Abstract
Background
Group model building is a process of engaging stakeholders in a participatory modeling process to elicit their perceptions of a problem and explore concepts regarding the origin, contributing factors, and potential solutions or interventions to a complex issue. Recently, it has emerged as a novel method for tackling complex, long-standing public health issues that traditional intervention models and frameworks cannot fully address. However, the extent to which group model building has resulted in the adoption of evidence-based practices, interventions, and policies for public health remains largely unstudied. The goal of this systematic review was to examine the public health and healthcare applications of GMB in the literature and outline how it has been used to foster implementation and dissemination of evidence-based interventions.
Methods
We searched PubMed, Web of Science, and other databases through August 2022 for studies related to public health or health care where GMB was cited as a main methodology. We did not eliminate studies based on language, location, or date of publication. Three reviewers independently extracted data on GMB session characteristics, model attributes, and dissemination formats and content.
Results
Seventy-two studies were included in the final review. Majority of GMB activities were in the fields of nutrition (n = 19, 26.4%), health care administration (n = 15, 20.8%), and environmental health (n = 12, 16.7%), and were conducted in the United States (n = 29, 40.3%) and Australia (n = 7, 9.7%). Twenty-three (31.9%) studies reported that GMB influenced implementation through policy change, intervention development, and community action plans; less than a third reported dissemination of the model outside journal publication. GMB was reported to have increased insight, facilitated consensus, and fostered communication among stakeholders.
Conclusions
GMB is associated with tangible benefits to participants, including increased community engagement and development of systems solutions. Transdisciplinary stakeholder involvement and more rigorous evaluation and dissemination of GMB activities are recommended.
Introduction
Group model building (GMB) is a process of engaging stakeholders in a participatory modeling process to elicit their perceptions of a problem and explore concepts regarding the origin, contributing factors, and potential solutions or interventions to a complex issue [1, 2]. For decades, GMB had been widely used in fields such as business, public policy, criminal justice, and environmental resource planning, among others [3]. More recently, however, it has emerged as a novel method for tackling complex, long-standing public health issues that traditional intervention models and frameworks cannot fully address.
In the past, conventional public health approaches have tended to lean towards more downstream, compartmentalized interventions that do not take into account the whole-system perspective. However, these approaches have been insufficient, as many public health issues meet the key criteria defining a dynamic complex system as defined by Sterman [4]: (a) strong interactions between the various actors of the system, (b) constant fluctuations and changes in trends and behaviors over time, (c) an internal complex causal structure subject to feedbacks from the different actors within the system, and (d) long delays between actions and effects. When not considered, these characteristics can lead to counterintuitive, unintended consequences that may be difficult to predict. For example, past attempts to address syndemic issues such as substance abuse through well-intentioned but single-perspective policies (e.g. increased policing or increased dispensing of medications for opioid use disorders) have instead, in the long term, led to a reinforcing cycle of stigma and compassion burnout [5, 6]. Therefore, it is evident that addressing these dynamically complex public health problems more effectively requires a shift from the traditional linear ways of thinking to a more holistic manner of examining the context, relationships, and systems within which they exist. GMB offers an organized, collaborative approach towards achieving that goal.
GMB adopts system dynamics (SD) methodology, which is a set of principles for framing and understanding the nonlinear behavior of complex systems as they change over time using feedback loops and stocks and flows [7]. SD involves a sequence of five stages: articulation of the problem that needs to be solved, formulation of a hypothesis that conceptualizes the dynamics of the system, formulation of a simulation model representing the system, model testing, and policy design and evaluation. In GMB, a purposefully selected, ideally diverse range of stakeholders, such as policy makers, community leaders, and persons with lived experience who can inform the project’s focus are engaged in these stages through a sequence of scripted group exercises carried out under the guidance of a skilled modeling team [8]. Scripts are used to direct facilitated structured small group exercises that ultimately inform the design, development and application of a systems dynamics model. Depending on the purpose of the GMB, facilitators select and carry out two or more scripts typically built around the following order of tasks (a) presentation (i.e. orienting or explaining SD concepts to participants) (b) divergent thinking (i.e. brainstorming), (c) convergent thinking (i.e. building consensus, shared understanding, or shared decision-making), and (d) evaluation (i.e. group assessment/group ranking of ideas). Table 1 presents examples of classic GMB scripts for each task. The end products of these activities are presented as causal loop diagrams (CLD) and/or stock and flow diagrams which can be simulated to explore the problem of interest (Fig 1) [9].
