Abstract
During 2019, the SARS‐CoV‐2 emerged from China, and during months, COVID‐19 spread in many countries around the world. The expanding data about pathogenesis of this virus could elucidate the exact mechanism by which COVID‐19 caused death in humans. One of the pathogenic mechanisms of this disease is coagulation. Coagulation disorders that affect both venous and arterial systems occur in patients with COVID‐19. The possible mechanism involved in the coagulation could be excessive inflammation induced by SARS‐CoV‐2. However, it is not yet clear well how SARS‐CoV‐2 promotes coagulopathy. However, some factors, such as pulmonary endothelial cell damage and some anticoagulant system disorders, are assumed to have an important role. In this study, we assessed conducted studies about COVID‐19‐induced coagulopathy to obtain clearer vision of the wide range of manifestations and possible pathogenesis mechanisms.
Keywords: anticoagulant, blood coagulation, coagulation disorders, coagulopathy, COVID‐19, SARS‐CoV‐2
In December 2019, a new coronavirus which named SARS‐CoV‐2 (Severe Acute Respiratory Syndrome Coronavirus‐2) emerged from China, and during months, COVID‐19 spread in many countries around the world. Clinical manifestation spectrum associated with COVID‐19 is various and not completely clear. The disease presentations can range from an asymptomatic infection or mild illness to severe pneumonia, sepsis, loss of organs function, and even death. Although most people with COVID‐19 will face mild manifestations, some patients will demonstrate severe clinical signs that lead to hospitalization and intensive care unit (ICU) admission. These clinical complications include severe lung dysfunction, sepsis, shock, or multiple organ failure. Coagulation disorders and thrombotic complications were reported in COVID‐19 patients. The mechanism of Coagulation disorders is not precise in COVID‐19 patients. The current study tried to provide a comprehensive view of the pathophysiology, mechanisms, therapeutic approaches, and considerations about the coagulopathy during COVID‐19.
1. INTRODUCTION
In December 2019, a new coronavirus which named SARS‐CoV‐2 (Severe Acute Respiratory Syndrome Coronavirus‐2) emerged in Wuhan, Hubei province, China. The conducted disease by this virus is coronavirus disease 2019 (COVID‐19) rapidly spread in many countries around the world. 1 , 2 , 3 , 4 After a while, this novel coronavirus caused one of the most important health issues worldwide. 5 , 6 , 7 , 8 Clinical manifestation spectrum associated with COVID‐19 is various and not completely clear. The disease presentations can range from an asymptomatic infection or mild illness to severe pneumonia, sepsis, loss of organs function and even death. 9 , 10 , 11 , 12 Previous important coronaviruses, SARS‐CoV (SARS‐CoV‐1) and the Middle East respiratory syndrome (MERS‐CoV), responsible for the outbreak in 2002–2003 and 2012, respectively, and associated with severe and fatal diseases. 13 , 14 , 15 Since the start of the pandemic by COVID‐19, different therapeutic approaches are suggested. 16 , 17 , 18 , 19 , 20 , 21 , 22 Although most people with COVID‐19 will face mild manifestations, some patients will demonstrate severe clinical signs that lead to hospitalization and intensive care unit (ICU) admission. These clinical complications include severe lung dysfunction, sepsis, shock or multiple organ failure. 23 , 24 There is a wide range of literature about the severity of COVID‐19 and its potential life‐threatening clinical conditions. 25 Coagulation disorders and thrombotic complications were reported in the COVID‐19 patients. 26 , 27 The mechanism of coagulation disorders is not precise in the COVID‐19 patients. In this regard, there are valuable researches available. 28 Furthermore, in this study, we conducted studies in COVID‐19‐associated coagulopathy to obtain a clearer vision of this wide range of manifestations and possible pathogenesis mechanisms. In addition, we tried to review the current literature in this particular field to provide an update for clinicians and researchers.
2. POSSIBLE MECHANISMS FOR COAGULATION DISORDERS IN COVID‐19
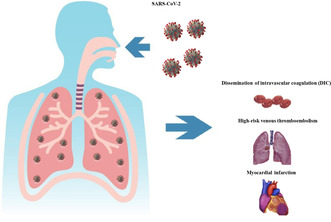
Disorders in coagulation system such as myocardial infarction and thrombotic complications that affect both venous and arterial systems occur in COVID‐19. 29 , 30 The coagulopathy conditions of COVID‐19 are not only limited to the primary course of the disease and could be during post‐infection or long COVID‐19 conditions. 31 These coagulation disorders are due to excessive induction of inflammation, disturbing gas exchange, immobilization and dissemination of intravascular coagulation (DIC). 26 , 27 , 32 It is not yet completely clear how SARS‐CoV‐2 promotes coagulopathy. However, some factors, such as damage to pulmonary endothelial cells and some disorders in the fibrinolysis system, are assumed to have an important role. It is demonstrated that the level of factor VIII, fibrinogen, and also von Willebrand (VWF) in the COVID‐19 disease are higher than in normal cases. Considering this, there is a growing body of research reports, which shows coagulation disorders despite the use of anticoagulant agents. 32 , 33 , 34 , 35 Some laboratory findings can support a poor prognosis in a patient infected by a novel coronavirus. Among those, some data obtained from coagulation parameters indicate that elevated levels of D‐dimer (>3000 ng/mL) can be considered to predict unfavorable outcomes include death in severe COVID‐19. 1 , 9 , 36 , 37 , 38 , 39 Besides arterial and venous thrombosis, pro‐inflammatory cytokines, which lead to cytokine storm (with unknown causes), are also associated with higher mortality risk. 40 , 41 The relationship between these two processes, thrombosis and inflammation, which strengthen each other, has been shown before and is compatible with the above findings. 42 , 43 It has been shown that anticoagulant factors like heparin and platelets, besides their original function, also act as anti‐inflammatory and can modulate immune response. 44 , 45 Additionally, medications like Dipyridamole with antiplatelet, antiviral and antioxidant features propose to be used in the COVID‐19 hospitalized patients. 46 , 47 Although, some patients are still developed thrombosis despite using drugs as a coagulant prevention strategy. Further studies are required due to incomplete documents about heparin efficacy, frequency of a dose and timely administration of anticoagulant agents. 48 Different studies recently suggested that low‐molecular‐weight heparin (LMWH) would induce statistically significant decrease in mortality rate of severe disease and who present sepsis‐induced coagulopathy (SIC) score ≥4 or D‐dimer levels >6‐fold upper from normal rang. 49 Disturb coagulation function, including elevated fibrinogen degradation products, factor VIII (FVIII), VWF levels and fibrinogen levels, reported in th COVID‐19 patients. 50 Derangement of hemostasis associated with proteins involved in the coagulation process can be caused by cytokine storm which leads to a fundamental change in pro and anticoagulant proteins activity. 41 , 51 In one study, Christophe et al. report that reactivation of the immune system stimulates coagulation disorders. Moreover, increasing fibrinogen and FVIII levels and disturbing the fibrinolysis process have been shown in all patients infected by COVID‐19. 52 Disorderliness in other thrombosis and fibrinolysis factors are also associated with severe thrombotic involvement. Levels of tPA (tissue‐type plasminogen activator), TAFIa/I (thrombin activatable fibrinolysis inhibitor) and PAI‐1 (plasminogen activator inhibitor 1) have a remarkable increase in the number of the critical patient than those patients who did not experience a severe form disease. High levels of TAFI antigen and PAI‐1 seems to be associated with mortality in cardiovascular disease and arterial thrombosis. 32
3. IMMUNE SYSTEM AND COAGULATION
Initiating immune response to invasive viral pathogens leads to disturbing the harmony between factors involved in the homeostatic mechanism associated with coagulation. Regardless of forming a clot, platelets mediate interaction between TLRs (toll‐like receptors) and activate inflammatory cascade to eliminate viral infections. 32 There are some pieces of evidence about the importance of TLRs in the COVID‐19 pathogenesis and induction of coagulopathy effects. 53 , 54 , 55 Too much‐activated platelet and the cascade of events leads to coagulation blood, responsible for elevated D‐dimer and thrombocytopenia. Apart from these, damages of the vascular endothelium, immune deregulation, increasing von Willebrand factor, and accumulation of macrophage, monocyte, platelet and lymphocyte have significant roles in coagulopathy after viral infection. 32 , 56 , 57 , 58 There is a relationship between endothelial cell activation and increasing in VWF level. Some observations suggest the elevation of VWF in COVID‐19. 50 , 59 , 60 ADAMTS13 (a disintegrin and metalloproteinase with thrombospondin type 1 motif, member 13) Enzyme, or VWFCP (von Willebrand factor‐cleaving protease), regulates the VWF multimers size during synthesized by endothelial cells and megakaryocytes. A low level of ADAMTS13 can cause thrombotic thrombocytopenic purpura (TTP). 61 , 62 , 63 , 64 One study reported that ADAMTS13 and ADAMTS13/VFW: Ag ratio among survivors and non‐survivors patients indicated a remarkable decrease in the deceased patients than survivors. 35
Also, poor clinical prognosis in the COVID‐19 patients with coagulation and death is frequently occurs in patients representing myocardial infarction than in patients without cardiac involvement. 65 Additionally, level of Troponin‐T in the COVID‐19 patients shows statistically significant association with increase PT, PTT and D‐dimer elevation.
4. COAGULATION ABNORMALITIES IN OTHER EMERGING CORONAVIRUSES
Similar to the COVID‐19 infection, coagulation abnormalities, PT and PTT prolongation elevated D‐dimer and high‐risk venous thromboembolism are reported in SARS‐CoV. 32 , 66 , 67 However, finding from lung autopsies in patients with SARS‐CoV typically identified pulmonary thromboembolism. 67 , 68 A postmortem autopsies study on a SARS‐CoV‐infected case indicated polyangiitis and blood vessel disorders lead to multi‐organ failure. 32 A few reported also implicated hypercoagulability in MERS‐CoV with a high incidence of DIC in deceased patients. 3 , 32 , 69
5. COVID‐19 COAGULOPATHY AND INDUCED THROMBOEMBOLIC EVENTS
Dysregulation in coagulation and the anti‐thrombotic system lead to thromboembolic events in COVID‐19. 70 , 71 , 72 These thromboembolic events could be represented in a variety of clinical manifestations. There are different terminology and clinical conditions for thromboembolic events. These phenomena could be exhibited as thrombosis, embolism, deep vein thrombosis (DVT) and venus thromboembolism (VTE). Furthermore, a summary of highlighted researches in the area of coagulopathy events and thrombosis are provided in Table 1.
TABLE 1.
