Abstract
Objective
To examine the impact on sexual function of treatments for lower urinary tract symptoms in men.
Design
Multicentre pragmatic randomised controlled trial of standard surgery (transurethral resection of the prostate), non-contact laser therapy, and conservative management (no active intervention).
Setting
Three clinical centres in the United Kingdom.
Participants
340 men aged between 48 and 90 years with lower urinary tract symptoms related to benign prostatic enlargement.
Main outcome measures
ICSsex questionnaire items concerned with erectile stiffness, ejaculatory volume, pain or discomfort on ejaculation, whether sex life was spoilt by urinary symptoms.
Results
Erectile and ejaculatory dysfunction were common (70%) and problematic at baseline and showed the expected trends with ageing. After treatment, reduced ejaculation was reported in all groups but was not significantly worse after standard surgery than after laser therapy. Erectile function was significantly improved after standard surgery; no significant difference was found between standard surgery and laser therapy (odds ratio 0.70, 95% confidence interval 0.36 to 1.38). Standard surgery was significantly better at relieving pain or discomfort on ejaculation than either conservative management (0.06, 0.007 to 0.49) or laser therapy (0.09, 0.01 to 0.73).
Conclusions
Compared with laser therapy standard surgery for lower urinary tract symptoms has a beneficial effect on aspects of sexual function—particularly in improving erectile function and reducing reported pain or discomfort on ejaculation. Older men who need treatment and want to retain or improve sexual function may thus want to consider standard surgery rather than non-contact laser therapy.
What is already known on this topic
Troublesome lower urinary tract symptoms and erectile dysfunction are common and often problematic in older men
Standard surgical treatment for lower urinary tract symptoms (transurethral resection of the prostate) has been reported to cause greater erectile and ejaculatory dysfunction than newer less invasive treatments such as laser therapy
What this study adds
While standard surgery and laser therapy are associated with reduced ejaculation, other aspects of sexual function, particularly erectile function and pain or discomfort on ejaculation are significantly improved after standard surgery, with few new cases of impotence
Standard surgery rather than minimally invasive therapies should be considered for older men who need treatment for problematic lower urinary tract symptoms and who wish to retain or improve sexual function
Introduction
Sexual function is accepted to be an important domain of quality of life, which tends to diminish with increasing age.1–4 Population surveys have shown high levels of sexual dysfunction in men over the age of 50 years.2–5 Lower urinary tract symptoms, such as reduced stream and increased frequency, are common in older men and are often related to enlargement of the prostate gland secondary to benign prostatic hyperplasia. Recent evidence has suggested a link between symptoms and sexual dysfunction in men both in the community and attending urology clinics.3,4,6 Standard surgery (transurethral resection of the prostate—TURP) has been reported to cause sexual dysfunction, with nearly three quarters of men experiencing retrograde ejaculation and over 13% experiencing impotence after standard surgery according to a systematic review.7 Although the results had wide confidence intervals, these figures have been broadly confirmed in recent randomised trials.8
Concerns about the morbidity associated with standard surgery have led to the introduction of less invasive treatments, including laser therapy.9,10 Results of some small scale trials have shown these treatments to cause less sexual dysfunction.11–14 However, one trial of contact laser therapy compared with standard surgery concluded that these treatments resulted in similar levels of impotence.15 One major methodologically rigorous trial concluded that standard surgery did not result in more impotence than watchful waiting.16 The impact of these treatments on sexual function thus remains uncertain because of the limited power of most previous studies combined with the lack of standardisation of what constitutes sexual dysfunction and often a failure to collect baseline as well as follow up data.
We investigated self reported sexual dysfunction at baseline and follow up in men with lower urinary tract symptoms who took part in a randomised trial of standard surgery, non-contact laser therapy, and conservative management (no active intervention).17
Methods
The trial was a multicentre, pragmatic randomised controlled trial stratified by centre.17 The study had approval from ethics committees at each of the three participating centres and all patients provided written informed consent.
