Summary:
Autologous reconstruction accounts for nearly one-quarter of all breast reconstruction cases in the United States, with the abdomen functioning as the most popular donor site. This case describes a 62-year-old woman who presented to our clinic with a remote history of estrogen receptor+/progesterone+ breast cancer and bilateral implant-based reconstruction. After grade IV capsular contracture of her left breast, she presented for autologous reconstruction. Due to her body habitus and prior belt lipectomy, deep inferior epigastric perforator flap reconstruction was contra-indicated. The thoracodorsal artery perforator (TDAP) flap is well described in the literature, and was chosen as an alternative salvage procedure to avoid latissimus harvest and the need for implants. The TDAP flap is often limited in volume and prone to distal tip necrosis, limiting its use in breast reconstruction. We have previously demonstrated the utility of the surgical delay phenomenon in improving the reliability of superficial inferior epigastric artery free flap breast reconstruction. In this case, we demonstrate the surgically delayed TDAP flap as a viable alternative to the latissimus flap with implants for bilateral total autologous breast reconstruction.
One in every eight women in the United States will be diagnosed with breast cancer, and one-third of these women will undergo mastectomy for treatment.1,2 Autologous reconstruction accounts for nearly one-quarter of breast reconstruction cases, and the abdomen is the most popular donor site; however, abdominal flaps are often contra-indicated secondary to surgical history, unfavorable anatomy, or body habitus.3,4 A popular alternative is the latissimus dorsi flap, which requires loss of muscle and often relies on an implant or fat grafting for additional volume. The pedicled thoracodorsal artery perforator (TDAP) flap represents a muscle-sparing alternative and has been well described; however flaps are often limited by volume and are prone to distal necrosis when the length extends beyond ~25 cm.5–7
The delay phenomenon increases flap reliability by opening choke vessels and encouraging vasculogenesis and angiogenesis.8–10 Our group has shown that delay increases the arterial diameter of the pedicle in superficial inferior epigastric artery flap breast reconstruction.10 We hypothesize that surgical delay will enable harvest of TDAP flaps with enough volume for muscle sparing, totally autologous breast reconstruction without distal fat necrosis or the need for an implant. We present a case of bilateral salvage autologous breast reconstruction after failed implant-based reconstruction, using surgically delayed TDAP flaps.
CASE
A 62-year-old female never-smoker presented to the senior authors’ clinic with a remote history of right-sided estrogen receptor+/progesterone+ breast cancer status postbilateral skin sparing mastectomy without radiation or chemotherapy. She underwent implant-based reconstruction (640 mL left, 685 mL right) 3 years prior but presented with a desire for implant removal and autologous reconstruction of her left breast. A surgical history of a belt lipectomy and her body habitus made this patient a poor candidate for deep inferior epigastric perforator flap or lumbar artery perforator flap reconstruction, and she wished to avoid profunda artery perforator flap scars. Upon examination, she had a body mass index of 36.15, painful left-sided grade IV capsular, right-sided grade II capsular contracture, and skin laxity with excess adiposity of the upper back, making her an excellent candidate for TDAP reconstruction (Fig. 1).
Fig. 1.
Preoperative image of a patient with a history of right-sided breast cancer status postbilateral skin sparing mastectomy with expander to implant reconstruction (640 mL left, 685 mL right) 3 years prior. She presented with grade IV capsular contracture on the left with a lateral contour deformity and grade II capsular contracture on the right. She desired implant removal and autologous reconstruction but had a prior belt lipectomy.
During the initial visit, Doppler and ultrasound were used to locate two left-sided thoracodorsal artery perforators within a 3 cm radius of a point 8 cm below the axilla along the palpable anterior border of latissimus dorsi.
The patient underwent two operations: creation of the left TDAP flap, followed by reconstruction. In the right lateral decubitus position, the perforators were approached from anterior to posterior and isolated circumferentially. Both were initially preserved. The remainder of the flap was raised superficial to the latissimus fascia, starting just lateral to the posterior midline and advancing towards the pedicle origin in the axilla with significant beveling of both the superior and inferior incisions to augment flap volume while taking care to preserve a skin and subcutaneous tissue bridge at the distalmost extent of the flap. The flap and skin paddle were oriented transversely across the back such that scars would be hidden within the bra line while also taking advantage of existing laxity to create a back lift effect. The final flap had a skin paddle that was 32 × 11 cm and a width of 14 cm (Fig. 2). After dissection, the flap was re-secured with deep and subcuticular sutures, and a drain was placed, which remained until reconstruction. This outpatient procedure totaled 83 minutes.
