Abstract
Objective:
We describe a structured approach to developing a standardized curriculum for surgical trainees in East, Central, and Southern Africa (ECSA).
Summary Background Data:
Surgical education is essential to closing the surgical access gap in ECSA. Given its importance for surgical education, the development of a standardized curriculum was deemed necessary.
Methods:
We utilized Kern’s 6-step approach to curriculum development to design an online, modular, flipped-classroom surgical curriculum. Steps included global and targeted needs assessments, determination of goals and objectives, the establishment of educational strategies, implementation, and evaluation.
Results:
Global needs assessment identified the development of a standardized curriculum as an essential next step in the growth of surgical education programs in ECSA. Targeted needs assessment of stakeholders found medical knowledge challenges, regulatory requirements, language variance, content gaps, expense and availability of resources, faculty numbers, and content delivery method to be factors to inform curriculum design. Goals emerged to increase uniformity and consistency in training, create contextually relevant material, incorporate best educational practices, reduce faculty burden, and ease content delivery and updates. Educational strategies centered on developing an online, flipped-classroom, modular curriculum emphasizing textual simplicity, multimedia components, and incorporation of active learning strategies. The implementation process involved establishing thematic topics and subtopics, the content of which was authored by regional surgeon educators and edited by content experts. Evaluation was performed by recording participation, soliciting user feedback, and evaluating scores on a certification examination.
Conclusions:
We present the systematic design of a large-scale, context-relevant, data-driven surgical curriculum for the ECSA region.
Keywords: curriculum design, curriculum development, global surgery, Surgical education, surgical curriculum, sub-Saharan Africa
Mini-abstract: We describe the design of a large-scale, standardized, surgical curriculum for trainees in East, Central, and Southern Africa using Kern’s 6-step approach. This systematic process resulted in the development of an online, modular, flipped-classroom surgical curriculum, written by regional surgical educators and with relevance to the sub-Saharan African context.
INTRODUCTION
Five billion people worldwide lack access to surgical care, with the greatest disparities in the rural areas of low- and middle-income countries (LMICs), like those of sub-Saharan Africa (SSA).1,2 Expanding the surgical workforce is necessary for developing surgical care and improving patient access.3 Therefore, surgical education is essential to closing this access gap in LMICs.4–6 As surgical training expands throughout SSA, there is increased recognition of the need to enhance the quality of education.7 Standardized curricula have increasingly become part of surgical education8 worldwide, mainly to identify and emphasize the skills and knowledge necessary for surgeons at the completion of training.9
The numerous benefits of standardized curricula are significant given the ongoing increases in required medical knowledge for surgeons.10 A standardized curriculum ensures trainees receive a uniform and targeted surgical education that enables flexibility within accepted parameters as a surgeon’s career progresses, allows for learning that does not rely solely on case volumes or case-mix that are variable in training, and may improve in-training examination performance.9–12
In 2005, the American Surgical Association Blue Ribbon Committee report on surgical education called for a national, standardized surgical curriculum to provide a foundational framework for surgical residency education in the United States.9 Consequently, the Surgical Council on Resident Education program was developed.13 Similarly, the United Kingdom-based Intercollegiate Surgical Training Program was created in 2007 to provide standardization of surgical curriculum for UK-trained surgeons.14,15 Despite the development of large-scale curricula for surgical training in high-income countries, similar standardized curricula have not been designed for training programs in SSA.5 Indeed, curricula that have input from and relevance to those working in SSA are recognized as a necessary part of surgical education in this region.16–19
The College of Surgeons of East, Central, and Southern Africa (COSECSA) is the largest surgical training institution in SSA. With training programs in 14 member countries and 6 affiliate countries,20 COSECSA aims to advance surgical education in rural settings.21 The institution offers a collegiate training program with a 2-year-plus-3-year graduate medical education structure. The first 2 years (the membership program) create a common foundation of surgical knowledge and practice. Following these 2 years of training, learners undergo written and oral examinations for certification as Members of the College of Surgeons (MCS).21,22 They then progress to fellowship training in general surgery or a surgical sub-specialty like orthopedics or pediatric surgery. COSECSA has 113 MCS training programs with 327 MCS trainees. There were 144 member candidates in the most recent year.
Despite active training programs, COSECSA has not had a standardized curriculum program for trainees. To address this void, we developed and implemented a standardized curriculum designed for MCS trainees using Kern’s 6-step approach to curriculum development, a widely endorsed process within medical education that allows the complexities of large-scale curriculum design to be anticipated and addressed.23,24 This method provided a comprehensive framework for designing a data-driven curriculum with a focus on currently established best educational practices. This study describes the process of curriculum design, development, and implementation according to that framework. In a follow-up study, we describe the outcomes of the successful development of our robust curriculum.
STEP 1: PROBLEM IDENTIFICATION AND NEEDS ASSESSMENT
There has been a lack of standardized curriculum for surgical trainees in the region,19,22,25 including COSECSA trainees, and curriculum decisions have depended on each training program and program director.21,26 The COSECSA Education and Examinations Committees recognized this deficit as contributing to inadequate continuity and uniformity in training. This was further observed in written and oral certification examination performance. Therefore, a standardized curriculum was identified by the committees as an essential next step in the growth of surgical education programs in East, Central and Southern Africa (ECSA). The COSECSA Education Committee endorsed the process of curriculum development.
