Death rates after surgical care are increasingly analysed to estimate prognosis and for clinical audit and quality assessment. Expectations are growing among health professionals and the public that hospitals will know about, and learn from, the death rates of their patients. However, routine statistics commonly provide information only on deaths that occur during the hospital admission in which surgery was done. Rates based on these deaths are conventionally known as in-hospital death rates and are typically analysed as those that occur within 30 days after admission or surgery.
Systems of national hospital statistics in England were designed in the 1960s and redesigned in the mid-1980s.1,2 Hospital statistics are not linked to death certificate data nationally, although this has long been feasible.3,4 Even the National Confidential Enquiry into Perioperative Deaths, a meticulous ongoing national study with local clinical reporting and case note review of deaths, is constrained practically to the identification of deaths in the hospital admissions in which the operations were done.5 By using hospital data linked to death certificate data, we studied the extent to which in-hospital deaths accounted for all deaths within 30 days of hospital admissions during which operations were done.
Methods and results
We used anonymised statistical abstracts of hospital records that were linked to data from death certificates in the former Oxford health region from 1963 to 1998. Data collection covered a population of 300 000 from 1963 to 1965, 850 000 from 1966 to 1974, 1.9 million from 1975 to 1986, and 2.5 million from 1987.
We identified all deaths within 30 days of an admission for surgery. Ideally, we would have related deaths to days from an operation but dates of surgery were incompletely recorded. We tabulated deaths at single day intervals between admission and death and present results for three periods: 1963-74, 1975-86, and 1987-98. More detailed analysis of successive years within 1987-98 showed that the pattern of death for individual years was similar to that in the whole period. Deaths were classified by place of occurrence: in hospital in the same admission as the operation, in hospital after readmission, after transfer to a different hospital, or outside hospital.
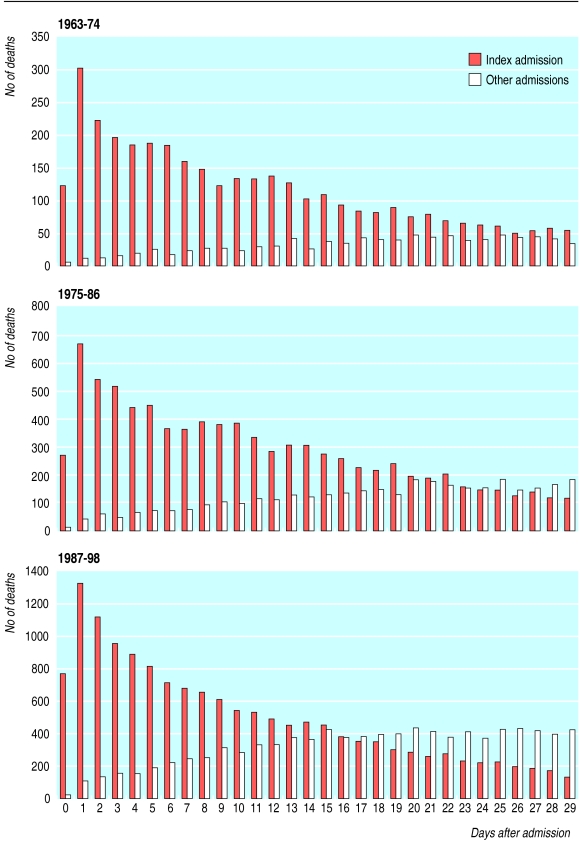
During 1963-98, 41 200 people died within 30 days after an admission in which they had surgery. Deaths in the admission in which surgery occurred (in-hospital deaths) represented 79.3% of all deaths within 30 days in 1963-74 (3552/4482), 71.2% in 1974-86 (8710/12 239), and 61.2% in 1987-98 (14 977/24 479).
Most deaths that occurred within a few days of surgery were in-hospital deaths (figure). With increasing time from admission, increasing numbers of deaths within 30 days occurred elsewhere and would have been missed by analysis of in-hospital mortality alone. The percentage of deaths that occurred after discharge or transfer increased substantially in the later years covered by the study.
Comment
The percentage of deaths within 30 days of an admission for surgery that are in-hospital deaths has fallen substantially since routine hospital statistics were first collected in the 1960s and 1970s. This reflects decreases in length of hospital stays and an increase in the transfer of acutely ill patients between hospitals for specialist care. In-hospital mortality alone is now an incomplete measure of mortality even within 30 days of care. To identify the missing deaths, hospital statistical records need to be linked to data from death certificates. This is now feasible nationally in England.
Figure.
Days from admission to death within 30 days of admission 1963-98, subdividing deaths into those during hospital admission for surgery and those occurring elsewhere
Footnotes
Funding: AM is funded by the Department of Health as part of its funding of the National Centre for Health Outcomes Development. The views expressed in this paper are those of the authors and not necessarily those of the Department of Health. The Unit of Health-Care Epidemiology is funded by the South East Regional Office of the NHS Executive.
Competing interests: None declared.
References
- 1.Department of Health and Social Security. Hospital activity analysis. London: DHSS; 1969. [Google Scholar]
- 2.Steering Group on Health Services Information. First report to the secretary of state. London: HMSO; 1982. [Google Scholar]
- 3.Acheson ED. Medical record linkage. Oxford: Oxford University Press; 1967. [Google Scholar]
- 4.Henderson J, Goldacre MJ, Simmons H, Griffith M. Recording of deaths in hospital information systems: implications for audit and outcome studies. J Epidemiol Community Health. 1992;42:297–299. doi: 10.1136/jech.46.3.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Callum KG, Gray AJG, Hoile RW, Ingram GS, Martin IC, Sherry KM, et al. Then and now. The 2000 report of the National Confidential Enquiry into Perioperative Deaths. London: National CEPOD; 2000. [Google Scholar]