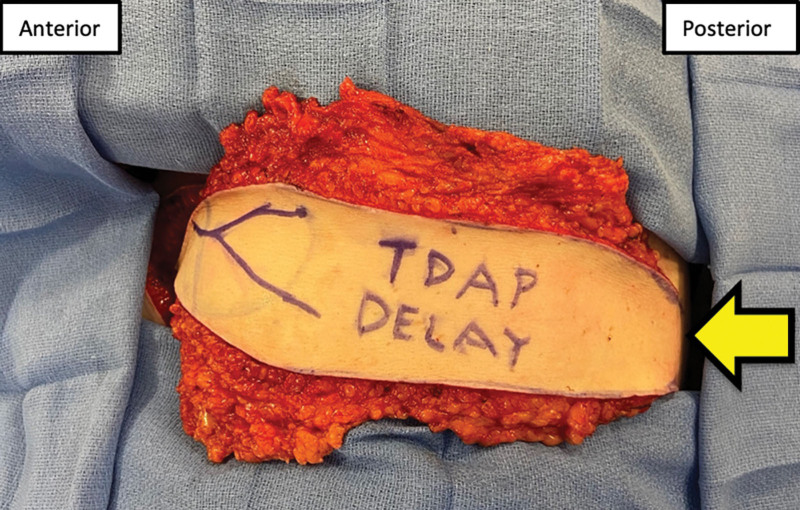
Fig. 2.
Intraoperative photograph of creation of TDAP flap with patient in the right lateral decubitus position. Note the Doppler-able portion of the pedicle marked on the skin paddle and the tissue connection remaining at the posterior midline (yellow arrow). The superior and inferior incisions were made in a beveled fashion away from the flap to recruit additional tissue volume.
Reconstruction occurred 7 days later. Ultrasound (GE Logiq, vascular probe/setting) demonstrated an increase in perforator diameter at the boarder of the latissimus from 1 mm before the delay to 1.6 mm during reconstruction. Peak systolic flow increased from 7.73 cm per second to 24.13 cm per second. In the supine position, the patient underwent prepectoral implant removal and capsulectomy. In the right lateral decubitus position, the flap was re-elevated. The larger perforator coursed anterior to the anterior latissimus boarder and was dissected as far proximally to the thoracodorsal branch as necessary to allow for 180 degrees rotation, whereas the smaller musculocutaneous perforator was ligated. The flap was tunneled through the axilla into the breast pocket (Fig. 3). The patient was positioned supine, and spy fluorescence imaging confirmed perfusion to the flap before de-epithelializing the entire flap for buried inset. The operative time was 219 minutes, and the patient was discharged one day later with drains in the donor site and breast pocket, which remained until output dropped below 30 mL per day for two consecutive days.
Fig. 3.
Delayed TDAP flap during reconstruction before de-epithelialization. The skin and subcutaneous tissue connection at the posterior midline was severed, and the flap was rotated 180 degrees clockwise for tunneling through the axillary tissue inset into the breast pocket in a buried fashion.
On follow-up day 189, the patient expressed satisfaction regarding her reconstruction and scar, which was well hidden by her bra. She desired implant removal and TDAP reconstruction of the right breast. The same procedure was performed (35 × 15 cm flap) with 5 days between flap creation and reconstruction. The right TDAP pre-delay arterial caliber and peak systolic flow were 1.8 mm and 13.0 cm per second, respectively, and postdelay values were 2.3 mm, and 55.0 cm per second. A donor site seroma was drained in clinic. No postoperative complications were noted by postoperative day 342 (left)/148 (right), at which time the patient received bilateral nipple tattoos (Fig. 4).
Fig. 4.
