Abstract
Objective
Patch technology has been the new technique in the treatment of partial thickness of the rotator cuff tear (PTRCTs) to address the limitation of traditional techniques. Compared with allogeneic patches and artificial materials, coracoacromial ligament is obviously closer to their own biology. The purpose of the study was to evaluate the functional and radiographic outcomes following arthroscopic autologous coracoacromial ligament augment technique for treatment of PTRCTs.
Method
This study included three female patients with PTRCTs who underwent arthroscopy operation in 2017 with an average age of 51 years (range from 50 to 52 years). The coracoacromial ligament implant was attached to the bursal side surface of the tendon. The clinical results were evaluated by American Shoulder and Elbow Surgeons (ASES) score, Simple Shoulder Test (SST), acromiohumeral distance (AHD) and muscle strength before and 12 months after operation. Magnetic resonance imaging (MRI) was performed 24 months after operation to assess the integrity of the anatomical structure of the original tear site.
Result
The average ASES score improved significantly from 57.3 preoperatively to 95.0 at 1‐year follow‐up. The strength improved significantly from grade 3 preoperatively to grade 5 at 1 year. Two of three patients underwent the MRI at 2‐year follow‐up. Radiographic released the complete healing of rotator cuff tear. No implant‐related serious adverse events were reported.
Conclusion
The new technique of using autogenous coracoacromial ligament patch augment provides good clinical results on patients with PTRCTs.
Keywords: Arthroscopic Rotator Cuff Repair, Autograft, Biologic Augmentation, Coracoacromial Ligament, Partial Thickness of Rotator Cuff Tear
After the coracoacromial ligament was released from the coracoid and acromion insertion and the initial repair of the rotator cuff, the autograft was inserted into the injured area to reinforce the rotator cuff.

Introduction
Partial thickness of rotator cuff tear (PTRCT) is a common disease of the shoulder joint with symptoms such as shoulder pain, tenderness, limited range of motion, and muscle atrophy. Its prevalence in the population varied from 13% to 40%, which is strongly correlated with age. 1 , 2 Studies have shown that some injured rotator cuff tissues are unlikely to heal spontaneously. Meanwhile, they can gradually develop into full‐thickness tears. 3 , 4 , 5 Ellman introduced a classification including the site (the articular surface, bursal surface, and intra‐tendinous) and extention of the partial tear. The grade of tear depth was defined as measured arthroscopically by a probe: Grade I tears had a depth of less than 3 mm; Grade II tears of 3–6 mm; Grade III tears had involvement of more than half of the thickness of the tendon. 6
At present, most studies believe that surgical treatment is usually considered for patients with PTRCTs with tear depth greater than 50%. 7 , 8 , 9 However, there are great differences on repair techniques in orthopaedic literature, making it hard to draw conclusions on the surgical management of PTRCTs. In situ repair, conversion of the lesion to a full‐thickness tear repair, and intratendon repair are the most common techniques for PTRCTs. 10 , 11 , 12 , 13 However, they all have certain limitations. Studies have shown that intratendon repair usually leads to shoulder discomfort, postoperative shoulder stiffness, and delayed recovery of shoulder function. 14 The conversion of the lesion to a full‐thickness tear will lead to the imbalance between the length and tension of the injured tendon and the adjacent healthy tendon, resulting in the deflection of tissue stress after repair,postoperative pain, shoulder discomfort, and retear. 15 , 16 , 17 , 18 Therefore, the traditional intervention cannot completely solve the shoulder pain which is caused by the injured rotator cuff tissues and the further development of injuries.
In recent years, researchers have carried out a series of technical innovations, such as platelet‐rich plasma, cell scaffolds, patch, etc. to solve the limitation. Some studies have applied patch technology on partial rotator cuff tears to make up for the limitations of traditional technology and to achieve good clinical results in the short‐ and long‐term follow‐up. 19 , 20 , 21 , 22 , 23 , 24
At present, collagen implants and xenogeneic implants are usually selected for PTRCT patches. But there is no research using autologous patch materials for the treatment of PTRCTs as rotator cuff tissue augmentation. The aim of the study was as follows: (1) to determine the clinical outcomes of arthroscopic autologous coracoacromial ligament augment technique for treatment of PTRCTs compared with the traditional procedure, (2) to assess the influence of the patch augment on the treatment of PTRCTs, (3) to evaluate the selection of using coracoacromial ligament as the autologous implant.
Technique
Indication
The target population of this study was patients with PTRCT. Inclusion criteria: (1) preoperative diagnosis with more than 50% of partial thickness of rotator cuff tear; (2) preoperative MRI evaluation of fat infiltration < III (goutallier classification); (3) patients over 18 years old. Exclusion criteria: (1) history of revision or other shoulder joint surgery; (2) shoulder dislocation, infection, or tumor; (3) brachial plexus injury or deltoid muscle dysfunction. This study was approved by the ethics committee of the Sun Yat‐sen memorial hospital (SYSEC‐KY‐KS‐2018‐036).