A summary of important studies in the field of the DVT, PE and VTE.
| Author name | Country | Population | Age | Background disease | Gender (male/female) | Prevalence | Pharmacological intervention | Main outcome | Ref. |
|---|---|---|---|---|---|---|---|---|---|
| Nahum | French | 34 | 62 ± 8 | DBT 15, HTN 13 | 29/5 | 23 | – | Better prognosis for anticoagulation treatment but despite anticoagulation the DVT should be consider | 78 |
| Demelo‐Rodrígueza | Spain | 156 | 66.7 ± 15.2 | – | 102/54 | 23 | Enoxaparin and bemiparin | D‐dimer >1570 ng/mL is associated with asymptomatic DVT | 174 |
| Giorgi‐Pierfranceschi | Italy | 124 | 71.8 | – | 77/46 | 9 and PE 5 | Enoxaparin | High prevalence of asymptomatic proximal DVT in hospitalized patients | 79 |
| Longchamp | Switzerland | 25 | 68 | Chronic therapeutic anticoagulation 2 | 16/9 | DVT 6, PE 5, and 3 both | Heparin | Prevalence of VTE is high (32%) among critically ill patients/VTE occurred early in course of the disease | 175 |
| Santoliquido | Italy | 84 | 67.6 | Obesity 14, HTN 44, DBT 20, CVD 11, Cancer 14, Previous VTE 3 | 61/23 | 10 | Enoxaparin or fondaparinux | DVT may occur among non‐ICU hospitalized patients for despite thromboprophylaxis | 176 |
| Ren | China | 48 | 70 | HTN 19, DBT 13, CVD 11, Cerebrovascular disease 7 | 26/22 | 35 | LMWH | High incidence of DVT in critically ill patients | 177 |
| Zhang | China | 143 | 63 | – | 74/69 | 66 | LMWH | The prevalence of DVT is high and is associated with adverse outcomes in hospitalized patients | 178 |
| Zhang | China | 81 | 62 | HTN, hyperglycemia, CVD, cerebral infarction, cerebral hemorrhage, malignancy | – | 55 | LMWH | High incidence of DVT and needs for LMWH and ultrasonography | 179 |
| Chen | China | 88 | 63 | HTN, DBT, malignancy, gastric ulcer, thyroid disease, HBV, fatty liver | 54/9 | 88 | LMWH | More effective VTE prevention and management strategies may need | 180 |
| Cho | USA | 158 | 67.4 ± 14.6 | DBT, ascites, CVD, HTN, malignancy | 85/73 | 52 | UFH and LMWH | D‐dimer<6494 ng/mL may exclude DVT | 181 |
| Ierardi | Italy | 234 | 61.6 | Asthma 10, Cancer 26, HTN 93 | 70/164 | 25 | Heparin | High rate of DVT found in severe patients and its correlation with respiratory parameters | 182 |
| Koleilat | USA | 135 | 64 | CVD 16, COPD 13, CKD 28, DBT 51, VTE 10, HTN 94 | 72/63 | 18 | Apixaban, bivalirudin, UF and LMWH | Increased risk of DVT, D‐dimer and fibrinigen are reflection of the risk | 183 |
| Pizzolo | Italy | 43 | 66 | HTN 23, DBT 6, cancer 4, CVD 14 | 29/14 | 12 | Enoxaparin | Have high prevalence of VTE regardless of a thromboprophylaxis | 184 |
| Jeune | France | 42 | 64.6 | HTN 20, DBT 13, CVD 7, cancer 3 | 23/19 | 8 | – | High prevalence asymptomatic DVT in the first days of hospitalization may be related to poor prognosis | 185 |
| Marone | Italy | 101 | 65 | Obesity 4, malignancy 2 | – | 42 DVT and 24 PE | LMWH | VTE can arise regardless of severity of respiratory impairment | 71 |
| Trimaille | France | 289 | 62 ± 17 | – | 171/118 | 49 VTE, 11 DVT, 40 PE | Enoxaparin, fondaparinux, UFH | Relationship between leukocytosis count and VTE | 186 |
| Artifoni | France | 71 | 64 | HTN 29, DBT 14, cancer 4, history of VTE 5 | 43/28 | DVT 15, PE 7 | – | Despite thromboprophylaxis, the risk of VTE is non‐ICU inpatients | 187 |
| Middeldorp | Netherlands | 198 | 61 | History of VTE 10, cancer 6 | 130/68 | DVT 26, VTE 39, PE 13 | – | VTE risk is high in ICU patients | 188 |
| Alonso‐Fernandez | Spain | 30 | 64.5 | CVD 12, RCD 5 | 19/11 | 15 | – | More age and D‐dimer>1 μg/mL presented a high prevalence of PE | 80 |
| Stefely | USA | 102 | 61 | – | 68/34 | DVT or PE 23% | Factor V activity >150 IU/dL frequent in VTE | 84 | |
| Chen | China | 25 | 65 | HTN 10 (40%), DBT5 (20%), CVDs 4 (16%), DVT 1 (4%) | 15/10 | 10 | LMWH | Importance of high D‐dimer level | 189 |
| Leonard‐Lorant | France | 106 | – | – | 80/26 | 32 | – | D‐dimer>2660 μg/L had a great sensitivity and specificity for PE | 1, 83 |
| Minuz | Italy | 10 | – | 4 HTN, 1 thromboembolic diseases | – | 6 | – | PE evaluation in high D‐dimer | 190 |
| Bompard | France | 134 | 64 | – | 94/40 | 32 | LMWH | Prophylactic anticoagulation did not avoid PE | 191 |
| Cobelli | Italy | 55 | 62 | 22 HTN, 7 CVD, 11 DBT, 4 COPD, 1 CKD | 39/16 | 28 | – | PE overlapping areas of ground‐glass opacities | 192 |
| Al‐Samkari | USA | 3239 | 61 | 464 DBT, 1977 HTN, 273 COPD, 431 CVD, 407 CKD | 2088/1141 | 204 | – | Early therapeutic anticoagulation did not affect survival | 193 |
| Patell | USA | 163 | – | – | – | 4 | Enoxaparin, Heparin | High rate of thrombosis after the discharge | 194 |
| Voicu | France | 56 | – | 26 HTN, 25 DBT, 11 CVD | 42/14 | 20 | Enoxaparin, Heparin | DVT patients had significantly higher D‐dimer compared with non‐DVT patients but no difference in fibrinogen | 195 |
Abbreviations: CKD, chronic kidney disease; CVD, Cardiovascular; DBT, diabetes; HBV, Hepatitis B virus infection; HTN, Hypertension; LMWH, Low molecular weight heparin; RCD, Respiratory chronic disease; UFH, unfractionated subcutaneous heparin; VTE, Venous thromboembolism.
5.1. Venus thromboembolism (VTE)
VTE events, in the form of the DVT, cerebral venous thrombosis (CVT), or pulmonary embolism (PE), are estimated as the cause of death in 5%–10% of hospitalized individuals with SARS‐CoV‐2. 73 , 74 VTEs are includes DVT, PE, CVT, or even a combination of these conditions. The incidence of VTE in the COVID‐19 patients was in range of 7%–26% based on the different clinical conditions of patients. 75 There are a significant number of studies about VTE and COVID‐19. Conducted studies on VTE suggested a higher incidence of the VTE in ICU (Intensive Care Units) admitted patients. 76 Regardless of other conducted reports in the field of coagulopathy and thromboembolic events in COVID‐19, a conducted study by Mei et al., 77 there was no statistically higher incidence of the VTE in comparison of the COVID‐19 hospitalized and community‐acquired pneumonia (CAP). Nevertheless, even Mei et al. 77 mention COVID‐19‐associated hypercoagulability. Furthermore, elevated D‐dimer was the most frequent laboratory finding. Besides that, Nahum et al. 78 highlighted a better prognosis for anticoagulation treatment in the COVID‐19 patients and the importance of the DVT consideration in these patients. This importance of the DVT could be an emphasis by considering the Giorgi‐Pierfranceschi and colleagues' study either. 79 Giorgi‐Pierfranceschi indicates higher prevalence of patients with asymptomatic DVT and associated PE in hospitalized individuals infected by SARS‐CoV‐2.
Alonso‐Fernández and colleagues 80 concluded an increased age and D‐dimer >1 μg/mL are frequent in COVID‐19 with PE presentation. The importance of D‐dimer monitoring was also suggested by other studies. 81 , 82 , 83 Regardless of the D‐dimer level, the factor V activity is suggested as a biomarker for PE monitoring during COVID‐19 by Stefely et al. 84
Meanwhile, investigation of cerebral venous sinus thrombosis represents good outcomes in the most COVID‐19 patients with CVT. 85 In addition, the gender assessment indicates the female gender as the dominant portion of the patients. Furthermore, Cavalcanti and colleagues 86 study suggested that the median duration between the COVID‐19 onset of symptom to development of thromboembolic events in patients with CVT is 2–7 days.
5.2. Anticoagulant treatment
There are varieties of studies investigating the anticoagulant treatment guidelines in the COVID‐19 patients. 87 , 88 , 89 , 90 Highlighted researches are listed in Table 2. These studies indicate that the Heparin/LMWH is used in the most common anticoagulation strategy, including for a wide range of the coagulopathy events such as DVT and VTE. In addition, heparin's anticoagulant activity is also familiar with antiviral activity against enveloped viruses, including coronaviruses. 91 , 92 This property of heparin results from the binding of viral glycoproteins to glycosaminoglycans (GAGS) such as heparan sulfate (HS) that have widespread functions within the body. In herpes simplex virus (HSV) infections, heparin competition with surface glycoproteins in host cells can inhibit viral entrance. In addition, in Zika virus infection heparin can reduce human neural progenitor cell death. 93 , 94 , 95 Moreover, it has indicated that soluble heparin can bind to SARS‐CoV‐2 spike, leading to viral entry inhibition. 96 , 97 , 98 , 99
TABLE 2.
Highlighted researches in the field of therapeutic approaches.
