Abstract
Skin wounds are characterized by injury to the skin due to trauma, tearing, cuts, or contusions. As such injuries are common to all human groups, they may at times represent a serious socioeconomic burden. Currently, increasing numbers of studies have focused on the role of mesenchymal stem cell (MSC)-derived extracellular vesicles (EVs) in skin wound repair. As a cell-free therapy, MSC-derived EVs have shown significant application potential in the field of wound repair as a more stable and safer option than conventional cell therapy. Treatment based on MSC-derived EVs can significantly promote the repair of damaged substructures, including the regeneration of vessels, nerves, and hair follicles. In addition, MSC-derived EVs can inhibit scar formation by affecting angiogenesis-related and antifibrotic pathways in promoting macrophage polarization, wound angiogenesis, cell proliferation, and cell migration, and by inhibiting excessive extracellular matrix production. Additionally, these structures can serve as a scaffold for components used in wound repair, and they can be developed into bioengineered EVs to support trauma repair. Through the formulation of standardized culture, isolation, purification, and drug delivery strategies, exploration of the detailed mechanism of EVs will allow them to be used as clinical treatments for wound repair. In conclusion, MSC-derived EVs-based therapies have important application prospects in wound repair. Here we provide a comprehensive overview of their current status, application potential, and associated drawbacks.
Keywords: Mesenchymal stem cell (MSC), Extracellular vesicles (EVs), Wound repair, Engineered nanoparticles
Background
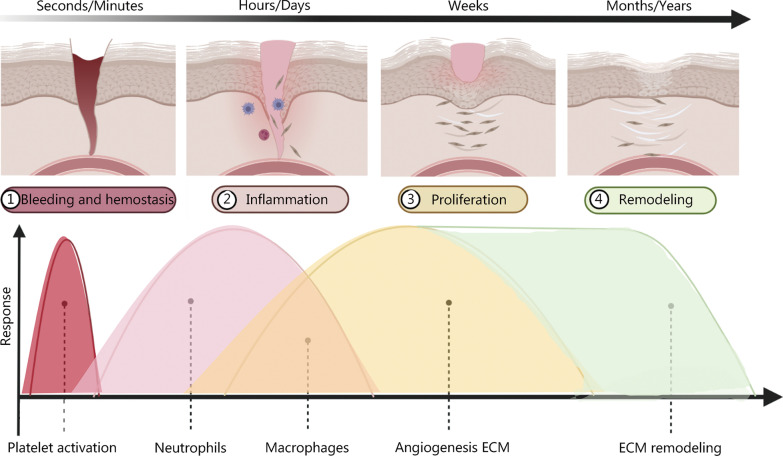
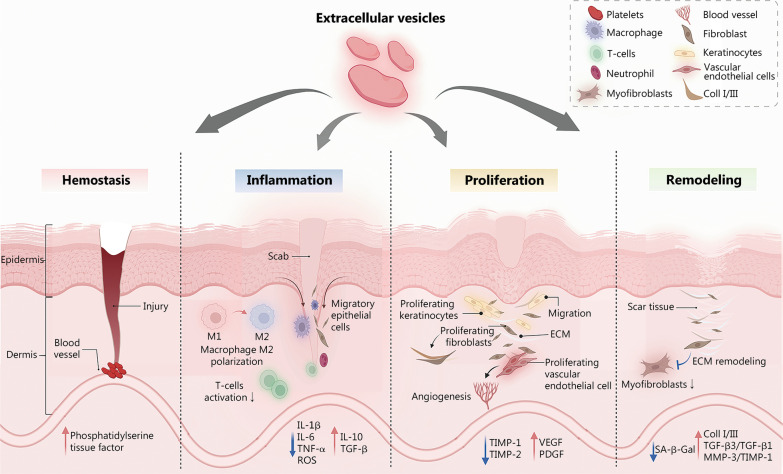
Cutaneous trauma and repair are major clinical challenges that entail substantial social and medical burdens. Wound healing is a complex process involving blood clotting, inflammation, new tissue formation, and tissue remodeling [1, 2]. In the process of wound healing, hemostasis occurs within seconds to minutes [3]. The damaged vessels contract, platelets are utilized, and coagulation pathways are activated through the exposure of the subendothelial matrix to form fibrin clots that provide a scaffold for inflammatory cells [4]. Neutrophils infiltrate the trauma area within 24 h, being attracted by chemokines, followed by macrophages that are attracted by cellular apoptotic by-products [3]. During the inflammatory phase of wound healing, macrophages are drawn to the wound and show polar M1 and M2 phenotypes. The first type, called M1 macrophage, is involved in cytokine release and pathogen elimination. Their phenotypes transition from M1 to M2 when macrophages phagocytose neutrophils. M2 macrophages support angiogenesis, extracellular matrix (ECM) repair, the release of anti-inflammatory cytokines, and the resolution of inflammation [5]. The proliferative phase begins on day 3 and normally lasts 3–6 weeks except for complicated wounds that are difficult to heal. At this time, endothelial cells proliferate and migrate to form new blood vessels [4]. Fibroblasts produce collagen I and III to form the ECM. The ECM is a cell-free collagen scaffold that creates an environment supporting enhanced proliferation and migration of fibroblasts and keratinocytes [6]. The remodeling process begins at week 3 and can last for several years. The ECM is degraded by matrix metalloproteinases (MMPs), and type I collagen replaces type III collagen [4], as Fig. 1 shows.
Fig. 1.
Schematic diagram of the skin repair process. The four phases of trauma repair, hemostasis, inflammation, proliferation, and remodeling phases, occur in order and can overlap. Platelets play a role in the hemostatic phase. Neutrophils play an anti-infection function primarily during the inflammatory phase. Macrophages are involved in both the inflammatory and proliferative phases and exert different roles depending on the phenotypic variation (M1 and M2). Vascularization as well as extracellular matrix (ECM) formation occurs during the proliferative phase, while ECM remodeling may take months or even years.
Reproduced with permission from Ref. [7]. Copyright 2021, Elsevier B.V. Reproduced with permission from Ref. [8]. Copyright 2022 Cialdai, Risaliti, and Monici
Traditional wound repair methods are often based on physical therapy, including dressing change, wound drainage, and skin grafting. However, traditional therapies are well known for their long duration and susceptibility to infection [9]. Regenerative medicine aims to replenish, replace, or repair traumatized cells, tissues, and organs, essentially providing a cure for vessel damage, nerve damage, and diabetic trauma [10]. In recent years, biotherapy has attracted much attention as a new treatment method that complements traditional regenerative medicine. Biotherapy comprises cell therapy, biomaterial implants, and tissue engineering. Among these treatments, mesenchymal stem cells (MSCs), as a group of cells with self-renewal activity, have shown substantial developmental potential, and thus have received interest in the field of wound repair [11, 12], as they are expected to have a transformative impact on the treatment of refractory wounds [13].
An increasing number of studies have found that compared with MSC-based cell therapy, MSC-derived extracellular vesicles (EVs) can effectively overcome the problems such as host rejection during skin repair treatment, and they have been shown to exert multiple therapeutic effects on skin regeneration [14, 15]. EVs, as a “cell-free therapy”, similar to “Trojan horses”, can transmit biological effectors that are beneficial to the treatment of adjacent cells or other target cells through natural or engineered methods. EVs have been demonstrated to be an effective drug delivery strategy in multiple areas, including tumors, the spinal cord, the cardiopulmonary system, the brain, and wound surfaces [16–19]. Moreover, as a novel cell-free treatment, MSC-derived EV-based therapy has demonstrated biosafety, high stability, and low immunogenicity. The therapeutic effects of EVs on wound healing and scar repair have been shown to be superior to those of MSC therapy, a treatment that showed excellent application prospects [20–22]. Previous studies have found that MSC-derived EVs carry biological factors targeting angiogenic [23–25], anti-inflammatory [26, 27], and antifibrosis-related pathways [28, 29]. Therefore, MSC-derived EVs can promote revascularization of wounds caused by trauma, initiate nerve repair, and function in the regeneration of wounded appendages, enhancing early and non-scarring healing by activating related pathways such as the phosphatase and tensin homolog deleted on chromosome 10 (PTEN)/Akt pathway [26] and the transforming growth factor-β1 (TGF-β1)/Smad2/3 signaling pathway [29].
Cutaneous trauma commonly occurs in our daily life. Recent advances in the area of MSC-derived EV-based therapy have provided promising treatment options to meet the challenges of impaired skin wound healing [21, 30]. In the present study, we provide a comprehensive overview of the latest progress in the use of MSC-derived EVs in wound repair, from the biological properties of MSC and EVs to their applications in trauma healing, including the regeneration of vessels, nerves, and hair follicles. In addition, we provide valuable suggestions for the clinical application of EVs in wound repair.
MSCs
Stem cells are a population of undifferentiated cells that have the potential for multidirectional differentiation, self-replication, and self-renewal. They are widely used in the treatment of various diseases and regenerative repair [31]. MSCs are mesoderm-derived multipotent stem cells that were originally described as having a fibroblast-like morphology in mouse bone marrow and spleen, and being capable of differentiating into osteoblasts [32]. The sources and preparation of MSCs are listed in Table 1.
Table 1.
Sources and preparation of MSCs
| Source of MSCs | Preparation of MSCs |
|---|---|
| Bone marrow-derived MSCs [33] | The enzymatic digestion method: collagenase, dispase, or trypsin [34] |
| Adipose tissue-derived MSCs [35] | Mechanical procedures based on non-enzymatic digestion: centrifugation and filtration [34] |
| Umbilical cord blood-derived MSCs [36] | The explant culture [37] |
| Wharton’s jelly-derived MSCs [38] | |
| Dermis-derived MSCs [39] | |
| Hair follicles-derived MSCs [40] | |
| Amniotic fluid-derived MSCs (AF-MSCs) [41] | |
| Placental MSCs [42] | |
| Gingival-derived MSCs [43] | |
| Salivary gland-derived MSCs [44] | |
| Menstrual blood-derived MSCs [45] | |
| Synovium mesenchymal stem cells [46] |
MSC mesenchymal stem cell
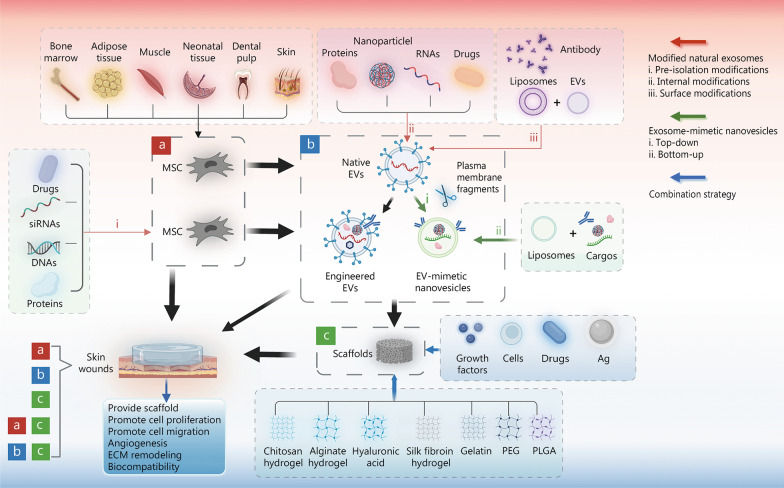
Regardless of their origin, MSCs play a crucial role in the orchestration of tissue repair by assisting in enhancing wound tensile strength, reducing scar formation, decreasing wound contraction, and increasing collagen synthesis. Some studies have shown that the paracrine interactions between MSCs and nearby cells, such as the production of bioactive substances (cytokines, chemokines) as well as EVs, produce the healing effect rather than cell transplantation [47–51]. MSCs have demonstrated their involvement in all stages of wound healing (Fig. 2), and their mechanisms of scar treatment include: 1) immunomodulatory effects, including the regulation of cytokines, macrophage phenotype polarization, and T-cell activity [52] to promote wound healing; 2) anti-fibrosis through decreases in myofibroblast differentiation and type I and III collagen production [53]; and 3) promotion of angiogenesis, which contributes to wound healing [54, 55].
Fig. 2.
Diagram illustrating the application of mesenchymal stem cell (MSC) in wound repair. a MSC therapy, including native MSC and pre-extracellular vesicles (EVs) isolation MSC modifications. b EV therapy, including native EVs, engineered EVs, and EV-mimetic nanovesicles. c Wound dressing therapy. For wound treatment, either a/b/c therapy alone or a combination of a/b with c can be used. The red arrows represent three modified natural EV methods, including pre-isolation modifications (i), internal modifications (ii), and surface modifications (iii). The green arrows represent EV-mimetic nanovesicle production methods such as top-down (i) and bottom-up (ii). The blue arrows show the combination strategies for wound dressing. It was created utilizing the templates on BioRender.com as a reference. Ag antibacterial material, ECM extracellular matrix, PEG polyethylene glycol, PLGA poly lactic-co-glycolic-acid
Current research focuses on the application of MSCs in wound repair and the potential for clinical treatment. Thus, cell therapy and regenerative medicine have advanced with the development of stem cell isolation, implantation, and expansion technologies to provide safe and cost-effective products [56]. However, there are still many aspects of MSCs such as the duration of effect, differentiation properties, and other unexplored effects that need further study.
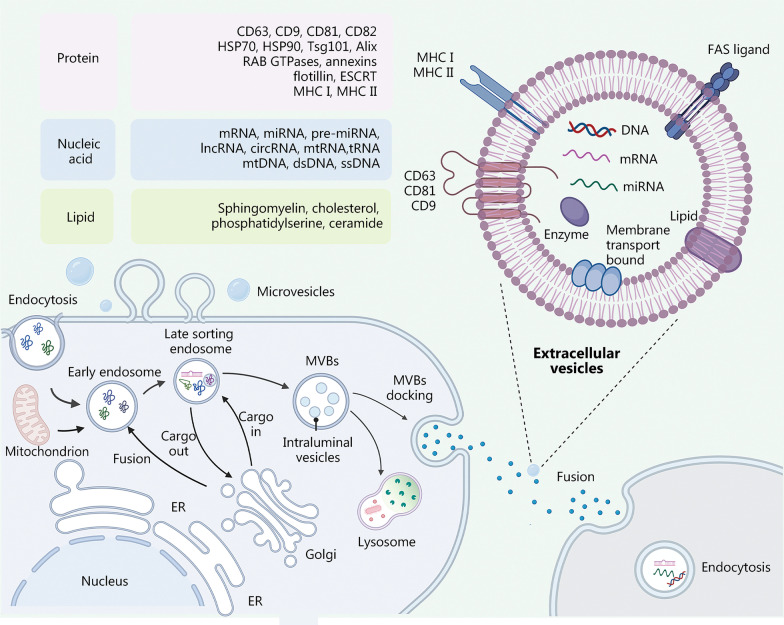
Biological properties of EVs
Exosomes were first discovered in the study of iron uptake by reticulocytes, being manifested as inner vesicles in a reticulocyte suspension supernatant [57]. Since 1987, when the term “exosome” was first utilized to describe small membrane vesicles formed by intracellular endosomes and released by exocytosis [58], exosomes have developed into a mainstay in the field of disease diagnosis, treatment, and regeneration. These vesicles can be separated from platelets [59], saliva [60], urine [61], or any other type of cell or body fluid. EVs are nanoscale particles actively secreted by cells and are roughly divided into three subgroups according to their biogenesis, release pathway, sizes, contents, and functions [62]: apoptotic vesicles, 50–5000 nm, microvesicles, 100–1000 nm, and exosomes, 30–200 nm [63]. The overlap between these size ranges indicates the limitation of this classification [64]. Numerous studies mentioning one kind of vesicle actually refer to the broader EV pool [65]. According to minimal information for studies of extracellular vesicles 2018 (MISEV2018), “extracellular vesicles” is the recommended nomenclature for describing the small membrane-bound particles naturally released from cells. In contrast to microvesicles and apoptotic bodies, which are generated by the outward budding and fission of the cell membrane, EVs are derived from the endolysosomal pathway in a stepwise manner [66]. EV production is the result of cell endocytosis that forms multivesicular bodies (MVBs) that bud into the extracellular space. Depending on their ultimate fate, MVBs may fuse with lysosomes to be degraded (degradative MVBs) or fuse with the plasma membrane (secretory MVBs) to release EVs into the extracellular space [66, 67] (Fig. 3). Both processes rely on the Rab family of small GTPases such as RAB27A, RAB11, and RAB31 [68]. The mechanisms regulating the process of cargo aggregation within EVs include the endosomal sorting complex required for transport (ESCRT)-dependent mechanism and an ESCRT-independent mechanism [62, 64]. RAB31 was shown to control ESCRT-independent mechanism regulating EV biogenesis, including driving intraluminal vesicles (ILVs) formation and inhibiting MVB degradation [69]. EVs consist of a lipid bilayer containing nucleic acids, lipids, and proteins [70, 71], and they perform a variety of functions ranging from targeting metabolism to inflammatory regulation. Lipids, including sphingomyelin, cholesterol, and phosphatidylserine, contribute to the formation and release of EVs. EVs contain a large number of proteins associated with membrane transport and fusion, including annexin, ESCRT, Rab-GTPases, actin, and β-tubulin. EVs also contain common membrane surface markers such as tetrapeptides (CD9, CD63, CD81, and CD82), heat shock proteins [heat shock protein 70 (HSP770) and HSP90], Tsg101, and Alix, which are utilized as common exosomal markers [16, 64, 65]. EVs have been reported to carry mRNA, microRNA (miRNA), ribosomal RNA, circular RNAs, DNA, long noncoding RNA (lncRNA), and some cytokines [72]. Exosomal RNAs such as miRNAs are not only the most valuable informative molecules for liquid biopsies but are also important in cellular regulatory functions.
Fig. 3.
Process of extracellular vesicles (EVs) biogenesis and the molecular composition of EVs are shown as follows: (1) various components of the extracellular environment, including proteins, lipids, and small molecule metabolites, are endocytosed to form early endosomes; (2) the early endosomes are transformed into late endosomes that in turn form multivesicular bodies (MVBs); (3) MVBs are formed into EVs by fusion with microtubules and the cytoskeleton to the plasma membrane. Otherwise, a part of the MVB is transported and merged with the lysosomes to degrade the cargo. EVs enter the recipient cell through various pathways, including endocytosis, macrophage uptake, phagocytosis, and direct fusion with the plasma membrane. It was created utilizing the templates on BioRender.com as a reference. CD cluster of differentiation, HSP heat shock protein, Tsg tumor susceptibility gene, Alix apoptosis-linked gene 2-interacting protein X, RAB Ras-like proteins in brain, GTPases guanosine triphosphate hydrolases, ESCRT endosomal sorting complex required for transport, MHC major histocompatibility complex, mRNA messenger ribonucleic acid, miRNA micro ribonucleic acid, lncRNA long non-coding ribonucleic acid, mtRNA mitochondrial ribonucleic acid, tRNA transfer ribonucleic acid, dsRNA double-stranded ribonucleic acid, ssDNA single-stranded deoxyribonucleic acid, FAS tumor necrosis factor receptor superfamily member 6, DNA deoxyribonucleic acid, ER endoplasmic reticulum
EV composition varies among tissues and cell sources, and heterogeneity can be found even among cells from the same tissue grown under the same conditions. The heterogeneity of EVs includes size, yield and quantity, contents, and functional effects on recipient cells. Different combinations lead to complex heterogeneity of EVs [73]. Differential gene expression between different cell sources, differences in gene expression and transcriptional fluctuations induced by culture conditions, genomic health of cells, variation in protein concentrations within the cytoplasm and membrane, and the limited carrying capacity of EVs lead to differences in EV biogenesis, resulting in heterogeneity [16, 19, 67]. The qualitative and quantitative components of specific EVs must be determined to guarantee the safety of clinical applications.
By transporting biochemical molecules, EVs play important roles in cellular communication, the delivery of genetic material, the regulation of signaling pathways, and the administration of nutrients. A recent study has found that when EVs are released into the extracellular environment, a protein corona will spontaneously form around the outer membrane [74]. The components of the corona are peripheral membrane proteins that establish interactions with the EV membrane and some nucleic acid molecules. Thiol interactions and electrostatic interactions are the main mechanisms involved in the formation of the corona [75]. The EV corona’s functional roles in angiogenesis, cutaneous regeneration, and immunomodulation can be eliminated through removal by ultracentrifugation [76]. The mechanisms by which EVs act must therefore be thoroughly investigated.
