Video Abstract
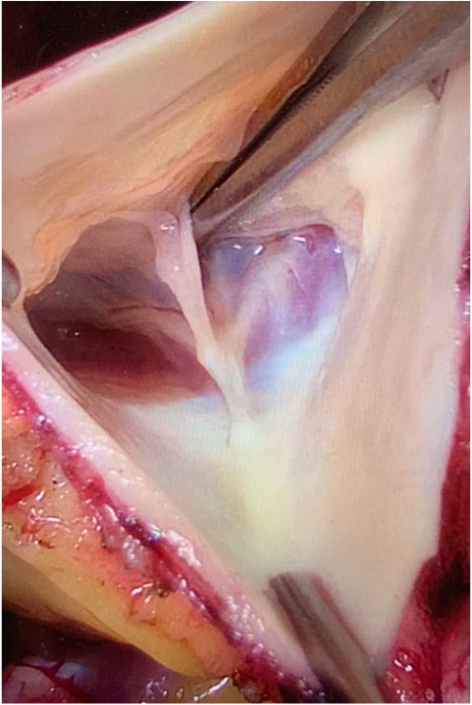
Intraoperative view of a bicuspid pulmonary valve.
Central Message.
In select patients with bicuspid or quadricuspid pulmonary autograft, good mid-term outcomes and valve function can be achieved. Careful valve analysis and implantation are of utmost importance.
Several recent publications have highlighted the advantages of the Ross procedure in terms of hemodynamics, quality of life, and survival.1,2 Congenital anomalies of the pulmonary valve (PV) have an estimated incidence of 0.1% and have been considered a relative contraindication, even with normal function. In this series, we aim to present the mid-term results of patients who underwent a Ross procedure with bicuspid or quadricuspid pulmonary autografts.
Methods
Patient Population
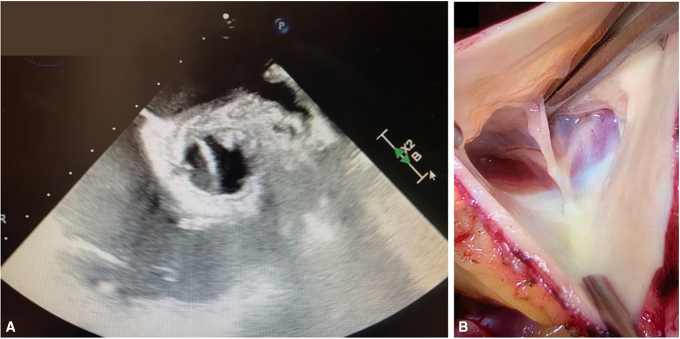
From 2010 to 2022, 640 Ross procedures have been performed in our institution. Eleven patients (8 bicuspid and 3 quadricuspid; 1.7% of the entire cohort) were diagnosed intraoperatively with a congenital anomaly of the PV (Figure 1, Video 1). Decision to proceed was made on an individual basis. Autograft was used in 7 patients, whereas it was abandoned in 4. Table 1 depicts demographics, surgical, as well as baseline and last follow-up echocardiogram data of these patients.
Figure 1.
Transesophageal echocardiography and intra-operative views of bicuspid pulmonary valve.
Table 1.
Demographics, preoperative echocardiograms, procedural characteristics, and last follow-up echocardiographic data
| Characteristics | Patients who underwent a Ross procedure (n = 7) | Patients in whom a Ross procedure was not performed (n = 4) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Demographics | |||||||||||
| Patient | 1∗ | 2 | 3 | 4 | 5 | 6 | 7 | 1 Mechanical Bentall |
2 Freestyle |
3 Freestyle |
4 Freestyle |
| Age, y | 50 | 20 | 43 | 49 | 60 | 26 | 35 | 50 | 49 | 60 | 59 |
| Sex | F | F | F | F | M | F | F | M | M | F | F |
| Indication | AS and PPM | AS | AS | AS | AS | AS | AR IE | AS and AR | AS and AR | AS | AS |
| AV morphology | Prosthesis | UAV | UAV | UAV | BAV | BAV | BAV | UAV | UAV | BAV | BAV |
| PV morphology | Bicuspid | Bicuspid | Quadricuspid | Quadricuspid | Quadricuspid | Bicuspid | Bicuspid | Bicuspid | Bicuspid | Bicuspid | Bicuspid |
| Associated comorbidities | DLP, AVR | Hypoplastic kidney | None | Coarctation repair | HTN, DLP, DM, smoker | HTN, DLP, asthma | None | Stroke in the past | None | HTN, DLP, previous PCI | DM, Asthma |
| Preoperative echocardiogram | |||||||||||
| LVEF, % | 70 | 60 | 65 | 60 | 65 | 60 | 65 | 65 | 45 | 75 | 65 |
| Mean aortic gradient, mm Hg | 61 | 43.9 | 57.3 | 36.2 | 68 | 57.7 | 4 | 53 | 21 | 37 | 64 |
| AVA, cm2 | 0.59 | 0.72 | 0.84 | 1 | 0.9 | 0.5 | N | 1.49 | 0.9 | 0.59 | 0.81 |
| Aortic annulus, mm | 21 | 19 | 21.2 | 22.3 | 21 | 23 | 26 | 28 | 30 | 20 | 23 |
| Sinus of Valsalva, mm | 26 | 25 | 26 | 39 | 39 | 32 | 31 | 44 | 48 | 28 | 18 |
| Procedural characteristics | |||||||||||
| Ross Technique | FSR | FSR | FSR | FSR | FSR | FSR | FSR | NA | NA | NA | NA |
| Autograft size, mm | 23 | 19 | 23 | 25.9 | 23 | 23 | 27 | NA | NA | NA | NA |
| Pulmonary homograft size, mm | 28 | 29 | 29 | 29 | 30 | 29 | 29 | NA | NA | NA | NA |
| Associated procedure | None | None | AAR | AAR | None | None | MVr | AAR | None | None | AAR |
| Last FU echocardiogram | |||||||||||
| FU | 8.2 y | 6.1 y | 5 y | 5 y | 4.7 y | 4.2 y | 7 mo | 5.9 y | 1 y | 6 mo | 1 y |