| First author | Country | Patients number | Pharmacological intervention | Objective | Patients background condition | Maine study outcome | Ref. | |
|---|---|---|---|---|---|---|---|---|
| Drug | Dose (mg or UI per day) | |||||||
| Santoro | Spain, Italy, Ecuador, Cuba, Germany, China, Canada | 7824 | Single or dual APT | – | APT efficacy in COVID | HTN, DBT, CVD | APT during hospitalisation could be associated with lower mortality, shorter mechanical ventilation and no risk of bleeding | 196 |
| Spiegelenberg | Netherlands | 1154 | 92 VKA and 98 DOAC | – | Prior therapeutic anticoagulation use and clinical outcome | – | No associations between prior use of therapeutic anticoagulation and overall mortality | 197 |
| Tremblay | USA | 3772 | Anticoagulant or APT | – | Empiric therapeutic anticoagulation | Lung disease, history of VTE, obesity | AC alone is unlikely to be protective for COVID‐19–related morbidity and mortality | 198 |
| Rivera‐Caravaca | HOPE registery | 110 | VKA and DOAC | – | Prior anticoagulant efficacy | CVD | Patients on OAC therapy at hospital admission showed lower survival and higher mortality risk but bias was reported in the comorbidity | 199 |
| Lachant | USA | 107 | DOAC, Warfarin, LMWH | – | Chronically anticoagulated before COVID | HTN, DBT, CKD, VTE, COPD | May protect against thrombotic complications and decrease disease severity | 200 |
| Santoliquido | Italy | 84 | Enoxaparin or fondaparinux | – | Thromboprophylaxis | HTN, DBT, cancer, VTE | DVT occur among non‐ICU patients despite guideline recommended thromboprophylaxis | 176 |
| Vlot | Netherlands | 16 | Anti Xa | 0.1–0.3 IU/mL | Anti Xa assessment | HTN | Anti Xa dose adjustment | 201 |
| LMWH | 7600 IU | |||||||
| Ayerbe | Spain | 2075 | Heparin | – | Heparin assessment | Non | 14% mortality in Heparin admitted group | 202 |
| Brouns | Netherlands | 101 | OAT | – | OAT assessment | No protection against mortality by OAT | 203 | |
| Christie | Georgia | 5 | tPA | 50 mg IV (25 mg bolus) | Case | All five patients improved | 204 | |
| Ferguson | USA | 141 | LMWH | 1.5 mg/kg | DVT prophylaxis | LMWH not useful for DVT prophylaxis in COVID‐19 patients | 205 | |
| Hanif | USA | 921 | Warfarin, UFH | – | Treatment and prophylaxis for VTE and thrombosis | 33 patients with anticoagulant prior to the admission | Patients on therapeutic anticoagulation had a higher mortality compared with patients on prophylactic anticoagulation | 206 |
| Shi | China | 42 (21 case and 21 control) | LMWH | – | LMWH efficacy | Non | LMWH could significantly decrease IL‐6 and improve the Lymphocyte count in COVID‐19 patients | 207 |
| Sivaloganathan | UK | 60 case/120 control | Anticoagulant or APT | – | Non | Pre‐admission anticoagulants or antiplatelet agents did not make difference in COVID‐19 mortality or ICU admission | 208 | |
| Stessel | Belgium | 78 | LMWH | – | HTN, DBT, CKD, CLD | CRRT could be reduced by implementation of thromboprophylaxis | 209 | |
| Yormaz | Turkey | 96 (48 case and 48 control | LMWH | 4000 UI | LMWH clinical outcome | HTN, DBT, CAD | LMWH shows improve in laboratory findings, lymphocyte count, CRP, and D‐dimer results | 210 |
| Mattioli | Italy | 105 | Enoxaparin | 80 mg | HTN, DBT, Obesity, Smoking | Intermediate doses of LMWH could be useful and also safe in patients with CKD | 211 | |
| Rossi | Italy | 70 | OAT | – | Direct oral anticoagulants | HTN, obesity, DBT | DOAC intake is associated with a decreased mortality risk | 212 |
| Tang | China | 449 | LMWH/UFH | – | Heparin efficacy on COVID‐19 | HTN, DBT | LMWH associated with better prognosis in severe COVID‐19 patients | 49 |
Abbreviations: anti Xa, anti‐factor Xa; APT, antiplatelet therapy; CAD, Coronary Artery Disease; CKD, Chronic kidney disease; CLD, Chronic liver disease; CRRT, continuous renal replacement therapy; DBT, Diabetes; DOAC, direct oral anticoagulants; HTN, hypertension; Non, represents no relevant medical history; OAT, oral antithrombotic therapy; tPA, tissue plasminogen activator; UFH, unfractionated heparin; VKA, vitamin K antagonists.
Despite Heparin's widespread use as an anticoagulant agent, it demonstrated that heparin is associated with anti‐inflammatory activity via interaction and modulates inflammation mediators. This anti‐inflammatory activity leads to a decreased level of IL‐8 and IL‐6. 99 , 100 , 101 heparin can also bind to acute‐phase proteins and complement factors ti induce the anti‐inflammatory function of heparin. 95 , 101 In this regard, the importance of anticoagulant therapy for reducing the cytokine storm has been declared. 102
Using heparin in the COVID‐19 patients will help to decrease the risk of thromboembolic incidence, which may be associated with fatal outcomes. However, the management of bleeding risk and administration of effective doses of drugs should be considered. Close monitoring of the D‐dimer, platelet count and PT (prothrombin time) in all patients with suspected or confirmed COVID‐19 are also recommended. Further investigation for the anti‐inflammatory effect of heparin due to the bidirectional interaction between these two systems, inflammation and coagulation seems to be necessary.
Despite all of the mentioned features and potential benefits of Heparin therapy, there are some concerns. For example, we mentioned Heparin‐induced thrombocytopenia (HIT) (due to the heparin attachment into the platelet factor 4) and Heparin resistance (due to the high‐dose UFH, for instance, UFH > 35,000 IU per day). Although Heparin resistance and HIT are rare events, even in COVID‐19. In the conducted study by Huang et al., 103 it's been suggested that heparin therapy and identification of HIT may be an essential element in the COVID‐19 mortality reduction. There is no exact information about the HIT in cases with COVID‐19. However, by considering these limited studies, the anticoagulant Argatroban seems to be a great replacement for fracture heparin in confirmed coronavirus patients involved with thromboembolic events and HIT.
Investigation of the etiologic factors for Heparin resistance in four cases of COVID‐19 suggested the Factor VIII level is increased in patients. 104 An increase in factor VIII could be a possible pathophysiology for heparin resistance in COVID‐19. Also, a high incidence of heparin resistance was reported by White et al. 105 This manner highlights the importance of further research in anticoagulation and optimization of the therapeutic dose for the treatment of coagulopathy events or even for prophylaxis in the COVID‐19 patients.
Furthermore, in the context of the anticoagulant treatment for COVID‐19 some points need to be considered include, there is any robust evidence that leads to indicate the unrestricted use of anticoagulants in patients infected with the COVID‐19, without clear confirmation of a thromboembolic event or hospitalization in intensive care. 106 , 107 It could be concluded that confirmation of COVID‐19 is not indicative of the use of anticoagulants. Patients in moderate stage of COVID‐19 could be concidered as a candidate for thromboprophylaxis if there was low‐bleeding risk, represents high D‐dimer levels, or require supplemental oxygen. 107
5.3. SARS‐CoV‐2 variants and coagulopathy
Effects of different SARS‐CoV‐2 variants in the severity of disease, epidemiological pattern, and clinical presentation of patients are previously described. 108 These difference in the severity of disease between variants also affects coagulopathy patterns. There are limited studies about this field of study. The in‐vitro study indicates more potential for coagulation in the alpha variant in compare with the Omicron. 109 In addition, in clinically evaluated samples, Omicron variants are less competent for micro clot formation or coagulation abnormalities in comparison with alpha, beta and delta variants. 110 , 111 As a point of view, it seems that one of the aspects of less sever Omicron variant infection in compare with previous variants is associated with its coagulation alteration profile.
6. NOVEL RESEARCH FOR THE PATHOPHYSIOLOGY OF COAGULOPATHY IN COVID‐19
There is some novel pathophysiology for coagulopathy in COVID‐19. In this study, we only provide a view of some of the most important novel mechanisms for coagulopathy in COVID‐19. Some important original researches about Endothelial cell dysfunction, Complement activation, or other important mechanisms are provided in Table 3. More discussion about these mechanisms are provided in the next sections. However, it should be considered that these mechanisms are tight links.
TABLE 3.
Some highlighted studies about the novel pathogenesis mechanisms of the COVID‐19 associated coagulopathy.
| First author | Country | Possible mechanism | Sample | Final conclusion | Ref | |
|---|---|---|---|---|---|---|
| Type | Number | |||||
| Cugno | Italy | Complement activation, endothelial damage and disease severity | COVID‐19 | 148 | MAC levels correlated with vWF and paralleled disease severity | 152 |
| Magro | USA | Complement activation, endothelial damage | COVID‐19 | 5 | Co‐localization Spike with C4d and MAC in lung and skin biopsy, microvascular injury and coagulopathy | 149 |
| Goshua | USA | Endotheliopathy | COVID‐19 | 68 | Increase in vWF and soluble P‐selectin mortality significantly correlated with VWF antigen and soluble | 59 |
| Nagashima | Brazil | Endothelial dysfunction | Postmortem | 6 | Endothelial dysfunction conditions might lead to systemic thrombotic events | 213 |
| Busch | Netherlands | Hypercoagulability and NETosis | COVID‐19 | 228 | Hypercoagulability and thrombotic events are driven by NETosis, contact activation of coagulation system, and complement | 214 |
| Cimmino | Italy | IL‐6, Vitamin D and | HUVEC | – | Vitamin D significantly reduced TF, adhesion molecules and ACE2 expression in IL‐6‐treated cells | 215 |
| Zuo | USA | Hypercoagulability and NETosis | COVID‐19 | 44 | Potential relationship between NETosis and thrombosis | 216 |
Abbreviations: CS, Cross‐sectional; HUV, Human Umbilical Vein Endothelial Cells; MAC, membrane attack complex; TF, tissue factor; vWF, von Willebrand factor.
6.1. Endothelial cells dysfunction
The vascular endothelium constitutes the inner cellular layer of vessels, which forms a barrier between blood and tissue. 112 Since it is related to both blood cells and other cells, it plays a critical role in different mechanisms such as maintaining hemostasis, prompting recruitment, adhesion surface and interaction of platelets and leucocytes on thrombogenic surfaces, and regulation of vascular tone through producing various vasoactive substances. 112 , 113
The required receptor for attachment of SARS‐CoV‐1 and 2 to epithelial cells is ACE2 which expressed on the surface of these cells. Yang and colleagues showed that epithelial cells infected by SARS‐CoV‐1 could be a target for autoantibodies. Therefore, we can conceive such an outcome in SARS‐CoV‐2. 114 The infection of endothelial cells with the virus and subsequent effects is the key point to endothelial dysfunction in patients. High levels of pro‐inflammatory cytokines such as IL‐1, IL‐6 and TNF and ferritin activate the endothelial cells of the lung vessels. 115 , 116 , 117 Furthermore, higher levels of VWF were seen in the COVID‐19 patients, which is related to reduced activity of disintegrins metalloproteinase with ADAMTS13. 118 All these events can eventually lead to the development of thrombotic microangiopathy. 119 Some other markers that indicate endothelial damage were also investigated in COVID‐19. Goshua and colleagues reported higher levels of P‐selectin (an indicator for endothelial cells and platelet activation) in ICU‐admitted patients. Moreover, they have seen that elevated amounts of thrombomodulin are associated with a higher mortality risk. 59 The other investigated factor is circulating endothelial cells (CECs), which are detached endothelial cells from damaged vessels. These cells exist in normal individuals at low levels; however, an increased count of CECs denotes the endothelial injury. Since other coronaviruses are cytopathic 120 and can induce the intracytoplasmic NOD‐like receptor protein 3 (NLRP3) inflammasome, which plays a role in the detachment of endothelial cells, as seen in the case of the Kawasaki disease 121 and also triggering cytokine storm. 122 Thereby, CECs are interesting potent markers in studying coagulopathies in COVID‐19. Guervilly and colleagues reported an increased number of CECs in the COVID‐19 patients, especially those who were admitted to ICU. They also showed that CECs are correlated to elevated plasma levels of soluble vascular cell adhesion molecule 1 (sVCAM1). 123 Falcinelli and colleagues also confirmed these results. In addition to sVCAM1, they reported an increased amount of soluble intercellular adhesion molecule 1 (sICAM1) in COVID‐19. 124 Taken together, we highly suggest implementing preventing measures such as blocking pro‐inflammatory cytokines and NLRP3 inflammasome as effective measures to reduce the risk of endothelium damage by COVID‐19.
