Abstract
Boating has exposed humans to elemental hazards for centuries. What was once a lifelong craft and time-honored skillset is now, with modern technology, a popular recreational activity. Boating safety has inherent limitations and has been historically challenging to enforce. These circumstances have given way to a rising number of watercraft-associated injuries and fatalities. This review aims to investigate the diagnosis, work-up, and management of watercraft-related injuries, including blunt mechanisms, propeller wounds, water-force trauma, associated marine infections, and submersion injuries, as well as outline gaps in current public health policy on watercraft injuries, potential interventions, and available solutions. Motorboats and personal watercraft differ in size, power modality, and differential risk for injury. Accidents aboard watercraft often share commonalities with motor vehicles and motorcycles, namely: rapid deceleration, ejection, and collision with humans. The complexity of care is added by the austere environment in which many watercraft accidents occur, as well as the added morbidity of drowning and hypothermia. Wounds can also become infected by marine organisms, which require wound care and antimicrobial therapy specific to the aquatic environment in which the injury occurred. The treatment of these patients can be further exacerbated by the prolonged transportation times due to complicated water rescue. There are many measures that can prevent or abate watercraft injuries, but inconsistent regulations and enforcement may impair the success of these interventions. Further research is needed to identify possible solutions to common causes of watercraft injuries, such as inconsistent lifejacket use and bow riding.
Keywords: watercraft injuries, boating safety, acute care surgeons, clinical management, prevention interventions
BACKGROUND
More Americans are enjoying hobbies on the water, and the incidence of boat-related injuries continues to rise annually.1 In 2019, the US Coast Guard documented 4,168 recreational boating accidents, which included 2,559 injuries and 613 deaths.2 Florida accounts for 10.1% of all boat-related accidents in the US, the highest proportion of any US state. In 2020, the Florida Fish, Wildlife, and Conservation Commission reported 717 people with watercraft accident-related injuries,3 averaging 2 trauma patients daily. This figure included 534 persons (74.5%) injured by boats and 183 persons (25.5%) involved in personal watercraft (PWC) accidents (eg, Jet Ski and WaveRunner). Texas and California rank 2nd and 3rd in boating accident injury incidence, respectively.2 However, these figures likely underestimate the true incidence of watercraft-related trauma as injuries are only reported when a vessel is involved in an accident that requires assistance from a marine patrol entity.
Given the recent increase in incidence and unique injury presentations, awareness of watercraft-related injury patterns and management should be a priority for acute care surgeons. However, there is a paucity of literature investigating watercraft-related injuries and watersport trauma with evidence-based recommendations. The objective of this review is to (1) investigate current evidence on the evaluation and management of watercraft-related injuries, including blunt mechanisms, propeller wounds, water-force trauma, associated marine infections, and submersion injuries; (2) provide clinical recommendations for adult and pediatric patient populations involved in accidents with boats and PWCs; and (3) outline gaps in current public health policy on watercraft injuries, potential interventions, and available solutions.
METHODS
Data Sources and Search Strategy
Articles that investigated watercraft-related injuries, including blunt mechanisms, propeller wounds, water-force trauma, marine infections, and submersion injuries were compiled through multiple queries of the PubMed and Medline databases. The literature was consulted through Boolean searches created to locate the foundation of available clinical articles for consideration for narrative review. The following search terms were used: [1] ((boating injuries) AND (trauma) AND (propellers) AND (English)) NOT (animals); [2] (Necrotizing fasciitis) OR (Vibrio OR marine bacteria) AND (marine infection); [3] (Drowning) AND (critical care) NOT (public health OR epidemiology); [4] ((personal floatation devices) AND (trauma) AND (boating) AND (English)) NOT (paddle sports) NOT (falls); [5] (waverunner) OR (jet ski) OR (personal watercraft) AND (injury); [6] (watercraft injury) AND (public health) AND (safety); and [7] (pressure jet) AND (injury) AND (water force). The last search was conducted on February 3, 2022.
Study Selection and Eligibility Criteria
Inclusion criteria were articles that investigated the management and/or prevention of watercraft-related injuries, including blunt mechanisms, propeller wounds, water-force trauma, marine infections, and submersion injuries. Case reports, case series, prospective cohort, retrospective cohort, randomized control trials, and reviews were included. We excluded studies that investigated simple falls, paddle sports, and propeller injuries to marine animals. Articles were also excluded if they were not peer-reviewed or not in English. Due to limited scholarly material in certain subcategories, the earliest relevant literature was published in 1949, through articles published up to February 3, 2022, were included. Articles in the discipline of autopsy pathology or forensic sciences, while informative, were not emphasized.
Data Screening and Collection Process
Five reviewers (J.E., K.N., S.D., M.M., and A.E.) independently conducted the initial literature search and then collaboratively screened study titles and abstracts for inclusion and exclusion criteria. Final review, data verification, and any discrepancies were resolved by all authors (J.E., K.N., S.D., M.M., and A.E.).
OVERVIEW OF MECHANISMS AND PREHOSPITAL CONSIDERATIONS
Overall, 24 studies met the inclusion criteria and were included in this review (Fig. 1). Most injuries involving watercraft result from (1) persons ejected from vessels, or (2) persons in the water struck by vessels, according to 2019 recreational boating statistics.4 Patients brought to medical attention through trauma system activation should be evaluated with the same principles as a high-velocity motor vehicle, motorcycle, and pedestrian accident seen on land.5 Additionally, patients presenting with watercraft-related trauma commonly have environmental exposures, such as hypothermia or fluid aspiration.6
FIGURE 1.
Illustrates common structural components of motorized watercraft.