| LVEF, % | 50 | 60 | 60 | 55 | 60 | 60 | 45 | 60 | 48 | 60 | 60 |
| Mean gradient, mm Hg | 4 | 5 | 4 | 2 | 4 | 3.9 | 2 | 7 | 5 | 6 | 6 |
| AVA, cm2 | 2.6 | 2.7 | 3.42 | 3.6 | 4.4 | 2.7 | 4.4 | 3.1 | 3.7 | 2.7 | 3.4 |
| Autograft regurgitation | Trivial | Trivial | Trivial | Trivial | Trivial | Mild | Mild | Trivial | Trivial | Trivial | Trivial |
| Annulus, mm | 19.4 | 20.6 | 22 | 23 | 25 | 21 | 24 | 24 | 27 | 20 | 24 |
| Sinus of Valsalva, mm | 43 | 21 | 35 | 20.1 | 35 | X | 20 | 31 | NA | NA | NA |
| Ascending aorta, mm | 28 | 33 | 40 | 31 | 39 | 39 | 32 | 31 | NA | 23 | 32 |
| NYHA status | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 2 | 1 |
F, Female; M, male; AS, aortic stenosis; PPM, patient–prosthesis mismatch; AR, aortic regurgitation; IE, infective endocarditis; AV, aortic valve; UAV, unicuspid aortic valve; BAV, bicuspid aortic valve; PV, pulmonary valve; DLP, dyslipidemia; AVR, aortic valve replacement; HTN, hypertension; DM, diabetes mellitus; PCI, percutaneous coronary intervention; LVEF, left ventricle ejection fraction; N, non available; AVA, aortic valve area; FSR, freestanding root replacement; NA, not available; AAR, ascending aorta replacement; MVr, mitral valve repair; FU, follow-up; NYHA, New York Heart Association status.
Patient was reoperated at day 6 for severe AR, eccentric jet, and valve prolapse; she was treated with valve repair.
Surgical Technique
All procedures were performed using the autograft as a freestanding root. Care was taken to maintain the symmetry of the autograft by placing the commissures at 90 or 180° (depending on the morphology). The autografts were implanted deep in the left ventricular outflow tract to ensure adequate support from the native annulus. The coronary buttons were mobilized to avoid any tension on the anastomoses. Yearly clinical and echocardiographic evaluation was performed for each patient. The median follow-up is 5 years (interquartile range, 4.7-8.2) and 100% complete. The study was approved by the institutional review board, and individual patient consent was waived (#2017-1974 obtained June 21, 2017).
Results
Early Outcomes
One patient required early aortic valve reintervention due to aortic regurgitation (AR) that was caused by cusp prolapse at the time of implantation. Valve repair was successfully performed on postoperative day 6, and the patient has not had recurrence of AR at 8 years of follow-up.3 All other patients had normal autograft valve function at discharge (AR ≤1, mean gradient ≤5 mm Hg). There was no stroke, reintervention for bleeding, myocardial infarction, or perioperative death.
Mid-Term Outcomes
At last follow-up, all patients were alive with no cases of endocarditis or valve-related complications (major bleeding, stroke, transient ischemic attack). At a median follow-up of 5 years, echocardiographic examination shows AR ≤1 in all patients.
Patients in Whom a Ross Procedure Was Not Performed
Four patients with bicuspid PVs were not deemed good candidates for a Ross procedure based on the anatomy of their PV. One patient, aged 60 years, received a Bentall procedure. Another patient had an important discrepancy between his aortic and pulmonary annulus diameters. Finally, 2 patients presented important PV fenestrations with more than mild pulmonary regurgitation on intraoperative echocardiography. The preoperative and intraoperative characteristics of these patients are summarized in Table 1.