6.2. Platelets activation in COVID‐19
Since there is a considerable number of platelets circulating in the blood vessels, they might be the first cells to face the virus in the blood. 125 The platelet response against the RNA viruses is initiated by the interaction between the viral genome and the toll‐like receptor 7 (TLR7) located in the endolysosomes of platelets. 126 , 127 While it is not clear whether platelets express ACE2 or not, 125 the SARS‐CoV‐2 genome is isolated from platelets by Zaid and colleagues. 128 The mechanism of internalizing ssRNA viruses and subsequent events have been shown in the case of influenza. The virus can enter the platelets through unknown receptor‐independent mechanisms. Following the entrance of the virus to the platelets and in acidic pH, activation of TLR7 leads to releaseing of α‐granule and interaction P‐selectin and CD40L in platelets with neutrophils. 127 In addition, activation of TLR7 triggers the release of the complement C3 component. The complement C3 stimulates the phenomena of NETosis by neutrophils, in which they release neutrophil extracellular traps (NETs), 126 extracellular components consist of cytosolic and granule proteins that are made of decondensed chromatin. NETs traps help the immune system in fighting different pathogens including viruses. 129 However, they are extremely prothrombotic and induce intravascular coagulation. Furthermore, C3 can also be activated by this thrombin and eventually continue the complement cascade, which plays a major role in inflammation. 130 Zuo and colleagues have investigated the NET markers expression level such as myeloperoxidase‐DNA complexes, and citrullinated histone H3 in the COVID‐19 patients and compared it with healthy controls. Their results showed that there are higher levels of these markers in the COVID‐19 patients. 131
The effects of COVID‐19 on platelet activation are comprehensively investigated by Canzano and colleagues. They found that the COVID‐19 patients represent higher levels of tissue factor (TF) positive platelets than healthy individuals and patients with coronary arthritis disease. Also, they found more up‐regulation of P‐selectin and formation of platelet–leukocyte aggregate in these patients. Interestingly, they have observed activation of platelets in healthy individuals' blood after mixture with the plasma of the COVID‐19 patients. 132 , 133
6.3. Complement activation and coagulopathy in COVID‐19
Innate immunity concidered as the first line of the body's defense against infectious agents. The complement system is a member of innate immune system and is comprised of a course of steps called complement cascade that trigger inflammation against infections and some other events. 134 The complement can be activated by classic, alternative and lectin pathways. Initiation of all of the mentioned pathways leads to the cleavage of a protein named C3. After cleavage, the protein will be divided into two proteins named C3a, which is a proinflammatory protein, and C3b, which opsonizes the pathogens and also continue the next steps. 135 C3b mediates the C5 cleavage and release C5a (anaphylatoxin) and, C5b, which is responsible for the formation of a membrane attack complex (C5b‐9). 136 Albeit the complement plays a major role in the protection of the body, its overreaction can inflict heavy damage to different organs. 136 , 137
Besides acting as an anaphylatoxin, C5a increases the tissue factor activity, 138 , 139 and plays important role in coagulation. 140 Furthermore, two proteins that start the lectin pathway, namely MASP1, and MASP2, can activate thrombin by prothrombin cleavage 141 and also activate fibrinogen and factor XIII. 142 , 143 Different studies showed that inhibition of complement cascade resulted in consequences of anticoagulation effects such as prolonged bleeding. 140 , 144 , 145 , 146
Most of our knowledge about the role of complements in coronavirus infection was obtained from studies on SARS‐CoV‐1 and MERS. 137 Gralinski and colleagues showed less severe symptoms in C3 deficient mice than intact mice, who were infected with SARS‐CoV‐1. 147 Jiang and colleagues observed elevated levels of C5a and higher expression of C5a receptor (C5aR) in leukocytes and pneumocytes of MERS‐infected mice. Also, blockage of C5a–C5aR axis lightened the tissue damage in those mice. 148 In the SARS‐CoV‐2, Magro and colleagues reported deposition of complement fragments including MASP‐2, C5b‐9 and C4d microvasculature of lung tissue of patients with severe symptoms. 149 According to Gao and colleagues, the N protein on the surface of coronaviruses binds the MASP2 and triggers the complement cascade. 150 Lam and colleagues used flow cytometry to survey the formation of bonds between red blood cells and some products during complement activation such as C3b, iC3b, C3dg and C4d in hospitalized patients of COVID‐19 compared with healthy individuals and they found a considerable increase in the COVID‐19 patients. 151 Cugno and colleagues monitored the levels of C5b‐9 and C5a and also VWF in hospitalized the COVID‐19 patients. They observed high levels of these factors in the patients. Moreover, they saw that their concentration decreased during the remission of these patients. 152 Altogether, this results illustrate the pivotal role of the complement in tissue damage as well as the development of coagulopathies and underlines the importance of preventive measures to control overreaction of this wing of the innate immunity.
6.4. Coagulopathy‐induced molecular changes in gene expression
As discussed above, coagulation and fibrinolysis cascade changes cause thrombosis in the COVID‐19 patients that finally leads to poor outcomes or even death. Changes in serum level of coagulation or fibrinolysis cascade in COVID‐19 are known today, so there is an urgent need for evaluating changes in transcriptomic level for better treatment and disease evaluation.
Jha et al. assessed transcriptional profile in lung epithelial cells that infected with different coronaviruses include SARS‐CoV‐2, MERS‐CoV or SARS‐CoV. They showed that changes in transcriptional levels of COVID‐19 infected lung epithelial cells were much different from those of other viruses. Increases F3 gene, which codes tissue factor, and decreases in the TFPI2 gene, which codes TFPI, have been shown in this article. 153 Jain et al. have investigated nasopharyngeal swaps of the COVID‐19 patients for transcriptomic changes. They found coagulation cascade dysregulated and increased anti‐Fibrinolysis genes, especially SERPINE1 and SERPINF2, which codes PAI‐1 and alpha2AP, respectively. 154 Mast et al. examined transcriptional profile BALF samples of the COVID‐19 patients. They determined reduction in anti‐coagulant like thrombomodulin and fibrinolysis system like urokinase and its receptor. They found increases in TFPI and no tissue factor increases, so they suggested that other pathways, except FVIIa/TF, can result in thrombosis related to COVID‐19. 155 Fitzgerald et al. examined circulating immune cells, primary respiratory epithelial cells, patient‐derived bronchial alveolar lavage cells of the COVID‐19 patients. They have found dysregulated coagulation cascade and suppressed plasminogen activation system in, in vitro infected primary respiratory epithelial cells, patients derived bronchial alveolar lavage cells. On the other hand, those changes have not been seen in circulating immune cells. Moreover influenza A infected normal human bronchial epithelial cells infected did not show the same changes with SARS‐CoV‐2. 156 Gill et al. conducted a study on the leucocyte transcriptional profile between COVID‐19‐associated patients and other ICU‐admitted patients. They showed an increase in expression of VWF, SERPINE1 and GZMB genes in the COVID‐19 positive patients. GZMB, which codes Granzyme B can be involved in thrombosis through damage to endothelial cells. 157 Manne et al. have performed a study on severe COVID‐19 with hemostatic abnormalities. They have observed an increase in expression level of P‐selectin in COVID‐19. They have also seen an elevation in MAPK pathway and thromboxane activation, leads to platelet hyperactivity related to SARS‐CoV‐2 hypercoagulation. 158
6.5. Renin‐angiotensin‐aldosterone system
Renin‐Angiotensin‐Aldosterone System (RAAS) is a part of the hormone system that spreads throughout of human body. In this system, the angiotensinogen is converted to Ang I through the enzymatic activity of Renin. Then, Ang I is turned to Ang II by angiotensin converting Enzyme (ACE I). Ang II is a stimulator of inflammation and coagulation and its role has been well‐known in cardiovascular disease. ACE II(angiotensin converting Enzyme II) converts Ang II to Ang (1–7), an anti‐inflammatory and anti‐coagulation protein to maintain balance. 159
Ang II binds to two different receptors named AT1R (angiotensin II type 1 receptor) and AT2R (angiotensin II type 2 receptor). Ang II affinity for AT1R is more than AT2R, and binding this protein to AT1R causes its inflammation and coagulation. Through binding to its receptor, Ang II increases TF and PAI‐1 and improves the chance of shaping thromboses. 160 So, using RAAS inhibitors, especially angiotensin receptor blockers (ARBs) and ACEIs (angiotensin‐converting enzyme inhibitors), have been discussed in many pathophysiologic situations like COVID‐19. 159
Kutz et al. have researched RAAS elements in the COVID‐19 patients and showed a decrease in RASS, especially in Ang (1–7), as a protective element. 161 Because overwhelming inflammatory and hypercoagulation in COVID‐19 using RAAS inhibitors are recommended, there have been some debates about using these drugs, however. Animal studies have shown that these drugs increase ACE II, SARS‐COV‐2 receptor, in the patents, and as already we know, the virus can use it as an entrance to host cells. 162 , 163 , 164 So, many arguments have arisen about continuing or discontinuing RAAS inhibitors after publishing a research letter in the lancet by Fang et al. that mentioned adverse consequences of usage of RAAS inhibitors in the COVID‐19 patients with comorbidities. 165 Most of the articles have mentioned that using these drugs are beneficial for the COVID‐19 patients, or at least they are neutral. For example, Safizadeh et al. have shown that using RAAS inhibitors in pre‐existing hypertensive the COVID‐19 patients are protective against mortality and hospitalization. 166 Dublin et al. have shown that, these drugs did not increased risk of mortality and hospitalization. 167 Loader et al. have stated that the early stages of RAAS inhibitors will not increase the risk of severe outcomes in the COVID‐19 patients, 168 and research that have been conducted by Park et al. in South Korea showed that taking RAAS inhibitors for the COVID‐19 patients are not harmful. 169 In addition, some systematic reviews and meta‐analyses have been done, and they have not shown an increased risk of mortality and hospitalization in using RAAS inhibitors. 170 , 171 , 172 , 173
7. CONCLUSION
COVID‐19 research implementation highlights the importance of coagulopathy and thromboembolic events in confirmed coronavirus cases, especially those associated with severe disease and hospitalization. The current study tried to provide a comprehensive view of the pathophysiology, mechanisms, therapeutic approaches and considerations about the coagulopathy during COVID‐19. This recent growing body of knowledge about coagulopathy in COVID‐19 critically needs further studies and could be a lead for coagulopathy disorders in other infectious diseases. High incidence of thrombosis or DVT, PE, during COVID‐19, emphasizes the need to screen coagulation profiles to manage thromboembolic events and optimize the prophylaxis programs for the COVID‐19 hospitalized patients to be required. In addition, we must emphasize the mechanism by which COVID‐19 caused coagulopathy and thromboembolic events, since the elucidation of the involved mechanism in these complications may represent some novel therapeutic avenue for tackling COVID‐19. The underlining mechanisms for coagulopathy in COVID‐19 include complement activation, platelets activation, endothelial cells dysfunction, NETs and RAAS derangement could lead to future studies and possible therapeutic options. It needs to be concidered that, all the mentioned mechanisms needs further investigations for a clear conclusion and possibility to considered as clinical therapeutic option.
AUTHOR CONTRIBUTIONS
PY, SS, GS, SAR and AF: design and concept of manuscript, AG, AZ, MHR, EA, GMI, BA, SK and AT: data collection and manuscript preparation, SS, PY, AT and AF: manuscript editing and manuscript review, all included authors read and approved the final manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest, financial or otherwise.
Yousefi P, Soltani S, Siri G, et al. Coagulopathy and thromboembolic events a pathogenic mechanism of COVID‐19 associated with mortality: An updated review. J Clin Lab Anal. 2023;37:e24941. doi: 10.1002/jcla.24941
Parastoo Yousefi and Saber Soltani are co‐first for this work.