Table 1. Examples of GMB scripts.
| Scripta | Description |
|---|---|
| A Graphs Over Time | Participants are asked to draw multiple graphs of variables over time showing important characteristics of the issue at hand. For example, if the issue is opioid use disorder, the graph over time could be used to sketch rates of opioid use, overdose deaths, access to preventive or treatment services in the community, over time. |
| B Variable Elicitation | The facilitators ask participants, “what are the key variables affecting the process and outcomes of the problem at hand?” Participants write down as many problem-related variables as they can on sheets of paper and then share their list with the rest of the group. The facilitators tape the variables to a wall and cluster them according to common themes. The facilitators then prompt discussion by asking participants questions such as, “Does this resonate with you? Are there other themes you notice, or any variables you think should be moved?” |
| C Creating a Causal Loop Diagram | The facilitators present the variables elicited from the group in the previous activity and ask the participants how the variables from the list interact and cause changes to the problem at hand. The group indicates the relationship between the variables by linking them and labeling the link with a positive (i.e. an increase in one variable will cause an increase in the other variable) or negative (i.e. an increase in one variable will cause a decrease in the other variable) polarity. |
| D Dots | This exercise is used when there is a need to select variables, graphs, or ideas that are most important to the participant group. For example, after the variable elicitation script, participants vote on what they perceive to be the most significant variables affecting the problem at hand by placing voting dots beside the elicited variables. The facilitators then tally the dots beside each item to create a ranked list of importance. |
a A full list of scripts may be accessed on Scriptapedia, a publicly available online repository of GMB scripts [10].
Fig 1. Images of GMB activities.
(A) Graphs over time: graphs drawn by participants depicting the behavior of variables over time. (B) Variable elicitation: variables affecting opioid use elicited from participants. (C) Creating a CLD: a CLD indicating connections and feedback behaviors between variables developed by participants (D) Dots exercise to address priorities: Output of a dots exercise demonstrating priority actions ranked by participants.
As the GMB process builds on an iterative cycle of collective deliberation, stakeholder consultation and verification, and collaborative modeling, the resultant models integrate scientific knowledge and practical experience [11], leading to the identification of systems strategies for intervention that addresses the target problem [12, 13]. Moreover, the added value of stakeholder engagement fosters group ownership of the model and engenders a shared insight of the system behavior surrounding the problem. Overall, the success of GMB lies not just in the construction of the model itself but in the process it takes to get there [14].
Applying GMB as a method to optimize processes for implementing interventions is fairly recent in public health and healthcare. Nonetheless, studies that document its application in these fields have begun to emerge in the past decade, providing insight into the extent to which it may be applicable across health issues. What remains largely unstudied is the extent to which GMB has resulted in the adoption and integration of evidence-based practices, interventions, and policies for public health. Further, despite the increase of GMB in social and behavioral research, no systematic review of its application and effectiveness in public health and healthcare has yet been conducted.
This paper is designed to examine the literature on GMB and how it has been used and disseminated to foster implementation of evidence-based interventions (EBIs) in public health and healthcare. The following research questions frame our systematic review: (a) where is the application of GMB most prevalent in public health and healthcare; (b) how have GMB activities and strategies been disseminated and applied to improve EBI implementation and systems thinking capacities; and (c) what individual, group/organizational, or community level outcomes have resulted from GMB activities.