EV isolation and purification are divided into five major categories: 1) ultracentrifugation, the most widely used but also the most time-consuming method, generally shows low yield and low purity [77] and results in coelution with a number of cytokines [78]; 2) ultrafiltration, which improves EV yield and separation efficiency [79]; 3) size exclusion chromatography, which removes residual contaminants from the results of standard ultracentrifugation enrichment methods to obtain high-purity EVs [80]; 4) immunoseparation, including immunoaffinity chromatography, and the immunomagnetic bead method. These methods can improve the purity of EVs, but they generally obtain low yields [78]; and 5) microfluidics has the characteristics of low cost, low sample volume, high throughput, and high precision [81].
The identification and quantification of EVs are performed through techniques such as transmission electron microscopy, scanning electron microscopy, Western blotting, atomic force microscopy, nanoparticle tracking analysis, dynamic light scattering, resistive pulse sensing, enzyme-linked immunosorbent assays, flow cytometry, fluorescence-activated cell sorting, and microfluidic and electrochemical biosensors [58, 82, 83].
MSC-derived EVs for wound repair
There is no evidence for the differentiation of MSCs into the typical resident skin cell phenotypes during skin wound healing. In contrast, MSC-derived EVs can stably transport cargo due to the protective effect of the lipid bilayer; their lower content of membrane-bound proteins makes them less immunogenic [84]. Therefore, cell-free therapy represented by MSC-derived EVs has numerous advantages over MSC therapy: low immunogenicity, low tumorigenicity, low cytotoxicity, easy preservation, high stability, lower degradability, penetration of the blood–brain barrier, possible intravenous injection, internalization into cells, possible cargo loading, and inherent homing properties [85]. In toxicity analysis, MSC-derived EVs have shown immunotolerance properties, absence of genotoxic effects, and no production of endotoxins [86]. Importantly, this treatment also has effects similar to those of MSCs and demonstrates superior effects in wound repair. Several studies have reported that EVs derived from MSCs (bone marrow [87], blood, fat [88], urine [89], gingiva [90], umbilical cord [91], Wharton’s jelly [92], and other sources) significantly promoted angiogenesis and skin re-epithelialization during skin wound healing [61]. KEGG and GO analyses revealed that the RNAs of MSC-derived EVs are associated with signaling pathways related to cytoskeletal organization and wound healing. A recent study demonstrated that stem cell-derived EVs regulated tissue repair and regeneration [93]. Overviews of experiments using MSC-derived EVs in vivo and in vitro in the context of wound healing are presented in Tables 2 and 3.
Table 2.
Summary of researches on EVs involved in in vivo wound repair
| Wound type | Animal model | EVs type | Cargo | Target | Function | References |
|---|---|---|---|---|---|---|
| Acute wound | Rat model of the skin-deep second-degree burn wound | HucMSC-derived EVs (30–100 nm) | – | Wnt/β-catenin | Proangiogenic effect↑ | [94] |
| Rat skin burn model | HucMSC-derived EVs | – | Wnt4 | Heat stress-induced apoptosis↓ | [95] | |
| Deep second-degree burn mice model | Blue light-treated MSC-derived EVs |
miR-135b-5p miR-499a-3p |
MEF2C | Proangiogenic ability↑ | [89] | |
| Severe burn rat model | HucMSC-derived EVs | miR-181c | Toll-like receptor 4 | Burn-induced inflammation↓ | [96] | |
| Rat full-thickness cutaneous wounds model | UCB-MSC-derived EVs |
miR-21-5p miR-125b-5p |
TGF-β receptor type II and TGF-β receptor type I | Anti-myofibroblast differentiation↑ | [91] | |
| Mouse full-thickness cutaneous wounds model | UCMSC-derived EVs (75.66 nm) | – | – |
Recruitment of fibroblasts↑ Cutaneous nerve regeneration↑ |
[97] | |
| Mouse full-thickness skin defects model | HucMSC-derived EVs (85% range from 20 to 200 nm) | – |
Inhibiting nuclear translocation of apoptosis-inducing factor Upregulating poly ADP ribose polymerase 1 (PARP-1) and poly (ADP-ribose) |
Epidermal re-epithelialization↑ Dermal angiogenesis↑ |
[98] | |
| Mouse skin wound model | BMSCs overexpressed with miR-126 EVs (Exo-miR-126, 30–200 nm) | miR-126 | Targeting phosphoinositol-3 kinase regulatory subunit 2 to activate the PI3K/Akt signalling pathway | Newly formed capillaries↑ | [24] | |
| Rat skin wound model | hiPSC-MSC-derived EVs | – | – |
Collagen synthesis↑ Angiogenesis↑ |
[47] | |
| Rat skin wound model | HucMSC-derived EVs | 14-3-3ζ proteins | Wnt/β-catenin signaling | Cutaneous regeneration | [99] | |
| Mouse retinal laser injury wound model | HucMSC-derived EVs (40–100 nm) | – | Downregulation of monocyte chemotactic protein-1 |
Apoptosis↓ Inflammatory responses↓ |
[100] | |
| Mouse full-thickness dermal wound injury model | FDMSC-derived EVs | – | Notch signaling pathway by Jagged 1 | Adult dermal fibroblast cell motility and secretion ability↑ | [101] | |
| Mouse full-thickness dorsal wound model | ADMSC-derived EVs | – | Regulating the ratios of collagen type III to type I, TGF-β3 to TGF-β1 and MMP-3 to TIMP-1 | ECM reconstruction↑ | [102] | |
| Mouse full-thickness dorsal wound model | ADMSC-derived EVs | miR-125a-3p | PTEN | Angiogenesis↑ | [103] | |
| Corneal epithelial wound model | HucMSC-derived EVs | miR-21 |
PTEN PI3K/Akt signaling pathway |
Corneal wound repair↑ | [104] | |
| Mouse excisional full-thickness wound model | ADMSC-derived EVs (113.6 nm) | miR-192-5p | miR-192-5p/IL-17RA/Smad axis | Anti-fibrotic properties↑ | [105] | |
| Mouse full-thickness skin wound model | TSG-6 overexpressed MSC-derived EVs | – | – |
Scar pathological injury↓ Collagen deposition↓ |
[106] | |
| Mouse full-thickness wound model | ADMSC-derived EVs | – | – |
Collagen expression↓ Scar formation↓ |
[107] | |
| Mouse skin-defective wound model | BMSC-derived EVs (20–200 nm) | miR-223 | PKNOX1 | M2 polarization of macrophages | [108] | |
| Mouse full-thickness skin defect model | HucMSC-derived EVs (30–150 nm) |
miR-21 miR-23a miR-125b miR-145 |
Transforming growth factor-β/Smad2 signaling pathway | Myofibroblast formation↓ | [109] | |
| Murine hind limb ischemia model | EVs released from hP-MSCs by NO stimulation |
VEGF miR-126 |
– | Angiogenic processes↑ | [110] | |
| Diabetic rat wound model | ATV pretreated BMSC (ATV-derived EVs, 80–120 nm) | miR-221-3p | Akt/eNOS signaling pathway | Angiogenesis effect↑ | [111] | |
| Chronic wound | Diabetic rat wound model | HucMSC-derived EVs (30–150 nm) | – | – | VEGF and TGF-β1↑ | [112] |
| Diabetic mouse cutaneous wound model | HucMSC-derived EVs (30–150 nm) | – | – |
Oxidative stress↓ Angiogenesis↑ |
[113] | |
| Eczema mouse wound model | MSC-derived EVs | – | – |
Inflammatory cell infiltration↓ Vascular formation↑ |
[114] | |
| Diabetic mouse wound model | Hypoxic ADMSC-derived EVs |
Upregulated miR-21-3p, miR-126-5p, miR-31-5p Downregulated miR-99b and miR-146-a |
PI3K/Akt signaling pathway |
Diabetic wounds healing↑ Inflammation↓ |
[115] | |
| Diabetic rat cutaneous wound model | LPS‐preconditioning of HucMSC-derived EVs (40–90 nm) | let-7b | let-7b/TLR4 pathway[116] | Regulatory abilities for macrophage polarization | [116] | |
| AD-like chronic allergic dermatitis mouse model | ADMSC-derived EVs | – | Facilitating the de novo synthesis of ceramides | Epidermal barrier functions↑ | [117] | |
| Rat diabetic foot ulcers model | Linc00511-overexpressing ADMSC-derived EVs | – | Suppressing PAQR3-induced Twist1 ubiquitin degradation | Angiogenesis↑ | [118] | |
| Diabetic rat wound model |
hBMSC-derived EVs hBMSC-MT-derived EVs (30–150 nm) |
– | PTEN/Akt pathway | Regulating macrophage M1 and M2 polarization | [26] | |
| SD rat skin photoaging model | ADMSC-derived EVs (30–150 nm) | – | – |
Type I collagen↑ Type III collagen, MMP-1, and MMP-3↓ |
[119] | |
| Wound model | ADMSCs overexpressing Nrf2-EVs | – | – |
Granulation tissue formation↑ Angiogenesis↑ Growth factor expression↑ Oxidative stress-related proteins↓ |
[120] | |
| Diabetic mouse cutaneous wound model | BMSC-derived EVs (50–150 nm) | lncRNA KLF3-AS1 | miR-383, VEGFA | Angiogenesis↑ | [121] | |
| Diabetic rat wound model | BMSCs preconditioned by deferoxamine-derived EVs (50–150 nm) | miR-126 |
PTEN PI3K/Akt signaling pathway |
Wound healing↑ Angiogenesis↑ |
[122] | |
| HucMSC-derived EVs (40–100 nm) | – | Downregulation of monocyte chemotactic protein-1 |
Apoptosis↓ Inflammatory responses↓ |
[100] |
EVs extracellular vesicles, HucMSC human umbilical cord mesenchymal stem cell, MSC mesenchymal stem cell, UCB-MSC umbilical cord blood mesenchymal stem cell, UCMSC umbilical cord mesenchymal stem cell, ADP adenosine diphosphate, BMSC bone marrow mesenchymal stem cell, Exo exosome, hiPSC human-induced pluripotent stem cells, FDMSC fetal dermal mesenchymal stem cell, ADMSC adipose-derived mesenchymal stem cell, MMP matrix metalloproteinases, PTEN phosphatase and tensin homolog deleted on chromosome 10, TSG-6 tumor necrosis factor alpha-stimulated gene 6, PKNOX1 homo sapiens PBX/knotted 1 homeobox 1, Smad Drosophila mothers against decapentaplegic proteins, hP-MSC human placenta-derived mesenchymal stem cell, ATV atorvastatin, LPS lipopolysaccharide, PAQR3 progestin and adipoQ receptor 3, hBMSC human bone marrow mesenchymal stem cell, IL interleukin, VEGFA vascular endothelial growth factor A, eNOS endothelial nitric oxide synthase, TLR toll-like receptor, AD atopic dermatitis
Table 3.
Summary of researches using EVs in vitro to examine wound repair
| Cell type | EVs type | Cargo | Target | Function | References |
|---|---|---|---|---|---|
| Hydrogen peroxide-induced HaCaT cells | HucMSC-derived EVs | miR-150-5p | Activating PI3K/Akt pathway through PTEN |
Apoptosis↓ Skin wound healing↑ |
[123] |
| Hydrogen peroxide-induced HaCaT cells | BMSC-derived EVs | miR-93-3p | miR-93-3p/APAF1 axis |
Proliferation ↑ Migration↑ Apoptosis↓ |
[87] |
| Fibroblast | HucMSC-derived EVs | – | Inhibit the TGF-β1/Smad2/3 signaling pathway | Fibroblasts-myofibroblasts transition↓ | [29] |
| Fibroblast | ADMSC-derived EVs |
miR- 132, miR-21, and miR-29a miR-223, miR-203, miR-146a |
Regulating the M2 phenotype |
M2 macrophage polarization↑ Immune modulation↑ |
[124] |
| Human umbilical vein endothelial cells | ADMSC-derived EVs (80.1 nm) | miR-132 and miR-146a | ROCK1/PTEN pathway |
Anti-inflammatory effects↑ Pro-angiogenic effects↑ |
[125] |
| Hydrogen peroxide-induced HaCaT cells and HDF cells | ADMSC-derived EVs | MALAT1 | Wnt/β-catenin pathway |
Proliferation↑ Migration↑ Apoptosis↓ |
[126] |
HucMSC human umbilical cord mesenchymal stem cell, PI3K phosphoinositide 3-kinase, Akt protein kinase B, BMSC bone marrow mesenchymal stem cell, APAF1 apoptosis protease-activating factor 1, ADMSC adipose-derived mesenchymal stem cell, ROCK1 Rho-associated protein kinase 1, PTEN phosphatase and tensin homolog deleted on chromosome 10, MALAT1 metastasis associated lung adenocarcinoma transcript 1, HDF human dermal fibroblast
Epidermal stem cell-derived EVs contain higher quantities of miRNAs than fibroblast-derived EVs that are related to stimulating cell proliferation and migration, and regulating inflammatory responses [127]. Compared to those of other cellular or humoral (e.g., tumor cells, plant cells, or urine) EVs, the role of MSC-derived EVs in wound repair includes the following: (1) Homing effect. EVs with homing properties can assist in wound healing [107] and can target tumor cells for drug delivery as a cancer therapy [85]. (2) Immunomodulation. Exosomal programmed cell death 1 ligand 1 (PD-L1) inhibits cytokine production by CD8+ T cells while suppressing the number of CD8+ T cells in the spleen and peripheral lymph nodes, thereby accelerating skin cell migration and wound healing in vivo [128]. (3) Antiapoptotic effects. Bone marrow mesenchymal stem cell (BMSC)-derived EVs can activate apoptosis protease-activating factor 1 (APAF1) to inhibit the apoptosis of epithelial HaCaT cells and accelerate the healing of wounds [87]. (4) Anti-inflammatory effects. EVs enhance anti-inflammatory effects by regulating macrophage polarization; for example, BMSC-derived EVs transfer miR-223 targeting homo sapiens PBX/knotted 1 homeobox 1 (PKNOX1) to induce macrophage M2 polarization to promote wound healing [108]. (5) Angiogenesis and promotion of vascular permeability. EVs have significant effects on cell proliferation, angiogenesis, and collagen deposition [47, 48, 94].
It has been reported in preclinical studies that the secretome derived from MSCs obtained from the conditioned media also has significant beneficial functions in skin wound repair [129]. The secretome is defined as a range of molecules produced by a donor cell in the extracellular environment that includes but is not limited to proteins, nucleic acids, proteasomes, EVs, miRNAs, and membrane vesicles [129–131]. Compared to EVs, the secretome contains more bioactive components that have not yet been fully explored, and biological safety is thus not guaranteed. Compared with secretomes, EVs as messengers of intercellular communication to deliver cargo own the benefits of protection against the degradation of cargo, biological targeting, and monitoring ability after artificial modification.
Pretreatment of EVs
Interestingly, the sources, pretreatment methods, culture conditions, and induction conditions of EVs all influence their structure, contents, and effects. EVs from various cell sources act differently, and their efficacy can be enhanced by appropriate pretreatment and induction. The following list details common pretreatment methods. (1) Hypoxia. Hypoxic EVs can upregulate miR-21-3p, miR-126-5p, and miR-31-5p while downregulating miR-99b and miR-146-a, as shown by high-throughput sequencing, indicating that they may play a role in promoting fibroblast proliferation and migration [115]. Chemical pretreatment of EVs to induce hypoxia using compounds such as desferrioxamine (DFO) [122] and valproic acid (VPA) [132] can achieve the same effect as hypoxia. (2) Cytokines. The proinflammatory microenvironment [γ interferon (IFN-γ) and tumour necrosis factor-α (TNF-α)] increases the immunosuppressive and anti-inflammatory potential of adipose-derived mesenchymal stem cell (ADMSC)-derived EVs. Measurable exosomal regulation of M2 phenotype miRNAs (miR-34a-5p, miR-21, and miR-146a-5p) upregulated by cytokine pre-stimulation in ADMSCs mimicking the inflammatory microenvironment induced a shift from the M1 phenotype to the M2 phenotype [88]. (3) Biochemicals such as nitric oxide [110], lipopolysaccharide (LPS) [116], and atorvastatin (ATV) [111]. EVs from MSCs pretreated with ATV and melatonin [26] activated the PTEN/Akt/endothelial nitric oxide synthase (eNOS) signaling pathway, enhancing the angiogenesis of endothelial cells by upregulating miR-211-3p [111] and promoting the activation of M2 macrophages [110]. (4) Light treatment. The exosomal upregulation of miR-135b-5p and miR-499a-3p by MSCs was significantly enhanced under blue light irradiation that stimulated the proangiogenic potential of endothelial cells [133]. (5) Culture conditions. A study has shown that in comparisons of EVs derived from three-dimensional spheroids (3D HDF-XOs) and the monolayer culture of human dermal fibroblast (HDF) (2D HDF-XOs), the former increased the expression of procollagen type I and reduced the expression of MMP-1 to regulate fibroblast activity and induce efficient collagen synthesis, thereby achieving a thicker skin matrix [134].
Pretreatment has been demonstrated to affect EVs’ internal miRNA and protein cargoes [115, 122]. For example, melatonin stimulation increased the ratio of anti-inflammatory to proinflammatory factors in EVs [26], while it did not significantly change the membrane proteins on the surface of EVs [26]. In addition, the effect of pretreatment on the size and yield of EVs varies. One study found that melatonin pretreatment considerably enhanced the size and yield of EVs [135], while another study found no significant differences [26]. The mechanism of pretreatment could involve the regulation of EV biogenesis by triggering exocytosis and autophagy, thus altering EV size, production, and function [73]. Although pretreatment can increase the yield of EVs and their capacity for regenerative repair, it is unclear whether the differences this engenders in the EVs will affect their safety.
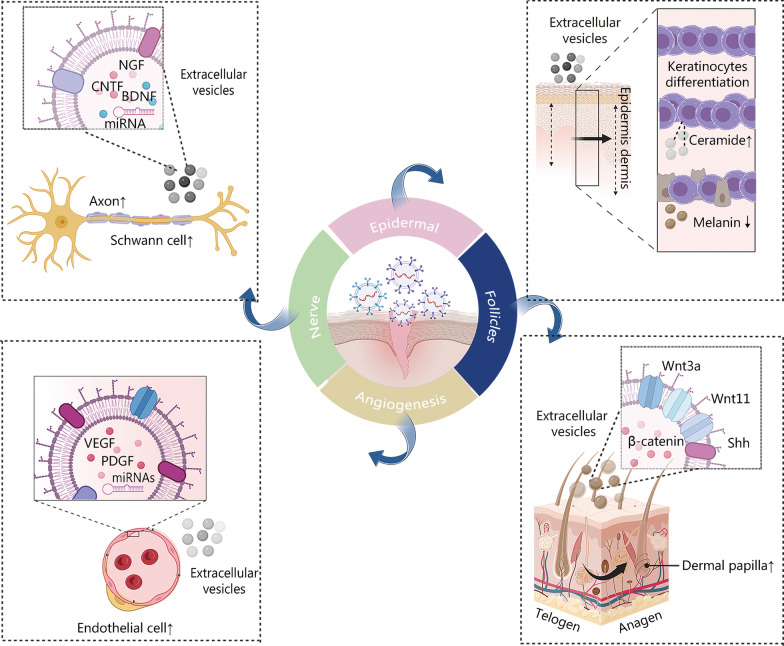
Action of MSC-derived EVs on the skin substructures
The key points of acute and chronic wound repair focus on the anatomical level, including the regeneration and repair of skin sublayers and substructures. MSC-derived EVs assist in tissue regeneration by promoting the regeneration of the epidermis, dermis, hair follicles, nerves, and blood vessels as well as reducing abnormal pigmentation (Fig. 4).
Fig. 4.
Schematic diagram of the effect of extracellular vesicles (EVs) on wound repair. EVs promote axon and Schwann cell proliferation via BDNF, NGF, CNTF, and miRNAs. The VEGF, PDGF, and miRNAs within the EVs promote endothelial cell growth and angiogenesis. EVs also participate in keratinocyte differentiation and facilitate the de novo synthesis of ceramides. Mesenchymal stem cell (MSC)-derived EVs containing Wnt3a and Wnt11 facilitate the reconstruction and proliferation of hair follicles to promote the transition from the telogen to the anagen phase. It was created utilizing the templates on BioRender.com as a reference. BDNF brain-derived neurotrophic factor, NGF nerve growth factor, CNTF ciliary neurotrophic factor, VEGF vascular endothelial growth factor, PDGF platelet-derived growth factor, Wnt wingless/integrated, Shh sonic hedgehog
The epidermis, as the outermost layer of the skin, shields the skin from external bacterial and mechanical damage. It includes accessory structures such as sebaceous glands, sweat glands, and hair follicles [4, 136]. EVs derived from ADMSCs encourage the formation of epidermal lamellar bodies and establish a lamellar layer at the interface between the stratum corneum and granular layers. This action restores the functions of the epidermal permeability barrier by promoting the differentiation of keratinocytes and facilitating the de novo synthesis of ceramides [117]. EV treatment improved trauma recovery by epidermal stratification after burn injury [137] and enhanced epidermal re-epithelialization [98]. Interestingly, EVs reduced the proportion of epidermal stratification and ameliorated skin photodamage in a rat model of photoaged skin [119].