We included men who were attending urology clinics if they presented with uncomplicated lower urinary tract symptoms (international prostate symptom score ⩾8,18 and a maximum urinary flow rate <15 ml/s). We excluded those with a life expectancy of less than six months, evidence of prostate cancer, previous prostatic surgery, neuropathic bladder function, serum creatinine concentration >250 μmol/l, or prostate size >120 cc. We stratified patients in each centre according to degree of obstruction and randomised them to treatment by consecutive sealed opaque envelopes.17 Allocation schedules were produced with computer generated randomised permuted blocks of six for each stratum separately by a researcher not involved in patient recruitment. Blinding patients to treatment was not appropriate or possible because of the conservative (no treatment) allocation. Patients randomised to standard surgery or non-contact laser therapy were scheduled for surgery immediately. Those randomised to conservative management (monitoring without drug or other active intervention) were given general advice and bladder training. All patients were followed up at 7.5 months.
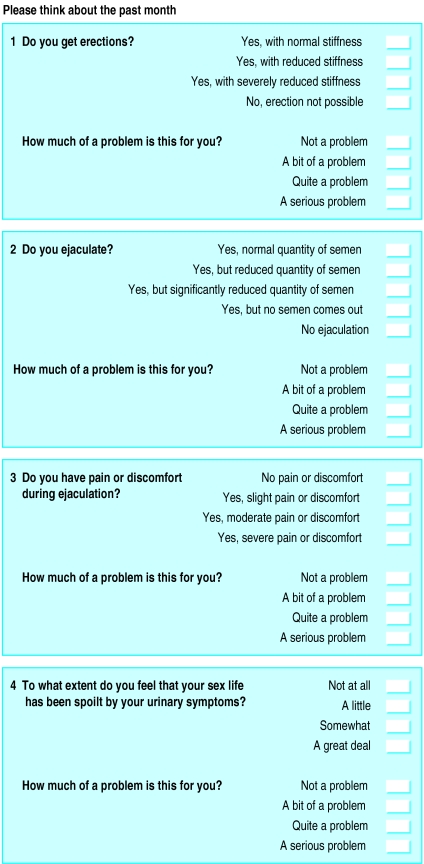
For assessment of sexual function men completed a sexual function questionnaire (International Continence Society, ICSsex, fig 1).6 For quantity of ejaculate we combined the categories of “no semen” and “no ejaculation” in all analyses because of small numbers and because the category measured the same basic dysfunction. We assessed symptoms with the validated seven item prostate symptom score18 and ICSmale questionnaires19 and quality of life for specific conditions by the single “impact on life” question attached to the prostate symptom score.
Figure 1.
ICSsex questions
We calculated the sample size to detect differences equivalent to a movement of one category along a scale of global assessment of improvement in the patient20; this corresponds to 0.43 SD on continuous outcomes such as the prostate symptom score.17 Previous research has suggested that for men undergoing conservative management the proportion reporting erectile dysfunction, ejaculatory dysfunction, pain or discomfort on ejaculation, and sex life spoilt by symptoms would be about 65%, 70%, 20%, and 45% respectively.6 A sample size of 110 per group would be large enough to detect differences of between 13% and 19% for these outcomes (with one percentage in the above range of estimated prevalences of reporting) at 80% power and a two sided 5% significance level. For the above base percentages, such differences would correspond to odds ratios of about 2.5.
Analysis
We used descriptive statistics to compare sociodemographic factors and the prevalence of sexual dysfunction across the treatment groups at randomisation and to examine the relations between the prevalence of sexual dysfunction and age at randomisation for all groups combined. We used proportional odds models with adjustment for age21 to examine the relations between sexual dysfunction and lower urinary tract symptoms at baseline. The odds ratios from these models represent the likelihood of having a worse outcome (more severe dysfunction) across the range of possible categories rather than dichotomising the outcome variable into presence or absence of dysfunction.
