Summary box.
Adolescents who are not in education, employment or training (NEET) are often left out of the health and social programming. This is a disproportionately large group in sub-Saharan Africa that has experienced extreme marginalisation during the pandemic.
Countries where young people are left behind and not cared for will struggle to achieve sustainable development and progress.
Health interventions especially psychosocial programmes and services are needed to understand their unique needs and develop responses towards bringing them back into fuller participation in various social institutions and opportunities that would build their capacities, and protect their rights.
Who is left behind?
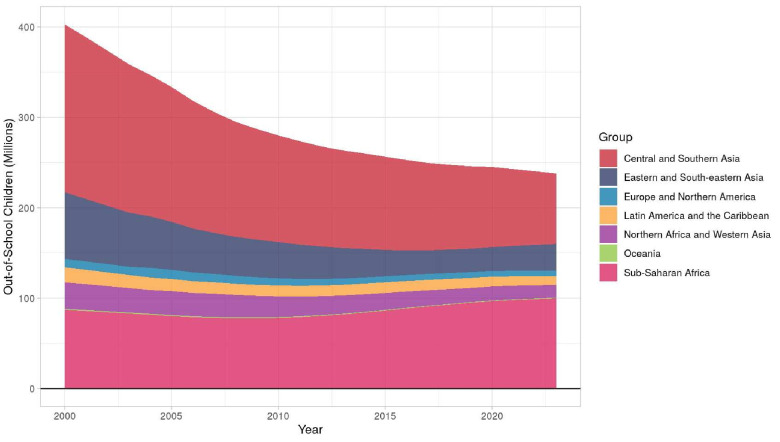
The COVID-19 pandemic has increased socioeconomic vulnerability in African populations at large and a big burden has been noticed from young people who are not in education, employment or training (NEET) as these are called. According to OECD,1 the number of 15–29 years (NEETs) remains higher than before the onset of the crisis in nearly all OECD countries which was 40.0 million in 2015. In sub-Saharan African, for example, the education exclusion rates are among the highest in the six developing world regions.2 3 The World Bank3 reports that over one-fifth of primary-age children are out of school, and almost 60% of youth between the ages of 15 and 17 are not in school. These are concerns around quality, affordable and accessible education and training programmes and the same report mentions that providing education is a source of challenge and stressor to parents. UNESCO4 5 suggests that there is an increase in this population of out of school children and youth who are falling under NEET. See figure 1 which shows that in Sub-Saharan Africa (SSA) there is a clear increase in NEET population. In a policy brief, it was highlighted that overall, 9% of primary school age children, 14% of lower secondary school age adolescents and 30% of upper secondary school age youth remain out of school. For low-income countries (many of these cover SSA region), one in three adolescents and more than one in two youth remain out of school.4 Of the 420 million young people in Africa today, more than 140 million are unemployed and another 130 million are underemployed and/or in working poverty.6
Figure 1.
Out of school rate across global regions. Source: UNESCO out of school rate (2020).
There is heterogeneity in the top causes and risk factors for overall morbidity and mortality, but trends show that injuries, mental disorders, sexual and reproductive health associated HIV/STDs impacts are the leading cause of disease burden in this demographic.7 Several reports and studies have underscored that public health, education and legal systems have not kept pace with shifting adolescent and youth needs and anticipated these rapid demographic changes.8 Lack of gender sensitive and adolescent responsive services and systems have contributed to poor educational and health outcomes in this growing demographic. What is worth keeping in mind here is that 50% of mental disorders have their onset before the age of 14 and 75% before 25.9
How do we address their unmet needs and compromised mental, sexual, reproductive health and rights that impede their well-being and quality of life?