Like trauma on land, most injuries are caused by blunt mechanisms.7 Nonetheless, there are situations that involve penetrating, mixed injuries, or unique “chopping” propeller injuries.8 Further, a person struck by the keel of a vessel, constituting blunt trauma, may then sustain a propeller injury; this pattern exemplifies a mixed mechanism.9
Mechanism of Injury, Physiology, and Initial Considerations
These accidents can cause virtually any pattern of injury. The literature is replete with case reports that have documented boat-related injuries to every anatomic region and physiologic system. Studies have documented all of the following: complex wounds,10,11 mangled extremities,12,13 burns from boat/yacht fires,14,15 open and closed fractures,16–18 open and closed skull/traumatic brain injuries,19,20 spinal cord injuries,16,21 major vascular injuries (ruptures and transections),8,22 sucking chest wounds,23 abdominal solid organ and visceral injuries,5,24 pressure-related gynecologic and anorectal injuries,25–27 facial nerve and salivary gland injuries,28,29 and more (Table 1, http://links.lww.com/AOSO/A108).
Management
There is no stereotypical pattern that can be assigned to a patient ejected from a recreational boat versus a PWC. For these reasons, patients require a thorough trauma evaluation aligned with the American College of Surgeons Advanced Trauma Life Support (ATLS) or similar protocols.30
In many areas, first responder transport for watercraft-related trauma can be prolonged. This is largely due to multifactorial issues with telephone and radio communication, likelihood that a vessel may be disabled, impaired rescue access in severe weather conditions, limited first aid medical supplies, and other unforeseen circumstances. For these reasons, maritime injuries can be regarded as rural trauma in nearly any geographic setting.
KEEL, SKEG, AND PROPELLER INJURIES
All motorized vessels share common structural components that are important to understand (Fig. 1). The anterior-most aspect of the vessel is known as the bow. The median segment below the waterline, known as the keel, represents the first part of a watercraft that could collide with a swimmer or overboard passenger. The underwater hull can pull swimmers beneath a vessel after a collision even if not hit directly by the keel. Propeller blades are often exposed, posing a great risk to overboard passengers and swimmers and are typically preceded by a perpendicular metal plate, known as the skeg.
Diagnosis
Persons struck by watercraft at speed can experience similar injuries to pedestrians struck by cars. Traumatic brain injuries, rib fractures, and orthopedic injuries are associated with these blunt mechanisms. Lacerations can occur, but these skin and soft tissue injuries require differentiation from those caused by propellers.
Propellers can be devastating, causing anything from large soft tissue injuries to nonsurvivable head, trunk, and limb injuries.31 Many observational studies have noted that watersports (eg skiing and wakeboarding) pose the highest risk of propeller injury, primarily because of repeated close interaction with the running motorboat when being picked up or resetting for another tow.7 The blunt impact of a vessel’s keel may cause a large laceration, but in contrast, propeller lacerations tend to be numerous and evenly spaced across an area.8,18
Field Work-Up
For patients with external hemorrhage, it may be difficult for first responders to quantify blood loss in an aquatic setting. Worse yet, coagulation cascades do not activate in the same manner when wounds are submerged,32 leading to uncontrollable hemorrhage in some cases.
Management
Water rescue, manual pressure, and tourniquet devices (for limb hemorrhage, may be created with available nautical rope) can temporize blood loss. Even after hemostasis is achieved, the soaking wet patient remains at high risk for hypothermia and coagulopathic derangement. Potential solutions to decrease the incidence of harmful and debilitating propeller injuries are offered in Table 1.
TABLE 1.
Common Public Health and Clinical Management Issues Involving Watercraft-Related Injury and Proposed Solutions
| Problem | Proposed Solutions |
|---|---|
| Public Health | |
| Propeller injuries are dangerous and disabling | • Install propeller guards on outboard motors |
| • Implement educational programs for boaters on how to approach swimmers while minimizing the chance of contact with propeller blades | |
| Inconsistent lifejacket uses among recreational boaters | • Educational programs for parents and other role-models to increase usage among youth |
| • Advertisement campaigns normalizing lifejacket use to decrease perceived social stigma | |
| • Increase minimum age requirements for lifejacket use | |
| Physical engine cutoff switches (ECOS) are easily circumvented | • Convert to wireless kill switches that automatically connect and are difficult to disable |
| • Increase surveillance, enforcement, and cost of noncompliance | |
| Bow riding is common and dangerous | • Improved consistency in legislature across states |
| • Increased public outreach and education about the dangers of bow riding | |
| • Use of cameras or sensor technology to improve visibility and warn boat drivers of an impending collision when vision is obstructed by bow riders | |
| Inexperienced boaters commonly decrease throttle when attempting to evade an impending crash, but their ability to maneuver is inhibited by the lack of thrust | • Required educational class before buying or renting a boat that details how to maneuver watercraft in emergency situations |
| • Use of visual graphics on watercraft warning labels to attract attention and increase understanding of proper boating technique | |
| Excessive speeding and reckless boating | • Increased surveillance and consequences for boating under the influence |
| • Improve awareness of reporting systems and encourage bystanders to report instances of unsafe boating | |
| Clinical Management | |
| Gynecologic and colorectal water-force injuries can be life threatening and can be missed during patient evaluation | • Have high index of suspicion for orifice water-force injuries for patients with risk factors (peritoneal area impact with water, falls off rear of PWC, and waterskiing injuries at high velocity) and presenting with clinical signs and symptoms (bleeding from rectum or vagina, abdominal pain, and urge to defecate) |
| • Incorporate orifice examinations with informed consent into trauma algorithms for patients with these risk factors and clinical signs | |
| Soft tissue injuries can become infected when exposed to aquatic microorganisms | • Emphasize early irrigation with sterile saline and debridement during management |
| • Cultures and biopsies should be collected from infected soft tissue injuries | |
| • Early communication with laboratory to ensure necessary media and stains are readily available | |
| • Antimicrobial prophylaxis should be specific to the water type exposed to the wound | |
ECOS, engine cutoff switches; PWC, personal watercraft.