Contributor Information
Alireza Tabibzadeh, Email: alireza.tabibzadeh@outlook.com.
Abbas Farahani, Email: abbasfarahani25@yahoo.com.
DATA AVAILABILITY STATEMENT
The authors confirm that the data supporting the findings of this study is available within the article.
REFERENCES
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565‐574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Giannis D, Ziogas IA, Gianni P. Coagulation disorders in coronavirus infected patients: COVID‐19, SARS‐CoV‐1, MERS‐CoV and lessons from the past. J Clin Virol. 2020;127:104362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Karampoor S, Zahednasab H, Farahmand M, et al. A possible pathogenic role of Syndecan‐1 in the pathogenesis of coronavirus disease 2019 (COVID‐19). Int Immunopharmacol. 2021;97:107684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019 [published January 24, 2020]. N Engl J Med. 2020;382:727‐733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mirzaei R, Attar A, Papizadeh S, et al. The emerging role of probiotics as a mitigation strategy against coronavirus disease 2019 (COVID‐19). Arch Virol. 2021;166:1‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mirzaei R, Mahdavi F, Badrzadeh F, et al. The emerging role of microRNAs in the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection. Int Immunopharmacol. 2021;90:107204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mirzaei R, Goodarzi P, Asadi M, et al. Bacterial co‐infections with SARS‐CoV‐2. IUBMB Life. 2020;72(10):2097‐2111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Marietta M, Ageno W, Artoni A, et al. COVID‐19 and haemostasis: a position paper from Italian society on thrombosis and Haemostasis (SISET). Blood Transfus. 2020;18(3):167‐169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID‐19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239‐1242. [DOI] [PubMed] [Google Scholar]
- 11. Mirzaei R, Mohammadzadeh R, Mahdavi F, et al. Overview of the current promising approaches for the development of an effective severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) vaccine. Int Immunopharmacol. 2020;88:106928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Goodarzi P, Mahdavi F, Mirzaei R, et al. Coronavirus disease 2019 (COVID‐19): immunological approaches and emerging pharmacologic treatments. Int Immunopharmacol. 2020;88:106885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cui J, Li F, Shi Z‐L. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol. 2019;17(3):181‐192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zhong N, Zheng B, Li Y, et al. Epidemiology and cause of severe acute respiratory syndrome (SARS) in Guangdong, People's Republic of China, in February, 2003. Lancet. 2003;362(9393):1353‐1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Drosten C, Günther S, Preiser W, et al. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med. 2003;348(20):1967‐1976. [DOI] [PubMed] [Google Scholar]
- 16. Rudrapal M, Celik I, Chinnam S, et al. Phytocompounds as potential inhibitors of SARS‐CoV‐2 Mpro and PLpro through computational studies. Saudi J Biol Sci. 2022;29(5):3456‐3465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rudrapal M, Issahaku AR, Agoni C, et al. In silico screening of phytopolyphenolics for the identification of bioactive compounds as novel protease inhibitors effective against SARS‐CoV‐2. J Biomol Struct Dyn. 2022;40(20):10437‐10453. [DOI] [PubMed] [Google Scholar]
- 18. Cao Z, Gao W, Bao H, et al. VV116 versus nirmatrelvir–ritonavir for oral treatment of covid‐19. N Engl J Med. 2023;388(5):406‐417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Senefeld JW, Franchini M, Mengoli C, et al. COVID‐19 convalescent plasma for the treatment of immunocompromised patients: a systematic review and meta‐analysis. JAMA Netw Open. 2023;6(1):e2250647‐e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pourkarim F, Pourtaghi‐Anvarian S, Rezaee H. Molnupiravir: a new candidate for COVID‐19 treatment. Pharmacol Res Perspect. 2022;10(1):e00909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Grainger R, Kim AH, Conway R, Yazdany J, Robinson PC. COVID‐19 in people with rheumatic diseases: risks, outcomes, treatment considerations. Nat Rev Rheumatol. 2022;18(4):191‐204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rudrapal M, Sowmya MPK. Design, synthesis, drug‐likeness studies and bio‐evaluation of some new chalconeimines. Pharm Chem J. 2019;53(9):814‐821. [Google Scholar]
- 23. Guan W‐j, Ni Z‐y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708‐1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rotzinger D, Beigelman‐Aubry C, von Garnier C, Qanadli S. Pulmonary embolism in patients with COVID‐19: time to change the paradigm of computed tomography. Thromb Res. 2020;190:58‐59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rudrapal M, Khairnar SJ, Borse LB, Jadhav AG. Coronavirus disease‐2019 (COVID‐19): an updated review. Drug Res (Stuttg). 2020;70(9):389‐400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Klok F, Kruip M, Van der Meer N, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID‐19. Thromb Res. 2020;191:145‐147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Oxley TJ, Mocco J, Majidi S, et al. Large‐vessel stroke as a presenting feature of covid‐19 in the young. N Engl J Med. 2020;382(20):e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Toshiaki I, Jerrold HL, Marcel L, Jecko T. Coagulopathy in COVID‐19. J Thromb Haemost. 2020;18:2103‐2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Teimury A, Khameneh MT, Khaledi EM. Major coagulation disorders and parameters in COVID‐19 patients. Eur J Med Res. 2022;27(1):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Len P, Iskakova G, Sautbayeva Z, et al. Meta‐analysis and systematic review of coagulation disbalances in COVID‐19: 41 studies and 17,601 patients. Front Cardiovasc Med. 2022;9:794092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Di Gennaro L, Valentini P, Sorrentino S, et al. Extended coagulation profile of children with long Covid: a prospective study. Sci Rep. 2022;12(1):18392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bellosta R, Luzzani L, Natalini G, et al. Acute limb ischemia in patients with COVID‐19 pneumonia. J Vasc Surg. 2020;72:1864‐1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Panigada M, Bottino N, Tagliabue P, et al. Hypercoagulability of COVID‐19 patients in intensive care unit. A report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020;18:1738‐1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ranucci M, Ballotta A, Di Dedda U, et al. The procoagulant pattern of patients with COVID‐19 acute respiratory distress syndrome. J Thromb Haemost. 2020;18:1747‐1751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Doevelaar AA, Bachmann M, Hoelzer B, et al. COVID‐19 is associated with relative ADAMTS13 deficiency and VWF multimer formation resembling TTP. medRxiv . 2020.
- 36. Moein ST, Hashemian SM, Mansourafshar B, Khorram‐Tousi A, Tabarsi P, Doty RL. Smell dysfunction: a biomarker for COVID‐19. Int Forum Allergy Rhinol. 2020;10:944‐950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Han H, Yang L, Liu R, et al. Prominent changes in blood coagulation of patients with SARS‐CoV‐2 infection. Clin Chem Lab Med. 2020;58:1. [DOI] [PubMed] [Google Scholar]
- 38. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844‐847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lippi G, Mullier F, Favaloro EJ. D‐dimer: old dogmas, new (COVID‐19) tricks. Clin Chem Lab Med. 2022;61:841‐850. [DOI] [PubMed] [Google Scholar]
- 40. Sarzi‐Puttini P, Giorgi V, Sirotti S, et al. COVID‐19, cytokines and immunosuppression: what can we learn from severe acute respiratory syndrome? Clin Exp Rheumatol. 2020;38(2):337‐342. [PubMed] [Google Scholar]
- 41. Charles J, Ploplis VA. COVID‐19 induces cytokine storm and dysfunctional hemostasis. Curr Drug Targets. 2022;23(17):1603‐1610. [DOI] [PubMed] [Google Scholar]
- 42. Jackson SP, Darbousset R, Schoenwaelder SM. Thromboinflammation: challenges of therapeutically targeting coagulation and other host defense mechanisms. Blood. 2019;133(9):906‐918. [DOI] [PubMed] [Google Scholar]
- 43. Iba T, Levy J. Inflammation and thrombosis: roles of neutrophils, platelets and endothelial cells and their interactions in thrombus formation during sepsis. J Thromb Haemost. 2018;16(2):231‐241. [DOI] [PubMed] [Google Scholar]
- 44. Claushuis T, De Stoppelaar S, Stroo I, et al. Thrombin contributes to protective immunity in pneumonia‐derived sepsis via fibrin polymerization and platelet–neutrophil interactions. J Thromb Haemost. 2017;15(4):744‐757. [DOI] [PubMed] [Google Scholar]
- 45. De Stoppelaar S. Platelets: versatile effector cells in pneumonia and sepsis. Thromb Haemost. 2014;112(2):666‐677. [DOI] [PubMed] [Google Scholar]
- 46. Li X, Ma X. The role of heparin in sepsis: much more than just an anticoagulant. Br J Haematol. 2017;179(3):389‐398. [DOI] [PubMed] [Google Scholar]
- 47. Liu X, Li Z, Liu S, et al. Therapeutic effects of dipyridamole on COVID‐19 patients with coagulation dysfunction. medRxiv . 2020.
