 to 2019?
-
4
Does the prevalence of treatment use for SUDs differ by age, gender, race/ethnicity, insurance coverage, and annual household income in the pooled sample of young adults in 2011–2019?
2. Methods
2.1. Data descriptions
The NSDUH is an annual cross-sectional survey conducted by the Substance Abuse and Mental Health Services Administration (SAMHSA) to provide the most updated information on tobacco, alcohol, drug use, mental health, and other health-related issues in the U.S. A stratified multistage area probability sampling method was applied to obtain nationally representative data for the civilian, noninstitutionalized population aged 12 or older (Substance Abuse and Mental Health Services Administration, 2019a). This survey study was approved by the institutional review board at RTI International.
For this study, we restricted our analysis to data in the 2011–2019 NSDUH. The 2020 and 2021 NSDUH data are available but not included in the study for two reasons. First, SUD estimates in 2020 and 2021 are based on criteria from the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5), which are not comparable with prior years of NSDUH that were based on DSM-IV criteria. Second, the 2020 estimates further reflect additional methodological changes in data collection due to COVID.
2.2. Measurements
Sociodemographic characteristics included young adults’ age groups (18–21 vs. 22–25), gender (male and female), race/ethnicity (White, Hispanic/Latino, non-Hispanic Black, non-Hispanic Asian/Native Hawaiian or other Pacific Islanders [NHPIs], non-Hispanic Native Americans, and two or more races), insurance type (uninsured, Medicaid/ Children's Health Insurance Program [CHIP], private insurance, and other), and household income (<$20,000, $20,000-$49,999, $50,000-$74,999, and $75,000 or higher). Particularly, young adults were divided into 2 age groups of 18–21 years and 22–25 years to allow comparisons across developmental stages based on prior work that has shown differences in drug use patterns (Bagley et al., 2020).
Substance use disorders: Participants were asked about their use of the following drugs in the past 12 months: cannabis, hallucinogens, inhalants, methamphetamine, cocaine, or heroin, and nonmedical use of psychotherapeutics, such as pain relievers, sedatives, stimulants, or tranquilizers. Participants were considered to have SUDs if meeting the criteria for the DSM-IV in the past year that included (1) one or more symptoms of drug abuse (e.g., role failure, hazardous use, use despite social problems) and (2) three or more symptoms of drug dependence (e.g., larger amounts used, tolerance, persistent desire, unsuccessful control, withdrawal, etc.).
Treatment for SUDs: Young adults were asked if they had used any treatment or counseling to help reduce or stop drug use at any location in the past 12 months. Those who reported having used treatment for SUDs were further asked about specific settings where the treatment occurred, including hospitals (inpatient), rehabilitation facilities (either residential or outpatient), mental health clinics, private physician's offices, emergency rooms, prisons or jails, and self-help groups (e.g., Alcoholics Anonymous).
2.3. Data analysis
Bivariate analyses were first conducted to assess time trends in the prevalence and treatment of any SUD, and the survey year was used as the continuous independent variable. For each bivariate regression model, the trend was considered statistically significant if the coefficient (i.e., slope) of the year was statistically significant. Following that, multiple logistic regressions were applied to examine sociodemographic differences in the prevalence and treatment of SUDs at the significance level of 0.05. All demographic variables, including gender, age, race/ethnicity, insurance status, and annual household income, were included in the multivariable models to predict the prevalence and treatment use of SUDs. The survey year was further included to control for potential time influence in all multivariable analyses. Missing data ranged from 0% to 2.7% for variables included and were listwise deleted as recommended by the NSDUH (Dong and Peng, 2013; Substance Abuse and Mental Health Services Administration, 2019a). Data were analyzed between April and May 2022 using R (Version 4.2.0), accounting for the complex survey design, nonresponse bias, and noncoverage bias via using sampling weights provided by the NSDUH.
3. Results
3.1. Demographic characteristics of young adults
Among the 207,895 Young adults aged 18 to 25 in 2011–2019, 52.7% were female and 67% aged between 22 and 25. Approximately 56% were White, followed by Hispanic (20%), Black (13%), and Asian/NHPIs (6%). Nearly 20% did not have insurance while 58.3% were covered by private insurance. One-third were from families with an annual household income from $20,000 to $49,999 and 23.5% had a family income of $75,000 or more (Table 1).
Table 1.
Sociodemographic characteristics of the pooled sample of young adults aged 18 to 25 in the NSDUH, 2011–2019 (N = 207,895).
| Characteristics | No. (%) |
|---|---|
| Gender | |
| Male | 98,388 (47.3) |
| Female | 109,507 (52.7) |
| Age | |
| 18–21 | 68,673 (33.0) |
| 22–25 | 139,222 (67.0) |
| Race/Ethnicity | |
| White, non-Hispanic | 116,877 (56.2) |
| Hispanic/Latino | 40,466 (19.5) |
| Black, non-Hispanic | 28,033 (13.4) |
| Asian/NHPI, non-Hispanic | 11,386 (5.5) |
| Native American, non-Hispanic | 3270 (1.6) |
| Two or more, non-Hispanic | 7863 (3.8) |
| Insurance Coverage | |
| No | 40,479 (19.7) |
| Medicaid/CHIP | 37,277 (18.1) |
| Private insurance | 119,847 (58.3) |
| Other insurance | 7991 (3.9) |
| Household income, $ | |
| <20,000 | 56,484 (27.2) |
| 20,000–49,999 | 71,540 (34.4) |
| 50,000–74,999 | 30,961 (14.9) |
| ≥75,000 | 48,910 (23.5) |
Note: Unweighted number of participants and weighted percentages are reported. NHPIs: Native Hawaiian or other Pacific Islanders. CHIP: Children's Health Insurance Program.
