Abstract
Objective
The objective is to examine whether one of the most used instruments for measuring attitudes towards caring for dying patients, the Frommelt Attitude Toward Care of the Dying (FATCOD-B) instrument, has the same meaning across different societal contexts, as exemplified by Swedish and Saudi Arabian intensive care professionals.
Methods
A cross-sectional design used the 30-item FATCOD-B questionnaire. It was distributed to intensive care professionals from Sweden and Saudi Arabia, generating a total sample of 227 participants. Ordinal logistic regression models were used to examine the differential item functioning (DIF) for each item.
Results
Up to 12 of the 30 items were found to have significant DIF values related to: (a) Swedish and Saudi Arabian intensive care professionals, (b) Swedish and Saudi Arabian registered nurses (RNs), (c) RNs’ levels of experience and (d) RNs and other intensive care professionals in Saudi Arabia.
Conclusions
The results indicate that FATCOD should be used cautiously when comparing attitudes towards death and dying across different societal and healthcare contexts.
Keywords: Differential item functioning, Ordinal logistic regression, Attitude scale, Palliative care, Intensive care, Death and dying
1. Introduction
Offering appropriate palliative care to patients and supporting their family members is a high priority globally, regardless of the healthcare setting. Advancements in modern medicine mean that most people nowadays die in a hospital setting rather than at home [1] When critically ill patients are admitted to an intensive care unit, they are cared for in an environment characterized by a high level of specialist competence, advanced monitoring and invasive treatments, all aimed at preventing and treating organ failure and allowing patients to retain their functions and a meaningful life. While most patients in such settings are discharged alive and then go through successful recovery processes, some have limited life expectancy and may die during or shortly after leaving intensive care [2], so that end-of-life care and death are often an inevitable part of the intensive care environment. The quality of end-of-life care – care provided in the short period before death – is generally associated with palliative care, whose intent is to actively relieve patients’ distress and pain and provide support to their family members. The American Academy of Hospice and Palliative Care defines palliative care as “the active holistic care of individuals with serious health related suffering due to severe illness and especially of those near the end of life,” [3]. The same source defines severe illness as “a condition that carries a high risk of mortality, impacts quality of life and daily function, and/or is burdensome in symptoms, treatments, or caregiver stress” [3]. Thus, palliative care strives to enhance the quality of life for patients and their families. While the care has a quality component, it has challenging constraints of life expectancy prediction, especially in the context of intensive care [4].
Palliative care guidelines are based on evidence that suggests providing patients and their families with optimized care, aiming at a positive impact on care outcomes in intensive care settings [5,6]. However, some studies have suggested that palliative care is interpreted differently within an intensive care setting [[7], [8], [9]], and a recent mixed-methods systematic review of 24 studies showed that organizational and personal factors influence the integration of provision of palliative care within intensive care settings [10]. While organizational factors and leadership are important, the competence, experiences and attitudes of intensive care professionals (all personal factors) are also highlighted as important contextual elements that affect palliative care in the context of intensive care [10]. Just as the kinds of strategies used to facilitate appropriate palliative care in intensive care have a considerable effect on healthcare delivery, so may intensive care professionals' attitudes towards death and dying [11,12]. Their perspectives are linked to their knowledge about death and palliative care in intensive care settings [13,14], so there may be a need to enhance the integration of palliative care in such settings. To inform that integration, it might be beneficial to assess intensive care professionals' attitudes towards death, dying, care for patients at the end of life, the provision of quality palliative care and support for patients’ family members in intensive care settings.
Several self-assessment instruments have been developed to measure the attitudes of healthcare professionals and students who care for critically ill patients in healthcare settings [12,15]. The Frommelt Attitude Toward Care of the Dying (FATCOD-A) instrument was initially designed to determine nurses' attitudes towards providing comfort to dying patients and to evaluate the effectiveness of end-of-life care delivery [16]. It was revised 10 years later, and the current version, FATCOD-B [17], is one of the best known and most widely used instruments in relation to death and dying [18] Originally developed in the US for nursing students, FATCOD-B was created as a single-dimension scale to measure the relationship between attitudes and variables, such as experience, education and spiritual beliefs, among student nurses [19]. The instrument has been psychometrically evaluated in various international contexts, such as Sweden, Japan and China [[20], [21], [22], [23]]. However, these studies suggest multidimensionality. For example, a study in Japan showed evidence of two dimensions, the FATCOD-I factor, concerning questions relating to attitudes towards death and dying, and the FATCOD-II factor, concerning topics relating to patients and family-centred care [24]. The Swedish validation showed similar dimensions, but the Cronbach's alpha values were quite low and the authors urged caution regarding the two dimensions and use of the total score [20]. An Italian study showed as many as four dimensions [25]. Several studies using the FATCOD-B instrument have investigated the impact of educational background, spiritual beliefs and other experiences [11,26,27]. It has been shown that more positive attitudes towards death and dying are related to an increased willingness to care for patients requiring palliative care and for their families [28] and that longer professional experience leads to more positive attitudes towards death and dying [29,30]. Because the original FATCOD-B, in the US context, was unidimensional and various publications from different countries have argued for multi-dimensionality, questions arise about the cultural, professional and societal impact on the understanding of and responses to the questionnaire across and within different contexts. These questions involve both the total score and the individual items. This could be problematic, as comparisons between different professions or countries are not unusual.
While there are some cross-national similarities in the contexts of providing both intensive and palliative care, there are also notable differences [31]. For instance, in Sweden, palliative care is integrated into the national healthcare system and includes both specialized and non-specialized palliative care services available in all types of healthcare settings, including intensive care. In Saudi Arabia, on the other hand, palliative care is offered within hospital cancer centres and has cancer care as its primary focus. In Saudi Arabia, collectivism, related to Islam, is a cultural feature, while culture in Sweden appears as individualism with its cultural heritage based on Christian traditions [9], albeit with increasingly marked cultural and religious diversification in current Swedish society. In addition, family participation in patient care has been impacted by the Islamic religion in Saudi Arabia, and although family participation is promoted in Sweden, it is secondary to the primacy of the patient's autonomy [32,33]. Note, however, that both countries employ multicultural workforces in their healthcare systems [34,35].
The use of FATCOD to compare different professional groups within and between countries depends on an understanding of the possible impacts of professional background, experience and different societal contexts. Differential item functioning (DIF) analysis is a widely used method to examine whether people's interpretations of and responses to items measuring psychological constructs may be influenced by contextual factors other than the construct being measured. To our knowledge, no study has been published that evaluates DIF of the FATCOD-B across different societal and healthcare contexts of intensive care. Therefore, the current study represents the first attempt to apply DIF to the FATCOD in the context of healthcare professionals working in intensive care settings in Sweden and Saudi Arabia.
2. Aim
The aim of this study is to examine whether the FATCOD-B overall measure has the same meaning across different societal and healthcare contexts, as exemplified by intensive care professionals in Sweden and Saudi Arabia. The research questions are as follows.
-
1.
What are the distributions of the FATCOD individual item responses and the total score?
-
2.To what extent are the responses to the FATCOD items explained by the following?
-
a.Whether the respondent is a Swedish or Saudi Arabian intensive care professional
-
b.Whether the respondent is a Swedish or Saudi Arabian intensive care nurse
-
c.The level of experience of intensive care nurses
-
d.Whether the respondent is a Saudi Arabian intensive care nurse or other intensive care professional
-
a.
3. Methods
A cross-sectional survey involving respondents from Saudi Arabia and Sweden was employed.