STEP 2: TARGETED NEEDS ASSESSMENT
Several unique factors were identified in assessing the characteristics, needs, and available resources of the trainees and faculty. These were identified through formal and informal discussions with trainees and surgical faculty at several COSECSA programs. Additional input was solicited from members of the Education and Examinations Committees of COSECSA. Findings from more than 20 structured interviews and focus groups, including more than 60 learner and educator participants in 5 countries, informed the design of the curriculum. The questions used for these interviews and focus groups are listed in Table 1. Specific factors uncovered during our needs assessment are described below.
TABLE 1.
COSECSA Educational Needs Assessment Questions
| Questions Used for Faculty | Questions Used for Trainees |
|---|---|
| Describe your position in the surgical education program here. What are your responsibilities? | Describe your position in the surgical education program here. What year? What responsibilities do you have in that year? |
| Tell me about the process of selecting trainees. What do you look for? | Tell me about the process of choosing where to train. |
| Tell me about the graduates of your program. | How did you ultimately end up here? |
| Describe a typical day for you. | Describe a typical day for you. |
| Describe the variety of patients you see. • Do residents rotate through any different locations, subspecialties? • If so, what has been especially valuable? What suggestions do you have to improve any gaps in patient population? |
Describe the variety of patients you care for. • Do you rotate through any different locations, subspecialties? • If so, what has been especially valuable? • What suggestions do you have to improve any gaps in patient population? |
| Tell me about the dedicated educational time here. • Who teaches? How often do you meet? • Is there a schedule? Who decides what topics are covered? • Tell me about topics that have been especially valuable. • What topics have you found challenging to teach? Difficult for learners? |
Tell me about the dedicated educational time here. • Who teaches? How often do you meet? • Is there a schedule? Who decides what topics are covered? • Tell me about topics that have been especially valuable. Tell me about a time that you learned something that changed how you cared for your patients. • What topics have been especially difficult? |
| Tell me about rounds. • Who participates? • Describe the teaching that takes place on rounds. |
Tell me about rounds. • Who participates? • Describe the learning that you get from rounds. |
| Tell me about learning in the operating room. • How does trainee responsibility progress through the years? • What is your style of teaching in the operating room? • What cases are most common? • What cases are most important for a surgeon to know? • What happens if a case goes poorly? Tell me about how you handle complications. |
Tell me about learning in the operating room. • How does your responsibility change as you progress through the years? • What cases are most common? • What cases are most important for a surgeon to know? • What happens if a case goes poorly? Tell me about how you handle complications. |
| Tell me about self-directed learning for trainees. • Do you recommend books? Journals? Online content? • What do you think is most utilized by trainees? • Are there barriers to accessing internet-based tools? |
Tell me about learning on your own. • Do you use books? Journals? Online content? • What has been the best for you? • Are there barriers to accessing internet-based tools? |
| • How do trainees prepare for the COSECSA examinations? | What was your experience like taking the COSECSA examination(s)? • How did you prepare? • Did the written test content seem representative? Did the oral test content seem representative? |
| How do you assess trainees? What happens if there is a trainee who is struggling? | What happens if there is a trainee who is struggling? |
| How do you think the training here prepares trainees well to practice on their own? | How do you think your training has prepared you well to practice on your own? |
| What suggestions do you have that could make it better? | What suggestions do you have to make it better? |
Medical Knowledge Challenges
COSECSA covers a geographically large area with tremendous diversity and heterogeneity. There is significant variability in medical education throughout ECSA, and baseline medical knowledge differs considerably upon matriculation into surgical training.21 Trainees must overcome these knowledge discrepancies to achieve a standard and acceptable level of competence in surgical training.
Regulatory Body Requirements
National regulatory bodies have different requirements and expectations for graduate medical education throughout the ECSA region. Medical boards and ministries of health that oversee training program accreditation and surgeon licensing increasingly require minimum standards of basic science course work to ensure appropriate quality of education and training within their countries.
Language Variance
The English language abilities of COSECSA surgical trainees were recognized to be quite varied, evoking concern for surgical education stakeholders. Though COSECSA as an institution decided that all surgical education should be conducted in English, undergraduate medical education is conducted in four languages (English, French, Portuguese, and Arabic) within the region.27 This results in inconsistent English-language comfort for learners entering COSECSA training programs.
Content Gaps
Content gaps occur when exclusively noncontext-tailored curriculum sources are used, either online curricula or textbooks.17,28,29 Historically, surgical textbooks have been the primary source of the core material required for trainees; yet these lack the comprehensiveness necessary for training surgical trainees in SSA. Most English-language surgical textbooks are written by North American or European authors, and the content focuses on disease processes common to those regions and highlights resources frequently unavailable in ECSA. Further, such textbooks often exclude disease processes frequently or exclusively seen in SSA, like typhoid intestinal perforations, hydatid disease, and rheumatic heart disease. Images in the most commonly used medical textbooks do not represent physical examination findings as they appear on darker skin tones.30 Additionally, general surgeons in SSA necessarily have a breadth of practice beyond what is classified as general surgery in high-resource contexts, performing surgical care in areas like obstetrics and gynecology, urology, neurosurgery, and orthopedics.19,31 Rarely, if ever, are these specialties covered adequately in general surgery curricula from high-resource areas.
