Abstract
Pregnancy-related acute kidney injury (AKI) is a major public health problem with substantial maternal and fetal morbidity and mortality. Women with pregnancy-related AKI require immediate access to nephrology care to prevent deleterious kidney and health outcomes. Patients with pregnancy-related AKI in low-income and lower-middle-income countries experience disparities in access to comprehensive nephrology care for many reasons. In this perspective, we highlight the burden of pregnancy-related AKI and explore the challenges among different low-income and lower-middle-income countries. The lack of adequate nephrology workforce and infrastructure for kidney health care represents a fundamental component of the problem. A shortage of nephrologists hampers the care of patients with pregnancy-related AKI leading to poor outcomes. The lack of diagnostic tools and therapeutic options, including kidney replacement therapy, impedes the implementation of effective management strategies. International efforts are warranted to empower women to get the right services and support at the right time. Dedicated preventive and early care programs are urgently needed to decrease the magnitude of pregnancy-related AKI, a complication under-represented in the literature.
Index Words: pregnancy related acute kidney injury, PRAKI, access to care, AKI
Introduction
Inviting the world to dream, the United Nations in 2012 launched the unprecedented sustainable development goals for global consultation under the banner “the world we want”. The ambitious sustainable development goals emphasized health as a core goal for international efforts aiming at sustaining healthier human lives. The world has realized that health challenges can no longer be addressed by the health sector acting alone and special emphasis should be given to reducing global inequalities.1
Health equity is a societal goal justifiable on moral grounds. An access to comprehensive health care service is a global human right, however, most people living in low-income and lower-middle-income countries are deprived of this right.2,3 Women in these countries are particularly susceptible because of a number of factors, including pregnancy- and childbirth-related issues, often not controlling economic resources, and being culturally disadvantaged.4 The lack of adequate perinatal care and inappropriate management of obstetric complications may contribute to devastating morbidities such as pregnancy-related acute kidney injury (AKI).5 Pregnancy-related AKI is a major public health problem with substantial maternal and fetal morbidity and mortality, characterized by an abrupt decline of kidney function during pregnancy and puerperium. 6, 7, 8, 9
Women with or at risk of pregnancy-related AKI should receive optimum care to prevent maternal and fetal morbidity and mortality.5 Potential disparities between high-income countries and low-income and lower-middle-income countries are due to the unavailability of health care resources including medications, medical equipment, trained professionals, dialysis infrastructure, and transportation facilities. These translate into delayed diagnosis which subsequently hinders the appropriate and timely management of pregnancy-related AKI.10,11 Complications related to pregnancy and childbirth are estimated to cause the death of about half a million women each year, of which 99% occur in low-income and middle-income countries.12 Significant efforts are urgently needed to decrease the magnitude of this problem.
In this perspective, we describe the disparities in access to health care for women with pregnancy-related AKI among different low-income and lower-middle-income countries in the world (Fig 1). We asked representative nephrologists from a selection of low-income and lower-middle-income countries to provide evidence-based answers, if available, to 4 questions regarding their countries: 1) prevalence of pregnancy-related AKI, 2) etiology, risk factors, and outcomes for pregnancy-related AKI, 3) availability of trained nephology workforce, and 4) availability of diagnostic and therapeutic tools to detect and treat pregnancy-related AKI. Our review includes 10 countries, namely, 8 African countries and 2 South-East Asian countries, classified on the basis of their gross national income per capita as presented by the World Bank’s classification: 3 low-income countries (Zambia, Democratic Republic of Congo [DRC], and Somalia), and 7 lower-middle-income countries (Egypt, Ghana, Cameroon, Zimbabwe, Nigeria, India, and Pakistan) (Table 1). Our aim is to achieve a better understanding of pregnancy-related AKI and its outcomes in low-income and lower-middle-income countries, which is a complication under-represented in the literature.
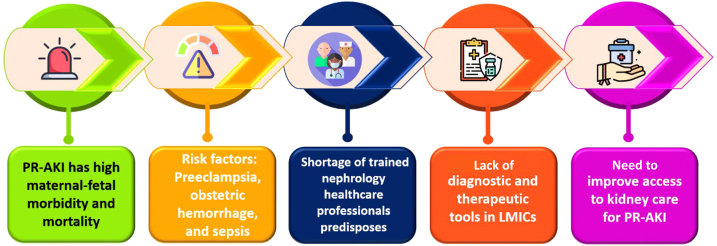
Figure 1.
Five key concepts regarding pregnancy-related AKI. Abbreviations: PR-AKI, pregnancy-related acute kidney injury; LMIC, lower-middle-income countries.