We used Wilcoxon matched pairs signed ranks tests (retaining the full range of responses to the questions) to examine the change in degree of dysfunction between randomisation and follow up within each of the treatment groups separately. We carried out primary comparisons between treatments on an intention to treat basis using proportional odds models to obtain odds ratios and 95% confidence intervals21 with adjustment for stratification and baseline level of the relevant outcome measure. We used a two sided 5% significance level for all outcomes for the global test across the treatment groups and the Bonferroni procedure for multiple comparisons to determine which of the three arms was significantly different from the others.22 We compared the occurrence of new cases of dysfunction after treatment between the three treatment groups using exact tests. Stata software was used for all statistical analyses.23
Results
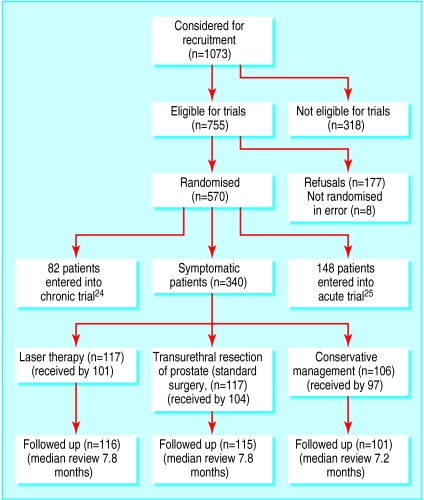
Of the 340 men recruited to the trial, 117 were randomised to standard surgery, 117 to laser therapy, and 106 to conservative management (fig 2). Baseline sociodemographic characteristics were similar between the treatment groups, as was mean age (66-67 years).17
Figure 2.
Profile of randomised trial of standard surgery, non-contact laser therapy, and conservative management
Sexual dysfunction at baseline
At baseline 298 men (88%) returned the ICSsex questionnaire. Despite the sensitive nature of the questions little information was missing (2-7% for erectile and ejaculatory function and pain or discomfort on ejaculation, 16% for sex life spoilt by urinary symptoms). The prevalence of each dysfunction and the problem caused was similar across the treatment groups at baseline. Erectile and ejaculatory dysfunction were common (reported by 70%) and became more common with increasing age (table 1). Pain or discomfort on ejaculation was less common but showed a similar relation with age, while sex life spoilt by symptoms declined with increasing age. All dysfunctions were reported to be highly problematic, particularly for younger men.
Table 1.
Levels of sexual dysfunction associated with lower urinary tract symptoms and whether this was perceived as bothersome according to age (years) at baseline. Variation in base numbers due to different numbers responding to each item
| Symptom |
No (%) with symptom
|
No (%) who were bothered by symptom
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| <60 | 60-9 | >69 | Total | <60 | 60-69 | >69 | Total | ||
| Erectile dysfunction | 20/52 (38) | 103/139 (74) | 83/99 (84) | 206/290 (71) | 19/20 (95) | 70/101 (69) | 32/81 (40) | 121/202 (60) | |
| Ejaculatory dysfunction | 22/51 (43) | 95/136 (70) | 76/90 (84) | 193/277 (70) | 12/22 (52) | 46/93 (49) | 20/75 (26) | 78/190 (41) | |
| Pain/discomfort on ejaculation | 7/51 (14) | 20/117 (17) | 15/65 (23) | 42/233 (18) | 5/7 (71) | 15/20 (75) | 11/15 (73) | 31/42 (74) | |
| Sex life spoilt by symptoms | 26/48 (54) | 49/123 (40) | 23/80 (29) | 98/251 (39) | 25/26 (96) | 43/48 (90) | 16/21 (76) | 84/95 (88) | |
Proportional odds models, adjusted for age, showed significant associations between the overall prostate symptom score and erectile dysfunction and sex life spoilt by symptoms at baseline (table 2). In both cases a higher prostate symptom score (that is, worse symptoms) was associated with more severe sexual dysfunction. No consistent relations were found between individual symptoms in the ICSmale questionnaire and sexual dysfunction, and none remained significant after we applied a Bonferroni correction for multiple significance tests.22 However, we found highly significant associations between the quality of life item on the prostate symptom score and erectile dysfunction, ejaculatory dysfunction, and sex life spoilt by symptoms (table 2).
Table 2.
Relations between sexual dysfunction and lower urinary tract symptoms at baseline adjusted for age
| Symptom |
I-PSS (symptom score)
|
I-PSS (quality of life item)
|
|||
|---|---|---|---|---|---|
| OR (95% CI)* | P value | OR (95% CI)* | P value | ||
| Erectile dysfunction | 1.04 (1.003 to 1.07) | 0.034 | 1.57 (1.28 to 1.92) | <0.0001 | |
| Ejaculatory dysfunction | 1.02 (0.99 to 1.06) | 0.19 | 1.61 (1.31 to 1.97) | <0.0001 | |
| Pain or discomfort on ejaculation | 1.02 (0.97 to 1.07) | 0.463 | 1.20 (0.89 to 1.61) | 0.23 | |
| Sex life spoilt by symptoms | 1.06 (1.02 to 1.10) | 0.004 | 1.43 (1.13 to 1.82) | 0.003 | |
Odds ratios >1 reflect higher risk of more severe dysfunction for increase of one point on I-PSS (international prostate symptom score).