- 48. Zhai Z, Li C, Chen Y, et al. Prevention and treatment of venous thromboembolism associated with coronavirus disease 2019 infection: a consensus statement before guidelines. Thromb Haemost. 2020;120(6):937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18(5):1094‐1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Helms J, Tacquard C, Severac F, et al. High risk of thrombosis in patients with severe SARS‐CoV‐2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46:1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID‐19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420‐422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Nougier C, Benoit R, Simon M, et al. Hypofibrinolytic state and high thrombin generation may play a major role in sars‐cov2 associated thrombosis. J Thromb Haemost. 2020;18(9):2215‐2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Mukherjee S. Toll‐like receptor 4 in COVID‐19: friend or foe?. Future Virol. 2022;17(7):415‐417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Jiang S, Ma J, Ye S, et al. Associations among disseminated intravascular coagulation, thrombocytopenia cytokines/chemokines and genetic polymorphisms of toll‐like receptor 2/4 in Chinese patients with sepsis. J Inflamm Res. 2022;15:1‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Biswas I, Khan GA. Coagulation disorders in COVID‐19: role of toll‐like receptors. J Inflamm Res. 2020;13:823‐828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Van Gorp E, Suharti C, Ten Cate H, et al. Infectious diseases and coagulation disorders. J Infect Dis. 1999;180(1):176‐186. [DOI] [PubMed] [Google Scholar]
- 57. Key NS, Vercellotti GM, Winkelmann JC, et al. Infection of vascular endothelial cells with herpes simplex virus enhances tissue factor activity and reduces thrombomodulin expression. Proc Natl Acad Sci USA. 1990;87(18):7095‐7099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Rondina MT, Guo L. The era of thromboinflammation: platelets are dynamic sensors and effector cells during infectious diseases. Front Immunol. 2019;10:2204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Goshua G, Pine AB, Meizlish ML, et al. Endotheliopathy in COVID‐19‐associated coagulopathy: evidence from a single‐Centre, cross‐sectional study. Lancet Haematol. 2020;7(8):e575‐e582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Rostami M, Mansouritorghabeh H, Parsa‐Kondelaji M. High levels of Von Willebrand factor markers in COVID‐19: a systematic review and meta‐analysis. Clin Exp Med. 2022;22(3):347‐357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Larsen CP, Bourne TD, Wilson JD, Saqqa O, Sharshir MA. Collapsing glomerulopathy in a patient with COVID‐19. Kidney Int Rep. 2020;5(6):935‐939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Escher R, Breakey N, Lämmle B. ADAMTS13 activity, von Willebrand factor, factor VIII and D‐dimers in COVID‐19 inpatients. Thromb Res. 2020;192:174‐175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Huisman A, Beun R, Sikma M, Westerink J, Kusadasi N. Involvement of ADAMTS13 and von Willebrand factor in thromboembolic events in patients infected with SARS‐CoV‐2. Int J Lab Hematol. 2020;42:e211‐e212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Seth R, McKinnon TA, Zhang XF. Contribution of the von Willebrand factor/ADAMTS13 imbalance to COVID‐19 coagulopathy. Am J Physiol Heart Circ Physiol. 2022;322(1):H87‐H93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Shi S, Qin M, Shen B, et al. Cardiac injury in patients with corona virus disease 2019. JAMA Cardiol. 2020;5(7):802‐810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Umapathi T, Kor AC, Venketasubramanian N, et al. Large artery ischaemic stroke in severe acute respiratory syndrome (SARS). J Neurol. 2004;251(10):1227‐1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Wong RS, Wu A, To K, et al. Haematological manifestations in patients with severe acute respiratory syndrome: retrospective analysis. BMJ. 2003;326(7403):1358‐1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Ding Y, Wang H, Shen H, et al. The clinical pathology of severe acute respiratory syndrome (SARS): a report from China. J Pathol. 2003;200(3):282‐289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Al‐Abdallat MM, Payne DC, Alqasrawi S, et al. Hospital‐associated outbreak of Middle East respiratory syndrome coronavirus: a serologic, epidemiologic, and clinical description. Clin Infect Dis. 2014;59(9):1225‐1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Marchandot B, Sattler L, Jesel L, et al. COVID‐19 related coagulopathy: a distinct entity? J Clin Med. 2020;9(6):1651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Marone EM, Bonalumi G, Curci R, et al. Characteristics of venous thromboembolism in COVID‐19 patients: a multicenter experience from northern Italy. Ann Vasc Surg. 2020;68:83‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. 2020;18:1421‐1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Anderson FA Jr, Zayaruzny M, Heit JA, Fidan D, Cohen AT. Estimated annual numbers of US acute‐care hospital patients at risk for venous thromboembolism. Am J Hematol. 2007;82(9):777‐782. [DOI] [PubMed] [Google Scholar]
- 74. Lau BD, Haut ER. Practices to prevent venous thromboembolism: a brief review. BMJ Qual Saf. 2014;23(3):187‐195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Porfidia A, Valeriani E, Pola R, Porreca E, Rutjes AWS, Di Nisio M. Venous thromboembolism in patients with COVID‐19: systematic review and meta‐analysis. Thromb Res. 2020;196:67‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Rieder M, Goller I, Jeserich M, et al. Rate of venous thromboembolism in a prospective all‐comers cohort with COVID‐19. J Thromb Thrombolysis. 2020;50(3):558‐566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Mei F, Fan J, Yuan J, et al. Comparison of venous thromboembolism risks between COVID‐19 pneumonia and community‐acquired pneumonia patients. Arterioscler Thromb Vasc Biol. 2020;40(9):2332‐2337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Nahum J, Morichau‐Beauchant T, Daviaud F, et al. Venous thrombosis among critically ill patients with coronavirus disease 2019 (COVID‐19). JAMA Netw Open. 2020;3(5):e2010478‐e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Giorgi‐Pierfranceschi M, Paoletti O, Pan A, et al. Prevalence of asymptomatic deep vein thrombosis in patients hospitalized with SARS‐CoV‐2 pneumonia: a cross‐sectional study. Intern Emerg Med. 2020;15:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Alonso‐Fernández A, Toledo‐Pons N, Cosío BG, et al. Prevalence of pulmonary embolism in patients with COVID‐19 pneumonia and high D‐dimer values: a prospective study. PLoS One. 2020;15(8):e0238216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Garcia‐Olivé I, Sintes H, Radua J, Capa JA, Rosell A. D‐dimer in patients infected with COVID‐19 and suspected pulmonary embolism. Respir Med. 2020;169:106023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Rodriguez‐Sevilla J, Rodó‐Pin A, Espallargas I, et al. Pulmonary embolism in patients with Covid‐19 pneumonia: the utility of D‐dimer. Arch Bronconeumol. 2020;56:758‐759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Leonard‐Lorant I, Delabranche X, Severac F, et al. Acute pulmonary embolism in COVID‐19 patients on CT angiography and relationship to D‐dimer levels. Radiology. 2020;296:E189‐E191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Stefely JA, Christensen BB, Gogakos T, et al. Marked factor V activity elevation in severe COVID‐19 is associated with venous thromboembolism. Am J Hematol. 2020;95:1522‐1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Mowla A, Shakibajahromi B, Shahjouei S, et al. Cerebral venous sinus thrombosis associated with SARS‐CoV‐2; a multinational case series. J Neurol Sci. 2020;419:117183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Cavalcanti DD, Raz E, Shapiro M, et al. Cerebral venous thrombosis associated with COVID‐19. Am J Neuroradiol. 2020;41(8):1370‐1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Jenner WJ, Kanji R, Mirsadraee S, et al. Thrombotic complications in 2928 patients with COVID‐19 treated in intensive care: a systematic review. J Thromb Thrombolysis. 2021;51:1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Chandra A, Chakraborty U, Ghosh S, Dasgupta S. Anticoagulation in COVID‐19: current concepts and controversies. Postgrad Med J. 2022;98(1159):395‐402. [DOI] [PubMed] [Google Scholar]
- 89. Pilia E, Belletti A, Fresilli S, Finco G, Landoni G. Efficacy and safety of heparin full‐dose anticoagulation in hospitalized non‐critically ill COVID‐19 patients: a meta‐analysis of multicenter randomized controlled trials. J Thromb Thrombolysis. 2022;54(3):420‐430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Cuker A, Tseng EK, Nieuwlaat R, et al. American Society of Hematology living guidelines on the use of anticoagulation for thromboprophylaxis in patients with COVID‐19: January 2022 update on the use of therapeutic‐intensity anticoagulation in acutely ill patients. Blood Adv. 2022;6(17):4915‐4923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Lang J, Yang N, Deng J, et al. Inhibition of SARS pseudovirus cell entry by lactoferrin binding to heparan sulfate proteoglycans. PLoS One. 2011;6(8):e23710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Vicenzi E, Canducci F, Pinna D, et al. Coronaviridae and SARS‐associated coronavirus strain HSR1. Emerg Infect Dis. 2004;10(3):413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Shukla D, Spear PG. Herpesviruses and heparan sulfate: an intimate relationship in aid of viral entry. J Clin Invest. 2001;108(4):503‐510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Ghezzi S, Cooper L, Rubio A, et al. Heparin prevents Zika virus induced‐cytopathic effects in human neural progenitor cells. Antiviral Res. 2017;140:13‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Thachil J. The versatile heparin in COVID‐19. J Thromb Haemost. 2020;18(5):1020‐1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Mycroft‐West C, Su D, Pagani I, et al. Heparin inhibits cellular invasion by SARS‐CoV‐2: structural dependence of the interaction of the surface protein (spike) S1 receptor binding domain with heparin. bioRxiv . 2020. [DOI] [PMC free article] [PubMed]
- 97. Kim SY, Jin W, Sood A, et al. Characterization of heparin and severe acute respiratory syndrome‐related coronavirus 2 (SARS‐CoV‐2) spike glycoprotein binding interactions. Antiviral Res. 2020;181:104873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Tandon R, Sharp JS, Zhang F, et al. Effective inhibition of SARS‐CoV‐2 entry by heparin and enoxaparin derivatives. bioRxiv . 2020. [DOI] [PMC free article] [PubMed]
- 99. Conzelmann C, Müller JA, Perkhofer L, et al. Inhaled and systemic heparin as a repurposed direct antiviral drug for prevention and treatment of COVID‐19. Clin Med. 2020;20:e218‐e221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Lever R, Page CP. Non‐Anticoagulant Effects of Heparin: an Overview. Heparin‐A Century of Progress. Springer; 2012:281‐305. [DOI] [PubMed] [Google Scholar]
- 101. Young E. The anti‐inflammatory effects of heparin and related compounds. Thromb Res. 2008;122(6):743‐752. [DOI] [PubMed] [Google Scholar]
- 102. Paar V, Wernly B, Zhou Z, et al. Anti‐coagulation for COVID‐19 treatment: both anti‐thrombotic and anti‐inflammatory? J Thromb Thrombolysis. 2021;51(1):226‐231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Huang C‐T, Hsu S‐Y, Chang K‐W, Huang C‐G, Yang C‐T, Cheng M‐H. Heparin‐induced thrombocytopenia and thrombosis in a patient with Covid‐19. Thromb Res. 2020;196:11‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Beun R, Kusadasi N, Sikma M, Westerink J, Huisman A. Thromboembolic events and apparent heparin resistance in patients infected with SARS‐CoV‐2. Int J Lab Hematol. 2020;42:19‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. White D, MacDonald S, Bull T, et al. Heparin resistance in COVID‐19 patients in the intensive care unit. J Thromb Thrombolysis. 2020;1:287‐291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Reis S, Popp M, Schießer S, et al. Anticoagulation in COVID‐19 patients–an updated systematic review and meta‐analysis. Thromb Res. 2022;219:40‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Spyropoulos AC, Connors JM, Douketis JD, et al. Good practice statements for antithrombotic therapy in the management of COVID‐19: guidance from the SSC of the ISTH. J Thromb Haemost. 2022;20(10):2226‐2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Zhang J, Zhang J, Tao Z. Effect of hypertension comorbidity on clinical characteristics of COVID‐19 patients infected by the wild‐type, the Delta or omicron variant SARS‐CoV‐2. Rev Cardiovasc Med. 2022;23(12):395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Gerber G, Pan X‐Z, Ranjan N, Warmack A, Brodsky R. Pathogenicity of Sars‐Cov‐2 spike protein variants correlates with coagulation and complement assays. Blood. 2022;140:2705. [Google Scholar]
