Learning objectives.
By reading this article you should be able to:
-
•
Define hanging and near-hanging and explain its epidemiology.
-
•
Describe the common injuries that are sustained after an attempted hanging.
-
•
Detail the initial management after hanging or near-hanging, highlighting the key airway concerns.
Key points.
-
•
Hanging is the most common cause of death from suicide in the UK.
-
•
The incidence of hanging is increasing in both males and females aged below 65 yrs.
-
•
Some 6% of patients who survive to hospital admission after a hanging attempt will have an injury to either their cervical spine, neck vasculature or laryngotracheal tree.
-
•
Those patients with near-hanging who survive to hospital discharge are likely to have a good neurological outcome.
-
•
Patients who have sustained a hanging-induced cardiac arrest during the hanging attempt have a worse prognosis.
Rates of suicide in England and Wales continue to increase with 10.6 suicides per 100,000 people registered in 2021. The proportion of suicides attributed to hanging is the highest it has been for 20 yrs, accounting for more than half of all suicides in 2021.1 Hanging is a violent method of suicide compared with poisoning, and often results in death. The estimated fatality rate for a suicide attempt by hanging is estimated to be 85%.2 Therefore, ∼15% of patients who attempt suicide by hanging will be found alive, and these patients will need emergency assessment and treatment in hospital. Despite this, there are no guidelines available to aid management, and most research into medical care is observational and retrospective. This article outlines the suggested management for these patients.
Definitions
Hanging is a form of asphyxia characterised by a constriction of the neck by a ligature tightened by the gravitational weight of the body or part of the body, which ultimately results in death of the individual.3
Complete hanging is when there is complete free suspension of the body. Hanging with incomplete suspension, with some part of the body in contact with the floor, is known as partial or incomplete hanging.4 Near-hanging is the term applied to patients who survive the initial hanging and reach hospital.5
Judicial hanging, a form of capital punishment not undertaken in the UK since 1964, involves a fall from height leading to a fracture-dislocation of the upper cervical spine and spinal cord. Some patients will attempt to recreate this form of hanging during a suicide attempt.
Other terms such as ‘attempted hanging’ or ‘failed hanging’, or misuse of ‘hanged’ for a patient who has survived the suspension, are often used colloquially in medical practice, but the formal definitions given above will be used for the remainder of this article, in line with the current literature on this subject.
Epidemiology
Hanging, along with strangulation and suffocation, is the most common cause of suicide in the UK. In 2018, a total of 3148 deaths, representing 57.6% of all suicides, were attributed to hanging.1
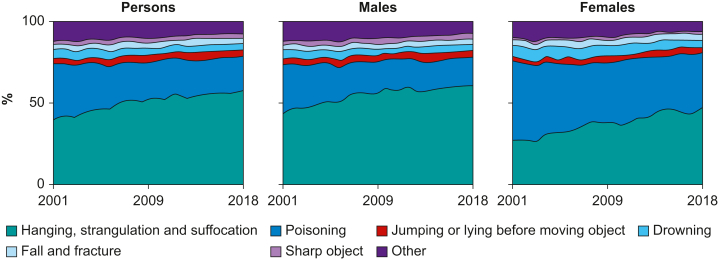
Between 2001 and 2018, the proportion of males committing suicide by this method increased from 43.8% to 60.9%, totalling 2511 deaths. Female deaths by hanging, although smaller in total number, also increased significantly in the same period from 26.8% to 47.5%, representing 637 deaths. This is a larger percentage increase than in males over the same period (Fig. 1). Since 2001, there has been a significant increase in the rate of hanging among people aged <65 yrs, but the rate in those >65 yrs during the same period remains broadly similar. Hanging, as a suicidal act, has a case fatality rate (CFR) of 85%, second only to firearms (CFR of 90%) in terms of lethality. Poisoning, the second most common mode of suicide in the UK (constituting 20.5% of all suicides), has a CFR of 8% whereas jumping from a height has a CFR of 47%.2 Most critical care physicians will see more poisoned patients in their practice than near hanged patients because of the significantly lower CFR of self-poisoning compared with hanging.
