Abstract
A 46-year-old female with preoperative vision 6/18 N18 (LogMar 0.5) in re and posterior subcapsular cataract underwent an uneventful phacoemulsification surgery under a peribulbar block. On the postoperative day 2, she complained of no visual gain in the operated eye. The reported vision was counting fingers close to the face. Through multimodal imaging (MMI), a diagnosis of branched retinal artery occlusion (BRAO) was made. A detailed consultation and history taking with the patient revealed a concealed history of four miscarriages in the past. A detailed systemic blood workup revealed antiphospholipid antibody (APLA) positive. BRAO postuneventful cataract surgery is a devasting outcome for the surgeon and patient undergoing surgery. The report focuses on the importance of taking detailed past medical history and usage of MMI early to rule out and diagnose unexpected scenarios. We suggest BRAO in our patient was a result of emboli formation, which is a common element in APLA-positive patients.
Keywords: Antiphospholipid syndrome, branched retinal artery occlusion, cataract surgery
Introduction
One of the most commonly performed surgeries worldwide; cataract surgery comes with its own set of complications. From minor complications such as corneal edema and inflammation to vision-threatening events such as posterior capsule tear,[1] endophthalmitis,[1] lens dislocation vitreous hemorrhage, and retinal detachment,[1] cataract surgery is full of challenges and surprises in the postoperative period. One of the most baffling events is retinal artery occlusion[2] (RAO) in an uneventful cataract surgery patient. RAO is one of the rarest and most serious complications witnessed by surgeons post an uneventful cataract surgery.
RAO has been attributed either to the mechanical effect of the bolus anesthetic compound or pharmacologically mediated changes in the vascular caliber. Most of the time, the cause remains unclear.
We report a case of branched RAO (BRAO) in an uncomplicated cataract surgery patient, which on an exhaustive history taking and systemic blood work up revealed the antiphospholipid autoimmune disease. We propose and discuss that antiphospholipid antibody (APLA)-positive patients are predisposed to the formation of antibodies that lead to clot formation in arteries and veins. These, in turn, might have embolized, leading to BRAO in our patients. We believe it’s one of the first case reports of BRAO postcataract surgery associated with APLA syndrome.
Case Report
A 46-year-old female with no reported systemic history visited us with chief complaints of diminution of vision in both eyes. The best-corrected visual acuity (BCVA) in both eyes was 6/18 (LogMar 0.5) N18, with intraocular pressure (IOP) of 16 and 18 mmHg. Pupillary reactions were normal. An anterior segment examination on a slit-lamp biomicroscope revealed a posterior subcapsular cataract in both eyes, grade P4 based on the Lens Opacities Classification System III grading system.
On the fundus, examination patient had a stable posterior pole and periphery with floaters reported in both eyes.
The patient was taken up for right eye microincision cataract surgery (MICS) under peribulbar anesthesia.
The patient was dilated using tropicamide 0.8% and phenylephrine hydrochloride 5.0% having chlorbutol 0.5% as preservative. The patient was operated on under peribulbar anesthesia with lidocaine 2% (2 ml), bupivacaine 0.5% (3 ml), and hyalase. There was no sign of any retrobulbar hemorrhage. The phacoemulsification surgery was uneventful, with the lens implanted in the bag. The duration of the surgery was around 15 min. The patient was operated on a Centurion machine with active fluidics. The eye was patched after giving 1 ml of subconjunctival dexamethasone. The eye was patched after the instillation of 0.3% moxifloxacin, and the patient was reviewed the next day for bandage opening. All the blood parameters, namely, blood pressure, heart rate, and saturation during the course of surgery and postoperative period, were noted to be within the normal limits.
First, postoperative day anterior segment examination revealed few Descemet’s folds, and the anterior chamber was of normal depth. The implanted intraocular lens (IOL) was central in position and within the bag; IOP recorded was 16 mmHg. The vision was not recorded 1st postoperative day, but the patient reported significant improvement in vision. The patient was started on two hourly moxifloxacin and steroid combination, a lubricant, oral antibiotic tablet cefuroxime 500 BD (dosage), and tablet acetazolamide 250 mg TDS for the next 3 days. The patient was asked to follow-up on the 7th postoperative day.
The patient returned to us on the 4th day with the complaint of sudden painless diminution of vision. On examination, the vision was counting fingers close to the face (LogMar 1.90) which was not improving on the pinhole. The pupillary reflexes were brisk and normal, the cornea was clear with no Descemet’s folds, and the anterior chamber was well-formed with IOL in the bag.