- 110. Grobbelaar LM, Kruger A, Venter C, et al. Relative hypercoagulopathy of the SARS‐CoV‐2 beta and delta variants when compared to the less severe omicron variants is related to TEG parameters, the extent of fibrin amyloid microclots, and the severity of clinical illness. Semin Thromb Hemost. 2022;48:858‐868. [DOI] [PubMed] [Google Scholar]
- 111. Matsuoka A, Koami H, Shinada K, Sakamoto Y. Investigation of differences in coagulation characteristics between hospitalized patients with SARS‐CoV‐2 alpha, Delta, and omicron variant infection using rotational thromboelastometry (ROTEM): a single‐center, retrospective, observational study. J Clin Lab Anal. 2022;36:e24796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Rajendran P, Rengarajan T, Thangavel J, et al. The vascular endothelium and human diseases. Int J Biol Sci. 2013;9(10):1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Michiels C. Endothelial cell functions. J Cell Physiol. 2003;196(3):430‐443. [DOI] [PubMed] [Google Scholar]
- 114. Yang YH, Huang YH, Chuang YH, et al. Autoantibodies against human epithelial cells and endothelial cells after severe acute respiratory syndrome (SARS)‐associated coronavirus infection. J Med Virol. 2005;77(1):1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Levi M, van der Poll T. Coagulation and sepsis. Thromb Res. 2017;149:38‐44. [DOI] [PubMed] [Google Scholar]
- 116. Liu L, Jing H, Wu X, et al. The cross‐talk of lung and heart complications in COVID‐19: endothelial cells dysfunction, thrombosis, and treatment. Front Cardiovasc Med. 2022;9:957006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Xu S‐w, Ilyas I, Weng J‐p. Endothelial dysfunction in COVID‐19: an overview of evidence, biomarkers, mechanisms and potential therapies. Acta Pharmacol Sin. 2022;44:1‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Martinelli N, Montagnana M, Pizzolo F, et al. A relative ADAMTS13 deficiency supports the presence of a secondary microangiopathy in COVID 19. Thromb Res. 2020;193:170‐172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Bonaventura A, Vecchié A, Dagna L, et al. Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID‐19. Nat Rev Immunol. 2021;21(5):319‐329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Yue Y, Nabar NR, Shi C‐S, et al. SARS‐coronavirus open Reading frame‐3a drives multimodal necrotic cell death. Cell Death Dis. 2018;9(9):1‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Jia C, Zhang J, Chen H, et al. Endothelial cell pyroptosis plays an important role in Kawasaki disease via HMGB1/RAGE/cathespin B signaling pathway and NLRP3 inflammasome activation. Cell Death Dis. 2019;10(10):1‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Paniri A, Akhavan‐Niaki H. Emerging role of IL‐6 and NLRP3 inflammasome as potential therapeutic targets to combat COVID‐19: role of lncRNAs in cytokine storm modulation. Life Sci. 2020;257:118114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Guervilly C, Burtey S, Sabatier F, et al. Circulating endothelial cells as a marker of endothelial injury in severe COVID‐19. J Infect Dis. 2020;222(11):1789‐1793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Falcinelli E, Petito E, Becattini C, et al. Role of endothelial dysfunction in the thrombotic complications of COVID‐19 patients. J Infect. 2021;82(5):186‐230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Koupenova M. Potential role of platelets in COVID‐19: implications for thrombosis. Res Pract Thromb Haemost. 2020;4(5):737‐740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Koupenova M, Corkrey HA, Vitseva O, et al. The role of platelets in mediating a response to human influenza infection. Nat Commun. 2019;10(1):1‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Koupenova M, Vitseva O, MacKay CR, et al. Platelet‐TLR7 mediates host survival and platelet count during viral infection in the absence of platelet‐dependent thrombosis. Blood. 2014;124(5):791‐802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Zaid Y, Puhm F, Allaeys I, et al. Platelets can associate with SARS‐Cov‐2 RNA and are hyperactivated in COVID‐19. Circ Res. 2020;127(11):1404‐1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Papayannopoulos V. Neutrophil extracellular traps in immunity and disease. Nat Rev Immunol. 2018;18(2):134‐147. [DOI] [PubMed] [Google Scholar]
- 130. Amara U, Rittirsch D, Flierl M, et al. Interaction between the coagulation and complement system. Adv Exp Med Biol. 2008;632:671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Zuo Y, Yalavarthi S, Shi H, et al. Neutrophil extracellular traps in COVID‐19. JCI Insight. 2020;5(11):e138999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Canzano P, Brambilla M, Porro B, et al. Platelet and endothelial activation as potential mechanisms behind the thrombotic complications of COVID‐19 patients. JACC Basic Transl Sci. 2021;6(3):202‐218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Iba T, Wada H, Levy JH. Platelet activation and thrombosis in COVID‐19. Semin Thromb Hemost. 2022;49:55‐61. [DOI] [PubMed] [Google Scholar]
- 134. Wang X, Sahu KK, Cerny J. Coagulopathy, endothelial dysfunction, thrombotic microangiopathy and complement activation: potential role of complement system inhibition in COVID‐19. J Thromb Thrombolysis. 2021;51(3):657‐662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Noris M, Benigni A, Remuzzi G. The case of complement activation in COVID‐19 multiorgan impact. Kidney Int. 2020;98(2):314‐322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Song W‐C, FitzGerald GA. COVID‐19, microangiopathy, hemostatic activation, and complement. J Clin Invest. 2020;130(8):3950‐3953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Perico L, Benigni A, Casiraghi F, Ng LFP, Renia L, Remuzzi G. Immunity, endothelial injury and complement‐induced coagulopathy in COVID‐19. Nat Rev Nephrol. 2021;17(1):46‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Ritis K, Doumas M, Mastellos D, et al. A novel C5a receptor‐tissue factor cross‐talk in neutrophils links innate immunity to coagulation pathways. J Immunol. 2006;177(7):4794‐4802. [DOI] [PubMed] [Google Scholar]
- 139. Ikeda K, Nagasawa K, Horiuchi T, Tsuru T, Nishizaka H, Niho Y. C5a induces tissue factor activity on endothelial cells. Thromb Haemost. 1997;77(2):394‐398. [PubMed] [Google Scholar]
- 140. Fletcher‐Sandersjöö A, Bellander B‐M. Is COVID‐19 associated thrombosis caused by overactivation of the complement cascade? A literature review. Thromb Res. 2020;194:36‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Krarup A, Wallis R, Presanis JS, Gál P, Sim RB. Simultaneous activation of complement and coagulation by MBL‐associated serine protease 2. PLoS One. 2007;2(7):e623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Hess K, Ajjan R, Phoenix F, Dobó J, Gál P, Schroeder V. Effects of MASP‐1 of the complement system on activation of coagulation factors and plasma clot formation. PLoS One. 2012;7(4):e35690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Dobó J, Schroeder V, Jenny L, Cervenak L, Závodszky P, Gál P. Multiple roles of complement MASP‐1 at the interface of innate immune response and coagulation. Mol Immunol. 2014;61(2):69‐78. [DOI] [PubMed] [Google Scholar]
- 144. Landsem A, Fure H, Christiansen D, et al. The key roles of complement and tissue factor in Escherichia coli‐induced coagulation in human whole blood. Clin Exp Immunol. 2015;182(1):81‐89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Dzik S. Complement and coagulation: cross talk through time. Transfus Med Rev. 2019;33(4):199‐206. [DOI] [PubMed] [Google Scholar]
- 146. Cugno M, Bos I, Lubbers Y, Hack CE, Agostoni A. In vitro interaction of C1‐inhibitor with thrombin. Blood Coagul Fibrinolysis. 2001;12(4):253‐260. [DOI] [PubMed] [Google Scholar]
- 147. Gralinski LE, Sheahan TP, Morrison TE, et al. Complement activation contributes to severe acute respiratory syndrome coronavirus pathogenesis. MBio. 2018;9(5):e01753‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Jiang Y, Zhao G, Song N, et al. Blockade of the C5a–C5aR axis alleviates lung damage in hDPP4‐transgenic mice infected with MERS‐CoV. Emerg Microbes Infect. 2018;7(1):1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Magro C, Mulvey JJ, Berlin D, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID‐19 infection: a report of five cases. Transl Res. 2020;220:1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Gao T, Hu M, Zhang X, et al. Highly pathogenic coronavirus N protein aggravates lung injury by MASP‐2‐mediated complement over‐activation. medRxiv . 2020.
- 151. Lam LM, Reilly JP, Rux AH, et al. Erythrocytes identify complement activation in patients with COVID‐19. Am J Physiol Lung Cell Mol Physiol. 2021;321(2):L485‐L489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Cugno M, Meroni PL, Gualtierotti R, et al. Complement activation and endothelial perturbation parallel COVID‐19 severity and activity. J Autoimmun. 2021;116:102560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Jha PK, Vijay A, Halu A, Uchida S, Aikawa M. Gene expression profiling reveals the shared and distinct transcriptional signatures in human lung epithelial cells infected with SARS‐CoV‐2, MERS‐CoV, or SARS‐CoV: potential implications in cardiovascular complications of COVID‐19. Front Cardiovasc Med. 2020;7:623012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Jain R, Ramaswamy S, Harilal D, et al. Host transcriptomic profiling of COVID‐19 patients with mild, moderate, and severe clinical outcomes. Comput Struct Biotechnol J. 2021;19:153‐160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Mast AE, Wolberg AS, Gailani D, et al. SARS‐CoV‐2 suppresses anticoagulant and fibrinolytic gene expression in the lung. Elife. 2021;10:e64330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. FitzGerald ES, Chen Y, Fitzgerald KA, Jamieson AM. Lung epithelial cell transcriptional regulation as a factor in COVID‐19–associated coagulopathies. Am J Respir Cell Mol Biol. 2021;64(6):687‐697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Gill SE, Dos Santos CC, O'Gorman DB, et al. Transcriptional profiling of leukocytes in critically ill COVID19 patients: implications for interferon response and coagulation. Intensive Care Med Exp. 2020;8(1):1‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Manne BK, Denorme F, Middleton EA, et al. Platelet gene expression and function in patients with COVID‐19. Blood. 2020;136(11):1317‐1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Henry BM, Vikse J, Benoit S, Favaloro EJ, Lippi G. Hyperinflammation and derangement of renin‐angiotensin‐aldosterone system in COVID‐19: a novel hypothesis for clinically suspected hypercoagulopathy and microvascular immunothrombosis. Clin Chim Acta. 2020;507:167‐173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Nakamura S, Nakamura I, Ma L, Vaughan DE, Fogo AB. Plasminogen activator inhibitor‐1 expression is regulated by the angiotensin type 1 receptor in vivo. Kidney Int. 2000;58(1):251‐259. [DOI] [PubMed] [Google Scholar]
- 161. Kutz A, Conen A, Gregoriano C, et al. Renin‐angiotensin‐aldosterone system peptide profiles in patients with COVID‐19. Eur J Endocrinol. 2021;184(4):543‐552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Albashir AAD. Renin‐angiotensin‐aldosterone system (RAAS) inhibitors and coronavirus disease 2019 (COVID‐19). South Med J. 2021;114(1):51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Ferrario CM, Jessup J, Chappell MC, et al. Effect of angiotensin‐converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin‐converting enzyme 2. Circulation. 2005;111(20):2605‐2610. [DOI] [PubMed] [Google Scholar]
- 164. Soler MJ, Ye M, Wysocki J, William J, Lloveras J, Batlle D. Localization of ACE2 in the renal vasculature: amplification by angiotensin II type 1 receptor blockade using telmisartan. Am J Physiol Renal Physiol. 2009;296(2):F398‐F405. [DOI] [PubMed] [Google Scholar]