Fig 1.
The proportion of suicide in England and Wales (2001–2018) attributable to each method by sex.
In Australia, hanging became the most common method of suicide for males in 1989 and for females in 1994 coinciding with a period of increasing firearms control.6 In the USA, where firearms are much more widely available, hanging is the second most common cause of suicide after firearms. Despite this, the rate of suicide by hanging in the USA has nearly doubled in the past 20 yrs. Where an individual has a strong suicidal intent and access to firearms is restricted by governmental legislation, hanging with its high chance of fatality is regrettably an increasingly common mode of attempted suicide. As a direct result, the incidence of near-hanged patients attending hospital in the future is likely to increase.
Of all hanging victims, 75% hang themselves within their own homes, 15% within public spaces and 10% whilst in police custody or within hospital premises.7 As most hangings are fatal and occur within private property, the ability of government and society to prevent hanging is limited, and mostly relies on addressing mental health issues and other predisposing risk factors to suicide such as drug and alcohol abuse.
Pathophysiology
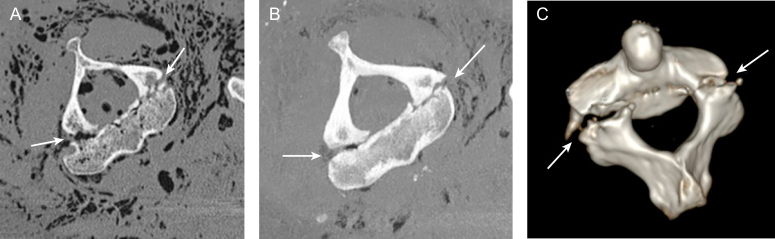
Some people attempt to recreate the process of judicial hanging by dropping from a height. Historically, the executioner would calculate a precise distance to fall based on the person's height and weight. This would normally involve falling at least the full height of the person being hanged. The resultant severe hyperextension and distraction of the neck causes bilateral pedicle fractures of the second cervical vertebra, known as the ‘Hangman's fracture’ (Fig. 2). This injury leads to the spinal cord becoming severed and rapid death ensues, therefore patients who have sustained a Hangman's fracture are rarely seen as inpatients. However, falling from this height is uncommon in self-induced hanging. When a fall from height has been excluded, there are thought to be three main mechanisms of death from hanging after a shorter drop or partial suspension:
-
•
Occlusion of the vasculature of the neck
-
•
Compression of the trachea
-
•
Vagal inhibition of the heart via pressure on the baroreceptors of the carotid sinus
Fig 2.
Images from a postmortem CT scan from a hanging victim demonstrating bipedicular fractures of C2, the so-called Hangman's fracture. (A) Unenhanced postmortem CT image in the transverse plane; (B) multiplanar reformatted image; (C) three-dimensional volume rendered image show bipedicular fracture of C2 (so-called hangman's fracture).
Recent studies from the Working Group on Human Asphyxia of filmed, non-judicial, hanging events have demonstrated that complete airway occlusion is not the usual cause of death. The agonal sequence of events that occurs during hanging supports vascular occlusion as the precipitant, rather than cardiac inhibition via vagal stimulation.4
The jugular veins within the neck are relatively easy to compress compared with the carotid or vertebral arteries because of the pressure within the arteries and the strength of the vessel walls. The trachea and larynx are harder to compress than the arteries because of the relative strength of the cartilaginous walls. A force of 35 N is required to compress the carotid artery whereas 150 N is required to compress the trachea.5
When the trachea is compressed by a ligature it is often not completely occluded and therefore airway compromise is not complete. Consequently, the hypoxic-ischaemic encephalopathy that results is likely to be caused by vascular occlusion. This compressive effect on the blood vessels can also lead to thrombosis and arterial dissection, further exacerbating cerebral ischaemic injury.8 Subarachnoid haemorrhage from vertebral artery dissection has also been reported.5
Near-hanging can also cause systemic complications including cardiac arrest, arrhythmias and acute respiratory distress syndrome (ARDS).9 Negative-pressure pulmonary oedema, caused by breathing attempts against a closed compressed airway, neurogenic pulmonary oedema and a whole-body inflammatory response from reperfusion injury are all thought to contribute to the development of ARDS after near-hanging.