4. Sample
The respondents were registered nurses (RNs) and other professionals involved in intensive care teams, including physicians and other allied healthcare professionals, such as respiratory therapists. The respondents were of different genders, had diverse backgrounds and nationalities, spoke different languages and had different work experience. They were recruited by convenience sampling and were all volunteers from either Sweden or Saudi Arabia. For the Swedish sample, participants were recruited through hospitals and universities and comprised critical care nurses (CCNs) and students enrolled in a critical care specialist nursing programme (second semester). For the Saudi Arabian sub-sample, participants were recruited through the Saudi Critical Care Society. Information about the respondents is provided in Table 1.
Table 1.
Characteristics of participants by country.
| Characteristics (# missing) | Saudi Cohort (N = 127) | Swedish cohort (N = 150) | Total (N = 277) |
|---|---|---|---|
| Age | |||
| Range | 22–60 | 25–68 | 22 |
| Mean (SD) | 37.5 (9.0) | 43.6 (11.6) | 40,84 |
| Gender (#1) | |||
| Male | 33% | 17% | 25% (68) |
| Female | 67% | 83% | 75% (208) |
| #missing | – | .8% (1) | .8% (1) |
| Professional (#0) | |||
| Registered nurses | 59% (75) | 79% (118) | 70% (193) |
| Registered nurses enrolled in higher education * | 0 | 21% (32) | 21% (32) |
| Physician | 12% (32) | 0 | 12% (32) |
| Respiratory therapist | 6% (16) | 0 | 6% (16) |
| Other professional** | 1%(4) | 0 | 1%(4) |
| Level of experience in the ICU (#3) | |||
| 0 years – 5years | 41% (52) | 43% (63) | 42% (115) |
| More than 5 years | 58% (74) | 57% (85) | 58% (159) |
| #Missing | .8% (1) | 1.3% (2) | 1% (3) |
| Previous education on death and dying (#0) | |||
| Course(s) in death and dying previously | 22% (28) | 16% (24) | 19% (52) |
| No specific education on death and dying, but material on the subject had been included in other courses | 47% (59) | 0 | 21% (59) |
| No education dealing with death and dying | 32% (40) | 84% (126) | 60% (166) |
| Experience in care for patients at the end of life (#0) | |||
| Previous end of life care experience | 88% (112) | 100% (150) | 95% (262) |
| No end of life care experience | 12% (15) | 0 | 5% (15) |
Note: * Registered nurses studying for a Postgraduate Diploma in Specialist Nursing in Intensive Care. ** Professionals involved dietician and physiotherapists.
4.1. Instrument
A survey was conducted using FATCOD-B, a self-administered questionnaire consisting of 30 items related to death, dying and end-of-life care, measured on a five-point Likert scale ranging from “strongly disagree” to “strongly agree”. The scale was developed in 1989 b y Frommelt [16] and later adjusted to assess the relationship between various demographic variables and attitudes, resulting in FATCOD-B.
FATCOD-B has an equal number of positive and negative items. Items that include positively worded statements are 1, 2, 4, 16, 18, 20, 21, 22, 23, 24, 25, 27 and 30 (See Table 2). The remaining items are negatively worded statements. A score of 30 or below represents an extremely negative attitude towards caring for dying patients and their families, while a score of 150 or above represents a very positive attitude [19]. FATCOD-B includes selected demographic variables, such as gender, previous education relating to death and dying, level of professional experience, previous experience of working in or dealing with end-of-life care and anticipation of losing a family member. The FATCOD-B scale was validated using content validity and a test–retest; the Cronbach's alpha value was 0.92 [19]. The FATCOD-B scale has been translated into several languages, such as Spanish, Swedish, Polish and Italian, and validated and tested in each [20,25,36]. In the Swedish, Spanish and Polish FATCOD-B samples, the Cronbach's alpha value ranged from 0.60 to 0.76 for the total scale [20,36,37]. Psychometric analysis of the Japanese version suggests two dimensions: FATCOD I (Cronbach's alpha = 0.73) containing 16 items and FATCOD II (Cronbach's alpha = 0.65) containing 13 items (Item 10 was omitted) [24]. The Italian version has four dimensions, with Cronbach's alpha values ranging from 0.11 to 0.71 [25]. In the present study, we make use of the original English version of FATCOD-B for the Saudi Arabian group and the validated Swedish version for the Swedish group.
Table 2.
Thirty FATCOD items with short descriptions of the meaning of each item.
|
FATCOD items 1–15 |
FATCOD items 16–30 |
|---|---|
| 1- Giving care to the dying person is a worthwhile experience (Care experiences) | 16- Families need emotional support to accept the behavior changes of the dying person. (Emotional support for family) |
| 2- Death is not the worst thing that can happen to a person. (There are worse things than dying) | 17- As a patient nears death, the nonfamily caregiver should withdraw from his/her involvement with the patient. (Nonfamily caregiver involvement) |
| 3- I would be uncomfortable talking about impending death with the dying person. (Uncomfortable with communication) | 18- Families should be concerned about helping their dying member make the best of his/her remaining life. (Family input into care) |
| 4- Caring for the patient's family should continue throughout the period of grief and bereavement. (Bereavement care) | 19- The dying person should not be allowed to make decisions about his/her physical care. (Dying person involvement in decision-making) |
| 5- I would not want to care for a dying person. (Uncomfortable offering care) | 20- Families should maintain as normal an environment as possible for their dying member (Maintain normality in the environment) |
| 6- The nonfamily caregivers should not be the ones to talk about death with the dying person. (Talk about death) | 21- It is beneficial for the dying person to verbalize his/her feelings. (Express feelings) |
| 7- The length of time required giving care to a dying person would frustrate me. (Lengthy duration of care) | 22- Care should extend to the family of the dying person. (Support family) |
| 8- I would be upset when the dying person I was caring for gave up hope of getting better. (Lack of hope from dying person) | 23- Caregivers should permit dying persons to have flexible visiting schedules. (Flexible visiting time) |
| 9- It is difficult to form a close relationship with the dying person. (Relationship with dying person) | 24- The dying person and his/her family should be the in-charge decision-makers. (Family authority) |
| 10- There are times when the dying person welcomes death. (Embrace death) | 25- Addiction to pain relieving medication should not be a concern when dealing with a dying person. (Pain medication) |
| 11- When a patient asks, “Am I dying?” I think it is best to change the subject to something cheerful (Ineffective Communication) | 26- I would be uncomfortable if I entered the room of a dying person and found him/her crying. (Uncomfortable with emotions) |
| 12- The family should be involved in the physical care of the dying person (Family involvement in the care) | 27- Dying persons should be given honest answers about their condition. (Honest communication) |
| 13- I would hope the person I'm caring for dies when I am not present. (Uncomfortable being present at time of death) | 28- Educating families about death and dying is not a nonfamily caregiver responsibility (Families education about death) |
| 14- I am afraid to become friends with a dying person. (Build strong relationship) | 29- Family members who stay close to a dying person often interfere with the professional's job with the patient. (Family interferes with care) |
| 15- I would want to run away when the person actually died. (Personal feelings at time of death) | 30- It is possible for nonfamily caregivers to help patients prepare for death. (Prepare for death) |
4.2. Procedures
In total, 227 participants from the two countries took part in the study. The Saudi respondent data was collected in two phases, with the first taking place at the 11th Saudi Critical Care Society conference in Riyadh in February 2020. In total, 5000 healthcare professionals attended the conference, with 293 surveys distributed at one location at the conference venue. The authors created a collection box to collect the completed questionnaires, and 89 were completed. The second data collection occurred later, with questionnaires being distributed online via the Critical Care Society to professionals who had not attended the conference. A link was sent via email from the Critical Care Society administration office to 1000 healthcare professionals who were members of the Critical Care Society. To detect possible duplicates, the online questionnaire included an item that screened potential respondents who had attended the conference and had already completed the questionnaire. The online questionnaires were issued between November 2020 and January 2021, and 38 completed questionnaires were received. The total Saudi sample thus consisted of 127 healthcare professionals working in Saudi intensive care settings.