3.2. Trends in the prevalence of young adult SUDs
Overall, the prevalence of any SUD among young adults increased linearly from 5.4% in 2011 to 6.2% in 2019 (OR = 1.01, 95% CI: 1.00–1.02, P < 0.05) (Fig. 1). As delineated in Table 2, across the 10 specific SUDs, cannabis use disorders were most common, which increased significantly from 3.6% in 2011 to 4.2% in 2019 (OR = 1.02, 95% CI: 1.00–1.03, P < 0.05). The second most common SUD was prescription pain relievers which decreased significantly from 1.5% to 0.7% (OR = 0.90, 95% CI: 0.88–0.92, P < 0.001). Methamphetamine use disorders were added to the 2015 NSDUH with an upward trend from 0.49% to 0.70% (OR = 1.14, 95% CI: 1.05–1.23, P < 0.01) from 2015 to 2019.
Fig. 1.
Time trend in the prevalence of 12-month substance use disorders among young adults in the US, 2011–2019.
Table 2.
Time trends in the 12-month prevalence of specific types of substance use disorders among young adults in the US, 2011–2019.
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | OR (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|---|
| 12-month prevalence,% | n = 24,809 | n = 24,107 | n = 23,588 | n = 21,459 | n = 23,637 | n = 22,411 | n = 22,626 | n = 22,431 | n = 22,827 | |
| Cannabis | 3.55 | 3.78 | 3.55 | 3.55 | 3.38 | 3.34 | 3.42 | 4.09 | 4.21 | 1.02 (1.00, 1.03) * |
| Hallucinogens | 0.34 | 0.30 | 0.20 | 0.21 | 0.23 | 0.31 | 0.28 | 0.29 | 0.26 | 0.99 (0.95, 1.04) |
| Inhalants | 0.05 | 0.00 | 0.01 | 0.01 | 0.00 | 0.00 | 0.01 | 0.01 | 0.00 | 1.08 (0.98, 1.18) |
| Methamphetaminea | N/A | N/A | N/A | N/A | 0.49 | 0.40 | 0.58 | 0.70 | 0.70 | 1.14 (1.05, 1.23) ⁎⁎ |
| Cocaine | 0.59 | 0.71 | 0.76 | 0.51 | 0.56 | 0.58 | 0.67 | 0.74 | 0.74 | 1.02 (0.98, 1.05) |
| Heroin | 0.40 | 0.46 | 0.53 | 0.59 | 0.55 | 0.53 | 0.52 | 0.38 | 0.32 | 0.98 (0.95, 1.01) |
| Prescription pain relievers | 1.49 | 1.78 | 1.53 | 1.29 | 1.23 | 1.01 | 1.02 | 0.83 | 0.72 | 0.90 (0.88, 0.92) ⁎⁎⁎ |
| Prescription sedatives | 0.03 | 0.10 | 0.07 | 0.07 | 0.07 | 0.06 | 0.06 | 0.06 | 0.08 | 1.01 (0.91, 1.12) |
| Prescription stimulants | 0.24 | 0.55 | 0.51 | 0.34 | 0.38 | 0.41 | 0.48 | 0.46 | 0.43 | 1.02 (0.98, 1.06) |
| Prescription tranquilizers | 0.35 | 0.56 | 0.43 | 0.33 | 0.44 | 0.42 | 0.61 | 0.49 | 0.41 | 1.02 (0.98, 1.06) |
P < 0.05;.
P < 0.01;.
P < 0.001.
Questions about methamphetamine use disorders were not asked before the year 2015. Unweighted number of participants and weighted percentages are reported. For each bivariate regression model, survey year was the continuous independent variable, and the trend was considered significant if the coefficient (i.e., slope) of the year was statistically significant.
3.3. Trends and patterns of treatment use for young adult SUDs
As displayed in Fig. 2, from 2011 to 2019, the overall prevalence of treatment use for SUDs at any treatment facility fluctuated between 10.9% and 16.9%, with no significant changes (Fig. 2). Across the survey years, most young adults with SUDs received treatment from self-help groups, with a significant decrease from 10.3% in 2011 to 7.7% in 2019 (OR = 0.96, 95% CI: 0.93–0.99, P < 0.001) (Table 3). Outpatient rehabilitation facilities were the second most commonly used settings for SUD treatment between 7.2% and 6.4%, followed by inpatient rehabilitation facilities fluctuating between 6.1% and 5.4%, with no significant changes in either settings. Around 10% of young adults in 2019 reported using SUD treatments in two or more facilities and the prevalence varied between 8.9% and 14.1%, with no significant time changes (Table 3).
Fig. 2.
Time trend in overall treatment use among young adults with any 12-month substance use disorders in the US, 2011–2019.
Table 3.
Time trends and patterns in setting-specific treatment use among young adults with any 12-month substance use disorders, 2011–2019.
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | OR (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Treatment use,% | n = 1623 | n = 1649 | n = 1506 | n = 1222 | n = 1388 | n = 1341 | n = 1402 | n = 1410 | n = 1459 | |
| Overnight in hospital | 4.65 | 5.67 | 5.49 | 6.49 | 3.99 | 3.62 | 6.42 | 3.66 | 3.57 | 0.96 (0.92, 1.00) |
| Residential rehabilitation facility | 6.13 | 6.67 | 7.40 | 7.20 | 5.16 | 5.37 | 7.91 | 4.56 | 5.40 | 0.97 (0.94, 1.01) |
| Outpatient rehabilitation facility | 7.15 | 6.96 | 10.00 | 9.54 | 7.95 | 6.89 | 10.81 | 6.88 | 6.43 | 0.99 (0.96, 1.02) |
| Mental health clinic | 5.06 | 4.92 | 5.37 | 6.12 | 5.42 | 5.26 | 8.47 | 5.41 | 5.37 | 1.02 (0.99, 1.06) |
| Private doctor's office | 3.31 | 3.81 | 4.41 | 4.78 | 3.61 | 3.98 | 5.69 | 4.25 | 4.75 | 1.04 (0.98, 1.09) |
| Emergency room | 3.16 | 2.65 | 3.55 | 3.37 | 2.70 | 3.16 | 4.82 | 3.72 | 3.34 | 1.03 (0.98, 1.09) |
| Prison or jail | 2.64 | 2.22 | 2.23 | 1.71 | 1.30 | 1.42 | 3.02 | 1.56 | 1.57 | 0.96 (0.89, 1.03) |
| Self-help group |
10.26 | 10.25 | 9.73 | 8.93 | 8.43 | 9.50 | 9.80 | 6.75 | 7.74 | 0.96 (0.93, 0.99)* |
| Two or more settingsa | 11.73 | 11.50 | 12.03 | 11.58 | 10.19 | 10.76 | 14.13 | 9.16 | 8.85 | 0.97 (0.94, 1.00) |
*P < 0.05, **P < 0.01, ***P < 0.001. Unweighted number of participants and weighted percentages are presented. Specific sources of treatment use are not mutually exclusive. No mathematical correction was made for multiple comparisons.