Despite a ligature mark being a common finding on physical examination, other local injuries are surprisingly uncommon. One study of 71 patients, all of whom underwent CT angiography after near-hanging, found only four patients suffered cervical spine injury, three patients suffered arterial injuries and two had laryngotracheal injuries.10 A similar, large, multicentre retrospective study also found vascular or laryngotracheal injuries to have occurred in only 6% of near-hanged patients.11 Dropping from a height is uncommon in non-judicial hanging and this likely explains the low incidence of cervical spine and spinal cord injuries in these patients. Within these studies there is likely to be survivorship bias because of the high mortality associated with sustaining a vascular, laryngotracheal or cervical spinal cord injury during a hanging attempt. These patients are less likely to survive and therefore are not represented in studies.
In a recent French and Belgian study, 51% (450) of patients admitted to ICU after near-hanging were initially in cardiac arrest at the scene, and then successfully resuscitated.11 Of these, 18% survived to hospital discharge. Although cardiac arrest in near-hanging is likely to be an indicator of a poor prognosis the rate reported in this study is higher than the 4.9% survival rate to hospital discharge reported in a recent French study of patients after out-of-hospital cardiac arrest (OOHCA) from all causes.12
Prehospital management
Prehospital resuscitation of a near-hanged patient involves unhanging the patient, without causing further injury, and assessing for signs of life. If cardiac arrest is confirmed, a decision will need to be made as whether to start advanced life support as per published guidelines or implement recognition of life extinct protocols. Where resuscitation is started, the head and neck should be stabilised as much as is reasonably possible, with priority given to maintaining the airway and optimising oxygenation and perfusion. Adequacy of airway, breathing and circulation should immediately be assessed. Supplemental oxygen should be administered and i.v. or intraosseous access obtained. Bag-valve-mask ventilation should be started for patients with inadequate respiratory effort, and airway adjuncts, such as an oropharyngeal airway, placed to maintain patency of the airway as required. Development of surgical emphysema should alert practitioners to laryngotracheal injury and possible impending airway obstruction and cardiac arrest, and possible pneumothorax which may be bilateral. Prehospital emergency medical crews should consider whether to undertake tracheal intubation in the prehospital setting or transfer rapidly to hospital, noting that as a result of associated neck trauma, this group of patients may be expected to have a higher incidence of difficult laryngoscopy.13
Hospital management
Patients who are spontaneously breathing and regain consciousness should be admitted to hospital for a period of observation and assessment of any neck or other injuries and later psychiatric assessment. Patients who present in cardiac arrest or with a decreased level of consciousness should undergo tracheal intubation to facilitate neuroprotective ventilation and reduce the risk of pulmonary aspiration. If there are signs of laryngotracheal injury (surgical emphysema, expanding neck haematomas, dyspnoea and respiratory distress) then the airway team need to be prepared for a difficult airway and the potential of producing a false passage. Airway management of blunt neck trauma has recently been discussed in this journal and can be referred to for further detailed guidance.14 Most patients who require tracheal intubation in the context of near-hanging with laryngotracheal injury are unlikely to be cooperative or conscious enough for an awake fibreoptic intubation to be undertaken. Consequently, rapid-sequence induction is the preferred method. Cricoid pressure should be avoided as it may further disrupt damaged structures. Videolaryngoscopy has the benefit of allowing visualisation of the structures of the mouth, pharynx and glottis and reduces force required during direct laryngoscopy to obtain the same view.15 It is recommended that a tracheal tube is mounted onto a fibreoptic bronchoscope and passed under vision through the glottis into the trachea.14 This technique may help diagnose any airway injuries and allow accurate placement of the tracheal tube cuff distal to the injury as it is railroaded over the fibreoptic bronchoscope. Ultimately, the operator needs to use the technique with which they are most familiar and comfortable, noting that fortunately airway injuries that are severe enough to make airway management very challenging are rare.13
Manual in-line stabilisation (MILS) of the cervical spine during tracheal intubation in trauma patients is advocated to prevent further damage to the spinal cord in the case of unstable cervical spine injuries.5,16 However, cervical spine injury is relatively rare in patients with near-hanging and there is a paucity of evidence suggesting that MILS protects against further cervical spinal cord injury during emergency tracheal intubation in trauma patients. MILS is also known to cause a degradation in the grade of laryngoscopy view.17 A pragmatic approach would be to use MILS during tracheal intubation but to release it if there is difficulty obtaining a satisfactory laryngoscopy view. The aims should be to minimise apnoea time and hypoxaemia, and to maintain optimal perfusion to the brain and spinal cord, thereby reducing secondary injury.