Sexual dysfunction after treatment
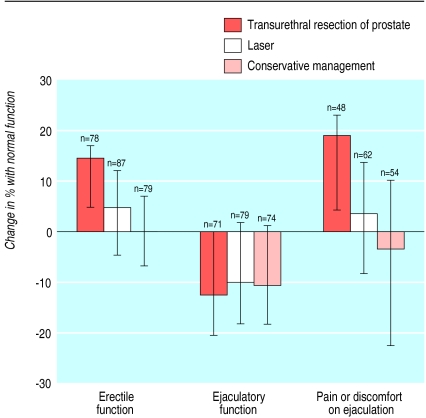
At follow up 277 men (81%) returned the ICSsex questionnaire. Table 3 shows the prevalence of sexual dysfunction within each of the treatment groups at baseline and at 7.5 month follow up. Figure 3 summarises the changes in sexual function between baseline and follow up. Analyses within groups showed that there was significant improvement in erectile function (15% increase in number with normal fuction, Wilcoxon P=0.012) and significant reduction in pain or discomfort (19% reduction in number with pain, Wilcoxon P=0.0064 ) after standard surgery. Ejaculatory function was significantly worse after all three treatments (average increase of 11% in number with dysfunction, Wilcoxon P<0.005 for all).
Table 3.
Levels of sexual dysfunction before and after treatment. Figures are numbers (percentage) of patients
|
Transurethral resection of prostate
|
Laser therapy
|
Conservative management
|
||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Follow up | Baseline | Follow up | Baseline | Follow up | |||
| Erectile dysfunction | 69 (70) | 47 (55)* | 71 (71) | 64 (66) | 73 (67) | 61 (72) | ||
| Ejaculatory dysfunction | 67 (70) | 68 (83)* | 70 (76) | 80 (86) | 57 (64) | 60 (73) | ||
| Pain on ejaculation | 14 (17) | 1 (2)* | 14 (18) | 16 (20) | 14 (19) | 17 (27) | ||
| Sex life spoilt by symptoms | 37 (43) | 34 (46) | 29 (33) | 38 (44) | 32 (42) | 36 (51) | ||
Significant change in dysfunction within groups between baseline and follow up (Wilcoxon P<0.02).
Figure 3.
Change in percentage (95% confidence intervals) of men who responded to item at baseline and follow up with normal function after treatment (positive change indicates an improvement). Confidence intervals, provided for descriptive purposes only and based on exact methods with data dichotomised within each group, do not yield identical findings to either Wilcoxon P values quoted in text or primary (between group) comparisons from proportional odds models that use ordinal response data
Table 4 shows the primary results between groups of proportional odds models with adjustment for centre and baseline level of dysfunction. Overall, there were significant differences between the treatment groups for each of the dysfunctions but not for sex life spoilt by symptoms. Men who had standard surgery were significantly more likely to have improved erectile function than those who had conservative management, while the comparison between standard surgery and laser was not significant (odds ratio 0.70, 95% confidence interval 0.36 to 1.38). Men who had standard surgery were also significantly less likely to report pain or discomfort during ejaculation than those who had laser or conservative management. Ejaculatory function was significantly worse among those who had standard surgery rather than conservative management. The apparently higher levels of ejaculatory dysfunction after standard surgery compared with laser were marginally significant (2.00, 1.03 to 3.87). This significance disappeared after adjustment for multiple comparisons; none of the other findings were altered. Adjustment for age did not materially affect any results.
Table 4.