The dermal papilla cells and outer root sheath keratinocytes comprise the hair follicles located in the dermis of the cutaneous layer. The hair follicle development cycle includes the anagen, catagen, and telogen phases [136]. Hair follicles are damaged when trauma defects reach the dermis [138–140]. MSC-derived EVs containing Wnt3a [141] and Wnt11 [142] facilitate the reconstruction and proliferation of hair follicles by enhancing the Wnt/β-catenin pathway and the Shh pathway to promote the transition from the telogen to the anagen phase. A recent study demonstrated significant improvements in hair density and thickness after 12 weeks of ADMSC-derived EVs treatment in 39 patients, none of whom reported serious adverse effects [143]. Melanocytes are the cells responsible for skin and hair pigmentation. EVs from human embryonic MSCs can alleviate hyperpigmentation by inhibiting melanin synthesis and promoting the degradation of melanosomes through miR-181a-5p and miR-199a [144].
The collagenous fibers, fibroblasts, arteries, and nerves that are abundant in the dermis provide strength, nutrition, and sensation to the skin [4, 136]. MSC-derived EVs enhance the amount of new dermis at the trauma surface [114, 119] and promote granulation tissue maturation and epidermal basement membrane structuring in burn wounds [137]. This process also inhibits the formation of hyperplastic scars and keloids through the miR-192-5p/interleukin (IL)-17RA/Smad axis and promotes dermal regeneration [105, 114].
Peripheral nerves are often damaged by acute trauma or chronic diseases such as diabetes mellitus or chronic ulcers. The life quality of patients is compromised by abnormal nerve sensations including pain, pruritus, numbness, and other abnormalities that are induced by infection, inflammation, or improper nerve regeneration [97, 145]. Numerous studies have shown that EVs exert neuroprotective effects by mediating axonal regeneration [97, 146–148], Schwann cell (SC) activation [146, 149], vascular regeneration [113, 122], and modulation of the inflammatory response [150, 151] via the following mechanisms [152]. (1) Promotion of the regeneration of axons. MSC-derived EVs may contain several neurotrophic factors, including nerve growth factor (NGF), brain-derived neurotrophic factor (BDNF), ciliary neurotrophic factor (CNTF), and glial cell line-derived neurotrophic factor [146]. The EVs that are involved in axon regeneration are also rich in histone deacetylases, amyloid A4 protein, and integrin-1 [147]. EVs may be involved in miRNA-mediated regulation of regeneration-related genes, promoting axon proliferation and length increase [97, 148] as well as the recovery of nerve conduction function [43, 150, 153]. (2) Facilitation of SC activation. SCs are the main glial cells of peripheral nerves, and they can be stimulated by EVs to secrete various neurotrophic factors such as NGF [97], BDNF, and CNTF [154]. Those neurotrophic factors then promote peripheral nerve regeneration by enhancing the proliferation, migration, and myelin formation of SCs [146, 149]. In addition, the delivery of mRNAs and miRNAs to support SC repair is another benefit of MSC-derived EVs [146]. This process inhibits SC autophagy by downregulating KPNA2 through miRNA-26b [155], reducing SC apoptosis by upregulating the mRNA expression of the antiapoptotic gene Bcl-2 and downregulating the mRNA expression of the proapoptotic gene Bax [149]. (3) Proangiogenic effects. There is a tight association between vascularization and nerve repair after injury, and EVs promote angiogenesis while facilitating nerve repair. (4) Modulation of inflammation. Inflammation exacerbates neurological dysfunction. M2 macrophages enhance proximal nerve regeneration by producing proteases and growth-promoting factors, promoting Wallerian degeneration and angiogenesis, and regulating SC activity. LPS-pretreated EVs promote macrophage polarization toward the M2 phenotype by inhibiting the nuclear factor kappa-B (NF-κB)/NOD-like receptor protein 3 (NLRP3) axis [151], activating the Toll-like receptor 4/NF-κB signaling pathway, and inhibiting proinflammatory genes [150] to promote peripheral nerve regeneration.
Both acute and chronic trauma under the dermis can result in vascular damage and reduced blood flow. Such a condition can exacerbate tissue hypoxia, induce inflammation, impair wound granulation, and delay tissue regeneration. Studies have shown that EVs promote angiogenesis by enhancing the expression of angiogenesis-related molecules [fibroblast growth factor 1 (FGF-1), vascular endothelial growth factor A (VEGFA), and vascular endothelial growth factor receptor 2 (VEGFR-2)] through miRNAs [110, 125, 133, 156, 157] to ameliorate ischemic injury. Although EVs possess multidirectional repair potential, the process requires optimal donor cells for different trauma conditions to maximize the therapeutic potential of the EVs. Currently, many mechanisms of trauma repair are yet to be elucidated. Hence, one can be optimistic concerning EVs’ potential in regenerative medicine.
Mechanism of MSC-derived EVs in wound healing and anti-scarring
The general wound repair consists of four stages: hemostasis, inflammation, proliferation, and remodeling (or maturation) [3]. Wound repair is a complex biological process that features a staggered timeline for the regeneration of different cell types. Abnormalities in the process can delay wound healing, causing an excessive inflammatory reaction and diminishment of cell proliferation that in turn may induce infection, cause persistent ulceration, and reduce the quality of life. Acute wounds include trauma and empyrosis, while chronic traumas are commonly induced by diabetes, vascular diseases, and aging [4]. Diabetes is a metabolic disorder that affects humans worldwide. Hyperglycemia alters the microenvironment or “soil” as well as the local and circulating cells or “seeds” [4]. The hypoxia response pathway [113], high expression of miR-15a-3p [158], miR-20b-5p interference with vascular endothelial cell function [159], and suppression of macrophage polarization [4] are several key processes in the skin that can cause damage. A hyperglycemic environment induces oxidative stress damage and inflammatory response in vascular endothelial cells and reduces the release of VEGF from multiple cells (macrophages, fibroblasts, and keratinocytes) to inhibit angiogenesis [113, 159].
Hypertrophic scars and keloids are the consequence of enhanced proliferative phases of healing and reduced collagen breakdown [3]. During the inflammatory and proliferative phases, overexpression of VEGF, type I collagen, and tissue inhibitors of metalloproteinase (TIMP)-1 are associated with hypertrophic scarring [160]. Key regulators such as Twist1, FOXO3, and Smad3 are involved in keloid fibroblast fibrogenesis. During the remodeling phase, scars are formed by excessive conversion of collagen type I and type III. Meanwhile, the differentiation of fibroblasts to myofibroblasts is a crucial step in scar tissue formation and involves the TGF-β signaling pathway [161]. Therefore, the fibroblast response during wound healing determines the outcome of tissue repair. It has been demonstrated that compared to wounds that healed with a scar, scarless wounds express more MMPs, particularly MMP-9 and MMP-2. MMP-9 is involved in the degradation of collagen type IV and type V, fibronectin, and elastin [54]. TIMPs, particularly TIMP-1 and TIMP-2, are associated with proliferative scar formation. An abnormal cellular microenvironment also plays an important role; for example, hypoxia can promote the conversion of dermal fibroblasts to myofibroblasts through activation of the TGF-β1/Smad3 signaling pathway, thereby promoting scar formation [162].
The role of EVs in wound repair
The role of EVs in wound repair is reflected in accelerating wound hemostasis, regulating the anti-inflammatory polarity of macrophages, stimulating the proliferation and migration of the vascular endothelial cells and fibroblasts, regulating the cytokine ratio, and remodeling the ECM (Fig. 5). The details are as follows. (1) In the hemostasis phase, due to the increases in phosphatidylserine and tissue factor expression, MSC-derived EVs have a significant procoagulant effect on human blood and platelet-free plasma [83]. (2) In the subsequent inflammation phase, EVs are involved in the amelioration of inflammation. MSC-derived EVs regulated oxidative stress and inflammatory response damage induced by a hyperglycemic environment in diabetic mice [113]. The mechanism may involve inducing the polarization of M2 macrophages and reducing proinflammatory factors (TNF-α, IL-6, and IL-8) [163]. (3) Cell proliferation and angiogenesis are accelerated by EVs in the proliferation phase. BMSC-derived EVs promoted the proliferation and migration of H2O2-injured HaCaT cells and inhibit apoptosis via the miR-93-3p/APAF1 axis in vitro [87]. DFO-pretreated BMSC-derived EVs activated the PI3K/Akt signaling pathway by downregulating PTEN through miR-126, which stimulated in vitro vascular generation [113, 122]. ADMSC-derived EVs increased the S-phase fraction of fibroblasts and stimulated the proliferation of fibroblasts to achieve skin regeneration [164]. (4) Finally, in the remodeling phase, EVs demonstrate antiaging and anti-scarring effects. EVs can ameliorate cellular senescence by reducing fibroblast senescence-associated β-galactosidase and MMP-1/-3 levels [165]. By suppressing the expression levels of ROS and inflammatory factors, ADMSC-derived EVs inhibited high glucose-induced cellular senescence in diabetic rats [120]. Additionally, HDF spheroids cultured in vitro displayed the potential to prevent and treat skin aging [134]. EVs inhibit TGF-β1 by increasing the ratio of type III to type I collagen, TGF-β3 to TGF-β1, and MMP-3 to TIMP-1, and remodeling the ECM by inhibiting the differentiation of fibroblasts into myofibroblasts through the TGF-β2/Smad2 pathway, thereby reducing scar formation and promoting wound healing [166–168].
Fig. 5.
Major events in each phase of mesenchymal stem cell (MSC)-derived extracellular vesicles (EVs)-promoted skin repair. EVs work through the factors in the four phases to accelerate hemostasis, regulate inflammation via processes such as macrophage polarization, promote angiogenesis and cell proliferation, and exhibit anti-aging and anti-scarring abilities. It was created utilizing the templates on BioRender.com as a reference. M1 M1 macrophage, M2 M2 macrophage, IL interleukin, TNF-α tumour necrosis factor-α, TGF-β transforming growth factor-β, ROS reactive oxygen species, TIMP tissue inhibitors of metalloproteinase, VEGF vascular endothelial growth factor, PDGF platelet-derived growth factor, MMP matrix metalloproteinase, ECM extracellular matrix
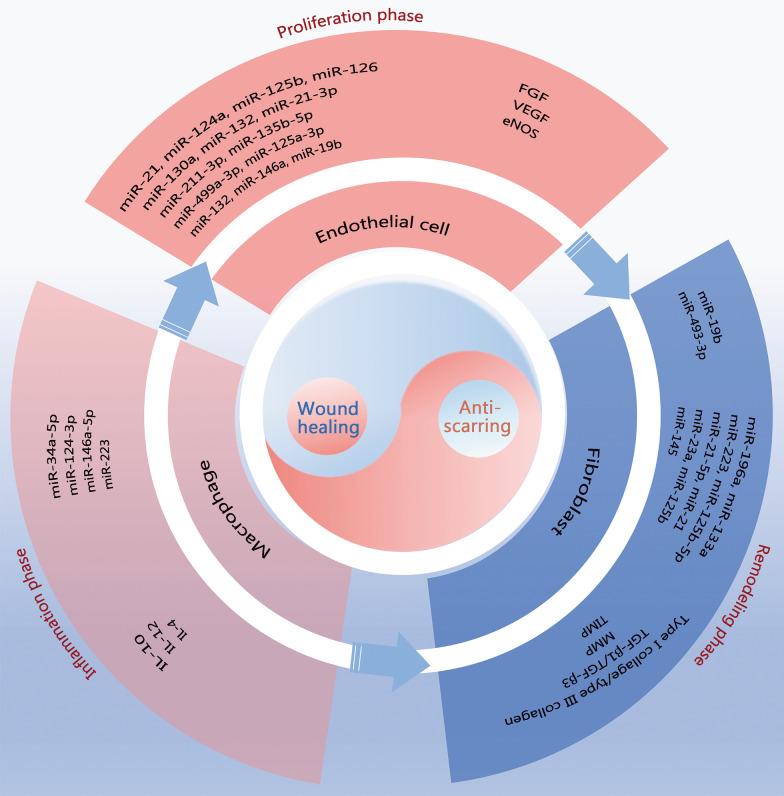
Exosomal roles include regulation at the genetic level, protein level, and metabolic level. The EVs assist and facilitate wound healing in all phases of wound repair (Fig. 6). EVs contain significant quantities of miRNAs and lncRNAs. Numerous studies have demonstrated that EVs are essential for mediating trauma repair at the miRNA level. Tables 4 and 5 present summaries of miRNAs and proteins associated with the roles of EVs in the regulation of angiogenesis, inflammation, and the ECM.
Fig. 6.
Schematic diagram of the role of extracellular vesicles (EVs) in wound repair. EVs have pro-repair and anti-scarring roles through macrophages in the inflammatory phase, through endothelial cells in the proliferative phase, and through fibroblasts in the remodeling phase. EV-associated miRNAs and proteins regulate the activity of these three types of cells. miR micro ribonucleic acid, FGF fibroblast growth factor, VEGF vascular endothelial growth factor, eNOS endothelial nitric oxide synthase, IL interleukin, TGF-β transforming growth factor β, MMP matrix metalloproteinase, TIMP tissue inhibitors of metalloproteinase
Table 4.
Summaries of miRNAs associated with the role of EVs in skin wound repair
| Macrophage polarization | Angiogenesis | Regulate myofibroblast differentiation | Lessen hyperpigmentation |
|---|---|---|---|
|
miR-34a-5p [124] miR-124-3p [124] miR-146a-5p [124] miR-223 [108] miR-181c [96] let-7b [116] |
miR-126 [169] miR-130a [169] miR-132 [169] miR-21-3p [23] miR-211-3p [111] miR-135b-5p [89] miR-499a-3p [89] miR-125a-3p [103] miR-132 [170] miR-146a [125] miR-383 [121] |
miR-223 [134] miR-125b-5p [91] miR-21-5p [91] miR-21 [109] miR-23a [109] miR-125b [109] miR-145 [109] miR-142-3p [171] |
miR-181a-5p [144] miR-199a [144] |
EVs extracellular vesicles
Table 5.
Summaries of proteins associated with the role of EVs in skin wound repair
| Macrophage polarization | Proliferation and migration | Angiogenesis | ECM secretion | Reduction of apoptosis | Nerve regeneration | Follicle growth |
|---|---|---|---|---|---|---|
|
CD73 [172] TSG-6 [173] CCR2 [174] EDA-FN1 [175] |
Wnt11 [142] Jagged1 [101] CD73 [172] Wnt3a [176] TGF-β1 [177] |
Wnt3a [176] NG2 [178] PDGF-D [179] VEGF [180] SDF1/CXCL12 [181] Wnt4 [94] |
CD73 [172] |
Wnt4 [94] MIF [182] |
NGF [146] CNTF [146] BDNF [146] GDNF [146] HDACs [147] APP [147] ITGB1 [147] |
Wnt3a [142] Wnt11 [142] |
EVs extracellular vesicles, TSG-6 tumor necrosis factor alpha-stimulated gene 6, CCR2 C-C motif chemokine receptor-2, EDA-FN1 alternatively spliced domain A-containing fibronectin 1, NG2 neural/glial antigen 2, PDGF-D platelet-derived growth factor D, SDF1 stromal derived factor 1, MIF macrophage migration inhibitory factor, CD cluster of differentiation, Wnt wingless/integrated, TGF-β transforming growth factor-β, VEGF vascular endothelial growth factor, CXCL C-X-C motif chemokine ligand, NGF nerve growth factor, CNTF ciliary neurotrophic factor, BDNF brain-derived neurotrophic factor, GDNF glial cell line-derived neurotrophic factor, HDAC histone deacetylase, APP amyloid-beta A4 protein, ITGB integrin beta
There are some miRNAs involved in different functions, since they may target different cells. For example, miR-21 occurs in three different forms, miR-21, miR-21-3p, and miR-21-5p, and performs two distinct functions. By suppressing PTEN and sprouty homolog 1, miR-21-3p plays a critical role in mediating the pro-angiogenic effects of umbilical cord blood (UCB)-derived EVs on endothelial cells [23]. The miR-21-5p targets TGF-β receptor type II cells to suppress myofibroblast development, thereby minimizing scarring and enhancing regenerative wound healing [91]. In addition, MSC-derived EVs block SC autophagy through miRNA-26b in neuronal repair [155]. EVs can also control melanin metabolism through miR-181a-5p and miR-199a to lessen hyperpigmentation during the later stages of damage repair [144].
EVs can transport protein molecules such as cytokines and enzymes. EVs function as immunomodulatory and anti-inflammatory mediators to facilitate the repair process [166]. First, EVs increase the expression levels of anti-inflammatory factors (IL-10 [167] and IL-4 [183]) while downregulating the expression of proinflammatory factors (IFN-γ, IL-1, IL-6, TNF-α, inducible nitric oxide synthase, cyclooxygenase-2 [168], IL-1β [96], and monocyte chemotactic protein-1 [100]). These functions of EVs promote macrophage M2 phenotype conversion and alleviate the intense inflammatory response in the early stages of injury. Second, EVs simultaneously increase the expression levels of VEGF, FGF, and eNOS to promote endothelial cell neovascularization [121]. EVs also carry several neurotrophic factors that facilitate the proliferation and migration of SCs [146, 154]. Meanwhile, EVs carry Wnt proteins to promote hair growth [139, 142] as previously mentioned. Lastly, reduced TGF-β3 expression may play a role in the formation of keloids [184]. EVs regulate the ratios of TIMP-1 and MMP-3, TGF-β3 and TGF-β1, and type III collagen and type I collagen, and the excessive differentiation of fibroblasts into myofibroblasts to rebuild the ECM and diminish scarring [91, 102, 109]. EVs facilitate the production of collagen I and III in the early stages of wound healing, while in the later stages, EVs can inhibit collagen expression to reduce scar formation [107, 185].
Regarding modulation at the gene and protein levels, EVs are capable of altering cell proliferation and apoptosis. EVs can promote the proliferation and migration of cells and facilitate vascular and ECM formation [169]. EVs regulate the metabolism of hair follicles [138, 139], SCs, and melanin as previously described.
