Abstract
Objective
Research on proximal fractures in the humeral bicipital groove (BG), a region in which bones are not commonly fractured, is considered sparse in the literature. The objective of this research was to present the definite characteristics and distribution of BG fractures.
Methods
This retrospective study included and enrolled 119 proximal humeral fractures in adult patients with complete radiography data to identify the fracture distribution in the BG from January 2021 to August 2021. The bicipital region was divided into three parts, i.e. the upper 1/3, middle 1/3, and lower 1/3 of the BG, and the distribution of fracture lines was transcribed on the male or female template, as appropriate. In addition, the normal contralateral humerus was used to calculate the cortical thickness of the supratubercular groove and different parts of the BG (upper, middle, and lower parts). The Mann–Whitney test or one‐way ANOVA along with LSD tests were used to determine differences in the fracture distribution and cortical thickness between men and women.
Results
Fractures of the BG in both men and women were mainly located in the upper 2/3 region of the BG, especially in the middle 1/3 of the BG. There were significant differences in the cortical thickness of the BG in men compared with that in women. The cortical thickness was highest in the supratubercular ridge but not the BG in men and women, respectively.
Conclusion
This research concluded that bony BG fractures were always observed in the middle part of the BG and were mainly found in patients with four fractures of the proximal humerus. As a unique fracture pattern, the existence of a bony BG fracture always means that a patient has been injured by a relatively severe mechanism, and more attention should be given to these proximal humeral fractures.
Keywords: Bicipital groove fracture, Cortical thickness, Proximal humeral fracture, Morphology
This study included 119 proximal humeral fractures in adult patients with available plain X‐rays and CT scans to identify the fracture distribution in the bicipital groove. In addition, the normal contralateral humeral were also used to calculate the cortical thickness of the supratubercular and different part of bicipital groove (upper, middle, and lower parts). At last, this research concluded that the bony BG fracture was always observed in middle part of BG and mainly found in patients with four‐part proximal humeral fractures.

Introduction
Proximal humeral fractures (PHFs) are commonly occurring fractures that affect patients' health. PHFs account for approximately 4% to 5% of all traumatic fractures. 1 , 2 , 3 A high incidence of PHFs has been observed in elderly patients, and these fractures are often caused by low‐energy injuries. 4 To further improve the understanding to this fracture type, a classification based on a four‐segment theory or on 3D computed tomography (CT) scans was proposed by Edelson to describe those injuries in detail. 5 , 6 , 7 , 8 CT images, especially 3D CT images, are more reliable than radiographs in the assessment of proximal humeral fracture reduction loss and rehabilitation. 9 However, as an indented structure, the bicipital groove (BG) between the lesser and greater tubercles in the proximal part of the humerus is often ignored, and no fracture classifications, including the traditional Neer or Edelson CT classification, illustrate its features in combination with other fracture types or discuss it alone. Therefore, as the BG is an important landmark of the proximal humerus, it is necessary to emphasize the importance of the BG or fractures involving the BG as a separate type.
There is a functional significance of the BG related to bone operation, and the BG is considered to be an important anatomic marker for the replacement of prostheses of the humerus. The morphology of the BG affect the biomechanics of the long head of biceps brachii tendon, associated pathologies and traumatic injuries. 10 Individuals participating in sporting activities that require repetitive overhead motions are also effected by the structure of BG. 11 Relative comprehension of its morphometry is important for the selection of prostheses (design or position). 12 Taylor conducted anatomical and histological research on bicipital tunnels and separated the BG into three zones. 13 A BG fracture above the distal lesser tuberosity is considered to be located in Zone I (the traditional bony BG). The BG fractures in our research were fractures located in Zone I.
Among the research on proximal humeral fractures, few studies have focused on BG fractures; bones in this region are considered difficult to fracture. Therefore, the importance of the BG has been grossly overlooked. However, it has been found that BG fractures are not uncommon in patients with proximal humeral fractures. Furthermore, the characteristics of these fractures and factors effecting the occurrence of BG fractures remain unknown. Therefore, the aim of this article was to (i) illustrate the distribution of BG fractures, (ii) compare the cortical thickness in different regions of the BG, and (iii) improve the understanding of this unique fracture pattern.