Expense and Availability
Beyond the knowledge gaps that can result for trainees, textbooks are expensive, difficult to ship, and require re-purchasing with new editions.18 E-learning resources from high-income countries often require paid subscriptions, even if initially made available through free trials or as part of a study.11,32 A prior pilot program has demonstrated a favorable response to existing online educational content when made available to trainees within SSA.32 However, typically, subscription costs are substantial and content inaccessible.
Limited Surgical Faculty
Several educators raised the issue of the paucity of surgical educators and faculty at many training programs in SSA.5,7,18,25 On average, there are 3 to 4 surgical faculty per COSECSA training program (internal communication). These faculty are responsible for the clinical care of patients in addition to the administrative and educational responsibilities related to surgical training. Further, they often do not have advanced or subspecialty surgical training, which at times limits comfort with teaching certain topics.7 We identified a desire for an educational intervention to offload the work burden on these faculty.
Online Resource Availability and Suitability for Content Delivery
Web-based curricula have been part of surgical education for many years,33,34 increasing substantially during the COVID pandemic.35 Although e-learning has grown in popularity, trainees have a desire for curricula that combine both web-based content and traditional teaching.34 Such technology-based blended learning models like the flipped classroom have had high receptivity in high-income countries,36 improving student learning compared to traditional teaching techniques.37 Widening mobile internet spread and expanding penetration of tablets, smartphones, and other internet-connected devices38 have provided the opportunity to deliver a web-based surgical curriculum within SSA.18,32 Additionally, learners within COSECSA training programs have become facile with an online learning platform, School for Surgeons (www.schoolforsurgeons.net). Created as part of the collaboration between COSECSA and the Royal College of Surgeons in Ireland (RCSI) and hosted by RCSI, trainees were already required to engage with journal articles and case scenarios throughout their MCS years.32,39 The use of an online learning platform was facilitated by the requirement for internet access for each training program, which is a prerequisite for certification as a COSECSA training program. This provided the opportunity for consideration of a web-based curriculum.
STEP 3: GOALS AND OBJECTIVES
Based on the targeted needs assessment, several broad goals and specific objectives were established for the curriculum.
Uniformity and Consistency
Standardized curricula should provide consistency in educational content. We recognized the need for our curriculum to create uniformity that would allow for a more consistent approach to surgical education within our context. While accounting for the heterogeneity of surgical disease in ECSA that our trainees must know, we sought to cover the foundational content necessary for surgeons practicing anywhere in the world. We further recognized that creating a curriculum that sufficiently covers this foundational material would likely satisfy the requirements of the regulatory bodies within various countries throughout the region. Considering the heterogeneity of SSA and the difficulties inherent in using content from high-resource settings,25,28 we set a goal of creating a context-specific curriculum regarding pathologies, available resources, skin color and gender representation, and breadth of surgical practice in our region. We set an objective that learners who used the curriculum would show improvement in medical knowledge assessed subjectively, via self- and instructor-report, and objectively, through improved certification examination scores upon completion of MCS training.
Best Educational Practices
Data-driven application of best educational practices should inform curriculum design. Given our opportunity to build a novel curriculum, we thought it prudent to use available evidence and incorporate current best educational practices. Active learning, supported by a wealth of data in undergraduate and graduate medical education, is a method of intentionally engaging the learner through educational experiences and reflection.40 This contrasts with the delivery of information to learners passively, as often occurs with traditional lecture-based teaching.41 Interactive teaching has been found to improve engagement, information retention, problem-solving, critical-thinking skills, and motivation in learning.41–46 The use of multimedia components further engages the learner in the education process,47 improving retention of information and the ability to transfer learned information to novel settings.48,49 Presentation of material using a more conversational and informal communication style has been shown to enhance retention of presented material,50 an important consideration considering the language challenges in our context. Given these benefits, we sought to incorporate active learning components into the curriculum, both in structure and content delivery. We set as an objective that authors and content creators should engage the use of multimedia components and focus on simplicity of the written text.
Reduce the Burden on Faculty Trainers
An efficient curriculum should reduce the burden on surgical educators.7 Given the low numbers of faculty and the scarcity of subspecialty expertise25 in training many programs, we determined that the curriculum should provide the resources necessary for any surgeon to teach, regardless of area of expertise. We set an objective to create a robust facilitator’s version of the curriculum with teaching aids to ease faculty workload.
Ease of Content Delivery and Updates
The curriculum should allow for ease of content delivery and updates. Given the large geographic area and marginal resources in ECSA, we prioritized ease of transfer of materials and limiting costs associated with the curriculum. We also focused on making the process of updating material and keeping content current more facile to better incorporate solicited feedback from users. We set as an objective the adoption of a platform that could be frequently updated and would remain accessible to trainees.
STEP 4: EDUCATIONAL STRATEGIES
Content
We determined necessary foundational material by evaluating existing surgical curricula and textbooks to formulate a 2-year content outline. The result was a year of content (Year A) focusing on underlying surgical principles and a year (Year B) focusing on organs and organ systems (Table 2). Rather than 1 year of content necessarily preceding the other, we opted to create a rolling curriculum; either year of content could be completed in a trainee’s first year of training. This was intended to make less work for faculty in training programs.
TABLE 2.