Methods
Search strategy
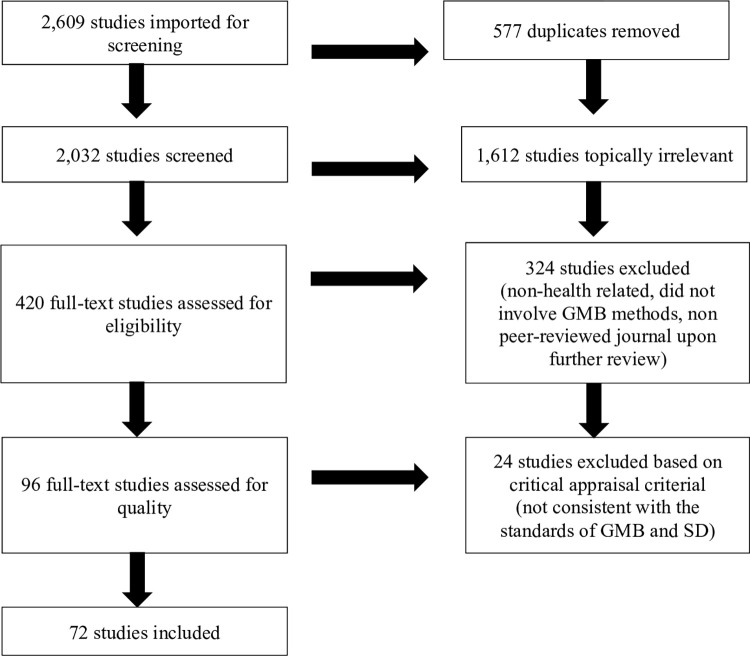
This is a systematic review of GMB applications in public health and implementation science. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Guidelines were used to delineate each step of the review process (Fig 2).
Fig 2. PRISMA diagram.
We consulted seven electronic databases (CINAHL, Embase, Web of Science, PubMed, ProQuest, Scopus and EBSCO) to ensure an exhaustive coverage of the literature from any year up to August 2022 using the following keywords: ("system dynamics modeling" OR "group model building" OR "participatory system dynamics" OR "participatory model building" OR "community based system dynamics" OR "mediated modeling" OR "collaborative modeling" OR "heterogenous problem solving" OR "participatory stakeholder engagement" OR "collaborative model building”) AND (“implementation” OR “dissemination”). After studies were selected through our inclusion criteria for the final review, the reference list of selected studies and systematic reviews were also checked as a secondary method of identifying relevant publications.
Inclusion and exclusion criteria
We included studies where research questions were related to public health or health care and GMB was cited as one of the main methodologies. We did not eliminate studies from our search based on language, geographic location, or date of publication. Systematic reviews, theoretical papers, and articles missing explicit mentions of GMB or its related terms were excluded from this study.
We used Covidence, an online systematic review software, to conduct study screening. Three authors (WE, PZ, and PI) independently screened all titles, abstracts, and full-text articles and noted reasons for excluding studies during full-text review. Differences in screening decisions were resolved by the corresponding author (NS) who served as a third independent reviewer. The decisions were also supported by a group discussion on the article’s eligibility until consensus was reached.
After screening, three authors (WE, NS, DL) conducted a critical appraisal on the final articles to ensure the quality of studies included in this systematic review. Studies were considered good quality if they met a minimum set of criteria defined by the study authors as consistent with the standards of GMB and SD, namely, (a) the study explicitly carried out activities or scripts that support collaborative model building, and (b) the study correctly described SD concepts (e.g. polarity of the causal links are indicated, the type of feedback loops are discussed, stocks and flows are well specified, and/or resulting simulation results are presented) in the results or discussion sections.
Data extraction
Three authors (WE, PZ, and PI) independently piloted a structured abstraction form on ten studies; the final abstraction form was approved by three co-authors (TH, DL, and NS). One of two authors (PZ and PI) independently extracted data such as participant type, GMB team composition, GMB session characteristics, model attributes, model dissemination, implementation effects, and outcomes from the included studies onto a shared spreadsheet. A third author (WE) reviewed each of the abstractions against the original articles to ensure accuracy and consistency.
The models resulting from the GMB sessions were coded by the reviewers into three developmental phases or stages of validation. Studies were considered to be in the demonstration phase, the first phase, if they involved developing a high-generality, low-resolution scoping and consensus-building model generated by the stakeholder groups involved in GMB. They were considered to be in the research modeling phase if they were characterized by the use of historical data to calibrate and test the model developed during the demonstration phase. Finally, they were in the management phase if they involved running different scenarios across the model to identify the most effective intervention and policy options [15].