Young adults’ treatment use for substance use disorders in any two or more of the 8 settings.
3.4. Sociodemographic disparities in SUD prevalence
As listed in the adjusted model (Table 4), compared to males and young adults aged 18–21, the overall prevalence of SUDs was lower in females (aOR = 0.53, 95% CI: 0.50–0.55, P < 0.001) and young adults aged 22–25 (aOR = 0.66, 95% CI: 0.63–0.69, P < 0.001). Relative to White participants, a lower prevalence of SUDs was found in Hispanic (aOR: 0.63, 95% CI: 0.58–0.68, P < 0.001), Black (aOR = 0.81, 95% CI: 0.74–0.87, P < 0.001), and Asian/NHPI participants (aOR = 0.40, 95% CI: 0.34–0.46, P < 0.001) while higher prevalence was found in those of two or more races (aOR = 1.22, 95% CI: 1.07–1.39, P < 0.01). While young adults with Medicaid/CHIP (aOR = 1.13, 95% CI: 1.04–1.22, P < 0.01) were more likely to be identified as having SUDs, those covered by private insurance (aOR = 0.69, 95% CI: 0.64–0.75, P < 0.001) were less likely to experience SUDs compared to uninsured young adults. Participants who were from higher-income families: $20,000-$49,999 (aOR = 0.81, 95% CI: 0.76–0.86, P < 0.001), $50,000-$74,999 (aOR = 0.77, 95% CI: 0.71–0.84, P < 0.001), and at least $75,000 (aOR = 0.73, 95% CI: 0.67–0.79, P < 0.001) were at lower odds of reporting SUDs than young adults with an annual family income of lower $20,000.
Table 4.
Multivariable differences in the prevalence of 12-month substance use disorders and treatment use in the pooled sample of young adults in the U.S., 2011–2019.
| Substance Use Disorders |
Treatment use |
|||||
|---|---|---|---|---|---|---|
| # of young adults | % | aOR (95% CI) | # of young adults with substance use disorders | % | AOR (95% CI) | |
| Year | — | — | 1.02 (1.01, 1.03) ⁎⁎ | — | — | 0.97 (0.95, 1.00) |
| Gender | ||||||
| Male | 98,388 | 17.57 | (ref.) | 7828 | 12.49 | (ref.) |
| Female | 109,507 | 10.89 | 0.53 (0.50, 0.55) ⁎⁎⁎ | 5172 | 14.49 | 1.07 (0.92, 1.25) |
| Age | ||||||
| 18–21 | 68,673 | 15.38 | (ref.) | 5489 | 9.08 | (ref.) |
| 22–25 | 139,222 | 13.86 | 0.66 (0.63, 0.69) ⁎⁎⁎ | 7511 | 15.21 | 1.67 (1.42, 1.95) ⁎⁎⁎ |
| Race/ethnicity | ||||||
| White, non-Hispanic | 116,877 | 15.76 | (ref.) | 7640 | 15.87 | (ref.) |
| Hispanic/Latino | 40,466 | 12.88 | 0.63 (0.58, 0.68) ⁎⁎⁎ | 2161 | 10.34 | 0.58 (0.46, 0.74) ⁎⁎⁎ |
| Black, non-Hispanic | 28,033 | 12.33 | 0.81 (0.74, 0.87) ⁎⁎⁎ | 1787 | 6.98 | 0.34 (0.26, 0.44) ⁎⁎⁎ |
| Asian/NHPI, non-Hispanic | 11,386 | 8.17 | 0.40 (0.34, 0.46) ⁎⁎⁎ | 373 | 6.79 | 0.42 (0.21, 0.84) * |
| Native American, non-Hispanic | 3270 | 20.27 | 1.16 (0.94, 1.42) | 309 | 16.99 | 1.08 (0.57, 2.08) |
| Two or more, non-Hispanic | 7863 | 16.81 | 1.22 (1.07, 1.39) ⁎⁎ | 730 | 10.43 | 0.61 (0.42, 0.90) * |
| Insurance type | ||||||
| No | 40,479 | 16.12 | (ref.) | 2947 | 12.65 | (ref.) |
| Medicaid/CHIP | 37,277 | 13.18 | 1.13 (1.04, 1.22) ⁎⁎ | 2875 | 21.14 | 1.99 (1.60, 2.48) ⁎⁎⁎ |
| Private | 119,847 | 13.77 | 0.69 (0.64, 0.75) ⁎⁎⁎ | 6493 | 10.21 | 0.78 (0.64, 0.96) * |
| Other | 7991 | 15.54 | 0.91 (0.78 1.06) | 563 | 10.89 | 0.89 (0.57, 1.40) |
| Family income, $ | ||||||
| <20,000 | 56,484 | 15.97 | (ref.) | 4340 | 15.25 | (ref.) |
| 20,000–49,999 | 71,540 | 14.08 | 0.81 (0.76, 0.86) ⁎⁎⁎ | 4308 | 12.18 | 0.79 (0.65, 0.96) * |
| 50,000–74,999 | 30,961 | 13.39 | 0.77 (0.71, 0.84 ⁎⁎⁎ | 1720 | 13.96 | 1.00 (0.78, 1.28) |
| ≥75,000 | 48,910 | 13.46 | 0.73 (0.67, 0.79) ⁎⁎⁎ | 2632 | 11.72 | 0.89 (0.71, 1.11) |
P ≤ 0.05;.