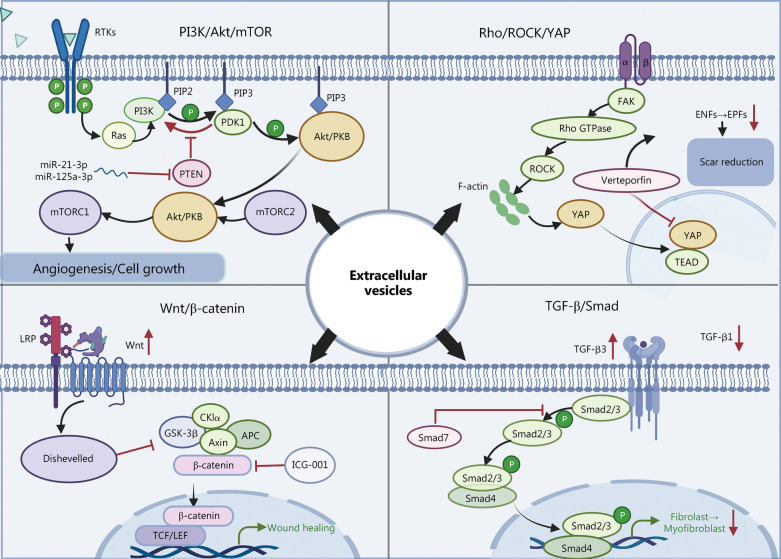
Signaling pathways of EVs involved in wound repair
Previous studies have confirmed that MSC-derived EVs also affect the wound repair process by involvement in a series of signaling pathways (Fig. 7). (1) PI3K/Akt/mTOR pathway. EVs can inhibit PTEN through miR-21 [104], miR-125a-3p [103], miR-126 [24], miR-21-3p [23], miR-150-5p [123], miR-493-3p [186], miR-152-3p [187], and lncRNA H19 [187] that activate the PI3K/Akt/mTOR pathway and promote angiogenesis, the proliferation and migration of fibroblasts and human umbilical vein endothelial cells [23–25], and inhibiting inflammation [26]. For example, hypoxic adipose stem cell EVs significantly induced the production of TGF-β, epidermal growth factor, and basic fibroblast growth factor in fibroblasts and activated the PI3K/Akt signaling pathway to enhance fibroblast proliferation and migration as well as the production of ECM and growth factors [115]. (2) TGF-β/Smad signaling pathway. By inhibiting the TGF-β1/Smad2/3 pathway, EVs downregulated the expression of TGF-β1 while upregulating the expression of TGF-β3 to reduce the phosphorylation levels of Smad2/3. In this way, EVs limited the conversion of fibroblasts to myofibroblasts and reduced the expression of α-SMA to effectively promote scarless skin wound regeneration [28, 29]. EVs were found to be enriched in miR-425-5p [171], miR-142-3p [171], miR-21-5p [91], miR-125b-5p [91], miR-21[109], miR-23a [109], miR-125b [109] and miR-145 [109], and thus play an important role in inhibiting myofibroblast differentiation by decreasing TGF-β1 expression in skin fibroblasts. (3) Wnt/β-catenin pathway. The Wnt/β-catenin pathway is activated in EVs [99], promoting increased expression of proliferating cell nuclear antigen, cyclin D3, N-calmodulin, and B-linked protein and decreased expression of E-calmodulin. These functions promote vascular proliferation for burn wound healing [94, 95, 126, 188]. (4) Rho/ROCK/YAP axis signaling pathway. Exosomes from platelet-rich plasma promote fibroblast proliferation and migration through activation of the Rho/ROCK/YAP axis signaling pathway [189]. Recent research demonstrated that the ROCK/YAP pathway, as a crucial pathway for the conversion of Engrailed-1-negative fibroblasts to Engrailed-1-positive fibroblasts (EPFs), is involved in the mechanism of scar formation related to the formation of EPFs. Thus, scar-free Engrailed regeneration of wounds can be facilitated by blocking the YAP pathway or by eliminating the formation of EPFs [190]. (5) Other pathways. Through the Notch signaling pathway, fetal dermal MSC-derived EVs can stimulate adult dermal fibroblast cell proliferation [101]. Human umbilical cord (Huc) MSC-derived EVs can activate fibroblast pro-wound healing signaling pathways to produce growth factors such as hepatocyte growth factor, IL-6, insulin growth factor-1, NGF, and stromal-derived growth factor-1, thus promoting wound healing [48].
Fig. 7.
Four major signaling pathways of mesenchymal stem cell (MSC)-derived extracellular vesicles (EVs) for skin repair. MSC-derived EVs affect the wound repair process through a series of signaling pathways, including the PI3K/Akt/mTOR pathway, the TGF-β/Smad signaling pathway, the Wnt/β-catenin pathway, and the Rho/ROCK/YAP axis signaling pathway. It was created utilizing the templates on BioRender.com as a reference. PI3K phosphoinositide 3-kinase, Akt protein kinase B, mTOR mammalian target of rapamycin, TGF-β transforming growth factor-β, Smad Drosophila mothers against decapentaplegic proteins, Wnt wingless/integrated, ROCK Rho-associated protein kinase, YAP Yes-associated protein, RTKs receptor tyrosine kinases, Ras Ras protein, PIP2 phosphatidylinositol 4,5-bisphosphate, PIP3 phosphatidylinositol 3,4,5-trisphosphate, PDK phosphoinositide-dependent kinases, PKB protein kinase B, PTEN phosphatase and tensin homolog deleted on chromosome 10, FAK focal adhesion kinase, Rho Ras homology, GTPase guanosine triphosphate hydrolases, TEAD YAP-transcriptional enhancer factor domain family member, ENFs Engrailed-1 lineage-negative fibroblasts, EPFs Engrailed-1 lineage-positive fibroblasts, LRP low-density lipoprotein receptor-related protein, GSK glycogen synthase kinase, APC adenomatous polyposis coli, ICG indocyanine green, TCF/LEF T-cell factor/lymphoid enhancer factor
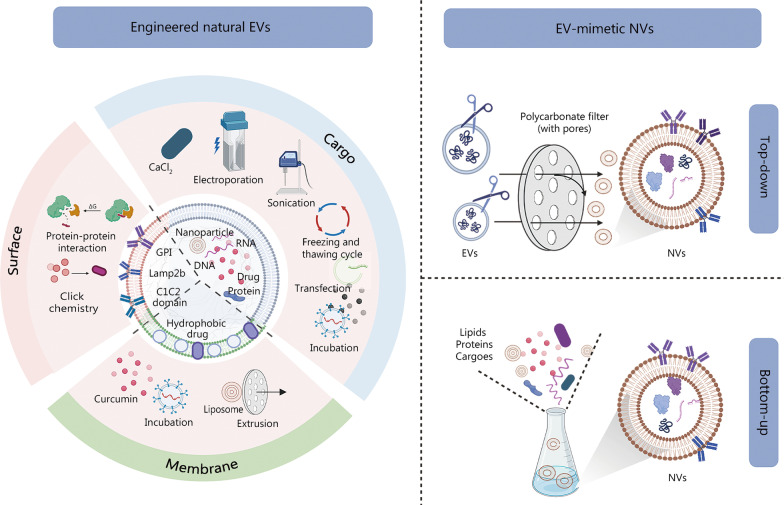
Engineered EVs for wound repair
EVs are utilized as carriers for loading small-molecule cargo such as proteins, nucleic acids, small interfering RNAs (siRNAs), lncRNAs, miRNAs, nanoparticles (NPs), and even clustered regularly interspaced short palindromic repeats/CRISPR-associated protein 9 (CRISPR/Cas9) due to their hydrophobic lipid bilayer and hydrophilic core-specific structure [191]. EVs are biogenic cell-free drug delivery systems with lower biotoxicity and production complexity than synthetic NPs. More importantly, their inherent immunomodulatory and tissue repair-promoting abilities make them extremely valuable in application. Despite the promising innate advantages of EVs, there are drawbacks, such as low targeting efficiency, low yield, limited tissue repair capacity, and restricted drug delivery ability. Therefore, the emergence of modified natural EVs is essential for future clinical translation. Refined drug delivery strategies targeting specific tissues or types of cells can avoid dispersed distribution to other tissues and prevent degradation due to the immune response [192].
Modified natural EVs
Surface and internal modifications can be applied to these structures (Fig. 8). Surface modifications can be engineered to recognize specific cell-surface receptors on membranes for targeted transfer to specific organs, tissues, and cells. For example, the integrin-associated protein CD47 emits a signal that prevents itself from being devoured by macrophages, which enables CD47 to bypass phagocytosis and assist in drug delivery [193]. Iron oxide NP-labeled EVs from NP-treated MSCs significantly enhanced angiogenic tubule formation in vivo and reduced scar formation [194]. Internal modifications involve modifying the cargo structures within EVs [195]. The classification according to cargo properties includes the following four categories: (1) Medicines composed of small molecules such as curcumin and adriamycin. Packaged adriamycin has significant bioactivity, targeting efficiency, and antitumor effects [82] and can penetrate biological barriers and target tumor cells to achieve more precise antitumor therapeutic effects. (2) Molecules of nucleic acids, including siRNAs, lncRNAs, miRNAs, and CRISPR/Cas9. EVs of linc00511-overexpressing ADSCs promoted angiogenesis by inhibiting progestin and adipoQ receptor 3 (PAQR3)-induced Twist1 ubiquitination and attenuated diabetic foot ulcers in rats [118]. (3) Proteins. Tumor necrosis factor alpha-stimulated gene 6 (TSG-6) overexpression in BMSC-derived EVs reduced pathological scar damage by lowering collagen deposition and suppressing inflammation [106]. (4) NPs. Some researchers have loaded EVs with Au NPs to selectively target specific cell types by photoinduced thermotherapy [196]. Currently, miRNAs make up most of the cargo in modified EVs employed in wound repair. For example, EVs carrying overexpressed miR-126 in BMSCs activated the PI3K/Akt pathway by inhibiting PIK3R2, thereby accelerating vascular remodeling [24]. EVs loaded with miR-31-5p were also demonstrated to facilitate diabetic wound repair [197].
Fig. 8.
Schematic diagram of engineered extracellular vesicles (EVs) modification. There are two main methods of EV modification: engineered natural EVs and EV-mimetic nanovesicles (NVs). The former comprises modifications of membranes, surfaces, and cargoes. The latter is divided into top-down and bottom-up methods. It was created utilizing the templates on BioRender.com as a reference. GPI glycosylphosphatidylinositol
There are two types of EV internal loading systems. (1) Pre-exosomal loading. Donor cells are genetically engineered using transfection, or the cargo is co-incubated with donor cells. Although transfection reagents are highly efficient, they can have some drawbacks, including the potential to alter the expression of the target genes in donor cells and the possibility that the remaining transfection reagents may have an impact on the encapsulation process and the behavior of modified EVs [198]. Co-incubation includes some lipid-soluble drugs such as curcumin and adriamycin as well as nucleic acid molecules such as siRNA. For example, cholesterol-conjugated siRNA (cc-siRNA) comprises a duplex region followed by phosphorothioated overhangs and is loaded into EVs by co-incubation [199]. Notably, the conditions such as temperature, period, and the ratio between the drug and EVs are important in these incubation strategies. (2) Postexosomal loading. This refers to cargo loading performed post-isolation of EVs and is divided into physical and chemical methods. The physical loading approach includes methods such as electroporation, sonication, extrusion, and freeze–thaw cycles [191, 200, 201]. Cargoes such as DNA, siRNA, and miRNA can be loaded utilizing electroporation [200, 202, 203]. Electroporation can maintain the integrity and functionality of EVs while encapsulating high level of RNA. However, electroporation is limited by siRNA self-aggregation and deposition, leading to an overestimation of the actual loading efficiency [198]. siRNA self-aggregation and deposition may be due to the quality of the electroporation equipment, buffers, EVs, and drugs [204]. Chemical loading includes saponin permeation and CaCl2 [201]. Saponin-assisted active encapsulation techniques can improve drug loading by up to 11 times [201].
Surface modification strategies rely on chemically loaded membrane modifications such as hydrophobic insertion strategies to mount maleimide onto the EV membrane surface [205]. Click chemistry uses strategies such as copper-catalyzed azide-alkyne cycloaddition to bind molecules to the EV surface [206]. There are also protein gene fusion strategies such as lactocalcin adhesion that specifically bind to phosphatidylserine-rich extracellular membranes via the C1C2 structural domain, depending on the extracellular body membrane. Enhanced targeting can be done by fusion of lysosome-associated membrane glycoprotein 2b with rabies virus glycoprotein [202, 207] and glycosyl phosphatidylinositol-anchored anti-EGFR nanoEVs [208]. However, the possibility of toxic reactions exists due to EVs’ inaccuracy in-target delivery. Donor cells’ extracellular surface and internal components will need to be precisely modified to improve targeting strategies in the future.
EV-mimetic nanovesicles (NVs)
Although engineered natural EVs can have enhanced capacity for regenerative repair and perform specific functions, there is still a lack of isolation and purification procedures to maintain an adequate yield [209]. EV-mimetic NVs, also known as bionic EVs or artificial EVs, are a potential substitute for EVs that have promising clinical applications [210]. These NVs retain the original cell membrane protein structure, and they have a significantly improved cost-effect ratio due to their high yield [211]. A study has demonstrated that EVs and NVs have very similar characteristics in terms of physical properties, key protein markers, liposome characteristics, and in vitro and in vivo behavior [212]. Moreover, cell-engineered NVs made from MSCs productivity is more than 300 times higher than that of natural EVs using spin cups via a cell shearing approach [213]. MSC-NVs have molecular characteristics that more resemble MSCs than MSC-derived EVs [213]. Their protein component contains a significant number of proteins representing the parental cellular proteome, potentially giving NVs an advantage as an alternative nanocarrier when spontaneous endosomal sorting of therapeutic agents is limited [210].
NV synthesis approaches are further divided into two categories (Fig. 8). (1) Top-down-based NP generation techniques use cells as precursors for plasma membrane fragments to produce artificial exosomal NVs. These are prepared using physical methods such as continuous extrusion through 10, 5, and 1 μm polycarbonate membranes [211], shearing [212], and freeze–thaw cycling [214]. (2) A bottom-up strategy is used to assemble individual molecules (lipids, proteins, and cargoes) into fully artificial NPs with pure and well-defined composition [215].
EVs and liposomes have also been combined to enhance the dosage and duration of drug delivery. The preparation methods include extrusion [216], the freeze–thaw method [217], and warm incubation [218]. For example, creating EV and liposome hybrid NPs loaded with expression vectors encapsulating the CRISPR/Cas9 system for genetic modification may be a new strategy for the delivery of CRISPR/Cas9 systems [218]. Based on current studies, NVs have significant potential for treating sepsis [211], promoting hair proliferation [219], improving neurological functions [220], accelerating wound healing [213, 221], and demonstrating antitumor effects [222], and their safety has been confirmed. For example, high-yielding NVs as a lncRNA H19 delivery system have been studied for their ability to neutralize hyperglycemia and significantly accelerate the healing of chronic wounds [221]. Although NVs have the advantages of high yield and convenient extraction, the possibility of lipid flipping as a side effect during their production, such as extrusion of lipid membranes, cannot be ruled out. The possibility of organelle and nuclear contamination during their preparation also needs to be considered. In addition, the variability of the composition of NV contents needs to be determined to ensure the consistency of their use in proteomics and genomics.
Combination strategy for trauma repair
Trauma repair management strategies focus on the early antimicrobial, antioxidant, and anti-inflammatory functions of drugs as well as the later anti-scarring and neurovascular regenerative functions [223]. However, neither natural EVs nor engineered EVs can completely fulfill the diverse needs of wound management. Unfortunately, it is difficult to meet multiple needs of wound management with EVs or engineered EVs alone. Consequently, future wound management may require a combined approach that utilizes two types of vesicles. For example, co-encapsulating MSCs and/or insulin-secreting cells (ISCs) into synthetic hydrogel dressings can provide immunological protection for both cell types and has been shown to improve the function and survival of ISCs. Chronic wound healing is accelerated by the combination of both cell types when they are co-encapsulated in a synthetic hydrogel dressing and is faster than when each cell type is supplied separately [224]. EVs containing antibacterial and antioxidant agents have been combined to treat infected wounds. For example, PUAO-CPO-EXO scaffolds were developed to reduce oxidative stress and deliver continuous oxygen to support tissue repair [225]. CTS-SF/SA/Ag-HucMSC-EVs possess broad-spectrum antibacterial activity, maintain and promote the electrolyte balance of wounds, and optimize wound healing capacity [226]. To achieve better cell proliferation and EV preservation, biopolymers are widely utilized on traumatic surfaces due to their similarity to the ECM regarding physical and biochemical properties. Biomaterials are applied to traumatic surfaces with functions that mimic the physical and biochemical properties of the ECM to achieve better cell proliferation and preservation of EVs. In wound therapy, EVs promote cell adhesion, proliferation, migration, and differentiation, while biomaterials provide scaffolding, biocompatibility, ease of degradation, and prolonged EV release time. Biomaterials, including natural polymers such as chitosan and alginate, have been extensively utilized as wound dressings and drug delivery vehicles either alone or in combination with other polymers to promote wound healing [195]. Synthetic polymers such as polylactic acid, polylactic-co-glycolic acid, and Pluronic F-127 [112, 128, 227] have been employed in EV delivery; these polymers are thermosensitive and can better provide a simulated ECM by forming a gel-like substance compatible with the complex and irregular regions of the wound. Several researchers have combined biomaterials with EVs to enhance wound treatment, thereby achieving excellent results. The research applications and advantages of the combination strategies of biomaterial hydrogels and EVs in recent years are listed in Table 6.
Table 6.
Summary of EVs combined with hydrogels used in wound repair
| Years | Biomaterial type | EV source | Disease model | Feature | References |
|---|---|---|---|---|---|
| 2020 | PF-127 HucMSC-EV hydrogel | HucMSC-derived EVs | SD diabetic rat full-thickness cutaneous skin resection model | Temperature sensitivity | [112] |
| 2021 | HucMSC-EV-loaded genipin-crosslinked hydrogel | HucMSC-derived EVs | Mouse full-thickness cutaneous skin resection model | Biodegradable, temperature and pH sensitive | [228] |
| 2020 | Chitosan hydrogel@ hEnSC-EV | hEnSC-derived EVs | BALB/c mouse full-thickness cutaneous skin resection model | Biodegradable | [229] |
| 2020 | CTS-SF/SA/Ag-Exo dressing | HucMSC-derived EVs | BALB/c male mouse infected full-thickness cutaneous skin resection model | Broad-spectrum antimicrobial activity, promoting wound healing, retaining moisture, maintaining electrolyte balance | [226] |
| 2020 | OxOBand (PUAO-CPO-EXO scaffolds) | ADMSC-derived EVs | Wistar diabetic rat infected full-thickness cutaneous skin resection model | Provide cell migration matrix, provide continuous oxygen to regenerate tissue, reduce oxidative stress, induce angiogenesis and proper collagen remodeling in regenerating tissue | [225] |
| 2019 | PF-127 hydrogel PD-L1-EV | Sk-mel-5 human malignant melanoma cells and B16F10 mouse melanoma cells EVs | BALB/c mouse full-thickness cutaneous skin resection model | Temperature sensitivity, protective effects against infection and inflammation, immunosuppression | [128] |
| 2019 | FHE@EV hydrogel (F127/OHA-EPL ADMSC-EV) | ADMSC-derived EVs | Diabetic mouse full-thickness cutaneous skin resection model | Injectable, self-healing and antibacterial, stimuli-responsive EV release | [227] |
| 2022 | HA@MnO2/FGF-2/Exo hydrogel | M2 macrophage-derived EVs | C57BL/6J diabetic mouse full-thickness cutaneous skin resection model | Rapid hemostasis, long-term antibacterial effects, oxidative stress reduction, oxygenated environment, injectable, adhesive, self-healing, timed release | [230] |
| 2021 | TISSEEL-PEP | Platelet-derived EVs | New Zealand great white rabbit ischemia full-thickness skin resection wound model | Clinical ease of use, promotion of angiogenesis, collagen reorganization, and skin regeneration | [231] |
| 2020 | ADMSC-EV-loaded Alg hydrogel | ADMSC-derived EVs | Wistar rat full-thickness cutaneous skin resection model | High biocompatibility, biodegradability, nonantigenicity, high water absorption | [232] |
| 2019 | FEP@ADMSC-EVs | ADMSC-derived EVs | ICR diabetic mice full-thickness cutaneous skin resection model | Thermosensitivity, injectability, self-healing, adhesion, antimicrobial, hemostasis, UV shielding | [233] |
| 2018 | Curcuma zedoaria polysaccharide PRP-Exos/ZWP | PRP-derived EVs | SD diabetic rat full-thickness cutaneous skin resection model | Hypoglycemic effect and weight loss reduction, hemostatic, antibacterial, biocompatible, and biodegradable | [234] |
| 2017 | GMSC Exos@chitosan/silk hydrogel sponge | GMSC-derived EVs | Diabetic mice full-thickness cutaneous skin resection model | Hemostatic, antibacterial, biocompatible and biodegradable | [90] |
| 2017 | SMSC-126-Exos@chitosan | SMSC-derived EVs | SD diabetic rat full-thickness cutaneous skin resection model | Angiogenesis | [46] |
| 2022 | MSC-Exos@CEC-DCMC HG | BMSC-derived EVs | SD diabetic rat full-thickness cutaneous skin resection model | Regulates the polarity of macrophages, promotion of angiogenesis, antibacterial | [235] |
PF-127 pluronic F-127, EVs extracellular vesicles, HucMSC human umbilical cord mesenchymal stem cell, hEnSC human endometrial stem cell, CTS chitosan, SF silk fibroin, SA stearic acid, PUAO antioxidant polyurethane, CPO calcium peroxide, Exo exosome, ADMSC adipose-derived mesenchymal stem cell, PD-L1 programmed death-ligand 1, OHA oxidized hyaluronic acid, EPL poly-ε-L-lysine, HA hyaluronic acid, MnO2 manganese dioxide, FGF-2 fibroblast growth factor 2, TISSEEL human fibrin seal, PEP platelets exosome product, Alg alginate, PRP-Exos platelet-rich plasma exosomes, ZWP one homogeneous polysaccharide, CEC carboxyethyl chitosan, DCMC dialdehyde carboxymethyl cellulose, HG hydrogel, GMSC gingival mesenchymal stem cell, SMSC synovium mesenchymal stem cell, BMSC bone marrow mesenchymal stem cell
However, achieving targeted homogeneous and sustained delivery of EVs with purely biological scaffolds is a challenge. In contrast, 3D bioprinting, a recently developed technology, allows for well-controlled fiber diameter and porosity. The design provides the mechanical and structural integrity of the scaffold for optimal vascularization and tunable degradation to control the release of the EVs for sustained delivery in long-term therapy. Thus, this method has the potential to improve regenerative outcomes [236]. For regenerative repair, 3D bioprinted scaffolds incorporating MSC-derived EVs have been constructed. For example, 3D-printed ECM/gelatin methacrylate/EV scaffolds promoted chondrocyte migration and the polarization of macrophages to the M2 phenotype for cartilage regeneration [237]. Through an increased crosslinker concentration, the initial EV release rate can be decreased without impacting the bioactivity of EVs [238]. In addition, 3D bioprinted structures loaded with human umbilical vein endothelium-derived EVs can support the in situ formation of new functional blood vessels and ischemic tissues for hemodynamic reconstruction [239]. The benefits and drawbacks of 3D-printed scaffolds compared with pure biological materials for wound treatment have yet to be evaluated. The chemical or physical interactions between EVs and biomaterials and the potential toxicity of residual unreacted crosslinkers during hydrogel manufacturing may affect the function of EVs. Additionally, it is crucial to understand how biomaterials affect the composition and effectiveness of EVs and thus select the corresponding strategy to enhance the material’s characteristics.