In Sweden, the invitation to participate was sent via email to the heads of nine different intensive care settings at university and regional hospitals (levels 1–2) and to the directors of critical care specialist programmes at seven universities (including university colleges). The invitation letter contained information about the aim of the study, the data collection procedure, voluntariness and confidentiality. The questionnaire was attached to the same email. After gaining formal consent from the heads of intensive care settings and programme directors, we distributed the questionnaire as a link, together with the information letter, to potential study participants. By answering the questionnaire, the participants agreed to take part anonymously in the study. This information was published on universities’ teaching platforms for critical care students and via a weekly newsletter to CCNs. Data were subsequently collected from seven hospitals and five universities (two intensive care wards and two universities declined to participate). In total, 364 intensive care nurses and 82 nurses studying for their critical care diploma received an email with a link to an online survey. The Swedish sample consisted of 150 respondents, 118 CCNs and 32 RNs studying for critical care diplomas, while 235 CCNs and 48 students did not respond to the survey and 11 CCNs and 2 students did not complete the survey in full. The data were collected between February and March 2020 and are presented in Table 1.
4.3. Statistical analysis
Descriptive statistics were used to analyse the distribution of the FATCOD scores for the groups to be compared. To compare the level of professional experience within the nursing group, the level of experience was divided into two categories: 0–5 years of experience and more than 5 years of experience. Factor analyses were subsequently conducted to ascertain the defensibility of a single overall dimension representing the FATCOD total score, and an internal Cronbach's alpha value was computed to confirm the survey's internal consistency and reliability. The first and second eigenvalues (based on an exploratory factor analysis of polychoric correlations to accommodate the ordinal distributions) were compared to ascertain the presence of a dominant dimension. A confirmatory factor analysis (CFA) was subsequently employed using a bifactor model, with one factor representing the FATCOD overall score and two uncorrelated “methods factors” to account for dependencies among the positively and negatively worded items [38,39] The acceptable fit of the models was based on the following criteria: comparative fit index (CFI), root mean square error of approximation (RMSEA) and standardized root mean square residual (SRMR) < 0.08 [40]. The mean- and variance-adjusted weighted least squares (WLSMV) estimator was used to accommodate the ordinal item distributions. Analyses were performed with MPlus version 8.3.
DIF analysis using the ordinal logistic regression (OLR) method was conducted to examine the extent to which responses to the FATCOD items could be explained by different sample characteristics, conditional on the total score. The study used OLR analysis, as developed by Zumbo (1999) [41]. Three OLR models were used to examine DIF for each item. Model 1 involved entering the total score as the independent variable. Model 2 involved investigating uniform DIF by regressing each item on the total score and the groups being compared. Model 3 involved investigating non-uniform DIF by adding an interaction between the total score and the grouping variable. By comparing the differences in the chi-square, the −2 log-likelihood values and the Naglekerke R2 between each model, it is possible to detect non-uniform or uniform DIF or both for each item. To determine the presence of DIF, we tested for simultaneous interaction and group effects using the two degrees of freedom chi-square test. The presence of DIF was indicated by a p-value less than or equal to 0.01. The following guidelines were used to evaluate the magnitude of DIF based on differences in Naglekerke R2 values: Less than 0.035 indicates negligible DIF, 0.035–0.070 indicates moderate DIF and greater than 0.070 indicates large DIF [17].