Fundus examination showed normal optic nerve head (ONH), mild tortuosity of the vessels and a pale white reflex involving the macula and extending inferior up to the arcade [Figure 1]. A 6 mm × 6 mm swept-source optical coherence tomography angiography (SS-OCTA) (PLEX® Elite 9000; Carl Zeiss Meditec, Inc., Dublin, CA) revealed decreased perfusion and disorganization of deep vascular plexus inferior and around the fovea [Figure 2]. HD-51 B scan revealed a hyperreflective and thickened inner retina with alteration of the foveal contour. The configuration of the outer retinal layer was intact. Fundus fluorescein angiography revealed a normal arm retina time with near-normal perfusion and a diffuse leak corresponding to the involved area on SS-OCTA. Carotid Doppler was within normal range. A diagnosis of BRAO was framed.
Figure 1.

Color fundus photo showing the area of retinal whitening involving the fovea (arrow) and extending inferiorly
Figure 2.
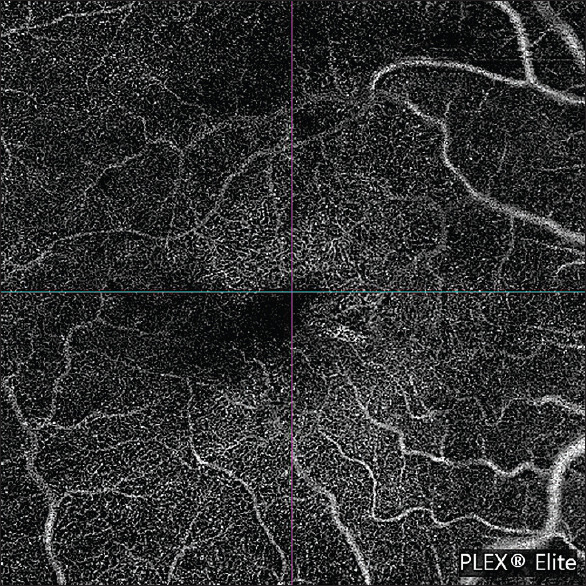
SS-OCTA 6 mm × 6 mm deep slab shows decreased perfusion and disorganization of vascular plexus around and inferior to the fovea. SS-OCTA: Swept-source optical coherence tomography angiography
The patient was taken up for a detailed past medical history. On repetitive inquiry, the patient revealed that she had a history of four miscarriages in the past 5 years. Patient reported no investigation was done for the same. A detailed blood workup was positive for the APLA.
After a rheumatologist’s opinion, the patient was started on oral wysolone (1 mg/kg body weight), tablet aspirin (100 mg daily), and injection enoxaparin (40 mg subcutaneous). Topically prednisolone 1% drops were notched up to the hourly regimen. Atropine 3% ointment was added. The patient was also advised to undergo 12 cycles of hyperbaric oxygen therapy (HBOT).
After 4 weeks and 12 cycles of HBOT, the BCVA had improved to 6/60 (LogMar 1.00). The retinal whitening area had reduced significantly. On SS-OCTA, the nonperfused area had reduced with a disorderly arrangement of vascular plexus. The inner retinal hyperreflectivity and thickness noted on the HD-51 scan previously had reduced notably [Figure 3a and b].
Figure 3.

(a) HD-51 scan shows hyperreflective and thickened inner retina with alteration of the foveal contour (yellow arrow), (b) Significant reduction in innerretinal hyperreflectivity( white arrow) and thickness noted in 4 weeks
The patient was asked to follow-up with a rheumatologist.
Discussion
We report a case of BRAO post uneventful MICS. In our opinion, the probable cause of BRAO was not caused by peribulbar block or a result of toxic effects of preservatives but was precipitated due to underlying antiphospholipid syndrome that caused the embolus for BRAO.
Cataract surgery is considered a smooth and straightforward surgery and a thorough past history is generally not taken. Our case report highlights the role of thorough and meticulous history taking for all surgical cases. The patient had a past medical history of four miscarriages which she did not disclose at the time of surgery. A detailed consultation post-BRAO with the patient revealed a history of miscarriages. Based on this, we ordered a battery of autoimmune blood tests. The patient turned out to be APLA positive and was referred to a rheumatologist. The patient also underwent 12 cycles of HBOT, which has been shown to maintain retinal oxygenation during ischemic events[3] by allowing oxygen to diffuse through choroidal capillaries that have been exposed to elevated partial pressures of oxygen. A timely initiated HBOT can reverse the ischemia-related damage.