Each of the GMB activities mentioned in the studies were coded as a GMB script based on the definitions provided on the free Scriptapedia website [10]. For example, GMB activities mentioned in the studies that asked participants to write down a list of key variables affecting a phenomenon or public health issue were coded as “Variable Elicitation,” as they corresponded with the definition for that script on Scriptapedia.
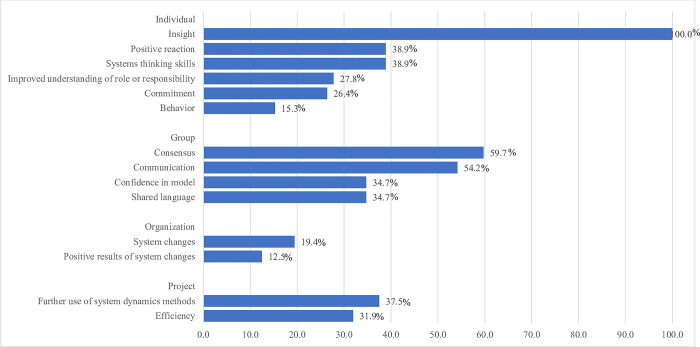
The studies were also reviewed to identify whether or not the outcomes proposed by Rouwette et al. [16] occurred as a result of the GMB sessions. These outcomes include reaction, insight, commitment, behavior, communication, consensus, shared language, system changes, results, further use method, and efficiency and are classified under four levels (individual, group, organization, and project). Three new variables, namely systems thinking skills, confidence in the model, and improved understanding of role and responsibility were also added as outcomes to reflect common GMB goals and findings reported in the literature [17–19]. These variables were coded positively if a study reported outcomes that were consistent with the definitions provided in Table 2. Outcomes that were not found or reported in the articles were coded as “not mentioned”.
Table 2. GMB outcomes adapted from Rouwette et al. [16].
| Level | Outcome | Definition |
|---|---|---|
| Individual | New insights | Gaining new perspectives or a deeper understanding about systems problems |
| Positive reaction | Positive personal evaluation of GMB or the resultant model | |
| Systems thinking skillsa | Development or improvement in ability to think about time-dependent patterns of change and causality | |
| Commitment | Decisive commitment to results attributable to GMB experience | |
| Improved understanding of role or responsibilitya | Improved understanding of individual role or responsibility within the system | |
| Behavior | Changes in personal strategies or approaches attributed to GMB experience | |
| Group | Consensus | Building a shared understanding of the problem and possible solutions |
| Communication | Change in the quality of communication among participants | |
| Confidence in modela | Trust in the model and its performance (i.e., structural and behavioral validity) | |
| Shared language | Understanding of other participants | |
| Organization | System changes | Organizational or physical changes (e.g., production lines, personnel policies) |
| Positive results of system changes | Desirable outcomes associated with model-informed policies and actions (e.g., increased profits or improved morale) | |
| Project | Further use of SD methods | Intention to use SD methods for future projects |
| Efficiency | Efficiency of GMB compared to traditional methods (e.g., a meeting) |
aAdditional codes identified by study authors
We calculated percentages for categorical variables and means and medians for continuous variables. We did not conduct a meta-analysis of the study findings due to the heterogeneity in how the outcomes were reported and presented across all the articles.
Results
The search yielded 2,032 unique articles for title and abstract screening, of which 420 articles were deemed potentially relevant and selected for full text review. A total of 324 studies was then excluded as further in-depth review revealed that they were not related to public health or health care, did not involve GMB methods, or were not published in a peer-reviewed journal. The critical appraisal of the remaining studies led to the additional exclusion of 24 studies as they did not meet the minimum criteria for quality. In these studies, modeling activities were not explicitly described or conducted, or the feedback loops, polarities, or stock and flow diagrams developed were not consistent with the standards of SD. In the end, 72 studies published from 2002 to 2022 were included in the final review. Fig 2 shows the selection of studies for review based on PRISMA while Table 3 outlines the list of all included studies and their outcomes.