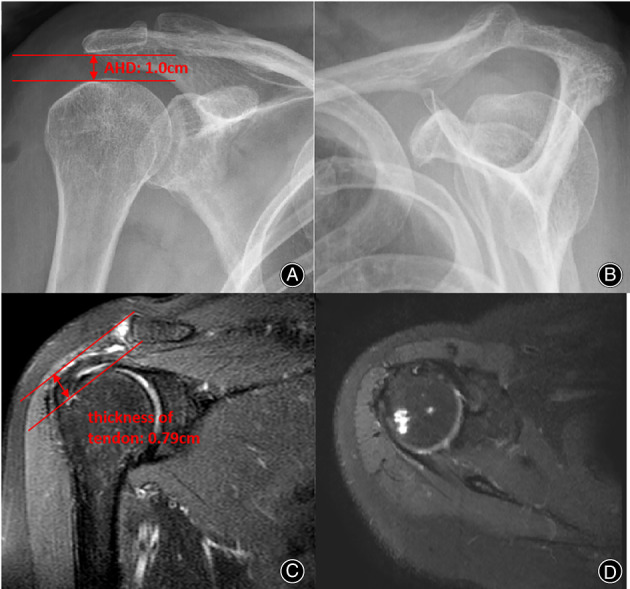
We included three patients, which two of them suffered 1‐year history of shoulder pain with the other one suffering 3‐year shoulder pain. And none of them had obvious trauma. In their preoperative physical examination, Jobe test and 0° Jobe test were positive. Two of them were Neer sign and Hawkins sign positive. MRI showed that all three patients appear to have partial thickness tears of supraspinatus greater than 50% (Ellman III). In addition, the tissue of infraspinatus and subscapularis muscles of all three patients were intact. Meanwhile, their fat infiltration were all the goutullier I grade. All three patients were evaluated for shoulder joint function before operation (Figure 1). The tear width of all three patients were measured respectively in the arthroscopic with probe.
Fig. 1.
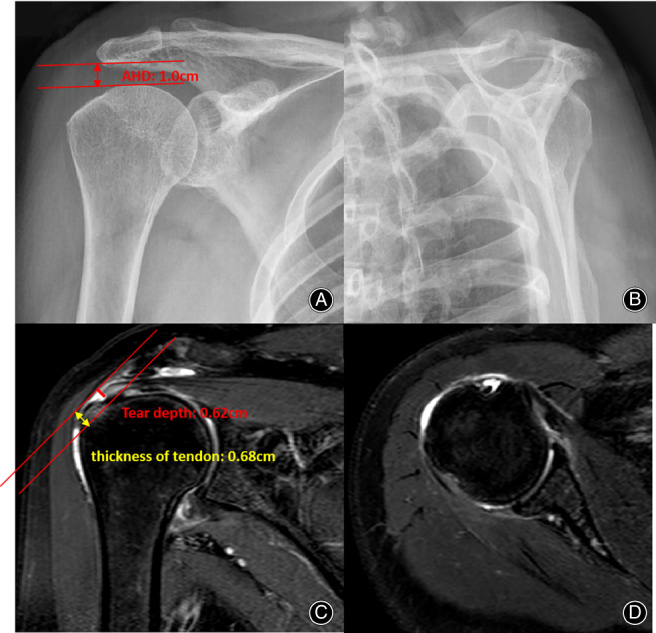
Preoperative shoulder radiograph. (A) The anterior‐posterior shoulder radiograph. It showed no bone injury. The AHD was 1.0 cm. (B) Supraspinatus export shoulder radiograph. (C) MRI showed the bursal side partial thickness of rotator cuff tear. The tear depth: 0.62 cm, Ellman III. The thickness of tendon was 0.68 cm. (D) MRI showed the tissue integrity of subscapularis and infraspinatus
Methods of Anesthesia and Patient Position
All patients underwent the operation under general anesthesia combined with brachial plexus block. They were turned to the lateral decubitus position with lateral traction to position the arm at 50° of abduction and 20° of forward flexion. We used routine shoulder approach, including posterior, anterior, lateral, and posterosuperior portals. (Figure 2).
Fig. 2.

(A) Routine portals were used including posterior, anterior, lateral and posterosuperior portals. (B) Patient were turned to the lateral decubitus position with lateral traction to position the arm at 50° of abduction and 20° of forward flexion
Approach Selection and Arthroscopic Evaluation
After the arthroscopic system was connected, the intra‐articular exploration was carried out through the posterior approach. And the articular cavity was cleaned. We performed joint capsule release in one of the patients. At the same time, we evaluated the integrity of the subscapular muscle and the long head tendon of biceps. In our intraoperative evaluation, all patients had good integrity of the long head tendon of biceps and the subscapular muscle so we do not take special treatment. After exploring the joint cavity, we probed the subacromial space through the posterior approach to explore the shape of the acromion and the integrity of supraspinatus and infraspinatus. All patients underwent acromioplasty and acromioplasty. Through arthroscopic rotator cuff tissue exploration, all patients showed more than 50% rotator cuff tissue injury on the bursal side. The tear size of rotator cuff was measured by measuring probe (Figure 3).
Fig. 3.