Materials and Methods
In our study, data from patients with unique identifying numbers (the admission number) who were identified as having a BG fracture were evaluated retrospectively in one orthopaedics center. Among the proximal humeral fractures from January 2021 to August 2021, adult proximal humeral fracture patients with available CT examinations were included. Formal ethical approval was received from the Regional Ethics Committee of our hospital (S2020‐016‐1), and the study followed the Declaration of Helsinki. Informed written consent was also obtained from the patients enrolled in our study (NCT04523415).
The inclusion criteria were presented as follows: (i) a clear record of demographic and complete CT imaging data, and (ii) patients older than 18 years with a BG fracture occurring less than 3 weeks before allocation and treatment. The exclusion criteria were as follows: pathological fracture (other than osteoporotic).
Finally, 119 closed BG fractures (40 men, 49.2 ± 17.2 years and 79 women, 59.2 ± 15.5 years) were included in this research (Figure 1). Among them, five were due to a fall from a height, 20 were due to a traffic accident, 84 were due to falling while standing, and 10 were due to crushing. In addition, 119 normal CT data points of the contralateral proximal humeral were recorded and collected to measure the cortical thickness of the BG.
FIGURE 1.

A flowchart of this research on bony BG fractures
Proximal Humeral Templates
The template was created based on the patients' contralateral shoulder CT scans. Anterior–posterior images of the three‐dimensional (3D) proximal humerus were collected from Mimics software (Materialize, Belgium). In this research, identical Hounsfield units were used as the threshold of the bone tissue. The 3D pictures were used to illustrate proximal fractures. Then, the images (3D) were imported into different software (AI, Adobe Illustrator) and used as a template to illustrate the BG fracture. 5
The actual fracture lines were transcribed on the male or female template to present the BG fracture line distribution. To facilitate the analysis, small or high comminution was represented by a simple single fracture line. To maximize the accuracy of the fracture line drawn, fracture line drawing was performed by the first author and was then evaluated by another experienced trauma surgeon. If obvious discrepancies between the two surgeons were observed, the fracture lines were finally determined by the experienced surgeon after re‐evaluation.
The BG was divided into three different regions based on its location (Figures 2A and 3A). The first upper line connected the upper point of the greater and lesser tuberosities. The others were lines drawn parallel to the first line. The lowest parallel line was drawn, which was located on the base of the lesser tuberosity. Then, the bicipital region was divided into three parts: the upper 1/3, middle 1/3, and lower 1/3 of the BG.
FIGURE 2.

The regional division and distribution of BG fractures in male patients. (A) The bony BG was divided into three parts (upper, middle, and lower). (B) The distribution of BG fractures in male patients
FIGURE 3.

The regional division and distribution of BG fractures in female patients. (A) The bony BG was divided into three parts (upper, middle, and lower). (B) The distribution of BG fractures in female patients
Cortical Thickness Measurement
The cortical thickness of the BG and the supratubercular ridge was calculated with Mimics and 3‐Matic software (Materialize, Belgium). After being constructed by Mimic with B30 CT data (bone window of CT), the 3D construction pictures were exported to another software package (3‐Matic). Wall thickness analysis was conducted, and then, the local cortical thickness with a triangular shape was measured within the software. The middle point of the BG in the upper, middle, and lower regions was used as the measurement point to minimize measurement error (Figure 4). BG fracture distribution maps were drawn for men and women separately.
FIGURE 4.