WATER FORCE AND PRESSURE JET-RELATED INJURIES
The mechanism of water-force injuries, such as in high-speed water skiing, is related to impact at the water surface.33 At speed, falls overboard or falls during watersports can injure vulnerable anatomical regions, such as the cervical spine and perineum. More specifically, colorectal and anal injuries can result from forceful trans-anal water entry. This can also occur when a PWC passenger falls off the back of the accelerating PWC, exposing the perineum to the high-pressure jet propulsion system, thereby forcing water into orifices.34 Pressurized water impact can cause tissue injury and hemorrhage as proximal as the sigmoid colon, as was reported in a case study of a 26-year-old man.35
Diagnosis
Watersport accidents, particularly in a sitting or crouched position, can produce a similar “waterskier’s enema.”36 This phenomenon presents as diffuse, cramping abdominal pain and urges to defecate. Similarly, female victims of high-speed falls can suffer a spectrum of gynecologic injuries from forceful water injection, including vaginal lacerations; some severe cases can cause hydrosalpinx and peritonitis.27 Presentations with pelvic or rectal pain merit informed patient consent for formal pelvic or rectal examinations.27 In some cases, these maneuvers may be impractical in the emergency department for some patients with severe pain. For these cases, examination under anesthesia can provide improved visualization of any potential injuries.
Work-Up
Diagnostic imaging is also imperative in the trauma setting. In stable patients, computed tomography (CT) of the abdomen and pelvis with intra-venous contrast may be used to detect gynecologic injury whereas CT with rectal contrast and rigid proctoscopy can detect colorectal injury.36 Perirectal fat stranding is characteristic of injury, and free pelvic fluid can be identified in some cases where the site of injury is above the peritoneal reflection. Like in other trauma, delayed phase CT imaging is helpful to fully evaluate for hemorrhage; however, laparoscopy is preferred over CT in unstable trauma patients.37
Management
Pelvic injuries related to water-force injuries or watersport accidents may need surgical intervention if trauma to the area is severe and interferes with normal urinary or bowel function. Fecal diversion, which can be either temporary or permanent, can include an ileostomy or colostomy.38 This procedure could be performed in response to destruction or infection of the rectal vault and/or the colon. Urinary diversion may be necessary if the bladder is significantly injured or damaged beyond repair.39 However, immediate operative repair is often sufficient to avoid diversion if the lower genitourinary tract and bladder can be repaired.40 Additionally, recommendations are offered to improve the detection and management of water force injuries in Table 1.
COMPLEX WOUND MANAGEMENT AND MARINE INFECTIONS
Diagnosis
Many patients brought to medical attention after a watercraft accident will have soft tissue wounds.41 In sizeable clinical analyses, the largest proportion of isolates are gram-negative organisms.14 Vibrio species have been isolated from contaminated wounds exposed to an estuary and warm coastal waters.42 Pathogenic bacterial species vary based on the ecosystem; therefore, antimicrobial therapy should be tailored to the particular environmental exposure (Table 2).
TABLE 2.
Antimicrobial Therapy for Wounds Exposed to Aquatic Environments
| Prophylaxis 12 | First-generation cephalosporin* (eg, cefazolin 1g IV every 8 hours) or clindamycin† 600 mg IV every 8 hours |
| Basic coverage | Plus fluoroquinolone (eg, levofloxacin 750 mg IV daily) |
| Estuary/ocean exposure | Add tetracycline (eg., doxycycline 100 mg IV every 12 hours)‡ |
| Contaminated water | Add metronidazole§ 500 mg IV every 6 hours |
| Targeted Therapy12 Vibrio vulnificus Mycobacterium marinum | 3rd generation cephalosporin (eg, ceftriaxone) plus tetracycline (doxycycline, minocycline, tigecycline) or fluoroquinolone (eg, levofloxacin) Follow in-vitro susceptibility testing; many strains are susceptible to rifampin, ethambutol, clarithromycin, and sulfa-containing antibiotics; generally resistant to isoniazid and pyrazinamide; long antibiotic course (mean 14 weeks) |
*Can consider 3rd generation cephalosporin (eg, ceftriaxone 1 g every 12 hours) for coverage of gram-negative marine organisms as standard prophylaxis in trauma bay or operating room setting.
†For patients allergic to penicillin or cephalosporins.
‡Standard prophylaxis for Vibrio and other gram-negative aquatic/marine species; administration route dependent on clinical picture: IV for severe wounds, hospitalized patients; PO therapy appropriate for patients to be discharged, or in situations where Vibrio prophylaxis is needed but patient cannot receive ceftriaxone due to allergies or outpatient setting.
§Not needed if patient is already covered with clindamycin.
IV, intra-venous.
Work-Up
Soft tissue wounds are commonly encountered injuries from watercraft accidents and can be large and require operative care.41 These wounds are also very high risk for contamination given the exposure to freshwater, saltwater, or brackish waters.43 These wounds should be irrigated liberally with saline solutions.44 For larger, deeper wounds, washout is preferably performed in the operating room. Before extensive irrigation or debridement, intraoperative cultures and biopsies should be collected for grossly contaminated or infected soft tissue injuries.45 Communication with laboratory services is important because unconventional stains and incubation methods may be required to identify and isolate aquatic microorganisms.14
Management
Management strategies usually involve serial washouts, debridement, and delayed primary closure.45,46 Planned return trips to the operating room for staged interventions allow surgeons to visualize wound healing and mitigate the risk of delaying care for necrotizing soft tissue infections.
Negative pressure wound therapy (NPWT) systems (eg, wound vacuum-assisted closure) can promote the healing of tissue beds.47 Early in wound care, serial irrigation and debridement procedures with wound sponge changes can be performed every 24–28 hours. Clinical wound appearance and culture results guide surgeons towards a closure strategy, either primary closure, delayed primary closure, or secondary closure. NPWT with instillation (eg, Vera-Flo) can augment granulation tissue formation and promote flushing of contaminated tissue beds.48
Standard prophylaxis includes first-generation cephalosporin (clindamycin for allergic patients) plus a fluoroquinolone. Tetracyclines are helpful in situations with a high clinical index of suspicion for Vibrio infection. Wounds believed to be contaminated by sewage (urban runoff or farm-associated) can be covered for parasitic organisms with metronidazole. In trauma from coastal settings, it is practical to administer ceftriaxone as initial wound prophylaxis over a first-generation cephalosporin, given its Vibrio coverage49. Additionally, all patients who sustain propeller trauma should be given a tetanus toxoid booster, as many boat propellers and skegs are corroded to some degree. We summarize several management considerations that should be followed to prevent and treat soft tissue wound infections in Table 1.