Thematic Topics and Weekly Modular Subtopics
| Year A | Year B | ||
|---|---|---|---|
| Topics | Weekly Modular Subtopics | Topics | Weekly Modular Subtopics |
| Statistics and Research Methods | Evidence-Based Surgery, Statistical Terminology, and Ethical Research | Breast | Anatomy, Physiology, and Benign Breast Disease |
| The Basics of Biostatistics | Malignant Breast Disease | ||
| Oncology | Biology of Cancer | Endocrine | Thyroid |
| Etiology of Cancer | Parathyroid and Adrenals | ||
| Principles of Cancer Treatment | Hepato-Pancreatico-Biliary | Liver | |
| Wound Healing | Physiology of Normal Wound Healing | Pancreas | |
| Pathophysiology of Impaired Wound Healing | Gallbladder and Extrahepatic Biliary System | ||
| Wound Classification and Identification | Pediatric Surgery | Pediatric Surgery 1 | |
| Wound Closure and Management | Pediatric Surgery 2 | ||
| Fluids and Electrolytes | Normal Body Compartments, Fluid Balance, and Electrolytes | Soft Tissue Sarcomas | Soft Tissue Sarcomas |
| Types of Intravenous Fluids, How to Treat Fluid Abnormalities | Skin and Soft Tissue | Skin and Subcutaneous Tissue | |
| Electrolyte Abnormalities and Considerations in Specific Patients | Plastic Surgery | Plastic and Reconstructive Surgery | |
| Acid-Base Disorders | Urology | Urology | |
| Systemic Response to Injury | Overview of Systemic Response to Injury | Gynecology | Gynecology |
| Mediators of Inflammation | Neurosurgery | Neurosurgery | |
| Surgical Metabolism | Vascular | Anatomy and Physiology | |
| Shock | Understanding Shock and Hypovolemic Shock | Mesenteric Ischemia, Aortic Disease, Visceral Vascular Conditions | |
| Bradycardic, Cardiogenic, and Obstructive Shock | Cerebrovascular Disease, Venous and Lymphatic Conditions | ||
| Vasodilatory Shock, Including Septic and Neurogenic Shock | Orthopedic Surgery | Orthopedic Oncology and Pediatric Orthopedics | |
| Differentiation of Shock | Joints and Sports Medicine | ||
| Hemostasis | Physiology of Hemostasis | Hand and Wrist | |
| Congenital and Acquired Impairments of Coagulation, Prothrombotic States | Thoracic | Anatomy, Physiology, and Benign Disease of the Lung; Pleura | |
| Transfusion Principles | Trachea, Chest Wall, and Mediastinum | ||
| Trauma | Initial Evaluation and Resuscitation of the Trauma Patient | Solitary Pulmonary Nodules, Premalignant and Malignant Lung Conditions | |
| General Principles of Trauma and Surgical Intensive Care Management | Cardiac | Acquired and Congenital Heart Disease | |
| Treatment of Specific Injuries | Head and Neck | Ear, Nose and Sinuses, and Salivary Glands | |
| Treatment of Specific Injuries | Oral Cavity, Larynx, and Neck | ||
| Traumatic Injury in Special Populations: Pediatric, Geriatric, Pregnancy | Abdomen | Abdominal Wall, Omentum, Mesentery, and Retroperitoneum | |
| Burns | Pathophysiology and Classification of Burns | Spleen | |
| Initial Treatment and Management of Burns | Inguinal Hernias | ||
| Other Considerations in Treatment and Complications of Burns | Alimentary Tract | Esophagus and Hiatal Hernias 1 | |
| Surgical Infections | Immunity and Clinical Microbiology | Esophagus and Hiatal Hernias 2 | |
| Infections in Surgical Patients | Stomach 1 | ||
| Anesthesia and Perioperative Care | Pharmacology and Anesthetic Agents | Stomach 2 | |
| Perioperative Considerations | Small Intestine | ||
| Colon, Rectum, and Anus 1 | |||
| Colon, Rectum, and Anus 2 | |||
| Colon, Rectum, and Anus 3 | |||
| Appendix | |||
Methods and Curriculum Structure
Given the COSECSA requirement of internet access for trainees, the support afforded by the COSECSA-RCSI collaboration, and the established use of online surgical training resources through the School for Surgeons e-learning platform, a web-based delivery vehicle for the curriculum was thought to be ideal. This was deemed feasible due to the increasing use of mobile internet in the region.38 Internet-based distribution of content facilitated several of the goals for the curriculum, including avoiding the purchasing and shipping of textbooks, allowing for ease of delivery and content updates, and supporting the increased use of multimedia elements. Although e-learning seemed an excellent option, we decided to make an offline version of the curriculum available to programs with internet stability concerns.
We designed the curriculum with a flipped-classroom structure. We combined an online module created through the Articulate Rise 360 e-learning software (Articulate, New York, NY, USA) and a semi-structured group teaching session with suggested prompts. Each module consists of specific learning objectives, a precontent multiple-choice assessment, content sections for the learning material, and a postcontent multiple-choice assessment. Although a minimum score is not mandated for the precontent formative assessment, trainees must complete this assessment to access the content. After completing the content, the postcontent assessment requires a score of 80% for the module to be recorded as complete. All material remains unlocked for learner reference during the postcontent assessment, and unlimited attempts are allowed to obtain a “passing” score.
Active learning techniques were incorporated into each module. These included case scenarios, “clinical connections” that relate learned concepts in clinically applicable ways, and strategic “knowledge check” prompts and questions that assess the learner’s understanding of the concepts. These strategies help to ensure the learner remains engaged in learning and is retaining presented information. Multimedia content in each module included images, interactive images, GIFs, activities like matching and sorting games, and videos. A video demonstrating a portion of the content from the Spleen module is included as Supplemental Digital File 1, http://links.lww.com/AOSO/A102.