The cortical thickness map in a normal humerus. The middle point along the longitudinal axis of the BG was selected as the measurement location. Three points were selected as the cortical thickness measurement points in the upper, middle, and lower parts of the BG. The redder the color, the thicker the cortex
Statistical Analysis
The Levene test was used to evaluate homogeneity for continuous variables. Mann–Whitney or one‐way ANOVA along with LSD tests were used to evaluate categorical variables. For this research, significant differences were set at the p < 0.05 level. All analyses were calculated with SPSS 22.0. According to the general requirements of statistics, taking α = 0.05 and β = 0.1, the preliminary experiment illustrated that the mean ± standard deviation of the cortical thickness in different groups was 7.89 ± 0.55, 5.03 ± 0.53, 5.01 ± 0.39, 5.39 ± 0.65, and 7.03 ± 0.65. PASS 11 software was used to determine the minimum number of cases to be completed in each group.
Results
The Distributions of BG Fractures in Patients with Fracture
The k values for the inter‐ and intraclass correlation coefficients between the first author and the experienced surgeon were calculated, and the results demonstrated excellent agreement (0.872 and 0.901). It was observed that there were more women who had this fracture than men (40 vs 79) and that the ages were also significantly different between male and female patients (49.2 ± 17.2 vs 59.2 ± 15.5, respectively, z = −3.511, p < 0.001). The distribution of patients based on age and injury mechanism illustrated that women had a bimodal distribution, and the most common injury mechanism was falling while standing (Figure 5). The classification requirement for a PHF diagnosed with a BG fracture was the fracture of three (men, 15; women, 25) or four (men, 12; women, 67) parts, mainly four parts (p < 0.05).
FIGURE 5.
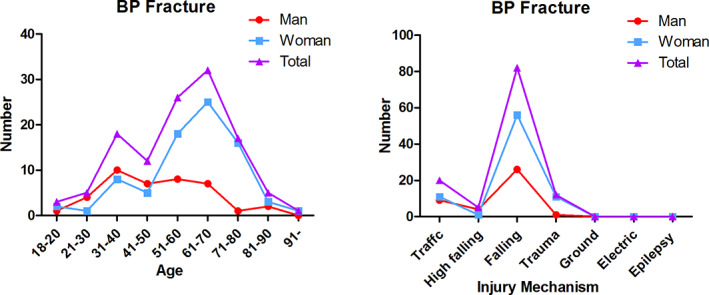
The age and injury mechanism distribution of fracture patients. (A) The patients' distribution by age. (B) The patients' distribution by different injury mechanisms. BP: bicipital groove fracture
The fractures of the BG in men were mainly located in the upper 2/3 of the BG; 19 fractures were located in the middle 1/3, six were in the upper 1/3, and one was in the lower 1/3. The other fractures were longitudinal fractures adjacent to the greater (eight) or lesser (four) tuberosity or located between the two tuberosities (two) (Figure 2). The BG fractures in women were also mainly located in the upper 2/3 of the BG; 45 fractures were located in the middle 1/3; eight were in the upper 1/3; eight were in the lower 1/3; and the others were longitudinal fractures adjacent to the greater (12) or lesser (six) tuberosity (Figure 3).
Cortical Thickness Compared to that of the Normal Contralateral Humeral Region
The cortical thickness of the BG was measured in the upper, middle, and lower parts of the BG, and significant differences were found between men and women in the upper (2.72 ± 0.45 mm vs 2.41 ± 0.60 mm, p = 0.001) and middle parts (2.39 ± 0.48 mm vs 2.00 ± 0.56 mm, p < 0.001). There were significant differences between men and women in the lower part of the BG (2.49 ± 0.47 mm vs 2.07 ± 0.61 mm, p < 0.001).
In men, no significant differences were found in the upper, middle, and lower regions of the BG. In women, the upper cortices were thicker than those of the middle region (p < 0.001) and had significant differences compared with those of the lower part (p < 0.001). However, there were no significant differences in cortical thickness between the middle and lower regions (p = 0.759).