4.4. Ethical considerations
In this study, we followed the ethical guidelines outlined in the Helsinki Declaration [42]. Respecting peoples’ autonomy, beneficence and non-malfeasance, confidentiality and justice were considered and guided the study. In addition, Swedish ethical approval was obtained from the Regional Ethical Review Board in Gothenburg (ID997-15). The participants were provided with information about the study, and voluntariness was stressed in the invitation. The head of each intensive care setting and programme directors for critical care education at the universities also consented to take part.
In Saudi Arabia, ethical approval was obtained from the Saudi Critical Care Society, thereby enabling this research to collect survey data from the conference and via the online questionnaire. At the conference, potential participants were told about the research by the first author, who was located at the society's booth and was thus able to provide written and oral information about the study and obtain the informed written consent of participants. Participants in the online survey were asked to provide informed consent prior to their participation in the survey. All responses to the questionnaire in both Sweden and Saudi Arabia were anonymous.
5. Results
5.1. Descriptive analysis
A combined total of 227 responses, including 150 intensive care RNs/postgraduate nursing students (MSc in intensive care nursing) from Sweden and 127 intensive care professionals from Saudi Arabia, were included in the study. A basic description of the respondents’ information is presented in Table 1. A high frequency of missing responses to the items was not evident among either group.
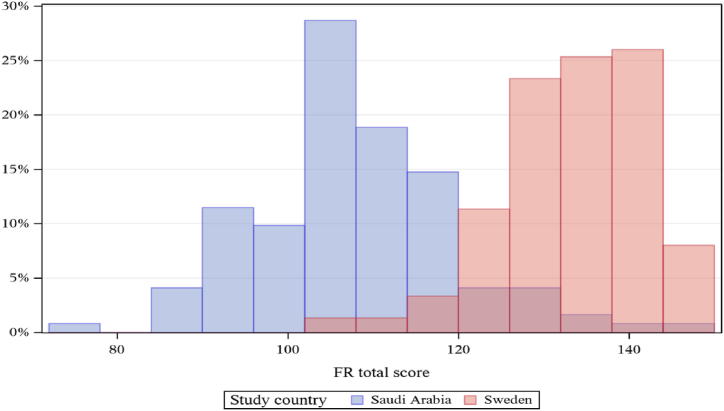
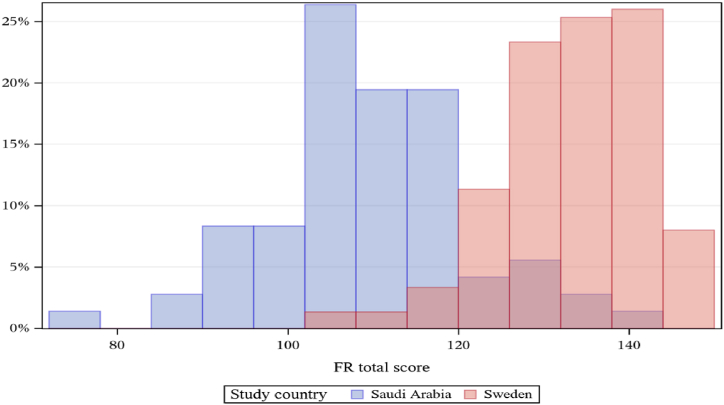
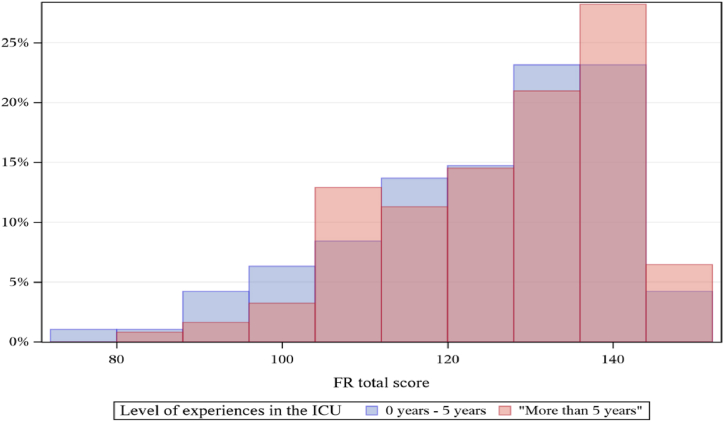
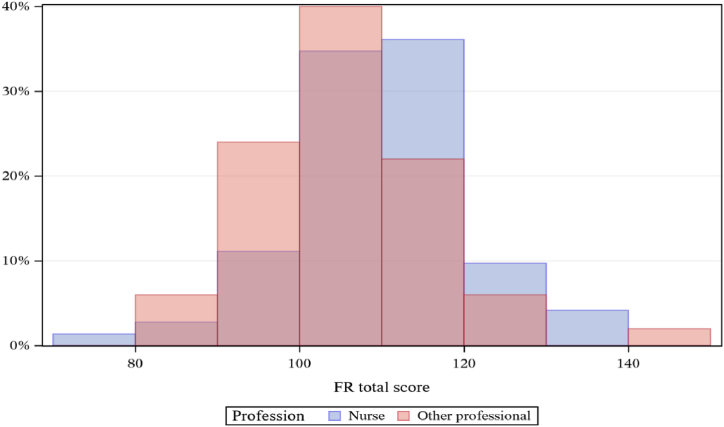
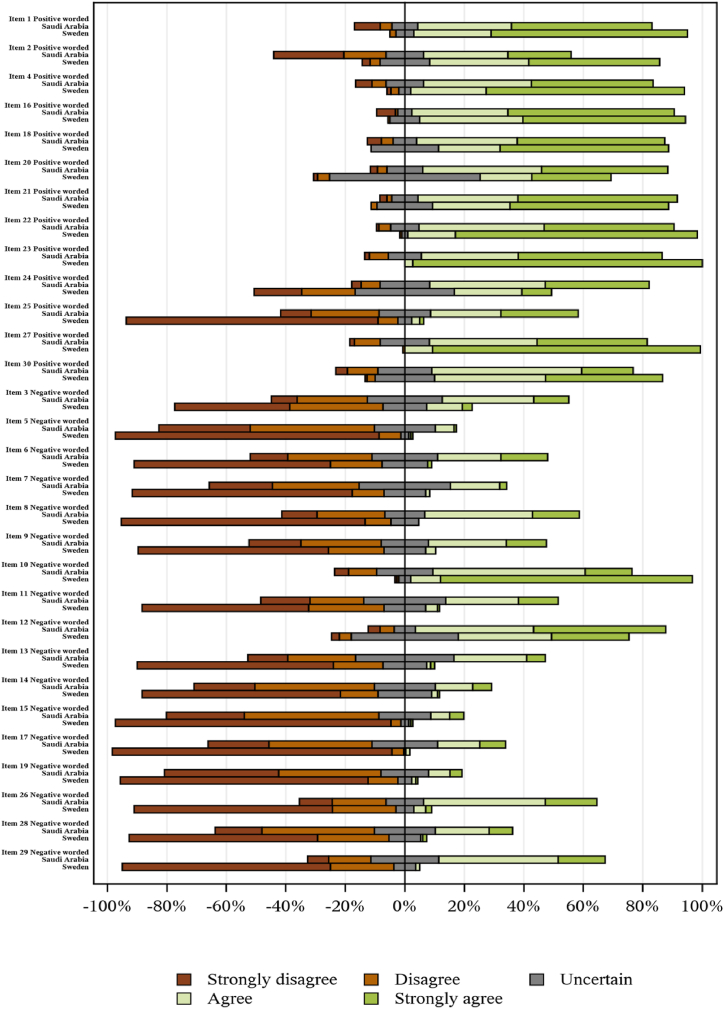
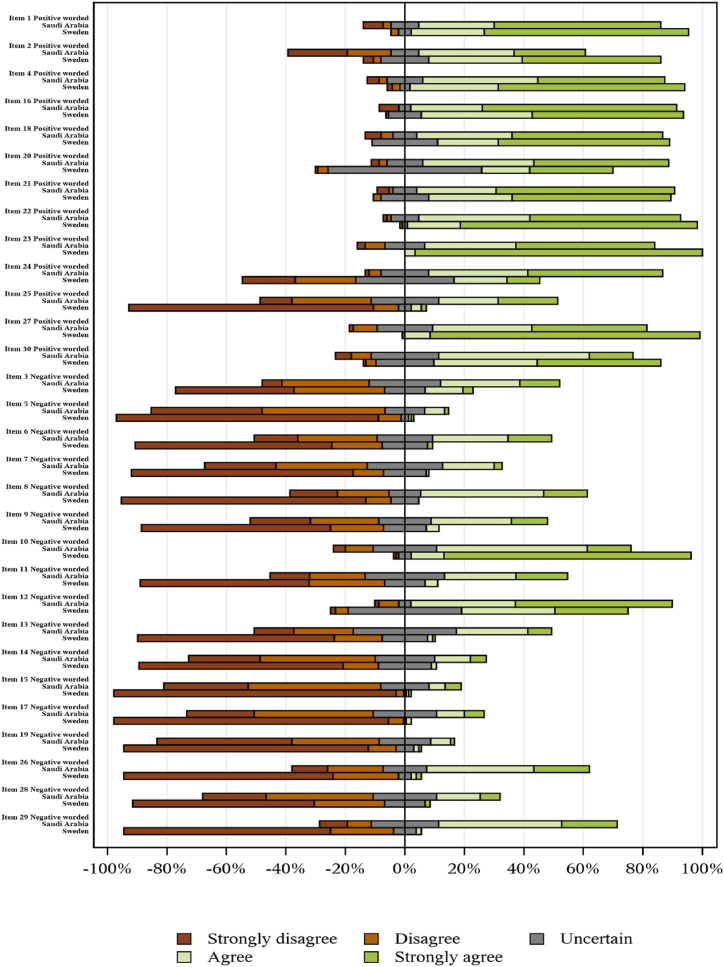
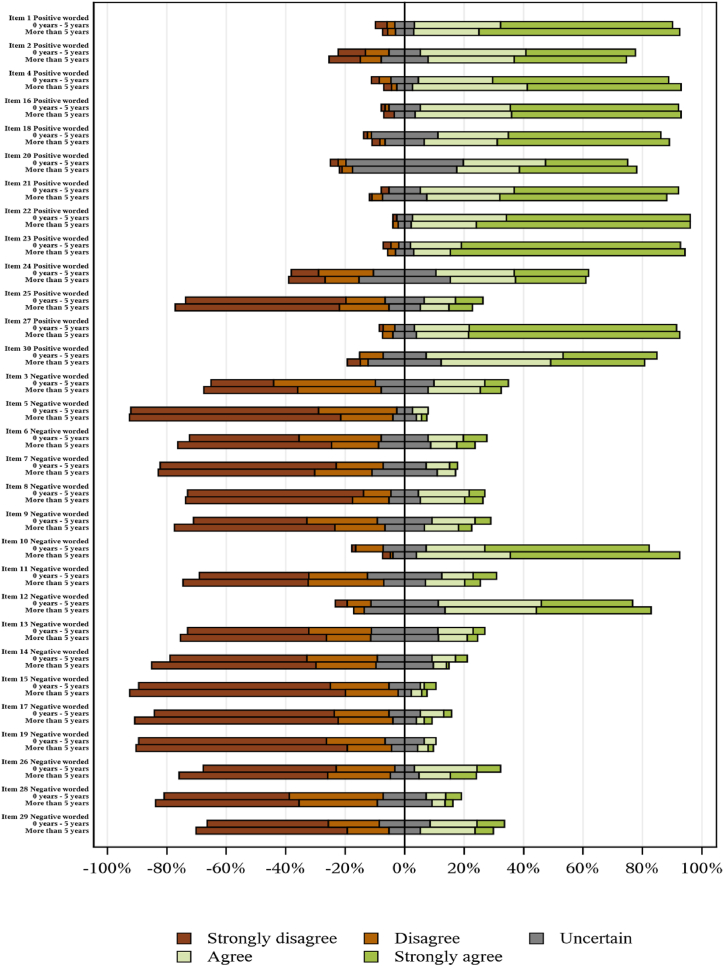
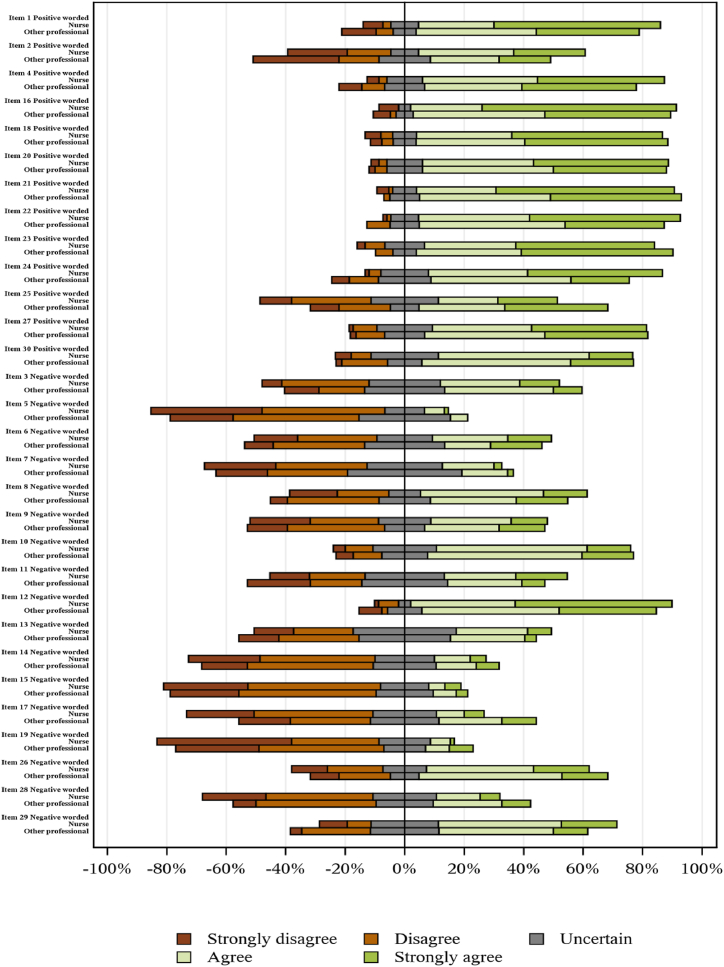
As shown in Fig. 1, the total score of the Swedish sample (mean = 133.0, median = 134, and standard deviation [std. dev.] = 8.4) was observed to be higher than that of the Saudi Arabian sample (mean = 107.5, median = 107, std. dev. = 11.7). Moreover, 193 intensive care nursing professionals responded to the FATCOD-B survey – 72 from Saudi Arabia and 118 from Sweden – and the Swedish nurses had a higher total score (mean = 132.9, median = 134.0, std. dev. = 8.3) than the Saudi nurses (mean = 109.2, median = 109.5, std. dev. = 11.8) (see Fig. 2). The level of professional experience within the RN group indicates that RNs with more than five years of experience generally scored higher (mean = 125.5, median = 128, std. dev. = 14.4) than those with five years of experience or less (mean = 121.7, median = 123, std. dev. = 16.2) (see Fig. 3). Saudi nurses generally had higher responses (mean = 109.2, median = 109.5, std. dev. = 11.8) than other health professionals (mean = 105.1, median = 105.5, std. dev. = 11.2) (see Fig. 4). The distributions of the individual items included in the FATCOD responses from all professionals from both countries are presented in Fig. 5, Fig. 6, Fig. 7, Fig. 8, showing the responses divided by country, profession and experience level.
Fig. 1.
FATCOD total score between the two groups (Sweden and Saudi Arabia) for all professional groups.
Fig. 2.
FACTOD total score between the two groups (Sweden and Saudi Arabia) for registered nurses only.
Fig. 3.
FATCOD total score between the professional experience levels of registered nurses from both countries.
Fig. 4.
FATCOD total score between the professional groups for participants from Saudi Arabia.
Fig. 5.
FATCOD distribution of items for all professional groups from both Sweden and Saudi Arabia.
Fig. 6.
FATCOD distribution of items for registered nurses only from both Sweden and Saudi Arabia.
Fig. 7.
FATCOD distribution of items for registered nurses from both countries comparing level of professional experience.
Fig. 8.