Final muscle-sparing bilateral delayed TDAP flap reconstructive outcome at postoperative day 342 for the left side and at day 148 for the right side. No fat necrosis, flap loss, or dehiscence occurred. The patient underwent nipple tattooing, and expressed overall satisfaction with her reconstructive outcome and donor site scars, which were hidden completely in her bra line.
DISCUSSION
In patients with contra-indications to abdominally-based autologous breast reconstruction, the pedicled TDAP flap is a promising alternative to the traditional latissimus flap ± implants due to its muscle-sparing nature, but it has often been limited in size by distal tip necrosis.5–7 Because surgical delay has been shown to produce reliable outcomes in superficial inferior epigastric artery breast reconstruction,10 the delayed TDAP flap may show promise for greater flap volume and utility. This case serves as a proof of concept that delayed TDAP flap breast reconstruction can provide sufficient volume for total, muscle-sparing, implant-free autologous breast reconstruction, even for relatively large breasts. The TDAP flap is inherently prone to distal tip necrosis; therefore, it is essential to maintain a skin and subcutaneous tissue bridge at posterior midline while the delay phenomenon is taking place.
CONCLUSIONS
This case highlights the feasibility and surgical technique for muscle-sparing delayed TDAP flap breast reconstruction in a salvage case of failed implant-based reconstruction. Prospective studies analyzing clinical outcomes and perforator changes in delayed TDAP flaps are underway to determine the viability of this procedure for widespread use.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
ACKNOWLEDGMENT
IRB approval was obtained for this case report (LSUHSC-NO IRB # 1998).
Footnotes
Published online 16 August 2023.
Presented at the Southeastern Society of Plastic and Reconstructive Surgeons 2022, Orlando, Florida, and will be presented at ASRM 2023 in Miami, Florida.
Disclosure statements are at the end of this article, following the correspondence information.
REFERENCES
- 1.DeSantis CE, Ma J, Gaudet MM, et al. Breast cancer statistics, 2019. CA Cancer J Clin. 2019;69:438–451. [DOI] [PubMed] [Google Scholar]
- 2.Mahmood U, Hanlon AL, Koshy M, et al. Increasing national mastectomy rates for the treatment of early stage breast cancer. Ann Surg Oncol. 2013;20:1436–1443. [DOI] [PubMed] [Google Scholar]
- 3.American Society of Plastic Surgeons. ASPS 2020 plastic surgery statistic report. ASPS Natl Clear Plast Surg Proced Stat. 2021:1–26. [Google Scholar]
- 4.Parrett BM, Caterson SA, Tobias AM, et al. DIEP Flaps in women with abdominal scars: are complication rates affected? Plast Reconstr Surg. 2008;121:1527–1531. [DOI] [PubMed] [Google Scholar]
- 5.Angrigiani C, Grilli D, Siebert J. Latissimus dorsi musculocutaneous flap without muscle. Plast Reconstr Surg. 1995;96:1608–1614. [DOI] [PubMed] [Google Scholar]
- 6.Guerra AB, Metzinger SE, Lund KM, et al. The thoracodorsal artery perforator flap: clinical experience and anatomic study with emphasis on harvest techniques. Plast Reconstr Surg. 2004;114:32–41; discussion 42. [DOI] [PubMed] [Google Scholar]
- 7.Santanelli F, Longo B, Germano S, et al. Total breast reconstruction using the thoracodorsal artery perforator flap without implant. Plast Reconstr Surg. 2014;133:251–254. [DOI] [PubMed] [Google Scholar]
- 8.Callegari PR, Taylor GI, Caddy CM, et al. An anatomic review of the delay phenomenon: I. Experimental studies. Plast Reconstr Surg. 1992;89:397–407; discussion 417–418. [PubMed] [Google Scholar]
- 9.Taylor GI, Corlett RJ, Caddy CM, et al. An anatomic review of the delay phenomenon: II. Clinical applications. Plast Reconstr Surg. 1992;89:408–416; discussion 417–418. [PubMed] [Google Scholar]
- 10.Hoffman RD, Maddox SS, Meade AE, St, et al. Surgical delay-induced hemodynamic alterations of the superficial inferior epigastric artery flap for autologous breast reconstruction. Ann Plast Surg. 2022;88:S414–S421. [DOI] [PubMed] [Google Scholar]