The cortical thickness in different parts was found to be highest in the connected region between the lesser tuberosity and humeral head, called the supratubercular ridge, which is a bony prominence that is continuous with the lesser tuberosity. Significant differences were found in men and women in the cortical thickness in the supratubercular region compared with that in the BG (upper, middle, and lower). There were significant differences between men and women in the supratubercular cortical thickness (4.41 ± 0.66 vs 3.26 ± 0.62, P < 0.001) (Figure 6) (Table 1).
FIGURE 6.

Comparisons of cortical thickness in different regions in men and women. * indicates that there is a significant difference compared with the upper BG (p < 0.05). # indicates that a significant difference existed compared with the middle BG. & indicates that there is a significant difference compared with the lower BG
TABLE 1.
Comparison between male and female cortical thickness in different part of BG
| Upper BG | Middle BG | Lower BG | Supratubercular Ridge | |||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | Male | Female | |
| Thickness | 2.72 ± 0.45 | 2.41 ± 0.60 | 2.39 ± 0.48 | 2.00 ± 0.56 | 2.49 ± 0.47 | 2.07 ± 0.61 | 4.41 ± 0.66 | 3.26 ± 0.62 |
| Z | −3.283 | −3.694 | −4.663 | −7.290 | ||||
| p value | 0.001 | <0.001 | <0.001 | <0.001 | ||||
Discussion
A BG fracture has been considered a rare fracture pattern among proximal humeral fractures; however, this study found that there are many proximal humeral fractures that occur along with a BG fracture. The average age of men diagnosed with a BG fracture was older than that of women. The BG was not the thickest region in the proximal humeral. The upper region was thicker than the lower part of the BG in men and women. Men had a thicker cortex in the BG than women. This research suggested that examination for fractures should be performed carefully; the structure of the BG is strong, but it is not the thickest of the proximal humeral regions. This research will be beneficial for surgeons and provides them with information which suggests that they should reconsider the fracture pattern identified by traditional classifications of proximal humeral fractures; moreover, treatments of BG fractures should be emphasized.
Distribution of Transverse BG Fractures
Taylor separated bicipital tunnels into three zones, and a BG fracture above the distal end of the lesser tuberosity was called a Zone I fracture (the traditional bony BG). 8 That research illustrated that most transverse BG fractures occur in the upper and middle regions, especially in the middle region (Figure 7). Although the region of the lower 1/3 of the BG is also characterized by a thick wall, fractures in this region were rare in our research. The reason for this can be assumed to be that the region is adjacent to the surgical neck, which is characterized by a lower wall thickness compared with the humeral shaft, and trauma in this region is more prone to cause a fracture in the surgical neck. Fractures in the upper 2/3 can be explained as a surgical neck fracture, and the force of the trauma resulting in the surgical neck fracture extended to the strongest region of the BG, which then fractured and created a serious fracture in the proximal humeral region. The results of the cortical thickness also supported that the middle region is more inclined to fracture compared with the lower and upper 1/3 of the BG region.
FIGURE 7.

An illustration of transverse BG fractures. (A, B) A BG fracture located in the upper 1/3 region; (C, D) A BG fracture located in the middle 1/3 region
Distribution of Longitudinal BG Fractures
This research illustrated that most longitudinal fracture lines are focused mainly along the connecting region of the greater tuberosity and BG, but there were also longitudinal fracture lines that ran along the connection of the lesser tuberosity and BG (Figure 8). The reason for this outcome is that the connection region has a rapid change in cortical thickness, which is illustrated in Figure 3. These regions might be epiphyseal regions when patients are young. There was also a transition zone located at the surgical neck, similar to the connection region between the BG and greater tuberosity or the region between the BG and lesser tuberosity; therefore, it was hypothesized that the epiphyseal region had a higher risk of fracture occurrence in adults. Furthermore, Hufeland reported that the ascending branches of the anterior circumflex supplied not only the long head biceps tendon but also nourished the BG itself, and it was notable that most branches of the artery penetrate the lateral wall of the BG; therefore, the longitudinal fracture lines located at the connecting region of the greater tuberosity and BG are more likely to affect the healing process of a BG fracture. 14 , 15
FIGURE 8.