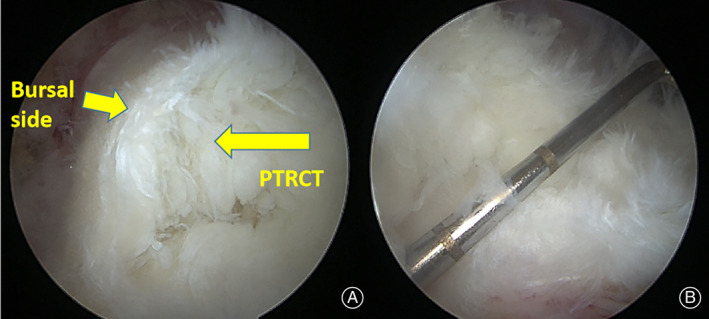
(A) It showed more than 50% rotator cuff tissue injury on the bursal side. (B) Tear size were measured with the probe. The measured value was 1.5 cm
Exploration and Resection of Coracoacromial Ligament
The acromial insertion of coracoacromial ligament was observed after subacromial synovial membrane releasing. We used the probe to evaluate the coracoacromial ligament to ensure that there was no injury or degeneration. Then, through the anterolateral approach, we dissociated the coracoacromial ligament from the acromial insertion to the coracoid process. Finally, the coracoacromial ligament was stripped from the coracoid process insertion point (Figure 4).
Fig. 4.
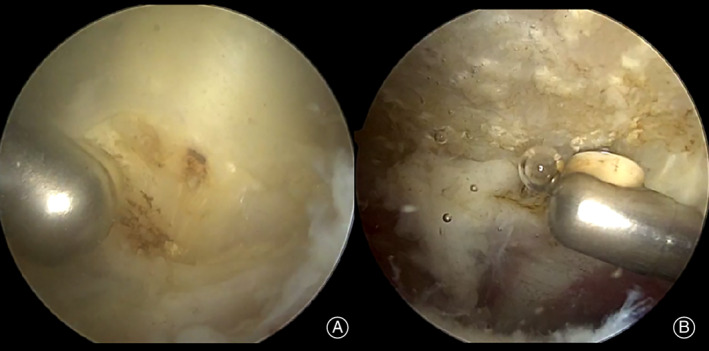
(A) The coracoacromial ligament was released from the coracoid insertion. (B) Then the coracoacromial ligament was released from the acromial insertion
Graft Preparation
After the coracoacromial ligament was dissociated, the assistant trimmed the coracoacromial ligament and prepared the graft. First, the integrity of coracoacromial ligament was examined to evaluate whether it can be used as a patch for rotator cuff augmentation. Then, the coracoacromial ligament was trimmed to an appropriate size according to the tear size of rotator cuff tissue. The degenerative tissue and attached synovium were removed, and the main structure of the ligament was retained. Generally, the graft size is slightly larger than the rotator cuff tear size (Figure 5).
Fig. 5.
(A) The coracoacromial ligament was trimmed to an appropriate size according to the tear size of rotator cuff tissue. (B) Fix the suture at one side of the coracoacromial ligament
Repair of Rotator Cuff Tissue
After the coracoacromial ligament was dissociated, the surgeon continued to repair the rotator cuff tissue. Conversion of the lesion to a full‐thickness tear repair technique was used in all patients. According to the tear size, we implanted one or two sutures (4.5 mm TwinFix Heart, America) at the tear site. Then, the suture line was passed through the medial side of the tear to repair the whole torn rotator cuff tissue, and all the proximal sutures were retained (Figure 6).
Fig. 6.
In situ suture technique was used in all patients.
We ensure that there is enough space between the sutures that the graft can slide under the acromion smoothly. Finally, the proximal suture passes through the medial side of the graft equally. With the assistance of arthroscopy, the graft is pushed under the acromion and close to the rotator cuff tissue. And the suture is fixed at the greater tubercle of humerus by using the double‐row repair with anchor (4.75 mm Swivelock C anchor, Arthrex) (Figure 7). Finally, the surgeon explored the rotator cuff again to confirm that the tear had been closed. The surgical diagrams are shown in Figure 8A–C.
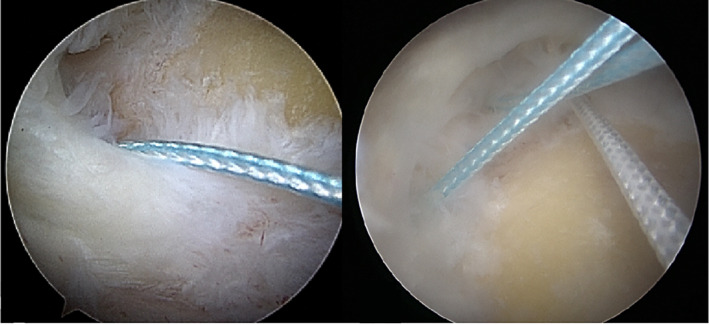
Fig. 7.
(A) The graft is pushed under the acromion and close to the rotator cuff tissue. (B) and (C) the suture is fixed at the greater tubercle of humerus by using the double‐row repair with anchor
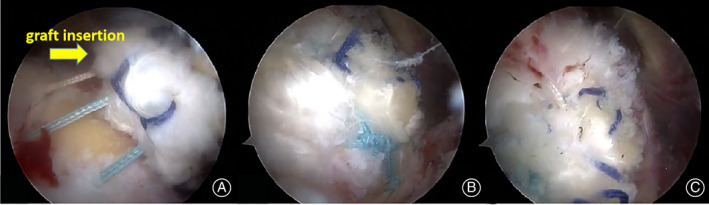
Fig. 8.