- 165. Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID‐19 infection? Lancet Respir Med. 2020;8(4):e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Safizadeh F, Nguyen TNM, Brenner H, Schöttker B. Association of renin–angiotensin–aldosterone system blocker use with Covid‐19 hospitalization and all‐cause mortality in the UK biobank. Authorea Preprints. 2021. [DOI] [PubMed]
- 167. Dublin S, Walker RL, Floyd JS, et al. Renin–angiotensin–aldosterone system inhibitors and COVID‐19 infection or hospitalization: a cohort study. Am J Hypertens. 2021;34(4):339‐347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Loader J, Lampa E, Gustafsson S, Cars T, Sundström J. Renin‐angiotensin aldosterone system inhibitors in primary prevention and COVID‐19. J Am Heart Assoc. 2021;10(15):e021154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Park J, Lee S‐H, You SC, Kim J, Yang K. Effect of renin‐angiotensin‐aldosterone system inhibitors on Covid‐19 patients in Korea. PLoS One. 2021;16(3):e0248058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Baral R, Tsampasian V, Debski M, et al. Association between renin‐angiotensin‐aldosterone system inhibitors and clinical outcomes in patients with COVID‐19: a systematic review and meta‐analysis. JAMA Netw Open. 2021;4(3):e213594‐e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Kaur U, Chakrabarti SS, Patel TK. Renin–angiotensin–aldosterone system blockers and region‐specific variations in COVID‐19 outcomes: findings from a systematic review and meta‐analysis. Ther Adv Drug Saf. 2021;12:20420986211011345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Laurentius A, Mendel B, Prakoso R. Clinical outcome of renin‐angiotensin‐aldosterone system blockers in treatment of hypertensive patients with COVID‐19: a systematic review and meta‐analysis. Egypt Heart J. 2021;73(1):1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Naveed H, Elshafeey A, Al‐Ali D, et al. The interplay between the immune system, the renin‐angiotensin‐aldosterone system (RAAS), and RAAS inhibitors may modulate the outcome of COVID‐19: a systematic review. J Clin Pharmacol. 2021;61:987‐1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Demelo‐Rodríguez P, Cervilla‐Muñoz E, Ordieres‐Ortega L, et al. Incidence of asymptomatic deep vein thrombosis in patients with COVID‐19 pneumonia and elevated D‐dimer levels. Thromb Res. 2020;192:23‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Longchamp A, Longchamp J, Manzocchi‐Besson S, et al. Venous thromboembolism in critically ill patients with Covid‐19: results of a screening study for deep vein thrombosis. Res Pract Thromb Haemost. 2020;4:842‐847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Santoliquido A, Porfidia A, Nesci A, et al. Incidence of deep vein thrombosis among non‐ICU patients hospitalized for COVID‐19 despite pharmacological thromboprophylaxis. J Thromb Haemost. 2020;18(9):2358‐2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Ren B, Yan F, Deng Z, et al. Extremely high incidence of lower extremity deep venous thrombosis in 48 patients with severe COVID‐19 in Wuhan. Circulation. 2020;142:181‐183. [DOI] [PubMed] [Google Scholar]
- 178. Zhang L, Feng X, Zhang D, et al. Deep vein thrombosis in hospitalized patients with coronavirus disease 2019 (COVID‐19) in Wuhan, China: prevalence, risk factors, and outcome. Circulation. 2020;142:114‐128. [DOI] [PubMed] [Google Scholar]
- 179. Zhang P, Qu Y, Tu J, et al. Applicability of bedside ultrasonography for the diagnosis of deep venous thrombosis in patients with COVID‐19 and treatment with low molecular weight heparin. J Clin Ultrasound. 2020;48(9):522‐526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Chen S, Zhang D, Zheng T, Yu Y, Jiang J. DVT incidence and risk factors in critically ill patients with COVID‐19. J Thromb Thrombolysis. 2020;51:1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Cho ES, McClelland PH, Cheng O, et al. Utility of d‐dimer for diagnosis of deep vein thrombosis in coronavirus disease‐19 infection. J Vasc Surg Venous Lymphat Disord. 2020;9:47‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Ierardi AM, Coppola A, Fusco S, et al. Early detection of deep vein thrombosis in patients with coronavirus disease 2019: who to screen and who not to with Doppler ultrasound? J Ultrasound. 2021;24(2):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183. Koleilat I, Galen B, Choinski K, et al. Clinical characteristics of acute lower extremity deep venous thrombosis diagnosed by duplex in patients hospitalized for coronavirus disease 2019. J Vasc Surg Venous Lymphat Disord. 2020;9:36‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184. Pizzolo F, Rigoni AM, De Marchi S, et al. Deep vein thrombosis in SARS‐CoV‐2 pneumonia‐affected patients within standard care units: exploring a submerged portion of the iceberg. Thromb Res. 2020;194:216‐219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Le Jeune S, Suhl J, Benainous R, et al. High prevalence of early asymptomatic venous thromboembolism in anticoagulated COVID‐19 patients hospitalized in general wards. J Thromb Thrombolysis. 2020;51:1‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Trimaille A, Curtiaud A, Marchandot B, et al. Venous thromboembolism in non‐critically ill patients with COVID‐19 infection. Thromb Res. 2020;193:166‐169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Artifoni M, Danic G, Gautier G, et al. Systematic assessment of venous thromboembolism in COVID‐19 patients receiving thromboprophylaxis: incidence and role of D‐dimer as predictive factors. J Thromb Thrombolysis. 2020;1:211‐216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Middeldorp S, Coppens M, van Haaps TF, et al. Incidence of venous thromboembolism in hospitalized patients with COVID‐19. J Thromb Haemost. 2020;18:1995‐2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189. Chen J, Wang X, Zhang S, et al. Characteristics of acute pulmonary embolism in patients with COVID‐19 associated pneumonia from the city of Wuhan. Clin Appl Thromb Hemost. 2020;26:1076029620936772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Minuz P, Mansueto G, Mazzaferri F, et al. High rate of pulmonary thromboembolism in patients with SARS‐CoV‐2 pneumonia. Clin Microbiol Infect. 2020;26:1572‐1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Bompard F, Monnier H, Saab I, et al. Pulmonary embolism in patients with Covid‐19 pneumonia. Eur Respir J. 2020;56:2001365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192. De Cobelli F, Palumbo D, Ciceri F, et al. Pulmonary vascular thrombosis in COVID‐19 pneumonia. J Cardiothorac Vasc Anesth. 2021;35:3631‐3641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Al‐Samkari H, Gupta S, Leaf RK, et al. Thrombosis, bleeding, and the observational effect of early therapeutic anticoagulation on survival in critically ill patients with COVID‐19. Ann Intern Med. 2021;174(5):622‐632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Patell R, Bogue T, Koshy A, et al. Postdischarge thrombosis and hemorrhage in patients with COVID‐19. Blood. 2020;136(11):1342‐1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195. Voicu S, Bonnin P, Stépanian A, et al. High prevalence of deep vein thrombosis in mechanically ventilated COVID‐19 patients. J Am Coll Cardiol. 2020;76(4):480‐482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Santoro F, Nuñez‐Gil IJ, Vitale E, et al. Antiplatelet therapy and outcome in COVID‐19: the health outcome predictive evaluation registry. Heart. 2022;108(2):130‐136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Spiegelenberg JP, van Gelder MM, Maas ML, et al. Prior use of therapeutic anticoagulation does not protect against COVID‐19 related clinical outcomes in hospitalized patients: a propensity score‐matched cohort study. Br J Clin Pharmacol. 2021;87:4839‐4847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198. Tremblay D, van Gerwen M, Alsen M, et al. Impact of anticoagulation prior to COVID‐19 infection: a propensity score–matched cohort study. Blood. 2020;136(1):144‐147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Rivera‐Caravaca JM, Núñez‐Gil IJ, Vivas D, et al. Clinical profile and prognosis in patients on oral anticoagulation before admission for COVID‐19. Eur J Clin Invest. 2021;51(1):e13436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Lachant DJ, Lachant NA, Kouides P, Rappaport S, Prasad P, White RJ. Chronic therapeutic anticoagulation is associated with decreased thrombotic complications in SARS‐CoV‐2 infection. J Thromb Haemost. 2020;18(10):2640‐2645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201. Vlot E, Van den Dool E, Hackeng C, Sohne M, Noordzij P, Van Dongen E. Anti Xa activity after high dose LMWH thrombosis prophylaxis in covid 19 patients at the intensive care unit. Thromb Res. 2020;196:1‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Ayerbe L, Risco C, Ayis S. The association between treatment with heparin and survival in patients with Covid‐19. J Thromb Thrombolysis. 2020;50:1‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Brouns SH, Brüggemann R, Linkens AE, et al. Mortality and the use of antithrombotic therapies among nursing home residents with COVID‐19. J Am Geriatr Soc. 2020;68(8):1647‐1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Christie DB III, Nemec HM, Scott AM, et al. Early outcomes with utilization of tissue plasminogen activator in COVID‐19–associated respiratory distress: a series of five cases. J Trauma Acute Care Surg. 2020;89(3):448‐452. [DOI] [PubMed] [Google Scholar]
- 205. Ferguson J, Volk S, Vondracek T, Flanigan J, Chernaik A. Empiric therapeutic anticoagulation and mortality in critically ill patients with respiratory failure from SARS‐CoV‐2: a retrospective cohort study. J Clin Pharmacol. 2020;60(11):1411‐1415. [DOI] [PubMed] [Google Scholar]
- 206. Hanif A, Khan S, Mantri N, et al. Thrombotic complications and anticoagulation in COVID‐19 pneumonia: a New York City hospital experience. Ann Hematol. 2020;99(10):2323‐2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Shi C, Wang C, Wang H, et al. The potential of low molecular weight heparin to mitigate cytokine storm in severe COVID‐19 patients: a retrospective clinical study. medRxiv . 2020. [DOI] [PMC free article] [PubMed]
- 208. Sivaloganathan H, Ladikou EE, Chevassut T. COVID‐19 mortality in patients on anticoagulants and antiplatelet agents. Br J Haematol. 2020;190(4):e192‐e195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209. Stessel B, Vanvuchelen C, Bruckers L, et al. Impact of implementation of an individualised thromboprophylaxis protocol in critically ill ICU patients with COVID‐19: a longitudinal controlled before‐after study. Thromb Res. 2020;194:209‐215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210. Yormaz B, ErgÜn D, Tülek B, Ergün R, Arslan U, Kanat F. The impact of the" low molecular weight heparin" administration on the clinical course of COVID‐19 disease. Turk J Med Sci. 2020;51:28‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211. Mattioli M, Benfaremo D, Mancini M, et al. Safety of intermediate dose of low molecular weight heparin in COVID‐19 patients. J Thromb Thrombolysis. 2020;51:1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212. Rossi R, Coppi F, Talarico M, Boriani G. Protective role of chronic treatment with direct oral anticoagulants in elderly patients affected by interstitial pneumonia in COVID‐19 era. Eur J Intern Med. 2020;77:158‐160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213. Nagashima S, Mendes MC, Camargo Martins AP, et al. Endothelial dysfunction and thrombosis in patients with COVID‐19—brief report. Arterioscler Thromb Vasc Biol. 2020;40(10):2404‐2407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214. Busch MH, Timmermans SA, Nagy M, et al. Neutrophils and contact activation of coagulation as potential drivers of COVID‐19. Circulation. 2020;142(18):1787‐1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215. Cimmino G, Conte S, Morello M, et al. Vitamin D inhibits IL‐6 pro‐atherothrombotic effects in human endothelial cells: a potential mechanism for protection against COVID‐19 infection? J Cardiovasc Dev Dis. 2022;9(1):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216. Zuo Y, Zuo M, Yalavarthi S, et al. Neutrophil extracellular traps and thrombosis in COVID‐19. J Thromb Thrombolysis. 2021;51(2):446‐453. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that the data supporting the findings of this study is available within the article.