Necrotizing fasciitis is the most severe consequence of wound infections occurring on the water or in coastal settings.50 One South Korean study recognized marine organisms as the largest cause of necrotizing fasciitis in coastal areas.51 Their 217 consecutive cases included 105 cases caused by Vibrio. Most infections were monomicrobial, in contrast to the typical polymicrobial growth seen in nonmarine settings. It is worth noting a strong correlation exists between chronic liver disease and fulminant Vibrio infection, comorbidity attributable to 75% of cases in the South Korean analysis.51 Mortality rates were staggering: 34.6% within 48 hours, and 45.6% within 30 days. Serial debridement operations were the mainstay surgical therapy, with an average of 4 procedures per patient.51
SUBMERSION INJURIES AND HYPOTHERMIA
Maritime-related trauma can be complicated by drowning and related conditions.52 The 2002 World Health Organization definition of drowning describes it as “The process of experiencing respiratory impairment from submersion or immersion in liquid.”53 The term is then subdivided into nonfatal and fatal drowning based on clinical outcomes. Confusion between the terms drowning, near drowning, submersion, immersion, suffocation, asphyxiation, water injuries, and aspiration were addressed in a 2005 systematic review by Papa et al.54
Drowning begins when the injured or fatigued patient can no longer protect their airway. Rising hypercarbia eventually stimulates the involuntary respiratory drive to gasp for air.55 Fluid entering the lower airway triggers the coughing reflex, and the process of aspiration and drowning enters a positive feedback cycle without rescue.56 In many patients, subsequent hypoxia leads to apnea. Cardiac consequences follow, from tachycardia, progression to bradycardia, ventricular arrhythmia, pulseless electrical activity, and asystole.56
Drowning events can have devastating outcomes, including central nervous system (CNS), respiratory, or cardiovascular (CV) demise. Cardiovascular demise can be initiated by the dive reflex, which is triggered by the stimulus of cold water making a forceful impact on the face.51 Breath-holding, peripheral vasoconstriction, and bradycardia can all contribute to decreased cardiac output and unstable hemodynamics.57 Decreased cerebral blood flow also affects brain tissue oxygenation, resulting in further CNS injury and cerebral watershed infarctions can result.57 Hospital care is often only supportive. For these reasons, high-quality field resuscitation with bystanders and first responders provides the highest chance of meaningful outcome for patients who are unstable or arrested from drowning and can minimize hypoxemia and hypotension, which can cause secondary damage to the brain.57
The extent of submersion injury guides resuscitation and management. Mass aspiration dilutes and washes away surfactant, disrupting the surface tension dynamics, which maintain alveolar shape and physiology.55 Osmotic gradient derangements then break down the blood-air barrier at the squamous alveolar lining. Pulmonary edema and clinical progression into acute respiratory distress syndrome (ARDS) can follow.55
Diagnosis
Hypothermia is a fall in core body temperature below 35°C.58 There are 2 types, the first being primary hypothermia, which occurs during states of depleted energy stores in healthy individuals.58 Inadequate heat production is usually secondary to environmental stressors, such as exposure to extreme cold. In contrast, secondary hypothermia is low body temperature resulting from a medical illness, trauma, or drug. In both types of hypothermia, level of consciousness, breathing, and circulation are affected, dramatically increasing morbidity and risk for adverse sequelae.58
Submersion following a watercraft-related injury can quickly incapacitate and kill victims. Even if rescued quickly, individuals can become hypothermic during transportation to shore.6 It is, therefore, critical that rescuers quickly remove the soaked garment from submerged victims, monitor core temperature, and apply heating devices in the prehospital setting.
Work-Up
Evaluation on arrival in the resuscitation bay should emphasize airway, breathing, circulation, disability, and exposure. For drowning patients, this means endotracheal intubation, mechanical ventilation guided by early arterial blood gases, advanced cardiac life support for hypoxic arrests when needed, neurologic evaluation with Glasgow Coma Score and pupillary examinations, and intentional strategies for whole-body warming to correct hypothermia.
Patients in respiratory distress or those coughing up water can be intubated on arrival; even in cases where neurologic status is relatively preserved.56 Endotracheal intubation serves multiple purposes by not only securing the airway but also allowing for protective mechanical ventilation strategies in patients at high risk of progressing to ARDS. It is beneficial to have arterial blood gas values shortly after the patient arrives for improved ventilator management by adjusting oxygenation settings with positive end-expiratory pressure and FiO2 to prevent subsequent cardiac dysfunction and neurologic injury.
Management
Hypothermia is often treated using rewarming techniques, classified based on the presence or absence of cardiac support. Noncardiac support techniques include: (1) external warmth; (2) minimally invasive rewarming, including heating blankets and warm parenteral fluids; (3) peritoneal dialysis; (4) hemodialysis; (5) intubation with heated ventilation; (6) esophageal warming devices (7) heated thoracic, gastric, or colonic lavage; and (8) venovenous extra-corporeal membrane oxygenation (ECMO). Rewarming with cardiac support techniques include (1) Venoarterial ECMO, and (2) cardiopulmonary bypass.58
Early bronchoscopy may be important in patients with submersion injury to visualize and clear the airway of foreign bodies, such as sand, algae, or seagrass debris that are not readily visualized on initial presentation.59 Bronchoscopy should be combined with bronchoalveolar lavage fluid (BALF) analysis to enhance and confirm findings. Pediatric literature has reported cases of sand aspiration where bronchoscopic BALF provided diagnostic and therapeutic value, whereas nonbronchoscopy-directed BALF analysis was nondiagnostic.60 Bronchial washing is often performed in conjunction with bronchoscopy; the irrigation fluid clears adherent bronchial debris and benefits patients.60
Hemodynamics-focused neurologic examination and arterial pH are critical for determining the extent of drowning injury and guiding the next steps in management.61 While there are no definitive clinical protocols for emergency department management of submersion injury patients, clinical classification systems have been developed for determining prognosis with 93% accuracy.62 However, the lack of standardized clinical protocols of submersion injuries calls for greater adherence to principles of ATLS for stabilization, followed by additional assessments to guide management strategies, such as rewarming and fluid administration.61
Patients with extensive injuries or submersion injuries requiring airway watch or intubation may require ICU-level care involving management for pulmonary injury, CV instability, and neurologic damage.61 Overall, the main goal of ICU management should be supportive care, adequate oxygenation, minimizing organ damage, and maximizing CV support.61
PUBLIC HEALTH AND PREVENTIONPersonal floatation devices (PFDs) (ie, lifejackets), engine cutoff switches, and banning of dangerous activities, such as bow-riding are public health measures that are currently being used for the prevention of traumatic watercraft injury. One of the simplest and most effective strategies is through consistent and proper use of PFDs. PFDs have not only been shown to decrease deaths by drowning,63 but also prevent drowning sequelae in patients with other injuries. Depending on PFD design, lifejacket use may also preserve body heat and mental acuity by raising the head and chest above the water surface.64 Additionally, almost all PFDs are brightly-colored with features, such as reflective tape and an attached whistle that improve the chances of locating and rescuing an injured person.