Table 1.
Comparison between participating countries in availability of PRAKI cases registry, nephrology workforce, availability of routine diagnostic tests, kidney biopsy and kidney replacement therapy modalities
| Cameroon | Democratic Republic of Congo | Egypt | Ghana | India | Nigeria | Pakistan | Somalia | Zambia | Zimbabwe | |
|---|---|---|---|---|---|---|---|---|---|---|
| Registry | n/a | reports | reports | n/a | available | reports | n/a | n/a | n/a | n/a |
| Nephrologyworkforce (pmp) | 1.1 | 0.3 | 21.6 | 0.47 | 1.86 | 0.75 | 2.2 | 0.32 | 0.52 | 0.33 |
| Routine diagnostic tools | Available | Not routinely available | Available | available in major cities | Available | Available | Available | Available in tertiary hospitals | Available at tertiary, secondary and first level | Available at tertiary centers |
| Biopsy | LM only, but rare | LM only | Available | Available | Available in all urban areas, restricted in rural areas | In areas with available nephrologists | Available | Not available | Not available | Available in private centers |
| KRT | HD available, in 8/10 regions (9 public centers, 4 private centers) | HD, PD available but costly and unevenly distributed | HD only | HD in 9/16 regions (strictly out of pocket). PD available but infrequent | HD is the primary modality available in all urban and few rural areas; PD acceptance is scarce due to financial constraints | HD available in urban only and costly; Acute PD is available in some tertiary centers but rarely used for PR-AKI | HD available majorly in urban areas; PD available but infrequent | HD only | HD available in 7/10 regions; PD available in 2 regions | HD only |
Abbreviations: KRT, Kidney replacement therapy; HD, hemodialysis; PD, peritoneal dialysis; LM, light microscopy; PR-AKI, pregnancy-related acute kidney injury; pmp, per million population; n/a, not available
Burden of Pregnancy-Related AKI in Low-Income and Lower-Middle-Income Countries
Identifying the burden of pregnancy-related AKI in each country is the initial step in problem solving, followed by exploring risk factors in each region and disparities in access to care. Provision of solutions based on the need of each country will eventually lead to improved outcomes. Unfortunately, the data about incidence and prevalence of pregnancy-related AKI in low-income and lower-middle-income countries are scarce.5 Most low-income and lower-middle-income countries lack studies reporting the national incidence of pregnancy-related AKI. Among the countries contributing to this report, only India has a national reported incidence of pregnancy-related AKI and its related outcomes. India reported a decline in pregnancy-related AKI requiring dialysis from 15% between the period 1982 and 1991 to 10% between the period 1992 and 2002, and a concurrent decrease in maternal mortality from 20% to 6.4% respectively.13 After 2010, the reported incidence of pregnancy-related AKI in India ranged from 4% to 10%.14, 15, 16 One of the largest centers from Pakistan reported that 25.6% (n=1441) of patients who presented with AKI were experiencing pregnancy-related AKI in the period from 1990 to 2014.17 Other countries like Egypt,6,18,19 Nigeria20, 21, 22 and DRC23 have a few single center reports on the incidence and outcomes of pregnancy-related AKI; however, these do not provide the national burden of pregnancy-related AKI in each country.