A systematic review found significantly high prevalence of depression, anxiety disorders emotional and behavioural difficulties, post-traumatic stress and suicidal behaviour in the general adolescent population covering 16 SSA countries with significant risks of developing long-standing mental disorders in orphaned, and those living in poverty.10 Mitigating the socioeconomic determinants that increase the risk for the above difficulties in adolescents and youth (as identified in the United Nations’ SGDs) could be achieved through integrated interventions. These interventions would work closely with families and communities in the promotion of effective and accessible basic provision including education and resources to empower the population in decision-making and targeting competencies such as developmet of self-efficacy to potentially bridge their psychological, economic, sexual and reproductive health-related gaps.11–18
What is the emerging research evidence and what should we prioritize currently?
Investing in mental health promotion and preventive interventions
Promotion is an approach aimed at strengthening positive aspects of mental health and psychosocial well-being, and is focused on empowering people to live healthy life (eg, by facilitating healthy lifestyles through policies, such as providing nutritious foods in school canteens or opportunities for physical exercise in accessible locations), rather than health interventions that are solely operated by formally trained health professionals- this is about whole-of-person and whole-of-society approach.19 It includes components to foster prosocial behaviour, self-esteem, coping, decision-making capacity and includes universal interventions, such as socio-economic interventions that address people’s social determinants of health that impact their well-being.
Prevention as an approach strives to reduce the likelihood of future disorder in the general population or for individuals who are identified as being at risk of a disorder. Prevention is further subdivided on the basis of the population targeted into universal, selective and indicative.19 Selective prevention refers to strategies that are targeted to subpopulations identified as being at elevated biological, social or psychological risk for a disorder, and also populations who are asymptomatic or have very minimal symptoms. These interventions involve human, supportive and practical help covering both a social and a psychological dimension. Interventions work through communication (asking about individual needs and concerns; listening to people and helping them to feel calm and less distressed), practical support (ie, providing meals, medicine, living assistance) and with a psychological approach including teaching stress management skills and helping young people cope with other life problems.20 Interventions also involve facilitation of community support for vulnerable individuals by activating social networks and communication. Structured cultural and recreational activities support the development of resilience,19 such as traditional dancing, art work, sports and puppetry. These activities may take place in equipped settings with the aim of increasing children’s sense of connectivity and safety. Indicative prevention includes strategies that are targeted to individuals who are identified (or individually screened) as having detectable signs or symptoms which can foreshadow, precede and may sometimes, if left unaddressed, lead to a full diagnosable mental disorder based on an individual assessment.
These interventions geared towards prevention of mental disorders may be delivered at individual or group level, be offered in a variety of settings (such as during vaccination campaigns (like ones that were organized during COVID-19 pandemic, antenatal and postnatal visits, home visits, community settings, market places, schools, etc). These interventions include psychosocial support for persons with subclinical levels of mental disorders,21 at times offered in the form of mentoring programmes. These are aimed at NEET adolescents with emotional or behavioural problems; include psychological first aid for people with heightened levels of psychological distress after exposure to severe stressors, loss or bereavement. In SSA, factors as the socioecology of issues such as poverty, malnutrition, socioeconomic instability, political conflicts, including lack or poor implementation of mental health policies, poor governance of health systems, and lower political prioritization of mental health influences the epidemiological evidence, intervention outcomes and treatment strategies offered to vulnerable populations.22 23
Several studies have also pointed out issues such as missed opportunities and delays in addressing NEET raised concerns around quality and affordable education in children and youth as promised by countries following global SDG commitment. There are other concerns emerging from within the field of development economics that has questioned how policy space has not made progress in understanding the issue of NEET youth better. There are also studies from countries like Mexico24 that have found that NEET in itself can be diverse group and they may have specific MH needs that remain unaddressed and further trigger socioeconomic marginalisation. In South Africa25 it has been found that girls are more impacted by NEET and report poor mental health outcomes than boys. This is often also called as a structural problem that will impact the least educated youth the most.1
One approach is to integrate them back into social protection and health programming by building in health education—covering treatment, preventive and promotive service all together.