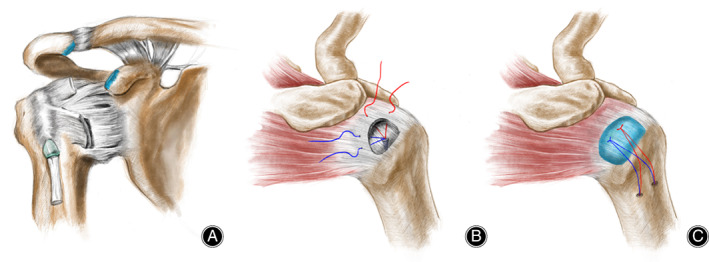
Surgical diagrams (A) The coracoacromial ligament released from the coracoid and acromion insertion. (B) Conversion of the lesion to a full‐thickness tear repair technique of PTRCT. (C) Operation completion diagram
Postoperative Care and Rehabilitation
All patients with PTRCTs received the same rehabilitation after operation. All patients' arms remained in abduction sling until 6 weeks after operation. Only limited and protected passive range were allowed during this period. From 6 weeks to 12 weeks after operation, active assisted elevation training was allowed, including forward flexion, abduction, external rotation, and adduction. Strength training is allowed after 12 weeks. All patients were evaluated for ASES, SST, and strength before and 1 year after operation. MRI was performed before and 2 years after operation. We considered ASES as the primary outcome indicator, strength and SST as the secondary outcome indicator. Acromiohumeral distance (AHD) was measured to evaluate whether the CAL can lead to humeral head migration due to loss of its anterosuperior stabilization function. MRI was used to evaluate the tissue integrity of rotator cuff.
Result
Population Characteristics
A total of three patients, aged 50, 52, and 52 years received arthroscopic autologous coracoacromial ligament augment technique. However, one of them was lost to follow‐up at 2 years after operation. Despite several communications, the patient refused to undergo MRI examination. The thickness of all patients are greater than 50%. In order to eliminate the interference, acromioplasty was performed in all patients. At 1 year after operation, the shoulder joint function score was evaluated. At 1 year follow‐up, the range of motion (ROM) of injured shoulder on all patients are almost the same as that of the general people (Figure 9).
Fig. 9.
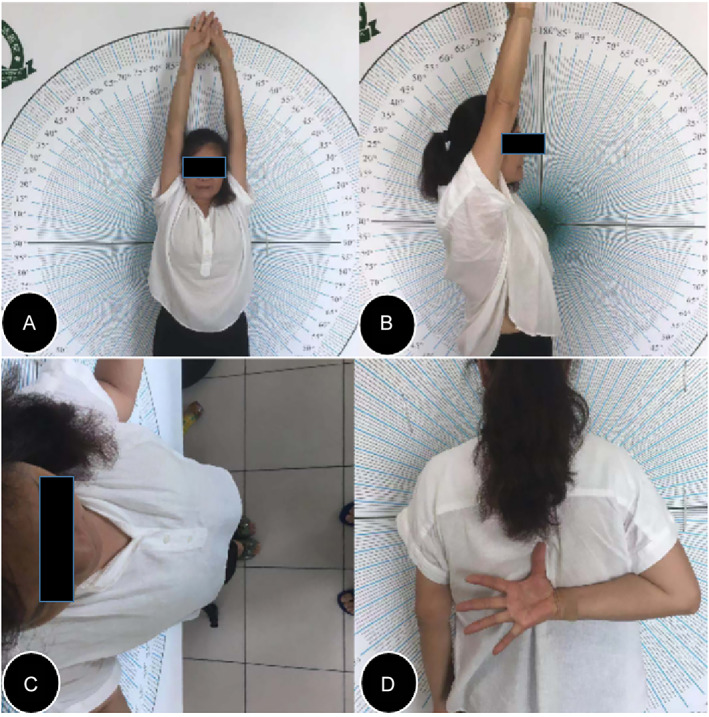
The evolution of ROM of injured shoulder (right shoulder) (A) forward flexion; (B) abduction; (C) external rotation; (D) internal rotation
The Assessment of Shoulder Function
The final average ASES score was from 57.3 (56, 54, 62) to 95.0 (92, 98, 95). The final average SST score was from 5.3 (5, 6) to 10.0 (9–11). The strength of all patients improved from grade 3 before operation to grade 5 at 1 year after operation (Table 1).
TABLE 1.
The comparation between preoperation and 1‐year follow‐up
| ASES | SST | Strength | ||||
|---|---|---|---|---|---|---|
| Patients | Preoperation | 1 year follow‐ up | Preoperation | 1 year follow‐ up | Preoperation | 1 year follow‐ up |
| A | 56 | 92 | 5 | 9 | 3 | 5 |
| B | 54 | 98 | 5 | 10 | 3 | 5 |
| C | 62 | 95 | 6 | 11 | 3 | 5 |
Abbreviations: ASES, American Shoulder and Elbow Surgeons; SST, Simple shoulder test.