Table 3. List of studies in the systematic review.
| Study | Project Purpose | Public Health Domain | Model Level of Analysis | Developmental Stage/Stage of Validation | Mode of Dissemination | Did GMB inform intervention design? | Outcomes |
|---|---|---|---|---|---|---|---|
| Calancie et al., 2022 (United States) [20] | Build a valid model Build rapport across and among stakeholders Design/improve implementation |
Nutrition | Community/ population | Demonstration | Open source White paper |
Yes | Positive reaction Insight Communication System change Improved understanding of role or responsibility Positive results of system changes |
| Gullett et al., 2022 (United States) [21] | Build a valid model Design/improve implementation |
Social work and development | Community/ population | Management | Open source Software interface |
Not mentioned | Insight Behavior change Communication Consensus Shared language Systems thinking skills Further use of SD methods |
| Hendricks et al., 2022 (South Africa) [22] | Build a valid model | Nutrition | Individual | Demonstration | Open source | Not mentioned | Insight |
| Broekhuizen et al., 2021 (Zambia) [23] | Design/improve implementation | Health care/Hospital administration and management | Group/ organization | Demonstration | Open source Online file sharing |
Not mentioned | Insight Communication Consensus |
| Broekhuizen et al., 2021 (Malawi) [24] | Build a valid model Foster decision making Design/improve implementation |
Health care/Hospital administration and management | Group/ organization | Management | Open source | Not mentioned | Insight |
| Susnik et al., 2021 (Latvia) [25] | Build a valid model Design/improve implementation |
Environmental health | Community/ population | Management | Non-open source | Not mentioned | Insight |
| Shire et al., 2020 (United Kingdom) [26] | Build a valid model Foster decision mking Design/improve implementation |
Health care/Hospital administration and management Pharmaceuticals |
Group/ organization | Management | Non-open source Software interface |
Not mentioned | Positive reaction Insight Confidence in model Communication Consensus Shared language Improved understanding of role or responsibility Systems thinking skills Further use of SD methods Efficiency |
| Guarigata et al., 2020 (Jamaica, St. Kitts and Nevis, St. Vincent, the Grenadines) [27] | Build a valid model Design/improve implementation |
Nutrition | Community/ population | Demonstration | Open source | Not mentioned | Positive reaction Insight Commitment Confidence in model Communication Consensus Systems thinking skills |
| Sarmiento et al., 2020 (Colombia) [28] | Build a valid model Build rapport across and among stakeholders Foster decision making |
Infrastructure | Community/ population | Demonstration | Open source | Yes | Insight |
| Weeks et al., 2020; Weeks et al., 2017 (United States) [29, 30] |
Build a valid model Foster decision-making Design/improve implementation |
Infectious diseases | Community/ population | Research | Open source Software interface Planning meeting |
Not mentioned | Positive reaction Insight Commitment Confidence in model Communication Consensus Shared language Systems thinking skills |
| Hennessy et al., 2020; Appel et al., 2019 (United States) [31, 32] | Build a valid model Design/improve implementation |
Non-communicable diseases Nutrition |
Community/ population | Demonstration | Non-open source | Yes | Insight Confidence in model Communication Shared language Further use of SD methods |
| Naumann et al., 2020 (United States) [33] | Build a valid model | Infrastructure | Community/ population | Demonstration | Non-open source | Not mentioned | Insight Communication Systems thinking skills |
| McGlashan et al., 2018 Allender et al., 2015; (Australia) [34, 35] | Build a valid model |
Nutrition | Community/ population | Demonstration | Open source Community meeting |
Yes | Positive reaction Insight Commitment Behavior Communication Consensus Shared language System changes Systems thinking skills Improved understanding of role or responsibility Positive results of system changes Further use of SD methods Efficiency |
| Langellier et al., 2019 (Peru, Brazil, Guatemala) [36] |
Build a valid model Build rapport across and among stakeholders |
Nutrition Infrastructure |
Community/ population | Demonstration | Open source Written report |
Yes | Positive reaction Insight Communication Consensus Shared language Systems thinking skills Further use of SD methods |
| Escobedo et al., 2019 (United States) [37] | Build a valid model Design/improve implementation |
Mental health/addiction and substance abuse | Community/ population | Demonstration | Non-open source | Not mentioned | Insight Consensus System changes Improved understanding of role or responsibility |