Risk Factors of Pregnancy-Related AKI
The early identification of risk factors of pregnancy-related AKI is a crucial step toward improving outcomes and preventing complications. Studies from Egypt revealed that lack of adequate antenatal care contributed to the development of pregnancy-related AKI. Pre-eclampsia, obstetric hemorrhages, and sepsis were the main causes of pregnancy-related AKI in Egypt. Moreover, maternal and fetal mortality rates were very high.6,18,19 In Pakistan, 1 study showed that the risk factors for pregnancy-related AKI included perinatal bleeding, placental abruption, intrauterine fetal death, sepsis, pre-eclampsia, and eclampsia. Other rare causes included surgical trauma, exposure to nephrotoxic antibiotics, and hemolysis with blood transfusion reaction.17 The same risk factors, mainly eclampsia and hemorrhage, were associated with pregnancy-related AKI in a retrospective study in Somalia.24 In India, septic abortions accounted for approximately 50% of pregnancy-related AKI in a study from Kashmir, in 2018.25 In Zambia, there has been an increasing prevalence of severe pre-eclampsia in women of childbearing age, which might contribute to the incidence of pregnancy-related AKI.26 A report from Ghana showed that postpartum hemorrhage and sepsis represented the major causes of pregnancy-related AKI, leading to dialysis in about 70% of cases.27 A systematic review including 14 African studies summarized the main causes of pregnancy-related AKI in emerging countries, which are pre-eclampsia, obstetric hemorrhage, and sepsis without substantial differences even if their definition and assessment varied across studies.5
Resources for Kidney Healthcare
Nephrology Workforce
The availability of nephrology workforce is the initial step in providing comprehensive nephrology care for patients with kidney diseases including pregnancy-related AKI. There are huge disparities in the distribution of the nephrology workforce in low-income and lower-middle-income countries, putting more strain on the already overloaded nephrology health care services. Even within a single country, regional mismatches between demand and supply exists.28 Africa has the lowest number of nephrologists per million population (pmp) in the world,2 with no or a maximum of 1 nephrologist pmp in most of the low-income and lower-middle-income countries of the continent, including Ghana, Zambia, and Nigeria, as well as South Africa, which represents one of the wealthiest countries in Africa.28
The distribution of nephrology workforce is the greatest in Egypt with 21.65 nephrologists pmp.28,29 With regard to South-East Asia, Pakistan has approximately 500 nephrologists serving a population of 220.9 million. India has one of the lowest nephrologist densities worldwide, with only about 2600 nephrologists (1.9 per million population).30
Notably, this shortage of nephrologists hampers the care of patients with pregnancy-related AKI leading to poor outcomes. Moreover, it makes referral of patients with pregnancy-related AKI exceedingly difficult in areas where nephrologists are unavailable or inadequate.
Health care professionals require optimum training to manage and prevent pregnancy-related AKI . Knowledge of non-nephrology health care workers’ regarding the broader spectrum of AKI seems deficient. The survey conducted by Kahindo et al31 in the East part of DRC revealed a significant gap between knowledge and practice among non-nephrology health care workers concerning AKI.31 Approximately 8% of health care workers with an average experience of 7 years had a good understanding of the definition and classification of AKI, while > 70% were unaware of populations at risk for AKI. This work is reproducible in other developing countries.
Adequate training of obstetricians to screen and detect kidney complications early can lead to timely referral because late referral of pregnant women developing kidney complications has been revealed as a contributing factor to poor outcomes of pregnancy-related AKI.32
Infrastructure for Nephrology Care
Priority needs to be given to prevention and early care of pregnancy-related AKI33, thereby promoting multidisciplinary care and responsibility. Screening policies with integration of serum creatinine, a basic low-cost marker of kidney function, in the routine work-up for pregnant patients has been largely advocated by the nephrology community.34 Moreover, postnatal screening is increasingly required in women who experience pregnancy complications. Special long-term screening programs should target women with prior episodes of pregnancy-related AKI and hypertensive disorders of pregnancy for early diagnosis of chronic kidney disease. Effective training programs aiming at improving the knowledge and skills of maternal health care providers should be planned to help early identification and referral of women at risk to nephrology care, particularly in high-burden countries; however, the lack of resources impedes the implementation of preventive strategies and screening programs. Late diagnosis of women with risks for pregnancy-related AKI and heterogeneity in terms of referral timing contribute to inconsistent and delayed referrals. Therefore, efforts should be intensified to maximize the awareness of health care providers regarding the optimum timing when women at risk of pregnancy-related AKI should be referred to a nephrologist.
For this reason, the Egyptian society of nephrology and transplantation is adopting an ongoing national project aimed at creating and validating consensus-based criteria for early referral of women at risk for pregnancy-related AKI to nephrology services. The consensus includes a set of simple, robust, and valid referral criteria which further aim to help health policy makers develop clinical care pathways and allocate appropriate resources.
To optimize care for women at elevated risk for pregnancy-related AKI during pregnancy or puerperium, pregnant women with current or past illness that represents a potential threat to the kidney, and women with de novo kidney problems during pregnancy or puerperium, should be referred early to a nephrologist or an obstetric nephrology service whenever available. Women with chronic kidney disease are particularly vulnerable to pregnancy-related AKI, and pregnant women with preexisting kidney disease should undertake an intensified follow-up program throughout pregnancy and puerperium. For instance, pregnant women with diabetes mellitus, current or past history of hypertensive disorders of pregnancy, immunologic diseases that potentially affect the kidney such as systemic lupus erythematosus, anatomical kidney abnormalities, and kidney donors should benefit from intensified care for both the mother and fetus according to these consensus criteria.