Imaging Evaluation
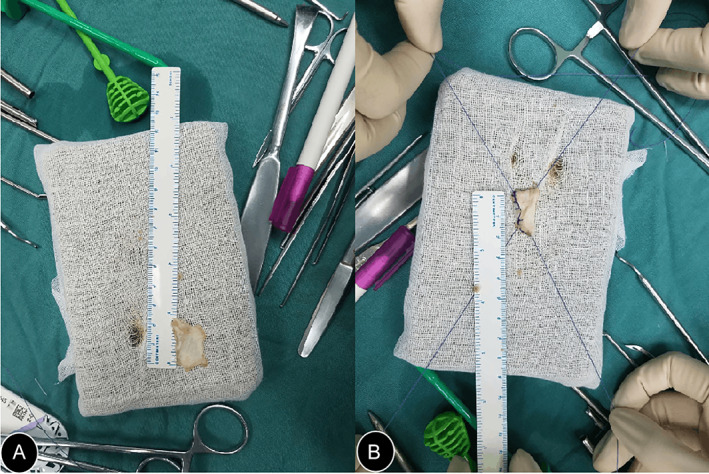
In the follow‐up, X‐ray showed that the AHD was 1.0 cm, which had no significant changes compared with the one before the operation. MRI showed that the intact tendon could be seen and the thickness of tendon increased from 0.68 cm to 0.79 cm. And no trace of implant was found (Figure 10).
Fig. 10.
Postoperative shoulder radiograph. (A) The anterior‐posterior shoulder radiograph. No bone injury occurred after the operation. AHD: 1.0 cm. (B) Supraspinatus export shoulder radiograph. (C) MRI showed that the rotator cuff had restored integrity. The thickness of the tendon increased from 0.68 to 0.79 cm. (D) MRI showed the tissue integrity of subscapularis and infraspinatus
No infection or adverse event related to surgery was found. No biological response to the patch was found. At the final follow‐up of this study, all patients had significant improvement in shoulder joint function.
Discussion
We introduced a new technique combining autogenous coracoacromial ligament and rotator cuff repair to restore the normal anatomical structure of the rotator cuff. We found that the ASES score, SST score, and strength were significantly increased. Meanwhile, radiographic sign showed that the intact tendon could be seen through the MRI. Previous research compared the arthroscopic debridement and repair in the bursal side PTRCTs. It showed that after the 18 months follow‐up, there was significant increase of shoulder function in both groups (ASES: 34.14 to 92.38 in debridement group; 33.10 to 93.63 in repair group). 25 Meanwhile another study explored the transtendon suture bridge repair in PTRCTs. The midterm outcomes showed that the shoulder function also increased significantly (ASES: 52 ± 14 to 94 ± 5; SST: 6 ± 2 to 11 ± 1). 26 Compared to the precious research, our study also showed the good clinical results (mean ASES: 57.3 to 95.0; mean SST: 5.3 to 10.0). It demonstrated that the transferred CA ligament as an augmentation is effective for PTRCTs.
The Limitation of the Traditional Operation Procedure
According to the previous studies, patients with PTRCTs were most commonly treated through in‐situ suture, conversion of the lesion to a full‐thickness tear suture or transtendon suture. However, some studies have shown that these traditional techniques have corresponding limitations, such as stress mismatch, shoulder discomfort, postoperative shoulder stiffness, and delayed recovery of shoulder function. 10 , 11 , 12 , 13 Yang et al. 17 evaluated the relationship between depth of bursal side partial thickness of rotator cuff tears and strain through biomechanical analysis. They found that the strain in the intact tendon rapidly increased nonlinearly with the tear depth greater than 50%. Several studies found that a higher failure rate happened after arthroscopic repair of bursal sided partial thickness of rotator cuff tears. 15 , 27 Other studies suggested that the strain imbalance caused by the length tension mismatch between the injured area and the surrounding intact tissue has became an important factor causing postoperative shoulder pain, progressive disease development, and even retear in patients with PTRCTs. 14 , 28 , 29 The new technique addresses several limitations of PTRCTs. The implant maintains the strain balanced which are caused by the length tension mismatch between the injured area and the surrounding intact tissue. And it may generate a natural healing.
The Technique of the Patch Augment on the Treatment of PTRCTs
With the continuous innovation of technology, patch technology has been developed and used to make up the defects of traditional technology. In recent years, the technology with using the patch has been commonly used in the arthroscopic treatment of rotator cuff tear. Several studies have introduced that the rotator cuff reinforcement through patch can also achieve satisfactory clinical results. In 2020, Amos et al. 20 used collagen‐based bioinductive implant to treat PTRCTs. They found that the shoulder function score and tendon depth were significantly improved after 1 year follow‐up. They believed that the implant can safely and effectively reduce the pain of patients with PTRCT and improve the function of shoulder joint. At the same time, they showed new tissue formation in the injured area of the rotator cuff tissue through imaging. Brandon et al. 30 introduced a multicenter randomized controlled study using bovine collagen implants to treat PTRCTs. They found that the implant can improve the shoulder function score (PROs) of patients with all levels of tear depth. And they believe that the implant can provide better early clinical results.
It has been found that strain can be significantly balanced by increasing the thickness of bursal side tissue. 23 The patch can improve the tendon healing environment by reducing the pressure in the tendon and preventing the rotator cuff tissue from retear due to strain imbalance. Through imaging, the researchers found that new tissue was formed in the rotator cuff tissue after collagen implant patch, and the patients' symptoms were significantly relieved. 20 , 30
Our research makes further innovation in patch technology. On the basis of repair of PTRCT, we enhanced the rotator cuff by patch augment, and restored the thickness of rotator cuff on the basis of maintaining its integrity and anatomical structure. At the last follow‐up, the final ASES scores of all three patients were significantly improved. Meanwhile, MRI showed that the rotator cuff returned to normal anatomical structure, and its depth was increased to a certain extent. Considering the two aspects, we believe that the patients have achieved excellent clinical results.