P ≤ 0.01;.
P ≤ 0.001. Unweighted sample sizes and weighted percentages are presented. All variables listed were included in the multivariable models to predict the prevalence and treatment use of substance use disorders. AOR: adjusted odds ratio. Ref.: reference group.
3.5. Sociodemographic disparities in SUD treatment use
Overall, no gender differences were observed in young adults’ treatment use for SUDs (Table 4). Young adults aged 22–25 were more likely to use SUD treatment compared to those aged 18–21 (aOR = 1.67, 95% CI: 1.42–1.95, P < 0.001). Compared to White participants, lower levels of treatment use were found in Hispanic (aOR = 0.58, 95% CI: 0.46–0.74, P < 0.001), Black (aOR = 0.34, 95% CI: 0.26–0.44, P < 0.001), and Asian/NHPI participants (aOR = 0.42, 95% CI: 0.21–0.84, P < 0.05), as well as young adults of two or more races (aOR = 0.61, 95% CI: 0.42–0.90, P < 0.001) were less likely to receive any SUD treatment. While higher odds of treatment use were noted in young adults with Medicaid/CHIP (aOR = 1.99, 95% CI: 1.60–2.48, P < 0.001) compared to those who were uninsured, lower odds were observed in those covered by private insurance (aOR = 0.78, 95% CI: 0.64–0.96, P < 0.05). Lastly, young adults from families with an annual income of $20,000-$49,999 were less likely to receive SUD treatment (aOR = 0.79, 95% CI: 0.65–0.96, P < 0.05) compared to those from families with an annual income of less than $20,000.
4. Discussion
Overall, an increasing trend was observed in the prevalence of any SUD among young adults in the U.S. from 2011 to 2019. The U.S. has approximately 34 million young adults aged 18–25 in 2018 (American Addiction Centers, 2022). This age span is characterized by identity exploration, increased independence, and changes in residence (Arnett, 2005). At this transition time, young adults are more likely to initiate or increase substance use than other age groups (Substance Abuse and Mental Health Services Administration, 2019b). Also, compared to adolescents and adults aged 26 and older, young adults tend to initiate and use drugs due to the higher level of perceived availability of substances (Lipari and Jean-Francois, 2016). Our nationally representative data showed cannabis use disorder was the most common SUD in young adults, with a significant increase from 2011 to 2019. Emerging evidence suggests that the perception of cannabis use as harmful has declined substantially among young adults (Sarvet et al., 2018; Wen et al., 2019) following state-level cannabis legalization and decriminalization (Cerdá et al., 2020; Leung et al., 2019; Smart and Pacula, 2019). To reverse the rising trend of SUDs, more public health campaigns are needed to educate young adults about harms associated with drug use.
Notably, our study revealed a decreasing trend in the prevalence of prescription pain reliever use disorders in young adults, from 1.49% in 2011 to 0.72% in 2019. Hydrocodone is one of the most common pain medications prescribed by clinicians for a variety of painful conditions, including coughs, dental and injury-related pain (Cofano and Yellon, 2022). It is also a long-acting and highly addictive opioid medication (Wang et al., 2022). To reduce misuse, the Drug Enforcement Administration (DEA) changed the schedule of hydrocodone combination products from Schedule III to Schedule II, indicating the substance has a higher potential for abuse and people could not obtain a prescription refilled at the pharmacy without seeing a doctor (Pergolizzi et al., 2017). The identified decrease in the prevalence of prescription pain reliever use disorders in this study coincides with the implementation of this policy change since 2014 (Pergolizzi et al., 2017). Nevertheless, hydrocodone remains one of the most abused opioid medications by patients (Wang et al., 2022). Considering the increasing rate of drug overdose deaths involving opioids in recent years (Mattson et al., 2021), ongoing surveillance of prescription pain reliever misuse in young adults is critical. As approximately 20% of individuals who misuse prescription pain relievers obtained these medications from healthcare providers (Lipari and Hughes, 2017), continued training on ethics and prescription practices of physicians are also important to combat the opioid epidemic (Singh and Pushkin, 2019; Enzinger and Wright, 2021).
Across the survey years, fewer than 15% of young adults with SUDs received any treatment, which was slightly higher than the prevalence of treatment use in the 2005–2009 period (at approximately 10%) but remained alarmingly low (Cook and Alegria, 2011). Young adults faced a plethora of barriers to accessing treatment for SUDs at the individual, provider, and system-related levels (Carr et al., 2008; Liebling et al., 2016; Sterling et al., 2010; Wu et al., 2011). Among young adults aged 18–25 in Rhode Island who reported non-medical prescription opioids, for example, approximately half of them had never attempted to participate in substance use disorder treatment and a fifth were unsuccessful in at least one attempt to enroll in treatment (Liebling et al., 2016). This highlights the importance of raising awareness at the individual level of the health-related consequences of SUDs and motivating young adults to seek services early. Additionally, young adults may fear disclosing their substance use to their parents or other caregivers, which can further reduce their likelihood of seeking treatment (Sterling et al., 2010).
At the system level, treatment accessibility is known to be impacted by program ownership; for example, private for-profit programs were twice as likely to provide on-demand treatment compared to public programs (Friedmann et al., 2003). Nonetheless, total waiting times for substance use treatment in the U.S. could take more than two months (Carr et al., 2008). In a previous study (Liebling et al., 2016), young adults who made attempts but were unsuccessful in enrolling in treatment for opioid use further cited financial barriers due to high deductibles and/or copayments, as well as providers not accepting all types of insurance. These barriers produce delays in enrollment and can mitigate motivation to participate in timely treatment. Taken together, to close the troubling SUD treatment gap, individual practice innovations targeting lack of awareness, stigma, and misinformation need be pursued in conjunction with wide scale policy changes and financial assistance that can facilitate access and expedite entry into treatment.