The accessibility of tools to diagnose and treat women with pregnancy-related AKI is essential for improving outcomes. These include diagnostic tools, pharmaceutical materials, interventions, and dialysis equipment. Nevertheless, the availability of basic diagnostic laboratory investigations, radiological workups and interventions like kidney biopsies is lacking in most low-income and lower-middle-income countries. On a global basis, obstetricians do not routinely check for serum urea and creatinine during antenatal care visits. A study conducted in Zambia found that only 35% of patients presenting with severe pre-eclampsia had laboratory results.35 The basic laboratory investigations are only routinely available at tertiary care hospitals in Zimbabwe and Somalia and about two-thirds of secondary hospitals in Ghana.36 Although diagnostic tools, imaging techniques, and kidney biopsies are widely available throughout Pakistan, there is a delay in patient referral from rural and remote areas. Egypt and India have almost full accessibility to basic laboratory tests, imaging, and kidney biopsy facilities. Nevertheless, the number of experienced nephropathologists to interpret kidney biopsies is deficient in Egypt. Of note, kidney biopsies helped to document a significant decline in the incidence of cortical necrosis from 50% in 1990 to 5%-8% in India throughout the past decade.37
Kidney Replacement Therapy
Women with pregnancy-related AKI may frequently require kidney replacement therapy (KRT). The availability of KRT techniques represents a significant problem for patients living in developing countries. Zambia per se, has hemodialysis units in 7 out of 10 regions localized to tertiary hospitals. In Zimbabwe, peritoneal dialysis (PD) is not available to manage AKI, and hemodialysis is the primary modality of KRT in private and public institutions. The dialysis prevalence in Zimbabwe is low, representing 33.4 patients pmp.38 Correspondingly, the accessibility to dialysis is still limited in Cameroon. It has been shown that nearly 28% of patients with AKI requiring dialysis in Cameron are not dialyzed due to lack of funds.39 Cameroon has 13 hemodialysis (HD) units, and 1 center for receiving acute PD which belongs to the Saving Young Living program and offers PD to children with AKI.40
In Nigeria, PD is only available rarely for women with pregnancy-related AKI requiring dialysis. HD centers are located in urban cities only, and many patients cannot afford the cost of dialysis. There is a substantial unmet need for dialysis across the country, which negatively affects the management of patients with pregnancy-related AKI requiring dialysis.41 In Somalia, only 5 HD centers are present in the 3 main cities, Mogadishu, Bosaso, and Hargeisa; 1 is a semi-private center, and the other 2 are private centers. PD is not available in Somalia.
The high cost and uneven distribution of dialysis services across DRC has greatly challenged the accessibility of dialysis.42 Masewu et al23 reported that only 6.5% of patients with AKI requiring KRT had access to dialysis.23
In Ghana, HD is the predominant modality of KRT for AKI. PD is exclusively provided by pediatric nephrologists. A study by Tannor et al showed that 9 out of the 16 administrative regions in Ghana have hemodialysis access, and therefore, manage patients with pregnancy-related AKI who require dialysis, while patients living in dialysis-lacking regions need referral to the equipped hospitals, which could lead to treatment delays and poor outcomes.43 Another barrier to accessing HD is the affordability of dialysis services. The cost of hemodialysis in Ghana is between US $45-50 per session which remains unaffordable for the average Ghanaian. Although the national health insurance is supposed to pay for the cost of dialysis for AKI, this is usually not forthcoming and difficult to access.44
In Egypt, most critically ill patients are treated in tertiary teaching hospitals; correspondingly, all the published studies were conducted at teaching hospitals where diagnostic and therapeutic facilities such as kidney biopsy, plasma exchange, and HD are relatively available.6,18,19 Hemodialysis is the primary modality in Egypt; the use of PD is presently limited due to the high cost of the treatment, the need for highly trained health care providers, and the lack of a national program to promote PD.45 Although there is no adequate data regarding the size of outpatient dialysis centers, it has been estimated that the number of dialysis machines exceeded 3000 in over 600 dialysis units in 2009.46 Of note, these centers are intended to provide dialysis services only for patients requiring long-term HD. Unlike patients receiving maintenance HD, for whom the government health insurance subsidizes Egyptian £500 for each HD session (approximately US $17),46 the situation is not that clear for patients receiving HD requiring AKI, and each center determines its own cost, which may or may not be covered by the government or insurance agencies.