Differences in sexual dysfunction at follow up in treatment groups, adjusted for centre and relevant baseline measurement
|
Erectile dysfunction
|
Ejaculatory dysfunction
|
Pain or discomfort on ejaculation
|
||||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI)* | P value‡ | OR (95% CI)† | P value‡ | OR (95% CI)* | P value‡ | |||
| TURP v conservative management | 0.37 (0.19 to 0.74) | 0.014 | 3.27 (1.69 to 6.35) | 0.0017 | 0.06 (0.007 to 0.49) | 0.0013 | ||
| Laser v conservative management | 0.53 (0.28 to 1.01) | 1.64 (0.91 to 2.97) | 0.70 (0.26 to 1.93) | |||||
| TURP v laser | 0.70 (0.36 to 1.38) | 2.00 (1.03 to 3.87) | 0.09 (0.01 to 0.73) | |||||
TURP=transurethral resection of prostate (standard surgery).
Odds ratios <1 reflect lower risk of more severe dysfunction for first treatment group compared with second.
Odds ratios >1 reflect higher risk of more severe dysfunction for first treatment group compared with second.
For global tests of treatment differences.
New cases of sexual dysfunction
We investigated new cases of sexual dysfunction among those who had reported “no dysfunction” at baseline. After standard surgery only one man (5% of those reporting no dysfunction at baseline) reported new erectile dysfunction, and only three (5% of those reporting potency at baseline) indicated impotence (defined here as erection not possible) at follow up. Corresponding figures for the other two groups were five (20%) and six (8%) for laser therapy and four (20%) and seven (10%) for conservative management (exact P=0.30 and 0.61 for the comparisons between the three groups for erectile dysfunction and impotence respectively). New cases of ejaculatory dysfunction were also not significantly different between the groups (exact P=0.26), with 12 (43%) such cases for conservative management, 13 (62%) for standard surgery, and 13 (65%) for laser therapy. There was one (3%) new case of pain or discomfort during ejaculation after standard surgery compared with five (10%) after laser therapy and eight (18%) after conservative management (exact P=0.11).
Discussion
In older men with lower urinary tract symptoms related to benign prostatic disease, erectile and ejaculatory dysfunction are common and perceived to be problematic. Pain or discomfort on ejaculation and the perception that sex life is spoilt by symptoms are less common but also problematic, particularly among younger men. This evidence from patients' reports of sexual dysfunction at baseline and follow up in a randomised controlled trial confirms the findings from previous research of a strong relation between age and symptoms of sexual dysfunction.1–4
Ejaculatory function significantly deteriorated after all treatment for benign prostatic disease (transurethral resection of the prostate (standard surgery) laser therapy, and conservative management). As expected we found significantly higher levels of retrograde ejaculation after standard surgery. However, in contrast with results of previous studies, other aspects of sexual function were no worse after standard surgery. Indeed, men were significantly less likely to experience erectile dysfunction than those undergoing conservative management and (though not significantly) laser therapy. In addition, pain or discomfort on ejaculation was significantly reduced after standard surgery than after laser therapy and conservative management. These results were further supported by the fact that new cases of erectile dysfunction and impotence occurred less often after transurethral resection, with a similar observation for pain or discomfort during ejaculation.
Implications of findings
This study is important for several reasons. Firstly, it contradicts the bulk of observational evidence that transurethral resection of the prostate can cause greater sexual dysfunction than minimally invasive treatments such as laser therapy. We found that transurethral resection resulted in improvement in erectile function and reduction in pain or discomfort on ejaculation. There were few new cases of impotence, as in other trials.15,16 In no instance was laser therapy significantly better than transurethral resection in maintaining or improving sexual function.
Secondly, our results strongly support the need to use valid and reliable measures of sexual function reported by patients at baseline and follow up. In this and other studies levels of sexual dysfunction were high among men with lower urinary tract symptoms,3,6 and previous reports of impotence after transurethral resection have probably been exaggerated by measurement error, differing definitions of “impotence,” and a failure to account for baseline levels.
Potential limitations of the study include possible response bias, though levels of missing data were low even for the questions on sexual function. It is difficult to validate fully a questionnaire to measure self reported sexual function. In this study, we used the ICSsex questionnaire, which has been shown to exhibit good levels of content and construct validity in terms of its comprehensibility to patients, low levels of missing data, ability to detect expected patterns with age, and ability to discriminate between community and clinic populations.6 We did not find the strong relation between individual symptoms and sexual dysfunction found previously,3,6 perhaps because of the smaller numbers in our trial, inclusion only of patients with relatively high overall levels of symptoms eligible for treatment, and the rarity of some symptoms. We found stronger associations between sexual dysfunction and the quality of life item relating to symptoms than the symptoms themselves, suggesting that there are close links between quality of life, sexual dysfunction, and the impact of lower urinary tract symptoms.4
In conclusion, assertions that minimally invasive treatment such as laser therapy may have less impact on sexual function than transurethral resection seem to be unjustified. Older men who need treatment for troublesome lower urinary tract symptoms and who wish to retain (or even improve) sexual function may thus want to consider transurethral resection.