Our results extended findings from a previous study conducted in 2011 (Wu et al., 2011) indicating self-help groups such as Alcoholics or Narcotics Anonymous were the most common settings where young adults received treatment for SUDs. With their ease of accessibility and free-of-charge recovery environment (Kelly and Myers, 2007), self-help groups are considered a promising avenue for SUD care in a cost-constricting climate, but the level of use remained low. This could, in part, be due to the abstinence-oriented framework and/or autocratic leadership style within peer groups that precludes membership participation (Nayar et al., 2004). More research is warranted to explore the reasons for the low usage of self-help groups amongst young adults in the U.S. Given the ongoing socioeconomic impacts of the COVID-19 pandemic, the implementation of mutual aid groups as after-care and recovery services would be beneficial for expanding the coverage of peer support in the community and reducing government health expenditure for addiction treatment.
We also found that residential and outpatient rehabilitation facilities were common sources of treatment use for young adults. Residential settings provide greater protection from both environmental and social determinants which results in higher rates of SUD treatment completion (Stahler et al., 2016). Nonetheless, most prior work has primarily focused on local data and used a single treatment facility (e.g., inpatient treatment), and examined a specific subgroup of participants (e.g., individuals who use opiates) (Brorson et al., 2013). This study is one of the first of its kind to employ national data to evaluate trends and patterns in setting-specific treatment use among young adults with past-year SUDs. These findings can lay the groundwork for identifying preferred modalities of SUD treatment that promote enrollment in this underserved population.
Extensive disparities were found in SUD treatment use for young adults. Particularly, older young adults aged 22–25 were more likely to seek treatment compared to those aged 18–21. These findings largely converge with previous studies (Bagley et al., 2021; Liebling et al., 2016; Windle et al., 1991; Wu et al., 2011). For example, the Primary Care Opioid Use Disorders (PROUD) trial revealed that less than one in six youth aged 16–17 received buprenorphine or naltrexone for opioid use disorders while about a third of young adults aged 18–25 years received medications for opioid use disorders (Bagley et al., 2021). Our findings underscore the pressing need for the treatment of SUDs, especially among younger young adults. Expanding convenient, de-stigmatizing entry points for SUD treatment for young adults, such as primary care clinics, is critical.
Young adults who identified as Hispanic, Black, Asian/NHPI, or multi-racial had comparatively lower odds of participating in SUD treatment than White young adults. The racial/ethnic disparities could be attributable to a combination of systematic and structural factors such as racism, discrimination, poverty, lack of health insurance, and geographic barriers (Dickerson et al., 2011; Farahmand et al., 2020; Substance Abuse and Mental Health Services Administration, 2020b). These factors may interact with access disparities, making it difficult for minoritized young adults to access SUD treatment services. For example, poverty and lack of health insurance may limit access to treatment services (Dickerson et al., 2011), while discrimination and social isolation may lead to mistrust of the healthcare system and reluctance to seek help for SUD problems (Substance Abuse and Mental Health Services Administration, 2020b). Additionally, prior research has suggested that individual-level factors such as less perceived need for substance use treatment (Wu et al., 2011), lower motivation to enroll in treatment (Liebling et al., 2016), and being more socially isolated may contribute to the relative under use of services by minoritized youth (Windle et al., 1991). For young adults, these disparities at treatment entry have consequential downstream effects, such as potentially delaying the initiation of treatment experiences and when accessed, reducing the likelihood of successful completion (Mennis and Stahler, 2016; Montgomery et al., 2020). Given the disproportionate underutilization of SUD treatment among these racial/ethnic groups, building more trusted and accessible referral systems for these underserved populations are necessary. More importantly, addressing the racial/ethnic disparities in access to SUD treatment requires a multi-faceted approach that addresses systematic and structural factors, while also providing targeted outreach and support for minoritized young adults.
In this study, young adults who came from families with an annual household income of $20,000-$49,999 were less likely to receive treatment for SUDs compared to those with a family income of less than $20,000. This finding is in line with the 2005–2009 report that more individuals with lower income participated in substance use disorder treatment because of greater exposure to government-sponsored treatment programs, especially in more disadvantaged neighborhoods (Cook and Alegria, 2011). Also, we found that young adults with Medicaid/CHIP reported higher levels of treatment use from 2011 to 2019 compared to uninsured young adults. Medicaid is currently the largest source of public funding for substance use disorder treatment in the U.S. (Tambling et al., 2021) and is thus central to efforts to address SUDs among young adults (Brooks and Gardner, 2018). Medicaid coverage expanded considerably during the study period but these expansions are not evenly distributed across the population (Peterson and Busch, 2018), and could possibly exacerbate racial disparities in substance use treatment (Andrews et al., 2015; Tambling et al., 2021). Hence, providing equitable access to Medicaid or other federally-supported health insurance across racial/ethnic groups could serve as an important promotive factor in treatment-seeking. Additionally, other reasons for the low uptake of SUD treatment are lack of health insurance or not being aware of health insurance coverage among those with private insurance (Cummings et al., 2014). Tailored outreach of insured young adults regarding benefits when using health insurance for SUD services may help foster SUD treatment initiation and continuation.
This study has several limitations. First, the NSDUH relies on self-report which can be influenced by recall bias or social desirability. Nevertheless, the implementation of computer-assisted personal interviewing may minimize these potential biases when collecting sensitive information. Second, high rates of opioid misuse and disorders were found among unstably housed (Stringfellow et al., 2016) and incarcerated samples (Fazel et al., 2017), but the NSDUH excluded these populations and this could impact the prevalence reported for young adults. Third, we did not include NSDUH 2020 and 2021 data into our analysis because of changes in SUD diagnosis criteria and methodology in data collection due to the influence of COVID. As more years of NSDUH data are being collected and released, continued monitoring is needed to examine how the pandemic and related changes in healthcare practices might have led to changes in patterns of SUD prevalence and treatment use in young adults during and after COVID, and beyond. Further, we did not conduct further analysis to examine sociodemographic disparities in the prevalence and treatment of specific SUDs due to small cell sample sizes of most disorders, e.g., Hallucinogens, inhalants, sedatives, which may lead to biased estimation. Lastly, several statistically significant results identified in this study had small effect sizes as indicated by low values of odds ratios. Therefore, caution should be used when interpreting findings from this study, particularly for statistically significant changes in annual proportions of young adults with specific SUDs and those who received treatment in respective settings. Strengths of this study include its high response rate and the level of generalizability drawn from its national sample, which combined may mitigate biased estimates.