RAO has been previously reported post uneventful cataract surgery. Most of them have been attributed to block or pharmacologically mediated changes in the vascular caliber. BRAO postphacoemulsification has been related to local anesthetic agents: [4,5,6] either due to the mechanical effect of the bolus injection or endothelial dysfunction resulting from anesthetic agents of the amide category lidocaine. Another potential cause of RAO is the suppositional effect of preservatives. As reported by Tappeiner and Garweg,[7] the toxic effect is appreciated in 2–14 days. Although our patient reported within the first 4 days of surgery, the absence of relative afferent pupillary defect and a healthy ONH[8] in the presence of positive APLA makes it unlikely to be block related.
APLA syndrome is a multisystem autoimmune disorder characterized by autoantibodies that are directed against phospholipid-binding proteins. The most common presentation of Antiphospholipid syndrome (APLS) is miscarriages and other pregnancy-related complications.[9] APLS can be fatal and can lead to transient ischemic attacks and recurrent ischemic strokes, leading to seizures and dementia.[10] One variant of APLS known as “Catastrophic APLS” has a high mortality rate of 48%. It is present in people with systemic lupus erythematosus and causes multiorgan involvement. Besides fetal loss and stroke, APLS can lead to pulmonary embolism, acute coronary syndrome, mesenteric thrombosis, or hepatic venous-occlusive disease. To prevent any thrombotic or embolic phenomenon in patients of APLS, the anticoagulation regimen should be very clearly defined. We suggest in the absence of anticoagulation due to concealed history; our patient suffered an embolic phenomenon that led to BRAO. The patient was put on aspirin and enoxaparin after the rheumatologist’s opinion.
The eyes have been considered a window to various systemic ailments, especially brain pathologies. Our case stands true to this. The patient was diagnosed as APLA positive after she suffered a BRAO episode post uneventful cataract surgery. This probably prevented a future fatal or debilitating cerebrovascular attack, pulmonary embolism, or even an acute coronary episode. The case highlights the role of prompt HBOT in cases of acute RAO, preferably within the first 24 h, that improves visual outcomes. The author suggests and presses on the role of detailed history taking and early intervention in acute RAO to avoid ocular morbidity and mortality. This helps in planning an effective treatment accordingly.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chan E, Mahroo OA, Spalton DJ. Complications of cataract surgery. Clin Exp Optom. 2010;93:379–89. doi: 10.1111/j.1444-0938.2010.00516.x. [DOI] [PubMed] [Google Scholar]
- 2.Swamy BN, Merani R, Hunyor A. Central retinal artery occlusion after phacoemulsification. Retin Cases Brief Rep. 2010;4:281–3. doi: 10.1097/ICB.0b013e3181ae7181. [DOI] [PubMed] [Google Scholar]
- 3.Hanley ME, Hendriksen S, Cooper JS. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2022. Hyperbaric Treatment Of Central Retinal Artery Occlusion. [Updated 2022 Aug 10] [PubMed] [Google Scholar]
- 4.Kumar CM, Eid H, Dodds C. Sub-Tenon's anaesthesia:Complications and their prevention. Eye (Lond) 2011;25:694–703. doi: 10.1038/eye.2011.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Azmon B, Alster Y, Lazar M, Geyer O. Effectiveness of sub-Tenon's versus peribulbar anesthesia in extracapsular cataract surgery. J Cataract Refract Surg. 1999;25:1646–50. doi: 10.1016/s0886-3350(99)00288-6. [DOI] [PubMed] [Google Scholar]
- 6.O'Donoghue E, Batterbury M, Lavy T. Effect on intraocular pressure of local anaesthesia in eyes undergoing intraocular surgery. Br J Ophthalmol. 1994;78:605–7. doi: 10.1136/bjo.78.8.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tappeiner C, Garweg JG. Retinal vascular occlusion after vitrectomy with retrobulbar anesthesia-observational case series and survey of literature. Graefes Arch Clin Exp Ophthalmol. 2011;249:1831–5. doi: 10.1007/s00417-011-1783-9. [DOI] [PubMed] [Google Scholar]
- 8.Vinerovsky A, Rath EZ, Rehany U, Rumelt S. Central retinal artery occlusion after peribulbar anesthesia. J Cataract Refract Surg. 2004;30:913–5. doi: 10.1016/j.jcrs.2003.08.021. [DOI] [PubMed] [Google Scholar]
- 9.Di Prima FA, Valenti O, Hyseni E, Giorgio E, Faraci M, Renda E, et al. Anti-phospholipid syndrome during pregnancy:The state of the art. J Prenat Med. 2011;5:41–53. [PMC free article] [PubMed] [Google Scholar]
- 10.Atanassova PA. Anti-phospholipid syndrome and vascular ischemic (occlusive) diseases:An overview. Yonsei Med J. 2007;48:901–26. doi: 10.3349/ymj.2007.48.6.901. [DOI] [PMC free article] [PubMed] [Google Scholar]