Independent completion of the module was to prepare learners to participate in a group teaching session. Prompts were provided with each week of content to help structure the group time. The prompts incorporated the learning objectives, reinforcing essential concepts within the content through active learning activities. Prompts included case-based discussions, role-playing exercises, competitions, and low-fidelity simulation projects.
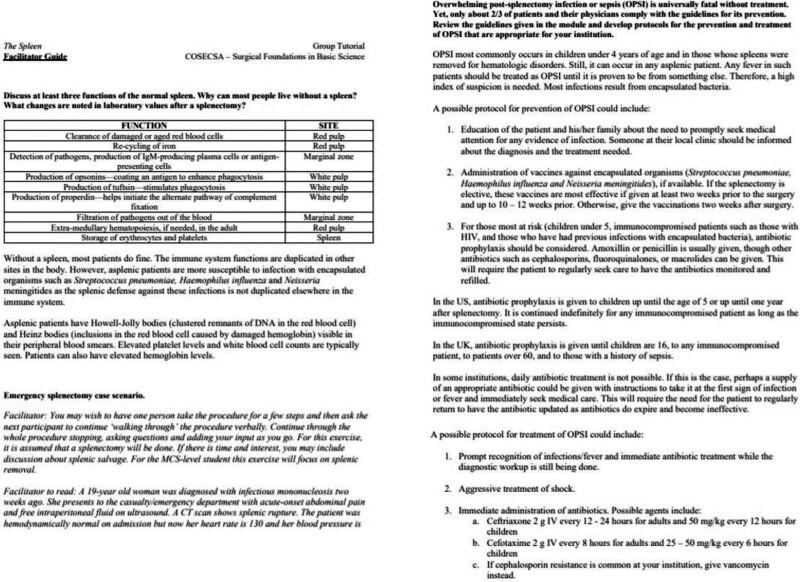
Given the goal of easing the burden on surgical faculty at training programs, we opted to provide the curriculum in 2 formats. One version is accessible to trainees and requires completion of the precontent multiple-choice assessment and a mandatory 80% on the postcontent multiple-choice assessment. Although both assessments can be repeated as many times as necessary or desired, correct answers are not revealed, requiring more work on the part of the learner. The second version is accessible only to surgical faculty or senior trainees who may facilitate group times and does not require completing the assessments. Correct answers to questions are also included in this version. Importantly, ideal solutions are provided for each group tutorial prompt so that minimal preparation is needed to facilitate group teaching activities (Fig. 1).
FIGURE 1.
Sample portions of facilitator guide for spleen (Year B).
STEP 5: IMPLEMENTATION
Thematic topics were outlined to ensure each subject was covered as comprehensively as necessary. Each topic was divided into 2 to 5 subtopics, depending on the amount of material to be covered. A module was created for each subtopic. We solicited the cooperation of surgeons and educators with significant experience in SSA to write content. We determined that regional surgical educators would be best suited as content writers to achieve the goal of context relevance within the curriculum. Content authors were identified by utilizing surgical education networks and personal contacts (A.P., K.H., R.W., A.B., and R.P.). Forty-seven individuals contributed material to the curriculum, of which 35 are surgical educators in ECSA. Contributions ranged from workshop participation involving content outline to authorship of one or more weeks of content, which included text writing, image curation, multiple-choice question creation, and development of group tutorial prompts and guides. Each author was given instructions to focus on the readability and simplicity of the written text and asked to emphasize the basic science (anatomy, physiology, histology, pathophysiology) aspects of each topic in addition to evaluation and diagnosis. Although management was discussed, a strong emphasis on operative techniques and complex decision-making was deemed more appropriate for the senior years of surgical training. Thus, this was not as heavily considered.
Written content submitted from the authors was entered into Rise 360. Multimedia components were added throughout the content. To avoid copyright infringement, content was chosen that was either (1) available to COSECSA trainees through the School for Surgeons library, (2) usable under creative commons licensing or within the public domain, (3) allowable for educational classroom usage, (4) hyperlinked for curated content, or (5) created by one of the authors or editors. Where relevant, permission was obtained for inclusion within the modules. Where possible, we used images and graphics that are appropriately representative of darker skin tones. After completing each module, editorial input was solicited from at least 2 content experts, who reviewed and edited the content for accuracy. Volunteer medical students reviewed each module for clarity, understandability, and grammatical correctness.
The curriculum was uploaded to the COSECSA education platform, School for Surgeons, as the Surgical Foundations in Basic Science curriculum. The platform allows tracking of participation and completion of the modules by each registered COSECSA MCS trainee. Thematic topics were uploaded and released monthly as completed. Each thematic topic had 2 to 5 subtopic weeks of modular content. Trainees were instructed to complete a module over a 1-week timeframe. Faculty were encouraged to choose a weekly time for the group teaching period. Once uploaded, all modules remain available to trainees and faculty. COSECSA now requires participation in the modular curriculum.
In preparation for the rollout of the modular curriculum, trainers and trainees were provided with an orientation module that discussed the purpose, format, outline, and access logistics of the curriculum. Several teaching and training sessions were held for program directors and faculty to become familiar with the modules’ structure, setup, and use. The modules were offered to faculty on USB drives in a fully functional offline HTML format. All content is designed to be utilized for educational purposes only. The curriculum is without any cost to trainees or trainers and is nonprofit.