The Selection of Using Coracoacromial Ligament as the Autologous Implant
We have also made innovations in the selection of implants. We chose to use autologous coracoacromial ligament as implant material for reinforcement. The coracoacromial ligament, as a part of the coracoacromial arch, is correlated to the supraspinatus. 31 Many studies have shown that the degeneration of coracoacromial ligament can cause rotator cuff tear. 32 , 33 , 34 , 35 For this reason, surgeongenerally remove 2/3 of coracoacromial ligament during subacromial debridement. In this way, the risk factor of rotator cuff tear caused by coracoacromial ligament degeneration were eliminated. Meanwhile, the remaining coracoacromial ligament also kept the original function of inhibiting humeral head upward movement. Bektaser et al. 36 had introduced the augmentation of coracoacromial ligament graft for massive rotator cuff tears with mini‐open repair. They took 26 months (range 16–52 months) follow‐up. The follow‐up results showed that mean shoulder flexion, abduction, and Constant–Murley score were increased significantly. No surgical complications happened in patients during the follow‐up period. The integrity and tendon thickness were restored to normal tendons at the end of follow‐up. Bektaser et al. 37 also evaluated the effect of rotatory cuff repair with coracoacromial ligament transfer on humeral head migration. They found that humeral head was not migrated in the patients who had partial CAL excision at the early postoperative period. Taniguchi et al. 38 suggested that postoperative AHI for only large‐massive tears are associated with combined superior and anterolateral migration of the humeral head. In this study, we took out the coracoacromial ligament which was routinely removed, and strengthened the rotator cuff in the form of patch augment, so as to restore the normal anatomical structure and physiological thickness of the rotator cuff tissue. Meanwhile, the AHD before and after operation did not have significant changes. It showed that although the CAL was taken, the humeral head did not migrate significantly. We suggested that coracoacromial ligament has several advantages as a patch. Firstly, coracoacromial ligament degeneration is one of the high‐risk factors of rotator cuff tear. We removed coracoacromial ligament to eliminate the risk of rotator cuff tear. Secondly, coracoacromial ligament has sufficient thickness and width, and its size meets the requirements of the patch. Thirdly, as an autologous patch, coracoacromial ligament is suitable for patients. There is no need to worry about the rejection of allogeneic patch and artificial patch. Fourth, the removal and implantation of coracoacromial ligament can be carried out through the conventional approach of shoulder arthroscopy, without the need for graft acquisition in other parts of the body. It would avoid the pain of graft removal site of patients after operation such as iliotibial tract.
Pitfalls, Pearls, and Advantage
The disadvantage of our operation is the challenge of surgical technique and the extension of operation time. This includes arthroscopic rotator cuff quality assessment, coracoacromial ligament quality assessment, coracoacromial ligament preparing, repairing, and implantation. Because different patients may have different types of coracoacromial ligaments, intraoperative classification of coracoacromial ligaments and measurement of the size of coracoacromial ligaments are the key steps to shorten the operation time. This operation is also a big challenge to the operator. How to optimize the operation steps and shorten the operation time is the key to the next breakthrough. This is a new technique of partial thickness of rotator cuff tear combining with the autograft to release the imbalance between the injured area and intact tissues. It shows a good result from the final shoulder function and radiographs. The concept of the technique is a novel one and deserves both recognition and study. The major innovation of this technique is to use the coracoacromial ligament to reinforce the rotator cuff. The CA ligament is one of the most significant risk factors in the rotator cuff tear. So, releasing the CA ligament to reinforce the rotator cuff meets the necessities of both the short‐term and long‐term rehabilitation of the shoulder joint. Unlike other grafts, the autograft decreases the potential side effect of the implant such as the immune response to the allograft. Meanwhile, all the manipulations are direct under the arthroscopy. It is more safe and clear. Unlike other autografts, there are not any other extra incisions for implanting the autograft which cause the pain of patients. So it meets the concept of the minimally invasive treatment.
Limitation
However, it has some limitations. First, there are only three patients who had been included in this study, which does not provide enough evidence to suggest the effectiveness of this technique., Therefore, more clinical data will be needed to support the technique in further research. Secondly, the complexity of the surgery will be increased and it will raise the risk of the intraoperative infection. So it will be needed to optimize the procedure of the operation in the further research.
Conclusion
The study shows that autogenous coracoacromial ligament patch augment procedure provides good clinical results on patients with PTRCTs, with the recovery of the shoulder function and the tissue healing.
Author's Contribution
YHZ designed and initiated the trial. JYH and MZ were responsible for logistics, patient recruitment, and data collection. RY was responsible for the operating and leading. JMZ, CHZ, and YL carried out experimental design, statistical analysis plan, and writing of the manuscript. YHZ drafted the manuscript. And all the authors read and approved the final manuscript.
Conflict of Interest Statement
The authors declare no conflicts of interests.
Acknowledgments
We would like to acknowledge all members of the team for this research. This study was supported by the National Natural Science Foundation of China (no. 82002342).
Yuanhao Zhang and Min Zhou contributed equally to this work and are the co‐first authors.