We would like to bring to attention a work we were involved in recently. The ‘ Bridging the Gaps’ pilot study evaluated the feasibility of integrating mental health screening and management into youth-led, lay mentor group empowerment sessions for 400 out of school adolescents (15–19 years), residing in Nairobi’s urban informal settlements. The sessions covered SRHR, gender norms, life skills, financial management, and mental health promotion and prevention. The mentors were also trained to provide one-on-one psychosocial support using the WHO Problem Management Plus intervention for adolescents deemed to be at higher risk for psychological distress. Mentors recruited adolescents into this study through door-to-door visitations of households within the pilot areas and invited adolescents to attend 18 months of weekly group sessions. The one-on-one counselling sessions spanned five consecutive weekly sessions. The intervention significantly improved Mental Health Literacy Scores of both mentors (mean difference of score +13.8) and mentees (mean difference score of +2.8), including awareness and destigmatisation of mental illness. A total of 70% of the cohort were able to freely access the individual psychological counselling sessions delivered by the community mentors. There were also improvements as seen on the General Help Seeking behaviour scores where we found statistically significant increases in adolescents reporting that they would seek help from a mental health professional or a mentor if they had a personal or emotional problem. Further evaluation needs to be carried out to measure the effectiveness of such an integrated programme.
In our work we learnt from the young people that livelihood programmes or short training courses with a strong practical component may be attractive to NEETs who cannot or will not go back to school due to lack of interest in academics, or frustrated by their previous schooling experience or, possibly, struggling with social and health issues. This demographic may include pregnant or parenting adolescents and youth including those living with chronic health conditions due to HIV, cancer, disabilities etc.
We need a focused effort towards finding solutions towards the socioeconomic marginalization that such vulnerable populations face. Only integrated programming that priortizes whole-of-health approach building in mental and behavioral health for NEET adolescents will address their increasing marginalization and lack of meaningful participation from society.
Footnotes
Twitter: @manasikumar229
Contributors: MK drafted the comment and JM and BK reviewed, edited and approved the draft.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; internally peer reviewed.
Data availability statement
Data is avaialble upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Population Council Institutional Review Board (Protocol 946) and the African Medical and Research Foundation (AMREF) Ethical and Scientific Review Committee (P916-2020). In addition, the protocol was reviewed by the Kenyan National Commission for Science, Technology and Innovation to obtain research permits for study investigators (NACOSTI/P/21/8948). Participants gave informed consent to participate in the study before taking part.
References
- 1.OECD . Society at a Glance 2019: OECD Social Indicators. Paris: OECD Publishing, 2019. [Google Scholar]
- 2.UNESCO . One in five children, adolescents and youth is out of school; 2018.
- 3.Klapper L, Panchamia MV. The high price of education in sub-Saharan Africa. n.d. Available: https://blogs.worldbank.org/developmenttalk/high-price-education-sub-saharan-africa
- 4.UNESCO . Inclusion and education: all means all. France, 2020. [Google Scholar]
- 5.UNESCO . New methodology shows that 258 million children, adolescents and youth are out of school. In: In Towards inclusion in education: status, trends and challenges: The UNESCO Salamanca Statement 25 years. Paris, France: UNESCO, 2020. [Google Scholar]
- 6.Cieslik K, Barford A, Vira B. Young people not in employment, education or training (NEET) in sub-Saharan Africa: sustainable development target 8.6 missed and reset young people not in employment, education or training. Journal of Youth Studies 2022;25:1126–47. 10.1080/13676261.2021.1939287 [DOI] [Google Scholar]
- 7.Ross DA, Mshana G, Guthold R. Tropical MED INT health - 2021- Ross- adolescent health series the health of adolescents in Sub‐Saharan Africa.Pdf. Trop Med Int Heal 2021;26:1326–32. 10.1111/tmi.13655 [DOI] [PubMed] [Google Scholar]