There are no formal guidelines on diagnostic imaging for this patient group. Patients who are of GCS 15, who do not meet the criteria for cervical spine imaging by conventional triage scores such as the NEXUS criteria and who do not have evidence of airway injury can be safely observed.18,19 However, we advise a low threshold for carrying out a CT scan as physical examination can be unreliable, near-hanging could be considered a high-risk mechanism of injury and there is potential for missing injuries to critical anatomical structures of the neck.10 CT scanning of the head and neck, and CT angiography of the neck will identify an injury in 6% of patients.11 Further imaging with MRI and MR angiography may help delineate such injuries further but are rarely needed in the initial resuscitation period of care. Patients with vascular injuries should be discussed with local vascular surgery teams to decide management, including indications for systemic anticoagulation and for endovascular and open surgery.20
The management of laryngotracheal injuries is complex. The immediate priority is to secure the airway. Once achieved, further investigations can be undertaken with input from ENT and cardiothoracic surgical teams.21
Cervical spine injuries should be urgently discussed with regional neurosurgical centres via regional major trauma networks to help guide further management. Whilst the management of these injuries is being decided, the patient should be managed with full spinal precautions, including head blocks and tape and spinal log rolling for nursing care and transfers.
Critical care management
Patients who have been successfully resuscitated after cardiac arrest as a result of near-hanging should be admitted to critical care for standard post-resuscitation care as per European resuscitation council guidelines.20
A number of patients who have sustained a cardiac arrest will also have sustained an injury to their spinal cord. Such patients will need to have an individualised approach to management goals focusing on neuroprotective management with increased MAP targets (>85 mmHg) and more liberal oxygenation Pao2(>10 kPa) to protect the spinal cord from secondary neurological injury.22
Pulmonary complications are a frequent cause of subsequent morbidity and mortality. Aspiration pneumonitis, ARDS and bronchopneumonia commonly occur. In one study of near-hanged patients in ICU, 92% developed respiratory failure.11 Non-cardiogenic pulmonary oedema is described and likely to be either neurogenic in origin or caused by complete or partial airway obstruction at the time of the attempted hanging. This causes a negative intrathoracic pressure and subsequent pulmonary oedema.13 Patients affected should receive standard respiratory support and ‘lung protective ventilation’ and an echocardiogram to rule out a cardiac cause of pulmonary oedema.23
Neurological complications
It is difficult to predict which patients have sustained a devastating brain injury even amongst those who have suffered cardiac arrest. At presentation to hospital, some patients will show evidence of hypoxic ischaemic encephalopathy (HIE) on CT but can make a good neurological recovery.24 Early evidence of HIE on CT scanning should not be used as the sole means of prognostication for these patients. The European Resuscitation Council advocates a multimodal approach for prognostication, using clinical examination, imaging, biomarkers and neurophysiological studies.25
Seizures frequently occur in patients after hypoxic ischaemic brain injury. These should be treated with benzodiazepines and conventional anticonvulsant medications. Again, when taken in isolation, the presence of seizures does not indicate a poor prognosis, but early myoclonic status epilepticus (within 72 h after event), when used alongside other clinical and investigatory features, is much more reliably suggestive of this.25
Outcomes
Outcomes are better amongst those who have not suffered a cardiac arrest. In a large retrospective study of 886 patients from hospitals in France and Belgium, 51% of near-hanged patients sustained a cardiac arrest before presentation to hospital, with 18% of these surviving to hospital discharge. In contrast, 96% of patients after near-hanging who did not sustain a cardiac arrest survived to hospital discharge.11 Of the 497 patients in this study who survived to discharge, 479 (96%) had a favourable neurological outcome as defined as a Glasgow outcome score of 4 or 5 (Table 1). Unfortunately, this study did not separate the neurological outcomes of the patients who suffered a cardiac arrest from those who did not.