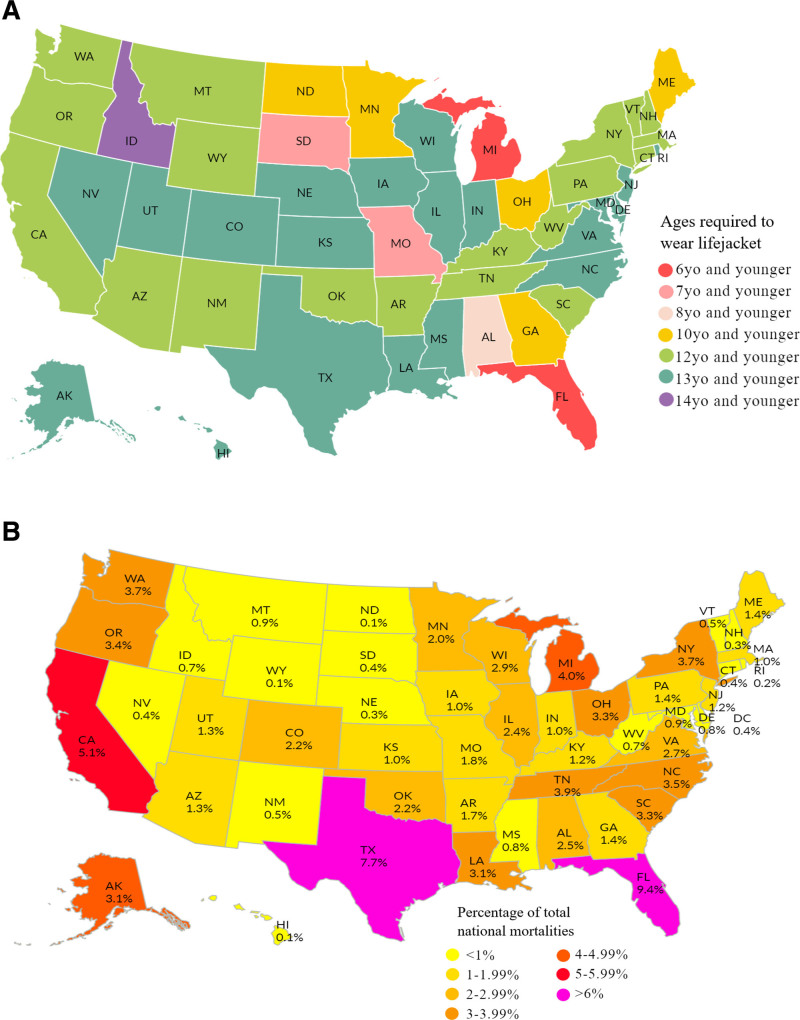
To meet US Coast Guard (USCG) requirements, watercraft are required to have a USCG-approved lifejacket for each person on board; however, actual use requirements vary by state.65 Currently, most states require passengers 12 or 13 years or younger to wear lifejackets when vessels are underway, though 10 states have lower age requirements (Fig. 2A). Interestingly, the two states with the lowest age requirement, only requiring those 6 years and younger to wear lifejackets while underway, are Florida and Michigan, which have the 1st and 4th highest proportion of watercraft-related deaths, respectively (Fig. 2B).
FIGURE 2.
(A) Age requirements for lifejackets use by state. (B) Distribution of 2020 watercraft-related mortalities by state.
Considering the dearth of legislation mandating PFD use, it is unsurprising that the majority of swimmers and boaters do not regularly wear PFDs during recreational water activities.66,67 A systematic review found that PFD use was associated with children, females, those on nonmotorized boats, those on small boats, and those in social circles where others wore PFDs.68 Another public health study also found that one of the most commonly cited reasons for not wearing a PFD among boaters was the belief that life jacket use would indicate inexperience or poor swimming ability.67 These findings demonstrate that one’s social environment is likely a key factor in PFD use. Several solutions are offered to improve lifejacket use among boaters in Table 1.
Another important safety feature is the use of engine cutoff switches (ECOSs) on boats and personal watercraft. ECOSs are physical or wireless connections that attach to the person operating a watercraft that automatically shut off the motor if the connection is interrupted. ECOSs prevent the situation where an operator falls or is launched off the watercraft, resulting in a runaway boat that can be dangerous for the ejected operator, other boaters, people in the water, or first responders. To increase the public usage of ECOS, the Elijah E. Cummings Coast Guard Authorization Act of 2020 was passed which requires all vessels less than 26 feet in length built beginning in January 2020 to install, maintain, and use an ECOS.69 The enforcement of this mandate is complicated by the ease at which physical ECOS can be circumvented and the lack of obvious visual indications to law enforcement that an ECOS is being used correctly. We offer several solutions to improve ECOS use in Table 1.