An illustration of longitudinal BG fractures. (A, B) A BG fracture located mainly along the connecting region of the greater tuberosity and BG; (C, D) A BG fracture located mainly along the connecting region of the lesser tuberosity and the BG
Mechanical Analysis Based on Corresponding Cortical Thickness
Although a mechanical experiment was not conducted, it is believed that the cortical thickness can represent the strength of the proximal humerus. The thicker the cortex is, the stronger the forces it can withstand. This study demonstrated that the BG has a thicker cortex than other regions of the proximal humerus. The middle region had a thinner cortex than the upper and lower regions, which was consistent with our results that most BG fractures were found in the middle 1/3 of the BG. In addition, it was found that the thickest region was located at the connection of the lesser tuberosity and humeral head called the supratubercular ridge. One reason for this is that the coalescence of the lesser tuberosity with the humeral head occurs early (at the age of 4–5 years), so the region is relatively strong. The second was that as the end point of the teres major and subscapular muscle, the pull force strengthens the region. Similar enforcement was also observed in the connection region of the greater tuberosity and humeral head. It may seem to contradict what we think about the BG being the strongest region in the clinic, but actually, the strength it sustains is affected not only by cortical thickness but also by the structure itself. The rear bulges (10 cm) in the passenger space are used to strengthen the bodies of German cars, which have a structure similar to the BG, and this may be one of the explanations for the stiffer BG.
Limitations and Strength
One limitation of this research is the limited number of enrolled patients. More volunteers will be enrolled in subsequent research. Second, the subjects enrolled consisted only of people with fractures, which may affect the results. Third, whether a transition region, such as that connecting the diaphysis and metaphysis or the greater tuberosity and BG, was present remains unclear. A strength of this research is that it is the first research to focus on the fracture line distribution of BG fractures and analyze the cortical thickness with powerful software. With more attention directed toward BG fractures, further understanding of these unique fractures will be gained. In our subsequent research, the transition regions illustrated in the cortical thickness map will be further studied to verify whether this connection region has a greater risk of fracture. A large‐scale study on the incidence of BG fractures will also be initiated, and a new fracture classification containing BG fractures will be proposed.
Conclusion
This research concluded that bony BG fractures were always observed in the middle part of the BG and were mainly found in patients with four‐part proximal humeral fractures. As a unique fracture pattern, the existence of bony BG fracture always means a relatively severe injury, and more attention should be given to these proximal humeral fractures.
Competing Interests
The authors have declared that no competing interests exist.
Authors' Contributions
Conceptualization: Yingze Zhang. Data curation: Meishuang Shang. Formal analysis: Weichong Dong. Investigation: Yali Zhou, Wei Chen. Methodology: Jialiang Guo. Project administration: Jialiang Guo, Yali Zhou. Resources: Yingze Zhang, Weichong Dong Software: Jialiang Guo, Xiaojuan Zhang. Supervision: Zhiyong Hou, Yingze Zhang. Validation: Zhiyong Hou, Yingze Zhang. Visualization: Zhiyong Hou. Writing—original draft: Jialiang Guo. Writing—review & editing: Jialiang Guo.
Ethics Approval and Consent to Participate
Ethical approval was received from the Regional Ethics Committee of our hospital (S2020‐016‐1), and the study was conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from all patients enrolled in the study.
Consent for Publication
All authors and participants gave consent for publication.
Availability of Data and Material
All relevant data are within the manuscript and its Supporting Information files.
Acknowledgements
The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The research was supported by National Natural Science Foundation of China (82072523, 82002281), Natural Science Foundation of Hebei (H2021206054, H2020206193), the Main Medical Scientific Research of Hebei (20210543) and China Postdoctoral Fund (2021M701785), the Science and Technology Project of Hebei Education Department (SLRC2019046), Government‐funded Clinical Medicine Outstanding Talent Training Project (2019), and the 14th Five‐Year Clinical Medicine Innovation Research Team of Hebei Medical University (2022). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Contributor Information
Weichong Dong, Email: 842178994@qq.com.