In India, the most common dialysis modality available nationwide is hemodialysis. PD is restricted to the wealthy sector (8500 patients received PD in 2019).47 A report in 2018 estimated the number of HD centers in India to be 12,881 distributed among all 28 states and 8 union territories.47 However, there is significant diversity in access to HD centers, with most HD centers located in urban areas and very few in rural areas. According to estimates in the Million Death Study, about 60% of patients have to travel > 50 km to access HD centers in India.48 This adds to the financial burden related to the cost of travel. It also hinders access to care for women who are already marginalized.49
A similar trend has been reported in Pakistan, where hemodialysis is the most widely available modality of KRT, almost all in urban areas. Nevertheless, individuals living in rural areas are generally unable to receive these benefits. Presently, there are 72 public and private HD centers in urban areas of Pakistan.50 The cost of HD adds to the financial burden of the family which further hampers access to care. In Pakistan, a single session of HD costs around Rs 3,000-8,000, resulting in an average cost of Rs 550,000-700,000 per year. Notably, the reported average annual income in Pakistan is approximately Rs 320,000.51
With these barriers in mind, it is vital for governments and health authorities in developing countries to monitor the incidence of pregnancy-related AKI, TO improve obstetric care by encouraging early referral of women with or at risk of pregnancy-related AKI, to provide diagnostic and therapeutic tools for adequate management of these patients, and to ensure provision of health care services with adequately trained nephrologists (Fig 2). In India, for example, the initial decline in the incidence of pregnancy-related AKI was predominantly attributed to legislation amendments, which led to a reduction in the incidence of first-trimester septic abortions.13 Optimization of obstetric care, including better management of hemorrhagic shock and early recognition and management of pre-eclampsia, contributed to the decline in incidence of pregnancy-related AKI. Nevertheless, lack of organized delivery systems (and corresponding lack of antenatal care) has been reported in up to 30%-60% of patients with pregnancy-related AKI in India.16,32,52
Figure 2.
Recommendations for improving care for individuals with pregnancy-related AKI.
Conclusion
Pregnancy-related AKI is a major public health problem, endangering the lives of mothers and their babies, particularly those living in developing countries. Potential disparities between high-income countries and low-income and lower-middle-income countries exist because of insufficient health care resources, nephrology workforce, and infrastructure. Access to comprehensive health care is a global human right and health equity should be attained according to the United Nation’s sustainable development goals. Therefore, priority should be given to allocating resources and investments to improve health care resources in low-income and lower-middle income countries. International organizations and societies should lend a helping hand to empower women in these countries to get the right service and support at the right time.
Article Information
Authors’ Full Names and Academic Degrees
Mohamed E. Elrggal, MD, Divya Bajpai, MD, Elliot Koranteng Tannor, FWACP, Rabeea Azmat, FCPS, Ahmed Muhammad Bashir, MD, Justor Banda, PhD, Nzana Victorine B, MD, Yannick Mayamba Nlandu, MD, Bala Waziri, PhD, Winfred Baah, FWACP, Rumbidzai Dahwa, MD, and Rasha Samir Shemies, MD
Support
None.
Financial Disclosure
The authors declare that they have no relevant financial interests.
Peer Review
Received February 13, 2023. Evaluated by 2 external peer reviewers, with direct editorial input from the Editor-in-Chief. Accepted in revised form May 14, 2023.
Footnotes
Complete author and article information provided before references.
References
- 1.Marmot M., Bell R. The Sustainable Development Goals and Health Equity. Epidemiology. 2018;29:5–7. doi: 10.1097/EDE.0000000000000773. [DOI] [PubMed] [Google Scholar]