Limitations and future perspectives of therapies using EVs derived from MSCs
Although MSC-derived EVs therapy has gained popularity as a cell-free treatment due to its numerous benefits, there are several drawbacks. (1) The absence of standard procedures in EV manufacture, purification, and isolation. In addition, the current EV production methods have the problems of low yield and purity, pragmatic concerns, and economic considerations. An approach to the stable generation of high-yield EVs is needed to achieve wider clinical use of EVs in the future [82]. (2) EVs’ uncertain composition. The composition of EVs may vary depending on the sources and culture conditions. There has yet to be an effective assessment protocol for evaluating the specific contents of EVs. (3) There is at present no information regarding EVs’ carcinogenic effects or their molecular properties in vivo. This therapeutic approach may present risks related to immunological rejection and toxicosis.
To date, several EV-based therapies have entered early clinical trials, ranging from treatments for Alzheimer’s disease to sepsis to coronavirus disease 2019, and all have demonstrated safety and efficacy. Both EV-only and engineered EV delivery platforms have shown no severe side effects in EV-based therapies. However, the clinical trials for wound repair by EVs comprise only a minor proportion of published studies. A summary of EV clinical trials for wound repair is shown in Table 7, including trials involving chronic ulcer and burn repair. In evaluating the safety and efficacy of MSC-derived EVs, prospective, randomized, and double-blind clinical trials are required. This would help to clarify the complications and possible side effects associated with MSC-derived EV treatment. Furthermore, such evaluations would establish an index for future clinical translation in determining the specific dose, route of administration, and optimal concentration of EVs. Currently, optimization of EVs’ generation, isolation and purification, characterization, and storage methods is needed to incorporate EV cell-free therapy for trauma repair safely and effectively.
Table 7.
Summary of clinical trials of EVs in wound repair
| Identifier | Condition or disease | Intervention/treatment | Phase |
|---|---|---|---|
| NCT02565264 | Intractable cutaneous wound ulcer | Plasma-derived EVs | Early phase 1 |
| NCT05078385 | Second degree burn wounds | BMSC-derived EVs | Phase 1 |
| NCT04134676 | Chronic ulcer wounds | Stem cell-conditioned medium | Phase 1 |
| NCT02138331 | Diabetes mellitus type 1 | MSC-derived EVs |
Phase 2 Phase 3 |
| NCT05243368 | Cutaneous ulcers in diabetics | MSC-derived EVs | Not applicable |
| NCT04652531 | Ulcer venous | Autologous EVs from serum | Not applicable |
| NCT05813379 | Skin rejuvenation (Anti-aging) | MSC-derived EVs |
Phase 1 Phase 2 |
| NCT05243368 | Diabetic foot | MSC-derived EVs | Not applicable |
| NCT05475418 | Wounds and injuries | Adipose tissue derived exosomes | Not applicable |
EVs extracellular vesicles, BMSC bone marrow mesenchymal stem cell
Firstly, changes in cell sources and culture conditions may alter EVs’ characteristics and functions. To achieve the best result in trauma treatment, it is therefore necessary to establish a quality control standard for EV production. The standards will provide a reference for different clinical conditions in selecting the best-matched sources of EVs. Commonly encountered clinical conditions include acute wounds (burns, trauma), chronic wounds (diabetic ulcers), and pathological scarring. Identifying the generation and status of EV-derived cells or creating immortalized stem cells is necessary since MSCs change their EV-derived features with cellular senescence. Therefore, specifying the generation and status of EV-derived cells or preparing immortalized stem cells may be effective solutions. The selection of MSCs must be controlled for early generations as well as fixed medium and culture conditions, and for MSCs, the cell morphology needs to be screened for normal rather than senescent forms.
Secondly, the current separation and purification methods are unable to guarantee the content and quality concerning the desired yield. To capture and ensure the desired content for clinical application, the EVs must undergo specification to determine their particle size, content, purity, and classification. Upon meeting the clinical standards, the EVs require new techniques to preserve their capability of activation and lengthen their longevity as carriers. As a consequence, careful consideration should be taken to develop a repeatable, standardized isolation technique that can mass-produce high-purity EVs at an economical cost.
The pharmacokinetics, pharmacodynamics, and biodistribution of each specific EV type in vivo should be determined as well as the optimal dose and route of administration for each disease and target tissue [240]. It is necessary to investigate the differences among EVs from various sources. A comprehensive understanding of EV differences would help to link each EV’s properties with an applicable clinical setting. Although the combination of EVs with biomaterials has demonstrated superior therapeutic efficacy, topical administration remains the main modality of EV use in trauma repair. Scoring standards for different wound types, such as infection, burning, and scarring, should be formulated to select EV biomaterials with corresponding efficacy to achieve clinically defined applications.
Additionally, to develop molecular-level medication therapy, research on the biological mechanisms of EVs should involve the cellular cascade response as well as deeper intrinsic molecular biological mechanisms rather than focusing only on the signaling pathway. Moreover, the identification and functional investigation of the contents of EVs are crucial to exploring the molecular substances that are critical in wound repair. Evaluation and comparisons of the efficacy of EVs will open up new horizons for regenerative medicine.
Finally, it is critical to establish criteria for assessing the efficacy and reliability of EV therapy. Critically evaluating the potential events of each biological response will avoid any inconsistency between preclinical research and clinical application. To ensure the biosafety of EVs, they must undergo clarification of their bioactive components, assessment of immunogenicity and cytotoxicity, and exclusion of potential safety risks before clinical application.
To achieve an “off-the-shelf” safe and effective product for clinical use in acute and chronic wound healing, researchers must overcome the drawbacks associated with EVs, achieve a more standard and high-yield EV production and extraction mode that features clear methodology and biological safety, and improve the accuracy and effectiveness of EV therapy.
Conclusions
MSC-derived EVs have significant potential in promoting wound healing, with the advantages of low immunogenicity, high stability, biodegradability, and barrier-crossing ability. EVs can be employed in the regeneration of vessels, nerves, and hair follicles and can also help achieve early and scar-free wound healing by accelerating hemostasis, improving inflammation, promoting endothelial cell and fibroblast proliferation, inhibiting ECM overproduction, improving tissue remodeling, and inhibiting scar formation. Numerous targets and signaling pathways have been found to be involved in the EV wound repair mechanism. Nevertheless, EVs are not commonly utilized due to their intrinsic drawbacks, including a narrow drug loading space, a limited therapeutic time window, an inability to sustain release, and an incapacity to distribute their cargo according to the shape of a wound. Currently, EVs can be adapted via surface modifications, membrane modifications, internal modifications, or by being used in combination with biological scaffolds to form engineered EVs or NVs that are more effective than EVs alone in wound repair. These methods provide a fresh strategy and direction for current wound regeneration treatment. In the future, EV cell-free therapy is anticipated to become a safe and effective medical treatment at the clinical level if the drawbacks of low yield and biosafety can be overcome. For the large-scale clinical production and utilization of EVs, it is important to standardize and optimize the cell source and culture conditions, select the best isolation, purification, and drug administration protocols, clarify the biological mechanisms, consider biosafety issues, and develop a standardized plan for EV sources and combined biological materials according to different types of trauma. Only in this way is EV cell-free therapy expected to become a clinically safe and effective medical product.
Acknowledgements
The authors would like to acknowledge the Biorender.com software that was used to create the Figs. 1, 2, 3, 4, 5, 7 and 8.
Abbreviations
- ADMSCs
Adipose-derived mesenchymal stromal cells
- BDNF
Brain-derived neurotrophic factor
- BMSC
Bone marrow mesenchymal stem cell
- CNTF
Ciliary neurotrophic factor
- ECM
Extracellular matrix
- EPFs
Engrailed-1-positive fibroblasts
- ESCRT
Endosomal sorting complex required for transport
- EVs
Extracellular vesicles
- LPS
Lipopolysaccharide
- MSC
Mesenchymal stem cell
- MMPs
Matrix metalloproteinases
- MVB
Multivesicular body
- NGF
Nerve growth factor
- NPs
Nanoparticles
- NVs
Nanovesicles
- PAQR3
Progestin and adipoQ receptor 3
- PTEN
Phosphatase and tensin homolog deleted on chromosome 10
- SC
Schwann cell
- TIMP
Tissue inhibitors of metalloproteinase
- UCB
Umbilical cord blood
- VEGF
Vascular endothelial growth factor
- VEGFA
Vascular endothelial growth factor A
- VEGFR-2
Vascular endothelial growth factor receptor 2
Authors' contributions
XKL, ZGW, and JSJ conceived the study, coordinated it, and helped draft the manuscript. JYD and MJC drafted the manuscript and substantively revised it. JYD and MJC designed the figures. LFW and GFS helped revise the figures. SJF and ZYL contributed to manuscript editing. LFW, GFS, SJF, ZYL, and XRC helped revise the manuscript. All authors read and approved the final manuscript.
Funding
This study was supported by the National Key Research and Development Project Intergovernmental Cooperation in Science and Technology of China (2018YFE0126900), the Key R&D Program of Lishui City (2021ZDYF12), and the National Natural Science Foundation of China (82271629).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Jia-Yi Ding and Min-Jiang Chen contributed equally to this work.
Contributor Information
Xiao-Kun Li, Email: xiaokunli@wmu.edu.cn, Email: lixk1964@163.com.
Zhou-Guang Wang, Email: wangzhouguang@wmu.edu.cn, Email: wzhouguang@gmail.com.
Jian-Song Ji, Email: jijiansong@zju.edu.cn.
References
- 1.Sun BK, Siprashvili Z, Khavari PA. Advances in skin grafting and treatment of cutaneous wounds. Science. 2014;346(6212):941–945. doi: 10.1126/science.1253836. [DOI] [PubMed] [Google Scholar]
- 2.Wei S, Wang W, Li L, Meng HY, Feng CZ, Dong YY, et al. Recombinant human epidermal growth factor combined with vacuum sealing drainage for wound healing in Bama pigs. Mil Med Res. 2021;8(1):18. doi: 10.1186/s40779-021-00308-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gantwerker EA, Hom DB. Skin: histology and physiology of wound healing. Facial Plast Surg Clin North Am. 2011;19(3):441–453. doi: 10.1016/j.fsc.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 4.Rodrigues M, Kosaric N, Bonham CA, Gurtner GC. Wound healing: a cellular perspective. Physiol Rev. 2019;99(1):665–706. doi: 10.1152/physrev.00067.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hassanshahi A, Moradzad M, Ghalamkari S, Fadaei M, Cowin AJ, Hassanshahi M. Macrophage-mediated inflammation in skin wound healing. Cells. 2022;11(19):2953. doi: 10.3390/cells11192953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dinh T, Braunagel S, Rosenblum BI. Growth factors in wound healing: The present and the future? Clin Podiatr Med Surg. 2015;32(1):109–119. doi: 10.1016/j.cpm.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 7.Villarreal-Leal RA, Healey GD, Corradetti B. Biomimetic immunomodulation strategies for effective tissue repair and restoration. Adv Drug Deliv Rev. 2021;179:113913. doi: 10.1016/j.addr.2021.113913. [DOI] [PubMed] [Google Scholar]
- 8.Cialdai F, Risaliti C, Monici M. Role of fibroblasts in wound healing and tissue remodeling on Earth and in space. Front Bioeng Biotechnol. 2022;10:958381. doi: 10.3389/fbioe.2022.958381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang PH, Huang BS, Horng HC, Yeh CC, Chen YJ. Wound healing. J Chin Med Assoc. 2018;81(2):94–101. doi: 10.1016/j.jcma.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 10.Li M, Fang F, Sun M, Zhang Y, Hu M, Zhang J. Extracellular vesicles as bioactive nanotherapeutics: an emerging paradigm for regenerative medicine. Theranostics. 2022;12(11):4879–4903. doi: 10.7150/thno.72812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zomer HD, Trentin AG. Skin wound healing in humans and mice: challenges in translational research. J Dermatol Sci. 2018;90(1):3–12. doi: 10.1016/j.jdermsci.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 12.Kirby GT, Mills SJ, Cowin AJ, Smith LE. Stem cells for cutaneous wound healing. Biomed Res Int. 2015;2015:285869. doi: 10.1155/2015/285869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jo H, Brito S, Kwak BM. Applications of mesenchymal stem cells in skin regeneration and rejuvenation. Int J Mol Sci. 2021;22(5):2410. doi: 10.3390/ijms22052410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nuschke A. Activity of mesenchymal stem cells in therapies for chronic skin wound healing. Organogenesis. 2014;10(1):29–37. doi: 10.4161/org.27405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Golchin A, Farahany TZ, Khojasteh A, Soleimanifar F, Ardeshirylajimi A. The clinical trials of mesenchymal stem cell therapy in skin diseases: an update and concise review. Curr Stem Cell Res Ther. 2019;14(1):22–33. doi: 10.2174/1574888X13666180913123424. [DOI] [PubMed] [Google Scholar]
- 16.Kalluri R, LeBleu VS. The biology, function, and biomedical applications of exosomes. Science. 2020;367(6478):eaau6977. doi: 10.1126/science.aau6977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.He C, Zheng S, Luo Y, Wang B. Exosome theranostics: biology and translational medicine. Theranostics. 2018;8(1):237–255. doi: 10.7150/thno.21945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liang Y, Duan L, Lu J, Xia J. Engineering exosomes for targeted drug delivery. Theranostics. 2021;11(7):3183–3195. doi: 10.7150/thno.52570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pegtel DM, Gould SJ. Exosomes. Annu Rev Biochem. 2019;88:487–514. doi: 10.1146/annurev-biochem-013118-111902. [DOI] [PubMed] [Google Scholar]
- 20.Bian D, Wu Y, Song G, Azizi R, Zamani A. The application of mesenchymal stromal cells (MSCs) and their derivative exosome in skin wound healing: a comprehensive review. Stem Cell Res Ther. 2022;13(1):1–17. doi: 10.1186/s13287-021-02697-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hu Y, Tao R, Chen L, Xiong Y, Xue H, Hu L, et al. Exosomes derived from pioglitazone-pretreated MSCs accelerate diabetic wound healing through enhancing angiogenesis. J Nanobiotechnology. 2021;19(1):1–17. doi: 10.1186/s12951-021-00894-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marofi F, Alexandrovna KI, Margiana R, Bahramali M, Suksatan W, Abdelbasset WK, et al. MSCs and their exosomes: a rapidly evolving approach in the context of cutaneous wounds therapy. Stem Cell Res Ther. 2021;12(1):1–20. doi: 10.1186/s13287-021-02662-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hu Y, Rao SS, Wang ZX, Cao J, Tan YJ, Luo J, et al. Exosomes from human umbilical cord blood accelerate cutaneous wound healing through miR-21-3p-mediated promotion of angiogenesis and fibroblast function. Theranostics. 2018;8(1):169–184. doi: 10.7150/thno.21234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang L, Ouyang P, He G, Wang X, Song D, Yang Y, et al. Exosomes from microRNA-126 overexpressing mesenchymal stem cells promote angiogenesis by targeting the PIK3R2-mediated PI3K/Akt signalling pathway. J Cell Mol Med. 2021;25(4):2148–2162. doi: 10.1111/jcmm.16192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wei P, Zhong C, Yang X, Shu F, Xiao S, Gong T, et al. Exosomes derived from human amniotic epithelial cells accelerate diabetic wound healing via PI3K-AKT-mTOR-mediated promotion in angiogenesis and fibroblast function. Burns Trauma. 2020;8:tkaa020. doi: 10.1093/burnst/tkaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu W, Yu M, Xie D, Wang L, Ye C, Zhu Q, et al. Melatonin-stimulated MSC-derived exosomes improve diabetic wound healing through regulating macrophage M1 and M2 polarization by targeting the PTEN/AKT pathway. Stem Cell Res Ther. 2020;11(1):259. doi: 10.1186/s13287-020-01756-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hu Q, Zhang S, Yang Y, Yao JQ, Tang WF, Lyon CJ, et al. Extracellular vesicles in the pathogenesis and treatment of acute lung injury. Mil Med Res. 2022;9(1):61. doi: 10.1186/s40779-022-00417-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jiang T, Wang Z, Sun J. Human bone marrow mesenchymal stem cell-derived exosomes stimulate cutaneous wound healing mediates through TGF-beta/Smad signaling pathway. Stem Cell Res Ther. 2020;11(1):198. doi: 10.1186/s13287-020-01723-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hu J, Chen Y, Huang Y, Su Y. Human umbilical cord mesenchymal stem cell-derived exosomes suppress dermal fibroblasts-myofibroblats transition via inhibiting the TGF-beta1/Smad 2/3 signaling pathway. Exp Mol Pathol. 2020;115:104468. doi: 10.1016/j.yexmp.2020.104468. [DOI] [PubMed] [Google Scholar]
- 30.Moghadasi S, Elveny M, Rahman HS, Suksatan W, Jalil AT, Abdelbasset WK, et al. A paradigm shift in cell-free approach: the emerging role of MSCs-derived exosomes in regenerative medicine. J Transl Med. 2021;19(1):1–21. doi: 10.1186/s12967-021-02980-6. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 31.Bacakova L, Zarubova J, Travnickova M, Musilkova J, Pajorova J, Slepicka P, et al. Stem cells: their source, potency and use in regenerative therapies with focus on adipose-derived stem cells—a review. Biotechnol Adv. 2018;36(4):1111–1126. doi: 10.1016/j.biotechadv.2018.03.011. [DOI] [PubMed] [Google Scholar]
- 32.Friedenstein AJ, Chailakhjan RK, Lalykina KS. The development of fibroblast colonies in monolayer cultures of guinea-pig bone marrow and spleen cells. Cell Tissue Kinet. 1970;3(4):393–403. doi: 10.1111/j.1365-2184.1970.tb00347.x. [DOI] [PubMed] [Google Scholar]