Discussion
Optimal aortic valve substitute in young and middle-aged adults remains a matter of debate. In recent years, there has been a renewed interest in the Ross procedure for this population. Several studies have highlighted the long-term benefits of this procedure and have contributed to expanding patient eligibility.1,4,5 Questions remain, however, about the suitability of a Ross procedure with a congenitally malformed PV.
Although the number of patients in this series is relatively small, several interesting findings emerge. Our experience suggests that the incidence of PV anomalies in patients with congenital aortic valve disease is ∼1% to 1.5%. This study also highlights the difficulty in identifying these anomalies on preoperative imaging. None of them were suspected despite comprehensive imaging, including preoperative cardiac magnetic resonance imaging in most patients.
PV anomalies have thus far represented relative contraindications to the Ross procedure. Although there have been some case reports suggesting good early- and mid-term outcomes, there has not been any series reporting systematic follow-up of patients with bicuspid or quadricuspid autograft.
Ultimately, the decision to perform a Ross procedure does not simply revolve around the anatomy of the PV. Several other factors, including age, aortic root anatomy, comorbidities, and the patient’s preferences must be considered. A 25-year-old woman contemplating pregnancy probably has a strong desire to avoid lifelong anticoagulation and is not a good candidate for a biological aortic valve replacement. In contrast, a 61-year-old man with AR who wishes to avoid open reintervention at any cost may have different opinions regarding these options. Thus, the decision to use a bicuspid or quadricuspid pulmonary autograft needs to be individualized, keeping these considerations in mind. When a bicuspid or quadricuspid PV is selected, it is important to maintain original commissural symmetry as to avoid inducing cusp prolapse.
Finally, the longitudinal follow-up of this series demonstrates that, in select patients, bicuspid and quadricuspid valves can maintain normal function and provide outcomes, within the first decade, that mirror those of patients with a tricuspid PV. Continued clinical and imaging follow-up is necessary to ensure that these valves maintain similar long-term performance (Video 1).
Footnotes
Disclosures: The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Supplementary Data
The Ross procedure using bicuspid and quadricuspid pulmonary valves. Video available at: https://www.jtcvs.org/article/S2666-2507(23)00140-2/fulltext.
Intraoperative inspection of a bicuspid pulmonary valve and postoperative transesophageal echocardiography showing short- and long-axis views of a bicuspid autograft. Video available at: https://www.jtcvs.org/article/S2666-2507(23)00140-2/fulltext.
References
- 1.Mazine A., El-Hamamsy I., Verma S., Peterson M.D., Bonow R.O., Yacoub M.H., et al. Ross procedure in adults for cardiologists and cardiac surgeons: JACC State-of-the-Art review. J Am Coll Cardiol. 2018;72:2761–2777. doi: 10.1016/j.jacc.2018.08.2200. [DOI] [PubMed] [Google Scholar]
- 2.El-Hamamsy I., Toyoda N., Itagaki S., Stelzer P., Varghese R., Williams E.E., et al. Propensity-matched comparison of the Ross procedure and prosthetic aortic valve replacement in adults. J Am Coll Cardiol. 2022;79:805–815. doi: 10.1016/j.jacc.2021.11.057. [DOI] [PubMed] [Google Scholar]
- 3.Vistarini N., Gebhard C., Desjardins G., El-Hamamsy I. Successful repair of a bicuspid pulmonary autograft valve causing early insufficiency after a Ross procedure. Ann Thorac Surg. 2016;101:e99–e101. doi: 10.1016/j.athoracsur.2015.06.119. [DOI] [PubMed] [Google Scholar]
- 4.Ghoneim A., Bouhout I., Losenno K., Poirier N., Cartier R., Demers P., et al. Expanding eligibility for the Ross procedure: a reasonable proposition? Can J Cardiol. 2018;34:759–765. doi: 10.1016/j.cjca.2018.01.023. [DOI] [PubMed] [Google Scholar]
- 5.Chauvette V., Bouhout I., Tarabzoni M., Wong D., Bozinovski J., Chu M.W.A., et al. The Ross procedure in patients older than 50: a sensible proposition? J Thorac Cardiovasc Surg. 2022;164:835–844.e5. doi: 10.1016/j.jtcvs.2020.09.121. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The Ross procedure using bicuspid and quadricuspid pulmonary valves. Video available at: https://www.jtcvs.org/article/S2666-2507(23)00140-2/fulltext.
Intraoperative inspection of a bicuspid pulmonary valve and postoperative transesophageal echocardiography showing short- and long-axis views of a bicuspid autograft. Video available at: https://www.jtcvs.org/article/S2666-2507(23)00140-2/fulltext.