- 2.Tannor E.K., Nlandu Y.M., Elrggal M.E. Kidney Health for All–Bridging the gap to better kidney care in Africa. Afr J of Nephrol. 2022;25:108–115. [Google Scholar]
- 3.Elrggal M.E., Beg S.G., Shendi A.M., Tannor E.K., Nlandu Y.M., Gaipov A. Disparities in Access to Kidney Transplantation in Developing Countries. Transplantation. 2021;105:2325–2329. doi: 10.1097/TP.0000000000003585. [DOI] [PubMed] [Google Scholar]
- 4.Murembe N., Kyomuhangi T., Manalili K., et al. Context matters in understanding the vulnerability of women: perspectives from southwestern Uganda. Arch Public Health. 2021;79:1–4. doi: 10.1186/s13690-020-00523-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shalaby A.S., Shemies R.S. Pregnancy-related acute kidney injury in the African continent: where do we stand? A systematic review. J Nephrol. 2022;35:1–15. doi: 10.1007/s40620-022-01349-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gaber T.Z., Shemies R.S., Baiomy A.A., et al. Acute kidney injury during pregnancy and puerperium: an Egyptian hospital-based study. J Nephrology. 2021;34:1611–1619. doi: 10.1007/s40620-021-01133-8. [DOI] [PubMed] [Google Scholar]
- 7.Bentata Y., Housni B., Mimouni A., Azzouzi A., Abouqal R. Acute kidney injury related to pregnancy in developing countries: etiology and risk factors in an intensive care unit. J Nephrol. 2012;25:764–775. doi: 10.5301/jn.5000058. [DOI] [PubMed] [Google Scholar]
- 8.Hildebrand A.M., Liu K., Shariff S.Z., et al. Characteristics and outcomes of AKI treated with dialysis during pregnancy and the postpartum period. J Am Soc Nephrol. 2015;26:3085–3091. doi: 10.1681/ASN.2014100954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferreira D.P., Amorim F.F., Matsuura A.J., et al. Pregnancy-related acute kidney injury: mortality and survival of patients treated at a maternal intensive care unit. J Nephrol. 2020;33:1361–1367. doi: 10.1007/s40620-020-00711-6. [DOI] [PubMed] [Google Scholar]
- 10.Cerdá J., Bagga A., Kher V., Chakravarthi R.M. The contrasting characteristics of acute kidney injury in developed and developing countries. Nat Clin Pract Nephrol. 2008;4:138–153. doi: 10.1038/ncpneph0722. [DOI] [PubMed] [Google Scholar]
- 11.Ponce D., Balbi A. Acute kidney injury: risk factors and management challenges in developing countries. Int J Nephrol Renovasc Dis. 2016;9:193–200. doi: 10.2147/IJNRD.S104209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duley L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol. 2009;33:130–137. doi: 10.1053/j.semperi.2009.02.010. [DOI] [PubMed] [Google Scholar]
- 13.Prakash J., Kumar H., Sinha D.K., et al. Acute Renal Failure in Pregnancy in a Developing Country: Twenty Years of Experience. Renal Failure. 2006;28:309–313. doi: 10.1080/08860220600583658. Preprint at. [DOI] [PubMed] [Google Scholar]
- 14.Gopalakrishnan N., Dhanapriya J., Muthukumar P., et al. Acute kidney injury in pregnancy—a single center experience. Renal Failure. 2015;37:1476–1480. doi: 10.3109/0886022x.2015.1074493. Preprint at. [DOI] [PubMed] [Google Scholar]
- 15.Bharani R., Kumar R., Pahwa N. Post-partum acute kidney injury. Saudi J Kidney Dis Transpl. 2014;25:1244. doi: 10.4103/1319-2442.144259. Preprint at. [DOI] [PubMed] [Google Scholar]
- 16.Godara S.M., Kute V.B., Trivedi H.L., et al. Clinical profile and outcome of acute kidney injury related to pregnancy in developing countries: a single-center study from India. Saudi J Kidney Dis Transpl. 2014;25:906–911. doi: 10.4103/1319-2442.135215. Preprint at. [DOI] [PubMed] [Google Scholar]
- 17.Naqvi R., Ahmed E., Sheikh R., Rizvi A. Obstetrical acute kidney injury: 25 years’ experience from nephrology care unit in Pakistan. OAlib. 2015;02:1–7. [Google Scholar]
- 18.Emara A., Bichari W., El-Salam M.A., El-Said A.E.H. Acute kidney injury secondary to obstetric complications in the third trimester of pregnancy and the puerperium. J Egypt Soc Nephrol Transplant. 2022;22:44. doi: 10.4103/jesnt.jesnt_27_21. Preprint at. [DOI] [Google Scholar]
- 19.Elshinnawy H.A., Aref H.M., Rezk K.M., Elkotb A.M., Mohamed A.Y. Study of Pregnancy related AKI in Egyptian patients: incidence, Risk factors and Outcome. QJM: Int J Med. 2020;113 doi: 10.1093/qjmed/hcaa052.016. Preprint at. [DOI] [Google Scholar]