“Bow-riding,” or sitting on the side gunnels or the stern of a vessel, is a dangerous yet popular boating activity. Often, bow-riding means the passenger’s legs will be dangling from the edge of the boat, potentially putting the rider in the path of the propeller if they were to fall. Bow-riding can affect the stability of a boat and obstruct the boat operator’s visibility, making it dangerous for both the passengers and any obstacle in the path of the watercraft. Due to the dangers of this activity, many recreational boating areas prohibit bow-riding or overloading. However, there are inconsistent regulations and enforcement of this dangerous activity. Several recommendations for preventing injuries from bow-riding are available in Table 1.
Certain states, especially large coastal states, such as FL, TX, and CA, contribute the largest proportion of watercraft-related deaths across the nation (Fig.2B). Legislation and regulation of watercraft are primarily at the state level; therefore, interventions should be targeted at the states with the highest proportion of watercraft-related deaths. Additionally, surgeons who practice at trauma centers near recreational water areas, especially in the states of FL, TX, and CA, should also be particularly trained on the unique evaluation and management considerations for watercraft trauma.
FUTURE RECOMMENDATIONS
Literature is currently limited to case studies on various watercraft-related injuries, such as propeller lacerations and marine infections. Future studies on larger cohorts should be conducted to determine the risk factors and outcomes associated with these injuries. Although several observational studies have investigated the prevalence of PFDs among recreational boaters, there is a paucity of literature evaluating the impact of educational programs and other governmental interventions on PFD use. Similarly, no studies have examined the impact of the 2020 national ECOS mandate on related injuries. Future studies should investigate these relationships to evaluate the effectiveness of interventions and provide lawmakers with information on how to prevent watercraft-related injuries. Additionally, cost-benefit analysis of public health programs related to boating safety may reveal additional benefits for implementing these interventions, as watercraft accidents are very costly.
LIMITATIONS
To the best of our knowledge, this review presents the most up-to-date information regarding the considerations and management of watercraft-related injuries; however, our review was not without limitations. The search criteria were intentionally broad, as was the timeframe of included articles, due to the scarcity of research on watercraft injuries. This led us to capture a wide range of studies, improving the generalizability of our findings; however, some of the subtleties of specific patient populations and injuries may have been lost. Additionally, the lack of studies other than case reports and small series limited the quality of evidence included in this review. Additionally, much of the literature on submersion injuries comes from studies with pediatric populations, as children are statistically more prone to drowning.
CONCLUSIONS
This review investigated clinical evidence on the complexities and management considerations for watercraft-related injuries. Accidents involving watercraft share commonalities with motor vehicles and require the same systematic evaluation as other trauma; however, these injuries can become complicated by drowning and hypothermia. Wounds can also become infected by marine organisms, which require specific wound care and antimicrobial therapy. The treatment of these patients can be further exacerbated by the prolonged transportation times due to complicated water rescue. There are many measures that can prevent or abate watercraft injuries, but inconsistent regulations and enforcement may impair the success of these interventions. Further research is needed to identify possible solutions to common causes of watercraft injuries, such as inconsistent lifejacket use and bow-riding.
Footnotes
Published online 14 March 2022
Disclosure: The authors declare that they have nothing to disclose.
Study design and conception: A.E. and J.E. Data collection, analysis, and interpretation: J.E., K.N., S.D. and A.E. Manuscript preparation and drafting: J.E., A.E., K.N., S.D. and M.M. Critical revisions of the manuscript: A.E., J.E., K.N., S.D. and M.M. All authors read and approved the final manuscript.
REFERENCES
- 1.Accident Statistics. United States Coast Guard. Available at: https://www.uscgboating.org/statistics/accident_statistics.php. Published July 2021. Accessed July 31, 2021.
- 2.Recreational Boating Statistics. U.S. 2019 Department of Homeland Security U.S. Coast Guard. Available at: https://www.uscgboating.org/library/accident-statistics/Recreational-Boating-Statistics-2019.pdf. Published June 4, 2020. Accessed August 2, 2021.
- 3.Boating Accident Statistical Reports. Florida Fish and Wildlife Conservation Commission. Available at: https://myfwc.com/boating/safety-education/accidents/. Published March 1, 2020. Accessed August 2, 2021.
- 4.U.S. Coast Guard. 2020 Recreational Boating Statistics. 2020. Available at: https://www.uscgboating.org/library/accident-statistics/Recreational-Boating-Statistics-2019.pdf. Accessed January 8, 2022
- 5.Xhemali B, Vyshka G, Sinamati A, et al. Pattern of lethal trauma among swimmers colliding with a personal watercraft. Int Marit Health. 2017;68:187–189. [DOI] [PubMed] [Google Scholar]
- 6.Giesbrecht GG, Hayward JS. Problems and complications with cold-water rescue. Wilderness Environ Med. 2006;17:26–30. [DOI] [PubMed] [Google Scholar]