FATCOD distribution of items for Saudi Arabian professionals only comparing professional groups.
5.2. Factor analysis
The factor analysis results identified a first eigenvalue of 11.2 and a second eigenvalue of 3.3. This represents a ratio of 3.4, suggesting the presence of a dominant factor and the possibility of a few smaller factors. We subsequently specified a bifactor model by adding two uncorrelated “methods factors” to accommodate the dependencies between the positively and negatively worded items [43]. A CFA of the bifactor model resulted in an acceptable model fit (CFI = 0.945, RMSEA = 0.067, SRMR = 0.067). Taken together, the results are consistent with an overall measure for the FATCOD.
5.3. Analysis of DIF
For an overall presentation of the different items at the DIF level, as well as whether the item responses pertaining to attitudes towards death and dying were negative or positive, see Table 3 and Table 4. The different comparisons within the sample show a considerable number of items (12 of 30 items) that present a statistically significant, moderate (R2 0.035–0.070) or large DIF (R2 above 0.07) (Tables 3 and 4). In the comparison between countries (all professionals) and between Swedish and Saudi Arabian RNs, the same eight items presented a large DIF (items 12, 16, 18, 20, 21, 24, 25 and 29). Professionals from both countries showed a moderate DIF for two items (items 8 and 30), whereas RNs showed a moderate DIF for items 1, 8, 15 and 30. The RNs’ level of experience did not show any significant DIFs. For the professional groups within the Saudi Arabian sample, one item had a moderate DIF (item 25), an item that showed a large DIF in all comparisons except for professional experience level.
Table 3.
The results of Chi-square/P-value and R-square differences related to responses to FATCOD Items (1–15) from Swedish and Saudi Arabian participants.
|
FATCOD items |
Professional groups from both countries |
Registered nurses from both countries |
Level of professional experience of registered nurses from both countries |
Professional groups within the Saudi Arabian group |
||||
|---|---|---|---|---|---|---|---|---|
| R-square differences | Chi-square Differences/P-value |
R-square differences | Chi-square Differences/P-value |
R-square differences | Chi-square Differences/P-value |
R-square differences | Chi-square Differences/P-value |
|
| 1.Care experiences | 0,038 | 8203/<0.001 | 0,049 | 9281/<0.001 | 0,007 | 1389/0,249 | 0022 | 4,19/0,061 |
| 2. There are worse things than dying | 0,001 | 0108/0,473 | 0 | 1,01/0,301 | 0002 | 1,77/0,206 | 0007 | 4763/0,046 |
| 3. Uncomfortable with communication | 0 | 11,871/0,001 | 0 | 12,81/<0.001 | 0,006 | 3,08/0,107 | 0 | 1421/0,245 |
| 4. Bereavement care | 0,015 | 4475/0,053 | 0007 | 4923/0,042 | −0,007 | 1732/0,210 | 0 | 0,138/0466 |
| 5. Uncomfortable offering care | 0,002 | 6567/0,018 | 0 | 0,138/0466 | 0,004 | 9295/0,004 | 0013 | 2,22/0,164 |
| 6. Talk about death | 0,015 | 9869/0,003 | 0024 | 8953/0,005 | 0007 | 3345/0,093 | 0001 | 0,911/0317 |
| 7. Lengthy duration of care | 0,001 | 2584/0,137 | 0001 | 0,575/0375 | 0,022 | 5105/0,038 | 0001 | 2363/0,153 |
| 8. Lack of hope from dying person | 0,054 | 26,112/<0.001 | 0,061 | 20,267/<0.001 | 0,016 | 20,893/<0.001 | 0,008 | 1605/0,224 |
| 9. Relationship with dying person) | 0,001 | 3305/0,095 | 0003 | 3907/0,070 | 0007 | 6718/0,017 | 0002 | 0,479/0393 |
| 10. Embrace death | 0,012 | 43,088/<0.001 | 0,022 | 8,7/0,006 | 0001 | 1246/0,017 | 0015 | 5,73/0,028 |
| 11. Ineffective Communication) | 0,005 | 5,54/0,031 | 0013 | 3613/0,082 | 0004 | 2117/0,173 | 0032 | 5527/0,031 |
| 12- Family involvement in the care | 0,274 | 81,674/<0.001 | 0,307 | 63,769/<0.001 | 0,01 | 2522/0,141 | 0018 | 5911/0,026 |
| 13. Uncomfortable being present at time of death | 0,012 | 7719/0,010 | 0,01 | 4274/0,059 | −0,001 | 2402/0,150 | 0012 | 2247/0,162 |
| 14. Build strong relationship | 0,002 | 1409/0,247 | 0001 | 2049/0,179 | 0005 | 3769/0,075 | 0003 | 0,565/0376 |
| 15. Personal feelings at time of death | 0,029 | 15,968/0,000 | 0045 | 13,261/<0.001 | −0,002 | 1138/0,283 | 0001 | 0,438/0401 |
Table 4.