- 20.Awowole I.O., Omitinde O.S., Arogundade F.A., Bola-Oyebamiji S.B., Adeniyi O.A. Pregnancy-related acute kidney injury requiring dialysis as an indicator of severe adverse maternal morbidity at a tertiary center in Southwest Nigeria. Eur J Obstet Gyneco. Reprod Biol. 2018;225:205–209. doi: 10.1016/j.ejogrb.2018.04.041. [DOI] [PubMed] [Google Scholar]
- 21.Adejumo O.A., Akinbodewa A.A., Enikuomehin O.C., Lawal O.M., Abolarin O.S., Alli O.E. Pregnancy-related acute kidney injury: etiologies and short-term outcomes in a tertiary hospital in Southwest Nigeria. Saudi J Kidney Dis Transpl. 2019;30:1423–1430. doi: 10.4103/1319-2442.275487. [DOI] [PubMed] [Google Scholar]
- 22.Makusidi A.M., Liman H.M., Yakubu A., Hassan M., Isah M.D., Chiijoke A. Hemodialysis among pregnancy related acute kidney injury patients: a single center experience in North-Western Nigeria. Indian J Nephrol. 2016;26:340–342. doi: 10.4103/0971-4065.171224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Masewu A., Makulo J.R., Lepira F., et al. Acute kidney injury is a powerful independent predictor of mortality in critically ill patients: a multicenter prospective cohort study from Kinshasa, the Democratic Republic of Congo. BMC Nephrol. 2016;17:1–7. doi: 10.1186/s12882-016-0333-4. Preprint at. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Omar N.M.S., Osman M.M., Hilowle I.A., et al. Demographic Characteristics and Risk Factors Affecting the Development of Postpartum Acute Kidney Injury in Somalia: single-Center Experience. Int J Womens Health. 2022;14:881–888. doi: 10.2147/IJWH.S372453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Najar M., Shah A.R., Wani I.A., et al. Pregnancy related acute kidney injury: a single center experience from the Kashmir Valley. Indian J Nephrol. 2008;18:159. doi: 10.4103/0971-4065.45291. Preprint at. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chowa P.E., Lin C., Goma F., South-Paul J. Prevalence of Hypertension Among Women of Child Bearing Age in Zambia. Med J Zambia. 2011;38:3–8. [Google Scholar]
- 27.Affram R.K., Mate-Kole M.O. Pregnancy related acute renal failure in Ghana. Ghana Med J. 1989;23:89–91. [Google Scholar]
- 28.Sharif M.U., Elsayed M.E., Stack A.G. The global nephrology workforce: emerging threats and potential solutions. Clin Kidney J. 2016;9:11–22. doi: 10.1093/ckj/sfv111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Osman M.A., Alrukhaimi M., Ashuntantang G.E., et al. Global nephrology workforce: gaps and opportunities toward a sustainable kidney care system. Kidney Int Suppl. 2018;8:52–63. doi: 10.1016/j.kisu.2017.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bharati J., Jha V. Global Dialysis Perspective: India. Kidney360. 2020;1:1141–1145. doi: 10.34067/kid.0003982020. Preprint at. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kahindo C.K., Mukuku O., Wembonyama S.O., Tsongo Z.K. Prevalence and factors associated with acute kidney injury in sub-Saharan African adults: a review of the current literature. Int J Nephrol. 2022;2022 doi: 10.1155/2022/5621665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saini S., Chaudhury A.R., Divyaveer S., et al. The changing face of pregnancy-related acute kidney injury from eastern part of India: a hospital-based, prospective, observational study. Saudi J Kidney Dis Transplant. 2020;31:493–502. doi: 10.4103/1319-2442.284025. Preprint at. [DOI] [PubMed] [Google Scholar]
- 33.Piccoli G.B., Alrukhaimi M., Liu Z.H., Zakharova E., Levin A. Women and kidney disease: reflections on world kidney day 2018. J Ren Care. 2018;44:3–11. doi: 10.1111/jorc.12232. [DOI] [PubMed] [Google Scholar]
- 34.Piccoli G.B., Chatrenet A., Cataldo M., et al. Adding creatinine to routine pregnancy tests: a decision tree for calculating the cost of identifying patients with CKD in pregnancy. Nephrol Dial Transplant. 2023;38:148–157. doi: 10.1093/ndt/gfac051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kaunda K., Kabwe J., Phiri C., Lubeya M.K. Management of Severe Pre-eclampsia within 24hours Postpartum at a Tertiary Hospital in Lusaka, Zambia: a clinical Audit. Med J Zambia. 2021;48:108–113. [Google Scholar]