Table 1.
Glasgow outcome score.
| Score | Functional state | Description |
|---|---|---|
| 5 | Good recovery | Returned to original function without deficit |
| 4 | Moderate disability | Minor neurological deficit that does not interfere with daily functioning or work |
| 3 | Severe disability | Significant neurological deficit that interferes with daily activities or prevents return to employment |
| 2 | Persistent vegetative state | Coma or severe deficit rendering the patient completely dependent |
| 1 | Death | Dead |
A smaller single-centre UK study included 33 patients who had been admitted to critical care between 2010 and 2016 after near-hanging. Nineteen (58%) had suffered a hanging-induced cardiac arrest and in this subgroup, only three (16%) were discharged with a good neurological outcome as defined by a cerebral performance category (CPC) status of 1 or 2 (Table 2), with the other 16 not surviving to discharge. In contrast, in the group who had not suffered a cardiac arrest, all patients survived to hospital discharge. Eleven out of 14 patients had a good neurological recovery (CPC 1 or 2) with three patients being discharged with a poor neurological outcome (CPC 3 for all three patients), and all patients in the noncardiac arrest group survived to discharge.24 The survival rate after hanging-induced cardiac arrest in this study was 16%, similar to that in the much larger Franco-Belgian study (18%).
Table 2.
Cerebral performance categories.
| CPC 1 | Good cerebral performance. Conscious, alert, able to work and live independently, might have mild neurological or psychological deficit. |
| CPC 2 | Moderate cerebral disability, conscious, sufficient cerebral function for independent activities of daily life. Able to work in sheltered environment. |
| CPC 3 | Severe cerebral disability. Conscious, dependent on others for daily support because of impaired brain function. Ranges from ambulatory state to severe dementia and paralysis. |
| CPC 4 | Coma or vegetative state. Any degree of coma without the presence of all brain death criteria. Unawareness, even if appears awake (vegetative state) without interaction with the environment; may have spontaneous eye opening and sleep/awake cycles. Cerebral unresponsiveness. |
| CPC 5 | Brain death, apnoea, brain stem areflexia, silent EEG. |
Those patients most likely to have the best neurological outcomes are therefore either those who do not suspend themselves sufficiently to induce cardiac arrest, or those who are found and unhung before cardiac arrest ensues, despite significant suspension. However, cardiac arrest is not universally associated with poor outcome and in a case series 16–18% of these patients have survived to hospital discharge with a good neurological outcome. It is also apparent that most patients who survive to hospital discharge after a near-hanging event make a good neurological recovery. This information should help inform difficult conversations with the families of patients who have hanged themselves when discussing possible outcomes and prognosis.