References
- 1. Matthewson G, Beach CJ, Nelson AA, Woodmass JM, Ono Y, Boorman RS, et al. Partial thickness rotator cuff tears: current concepts. Adv Orthop. 2015;2015:458786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Oh JH, Lee YH, Lee TH, Jang SI, Kwon J. The natural history of high‐grade partial thickness rotator cuff tears: the conversion rate to full thickness tears and affecting factors. Clin Orthop Surg. 2020;12(4):514–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fukuda H, Hamada K, Nakajima T, Tomonaga A. Pathology and pathogenesis of the intratendinous tearing of the rotator cuff viewed from en bloc histologic sections. Clin Orthop Relat Res. 1994;304:60–7. [PubMed] [Google Scholar]
- 4. Strauss EJ, Salata MJ, Kercher J, Barker JU, McGill K, Bach BR Jr, et al. Multimedia article. The arthroscopic management of partial‐thickness rotator cuff tears: a systematic review of the literature. Arthroscopy. 2011;27(4):568–80. [DOI] [PubMed] [Google Scholar]
- 5. Xiao J, Cui GQ, Wang JQ. Diagnosis of bursal‐side partial‐thickness rotator cuff tears. Orthop Surg. 2010;2(4):260–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ellman H. Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res. 1990;254:64–74. [PubMed] [Google Scholar]
- 7. Fukuda H. The management of partial‐thickness tears of the rotator cuff. J Bone Jt Surg. 2003;85(1):3–11. [DOI] [PubMed] [Google Scholar]
- 8. Kim KC, Shin HD, Cha SM, Park JY. Repair integrity and functional outcome after arthroscopic conversion to a full‐thickness rotator cuff tear: articular‐ versus bursal‐side partial tears. Am J Sports Med. 2014;42(2):451–6. [DOI] [PubMed] [Google Scholar]
- 9. Chung SW, Kim JY, Yoon JP, Lyu SH, Rhee SM, Oh SB. Arthroscopic repair of partial‐thickness and small full‐thickness rotator cuff tears: tendon quality as a prognostic factor for repair integrity. Am J Sports Med. 2015;43(3):588–96. [DOI] [PubMed] [Google Scholar]
- 10. Rossi LA, Atala NA, Bertona A, Bongiovanni S, Tanoira I, Maignon G, et al. Long‐term outcomes after In situ arthroscopic repair of partial rotator cuff tears. Arthroscopy. 2019;35(3):698–702. [DOI] [PubMed] [Google Scholar]
- 11. Ide J, Maeda S, Takagi K. Arthroscopic transtendon repair of partial‐thickness articular‐side tears of the rotator cuff: anatomical and clinical study. Am J Sports Med. 2005;33(11):1672–9. [DOI] [PubMed] [Google Scholar]
- 12. Kim KC, Rhee KJ, Shin HD, Kim PS. Arthroscopic footprint reconstruction of bursal‐side delaminated rotator cuff tears using the suture‐bridge technique. Knee Surg Sports Traumatol Arthrosc. 2009;17(7):840–3. [DOI] [PubMed] [Google Scholar]
- 13. Wolff AB, Magit DP, Miller SR, Wyman J, Sethi PM. Arthroscopic fixation of bursal‐sided rotator cuff tears. Arthroscopy. 2006;22(11):1247.e1–4. [DOI] [PubMed] [Google Scholar]
- 14. Huberty DP, Schoolfield JD, Brady PC, Vadala AP, Arrigoni P, Burkhart SS. Incidence and treatment of postoperative stiffness following arthroscopic rotator cuff repair. Arthroscopy. 2009;25(8):880–90. [DOI] [PubMed] [Google Scholar]
- 15. Kamath G, Galatz LM, Keener JD, Teefey S, Middleton W, Yamaguchi K. Tendon integrity and functional outcome after arthroscopic repair of high‐grade partial‐thickness supraspinatus tears. J Bone Jt Surg. 2009;91(5):1055–62. [DOI] [PubMed] [Google Scholar]
- 16. Reilly P, Amis AA, Wallace AL, Emery RJ. Supraspinatus tears: propagation and strain alteration. J Shoulder Elbow Surg. 2003;12(2):134–8. [DOI] [PubMed] [Google Scholar]
- 17. Yang S, Park HS, Flores S, Levin SD, Makhsous M, Lin F, et al. Biomechanical analysis of bursal‐sided partial thickness rotator cuff tears. J Shoulder Elbow Surg. 2009;18(3):379–85. [DOI] [PubMed] [Google Scholar]
- 18. Xu W, Xue Q. Application of platelet‐rich plasma in arthroscopic rotator cuff repair: a systematic review and meta‐analysis. Orthop J Sports Med. 2021;9(7):23259671211016847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Schlegel TF, Abrams JS, Angelo RL, Getelman MH, Ho CP, Bushnell BD. Isolated bioinductive repair of partial‐thickness rotator cuff tears using a resorbable bovine collagen implant: two‐year radiologic and clinical outcomes from a prospective multicenter study. J Shoulder Elbow Surg. 2021;30(8):1938–48. [DOI] [PubMed] [Google Scholar]
- 20. Dai A, Campbell A, Bloom D, et al. Collagen‐based bioinductive implant for treatment of partial thickness rotator cuff tears. Bull Hosp Jt Dis. 2013;78(3):195–201. [PubMed] [Google Scholar]