- 8.Azzopardi PS, Hearps SJC, Francis KL, et al. Progress in adolescent health and wellbeing: tracking 12 headline indicators for 195 countries and territories, 1990-2016. Lancet 2019;393:1101–18. 10.1016/S0140-6736(18)32427-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brits E. High mental health burden for Africa’s youth: young people in Africa are particularly at risk of mental disorders and healthcare systems are not well equipped to deal with them. Available: https://www.nature.com/articles/d44148-021-00097-y
- 10.Jörns-Presentati A, Napp A-K, Dessauvagie AS, et al. The prevalence of mental health problems in Sub-Saharan adolescents: a systematic review. PLoS One 2021;16. 10.1371/journal.pone.0251689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Musindo O, Jafry S, Nyamiobo J, et al. Mental health and Psychosocial interventions integrating sexual and reproductive rights and health, and HIV care and prevention for adolescents and young people (10-24 years) in sub-Saharan Africa: a systematic Scoping review. EClinicalMedicine 2023;57:101835. 10.1016/j.eclinm.2023.101835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alfvén T, Dahlstrand J, Humphreys D, et al. Placing children and adolescents at the centre of the sustainable development goals will deliver for current and future generations. Glob Health Action 2019;12. 10.1080/16549716.2019.1670015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Desrosiers A, Betancourt T, Kergoat Y, et al. A systematic review of sexual and reproductive health interventions for young people in humanitarian and lower-and-middle-income country settings. BMC Public Health 2020;20:1–21. 10.1186/s12889-020-08818-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vanderkruik R, Gonsalves L, Kapustianyk G, et al. Mental health of adolescents associated with sexual and reproductive outcomes: a systematic review. Bull World Health Organ 2021;99:359–373K. 10.2471/BLT.20.254144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mann M, Hosman CMH, Schaalma HP, et al. De self-esteem in a broad-spectrum approach for mental health promotion. Health Educ Res 2004;19:357–72. 10.1093/her/cyg041 [DOI] [PubMed] [Google Scholar]
- 16.Dalgaard NT, Flensborg Jensen MC, Bengtsen E, et al. PROTOCOL: group-based community interventions to support the social reintegration of Marginalised adults with mental illness. Campbell Syst Rev 2022;18. 10.1002/cl2.1254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jamali S, Sabokdast S, Sharif Nia H, et al. The effect of life skills training on mental health of Iranian middle school students: a preliminary study. Iran J Psychiatry 2016;11:269–72. [PMC free article] [PubMed] [Google Scholar]
- 18.Shenderovich Y, Boyes M, Esposti MD, et al. Relationships with caregivers and mental health outcomes among adolescents living with HIV: a prospective cohort study in South Africa. BMC Public Health 2021;21:172. 10.1186/s12889-020-10147-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Research Council, (US); Institute of Medicine, (US) . Committee on the prevention of mental disorders and substance abuse among children, youth, and young adults: research advances and promising interventions. In: O’Connell ME, Boat T, Warner K, eds. Preventing Mental, Emotional, and Behavioral Disorders Among Young People: Progress and Possibilities. 2009. [Google Scholar]
- 20.WHO . Mental health atlas. Geneva, 2021. [Google Scholar]
- 21.Purgato M, Carswell K, Acarturk C, et al. Effectiveness and cost-effectiveness of self-help plus (SH +) for preventing mental disorders in refugees and asylum seekers in Europe and Turkey: study protocols for two randomised controlled trials. BMJ Open 2019;9:1–9. 10.1136/bmjopen-2019-030259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yasamy MT, Maulik PK, Tomlinson M, et al. Responsible governance for mental health research in low resource countries. PLoS Med 2011;8:1–6. 10.1371/journal.pmed.1001126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baingana F, Becker AE, Pringle B, et al. Global research challenges and opportunities for mental health and substance-use disorders. Nature 2015;527:S172–7. 10.1038/nature16032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gutiérrez-García RA, Benjet C, Borges G, et al. Emerging adults not in education, employment or training (NEET): socio-demographic characteristics, mental health and reasons for being NEET. BMC Public Health 2018;18. 10.1186/s12889-018-6103-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sherif S, Vermaak C. NEET status and mental health in South Africa: a bidirectional longitudinal analysis; 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is avaialble upon reasonable request.