- 33.Lin H, Sohn J, Shen H, Langhans MT, Tuan RS. Bone marrow mesenchymal stem cells: aging and tissue engineering applications to enhance bone healing. Biomaterials. 2019;203:96–110. doi: 10.1016/j.biomaterials.2018.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gentile P, Calabrese C, De Angelis B, Pizzicannella J, Kothari A, Garcovich S. Impact of the different preparation methods to obtain human adipose-derived stromal vascular fraction cells (AD-SVFs) and human adipose-derived mesenchymal stem cells (AD-MSCs): enzymatic digestion versus mechanical centrifugation. Int J Mol Sci. 2019;20(21):5471. doi: 10.3390/ijms20215471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang D, Ni N, Wang Y, Tang Z, Gao H, Ju Y, et al. CircRNA-vgll3 promotes osteogenic differentiation of adipose-derived mesenchymal stem cells via modulating miRNA-dependent integrin alpha5 expression. Cell Death Differ. 2021;28(1):283–302. doi: 10.1038/s41418-020-0600-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee OK, Kuo TK, Chen WM, Lee KD, Hsieh SL, Chen TH. Isolation of multipotent mesenchymal stem cells from umbilical cord blood. Blood. 2004;103(5):1669–1675. doi: 10.1182/blood-2003-05-1670. [DOI] [PubMed] [Google Scholar]
- 37.Mushahary D, Spittler A, Kasper C, Weber V, Charwat V. Isolation, cultivation, and characterization of human mesenchymal stem cells. Cytometry A. 2018;93(1):19–31. doi: 10.1002/cyto.a.23242. [DOI] [PubMed] [Google Scholar]
- 38.Kassem DH, Kamal MM. Wharton’s Jelly MSCs: potential weapon to sharpen for our battle against DM. Trends Endocrinol Metab. 2020;31(4):271–273. doi: 10.1016/j.tem.2020.01.001. [DOI] [PubMed] [Google Scholar]
- 39.Niu X, Li J, Zhao X, Wang Q, Wang G, Hou R, et al. Dermal mesenchymal stem cells: A resource of migration-associated function in psoriasis? Stem Cell Res Ther. 2019;10(1):54. doi: 10.1186/s13287-019-1159-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aamar E, Avigad Laron E, Asaad W, Harshuk-Shabso S, Enshell-Seijffers D. Hair-follicle mesenchymal stem cell activity during homeostasis and wound healing. J Investig Dermatol. 2021;141(12):2797–807.e6. doi: 10.1016/j.jid.2021.05.023. [DOI] [PubMed] [Google Scholar]
- 41.Subhan BS, Kwong J, Kuhn JF, Monas A, Sharma S, Rabbani PS. Amniotic fluid-derived multipotent stromal cells drive diabetic wound healing through modulation of macrophages. J Transl Med. 2021;19(1):16. doi: 10.1186/s12967-020-02674-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cao X, Duan L, Hou H, Liu Y, Chen S, Zhang S, et al. IGF-1C hydrogel improves the therapeutic effects of MSCs on colitis in mice through PGE(2)-mediated M2 macrophage polarization. Theranostics. 2020;10(17):7697–7709. doi: 10.7150/thno.45434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rao F, Zhang D, Fang T, Lu C, Wang B, Ding X, et al. Exosomes from human gingiva-derived mesenchymal stem cells combined with biodegradable chitin conduits promote rat sciatic nerve regeneration. Stem Cells Int. 2019;2019:2546367. doi: 10.1155/2019/2546367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pu W, Xu D, Zhang C, Zhao Z, Yang M. Rapid generation of functional hepatocyte-like cells from human minor salivary gland-derived stem cells. Biochem Biophys Res Commun. 2020;522(3):805–810. doi: 10.1016/j.bbrc.2019.11.173. [DOI] [PubMed] [Google Scholar]
- 45.Chen L, Qu J, Xiang C. The multi-functional roles of menstrual blood-derived stem cells in regenerative medicine. Stem Cell Res Ther. 2019;10(1):1. doi: 10.1186/s13287-018-1105-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tao SC, Guo SC, Li M, Ke QF, Guo YP, Zhang CQ. Chitosan wound dressings incorporating exosomes derived from MicroRNA-126-overexpressing synovium mesenchymal stem cells provide sustained release of exosomes and heal full-thickness skin defects in a diabetic rat model. Stem Cells Transl Med. 2017;6(3):736–747. doi: 10.5966/sctm.2016-0275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang J, Guan J, Niu X, Hu G, Guo S, Li Q, et al. Exosomes released from human induced pluripotent stem cells-derived MSCs facilitate cutaneous wound healing by promoting collagen synthesis and angiogenesis. J Transl Med. 2015;13:49. doi: 10.1186/s12967-015-0417-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shabbir A, Cox A, Rodriguez-Menocal L, Salgado M, Van Badiavas E. Mesenchymal stem cell exosomes induce proliferation and migration of normal and chronic wound fibroblasts, and enhance angiogenesis in vitro. Stem Cells Dev. 2015;24(14):1635–1647. doi: 10.1089/scd.2014.0316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kim WS, Park BS, Sung JH, Yang JM, Park SB, Kwak SJ, et al. Wound healing effect of adipose-derived stem cells: a critical role of secretory factors on human dermal fibroblasts. J Dermatol Sci. 2007;48(1):15–24. doi: 10.1016/j.jdermsci.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 50.Caplan AI, Correa D. The MSC: an injury drugstore. Cell Stem Cell. 2011;9(1):11–15. doi: 10.1016/j.stem.2011.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bjorge IM, Kim SY, Mano JF, Kalionis B, Chrzanowski W. Extracellular vesicles, exosomes and shedding vesicles in regenerative medicine—a new paradigm for tissue repair. Biomater Sci. 2017;6(1):60–78. doi: 10.1039/C7BM00479F. [DOI] [PubMed] [Google Scholar]
- 52.Malhotra P, Shukla M, Meena P, Kakkar A, Khatri N, Nagar RK, et al. Mesenchymal stem cells are prospective novel off-the-shelf wound management tools. Drug Deliv Transl Res. 2022;12(1):79–104. doi: 10.1007/s13346-021-00925-6. [DOI] [PubMed] [Google Scholar]
- 53.Li T, Yan Y, Wang B, Qian H, Zhang X, Shen L, et al. Exosomes derived from human umbilical cord mesenchymal stem cells alleviate liver fibrosis. Stem Cells Dev. 2013;22(6):845–854. doi: 10.1089/scd.2012.0395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lee HJ, Jang YJ. Recent understandings of biology, prophylaxis and treatment strategies for hypertrophic scars and keloids. Int J Mol Sci. 2018;19(3):711. doi: 10.3390/ijms19030711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Las Heras K, Royo F, Garcia-Vallicrosa C, Igartua M, Santos-Vizcaino E, Falcon-Perez JM, et al. Extracellular vesicles from hair follicle-derived mesenchymal stromal cells: isolation, characterization and therapeutic potential for chronic wound healing. Stem Cell Res Ther. 2022;13(1):147. doi: 10.1186/s13287-022-02824-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Goodarzi P, Larijani B, Alavi-Moghadam S, Tayanloo-Beik A, Mohamadi-Jahani F, Ranjbaran N, et al. Mesenchymal stem cells-derived exosomes for wound regeneration. Adv Exp Med Biol. 2018;1119:119–131. doi: 10.1007/5584_2018_251. [DOI] [PubMed] [Google Scholar]
- 57.Harding C, Stahl P. Transferrin recycling in reticulocytes: pH and iron are important determinants of ligand binding and processing. Biochem Biophys Res Commun. 1983;113(2):650–658. doi: 10.1016/0006-291X(83)91776-X. [DOI] [PubMed] [Google Scholar]
- 58.Colombo M, Raposo G, Thery C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annu Rev Cell Dev Biol. 2014;30:255–289. doi: 10.1146/annurev-cellbio-101512-122326. [DOI] [PubMed] [Google Scholar]
- 59.Flaumenhaft R, Mairuhu AT, Italiano JE. Platelet- and megakaryocyte-derived microparticles. Semin Thromb Hemost. 2010;36(8):881–887. doi: 10.1055/s-0030-1267042. [DOI] [PubMed] [Google Scholar]
- 60.Mi B, Chen L, Xiong Y, Yan C, Xue H, Panayi AC, et al. Saliva exosomes-derived UBE2O mRNA promotes angiogenesis in cutaneous wounds by targeting SMAD6. J Nanobiotechnology. 2020;18(1):68. doi: 10.1186/s12951-020-00624-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chen CY, Rao SS, Ren L, Hu XK, Tan YJ, Hu Y, et al. Exosomal DMBT1 from human urine-derived stem cells facilitates diabetic wound repair by promoting angiogenesis. Theranostics. 2018;8(6):1607–1623. doi: 10.7150/thno.22958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Doyle LM, Wang MZ. Overview of extracellular vesicles, their origin, composition, purpose, and methods for exosome isolation and analysis. Cells. 2019;8(7):727. doi: 10.3390/cells8070727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Walsh SA, Hoyt BW, Rowe CJ, Dey D, Davis TA. Alarming cargo: the role of exosomes in trauma-induced inflammation. Biomolecules. 2021;11(4):522. doi: 10.3390/biom11040522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Juan T, Furthauer M. Biogenesis and function of ESCRT-dependent extracellular vesicles. Semin Cell Dev Biol. 2018;74:66–77. doi: 10.1016/j.semcdb.2017.08.022. [DOI] [PubMed] [Google Scholar]
- 65.Hade MD, Suire CN, Mossell J, Suo Z. Extracellular vesicles: emerging frontiers in wound healing. Med Res Rev. 2022;42(6):2102–2125. doi: 10.1002/med.21918. [DOI] [PubMed] [Google Scholar]
- 66.Yang B, Chen Y, Shi J. Exosome biochemistry and advanced nanotechnology for next-generation theranostic platforms. Adv Mater. 2019;31(2):e1802896. doi: 10.1002/adma.201802896. [DOI] [PubMed] [Google Scholar]
- 67.Han QF, Li WJ, Hu KS, Gao J, Zhai WL, Yang JH, et al. Exosome biogenesis: machinery, regulation, and therapeutic implications in cancer. Mol Cancer. 2022;21(1):207. doi: 10.1186/s12943-022-01671-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ostrowski M, Carmo NB, Krumeich S, Fanget I, Raposo G, Savina A, et al. Rab27a and Rab27b control different steps of the exosome secretion pathway. Nat Cell Biol. 2010;12(1):19–30. doi: 10.1038/ncb2000. [DOI] [PubMed] [Google Scholar]
- 69.Wei D, Zhan W, Gao Y, Huang L, Gong R, Wang W, et al. RAB31 marks and controls an ESCRT-independent exosome pathway. Cell Res. 2021;31(2):157–177. doi: 10.1038/s41422-020-00409-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Miller IV, Grunewald TG. Tumour-derived exosomes: tiny envelopes for big stories. Biol Cell. 2015;107(9):287–305. doi: 10.1111/boc.201400095. [DOI] [PubMed] [Google Scholar]
- 71.Thery C, Zitvogel L, Amigorena S. Exosomes: composition, biogenesis and function. Nat Rev Immunol. 2002;2(8):569–579. doi: 10.1038/nri855. [DOI] [PubMed] [Google Scholar]
- 72.Dong R, Liu Y, Yang Y, Wang H, Xu Y, Zhang Z. MSC-derived exosomes-based therapy for peripheral nerve injury: a novel therapeutic strategy. Biomed Res Int. 2019;2019:6458237. doi: 10.1155/2019/6458237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhou Z, Wang R, Wang J, Hao Y, Xie Q, Wang L, et al. Melatonin pretreatment on exosomes: heterogeneity, therapeutic effects, and usage. Front Immunol. 2022;13:933736. doi: 10.3389/fimmu.2022.933736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Toth EA, Turiak L, Visnovitz T, Cserep C, Mazlo A, Sodar BW, et al. Formation of a protein corona on the surface of extracellular vesicles in blood plasma. J Extracell Vesicles. 2021;10(11):e12140. doi: 10.1002/jev2.12140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Buzas EI. Opportunities and challenges in studying the extracellular vesicle corona. Nat Cell Biol. 2022;24(9):1322–1325. doi: 10.1038/s41556-022-00983-z. [DOI] [PubMed] [Google Scholar]
- 76.Wolf M, Poupardin RW, Ebner-Peking P, Andrade AC, Blöchl C, Obermayer A, et al. A functional corona around extracellular vesicles enhances angiogenesis, skin regeneration and immunomodulation. J Extracell Vesicles. 2022;11(4):e12207. doi: 10.1002/jev2.12207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Livshits MA, Khomyakova E, Evtushenko EG, Lazarev VN, Kulemin NA, Semina SE, et al. Isolation of exosomes by differential centrifugation: theoretical analysis of a commonly used protocol. Sci Rep. 2015;5:17319. doi: 10.1038/srep17319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shu S, Yang Y, Allen CL, Hurley E, Tung KH, Minderman H, et al. Purity and yield of melanoma exosomes are dependent on isolation method. J Extracell Vesicles. 2020;9(1):1692401. doi: 10.1080/20013078.2019.1692401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lobb RJ, Becker M, Wen SW, Wong CS, Wiegmans AP, Leimgruber A, et al. Optimized exosome isolation protocol for cell culture supernatant and human plasma. J Extracell Vesicles. 2015;4:27031. doi: 10.3402/jev.v4.27031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Foers AD, Chatfield S, Dagley LF, Scicluna BJ, Webb AI, Cheng L, et al. Enrichment of extracellular vesicles from human synovial fluid using size exclusion chromatography. J Extracell Vesicles. 2018;7(1):1490145. doi: 10.1080/20013078.2018.1490145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Guo SC, Tao SC, Dawn H. Microfluidics-based on-a-chip systems for isolating and analysing extracellular vesicles. J Extracell Vesicles. 2018;7(1):1508271. doi: 10.1080/20013078.2018.1508271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Meng W, He C, Hao Y, Wang L, Li L, Zhu G. Prospects and challenges of extracellular vesicle-based drug delivery system: considering cell source. Drug Deliv. 2020;27(1):585–598. doi: 10.1080/10717544.2020.1748758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Silachev DN, Goryunov KV, Shpilyuk MA, Beznoschenko OS, Morozova NY, Kraevaya EE, et al. Effect of MSCs and MSC-derived extracellular vesicles on human blood coagulation. Cells. 2019;8(3):258. doi: 10.3390/cells8030258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lou G, Chen Z, Zheng M, Liu Y. Mesenchymal stem cell-derived exosomes as a new therapeutic strategy for liver diseases. Exp Mol Med. 2017;49(6):e346. doi: 10.1038/emm.2017.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Garofalo M, Villa A, Crescenti D, Marzagalli M, Kuryk L, Limonta P, et al. Heterologous and cross-species tropism of cancer-derived extracellular vesicles. Theranostics. 2019;9(19):5681–5693. doi: 10.7150/thno.34824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Maji S, Yan IK, Parasramka M, Mohankumar S, Matsuda A, Patel T. In vitro toxicology studies of extracellular vesicles. J Appl Toxicol. 2017;37(3):310–318. doi: 10.1002/jat.3362. [DOI] [PubMed] [Google Scholar]
- 87.Shen C, Tao C, Zhang A, Li X, Guo Y, Wei H, et al. Exosomal microRNA rectangle93 rectangle3p secreted by bone marrow mesenchymal stem cells downregulates apoptotic peptidase activating factor 1 to promote wound healing. Bioengineered. 2022;13(1):27–37. doi: 10.1080/21655979.2021.1997077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Domenis R, Cifu A, Quaglia S, Pistis C, Moretti M, Vicario A, et al. Pro inflammatory stimuli enhance the immunosuppressive functions of adipose mesenchymal stem cells-derived exosomes. Sci Rep. 2018;8(1):13325. doi: 10.1038/s41598-018-31707-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yang K, Li D, Wang M, Xu Z, Chen X, Liu Q, et al. Exposure to blue light stimulates the proangiogenic capability of exosomes derived from human umbilical cord mesenchymal stem cells. Stem Cell Res Ther. 2019;10(1):358. doi: 10.1186/s13287-019-1472-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Shi Q, Qian Z, Liu D, Sun J, Wang X, Liu H, et al. GMSC-derived exosomes combined with a chitosan/silk hydrogel sponge accelerates wound healing in a diabetic rat skin defect model. Front Physiol. 2017;8:904. doi: 10.3389/fphys.2017.00904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhang Y, Pan Y, Liu Y, Li X, Tang L, Duan M, et al. Exosomes derived from human umbilical cord blood mesenchymal stem cells stimulate regenerative wound healing via transforming growth factor-beta receptor inhibition. Stem Cell Res Ther. 2021;12(1):434. doi: 10.1186/s13287-021-02517-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bakhtyar N, Jeschke MG, Herer E, Sheikholeslam M, Amini-Nik S. Exosomes from acellular Wharton's jelly of the human umbilical cord promotes skin wound healing. Stem Cell Res Ther. 2018;9(1):193. doi: 10.1186/s13287-018-0921-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Luo T, Chen SY, Qiu ZX, Miao YR, Ding Y, Pan XY, et al. Transcriptomic features in a single extracellular vesicle via single-cell RNA sequencing. Small Methods. 2022;6(11):e2200881. doi: 10.1002/smtd.202200881. [DOI] [PubMed] [Google Scholar]
- 94.Zhang B, Wu X, Zhang X, Sun Y, Yan Y, Shi H, et al. Human umbilical cord mesenchymal stem cell exosomes enhance angiogenesis through the Wnt4/beta-catenin pathway. Stem Cells Transl Med. 2015;4(5):513–522. doi: 10.5966/sctm.2014-0267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zhang B, Wang M, Gong A, Zhang X, Wu X, Zhu Y, et al. HucMSC-exosome mediated-Wnt4 signaling is required for cutaneous wound healing. Stem Cells. 2015;33(7):2158–2168. doi: 10.1002/stem.1771. [DOI] [PubMed] [Google Scholar]
- 96.Li X, Liu L, Yang J, Yu Y, Chai J, Wang L, et al. Exosome derived from human umbilical cord mesenchymal stem cell mediates miR-181c attenuating burn-induced excessive inflammation. EBioMedicine. 2016;8:72–82. doi: 10.1016/j.ebiom.2016.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhu Z, Zhang X, Hao H, Xu H, Shu J, Hou Q, et al. Exosomes derived from umbilical cord mesenchymal stem cells treat cutaneous nerve damage and promote wound healing. Front Cell Neurosci. 2022;16:913009. doi: 10.3389/fncel.2022.913009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zhao G, Liu F, Liu Z, Zuo K, Wang B, Zhang Y, et al. MSC-derived exosomes attenuate cell death through suppressing AIF nucleus translocation and enhance cutaneous wound healing. Stem Cell Res Ther. 2020;11(1):174. doi: 10.1186/s13287-020-01616-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zhang B, Shi Y, Gong A, Pan Z, Shi H, Yang H, et al. HucMSC exosome-delivered 14-3-3zeta orchestrates self-control of the Wnt response via modulation of YAP during cutaneous regeneration. Stem Cells. 2016;34(10):2485–2500. doi: 10.1002/stem.2432. [DOI] [PubMed] [Google Scholar]
- 100.Yu B, Shao H, Su C, Jiang Y, Chen X, Bai L, et al. Exosomes derived from MSCs ameliorate retinal laser injury partially by inhibition of MCP-1. Sci Rep. 2016;6:34562. doi: 10.1038/srep34562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wang X, Jiao Y, Pan Y, Zhang L, Gong H, Qi Y, et al. Fetal dermal mesenchymal stem cell-derived exosomes accelerate cutaneous wound healing by activating notch signaling. Stem Cells Int. 2019;2019:2402916. doi: 10.1155/2019/2402916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wang L, Hu L, Zhou X, Xiong Z, Zhang C, Shehada HMA, et al. Exosomes secreted by human adipose mesenchymal stem cells promote scarless cutaneous repair by regulating extracellular matrix remodelling. Sci Rep. 2017;7(1):13321. doi: 10.1038/s41598-017-12919-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Pi L, Yang L, Fang BR, Meng XX, Qian L. Exosomal microRNA-125a-3p from human adipose-derived mesenchymal stem cells promotes angiogenesis of wound healing through inhibiting PTEN. Mol Cell Biochem. 2022;477(1):115–127. doi: 10.1007/s11010-021-04251-w. [DOI] [PubMed] [Google Scholar]
- 104.Liu X, Li X, Wu G, Qi P, Zhang Y, Liu Z, et al. Umbilical cord mesenchymal stem cell-derived small extracellular vesicles deliver miR-21 to promote corneal epithelial wound healing through PTEN/PI3K/Akt pathway. Stem Cells Int. 2022;2022:1252557. doi: 10.1155/2022/1252557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Li Y, Zhang J, Shi J, Liu K, Wang X, Jia Y, et al. Exosomes derived from human adipose mesenchymal stem cells attenuate hypertrophic scar fibrosis by miR-192-5p/IL-17RA/Smad axis. Stem Cell Res Ther. 2021;12(1):221. doi: 10.1186/s13287-021-02290-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Jiang L, Zhang Y, Liu T, Wang X, Wang H, Song H, et al. Exosomes derived from TSG-6 modified mesenchymal stromal cells attenuate scar formation during wound healing. Biochimie. 2020;177:40–49. doi: 10.1016/j.biochi.2020.08.003. [DOI] [PubMed] [Google Scholar]