STEP 6: EVALUATING THE EFFECTIVENESS
The curriculum was made available for use in January 2020 by MCS trainees in the 17 COSECSA countries that had MCS training programs at that time. In the first year, 271 (96%) of trainees accessed at least 1 weekly module. Trainees completed a median of 9 of 10 thematic topics that were available in the first year. Curriculum effectiveness was assessed in several ways. Satisfaction with the curriculum and subjective judgments of learning was evaluated by qualitative and quantitative feedback responses. At the end of each week of modular content, a feedback survey was embedded as a Google form (Google LLC). This form used open- and closed-ended questions, as shown in Table 3, to assess trainee perceptions of learning and confidence related to the learning objectives, quality of the modular content, and whether the learner experienced challenges, found the content helpful, or had suggestions for improvements. Therefore, all participants were included as part of the census strategy for feedback. We were also interested in the curriculum’s impact on performance on a standardized written certification examination. Following 2 years of surgical training, candidates must take a written membership examination, which qualifies them for an objective structured clinical examination. Successful completion of both the written and oral examinations certifies the trainee as an MCS and qualifies the learner for ongoing training in general surgery or a surgical subspecialty. Comparison of the performances of those trainees who had completed modules with those who had not could demonstrate an objective measure of the effectiveness of the curriculum.51 Module completion for each trainee was electronically tracked through the learning management system.
TABLE 3.
Postmodule Feedback Survey Embedded as a Google Form
| Question | Response |
|---|---|
| Please rate the amount of learning you experienced in each of the following areas, as a result of this module (asked for each learning objective). | None at all A small amount A moderate amount A large amount |
| Please rate your confidence level in achieving each of the following objectives, as a result of this module (asked for each learning objective). | No confidence Slight confidence Moderate confidence High confidence |
| Please rate the quality of questions asked in the quizzes. | Poor Fair Good Very good |
| Please rate the value of the online module content (text, diagrams, pictures, videos). | Poor Fair Good Very good |
| How easy was the online module to use? | Very easy Somewhat easy Somewhat difficult Very difficult |
| Please list any specific technical challenges or issues you encountered while using the online module. | Free response |
| Please list any components of the module that were particularly helpful. | Free response |
| Please provide any suggestions on how to improve this module. | Free response |
LESSONS LEARNED AND FUTURE DIRECTIONS
By following an established and accepted framework for curriculum design, we were able to anticipate and address the needs and desires of surgical faculty and trainees, incorporating these findings into the design of the MCS curriculum. This reduced speculation as to what components and factors would best serve the trainers and trainees in our region. Given the heterogeneity of the learning environments across such a vast geographical region, upfront needs evaluations and translating those to discrete goals and objectives, we believe, saved tremendous time and frustration in the process. It also allowed the opportunity to merge educational theory and best practices with the practical needs of surgeons in a specific context. Finally, incorporating assessment structures into the curriculum allowed the prospective collection of data about outcomes, vital for improvements. In the second article of this pair,51 we describe the quantitative and qualitative results of the first year following the implementation of the curriculum and future directions for this curriculum, including ongoing revisions and updates based on feedback and beginning development of a curriculum for senior general surgical trainees.
CONCLUSIONS
Substantial strides have been made in designing a standardized surgical curriculum for trainees in ECSA, written by regional contributors and reflecting context-specific pathologies and resource availability. Importantly, this curriculum incorporates current best educational practices and is data-driven in its flipped-classroom structure and inclusion of active learning techniques and multimedia content. Use of Kern’s 6-step process for curriculum development enabled the successful design and implementation of this large-scale, novel curriculum. As surgical trainees throughout SSA utilize this curriculum, we expect it will improve surgical education and advance surgical care and quality in a region of great need.
Supplementary Material
Footnotes
Published online 2 March 2022
Disclosure: The authors declare that they have nothing to disclose.
Data: Supporting data underlying this article may be available upon request to the corresponding author.Author Justification for Manuscript: Design of a novel online, modular, flipped-classroom surgical curriculum for East, Central, and Southern Africa. All authors listed in this article meet the criteria for authorship under Annals of Surgery guidelines. As this is a multi-national, large-scale initiative, there are numerous collaborators with various levels of involvement. We have tried to include all individuals who have provided a meaningful contribution to the design of the curriculum and thus have included all individuals who authored a week’s worth of content. Given the structure of this article as describing a curriculum design and implementation, written submission of content is considered in lieu of data acquisition as significant to the implementation process. All authors have given final approval of the version to be submitted. A.P. made substantial contributions to the conception, design, and authorship of the modular content (acquisition of data), to the design of this study, analysis and interpretation of data, and to writing the article. K.H. made substantial contributions to the conception and design of the curriculum and has critically revised the article. B.S. made substantial contributions to the authorship of the modular content (acquisition of data) and has critically revised the article. M.B., C.B., N.C., R.D., J.D., D.E., A.F., J.K., R.K., F.K., P.K., J.L., H.M., V.M., A.McC., P.M., E.N., W.N., P.O., D.O., M.P., S.R., K.R., K.S., J.S., D.S., M.W., and M.W. made substantial contributions to the authorship of the modular content (acquisition of data) and have reviewed and revised any necessary components of the article. D.M., E.O’F., and N.B. made substantial contributions to the conception and design of the curriculum and have critically revised the article. L.T. has substantially contributed to analysis and interpretation of data and has critically revised the article. R.W. and A.B. made substantial contributions to the conception, design, and authorship of the modular content (acquisition of data) and have critically revised the article. R.P. has substantially contributed to the conception, design, and authorship of the modular content (acquisition of data), to the design of this study, analysis and interpretation of data, and writing and critical revision of the article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.annalsofsurgery.com).