Acknowledgments
Bard UK provided the laser fibres. We thank D M D Essenhigh, R R Hall, F C Hamdy, A Hinchcliffe, P H Powell, P D Ramsden, R Feneley, D A Gillatt, J C Gingell, A G Timoney, D R Greene, J K Mellon, and A C Thorpe for their help in the conduct of the study. L Gail Kennedy, K Ninan Chacko, Sandeep Gujral, Mark Wright, Linda Kelly, Esther Bartlett, Julie Ellis-Jones, Deborah Nevin, and Hazel Kay played an essential role in the collection of data and coordination of the study.
Footnotes
Funding: South West and Northern Regional NHS Research and Development Directorates.
Competing interests: TJP has received expenses and a fee from Sanofi-Synthelabo for speaking at a symposium.
References
- 1.Libman E, Fichten CS. Prostatectomy and sexual function. Urology. 1987;29:467–478. doi: 10.1016/0090-4295(87)90031-8. [DOI] [PubMed] [Google Scholar]
- 2.Bortz WM, Wallace DH, Wiley D. Sexual function in 1,202 aging males: differentiating aspects. J Gerontol. 1999;54A:M237–M241. doi: 10.1093/gerona/54.5.m237. [DOI] [PubMed] [Google Scholar]
- 3.Macfarlane GJ, Botto H, Sagnier PP, Teillac P, Richard F, Boyle P. The relationship between sexual life and urinary condition in the French community. J Clin Epidemiol. 1996;49:1171–1176. doi: 10.1016/0895-4356(96)00213-2. [DOI] [PubMed] [Google Scholar]
- 4.Namasivayam S, Minhas S, Brooke J, Joyce AD, Prescott S, Eardley I. The evaluation of sexual function in men presenting with symptomatic benign prostatic hyperplasia. Br J Urol. 1998;82:842–846. doi: 10.1046/j.1464-410x.1998.00868.x. [DOI] [PubMed] [Google Scholar]
- 5.Dunn KM, Croft PR, Hackett GI. Sexual problems: a study of the prevalence and need for health care in the general population. Fam Pract. 1999;15:519–524. doi: 10.1093/fampra/15.6.519. [DOI] [PubMed] [Google Scholar]
- 6.Frankel SJ, Donovan JL, Peters TJ, Abrams P, Dabhoiwala NF, Osawa D, et al. Sexual dysfunction in men with lower urinary tract symptoms. J Clin Epidemiol. 1998;51:677–685. doi: 10.1016/s0895-4356(98)00044-4. [DOI] [PubMed] [Google Scholar]
- 7.US Department of Health and Human Services. Benign prostatic hyperplasia: diagnosis and treatment. Bethesda, MD: Agency for Health Care Policy and Research; 1994. [Google Scholar]
- 8.Soderdahl DW, Knight RW, Hansberry KL. Erectile dysfunction following transurethral resection of the prostate. J Urol. 1996;156:1354–1356. [PubMed] [Google Scholar]
- 9.Oesterling JE. Benign prostatic hyperplasia. Medical and minimally invasive treatment options. N Engl J Med. 1995;332:99–109. doi: 10.1056/NEJM199501123320207. [DOI] [PubMed] [Google Scholar]
- 10.Barry MJ, Mulley AG, Jr, Fowler FJ, Wennberg JW. Watchful waiting vs immediate transurethral resection for symptomatic prostatism. The importance of patients' preferences. JAMA. 1988;259:3010–3017. [PubMed] [Google Scholar]
- 11.Graversen PH, Gasser TC, Wasson JH, Hinman F, Bruskewitz RC. Controversies about indications for transurethral resection of the prostate. J Urol. 1989;141:475–481. doi: 10.1016/s0022-5347(17)40864-0. [DOI] [PubMed] [Google Scholar]
- 12.Anson K, Nawrocki J, Buckley J, Fowler C, Kirby R, Lawrence W, et al. A multicenter, randomized, prospective study of endoscopic laser ablation versus transurethral resection of the prostate. Urology. 1995;46:305–310. doi: 10.1016/S0090-4295(99)80211-8. [DOI] [PubMed] [Google Scholar]