5. Conclusion
From 2011 to 2019, an increasing trend was observed in the prevalence of any SUD among young adults. Findings indicate an alarming level of unmet SUD treatment need and significant disparities in treatment utilization among young adults, especially for racial/ethnic minorities. These results underscore the necessity of novel strategies tailored to young adults that can improve SUD detection, treatment access, and treatment entry. Reducing barriers to treatment utilization will likely necessitate coordinated efforts that leverage policy and structural changes alongside innovations to how young adults access and engage with SUD care. Interventions are crucial that focus on raising awareness of the harms from SUDs and addressing stigma-related hurdles to disclosing their health concerns as well as participating in treatment services. It is additionally important to develop effective linkage networks for young adults — especially those from low-income families — to evidence-based treatment.
Contributors
Wenhua Lu and Teresa Lopez-Castro conceptualized the study. Wenhua Lu conducted the data analysis. Thinh Vu and Wenhua Lu drafted the initial version of the manuscript, and all authors commented on and revised previous versions of the manuscript. All authors read and approved the final manuscript.
Declaration of Competing Interest
No conflict declared
References
- Ali B., Fisher D.A., Miller T.R., Lawrence B.A., Spicer R.S., Swedler D.I., Allison J. Trends in drug poisoning deaths among adolescents and young adults in the United States, 2006-2015. J. Stud. Alcohol Drugs. 2019;80(2):201–210. doi: 10.15288/jsad.2019.80.201. https://www.ncbi.nlm.nih.gov/pubmed/31014465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Addiction Centers . 2022. Substance Abuse among Young Adults.https://americanaddictioncenters.org/rehab-guide/addiction-statistics/young-adults Retrieved May 52022, from. [Google Scholar]
- Andrews C.M., Guerrero E.G., Wooten N.R., Lengnick-Hall R. The medicaid expansion gap and racial and ethnic minorities with substance use disorders. Am. J. Public Health. 2015;105(3):S452–S454. doi: 10.2105/AJPH.2015.302560. Suppl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnett J.J. The developmental context of substance use in emerging adulthood. J. Drug Issues. 2005;35(2):235–254. doi: 10.1177/002204260503500202. [DOI] [Google Scholar]
- Bagley S.M., Larochelle M.R., Xuan Z., Wang N., Patel A., Bernson D., et al. Characteristics and receipt of medication treatment among young adults who experience a nonfatal opioid-related overdose. Ann. Emerg. Med. 2020;75(1):29–38. doi: 10.1016/j.annemergmed.2019.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagley S.M., Chavez L., Braciszewski J.M., Akolsile M., Boudreau D.M., Lapham G., Campbell C.I., Bart G., Yarborough B.J.H., Samet J.H., Saxon A.J., Rossom R.C., Binswanger I.A., Murphy M.T., Glass J.E., Bradley K.A., Collaborative P Receipt of medications for opioid use disorder among youth engaged in primary care: data from 6 health systems. Addict. Sci. Clin. Pract. 2021;16(1):46. doi: 10.1186/s13722-021-00249-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks, T., & Gardner, A. (2018). Snapshot of children with medicaid by race and ethnicity. Retrieved May 5 from https://ccf.georgetown.edu/wp-content/uploads/2020/07/Snapshot-Medicaid-kids-race-ethnicity-v4.pdf.
- Brorson H.H., Ajo Arnevik E., Rand-Hendriksen K., Duckert F. Drop-out from addiction treatment: a systematic review of risk factors. Clin. Psychol. Rev. 2013;33(8):1010–1024. doi: 10.1016/j.cpr.2013.07.007. [DOI] [PubMed] [Google Scholar]
- Carr C.J., Xu J., Redko C., Lane D.T., Rapp R.C., Goris J., Carlson R.G. Individual and system influences on waiting time for substance abuse treatment. J. Subst. Abuse Treat. 2008;34(2):192–201. doi: 10.1016/j.jsat.2007.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment. (1999). Brief Interventions and Brief Therapies For Substance Abuse. Treatment Improvement Protocol (TIP) Series, No. 34. Rockville, MD: Substance Abuse and Mental Health Services Administration Retrieved from https://store.samhsa.gov/sites/default/files/d7/priv/sma12-3952.pdf. [PubMed]
- Centers for Disease Control and Prevention . 2022. Provisional Drug Overdose Death Counts.https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm 2022. Retrieved May 5 from. [Google Scholar]
- Cerd´ a M., Mauro C., Hamilton A., Levy N.S., Santaella-Tenorio J., Hasin D.S., Wall M.M., Keyes K.M., Martins S.S. Association between recreational marijuana legalization in the united states and changes in marijuana use and cannabis use disorder from 2008 to 2016. JAMA Psychiat. 2020;77(2):165–171. doi: 10.1001/jamapsychiatry.2019.3254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cofano S., Yellon R. Hydrocodone. In StatPearls [Internet] 2022 https://www.ncbi.nlm.nih.gov/books/NBK537288/ StatPearls Publishing. Retrieved July 17, 2023, from. [PubMed] [Google Scholar]
