Abstract
Papillary glioneuronal tumors are a rare and typically benign entity with pathological and radiographic complexity. Presentation can mimic other neoplasms, making diagnosis more challenging. The literature to date describes the clinical understanding, diagnostic, therapeutic, and prognostic characteristics of this limited number of patients. In this article, we report an unusual case of a glioneuronal tumor with multifocal presentation, normal pressure hydrocephalus-like symptoms, and large peritumoral parenchymal cysts, which guided the surgical approach. This unusual presentation has not previously been reported and adds valuable information to the clinical recognition and management literature.
Keywords: Papillary glioneural tumor, Intraventricular spread, Low-pressure hydrocephalus
Introduction
Papillary glioneuronal tumors (PGNTs) are a rare, benign neoplasm initially identified as a distinct entity in the late 1990s [1]. They are typically solid or solid/cystic, well-circumscribed, typically parenchymal and solitary, and often calcify. While intraventricular location, tumoral hemorrhage [2], and/or high-pressure obstructive hydrocephalus have been described [3], presentation with multifocal disease and normal pressure hydrocephalus (NPH)-like symptoms has not. This case report describes the novel presentation of an otherwise uncommon glioneuronal tumor distinctly presenting with NPH-like symptoms from intraventricular spread and the associated management.
Case report
The patient, in his mid-50s, presented with unsteady gait for over a year and mild short-term memory impairment, initially concerning clinically for NPH. Additional symptoms included mild nonspecific visual changes. Past medical history was significant for hyperlipidemia and solitary kidney from birth. Neurological exam revealed a shuffling gait but normal vision; the patient denied any other localizing symptoms. Outpatient neurology workup included magnetic resonance imaging (MRI) of the brain revealing a complex hemorrhagic and calcified lesion in the right atrium of the lateral ventricle, in the setting of mild, triventricular enlargement without transependymal flow, with a separate enhancing lesion at the outflow of the cerebral aqueduct. Surrounding the atrial mass were multiple large intraparenchymal cysts extending to the parietal cortex consistent with cerebrospinal fluid (CSF) on all MRI sequences (Fig. 1). Systemic workup was negative for metastatic disease. The patient underwent a transcortical resection of the intraventricular tumor through the CSF-filled parenchymal cysts. Intraoperatively the tumor appeared to be exophytic from the atrial choroid plexus.
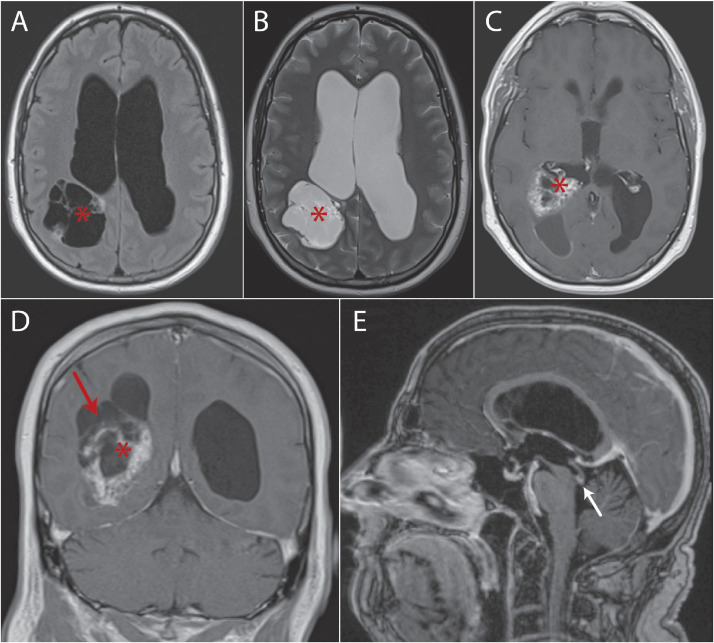
Fig. 1.
Preoperative MRI. Axial FLAIR and T2 (A and B) images showing CSF-consistency parenchymal cysts extending from the tumor to the subcortical region (asterisk). Contrasted T1 images (C axial and D coronal) show the atrial tumor (asterisk) and the surgical corridor through the parenchymal cysts (red arrow). Figure E shows the satellite lesion (white arrow) in the distal aqueduct causing the clinical hydrocephalic presentation. MRI: magnetic resonance imaging.
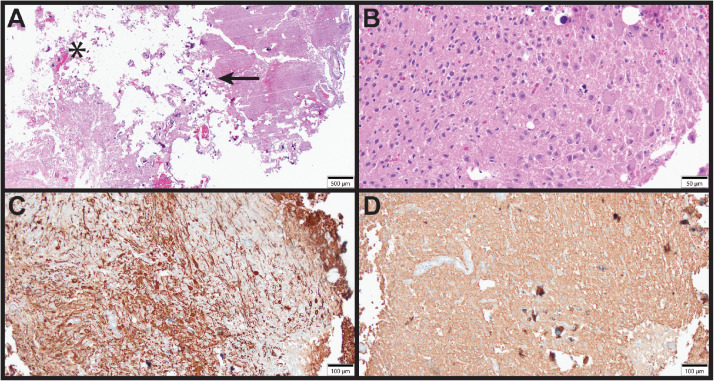
Histologic examination revealed a neuroepithelial neoplasm composed of atypical ganglion cells and a population of smaller neurocytic cells (Fig. 2). The tumor revealed heavy mineralization; numerous hyalinized vessels and pseudopapillary structures were noted. By immunohistochemistry, the gangliocytic population showed staining for neurofilament and synaptophysin and was negative for nuclear NeuN. A subset of the gangliocytic cells expressed GFAP. The small neurocytic cell population was weakly to moderately positive for synaptophysin and displayed some variable positivity for Olig2 and GFAP. The tumor cells were essentially negative for CD34 and TTF-1. High-grade morphologic features (significant mitotic activity, necrosis, endothelial proliferation) were absent, although cytologic atypia was focally increased. The Ki67 proliferation index was less than 1%. Next-generation sequencing studies identified the classic SLC44A1::PRKCA fusion, confirming diagnosis of PGNT. Gangliocytic differentiation and extensive mineralization are unusual histologic features in PGNT but have been previously reported [4]. Interestingly, this tumor failed to classify on DNA methylation array analysis using the Heidelberg central nervous system classifier v12.5 (this entity is not present in the v11b4 version of the classifier); the significance of this finding is unknown.