- 21. McIntyre LF, Bishai SK, Brown PR, Bushnell BD, Trenhaile SW. Patient‐reported outcomes after use of a bioabsorbable collagen implant to treat partial and full‐thickness rotator cuff tears. Arthroscopy. 2019;35(8):2262–71. [DOI] [PubMed] [Google Scholar]
- 22. Schlegel TF, Abrams JS, Bushnell BD, Brock JL, Ho CP. Radiologic and clinical evaluation of a bioabsorbable collagen implant to treat partial‐thickness tears: a prospective multicenter study. J Shoulder Elbow Surg. 2018;27(2):242–51. [DOI] [PubMed] [Google Scholar]
- 23. Bokor DJ, Sonnabend D, Deady L, Cass B, Young A, van Kampen C, et al. Evidence of healing of partial‐thickness rotator cuff tears following arthroscopic augmentation with a collagen implant: a 2‐year MRI follow‐up. Muscles, Ligaments Tendons J. 2016;6(1):16–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wang AW, Bauer S, Goonatillake M, Breidahl W, Zheng MH. Autologous tenocyte implantation, a novel treatment for partial‐thickness rotator cuff tear and tendinopathy in an elite athlete. BMJ Case Rep. 2013;2013:bcr2012007899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wang T, Ren Z, Zhang Y, Zhao X, Liu X, Yu T, et al. Comparison of arthroscopic debridement and repair in the treatment of Ellman grade II bursal‐side partial‐thickness rotator cuff tears: a prospective randomized controlled trial. Orthop Surg. 2021;13(7):2070–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Suh D, Park SE, Han YH, Kim ES, Ji JH. Transtendon suture bridge repair of both‐sided partial‐thickness rotator cuff tears: midterm outcomes. Am J Sports Med. 2021;49(12):3202–11. [DOI] [PubMed] [Google Scholar]
- 27. Frisch KE, Marcu D, Baer GS, Thelen DG, Vanderby R. The influence of partial and full thickness tears on infraspinatus tendon strain patterns. J Biomech Eng. 2014;136(5):051004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bey MJ, Ramsey ML, Soslowsky LJ. Intratendinous strain fields of the supraspinatus tendon: effect of a surgically created articular‐surface rotator cuff tear. J Shoulder Elbow Surg. 2002;11(6):562–9. [DOI] [PubMed] [Google Scholar]
- 29. Huang CY, Wang VM, Pawluk RJ, Bucchieri JS, Levine WN, Bigliani LU, et al. Inhomogeneous mechanical behavior of the human supraspinatus tendon under uniaxial loading. J Orthop Res. 2005;23(4):924–30. [DOI] [PubMed] [Google Scholar]
- 30. Bushnell BD, Bishai SK, Krupp RJ, McMillan S, Schofield BA, Trenhaile SW, et al. Treatment of partial‐thickness rotator cuff tears with a resorbable bioinductive bovine collagen implant: 1‐year results from a prospective multicenter registry. Orthop J Sports Med. 2021;9(8):23259671211027850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rothenberg A, Gasbarro G, Chlebeck J, Lin A. The coracoacromial ligament: anatomy, function, and clinical significance. Orthop J Sports Med. 2017;5(4):2325967117703398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Alraddadi A, Alashkham A, Lamb C, Soames R. The association between coracoacromial ligament morphology and rotator cuff tears: a cadaveric study. Clin Anat. 2022;35(4):461–8. [DOI] [PubMed] [Google Scholar]
- 33. Panni AS, Milano G, Lucania L, Fabbriciani C, Logroscino CA. Histological analysis of the coracoacromial arch: correlation between age‐related changes and rotator cuff tears. Arthroscopy. 1996;12(5):531–40. [DOI] [PubMed] [Google Scholar]
- 34. Kijima H, Minagawa H, Saijo Y, Sano H, Tomioka T, Yamamoto N, et al. Degenerated coracoacromial ligament in shoulders with rotator cuff tears shows higher elastic modulus: measurement with scanning acoustic microscopy. J Orthop Sci. 2009;14(1):62–7. [DOI] [PubMed] [Google Scholar]
- 35. Kanatli U, Ayanoglu T, Aktas E, et al. Grade of coracoacromial ligament degeneration as a predictive factor for impingement syndrome and type of partial rotator cuff tear. J Shoulder Elbow Surg. 2016;25(11):1824–8. [DOI] [PubMed] [Google Scholar]
- 36. Bektaser B, Ocguder A, Solak S, et al. Free coracoacromial ligament graft for augmentation of massive rotator cuff tears treated with mini‐open repair. Acta Orthop Traumatol Turc. 2010;44(6):426–30. [DOI] [PubMed] [Google Scholar]
- 37. Bektaser SB, Yalcin N, Ocguder DA, et al. Ultrasonographic measurement of the effect of rotatory cuff repair with coracoacromial ligament transfer on humeral head migration. Eklem Hastalik Cerrahisi. 2011;22(2):89–93. [PubMed] [Google Scholar]
- 38. Taniguchi N, D'Lima DD, Suenaga N, et al. Translation of the humeral head scale is associated with success of rotator cuff repair for large‐massive tears. BMC Musculoskeletal Disord. 2017;18(1):511. [DOI] [PMC free article] [PubMed] [Google Scholar]