- 107.Hu L, Wang J, Zhou X, Xiong Z, Zhao J, Yu R, et al. Exosomes derived from human adipose mensenchymal stem cells accelerates cutaneous wound healing via optimizing the characteristics of fibroblasts. Sci Rep. 2016;6:32993. doi: 10.1038/srep32993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.He X, Dong Z, Cao Y, Wang H, Liu S, Liao L, et al. MSC-derived exosome promotes M2 polarization and enhances cutaneous wound healing. Stem Cells Int. 2019;2019:7132708. doi: 10.1155/2019/7132708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Fang S, Xu C, Zhang Y, Xue C, Yang C, Bi H, et al. Umbilical cord-derived mesenchymal stem cell-derived exosomal microRNAs suppress myofibroblast differentiation by inhibiting the transforming growth factor-beta/SMAD2 pathway during wound healing. Stem Cells Transl Med. 2016;5(10):1425–1439. doi: 10.5966/sctm.2015-0367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Du W, Zhang K, Zhang S, Wang R, Nie Y, Tao H, et al. Enhanced proangiogenic potential of mesenchymal stem cell-derived exosomes stimulated by a nitric oxide releasing polymer. Biomaterials. 2017;133:70–81. doi: 10.1016/j.biomaterials.2017.04.030. [DOI] [PubMed] [Google Scholar]
- 111.Yu M, Liu W, Li J, Lu J, Lu H, Jia W, et al. Exosomes derived from atorvastatin-pretreated MSC accelerate diabetic wound repair by enhancing angiogenesis via AKT/eNOS pathway. Stem Cell Res Ther. 2020;11(1):350. doi: 10.1186/s13287-020-01824-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yang J, Chen Z, Pan D, Li H, Shen J. Umbilical cord-derived mesenchymal stem cell-derived exosomes combined pluronic F127 hydrogel promote chronic diabetic wound healing and complete skin regeneration. Int J Nanomed. 2020;15:5911–5926. doi: 10.2147/IJN.S249129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Yan C, Xv Y, Lin Z, Endo Y, Xue H, Hu Y, et al. Human umbilical cord mesenchymal stem cell-derived exosomes accelerate diabetic wound healing via ameliorating oxidative stress and promoting angiogenesis. Front Bioeng Biotechnol. 2022;10:829868. doi: 10.3389/fbioe.2022.829868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Wang M, Zhao Y, Zhang Q. Human mesenchymal stem cell-derived exosomes accelerate wound healing of mice eczema. J Dermatol Treat. 2022;33(3):1401–1405. doi: 10.1080/09546634.2020.1820935. [DOI] [PubMed] [Google Scholar]
- 115.Wang J, Wu H, Peng Y, Zhao Y, Qin Y, Zhang Y, et al. Hypoxia adipose stem cell-derived exosomes promote high-quality healing of diabetic wound involves activation of PI3K/Akt pathways. J Nanobiotechnol. 2021;19(1):202. doi: 10.1186/s12951-021-00942-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ti D, Hao H, Tong C, Liu J, Dong L, Zheng J, et al. LPS-preconditioned mesenchymal stromal cells modify macrophage polarization for resolution of chronic inflammation via exosome-shuttled let-7b. J Transl Med. 2015;13:308. doi: 10.1186/s12967-015-0642-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Shin KO, Ha DH, Kim JO, Crumrine DA, Meyer JM, Wakefield JS, et al. Exosomes from human adipose tissue-derived mesenchymal stem cells promote epidermal barrier repair by inducing de novo synthesis of ceramides in atopic dermatitis. Cells. 2020;9(3):680. doi: 10.3390/cells9030680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Qiu J, Shu C, Li X, Ye C, Zhang WC. Exosomes from linc00511-overexpressing ADSCs accelerates angiogenesis in diabetic foot ulcers healing by suppressing PAQR3-induced Twist1 degradation. Diabetes Res Clin Pract. 2021;180:109032. doi: 10.1016/j.diabres.2021.109032. [DOI] [PubMed] [Google Scholar]
- 119.Liang JX, Liao X, Li SH, Jiang X, Li ZH, Wu YD, et al. Antiaging properties of exosomes from adipose-derived mesenchymal stem cells in photoaged rat skin. Biomed Res Int. 2020;2020:6406395. doi: 10.1155/2020/6406395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Li X, Xie X, Lian W, Shi R, Han S, Zhang H, et al. Exosomes from adipose-derived stem cells overexpressing Nrf2 accelerate cutaneous wound healing by promoting vascularization in a diabetic foot ulcer rat model. Exp Mol Med. 2018;50(4):1–14. doi: 10.1038/s12276-018-0058-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Han ZF, Cao JH, Liu ZY, Yang Z, Qi RX, Xu HL. Exosomal lncRNA KLF3-AS1 derived from bone marrow mesenchymal stem cells stimulates angiogenesis to promote diabetic cutaneous wound healing. Diabetes Res Clin Pract. 2022;183:109126. doi: 10.1016/j.diabres.2021.109126. [DOI] [PubMed] [Google Scholar]
- 122.Ding J, Wang X, Chen B, Zhang J, Xu J. Exosomes derived from human bone marrow mesenchymal stem cells stimulated by deferoxamine accelerate cutaneous wound healing by promoting angiogenesis. Biomed Res Int. 2019;2019:9742765. doi: 10.1155/2019/9742765. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 123.Xiu C, Zheng H, Jiang M, Li J, Zhou Y, Mu L, et al. MSCs-derived miR-150-5p-expressing exosomes promote skin wound healing by activating PI3K/AKT pathway through PTEN. Int J Stem Cells. 2022;15(4):359–371. doi: 10.15283/ijsc21135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Heo JS, Kim S, Yang CE, Choi Y, Song SY, Kim HO. Human adipose mesenchymal stem cell-derived exosomes: a key player in wound healing. Tissue Eng Regen Med. 2021;18(4):537–548. doi: 10.1007/s13770-020-00316-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Heo JS, Kim S. Human adipose mesenchymal stem cells modulate inflammation and angiogenesis through exosomes. Sci Rep. 2022;12(1):2776. doi: 10.1038/s41598-022-06824-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.He L, Zhu C, Jia J, Hao XY, Yu XY, Liu XY, et al. ADSC-Exos containing MALAT1 promotes wound healing by targeting miR-124 through activating Wnt/beta-catenin pathway. Biosci Rep. 2020;40(5):BSR20192549. doi: 10.1042/BSR20192549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Wang P, Theocharidis G, Vlachos IS, Kounas K, Lobao A, Shu B, et al. Exosomes derived from epidermal stem cells improve diabetic wound healing. J Investig Dermatol. 2022;142(9):2508–2517.e13. doi: 10.1016/j.jid.2022.01.030. [DOI] [PubMed] [Google Scholar]
- 128.Su D, Tsai HI, Xu Z, Yan F, Wu Y, Xiao Y, et al. Exosomal PD-L1 functions as an immunosuppressant to promote wound healing. J Extracell Vesicles. 2019;9(1):1709262. doi: 10.1080/20013078.2019.1709262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Marques da Silva M, Olsson DC, Teixeira BL, Jeremias TDS, Trentin AG. Mesenchymal stromal cell-secretome for therapeutic application in skin wound healing: a systematic review of preclinical studies. Cells Tissues Organs. 2022 doi: 10.1159/000526093. [DOI] [PubMed] [Google Scholar]
- 130.Gemayel J, Chaker D, El Hachem G, Mhanna M, Salemeh R, Hanna C, et al. Mesenchymal stem cells-derived secretome and extracellular vesicles: perspective and challenges in cancer therapy and clinical applications. Clin Transl Oncol. 2023;25(7):2056–2068. doi: 10.1007/s12094-023-03115-7. [DOI] [PubMed] [Google Scholar]
- 131.Ibrahim R, Mndlovu H, Kumar P, Adeyemi SA, Choonara YE. Cell secretome strategies for controlled drug delivery and wound-healing applications. Polymers (Basel) 2022;14(14):2929. doi: 10.3390/polym14142929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.An SY, Han J, Lim HJ, Park SY, Kim JH, Do BR, et al. Valproic acid promotes differentiation of hepatocyte-like cells from whole human umbilical cord-derived mesenchymal stem cells. Tissue Cell. 2014;46(2):127–135. doi: 10.1016/j.tice.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 133.Jing X, Yang F, Shao C, Wei K, Xie M, Shen H, et al. Role of hypoxia in cancer therapy by regulating the tumor microenvironment. Mol Cancer. 2019;18(1):157. doi: 10.1186/s12943-019-1089-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Hu S, Li Z, Cores J, Huang K, Su T, Dinh PU, et al. Needle-free injection of exosomes derived from human dermal fibroblast spheroids ameliorates skin photoaging. ACS Nano. 2019;13(10):11273–11282. doi: 10.1021/acsnano.9b04384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Abd-Elhafeez HH, Mokhtar DM, Hassan AH. Effect of melatonin on telocytes in the seminal vesicle of the soay ram: an immunohistochemical, ultrastructural and morphometrical Study. Cells Tissues Organs. 2017;203(1):29–54. doi: 10.1159/000449500. [DOI] [PubMed] [Google Scholar]
- 136.Ha DH, Kim HK, Lee J, Kwon HH, Park GH, Yang SH, et al. Mesenchymal stem/stromal cell-derived exosomes for immunomodulatory therapeutics and skin regeneration. Cells. 2020;9(5):1157. doi: 10.3390/cells9051157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Liliac IM, Popescu EL, Vaduva IA, Pirici D, Mogosanu GD, Streba CT, et al. Nanoparticle-functionalized dressings for the treatment of third-degree skin burns - histopathological and immunohistochemical study. Rom J Morphol Embryol. 2021;62(1):159–168. doi: 10.47162/RJME.62.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hu S, Li Z, Lutz H, Huang K, Su T, Cores J, et al. Dermal exosomes containing miR-218-5p promote hair regeneration by regulating beta-catenin signaling. Sci Adv. 2020;6(30):eaba1685. doi: 10.1126/sciadv.aba1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Kim H, Jang Y, Kim EH, Jang H, Cho H, Han G, et al. Potential of colostrum-derived exosomes for promoting hair regeneration through the transition from telogen to anagen phase. Front Cell Dev Biol. 2022;10:815205. doi: 10.3389/fcell.2022.815205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Carrasco E, Soto-Heredero G, Mittelbrunn M. The role of extracellular vesicles in cutaneous remodeling and hair follicle dynamics. Int J Mol Sci. 2019;20(11):2758. doi: 10.3390/ijms20112758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Li J, Zhao B, Dai Y, Zhang X, Chen Y, Wu X. Exosomes Derived from dermal papilla cells mediate hair follicle stem cell proliferation through the Wnt3a/beta-catenin signaling pathway. Oxid Med Cell Longev. 2022;2022:9042345. doi: 10.1155/2022/9042345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Shi H, Xu X, Zhang B, Xu J, Pan Z, Gong A, et al. 3,3'-Diindolylmethane stimulates exosomal Wnt11 autocrine signaling in human umbilical cord mesenchymal stem cells to enhance wound healing. Theranostics. 2017;7(6):1674–1688. doi: 10.7150/thno.18082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Park BS, Choi HI, Huh G, Kim WS. Effects of exosome from adipose-derived stem cell on hair loss: a retrospective analysis of 39 patients. J Cosmet Dermatol. 2022;21(5):2282–2284. doi: 10.1111/jocd.14846. [DOI] [PubMed] [Google Scholar]
- 144.Wang XY, Guan XH, Yu ZP, Wu J, Huang QM, Deng KY, et al. Human amniotic stem cells-derived exosmal miR-181a-5p and miR-199a inhibit melanogenesis and promote melanosome degradation in skin hyperpigmentation, respectively. Stem Cell Res Ther. 2021;12(1):501. doi: 10.1186/s13287-021-02570-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Wang M, Huang X, Zheng H, Tang Y, Zeng K, Shao L, et al. Nanomaterials applied in wound healing: mechanisms, limitations and perspectives. J Control Release. 2021;337:236–247. doi: 10.1016/j.jconrel.2021.07.017. [DOI] [PubMed] [Google Scholar]
- 146.Haertinger M, Weiss T, Mann A, Tabi A, Brandel V, Radtke C. Adipose stem cell-derived extracellular vesicles induce proliferation of schwann cells via internalization. Cells. 2020;9(1):163. doi: 10.3390/cells9010163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Rau CS, Kuo PJ, Wu SC, Huang LH, Lu TH, Wu YC, et al. Enhanced nerve regeneration by exosomes secreted by adipose-derived stem cells with or without FK506 stimulation. Int J Mol Sci. 2021;22(16):8545. doi: 10.3390/ijms22168545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Zhao J, Ding Y, He R, Huang K, Liu L, Jiang C, et al. Dose-effect relationship and molecular mechanism by which BMSC-derived exosomes promote peripheral nerve regeneration after crush injury. Stem Cell Res Ther. 2020;11(1):360. doi: 10.1186/s13287-020-01872-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Liu CY, Yin G, Sun YD, Lin YF, Xie Z, English AW, et al. Effect of exosomes from adipose-derived stem cells on the apoptosis of Schwann cells in peripheral nerve injury. CNS Neurosci Ther. 2020;26(2):189–196. doi: 10.1111/cns.13187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Fan B, Li C, Szalad A, Wang L, Pan W, Zhang R, et al. Mesenchymal stromal cell-derived exosomes ameliorate peripheral neuropathy in a mouse model of diabetes. Diabetologia. 2020;63(2):431–443. doi: 10.1007/s00125-019-05043-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Li C, Li X, Shi Z, Wu P, Fu J, Tang J, et al. Exosomes from LPS-preconditioned bone marrow MSCs accelerated peripheral nerve regeneration via M2 macrophage polarization: involvement of TSG-6/NF-kappaB/NLRP3 signaling pathway. Exp Neurol. 2022;356:114139. doi: 10.1016/j.expneurol.2022.114139. [DOI] [PubMed] [Google Scholar]
- 152.Yu T, Xu Y, Ahmad MA, Javed R, Hagiwara H, Tian X. Exosomes as a promising therapeutic strategy for peripheral nerve injury. Curr Neuropharmacol. 2021;19(12):2141–2151. doi: 10.2174/1570159X19666210203161559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Fan B, Chopp M, Zhang ZG, Liu XS. Treatment of diabetic peripheral neuropathy with engineered mesenchymal stromal cell-derived exosomes enriched with microRNA-146a provide amplified therapeutic efficacy. Exp Neurol. 2021;341:113694. doi: 10.1016/j.expneurol.2021.113694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Chen J, Ren S, Duscher D, Kang Y, Liu Y, Wang C, et al. Exosomes from human adipose-derived stem cells promote sciatic nerve regeneration via optimizing Schwann cell function. J Cell Physiol. 2019;234(12):23097–23110. doi: 10.1002/jcp.28873. [DOI] [PubMed] [Google Scholar]
- 155.Yin G, Yu B, Liu C, Lin Y, Xie Z, Hu Y, et al. Exosomes produced by adipose-derived stem cells inhibit schwann cells autophagy and promote the regeneration of the myelin sheath. Int J Biochem Cell Biol. 2021;132:105921. doi: 10.1016/j.biocel.2021.105921. [DOI] [PubMed] [Google Scholar]
- 156.Yan B, Zhang Y, Liang C, Liu B, Ding F, Wang Y, et al. Stem cell-derived exosomes prevent pyroptosis and repair ischemic muscle injury through a novel exosome/circHIPK3/FOXO3a pathway. Theranostics. 2020;10(15):6728–6742. doi: 10.7150/thno.42259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Li X, Jiang C, Zhao J. Human endothelial progenitor cells-derived exosomes accelerate cutaneous wound healing in diabetic rats by promoting endothelial function. J Diabetes Complicat. 2016;30(6):986–992. doi: 10.1016/j.jdiacomp.2016.05.009. [DOI] [PubMed] [Google Scholar]
- 158.Xiong Y, Chen L, Yu T, Yan C, Zhou W, Cao F, et al. Inhibition of circulating exosomal microRNA-15a-3p accelerates diabetic wound repair. Aging (Albany NY) 2020;12(10):8968–8986. doi: 10.18632/aging.103143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Xiong Y, Chen L, Yan C, Zhou W, Endo Y, Liu J, et al. Circulating exosomal miR-20b-5p inhibition restores Wnt9b signaling and reverses diabetes-associated impaired wound healing. Small. 2020;16(3):e1904044. doi: 10.1002/smll.201904044. [DOI] [PubMed] [Google Scholar]
- 160.Wang P, Jiang LZ, Xue B. Recombinant human endostatin reduces hypertrophic scar formation in rabbit ear model through down-regulation of VEGF and TIMP-1. Afr Health Sci. 2016;16(2):542–553. doi: 10.4314/ahs.v16i2.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Liu X, Chen W, Zeng Q, Ma B, Li Z, Meng T, et al. Single-cell RNA-sequencing reveals lineage-specific regulatory changes of fibroblasts and vascular endothelial cells in Keloids. J Investig Dermatol. 2022;142(1):124–35.e11. doi: 10.1016/j.jid.2021.06.010. [DOI] [PubMed] [Google Scholar]
- 162.Zhao B, Guan H, Liu JQ, Zheng Z, Zhou Q, Zhang J, et al. Hypoxia drives the transition of human dermal fibroblasts to a myofibroblast-like phenotype via the TGF-beta1/Smad3 pathway. Int J Mol Med. 2017;39(1):153–159. doi: 10.3892/ijmm.2016.2816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Han X, Wu P, Li L, Sahal HM, Ji C, Zhang J, et al. Exosomes derived from autologous dermal fibroblasts promote diabetic cutaneous wound healing through the Akt/beta-catenin pathway. Cell Cycle. 2021;20(5–6):616–629. doi: 10.1080/15384101.2021.1894813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Choi EW, Seo MK, Woo EY, Kim SH, Park EJ, Kim S. Exosomes from human adipose-derived stem cells promote proliferation and migration of skin fibroblasts. Exp Dermatol. 2018;27(10):1170–1172. doi: 10.1111/exd.13451. [DOI] [PubMed] [Google Scholar]
- 165.Oh M, Lee J, Kim YJ, Rhee WJ, Park JH. Exosomes derived from human induced pluripotent stem cells ameliorate the aging of skin fibroblasts. Int J Mol Sci. 2018;19(6):1715. doi: 10.3390/ijms19061715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Wu P, Zhang B, Shi H, Qian H, Xu W. MSC-exosome: a novel cell-free therapy for cutaneous regeneration. Cytotherapy. 2018;20(3):291–301. doi: 10.1016/j.jcyt.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 167.Eirin A, Zhu XY, Puranik AS, Tang H, McGurren KA, van Wijnen AJ, et al. Mesenchymal stem cell-derived extracellular vesicles attenuate kidney inflammation. Kidney Int. 2017;92(1):114–124. doi: 10.1016/j.kint.2016.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Yang J, Liu XX, Fan H, Tang Q, Shou ZX, Zuo DM, et al. Extracellular vesicles derived from bone marrow mesenchymal stem cells protect against experimental colitis via attenuating colon inflammation, oxidative stress and apoptosis. PLoS One. 2015;10(10):e0140551. doi: 10.1371/journal.pone.0140551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Geiger A, Walker A, Nissen E. Human fibrocyte-derived exosomes accelerate wound healing in genetically diabetic mice. Biochem Biophys Res Commun. 2015;467(2):303–309. doi: 10.1016/j.bbrc.2015.09.166. [DOI] [PubMed] [Google Scholar]
- 170.Ma T, Chen Y, Chen Y, Meng Q, Sun J, Shao L, et al. MicroRNA-132, delivered by mesenchymal stem cell-derived exosomes, promote angiogenesis in myocardial infarction. Stem Cells Int. 2018;2018:3290372. doi: 10.1155/2018/3290372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Duan M, Zhang Y, Zhang H, Meng Y, Qian M, Zhang G. Epidermal stem cell-derived exosomes promote skin regeneration by downregulating transforming growth factor-beta1 in wound healing. Stem Cell Res Ther. 2020;11(1):452. doi: 10.1186/s13287-020-01971-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Amarnath S, Foley JE, Farthing DE, Gress RE, Laurence A, Eckhaus MA, et al. Bone marrow-derived mesenchymal stromal cells harness purinergenic signaling to tolerize human Th1 cells in vivo. Stem Cells. 2015;33(4):1200–1212. doi: 10.1002/stem.1934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.An JH, Li Q, Ryu MO, Nam AR, Bhang DH, Jung YC, et al. TSG-6 in extracellular vesicles from canine mesenchymal stem/stromal is a major factor in relieving DSS-induced colitis. PLoS One. 2020;15(2):e0220756. doi: 10.1371/journal.pone.0220756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Shen B, Liu J, Zhang F, Wang Y, Qin Y, Zhou Z, et al. CCR2 positive exosome released by mesenchymal stem cells suppresses macrophage functions and alleviates ischemia/reperfusion-induced renal injury. Stem Cells Int. 2016;2016:1240301. doi: 10.1155/2016/1240301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Zhang B, Yin Y, Lai RC, Tan SS, Choo AB, Lim SK. Mesenchymal stem cells secrete immunologically active exosomes. Stem Cells Dev. 2014;23(11):1233–1244. doi: 10.1089/scd.2013.0479. [DOI] [PubMed] [Google Scholar]