Fig. 2.
Histologic features. (A) Low-power view of hematoxylin and eosin (H&E) stained section. The tumor was heavily fragmented and mineralized. Large areas were hypocellular and showed numerous hyalinized vessels (asterisk) while other areas were more cellular (arrow). The adjacent brain parenchyma showed reactive piloid gliosis (not shown). (B) Higher-power view. The tumor was composed of a gangliocytic component and a smaller neurocytic component. Mitotic activity was not prominent and there was no endothelial proliferation or necrosis. Cytologic atypia was focally increased (not shown). (C and D) Immunohistochemical staining for neurofilament and synaptophysin, respectively. The gangliocytic cells showed variable somal positivity for neurofilament. Synaptophysin highlights a neuropil background and was weakly to moderately positive in both the gangliocytic and smaller neurocytic components.
Postoperatively, the patient had initial resolution of his NPH-like symptoms, as the resection corridor acted as a ventriculostomy around his aqueductal obstruction from the daughter tumor; however, this ultimately closed off and his symptoms returned. His residual hydrocephalus was subsequently managed via endoscopic third ventriculostomy with resolution of his gait and cognitive symptoms. Initial postoperative visual field deficit resolved on follow-up examination.
Discussion
PGNT is now a well-recognized, albeit rare, usually benign primary central nervous system neoplasm that can present in numerous intracranial locations [3]. While localized intraventricular PGNTs have been reported in the literature, this is the first reported case of a glioneuronal tumor presenting with multifocal disease and normal pressure hydrocephalus-like symptoms, including peritumoral parenchymal CSF cysts. This case presents some novel and important learning points.
The preoperative radiographic differential for this lesion includes other uncommon, low-grade glial neoplasms such as pleomorphic xanthoastrocytoma, ganglioglioma, or pilocytic astrocytoma, both of which would be unusual for an intraventricular location but are often ventricle-adjacent, or a choroid plexus neoplasm5. The presence of multifocal disease raises the concern for a higher-grade primary neoplasm. No primary site was identified to suggest metastatic disease, and the tumor was histologically identified as a Grade 1 PGNT. This is unusual from a pathological perspective, and the novel presentation is of importance, as ventricular dissemination of the tumor does not portend a higher pathologic grade in this case. Also of interest, the tumor histologically contained numerous ganglion cells - a feature that has only rarely been reported in the papillary glioneuronal literature. Additionally, it did not match well by methylation to more common cases, despite having the classic diagnostic fusion.
Conclusion
In this unusual case, the tumor presented with multifocal disease from presumed intraventricular spread, which has not previously been described, with remote disease obstructing the cerebral aqueduct. The ventricular system decompressed through the tumor, creating intraparenchymal CSF cavities and thus presenting as a lower-pressure, chronic hydrocephalus while providing surgical access for resection without deficit. This case report describes the unique presentation of this multifocal intraventricular tumor and its subsequent management.
Patient consent
Written informed consent was obtained from the patient for publication of this case report.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Komori T, Scheithauer BW, Anthony DC, Rosenblum MK, McLendon RE, Scott RM, et al. Papillary glioneuronal tumor: a new variant of mixed neuronal-glial neoplasm. Am J Surg Pathol. 1998;22(10):1171–1183. doi: 10.1097/00000478-199810000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Benzagmout M, Karachi C, Mokhtari K, Capelle L. Hemorrhagic papillary glioneuronal tumor mimicking cavernoma: two case reports. Clin Neurol Neurosurg. 2013;115(2):200–203. doi: 10.1016/j.clineuro.2012.04.021. [DOI] [PubMed] [Google Scholar]
- 3.Li D, Wang JM, Li GL, Hao SY, Yang Y, Wu Z, et al. Clinical, radiological, and pathological features of 16 papillary glioneuronal tumors. Acta Neurochir. 2014;156(4):627–639. doi: 10.1007/s00701-014-2023-y. [DOI] [PubMed] [Google Scholar]
- 4.Hou Y, Pinheiro J, Sahm F, Reuss DE, Schrimpf D, Stichel D, et al. Papillary glioneuronal tumor (PGNT) exhibits a characteristic methylation profile and fusions involving PRKCA. Acta Neuropathol. 2019;137(5):837–846. doi: 10.1007/s00401-019-01969-2. [DOI] [PubMed] [Google Scholar]