The results of Chi-square/P-value and R-square differences related to responses to FATCOD Items (16–30) from Swedish and Saudi Arabian participants.
|
FATCOD items |
Professional groups from both countries |
Registered nurses from both countries |
Level of professional experience of registered nurses from both countries |
Professional groups within the Saudi Arabian group |
||||
|---|---|---|---|---|---|---|---|---|
| R-square differences | Chi-square Differences/P-value |
R-square differences | R-square differences | R-square differences | Chi-square Differences/P-value |
R-square differences | Chi-square Differences/P-value |
|
| 16. Emotional support for family | 0,136 | 36,891/<0.001 | 0,19 | 35,757/<0.001 | −0,001 | 0012/0,497 | 0015 | 2558/0,139 |
| 17. Nonfamily caregiver involvement | 0,05 | 17,207/<0.001 | 0,032 | 10,599/0,002 | −0,001 | 1242/0,268 | 0014 | 3237/0,099 |
| 18. Family input into care | 0,096 | 26,455/<0.001 | 0,126 | 26,610/<0.001 | 0,002 | 0061/0,484 | 0009 | 4842/0,044 |
| 19. Dying person involvement in decision-making | 0,004 | 1859/0,197 | 0012 | 4,82/0,044 | 0009 | 1296/0,261 | 0008 | 1437/0,243 |
| 20. Maintain normality in the environment | 0,233 | 65,985/<0.001 | 0,254 | 48,422/<0.001 | 0,011 | 2048/0,179 | 0 | 0,135/0467 |
| 21. Express feelings | 0,119 | 31,711/<0.001 | 0,17 | 27,052/<0.001 | 0,033 | 0545/0,380 | 0003 | 2376/0,152 |
| 22. Support family | 0,005 | 5128/0,038 | 0024 | 5193/0,037 | 0006 | 2743/0,126 | 0007 | 4673/0,048 |
| 23. Flexible visiting time | 0,029 | 9699/0,003 | 0025 | 5891/0,026 | 0002 | 0,346/0430 | 0,027 | 4,21/0,060 |
| 24. Family authority | 0,279 | 85,971/<0.001 | 0,317 | 72,124/<0.001 | −0,001 | 0371/0,415 | 0035 | 6866/0,016 |
| 25. Pain medication | 0,135 | 69,654/<0.001 | 0,122 | 39,479/<0.001 | 0,005 | 0525/0,384 | 0064 | 8286/<0.001 |
| 26. Uncomfortable with emotions | 0,01 | 19,841/<0.001 | 0,016 | 16,076/<0.001 | 0 | 1669/0,217 | 0 | 0,127/0469 |
| 27. Honest communication | 0,03 | 10,36/0,002 | 0,05 | 11,393/0,001 | 0016 | 3959/0,069 | 0002 | 1647/0,219 |
| 28. Families education about death | 0 | 8232/0,008 | 0004 | 5567/0,030 | 0001 | 0,77/0,340 | 0015 | 2261/0,161 |
| 29. Family interferes with care | 0,071 | 39,224/<0.001 | 0,082 | 31,245/<0.001 | 0,001 | 1879/0,195 | 0023 | 3034/0,109 |
| 30. Prepare for death | 0,049 | 37,103/<0.001 | 0,036 | 31,818/<0.001 | 0,019 | 4241/0,059 | 0023 | 5081/0,039 |
Note: (The green FATCOD items are positively worded questions), light orange represents (Zumbo criteria, R2 values moderate (0.035–0.070), while red represents (greater than 0.070 is large). The p-value is less than or equal to 0.01.
The items with the largest DIFs primarily related to family-centred care questions: family involvement in the physical care of their loved one (item 12), emotional support for the family (item 16), the involvement of family in supporting the dying person (item 18), creating a familiar environment for the dying person (item 20), family and the dying person should be in charge of decision making (item 24) and an item concerning families’ negative interaction (interfering) with healthcare professionals (item 29). The remaining two items (items 21 and 25) covered attitudes towards patient communication and pain medication strategies with regard to possible addiction problems.
6. Discussion
This study examined the possibility of societal, professional and experience-related influences on how participants' responses to the items reflected their overall attitudes towards death and dying by using one of the most frequently used instruments to measure this construct, FATCOD-B. Research has shown that such attitudes are important prerequisites for the successful integration of palliative care outside specialized settings for such care. The present study suggests that, in terms of intensive care settings, FATCOD-B is challenging if it is intended to be used to compare results from different countries. However, differences were not observed when comparing RNs and other professional groups within the same country or when comparing RNs’ levels of experience in the two countries.
When a self-evaluative instrument is used in different populations, the general assumption is that the meanings of the items and scores are equivalent across populations. Psychometric methods, such as DIF (and, for example, response shift analysis of changes over time), are important statistical approaches for assessing this assumption for both new and existing instruments because they enable investigation of their relevance for comparisons (among, for example, countries/societies, professional groups and organizations; here, country was used as a proxy for other influencing factors). As shown in the present study, the total score for FATCOD-B initially suggests a difference in attitudes between the countries, which cannot be interpreted in light of the moderate to large differences in DIF. We found that 12 of the 30 items presented moderate to large DIF when comparing different geographical and professional populations. This demonstrates that the FATCOD-B items and corresponding scores may not have the same meaning across different societal contexts. Using FATCOD-B to compare attitudes towards death and dying across different professional groups and countries may therefore not be warranted. Still, these results do not necessarily preclude the use of FATCOD-B within a country, at least not within the same professional groups.
Palliative care aims to provide high-quality care for critically ill people at the end of life by focusing on comforting them and supporting their family members [5,6]. In view of this, it is interesting to see that the greatest DIF items (8 of 30 items) were linked to attitudes towards family-centred care, such as involvement in decision making, taking part in physical care and supporting families emotionally. This suggests that the concept of family and its involvement have different meanings in Swedish and Saudi society. However, as visualized in Fig. 8, there is a difference between professional groups, not least concerning the attitudes towards pain management strategies with regard to possible addiction problems. This could suggest that the use of FATCOD-B should be evaluated further between different professional groups, such as physicians and RNs. As pain management is a fundamental part of end-of-life palliative care, the large discrepancy regarding pain management and addiction is worth more detailed investigation, at least as the ongoing opioid crisis in many countries (including the US, Canada and Sweden) continues to challenge the healthcare system in terms of high morbidity and mortality rates [44].