- 176.McBride JD, Rodriguez-Menocal L, Guzman W, Candanedo A, Garcia-Contreras M, Badiavas EV. Bone marrow mesenchymal stem cell-derived CD63+ exosomes transport Wnt3a exteriorly and enhance dermal fibroblast proliferation, migration, and angiogenesis in vitro. Stem Cells Dev. 2017;26(19):1384–1398. doi: 10.1089/scd.2017.0087. [DOI] [PubMed] [Google Scholar]
- 177.Fan Y, Herr F, Vernochet A, Mennesson B, Oberlin E, Durrbach A. Human fetal liver mesenchymal stem cell-derived exosomes impair natural killer cell function. Stem Cells Dev. 2019;28(1):44–55. doi: 10.1089/scd.2018.0015. [DOI] [PubMed] [Google Scholar]
- 178.Barilani M, Peli V, Cherubini A, Dossena M, Dolo V, Lazzari L. NG2 as an identity and quality marker of mesenchymal stem cell extracellular vesicles. Cells. 2019;8(12):1524. doi: 10.3390/cells8121524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Ma J, Zhao Y, Sun L, Sun X, Zhao X, Sun X, et al. Exosomes derived from Akt-modified human umbilical cord mesenchymal stem cells improve cardiac regeneration and promote angiogenesis via activating platelet-derived growth factor D. Stem Cells Transl Med. 2017;6(1):51–59. doi: 10.5966/sctm.2016-0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Ahn SY, Park WS, Kim YE, Sung DK, Sung SI, Ahn JY, et al. Vascular endothelial growth factor mediates the therapeutic efficacy of mesenchymal stem cell-derived extracellular vesicles against neonatal hyperoxic lung injury. Exp Mol Med. 2018;50(4):1–12. doi: 10.1038/s12276-018-0055-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Gong XH, Liu H, Wang SJ, Liang SW, Wang GG. Exosomes derived from SDF1-overexpressing mesenchymal stem cells inhibit ischemic myocardial cell apoptosis and promote cardiac endothelial microvascular regeneration in mice with myocardial infarction. J Cell Physiol. 2019;234(8):13878–13893. doi: 10.1002/jcp.28070. [DOI] [PubMed] [Google Scholar]
- 182.Liu X, Li X, Zhu W, Zhang Y, Hong Y, Liang X, et al. Exosomes from mesenchymal stem cells overexpressing MIF enhance myocardial repair. J Cell Physiol. 2020;235(11):8010–8022. doi: 10.1002/jcp.29456. [DOI] [PubMed] [Google Scholar]
- 183.Heidari N, Abbasi-Kenarsari H, Namaki S, Baghaei K, Zali MR, Ghaffari Khaligh S, et al. Adipose-derived mesenchymal stem cell-secreted exosome alleviates dextran sulfate sodium-induced acute colitis by Treg cell induction and inflammatory cytokine reduction. J Cell Physiol. 2021;236(8):5906–5920. doi: 10.1002/jcp.30275. [DOI] [PubMed] [Google Scholar]
- 184.Bock O, Yu H, Zitron S, Bayat A, Ferguson MW, Mrowietz U. Studies of transforming growth factors beta 1–3 and their receptors I and II in fibroblast of keloids and hypertrophic scars. Acta Derm Venereol. 2005;85(3):216–220. doi: 10.1080/00015550410025453. [DOI] [PubMed] [Google Scholar]
- 185.Hu P, Yang Q, Wang Q, Shi C, Wang D, Armato U, et al. Mesenchymal stromal cells-exosomes: a promising cell-free therapeutic tool for wound healing and cutaneous regeneration. Burns Trauma. 2019;7:38. doi: 10.1186/s41038-019-0178-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Zhu Z, Chen B, Peng L, Gao S, Guo J, Zhu X. Blockade of LINC01605-enriched exosome generation in M2 macrophages impairs M2 macrophage-induced proliferation, migration, and invasion of human dermal fibroblasts. Int J Immunopathol Pharmacol. 2021;35:20587384211016724. doi: 10.1177/20587384211016724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Li B, Luan S, Chen J, Zhou Y, Wang T, Li Z, et al. The MSC-derived exosomal lncRNA H19 promotes wound healing in diabetic foot ulcers by upregulating PTEN via microRNA-152-3p. Mol Ther Nucleic Acids. 2020;19:814–826. doi: 10.1016/j.omtn.2019.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Ma T, Fu B, Yang X, Xiao Y, Pan M. Adipose mesenchymal stem cell-derived exosomes promote cell proliferation, migration, and inhibit cell apoptosis via Wnt/beta-catenin signaling in cutaneous wound healing. J Cell Biochem. 2019;120(6):10847–10854. doi: 10.1002/jcb.28376. [DOI] [PubMed] [Google Scholar]
- 189.Guo SC, Tao SC, Yin WJ, Qi X, Yuan T, Zhang CQ. Exosomes derived from platelet-rich plasma promote the re-epithelization of chronic cutaneous wounds via activation of YAP in a diabetic rat model. Theranostics. 2017;7(1):81–96. doi: 10.7150/thno.16803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Mascharak S, des Jardins-Park HE, Davitt MF, Griffin M, Borrelli MR, Moore AL, et al. Preventing Engrailed-1 activation in fibroblasts yields wound regeneration without scarring. Science. 2021;372(6540):eaba2374. doi: 10.1126/science.aba2374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Villata S, Canta M, Cauda V. EVs and bioengineering: from cellular products to engineered nanomachines. Int J Mol Sci. 2020;21(17):6048. doi: 10.3390/ijms21176048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Xu M, Yang Q, Sun X, Wang Y. Recent advancements in the loading and modification of therapeutic exosomes. Front Bioeng Biotechnol. 2020;8:586130. doi: 10.3389/fbioe.2020.586130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Villa F, Quarto R, Tasso R. Extracellular vesicles as natural, safe and efficient drug delivery systems. Pharmaceutics. 2019;11(11):557. doi: 10.3390/pharmaceutics11110557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Li X, Wang Y, Shi L, Li B, Li J, Wei Z, et al. Magnetic targeting enhances the cutaneous wound healing effects of human mesenchymal stem cell-derived iron oxide exosomes. J Nanobiotechnology. 2020;18(1):113. doi: 10.1186/s12951-020-00670-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Golchin A, Shams F, Basiri A, Ranjbarvan P, Kiani S, Sarkhosh-Inanlou R, et al. Combination therapy of stem cell-derived exosomes and biomaterials in the wound healing. Stem Cell Rev Rep. 2022;18(6):1892–1911. doi: 10.1007/s12015-021-10309-5. [DOI] [PubMed] [Google Scholar]
- 196.Pan S, Pei L, Zhang A, Zhang Y, Zhang C, Huang M, et al. Passion fruit-like exosome-PMA/Au-BSA@Ce6 nanovehicles for real-time fluorescence imaging and enhanced targeted photodynamic therapy with deep penetration and superior retention behavior in tumor. Biomaterials. 2020;230:119606. doi: 10.1016/j.biomaterials.2019.119606. [DOI] [PubMed] [Google Scholar]
- 197.Huang J, Yu M, Yin W, Liang B, Li A, Li J, et al. Development of a novel RNAi therapy: engineered miR-31 exosomes promoted the healing of diabetic wounds. Bioact Mater. 2021;6(9):2841–2853. doi: 10.1016/j.bioactmat.2021.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Kooijmans SAA, Stremersch S, Braeckmans K, de Smedt SC, Hendrix A, Wood MJA, et al. Electroporation-induced siRNA precipitation obscures the efficiency of siRNA loading into extracellular vesicles. J Control Release. 2013;172(1):229–238. doi: 10.1016/j.jconrel.2013.08.014. [DOI] [PubMed] [Google Scholar]
- 199.O’Loughlin AJ, Mager I, de Jong OG, Varela MA, Schiffelers RM, El Andaloussi S, et al. Functional delivery of lipid-conjugated siRNA by extracellular vesicles. Mol Ther. 2017;25(7):1580–1587. doi: 10.1016/j.ymthe.2017.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Lamichhane TN, Raiker RS, Jay SM. Exogenous DNA loading into extracellular vesicles via electroporation is size-dependent and enables limited gene delivery. Mol Pharm. 2015;12(10):3650–3657. doi: 10.1021/acs.molpharmaceut.5b00364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Fuhrmann G, Serio A, Mazo M, Nair R, Stevens MM. Active loading into extracellular vesicles significantly improves the cellular uptake and photodynamic effect of porphyrins. J Control Release. 2015;205:35–44. doi: 10.1016/j.jconrel.2014.11.029. [DOI] [PubMed] [Google Scholar]
- 202.Alvarez-Erviti L, Seow Y, Yin H, Betts C, Lakhal S, Wood MJ. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat Biotechnol. 2011;29(4):341–345. doi: 10.1038/nbt.1807. [DOI] [PubMed] [Google Scholar]
- 203.Wahlgren J, De LKT, Brisslert M, Vaziri Sani F, Telemo E, Sunnerhagen P, et al. Plasma exosomes can deliver exogenous short interfering RNA to monocytes and lymphocytes. Nucleic Acids Res. 2012;40(17):e130. doi: 10.1093/nar/gks463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Nasiri Kenari A, Cheng L, Hill AF. Methods for loading therapeutics into extracellular vesicles and generating extracellular vesicles mimetic-nanovesicles. Methods. 2020;177:103–113. doi: 10.1016/j.ymeth.2020.01.001. [DOI] [PubMed] [Google Scholar]
- 205.Di H, Zeng E, Zhang P, Liu X, Zhang C, Yang J, et al. General approach to engineering extracellular vesicles for biomedical analysis. Anal Chem. 2019;91(20):12752–12759. doi: 10.1021/acs.analchem.9b02268. [DOI] [PubMed] [Google Scholar]
- 206.Smyth T, Petrova K, Payton NM, Persaud I, Redzic JS, Graner MW, et al. Surface functionalization of exosomes using click chemistry. Bioconjug Chem. 2014;25(10):1777–1784. doi: 10.1021/bc500291r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Yang J, Zhang X, Chen X, Wang L, Yang G. Exosome mediated delivery of miR-124 promotes neurogenesis after ischemia. Mol Ther Nucleic Acids. 2017;7:278–287. doi: 10.1016/j.omtn.2017.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Kooijmans SA, Aleza CG, Roffler SR, van Solinge WW, Vader P, Schiffelers RM. Display of GPI-anchored anti-EGFR nanobodies on extracellular vesicles promotes tumour cell targeting. J Extracell Vesicles. 2016;5:31053. doi: 10.3402/jev.v5.31053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Jo W, Kim J, Yoon J, Jeong D, Cho S, Jeong H, et al. Large-scale generation of cell-derived nanovesicles. Nanoscale. 2014;6(20):12056–12064. doi: 10.1039/C4NR02391A. [DOI] [PubMed] [Google Scholar]
- 210.Nasiri Kenari A, Kastaniegaard K, Greening DW, Shambrook M, Stensballe A, Cheng L, et al. Proteomic and post-translational modification profiling of exosome-mimetic nanovesicles compared to exosomes. Proteomics. 2019;19(8):e1800161. doi: 10.1002/pmic.201800161. [DOI] [PubMed] [Google Scholar]
- 211.Park KS, Svennerholm K, Shelke GV, Bandeira E, Lasser C, Jang SC, et al. Mesenchymal stromal cell-derived nanovesicles ameliorate bacterial outer membrane vesicle-induced sepsis via IL-10. Stem Cell Res Ther. 2019;10(1):231. doi: 10.1186/s13287-019-1352-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Goh WJ, Zou S, Ong WY, Torta F, Alexandra AF, Schiffelers RM, et al. Bioinspired cell-derived nanovesicles versus exosomes as drug delivery systems: a cost-effective alternative. Sci Rep. 2017;7(1):14322. doi: 10.1038/s41598-017-14725-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Han C, Jeong D, Kim B, Jo W, Kang H, Cho S, et al. Mesenchymal stem cell engineered nanovesicles for accelerated skin wound closure. ACS Biomater Sci Eng. 2019;5(3):1534–1543. doi: 10.1021/acsbiomaterials.8b01646. [DOI] [PubMed] [Google Scholar]
- 214.Ko KW, Yoo YI, Kim JY, Choi B, Park SB, Park W, et al. Attenuation of tumor necrosis factor-alpha induced inflammation by umbilical cord-mesenchymal stem cell derived exosome-mimetic nanovesicles in endothelial cells. Tissue Eng Regen Med. 2020;17(2):155–163. doi: 10.1007/s13770-019-00234-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Garcia-Manrique P, Matos M, Gutierrez G, Pazos C, Blanco-Lopez MC. Therapeutic biomaterials based on extracellular vesicles: classification of bio-engineering and mimetic preparation routes. J Extracell Vesicles. 2018;7(1):1422676. doi: 10.1080/20013078.2017.1422676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Sun L, Fan M, Huang D, Li B, Xu R, Gao F, et al. Clodronate-loaded liposomal and fibroblast-derived exosomal hybrid system for enhanced drug delivery to pulmonary fibrosis. Biomaterials. 2021;271:120761. doi: 10.1016/j.biomaterials.2021.120761. [DOI] [PubMed] [Google Scholar]
- 217.Cheng L, Zhang X, Tang J, Lv Q, Liu J. Gene-engineered exosomes-thermosensitive liposomes hybrid nanovesicles by the blockade of CD47 signal for combined photothermal therapy and cancer immunotherapy. Biomaterials. 2021;275:120964. doi: 10.1016/j.biomaterials.2021.120964. [DOI] [PubMed] [Google Scholar]
- 218.Lin Y, Wu J, Gu W, Huang Y, Tong Z, Huang L, et al. Exosome-liposome hybrid nanoparticles deliver CRISPR/Cas9 system in MSCs. Adv Sci (Weinh) 2018;5(4):1700611. doi: 10.1002/advs.201700611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Cao L, Tian T, Huang Y, Tao S, Zhu X, Yang M, et al. Neural progenitor cell-derived nanovesicles promote hair follicle growth via miR-100. J Nanobiotechnol. 2021;19(1):20. doi: 10.1186/s12951-020-00757-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Dong X, Gao J, Zhang CY, Hayworth C, Frank M, Wang Z. Neutrophil membrane-derived nanovesicles alleviate inflammation to protect mouse brain injury from ischemic stroke. ACS Nano. 2019;13(2):1272–1283. doi: 10.1021/acsnano.8b06572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Tao SC, Rui BY, Wang QY, Zhou D, Zhang Y, Guo SC. Extracellular vesicle-mimetic nanovesicles transport LncRNA-H19 as competing endogenous RNA for the treatment of diabetic wounds. Drug Deliv. 2018;25(1):241–255. doi: 10.1080/10717544.2018.1425774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Tang J, Su T, Huang K, Dinh PU, Wang Z, Vandergriff A, et al. Targeted repair of heart injury by stem cells fused with platelet nanovesicles. Nat Biomed Eng. 2018;2:17–26. doi: 10.1038/s41551-017-0182-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Conese M, Portincasa A. Mesenchymal stem cells, secretome and biomaterials in in-vivo animal models: regenerative medicine application in cutaneous wound healing. Biocell. 2022;46(8):1815–1826. doi: 10.32604/biocell.2022.019448. [DOI] [Google Scholar]
- 224.Aijaz A, Teryek M, Goedken M, Polunas M, Olabisi RM. Coencapsulation of ISCs and MSCs enhances viability and function of both cell types for improved wound healing. Cell Mol Bioeng. 2019;12(5):481–493. doi: 10.1007/s12195-019-00582-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Shiekh PA, Singh A, Kumar A. Exosome laden oxygen releasing antioxidant and antibacterial cryogel wound dressing OxOBand alleviate diabetic and infectious wound healing. Biomaterials. 2020;249:120020. doi: 10.1016/j.biomaterials.2020.120020. [DOI] [PubMed] [Google Scholar]
- 226.Qian Z, Bai Y, Zhou J, Li L, Na J, Fan Y, et al. A moisturizing chitosan-silk fibroin dressing with silver nanoparticles-adsorbed exosomes for repairing infected wounds. J Mater Chem B. 2020;8(32):7197–7212. doi: 10.1039/D0TB01100B. [DOI] [PubMed] [Google Scholar]
- 227.Wang C, Wang M, Xu T, Zhang X, Lin C, Gao W, et al. Engineering bioactive self-healing antibacterial exosomes hydrogel for promoting chronic diabetic wound healing and complete skin regeneration. Theranostics. 2019;9(1):65–76. doi: 10.7150/thno.29766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Li Q, Gong S, Yao W, Yang Z, Wang R, Yu Z, et al. Exosome loaded genipin crosslinked hydrogel facilitates full thickness cutaneous wound healing in rat animal model. Drug Deliv. 2021;28(1):884–893. doi: 10.1080/10717544.2021.1912210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Nooshabadi VT, Khanmohamadi M, Valipour E, Mahdipour S, Salati A, Malekshahi ZV, et al. Impact of exosome-loaded chitosan hydrogel in wound repair and layered dermal reconstitution in mice animal model. J Biomed Mater Res A. 2020;108(11):2138–2149. doi: 10.1002/jbm.a.36959. [DOI] [PubMed] [Google Scholar]
- 230.Xiong Y, Chen L, Liu P, Yu T, Lin C, Yan C, et al. All-in-one: multifunctional hydrogel accelerates oxidative diabetic wound healing through timed-release of exosome and fibroblast growth factor. Small. 2022;18(1):e2104229. doi: 10.1002/smll.202104229. [DOI] [PubMed] [Google Scholar]
- 231.Shi A, Li J, Qiu X, Sabbah M, Boroumand S, Huang TC, et al. TGF-beta loaded exosome enhances ischemic wound healing in vitro and in vivo. Theranostics. 2021;11(13):6616–6631. doi: 10.7150/thno.57701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Shafei S, Khanmohammadi M, Heidari R, Ghanbari H, Taghdiri Nooshabadi V, Farzamfar S, et al. Exosome loaded alginate hydrogel promotes tissue regeneration in full-thickness skin wounds: an in vivo study. J Biomed Mater Res A. 2020;108(3):545–556. doi: 10.1002/jbm.a.36835. [DOI] [PubMed] [Google Scholar]
- 233.Wang M, Wang C, Chen M, Xi Y, Cheng W, Mao C, et al. Efficient angiogenesis-based diabetic wound healing/skin reconstruction through bioactive antibacterial adhesive ultraviolet shielding nanodressing with exosome release. ACS Nano. 2019;13(9):10279–10293. doi: 10.1021/acsnano.9b03656. [DOI] [PubMed] [Google Scholar]
- 234.Xu N, Wang L, Guan J, Tang C, He N, Zhang W, et al. Wound healing effects of a Curcuma zedoaria polysaccharide with platelet-rich plasma exosomes assembled on chitosan/silk hydrogel sponge in a diabetic rat model. Int J Biol Macromol. 2018;117:102–107. doi: 10.1016/j.ijbiomac.2018.05.066. [DOI] [PubMed] [Google Scholar]
- 235.Geng X, Qi Y, Liu X, Shi Y, Li H, Zhao L. A multifunctional antibacterial and self-healing hydrogel laden with bone marrow mesenchymal stem cell-derived exosomes for accelerating diabetic wound healing. Biomater Adv. 2022;133:112613. doi: 10.1016/j.msec.2021.112613. [DOI] [PubMed] [Google Scholar]
- 236.Han P, Ivanovski S. 3D bioprinted extracellular vesicles for tissue engineering - a perspective. Biofabrication. 2022 doi: 10.1088/1758-5090/ac9809. [DOI] [PubMed] [Google Scholar]
- 237.Chen P, Zheng L, Wang Y, Tao M, Xie Z, Xia C, et al. Desktop-stereolithography 3D printing of a radially oriented extracellular matrix/mesenchymal stem cell exosome bioink for osteochondral defect regeneration. Theranostics. 2019;9(9):2439–2459. doi: 10.7150/thno.31017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Born LJ, McLoughlin ST, Dutta D, Mahadik B, Jia X, Fisher JP, et al. Sustained released of bioactive mesenchymal stromal cell-derived extracellular vesicles from 3D-printed gelatin methacrylate hydrogels. J Biomed Mater Res A. 2022;110(6):1190–1198. doi: 10.1002/jbm.a.37362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Maiullari F, Chirivi M, Costantini M, Ferretti AM, Recchia S, Maiullari S, et al. In vivoorganized neovascularization induced by 3D bioprinted endothelial-derived extracellular vesicles. Biofabrication. 2021 doi: 10.1088/1758-5090/abdacf. [DOI] [PubMed] [Google Scholar]
- 240.Roefs MT, Sluijter JPG, Vader P. Extracellular vesicle-associated proteins in tissue repair. Trends Cell Biol. 2020;30(12):990–1013. doi: 10.1016/j.tcb.2020.09.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.