Conclusions
Hanging and near hanging events are unfortunately increasing in incidence. As a result, the numbers of patients admitted to hospital and critical care are also likely to increase. There are no national or international guidelines to inform management. The care of these patients is largely supportive with attention to the airway, breathing and circulation, lung protective ventilation and management of traumatic injuries sustained from the ligature. Airway control with tracheal intubation is usually uneventful but teams must be prepared to encounter a ‘can't intubate, can't oxygenate’ scenario caused by laryngotracheal injury. Near-hanged patients who sustain a cardiac arrest have a worse neurological outcome and higher mortality than patients who do not sustain a cardiac arrest. However, when compared with other causes of cardiac arrest, near-hanged patients have a better prognosis. Knowing which of these patients will have sustained a devastating brain injury is difficult to predict and will only become clear after a period of neuroprotective management and careful ongoing neurological assessment over time. Lastly, caring for these patients and their families is often emotionally challenging. We feel that these challenges need to be recognised and discussed by the team in order to help protect their wellbeing.
Declaration of interests
The authors declare that they have no conflicts of interest.
MCQs
The associated MCQs (to support CME/CPD activity) will be accessible at www.bjaed.org/cme/home by subscribers to BJA Education.
Biographies
Alex Coombs MRCEM FRCA FFICM is a consultant in critical care and anaesthesia at University Hospitals Plymouth NHS Trust.
David Ashton-Cleary FRCA FFICM FHEA DIMC RCSEd DICM is a consultant in critical care and anaesthesia at the Royal Cornwall Hospital. He is the lead consultant for critical care transfers at the Royal Cornwall Hospital and deputy lead consultant and Peninsula lead for Retrieve, South West Adult Critical Care Transfer Service. Dr Ashton-Cleary is the lead consultant for Cornwall Air Ambulance service.
Matrix codes: 1B04, 2A02, 3A10
References
- 1.Office for National Statistics . 2022. Recent trends in suicides: death occurrences in England and Wales between 2001 and 2018.https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/recenttrendsinsuicidedeathoccurrencesinenglandandwalesbetween2001and2018/2020-12-08 Available from: [Google Scholar]
- 2.Cai Z., Junus A., Chang Q., Yip P.S.F. The lethality of suicide methods: a systematic review and meta-analysis. J Affect Disord. 2022;300:121–129. doi: 10.1016/j.jad.2021.12.054. [DOI] [PubMed] [Google Scholar]
- 3.Sauvageau A., Boghossian E.J. Classification of asphyxia: the need for standardization. Forensic Sci. 2010;55:1259–1267. doi: 10.1111/j.1556-4029.2010.01459.x. [DOI] [PubMed] [Google Scholar]
- 4.Sauvageau A., La Harpe R., Geberth V.J., et al. Agonal sequences in eight filmed hangings: analysis of respiratory and movement responses to asphyxia by hanging. J Forensic Sci. 2010;55:1278–1281. doi: 10.1111/j.1556-4029.2010.01434.x. [DOI] [PubMed] [Google Scholar]
- 5.Adams N. Near hanging. Emerg Med. 1999;11:17–21. [Google Scholar]
- 6.Australian Institute of Health and Welfare Suicide and self harm monitoring. Deaths by suicide over time. 2022. https://www.aihw.gov.au/suicide-self-harm-monitoring/data/deaths-by-suicide-in-australia/suicide-deaths-over-time Available from:
- 7.Gunnell D., Bennewith O., Hawton K., Simkin S., Kapur N. The epidemiology and prevention of suicide by hanging: a systematic review. Int J Epidemiol. 2005;34:433–442. doi: 10.1093/ije/dyh398. [DOI] [PubMed] [Google Scholar]