- 7.Keijzer R, Smith GF, Georgeson KE, et al. Watercraft and watersport injuries in children: trauma mechanisms and proposed prevention strategies. J Pediatr Surg. 2013;48:1757–1761. [DOI] [PubMed] [Google Scholar]
- 8.Ihama Y, Ninomiya K, Noguchi M, et al. Fatal propeller injuries: three autopsy case reports. J Forensic Leg Med. 2009;16:420–423. [DOI] [PubMed] [Google Scholar]
- 9.Kononov NV, Fetisov VA, Nazarov YV. [Problematic issues of the forensic medical examination of a fatal injury induced by modern small-scale water transport]. Sud Med Ekspert. 2020;63:47–51. [DOI] [PubMed] [Google Scholar]
- 10.Hargarten SW, Karlson T, Vernick JS, et al. Motorboat propeller injuries in Wisconsin: enumeration and prevention. J Trauma. 1994;37:187–190. [DOI] [PubMed] [Google Scholar]
- 11.Brehm TT, Berneking L, Rohde H, et al. Wound infection with Vibrio harveyi following a traumatic leg amputation after a motorboat propeller injury in Mallorca, Spain: a case report and review of literature. BMC Infect Dis. 2020;20:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Noonburg GE. Management of extremity trauma and related infections occurring in the aquatic environment. J Am Acad Orthop Surg. 2005;13:243–253. [DOI] [PubMed] [Google Scholar]
- 13.Di Nunno N, Di Nunno C. Motorboat propeller injuries. J Forensic Sci. 2000;45:917–919.. [PubMed] [Google Scholar]
- 14.Shergill G, Scerri GV, Regan PJ, et al. Burn injuries in boating accidents. Burns. 1993;19:229–231. [DOI] [PubMed] [Google Scholar]
- 15.Ben DF, Ma B, Chen XL, et al. Burn injuries caused by ship fire: a 12-year study in Shanghai. Burns. 2010;36:576–580. [DOI] [PubMed] [Google Scholar]
- 16.Maempel JF, Maempel FZ. The speedboat vertebral fracture: a hazard of holiday watersports. Scott Med J. 2019;64:42–48. [DOI] [PubMed] [Google Scholar]
- 17.Mann RJ. Propeller injuries. South Med J. 1976;69:567–569. [DOI] [PubMed] [Google Scholar]
- 18.Mendez-Fernandez MA. Motorboat propeller injuries. Ann Plast Surg. 1998;41:113–118. [DOI] [PubMed] [Google Scholar]
- 19.Jackson FE. High speed propeller injuries of the brain; report of two cases. Am J Surg. 1965;110:473–476. [DOI] [PubMed] [Google Scholar]
- 20.Dhall SS, Lin FJ, Tumialan LM, et al. Significant neurologic recovery following a catastrophic open head injury from a motorboat propeller: case illustration. J Trauma. 2008;65:249–250. [DOI] [PubMed] [Google Scholar]
- 21.Wild G. Vertebral wedge fracture after speedboat ‘splash down’. J R Nav Med Serv. 2007;93:75–77. [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention (CDC). Boat-propeller-related injuries--Texas, 1997. MMWR Morb Mortal Wkly Rep. 1998;47:354–356.. [PubMed] [Google Scholar]
- 23.Sladden D, Casha AR, Manche A. Chest wall reconstruction following a speedboat propeller injury. Malta Med J. 2014;26:48–51.. [Google Scholar]
- 24.Semeraro D, Passalacqua NV, Symes S, et al. Patterns of trauma induced by motorboat and ferry propellers as illustrated by three known cases from Rhode Island. J Forensic Sci. 2012;57:1625–1629. [DOI] [PubMed] [Google Scholar]
- 25.Katano K, Furutani Y, Hiranuma C, et al. Anorectal injury related to a personal watercraft: a case report and literature review. Surg Case Rep. 2020;6:226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Di Flumeri G, Carcaboulias C, Dall’Olio C, et al. Anorectal and perineal injury due to a personal watercraft accident: case report and review of the literature. Chir Ital. 2009;61:131–134. [PubMed] [Google Scholar]
- 27.Gauthier I, Clancy AA, Lipson J, et al. Water-related vaginal injury: a case report and review of the literature. J Obstet Gynaecol Can. 2018;40:926–930. [DOI] [PubMed] [Google Scholar]
- 28.Gallagher JP. Propeller injury of the face and head. Bull Georgetown Univ Med Cent. 1949;2:215. [PubMed] [Google Scholar]
- 29.Kambeyanda R, Singh R, Armstrong M. Propeller damage to the parotid duct. Am Surg. 2017;83:e308–e310. [PubMed] [Google Scholar]
- 30.Advanced Trauma Life Support. American College of Surgeons. Available at: https://www.facs.org/quality-programs/trauma/atls. Accessed August 5, 2021.
- 31.Hummel G, Gainor BJ. Waterskiing-related injuries. Am J Sports Med. 1982;10:215–218. [DOI] [PubMed] [Google Scholar]
- 32.Ports TA, Deuel TF. Intravascular coagulation in fresh-water submersion: report of three cases. Ann Intern Med. 1977;87:60–61. [DOI] [PubMed] [Google Scholar]
- 33.Baker JI, Griffin R, Brauneis PF, et al. A comparison of wakeboard-, water skiing-, and tubing-related injuries in the United States, 2000-2007. J Sports Sci Med. 2010;9:92–97.. [PMC free article] [PubMed] [Google Scholar]
- 34.Freeman MD, Everson TM, Kohles SS. Forensic epidemiologic and biomechanical analysis of a pelvic cavity blowout injury associated with ejection from a personal watercraft (jet-ski). J Forensic Sci. 2013;58:237–244. [DOI] [PubMed] [Google Scholar]
- 35.Mavrelis PG, Wylie RR. Water-ski colon. N Engl J Med. 1984;311:1128. [DOI] [PubMed] [Google Scholar]
- 36.Trust MD, Veith J, Brown CVR, et al. ; AAST Contemporary Management of Rectal Injuries Study Group. Traumatic rectal injuries: Is the combination of computed tomography and rigid proctoscopy sufficient? J Trauma Acute Care Surg. 2018;85:1033–1037. [DOI] [PubMed] [Google Scholar]
- 37.Morey AF, Brandes S, Dugi DD, III, et al. ; American Urological Assocation. Urotrauma: AUA guideline. J Urol. 2014;192:327–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lightner AL, Pemberton JH. The role of temporary fecal diversion. Clin Colon Rectal Surg. 2017;30:178–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sperling CD, Lee DJ, Aggarwal S. Urinary diversion: core curriculum 2021. Am J Kidney Dis. 2021;78:293–304. [DOI] [PubMed] [Google Scholar]
- 40.Goldman HB, Idom CB, Jr, Dmochowski RR. Traumatic injuries of the female external genitalia and their association with urological injuries. J Urol. 1998;159:956–959. [PubMed] [Google Scholar]