- Cook B.L., Alegria M. Racial-ethnic disparities in substance abuse treatment: the role of criminal history and socioeconomic status. Psychiatr. Serv. 2011;62(11):1273–1281. doi: 10.1176/ps.62.11.pss6211_1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings J.R., Wen H., Ritvo A., Druss B.G. Health Insurance coverage and the receipt of specialty treatment for substance use disorders among U.S. adults. Psychiatr. Serv. 2014;65(8):1070–1073. doi: 10.1176/appi.ps.201300443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson D.L., Spear S., Marinelli-Casey P., Rawson R., Li L., Hser Y.-I. American indians/alaska natives and substance abuse treatment outcomes: positive signs and continuing challenges. J. Addict. Dis. 2011;30(1):63–74. doi: 10.1080/10550887.2010.531665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong Y., Peng C.Y. Principled missing data methods for researchers. Springerplus. 2013;2(1):222. doi: 10.1186/2193-1801-2-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enzinger A.C., Wright A.A. Reduced opioid prescribing by oncologists: progress made, or ground lost? NCI: J. Natl. Cancer Inst. 2021;113:225–226. doi: 10.1093/jnci/djaa112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farahmand P., Arshed A., Bradley Mark V. Systemic racism and substance use disorders. Psychiatr. Ann. 2020;50(11):494–498. doi: 10.3928/00485713-20201008-01. [DOI] [Google Scholar]
- Fazel S., Yoon I.A., Hayes A.J. Substance use disorders in prisoners: an updated systematic review and meta-regression analysis in recently incarcerated men and women. Addiction. 2017;112(10):1725–1739. doi: 10.1111/add.13877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedmann P.D., Lemon S.C., Stein M.D., D'Aunno T.A. Accessibility of addiction treatment: results from a national survey of outpatient substance abuse treatment organizations. Health Serv. Res. 2003;38(3):887–903. doi: 10.1111/1475-6773.00151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaither J.R., Shabanova V., Leventhal J.M. US National trends in pediatric deaths from prescription and illicit opioids, 1999-2016. JAMA Netw. Open. 2018;1(8) doi: 10.1001/jamanetworkopen.2018.6558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadland S.E., Wharam J.F., Schuster M.A., Zhang F., Samet J.H., Larochelle M.R. Trends in receipt of buprenorphine and naltrexone for opioid use disorder among adolescents and young adults, 2001-2014. JAMA Pediatr. 2017;171(8):747–755. doi: 10.1001/jamapediatrics.2017.0745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B., Compton W.M., Blanco C., DuPont R.L. National trends in substance use and use disorders among youth. J. Am. Acad. Child Adolesc. Psychiatry. 2017;56(9):747–754. doi: 10.1016/j.jaac.2017.06.011. e743. [DOI] [PubMed] [Google Scholar]
- Han B., Compton W.M., Jones C.M., Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003-2013. JAMA. 2015;314(14):1468–1478. doi: 10.1001/jama.2015.11859. [DOI] [PubMed] [Google Scholar]
- Kelly J.F., Myers M.G. Adolescents' participation in alcoholics anonymous and narcotics anonymous: review, implications and future directions. J. Psychoactive Drugs. 2007;39(3):259–269. doi: 10.1080/02791072.2007.10400612. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Aguilar-Gaxiola S., Berglund P.A., Caraveo-Anduaga J.J., DeWit D.J., Greenfield S.F., Kolody B., Olfson M., Vega W.A. Patterns and predictors of treatment seeking after onset of a substance use disorder. Arch. Gen. Psychiatry. 2001;58(11):1065–1071. doi: 10.1001/archpsyc.58.11.1065. [DOI] [PubMed] [Google Scholar]
- Leung J., Chiu V., Chan G.C.K., Stjepanovi´c D., Hall W.D. What have been the public health impacts of cannabis legalisation in the USA? A review of evidence on adverse and beneficial effects. Curr. Addict. Rep. 2019;6(4):418–428. doi: 10.1007/s40429-019-00291-x. [DOI] [Google Scholar]
- Liebling E.J., Yedinak J.L., Green T.C., Hadland S.E., Clark M.A., Marshall B.D. Access to substance use treatment among young adults who use prescription opioids non-medically. Subst. Abuse Treat. Prev. Policy. 2016;11(1):38. doi: 10.1186/s13011-016-0082-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipari, R.N., & Van Horn, S.L. (2013). Trends in substance use disorders among adults aged 18 or older. In The CBHSQ Report (pp. 1–10). https://www.ncbi.nlm.nih.gov/pubmed/28792721. [PubMed]
- Lipari, R., & Jean-Francois, B. (2016). Trends in perception of risk and availability of substance use among full-time college students. https://www.samhsa.gov/data/sites/default/files/report_2418/ShortReport-2418.html. [PubMed]
- Lipari R.N., Hughes A. How people obtain the prescription pain relievers they misuse. The CBHSQ report: substance abuse and mental health services administration (US), 2017. Available at: https://www.samhsa.gov/data/sites/default/files/report_2686/ShortReport-2686.html. [PubMed]
- Lu W., Muñoz-Laboy M., Sohler N., Goodwin R.D. Trends and disparities in treatment for co-occurring major depression and substance use disorders among US adolescents from 2011 to 2019. JAMA Netw. Open. 2021;4(10) doi: 10.1001/jamanetworkopen.2021.30280. -e2130280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins S.S., Fenton M.C., Keyes K.M., Blanco C., Zhu H., Storr C.L. Mood and anxiety disorders and their association with non-medical prescription opioid use and prescription opioid-use disorder: longitudinal evidence from the national epidemiologic study on alcohol and related conditions. Psychol. Med. 2012;42(6):1261–1272. doi: 10.1017/S0033291711002145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattson C.L., Tanz L.J., Quinn K., Kariisa M., Patel P., Davis N.L. Trends and geographic patterns in drug and synthetic opioid overdose deaths — United States, 2013–2019. MMWR Morb. Mortal. Wkly. Rep. 2021;70:202–207. doi: 10.15585/mmwr.mm7006a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mennis J., Stahler G.J. Racial and ethnic disparities in outpatient substance use disorder treatment episode completion for different substances. J. Subst. Abuse Treat. 2016;63:25–33. doi: 10.1016/j.jsat.2015.12.007. [DOI] [PubMed] [Google Scholar]