REFERENCES
- 1.Meara JG, Leather AJ, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386:569–624. [DOI] [PubMed] [Google Scholar]
- 2.Alkire BC, Raykar NP, Shrime MG, et al. Global access to surgical care: a modelling study. Lancet Glob Health. 2015;3:e316–e323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luboga S, Macfarlane SB, von Schreeb J, et al. ; Bellagio Essential Surgery Group (BESG). Increasing access to surgical services in sub-Saharan Africa: priorities for national and international agencies recommended by the Bellagio Essential Surgery Group. PLoS Med. 2009;6:e1000200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blanchard RJ, Merrell RC, Geelhoed GW, et al. Training to serve unmet surgical needs worldwide. J Am Coll Surg. 2001;193:417–427. [DOI] [PubMed] [Google Scholar]
- 5.Rickard J. Systematic review of postgraduate surgical education in low- and middle-income countries. World J Surg. 2016;40:1324–1335. [DOI] [PubMed] [Google Scholar]
- 6.O’Neill JA, Jr, Hansen EN, Nyagetuba JM, et al. A plan for surgical education in low-and middle-income countries. J Trauma Acute Care Surg. 2017;83:784–787.. [Google Scholar]
- 7.Galukande M, Luboga S, Elobu E. Challenges facing surgical training in the Great Lakes region in sub-Saharan Africa: a review article. East Cent Afr J Surg. 2013;18:3–11.. [Google Scholar]
- 8.Bell RH, Jr. Graduate education in general surgery and its related specialties and subspecialties in the United States. World J Surg. 2008;32:2178–2184. [DOI] [PubMed] [Google Scholar]
- 9.Debas HT, Bass BL, Brennan MF, et al. ; American Surgical Association Blue Ribbon Committee. American Surgical Association Blue Ribbon Committee Report on Surgical Education: 2004. Ann Surg. 2005;241:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lambert DR, Lurie SJ, Lyness JM, et al. Standardizing and personalizing science in medical education. Acad Med. 2010;85:356–362. [DOI] [PubMed] [Google Scholar]
- 11.Smeds MR, Sheahan MG, Shames ML, et al. A modern appraisal of current vascular surgery education. J Vasc Surg. 2021;73:1430–1435. [DOI] [PubMed] [Google Scholar]
- 12.Kelly DM, London DA, Siperstein A, et al. A structured educational curriculum including online training positively impacts American Board of Surgery In-Training Examination Scores. J Surg Educ. 2015;72:811–817. [DOI] [PubMed] [Google Scholar]
- 13.Bell RH. Surgical Council on Resident Education: a new organization devoted to graduate surgical education. J Am Coll Surg. 2007;204:341–346. [DOI] [PubMed] [Google Scholar]
- 14.Allum W. Intercollegiate surgical curriculum programme: an evaluation. Bull Roy Coll Surg Engl. 2013;95:92–94.. [Google Scholar]
- 15.Programme ISC. About Us – ISCP, 2020. Available at: https://www.iscp.ac.uk/iscp/about-us/about-iscp/#. Accessed October 31, 2021.
- 16.Jayaram A, Pawlak N, Kahanu A, et al. Academic global surgery curricula: current status and a call for a more equitable approach. J Surg Res. 2021;267:732–744. [DOI] [PubMed] [Google Scholar]
- 17.Cameron BH, Rambaran M, Sharma DP, et al. The development of postgraduate surgical training in Guyana. Can J Surg. 2010;53:11. [PMC free article] [PubMed] [Google Scholar]
- 18.Krishnaswami S, Nwomeh BC, Ameh EA. The pediatric surgery workforce in low- and middle-income countries: problems and priorities. Semin Pediatr Surg. 2016;25:32–42. [DOI] [PubMed] [Google Scholar]
- 19.Rickard JL, Ntakiyiruta G, Chu KM. Identifying gaps in the surgical training curriculum in Rwanda through evaluation of operative activity at a teaching hospital. J Surg Educ. 2015;72:e73–e81. [DOI] [PubMed] [Google Scholar]
- 20.Mulwafu W, Fualal J, Bekele A, et al. The impact of COSECSA in developing the surgical workforce in East Central and Southern Africa. Surgeon. 2022;20:2–8. [DOI] [PubMed] [Google Scholar]
- 21.Galukande M, Ozgediz D, Elobu E, et al. Pretraining experience and structure of surgical training at a sub-Saharan African university. World J Surg. 2013;37:1836–1840. [DOI] [PubMed] [Google Scholar]
- 22.Kakande I, Mkandawire N, Thompson M. A review of surgical capacity and surgical education programmes in the COSECSA region. East Cent Afr J Surg. 2011;16:6–34.. [Google Scholar]
- 23.Chen BY, Kern DE, Kearns RM, et al. From modules to MOOCs: application of the six-step approach to online curriculum development for medical education. Acad Med. 2019;94:678–685. [DOI] [PubMed] [Google Scholar]
- 24.Sweet LR, Palazzi DL. Application of Kern’s Six-step approach to curriculum development by global health residents. Educ Health (Abingdon). 2015;28:138–141. [DOI] [PubMed] [Google Scholar]
- 25.Rickard J, Ntirenganya F, Ntakiyiruta G, et al. Global Health in the 21st century: equity in surgical training partnerships. J Surg Educ. 2019;76:9–13. [DOI] [PubMed] [Google Scholar]