- 8.Stellpflug S.J., Weber W., Dietrich A., et al. Approach considerations for the management of strangulation in the emergency department. J Am Coll Emerg Physicians Open. 2022;3 doi: 10.1002/emp2.12711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schellenberg M. Near-hanging injuries: understanding outcomes among the critically ill. Chest. 2020;158:2243–2244. doi: 10.1016/j.chest.2020.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Schellenberg M., Inaba K., Warriner Z., et al. Near hangings: epidemiology, injuries, and investigations. J Trauma Acute Care Surg. 2019;86:454–457. doi: 10.1097/TA.0000000000002134. [DOI] [PubMed] [Google Scholar]
- 11.De Charentenay L., Schnell G., Pichon N., et al. Outcomes in 886 critically ill patients after near-hanging injury. Chest. 2020;158:2404–2413. doi: 10.1016/j.chest.2020.07.064. [DOI] [PubMed] [Google Scholar]
- 12.Luc G., Baert V., Escutnaire J., et al. Epidemiology of out-of-hospital cardiac arrest: a French national incidence and mid-term survival rate study. Anaesth Crit Care Pain Med. 2019;38:131–135. doi: 10.1016/j.accpm.2018.04.006. [DOI] [PubMed] [Google Scholar]
- 13.Kaki A., Crosby E.T., Lui A.C. Airway and respiratory management following non-lethal hanging. Can J Anaesth. 1997;44:445–450. doi: 10.1007/BF03014468. [DOI] [PubMed] [Google Scholar]
- 14.Shilston J., Evans D.L., Simons A., Evans D.A. Initial management of blunt and penetrating neck trauma. BJA Educ. 2021;21:329–335. doi: 10.1016/j.bjae.2021.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Russell T., Khan S., Elman J., Katznelson R., Cooper R.M. Measurement of forces applied during Macintosh direct laryngoscopy compared with GlideScope® videolaryngoscopy. Anaesthesia. 2012;67:626–631. doi: 10.1111/j.1365-2044.2012.07087.x. [DOI] [PubMed] [Google Scholar]
- 16.National Institute for Health And Care Excellence . 2016. Spinal injury: assessment and initial management.www.nice.org.uk/guidance/ng41 NG41. Available from. [PubMed] [Google Scholar]
- 17.Wiles M.D. Manual in-line stabilisation during tracheal intubation: effective protection or harmful dogma? Anaesthesia. 2021;76:850–853. doi: 10.1111/anae.15472. [DOI] [PubMed] [Google Scholar]
- 18.Subramanian M., Hranjec T., Liu L., Hodgman E.I., Minshall C.T., Minei J.P. A case for less workup in near hanging. J Trauma Acute Care Surg. 2016;81:925–930. doi: 10.1097/TA.0000000000001231. [DOI] [PubMed] [Google Scholar]
- 19.Bordia R., Freeman C., Kou H.H., Culhane J. Do we need neuroimaging in every case of near-hanging?: experience from a level 1 trauma center and analysis of the National Trauma Data Bank. Emerg Radiol. 2021;29:49–57. doi: 10.1007/s10140-021-01979-2. [DOI] [PubMed] [Google Scholar]
- 20.Shahan C.P., Sharpe J.P., Stickley S.M. The changing role of endovascular stenting for blunt cerebrovascular injuries. J Trauma Acute Care Surg. 2018;84:308–311. doi: 10.1097/TA.0000000000001740. [DOI] [PubMed] [Google Scholar]
- 21.Moonsamy P., Sachdeva U.M., Morse C.R. Management of laryngotracheal trauma. Ann Cardiothorac Surg. 2018;7:210–216. doi: 10.21037/acs.2018.03.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eli L., Lerner D.P., Ghogawala Z. Acute traumatic spinal cord injury. Neurol Clin. 2021;39:471–488. doi: 10.1016/j.ncl.2021.02.004. [DOI] [PubMed] [Google Scholar]
- 23.Griffiths M.J.D., McAuley D.F., Perkins G.D., et al. Guidelines on the management of acute respiratory distress syndrome. BMJ Open Respir Res. 2019;6 doi: 10.1136/bmjresp-2019-000420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sutcliffe W.J.C., Saayman A.G. Hanging and asphyxia: interventions, patient outcomes and resource utilisation in a UK tertiary intensive care unit. J Intensive Care Soc. 2018;19:201–208. doi: 10.1177/1751143717742067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nolan J.P., Sandroni C., Böttiger B.W., et al. European resuscitation council and European society of intensive care medicine guidelines 2021: post-resuscitation care. Resuscitation. 2021;161:220–269. doi: 10.1016/j.resuscitation.2021.02.012. [DOI] [PubMed] [Google Scholar]