- 13.Boon TA, van Swol CFP, van Venrooij GEPM, Beerlage HP, Verdaasdonk RM. Laser prostatectomy for patients with benign prostatic hyperplasia: a prospective randomized study comparing two different techniques using the Prolase-II fiber. World J Urol. 1995;13:123–125. doi: 10.1007/BF00183628. [DOI] [PubMed] [Google Scholar]
- 14.Kabalin JN, Gill HS, Bite G, Wolfe V. Comparative study of laser versus electrocautery prostatic resection: 18-month followup with complex urodynamic assessment. J Urol. 1995;153:94–97. doi: 10.1097/00005392-199501000-00033. [DOI] [PubMed] [Google Scholar]
- 15.Keoghane SR, Doll HA, Lawrence KC, Jenkinson CP, Cranston DW. The Oxford laser prostate trial: sexual function data from a randomized controlled trial of contact laser prostaectomy. Eur Urol. 1996;30:424–428. doi: 10.1159/000474210. [DOI] [PubMed] [Google Scholar]
- 16.Wasson JH, Reda DJ, Bruskewitz RC, Elinson J, Keller AM, Henderson WG. A comparison of transurethral surgery with watchful waiting for moderate symptoms of benign prostatic hyperplasia. N Engl J Med. 1995;332:75–79. doi: 10.1056/NEJM199501123320202. [DOI] [PubMed] [Google Scholar]
- 17.Donovan JL, Peters TJ, Neal DE, Brookes ST, Gujral S, Chacko KN, et al. A randomized trial comparing transurethral resection of the prostate, laser therapy and conservative management in men with symptoms associated with benign prostatic enlargement: the CLasP study. J Urol. 2000;164:65–70. [PubMed] [Google Scholar]
- 18.Cockett AT, Aso Y, Denis L, Khoury S, Barry M, Carlton CE, et al. Recommendations of the International Consensus Committee. In: Cockett AT, Aso Y, Chatelain C, Denis L, Griffiths K, Khoury S, et al., editors. Proceedings of the World Health Organisation International Consultation on BPH 1991. Jersey: Scientific International; 1991. [Google Scholar]
- 19.Donovan JL, Abrams P, Peters TJ, Kay HE, Reynard J, Chapple C, et al. The ICH-“BPH” study: the psychometric validity and reliability of the ICSmale questionnaire. Br J Urol. 1996;77:554–562. doi: 10.1046/j.1464-410x.1996.93013.x. [DOI] [PubMed] [Google Scholar]
- 20.Barry MJ, Williford WO, Chang Y, Machi M, Jones KM, Walker-Corkery E, et al. Benign prostatic hyperplasia specific health status measures in clinical research: how much change in the American Urological Association symptom index and the benign prostatic hyperplasia impact index is perceptible to patients? J Urol. 1995;154:1770–1774. doi: 10.1016/s0022-5347(01)66780-6. [DOI] [PubMed] [Google Scholar]
- 21.Bender R, Grouven U. Ordinal logistic regression in medical research. J R Coll Physicians Lond. 1997;31:546–551. [PMC free article] [PubMed] [Google Scholar]
- 22.Armitage P, Berry G. Statistical methods in medical research. 3rd ed. Oxford: Blackwell; 1994. [Google Scholar]
- 23.StataCorp. Stata statistical software: release 6.0. College Station, TX: Stata Corporation; 1999. [Google Scholar]
- 24.Gujral S, Abrams P, Donovan JL, Neal DE, Brookes ST, Chacko KN, et al. A prospective randomized trial comparing transurethral resection of the prostate and laser therapy in men with chronic urinary retention: the CLasP study. J Urol. 2000;164:59–64. [PubMed] [Google Scholar]
- 25.Chacko KN, Donovan JL, Abrams P, Peters TJ, Brookes ST, Thorpe AC, et al. Transurethral prostatic resection or laser therapy for men with acute urinary retention: the CLasP randomized trial. J Urol. 2001;166:166–170. [PubMed] [Google Scholar]