- 36.Tannor E.K., Hussein K.K., Agyei M., Boima V. Early detection of kidney disease in Ghana-a situational survey of secondary hospitals in the Ashanti Region of Ghana. African J Curr Med Res. 2021;4 [Google Scholar]
- 37.Prakash J., Vohra R., Wani I.A., et al. Decreasing incidence of renal cortical necrosis in patients with acute renal failure in developing countries: a single-centre experience of 22 years from Eastern India. Nephrol Dial Transplant. 2007;22:1213–1217. doi: 10.1093/ndt/gfl761. [DOI] [PubMed] [Google Scholar]
- 38.Dahwa R., Rutsito L., Siriwardana A.N., Nath Kumar N., Gallagher M.P. Dialysis Prevalence in Zimbabwe: a Cross-Sectional Descriptive Study. Am J Kidney Dis. 2022;80:813–816. doi: 10.1053/j.ajkd.2022.04.002. [DOI] [PubMed] [Google Scholar]
- 39.Fouda, Ashuntantang, Halle, Kaze. The epidemiology of acute kidney injury in a tertiary hospital in Cameroon: a 13 months review. J Nephrol. Ther. 2016;6:3. [Google Scholar]
- 40.Palmer D., Lawton W.J., Barrier C., Jr., et al. Peritoneal dialysis for AKI in cameroon: commercial vs locally-made solutions. Perit Dial Int. 2018;38:246–250. doi: 10.3747/pdi.2017.00190. [DOI] [PubMed] [Google Scholar]
- 41.Jones E., Rayner B.L., Effa E.E., Okpechi I.G., Schmitz M., Heering P.J. Survey on available treatment for acute kidney injury in the Southern African Development Community and Nigeria: are we ready for zero deaths by 2025 in sub-Saharan Africa? BMJ Open. 2019;9 doi: 10.1136/bmjopen-2019-029001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Izeidi P.P.M., Nlandu Y.M., Lepira F.B., et al. Cost estimate of chronic hemodialysis in Kinshasa, the Democratic Republic of the Congo: a prospective study in two centers. Hemodial. Int. 2020;24:121–128. doi: 10.1111/hdi.12802. [DOI] [PubMed] [Google Scholar]
- 43.E.K. Tannor K, Hutton-Mensah P, Opare-Addo, et al. Fifty years of hemodialysis in Ghana - current status, utilization and cost of dialysis services, Research Square; 2023, PREPRINT (Version 1). Available at: Accessed July 24, 2023. 10.21203/rs.3.rs-3017640/v1 Accessed July 24, 2023. [DOI] [PMC free article] [PubMed]
- 44.Antwi S. State of renal replacement therapy services in Ghana. Blood Purif. 2015;39:137–140. doi: 10.1159/000368942. [DOI] [PubMed] [Google Scholar]
- 45.Mahmoud K.M., Sheashaa H.A., Gheith O.A., et al. Continuous Ambulatory Peritoneal Dialysis in Egypt: progression despite Handicaps. Perit Dial Int. 2010;30:269–273. doi: 10.3747/pdi.2009.00001. Preprint at. [DOI] [PubMed] [Google Scholar]
- 46.Farag Y.M.K., El-Sayed E. Global Dialysis Perspectives: Egypt. Kidney360. 2022;3:1263–1268. doi: 10.34067/kid.0007482021. Preprint at. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jha V., Ur-Rashid H., Agarwal S.K., et al. The state of nephrology in South Asia. Kidney Int. 2019;95:31–37. doi: 10.1016/j.kint.2018.09.001. Preprint at. [DOI] [PubMed] [Google Scholar]
- 48.Dare A.J., Fu S.H., Patra J., Rodriguez P.S., Thakur J.S., Jha P. Renal failure deaths and their risk factors in India 2001–13: nationally representative estimates from the Million Death Study. Lancet Glob Health. 2017;5:e89–e95. doi: 10.1016/s2214-109x(16)30308-4. Preprint at. [DOI] [PubMed] [Google Scholar]
- 49.Shaikh M., Woodward M., John O., et al. Utilization, costs, and outcomes for patients receiving publicly funded hemodialysis in India. Kidney Int. 2018;94:440–445. doi: 10.1016/j.kint.2018.03.028. [DOI] [PubMed] [Google Scholar]
- 50.Ali Jaffar Naqvi S. Nephrology services in Pakistan. Nephrol Dial Transplant. 2000;15:769–771. doi: 10.1093/ndt/15.6.769. [DOI] [PubMed] [Google Scholar]
- 51.Imtiaz S., Alam A. Is haemodialysis the most feasible dialysis modality for Pakistan? J Pak Med Assoc. 2021;71:528–530. doi: 10.47391/JPMA.129. [DOI] [PubMed] [Google Scholar]
- 52.Prakash J., Gangier V.C., Prakash S., et al. Acute kidney injury in pregnancy with special reference to pregnancy-specific disorders: a hospital based study (2014–2016) J Nephrol. 2018;31:79–85. doi: 10.1007/s40620-017-0466-y. [DOI] [PubMed] [Google Scholar]