Yingze Zhang, Email: 460706223@qq.com.
References
- 1. Jo YH, Lee KH, Lee BG. Surgical trends in elderly patients with proximal humeral fractures in South Korea: a population‐based study. BMC Musculoskelet Disord. 2019;20(1):136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Du S, Ye J, Chen H, Li X, Lin Q. Interventions for treating 3‐ or 4‐part proximal humeral fractures in elderly patient: a network meta‐analysis of randomized controlled trials. Int J Surg. 2017;48:240–6. [DOI] [PubMed] [Google Scholar]
- 3. Zhao L, Qi YM, Ang L, Wang GR, Zheng SN, Wang Q, et al. Comparison of the effects of proximal humeral internal locking system (PHILOS) alone and PHILOS combined with fibular allograft in the treatment of Neer three‐ or four‐part proximal Humerus fractures in the elderly. Orthop Surg. 2019;11(6):1003–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Liu ZZ, Zhang GM, Ge T. Use of a proximal humeral internal locking system enhanced by injectable graft for minimally invasive treatment of osteoporotic proximal humeral fractures in elderly patients. Orthop Surg. 2011;3(4):253–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Edelson G, Kelly I, Vigder F. Reis ND.A three‐dimensional classification for fractures of the proximal humerus. J Bone Jt Surg. 2004;86(3):413–25. [DOI] [PubMed] [Google Scholar]
- 6. Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, et al. Fracture and dislocation classification compendium ‐ 2007: Orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma. 2007;10 Suppl:S1–133. [DOI] [PubMed] [Google Scholar]
- 7. Hasan AP, Phadnis J, Jaarsma RL, Bain GI. Fracture line morphology of complex proximal humeral fractures. J Shoulder Elbow Surg. 2017;26:e300–8. [DOI] [PubMed] [Google Scholar]
- 8. Edelson G, Saffuri H, Obid E, Vigder F. The three‐dimensional anatomy of proximal humeral fractures. J Shoulder Elbow Surg. 2009;26(10):e300–8. [DOI] [PubMed] [Google Scholar]
- 9. Jia XY, Chen YX, Qiang MF, Zhang K, Li HB, Jiang YC, et al. Postoperative evaluation of reduction loss in proximal humeral fractures: a comparison of plain radiographs and computed tomography. Orthop Surg. 2017;9(2):167–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Khan R, Satyapal KS, Naidoo N, Orthop LLJ. Dimensional analysis of the bicipital groove and its associated pathology in a South African population. 2019;19:128–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Srimani P, Saha R, Goswami B, Mazumdar S. Morphometric analysis of bicipitalgroove of humerus with clinical implications: a study in West Bengal. Int J Anat Res. 2016;4(4):3009–15. [Google Scholar]
- 12. Yahuaca BI, Simon P, Christmas KN, Patel S, Gorman RA 2nd, Mighell MA, et al. Acute surgical management of proximal humerus fractures: ORIF vs. hemiarthroplasty vs. reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2020;29(7s):S32–s40. [DOI] [PubMed] [Google Scholar]
- 13. Taylor SA, Fabricant PD, Bansal M, Khair MM, McLawhorn A, DiCarlo EF, et al. The anatomy and histology of the bicipital tunnel of the shoulder. J Shoulder Elbow Surg. 2015;24(4):511–9. [DOI] [PubMed] [Google Scholar]
- 14. Hufeland M, Hamed H, Kubo H, Pilge H, Krauspe R, Filler T, et al. Blood supply in the bicipital groove: a histological analysis. Orthop Rev. 2019;11(1):8106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hufeland M, Wicke S, Verde PE, Krauspe R, Patzer T. Biceps tenodesis versus tenotomy in isolated LHB lesions: a prospective randomized clinical trial. Arch Orthop Trauma Surg. 2019;139(7):961–70. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.