When comparing participants from different countries, geographical differences are not the only ones involved. For healthcare structures, there are striking differences, with Sweden having a small number of intensive care beds (551) [45] while Saudi Arabia has many more (6,341) [46]. There are also societal and cultural differences. Although each country has a single official language (Swedish in Sweden and Arabic in Saudi Arabia), the professional language among healthcare professionals in Saudi Arabia is most often English. A third of the Saudi Arabian population consists of migrants and guest workers [47], while the Swedish population has only a fifth [48]. The religious heritage in Sweden is Christian, and current Swedish society is marked by multi-religious approaches and multiculturalism. Saudi Arabia has Islamic heritage and a healthcare system that relies on guest workers with different religious and cultural backgrounds [34,35]. All these circumstances and more result in different cultural influences affecting intensive care professionals in Sweden and Saudi Arabia.
6.1. Limitations of the study
This study has several limitations. First, the sample sizes in this study were quite small, and the number of participants was unequally divided between different professional groups, as most respondents were RNs. A discrepancy arose because only RNs were included in the Swedish sample, while RNs and other intensive care professionals (mainly physicians) were included in the Saudi sample. Second, different sampling methods were used for each group, which may have a negative influence on the findings, together with the fact that the responses from the Saudi Arabian group were collected at the beginning of the Covid-19 pandemic, which could explain the low response rate. DIF tests are usually based on larger samples than those that we used, which potentially limits the results of the study. However, as the DIF results are quite consistent, we still argue for caution when comparing the results of FATCOD-B across different countries/societies and professional groups. Although our results suggest a dominant overall dimension representing attitudes towards death and dying, further research on dimensionality is recommended.
7. Conclusions
Our findings suggest that intensive care professionals in Sweden and Saudi Arabia do not respond similarly to several FATCOD items. Consequently, the FATCOD total scores might have different meanings in Swedish and Saudi Arabian intensive care contexts and therefore may not provide a fair comparison of these populations. Further analysis of the dimensionality and measurement equivalence of the FATCOD scale is recommended, particularly in terms of the instrument's applicability and relevance as a measure of knowledge translation or integration of palliative care.
Author contribution statement
Hanan Hamdan Alshehri: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper. Joakim Öhlén: Conceived and designed the experiments; Analyzed and interpreted the data; Wrote the paper. Rick Sawatzky and Axel Wolf: Conceived and designed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper. Sepideh Olausson: Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Data availability statement
The data that has been used is confidential.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e18864.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Costa V., Earle Craig C., Esplen Mary Jane, Fowler, Robert, Goldman, Russell Grossman, Daphna Levin, Manuel Leslie, Douglas G., Sharkey Shirlee, Tanuseputro P. The determinants of home and nursing home death: a systematic review and meta-analysis. BMC Palliat. Care. 2016;15(1):1–15. doi: 10.1186/s12904-016-0077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Takaoka A H.-A., Cook D.J., Kho Michelle E. The association between frailty and short-term outcomes in an intensive care unit rehabilitation trial: an exploratory analysis. J Frailty Aging. 2021;10(1):49–55. doi: 10.14283/jfa.2020.52. [DOI] [PubMed] [Google Scholar]
- 3.Radbruch L., De Lima, Liliana F. Knaul, Wenk Roberto, Ali Zipporah, Bhatnaghar Sushma, Blanchard C., Bruera Eduardo, Buitrago Rosa, Burla Claudia. Redefining palliative care—a new consensus-based definition. J. Pain Symptom Manag. 2020;60(4):754–764. doi: 10.1016/j.jpainsymman.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marilyn J F., Cassel Christine K. In: Palliative Care: Transforming the Care of Serious Illness. Meier S.L.I. Diane E., Hughes Robert., editors. The Robort Wood Johnson Foundation: Unitied States of American; 2010. Approaching death: improving care at the end of life; p. 79. [Google Scholar]
- 5.Aslakson R.A., Curtis J.R., Nelson J.E. The changing role of palliative care in the ICU. Crit. Care Med. 2014;42(11):2418. doi: 10.1097/CCM.0000000000000573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Edwards J., Voigt Louis P., Nelson J.E. Ten key points about ICU palliative care. Intensive Care Med. 2017;43(1):83–85. doi: 10.1007/s00134-016-4481-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nelson J.E., Bassett Rick, et al. Models for structuring a clinical initiative to enhance palliative care in the intensive care unit: a report from the IPAL-ICU Project (Improving Palliative Care in the ICU) Crit. Care Med. 2010;38(9):1765. doi: 10.1097/CCM.0b013e3181e8ad23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nelson J.E., Puntillo Kathleen A., Pronovost Peter J., Walker Amy S., McAdam J.L., Ilaoa Debra, Penrod J. In their own words: patients and families define high-quality palliative care in the intensive care unit. Crit. Care Med. 2010;38(3):808–818. doi: 10.1097/ccm.0b013e3181c5887c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hart J.L., Harhay, Michael O., s N., Gabler Ratcliffe, Sarah J., Quill C.M., Halpern, Scott D. Variability among US intensive care units in managing the care of patients admitted with preexisting limits on life-sustaining therapies. JAMA Intern. Med. 2015;175(6):1019–1026. doi: 10.1001/jamainternmed.2015.0372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alshehri H., O S., Ohlen J Wolf A. Factors influencing the integration of a palliative approach in intensive care units: a systematic mixed-methods review. BMC Palliat. Care. 2020;19(1):1–18. doi: 10.1186/s12904-020-00616-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matsui M., Braun K. Nurses' and care workers' attitudes toward death and caring for dying older adults in Japan. Int. J. Palliat. Nurs. 2010;16(12):593–598. doi: 10.12968/ijpn.2010.16.12.593. [DOI] [PubMed] [Google Scholar]
- 12.Patrick D., J C., Engelberg R., Nielsen E M.E. Measuring and improving the quality of dying and death. Ann. Intern. Med. 2003;139(5 Pt 2):410–415. doi: 10.7326/0003-4819-139-5_part_2-200309021-00006. [DOI] [PubMed] [Google Scholar]
- 13.Bluck S.M., Baron E.L., Lee J. Providers' perspectives on palliative care in a neuromedicine-intensive care unit: end-of-life expertise and barriers to referral. J. Palliat. Med. 2019;22(4):364–369. doi: 10.1089/jpm.2018.0282. [DOI] [PubMed] [Google Scholar]
- 14.Morris M.M.E., Popescu C., Baron-Lee, Busl K.M. Palliative care services in the NeuroICU: opportunities and persisting barriers. Am J Hosp Palliat Care. 2021;38(11):1342–1347. doi: 10.1177/1049909120987215. [DOI] [PubMed] [Google Scholar]
- 15.Kentish-Barnes N., S V., Legriel S., Cariou A., Jaber S., Lefrant J., et al. CAESAR: a new tool to assess relatives' experience of dying and death in the ICU. Intensive Care Med. 2016;42(6):995–1002. doi: 10.1007/s00134-016-4260-4. [DOI] [PubMed] [Google Scholar]