- 26.O’Neill JA, Jr. A model for humanitarian outreach in today’s world. J Pediatr Surg. 2018;53:21–24.. [DOI] [PubMed] [Google Scholar]
- 27.Chen C, Buch E, Wassermann T, et al. A survey of Sub-Saharan African medical schools. Hum Resour Health. 2012;10:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Talib Z, Narayan L, Harrod T. Postgraduate medical education in Sub-Saharan Africa: a scoping review spanning 26 years and lessons learned. J Grad Med Educ. 2019;11(4 suppl):34–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lett R. International surgery: definition, principles and Canadian practice. Can J Surg. 2003;46:365–372. [PMC free article] [PubMed] [Google Scholar]
- 30.Louie P, Wilkes R. Representations of race and skin tone in medical textbook imagery. Soc Sci Med. 2018;202:38–42. [DOI] [PubMed] [Google Scholar]
- 31.Parker RK, Topazian HM, Ndegwa W, et al. Surgical training throughout Africa: a review of operative case volumes at multiple training centers. World J Surg. 2020:44:2100–2107.. [DOI] [PubMed] [Google Scholar]
- 32.Goldstein SD, Papandria D, Linden A, et al. A pilot comparison of standardized online surgical curricula for use in low- and middle-income countries. JAMA Surg. 2014;149:341–346. [DOI] [PubMed] [Google Scholar]
- 33.Jayakumar N, Brunckhorst O, Dasgupta P, et al. e-Learning in surgical education: a systematic review. J Surg Educ. 2015;72:1145–1157. [DOI] [PubMed] [Google Scholar]
- 34.Ekenze SO, Okafor CI, Ekenze OS, et al. The value of internet tools in undergraduate surgical education: perspective of medical students in a developing country. World J Surg. 2017;41:672–680. [DOI] [PubMed] [Google Scholar]
- 35.Chick RC, Clifton GT, Peace KM, et al. Using technology to maintain the education of residents during the COVID-19 pandemic. J Surg Educ. 2020;77:729–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liebert CA, Mazer L, Bereknyei Merrell S, et al. Student perceptions of a simulation-based flipped classroom for the surgery clerkship: a mixed-methods study. Surgery. 2016;160:591–598. [DOI] [PubMed] [Google Scholar]
- 37.Rotellar C, Cain J. Research, perspectives, and recommendations on implementing the flipped classroom. Am J Pharm Educ. 2016;80:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nyirenda-Jere T, Biru T. Internet development and Internet governance in Africa. Internet Soc. 2015;1–44.. [Google Scholar]
- 39.Animasahun VJ, Harrop T, Aird JJ, et al. Evaluation of an online journal club–style course on evidence-based surgery for trainees of the College of Surgeons of East, Central and Southern Africa [published online ahead of print May 13, 2021]. East Cent Afr J Surg. [Google Scholar]
- 40.Prince M. Does active learning work? A review of the research. J Eng Educ. 2004;93:223–231.. [Google Scholar]
- 41.Cooper AZ, Richards JB. Lectures for adult learners: breaking old habits in graduate medical education. Am J Med. 2017;130:376–381. [DOI] [PubMed] [Google Scholar]
- 42.McCoy L, Pettit RK, Kellar C, et al. Tracking active learning in the medical school curriculum: a learning-centered approach. J Med Educ Curric Dev. 2018;5:2382120518765135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schmidt HG, Cohen-Schotanus J, Arends LR. Impact of problem-based, active learning on graduation rates for 10 generations of Dutch medical students. Med Educ. 2009;43:211–218. [DOI] [PubMed] [Google Scholar]
- 44.Pettit RK, McCoy L, Kinney M. What millennial medical students say about flipped learning. Adv Med Educ Pract. 2017;8:487–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Morrison CD. From ‘sage on the stage’ to ‘guide on the side’: a good start. IJ-SoTL. 2014;8:Article 4. [Google Scholar]
- 46.Luc JGY, Antonoff MB. Active learning in medical education: application to the training of surgeons. J Med Educ Curric Dev. 2016;3:JMECD.S18929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shariff U, Seretis C, Lee D, et al. The role of multimedia in surgical skills training and assessment. Surgeon. 2016;14:150–163. [DOI] [PubMed] [Google Scholar]
- 48.Mayer RE. Based principles for designing multimedia instruction. Ack Dedic. 2014;59. [Google Scholar]
- 49.Issa N, Mayer RE, Schuller M, et al. Teaching for understanding in medical classrooms using multimedia design principles. Med Educ. 2013;47:388–396. [DOI] [PubMed] [Google Scholar]
- 50.Mayer RE, Fennell S, Farmer L, et al. A personalization effect in multimedia learning: Students learn better when words are in conversational style rather than formal style. J Educ Psychol. 2004;96:389. [Google Scholar]
- 51.Parker AS, Steffes BC, Hill K, et al. An online, modular curriculum enhances surgical education and improves learning outcomes in East, Central, and Southern Africa: A mixed-methods study. Ann Surg Open. 2022;1:e140. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.