- Montgomery L., Burlew A.K., Haeny A.M., Jones C.A. A systematic scoping review of research on black participants in the national drug abuse treatment clinical trials network. Psychol. Addict. Behav. 2020;34(1):117–127. doi: 10.1037/adb0000483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nayar K.R., Kyobutungi C., Razum O. Self-help: what future role in health care for low and middle-income countries? Int. J. Equity Health. 2004;3(1):1. doi: 10.1186/1475-9276-3-1. -1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pergolizzi J., Breve F., Taylor R., Zampogna G., LeQuang J. The aftermath of hydrocodone rescheduling: intentional and unintended consequences. Int. J. Anesth. Res. 2017;5:377–382. [Google Scholar]
- Peterson E., Busch S. Achieving mental health and substance use disorder treatment parity: a quarter century of policy making and research. Annu. Rev. Public Health. 2018;39:421–435. doi: 10.1146/annurev-publhealth-040617-013603. [DOI] [PubMed] [Google Scholar]
- Romo E., Ulbricht C.M., Clark R.E., Lapane K.L. Correlates of specialty substance use treatment among adults with opioid use disorders. Addict. Behav. 2018;86:96–103. doi: 10.1016/j.addbeh.2018.03.012. [DOI] [PubMed] [Google Scholar]
- Sarvet A.L., Wall M.M., Keyes K.M., Cerda ‘.M., Schulenberg J.E., O'Malley P.M., Johnston L.D., Hasin D.S. Recent rapid decrease in adolescents’ perception that marijuana is harmful, but no concurrent increase in use. Drug Alcohol Depend. 2018;186:68–74. doi: 10.1016/j.drugalcdep.2017.12.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seitz N.-N., Lochbühler K., Atzendorf J., Rauschert C., Pfeiffer-Gerschel T., Kraus L. Trends in substance use and related disorders: analysis of the epidemiological survey of substance abuse 1995 to 2018. Dtsch. Arztebl. Int. 2019;116(35–36):585–591. doi: 10.3238/arztebl.2019.0585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh R., Pushkin G.W. How should medical education better prepare physicians for opioid prescribing? AMA J. Ethics. 2019;21(8):636–641. doi: 10.1001/amajethics.2019.636. [DOI] [PubMed] [Google Scholar]
- Smart R., Pacula R.L. Early evidence of the impact of cannabis legalization on cannabis use, cannabis use disorder, and the use of other substances: findings from state policy evaluations. Am. J. Drug Alcohol Abuse. 2019;45(6):644–663. doi: 10.1080/00952990.2019.1669626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squeglia L.M., Jacobus J., Tapert S.F. The influence of substance use on adolescent brain development. Clin. EEG Neurosci. 2009;40(1):31–38. doi: 10.1177/155005940904000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahler G.J., Mennis J., DuCette J.P. Residential and outpatient treatment completion for substance use disorders in the U.S.: moderation analysis by demographics and drug of choice. Addict. Behav. 2016;58:1873. doi: 10.1016/j.addbeh.2016.02.030. -6327 (Electronic)) [DOI] [PubMed] [Google Scholar]
- Sterling S., Weisner C., Hinman A., Parthasarathy S. Access to treatment for adolescents with substance use and co-occurring disorders: challenges and opportunities. J. Am. Acad. Child Adolesc. Psychiatry. 2010;49(7):637–646. doi: 10.1016/j.jaac.2010.03.019. quiz 725-636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringfellow E.J., Kim T.W., Gordon A.J., Pollio D.E., Grucza R.A., Austin E.L., Johnson N.K., Kertesz S.G. Substance use among persons with homeless experience in primary care. Subst. Abus. 2016;37(4):534–541. doi: 10.1080/08897077.2016.1145616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . 2019. National Survey on Drug Use and Health.https://www.samhsa.gov/data/data-we-collect/nsduh-national-survey-drug-use-and-health Retrieved April 29 from. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . 2019. Substance Misuse Prevention For Young Adults.https://store.samhsa.gov/sites/default/files/d7/priv/pep19-pl-guide-1.pdf [Google Scholar]
- Substance Abuse and Mental Health Services Administration . HHS Publication No; 2020. Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey On Drug Use and Health.https://www.samhsa.gov/data/release/2019-national-survey-drug-use-and-health-nsduh-releases PEP20-07-01-001, NSDUH Series H-55) [Google Scholar]
- Substance Abuse and Mental Health Services Administration . O. o. B. H. E. S. A. a. M. H. S. Administration; 2020. The Opioid Crisis and the Black/African American Population: An Urgent Issue.https://store.samhsa.gov/sites/default/files/pep20-05-02-001.pdf [Google Scholar]
- Tambling R.R., Russell B., D'Aniello C. Where is the family in young adult substance use treatment? The case for systemic family therapy for young adults with substance use disorders. Int. J. Ment. Health Addict. 2021:1–12. doi: 10.1007/s11469-020-00471-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Wu D., Chan A., Chang C.H., Lee V.W., Nichol M.B. Temporal trend of opioid and nonopioid pain medications: results from a national in-home survey, 2001 to 2018. Pain Rep. 2022;7(3):e1010. doi: 10.1097/PR9.0000000000001010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen H., Hockenberry J.M., Druss B.G. The effect of medical marijuana laws on marijuana-related attitude and perception among us adolescents and young adults. Prev. Sci. 2019;20(2):215–223. doi: 10.1007/s11121-018-0903-8. [DOI] [PubMed] [Google Scholar]
- Windle M., Miller-Tutzauer C., Barnes G.M., Welte J. Adolescent perceptions of help-seeking resources for substance abuse. Child Dev. 1991;62(1):179–189. doi: 10.1111/j.1467-8624.1991.tb01523.x. [DOI] [PubMed] [Google Scholar]
- Wu L.T., Blazer D.G., Li T.K., Woody G.E. Treatment use and barriers among adolescents with prescription opioid use disorders. Addict. Behav. 2011;36(12):1233–1239. doi: 10.1016/j.addbeh.2011.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]