- 16.Frommelt, Katherine The effects of death education on nurses' attitudes toward caring for terminally ill persons and their families. Am. J. Hosp. Palliat. Med. 1991;8(5):37–43. doi: 10.1177/104990919100800509. [DOI] [PubMed] [Google Scholar]
- 17.Gelin M.N., Zumbo B.D. Differential item functioning results may change depending on how an item is scored: an illustration with the Center for Epidemiologic Studies Depression Scale. Educ. Psychol. Meas. 2003;63(1):65–74. [Google Scholar]
- 18.Frey R.A., Gott Merryn, Neil Hayley. Instruments used to measure the effectiveness of palliative care education initiatives at the undergraduate level: a critical literature review. BMJ Support. Palliat. Care. 2013;3(1):114–119. doi: 10.1136/bmjspcare-2012-000306. [DOI] [PubMed] [Google Scholar]
- 19.Frommelt K.H. Attitudes toward care of the terminally ill: an educational intervention. Am J Hosp Palliat Care. 2003;20(1):13–22. doi: 10.1177/104990910302000108. [DOI] [PubMed] [Google Scholar]
- 20.Henoch I., Browall M., Melin-Johansson C., Danielson E., Udo C., Johansson Sundler A., Bjork M.E., Hammarlund K., K, Bergh S I.S. The Swedish version of the Frommelt Attitude toward Care of the Dying scale: aspects of validity and factors influencing nurses' and nursing students' attitudes. Cancer Nurs. 2014;37(1):E1–E11. doi: 10.1097/NCC.0b013e318279106b. [DOI] [PubMed] [Google Scholar]
- 21.Molinengo G., Loera Barbara, Miniotti M.L., Paolo Shortening the frommelt attitude toward the care of the dying scale (FATCOD-B): a brief 9-item version for medical education and practice. J. Cancer Educ. 2021:1–7. doi: 10.1007/s13187-021-02020-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nakanishi M., Miyamoto Y. Palliative care for advanced dementia in Japan: knowledge and attitudes. Br. J. Nurs. 2016;25(3):146–155. doi: 10.12968/bjon.2016.25.3.146. [DOI] [PubMed] [Google Scholar]
- 23.Wang L.L., Yan W., Li G. Development and psychometric testing Chinese version of the frommelt attitude toward care of the dying scale, form B in nurses and nursing students. J. Cancer Educ. 2016;31(1):123–130. doi: 10.1007/s13187-015-0810-7. [DOI] [PubMed] [Google Scholar]
- 24.Nakai Y. Factor structure and reliability of the Japanese version of the Frommelt attitude toward care of dying scale. Japanese Journal of Cancer Nursing. 2006;11(6):723–729. [Google Scholar]
- 25.Mastroianni C P.M., Taboga C., Mirabella F M.E., Casale G., Matarese M F.K., De Marinis M. Frommelt attitudes toward care of the dying scale form B: psychometric testing of the Italian version for students. Omega. 2015;70(3):227–250. doi: 10.1177/0030222815568944. [DOI] [PubMed] [Google Scholar]
- 26.Laporte P J.T., Desbiens J., Tapp D P.J., Bornet M. Factors affecting attitudes towards caring for terminally ill patients among nursing students in Switzerland: a cross-sectional study. BMJ Open. 2020;10(9) doi: 10.1136/bmjopen-2020-037553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paul S.S., Renu G., Thampi P.T. Creating a positive attitude toward dying patients among nursing students: is the current curriculum adequate? Indian J. Palliat. Care. 2019;25(1):142. doi: 10.4103/IJPC.IJPC_148_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang L., C J., Du Y., Wang Z., Li Z., Dong Z. Factors influencing Chinese nursing students' attitudes toward the care of dying patients. J. Hospice Palliat. Nurs. 2017;19(4):343–350. [Google Scholar]
- 29.Lange M., Thom Bridgette, Kline N.E. Oncology Nursing Forum. 2008. Assessing nurses' attitudes toward death and caring for dying patients in a comprehensive cancer center. [DOI] [PubMed] [Google Scholar]
- 30.Mahiro S., Takashi N., Satoko N. Work engagement and attitudes toward caring for dying patients and families among home-visiting nurses in Japan. Int. J. Palliat. Nurs. 2014;20(7):343–348. doi: 10.12968/ijpn.2014.20.7.343. [DOI] [PubMed] [Google Scholar]
- 31.Sánchez-Cárdenas M.A., et al. BMJ Supportive & Palliative Care; 2021. Palliative Care Integration Indicators: an European Regional Analysis. [DOI] [PubMed] [Google Scholar]
- 32.Palstam A., Sjödin A., Sunnerhagen K.S. Participation and autonomy five years after stroke: a longitudinal observational study. PLoS One. 2019;14(7) doi: 10.1371/journal.pone.0219513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bylund-Grenklo T., et al. Dignity in life and care: the perspectives of Swedish patients in a palliative care context. Int. J. Palliat. Nurs. 2019;25(4):193–201. doi: 10.12968/ijpn.2019.25.4.193. [DOI] [PubMed] [Google Scholar]
- 34.Albejaidi F., Nair K.S. Building the health workforce: Saudi Arabia's challenges in achieving Vision 2030. Int. J. Health Plann. Manag. 2019;34(4):e1405–e1416. doi: 10.1002/hpm.2861. [DOI] [PubMed] [Google Scholar]
- 35.Simmons C., Rodrigues R., Szebehely M. Working conditions in the long‐term care sector: a comparative study of migrant and native workers in Austria and Sweden. Health Soc. Care Community. 2022;30(5):e2191–e2202. doi: 10.1111/hsc.13657. [DOI] [PubMed] [Google Scholar]
- 36.Edo-Gual M., et al. Spanish adaptation of the frommelt attitude toward care of the dying scale (FATCOD-S) in nursing undergraduates. Omega: J. Death Dying. 2018;78(2):120–142. doi: 10.1177/0030222816688294. [DOI] [PubMed] [Google Scholar]
- 37.Sadowska A., Nowak M., Czarkowska-Pączek B. Assessment of the reliability of the Polish language version of the FATCOD-B scale among nursing students. J. Cancer Educ. 2021;36(3):561–566. doi: 10.1007/s13187-019-01665-5. [DOI] [PubMed] [Google Scholar]
- 38.Lindwall M., Barkoukis Vassilis, Grano Caterina, Lucidi F., Raudsepp Lennart, Liukkonen J. Thøgersen-ntoumani, cecilie. Method effects: The problem with negatively versus positively keyed items. Journal of personality assessment. 2012;94(2):196–204. doi: 10.1080/00223891.2011.645936. [DOI] [PubMed] [Google Scholar]
- 39.Markon K.E. Bifactor and hierarchical models: specification, inference, and interpretation. Annu. Rev. Clin. Psychol. 2019;15:51–69. doi: 10.1146/annurev-clinpsy-050718-095522. [DOI] [PubMed] [Google Scholar]
- 40.Chen F.F. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct. Equ. Model.: A Multidiscip. J. 2007;14(3):464–504. [Google Scholar]
- 41.Zumbo B.D. National Defense Headquarters; Ottawa: 1999. A Handbook on the Theory and Methods of Differential Item Functioning (DIF) pp. 1–57. [Google Scholar]
- 42.WorldMedicalAssociation . 2013. WMA Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects. [Google Scholar]
- 43.Reise S.P. The rediscovery of bifactor measurement models. Multivariate Behav. Res. 2012;47(5):667–696. doi: 10.1080/00273171.2012.715555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Berterame S., Erthal Juliana, Thomas Johny, Fellner Sarah, Vosse Benjamin, Clare Philip, Hao W., Johnson David T., Mohar Alejandro, Pavadia Jagjit. Use of and barriers to access to opioid analgesics: a worldwide, regional, and national study. Lancet. 2016;387(10028):1644–1656. doi: 10.1016/S0140-6736(16)00161-6. [DOI] [PubMed] [Google Scholar]
- 45.Svenska intensivvårdsregistret. Yearly Report. 2021 [Google Scholar]
- 46.Edelen M., T D., Teresi J., Kleinman M., Ocepek-Welikson K. Identification of differential item functioning using item response theory and the likelihood-based model comparison approach - application to the Mini-Mental State Examination. Med. Care. 2006;44(11):S134–S142. doi: 10.1097/01.mlr.0000245251.83359.8c. [DOI] [PubMed] [Google Scholar]
- 47.General Authority for Statistics . 2019. Statistical Yearbook Methodology. [Google Scholar]
- 48.Statistics Sweden . 2020. Summary of Population Statistics 1960–2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that has been used is confidential.