- 41.White MW, Cheatham ML. The underestimated impact of personal watercraft injuries. Am Surg. 1999;65:865–869.. [PubMed] [Google Scholar]
- 42.Kaiser RE, Jr, Armenia D, Baron R, et al. Waterskier’s enema. N Engl J Med. 1980;302:1264. [DOI] [PubMed] [Google Scholar]
- 43.Foote A, Henderson R, Lindberg A, et al. The australian mid-west coastal marine wound infections study. Aust Fam Physician. 2017;46:923–927. [PubMed] [Google Scholar]
- 44.Tomenchok LE, Gidley ML, Mena KD, et al. Children’s abrasions in recreational beach areas and a review of possible wound infections. Int J Environ Res Public Health. 2020;17:E4060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hundenborn J, Thurig S, Kommerell M, et al. Severe wound infection with photobacterium damselae ssp. damselae and vibrio harveyi, following a laceration injury in marine environment: a case report and review of the literature. Case Rep Med. 2013;2013:610632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Diaz JH, Lopez FA. Skin, soft tissue and systemic bacterial infections following aquatic injuries and exposures. Am J Med Sci. 2015;349:269–275. [DOI] [PubMed] [Google Scholar]
- 47.Kim PJ, Attinger CE, Steinberg JS, et al. Negative pressure wound therapy with instillation: past, present, and future. Surg Technol Int. 2015;26:51–56. [PubMed] [Google Scholar]
- 48.Hill R. Utilizing negative pressure wound therapy with instillation and dwell time to achieve source control of complex polymicrobial necrotizing Aeromonas hydrophila infection following a traumatic amputation: a case report. Wounds. 2020;32:364–368.. [PubMed] [Google Scholar]
- 49.Kim J, Chun BC. Effect of seawater temperature increase on the occurrence of coastal vibrio vulnificus cases: Korean national surveillance data from 2003 to 2016. Int J Environ Res Public Health. 2021;18:4439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mozer MA, Mozer CH, Kujath SW. A unique waterskiing injury leading to a necrotizing foot infection in an insulin-dependent diabetic. Int J Low Extrem Wounds. 2006;5:96–100. [DOI] [PubMed] [Google Scholar]
- 51.Park KH, Jung SI, Jung YS, et al. Marine bacteria as a leading cause of necrotizing fasciitis in coastal areas of South Korea. Am J Trop Med Hyg. 2009;80:646–650. [PubMed] [Google Scholar]
- 52.Wu J, Shamah S, Tsui E, et al. Trauma on the high seas: an overview of recreational water use injuries. Emerg Radiol. 2020;27:423–431. [DOI] [PubMed] [Google Scholar]
- 53.van Beeck EF, Branche CM, Szpilman D, et al. A new definition of drowning: towards documentation and prevention of a global public health problem. Bull World Health Organ. 2005;83:853–856. [PMC free article] [PubMed] [Google Scholar]
- 54.Papa L, Hoelle R, Idris A. Systematic review of definitions for drowning incidents. Resuscitation. 2005;65:255–264. [DOI] [PubMed] [Google Scholar]
- 55.Sachdeva RC. Near drowning. Crit Care Clin. 1999;15:281–296. [DOI] [PubMed] [Google Scholar]
- 56.Szpilman D, Morgan PJ. Management for the drowning patient. Chest. 2021;159:1473–1483. [DOI] [PubMed] [Google Scholar]
- 57.Ibsen LM, Koch T. Submersion and asphyxial injury. Crit Care Med. 2002;30(11 suppl):S402–S408.. [DOI] [PubMed] [Google Scholar]
- 58.Brown DJ, Brugger H, Boyd J, et al. Accidental hypothermia. N Engl J Med. 2012;367:1930–1938. [DOI] [PubMed] [Google Scholar]
- 59.Estella AA, Bello Fontaiña LP. Sea drowning: a case report and review of the literature. Monaldi Arch Chest Dis. 2011;75:135–137. [DOI] [PubMed] [Google Scholar]
- 60.Kapur N, Slater A, McEniery J, et al. Therapeutic bronchoscopy in a child with sand aspiration and respiratory failure from near drowning–case report and literature review. Pediatr Pulmonol. 2009;44:1043–1047. [DOI] [PubMed] [Google Scholar]
- 61.Christensen DW, Jansen P, Perkin RM. Outcome and acute care hospital costs after warm water near drowning in children. Pediatrics. 1997;99:715–721; Erratum in: Pediatrics. 1998;101(1 pt 1): 105. [PubMed] [Google Scholar]
- 62.Bugeja L, Cassell E, Brodie LR, et al. Effectiveness of the 2005 compulsory personal flotation device (PFD) wearing regulations in reducing drowning deaths among recreational boaters in Victoria, Australia. Inj Prev. 2014;20:387–392.. [DOI] [PubMed] [Google Scholar]
- 63.Lockhart TL, Jamieson CP, Steinman AM, et al. Life jacket design affects dorsal head and chest exposure, core cooling, and cognition in 10 degrees C water. Aviat Space Environ Med. 2005;76:954–962. [PubMed] [Google Scholar]
- 64.Uscgboating. Life Jacket Wear / Wearing Your Life Jacket. United States Coast Guard. Available at: https://uscgboating.org/recreational-boaters/life-jacket-wear-wearing-your-life-jacket.php. Published July 2021. Accessed August 1, 2021.
- 65.Quan L, Mangione T, Bennett E, et al. Use of life jackets and other types of flotation for in-water recreation in designated swim areas in Washington State. Inj Prev. 2018;24:123–128. [DOI] [PubMed] [Google Scholar]
- 66.Quistberg DA, Bennett E, Quan L, et al. Low life jacket use among adult recreational boaters: a qualitative study of risk perception and behavior factors. Accid Anal Prev. 2014;62:276–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Peden AE, Demant D, Hagger MS, et al. Personal, social, and environmental factors associated with lifejacket wear in adults and children: a systematic literature review. PLoS One. 2018;13:e0196421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Elijah E. Cummings Coast Guard. Authorization Act of 2020. U.S. Government Publishing Office. Available at: https://www.govinfo.gov/content/pkg/BILLS-116hr6395enr/pdf/BILLS-116hr6395enr.pdf. Accessed July 25, 2021.
- 69.Shatz D, Kirton O, McKenney M, et al. Personal watercraft crash injuries: an emerging problem. J Trauma. 1998;44:198–201.. [DOI] [PubMed] [Google Scholar]