| Fowler et al., 2019 (United States) [38] | Build a valid model Build rapport across and among stakeholders |
Social work and development | Group/ organization | Demonstration | Non-open source Written report Organizational presentations |
Not mentioned | Insight Confidence in model Communication Consensus Improved understanding of role or responsibility |
| Dianati et al., 2019 (Kenya) [39] | Build a valid model Foster decision making |
Environmental health | Community/ population | Management | Open source | Not mentioned | Positive reaction Insight Confidence in model Consensus Systems thinking skills |
| Ansah et al., 2019 (Cambodia) [40] | Build a valid model Build rapport across and among stakeholders |
Non-communicable diseases | Community/ population | Demonstration | Open source | Not mentioned | Positive reaction Insight Communication Consensus Further use of SD methods |
| Gamble et al., 2019 (United States) [41] | Build a valid model Build rapport across and among stakeholders Design/improve implementation |
Health care/Hospital administration and management | Group/ organization | Demonstration | Non-open source | Yes | Positive reaction Insight Commitment Behavior Communication Shared language Systems change Systems thinking skills Positive results of system changes Further use of SD methods |
| Qayoom et al., 2019 (Pakistan) [42] | Build a valid model | Occupational health | Group/ organization | Management | Non-open source | Not mentioned | Insight Confidence in model |
| Hosseinichimeh et al., 2019 (United States) [43] | Build a valid model | Maternal and child health | Community/ population Group/ organization Individual |
Management | Non-open source Website Organizational presentation |
Not mentioned | Insight Communication Shared language Improved understanding of role or responsibility Further use of SD methods Efficiency |
| Baker et al., 2019 (Switzerland) [44] | Build a valid model Design/improve implementation Foster decision making |
Nutrition, Health care/Hospital administration and management | Group/ organization | Demonstration | Non-open source | Not mentioned | Insight |
| Gerritsen et al., 2019 (New Zealand) [45] | Build a valid model Design/improve implementation |
Nutrition | Community/ population | Demonstration | Open source | Yes | Positive reaction Insight Commitment System changes Further use of SD methods |
| Urwannachotima et al., 2019 (Thailand) [46] | Build a valid model Foster decision-making |
Nutrition | Community/ population | Demonstration | Open source | Not mentioned | Insight Confidence in model Communication Consensus Further use of SD methods |
| Purwanto et al., 2019 (Indonesia) [47] | Build a valid model Build rapport across and among stakeholders Foster decision making |
Environmental health | Community/ population | Demonstration | Non-open source | Not mentioned | Positive reaction Insight Consensus Improved understanding of role or responsibility Systems thinking skills |
| Roberts et al., 2019 (Australia) [48] | Build a valid model Foster decision making |
Nutrition | Community/ population | Management | Open source | Not mentioned | Insight Communication Consensus Further use of SD methods Efficiency |
| Mui et al., 2019 (United States) [49] | Build a valid model Build rapport across and among stakeholders Design/improve implementation |
Nutrition | Community/ population | Demonstration | Open source | Not mentioned | Insight Communication Further use of SD methods Efficiency |
| Pagano et al., 2019 (Slovenia) [50] | Build rapport across and among stakeholders Design/improve implementation |
Environmental health | Community/ population | Management | Open source Stella interface |
Yes | Positive reaction Insight Communication Consensus Shared language Further use of SD methods |
| Malard et al., 2018 (Mexico) [51] | Build a valid model Foster decision-making |
Environmental health | Community/ population | Demonstration | Open source Conference presentation |
Not mentioned | Positive reaction Insight Communication Consensus Improved understanding of role or responsibility Further use of SD methods |
| Koh et al., 2018 (United States) [52] | Build a valid model | Nutrition | Community/ population | Research | Open source Website Online file sharing program |
Not mentioned | Insight Confidence in model Shared language Systems thinking skills Efficiency |
| Ansah et al., 2018 (Singapore) [53] | Build a valid model | Health care/Hospital administration and management | Group/ organization | Demonstration | Non-open source | Not mentioned | Insight Systems thinking skills Further use of SD methods |
| Eker et al., 2018 (United Kingdom) [54] | Build a valid model Foster decision making |
Environmental health Infrastructure |
Community/ population | Research | Open source Stakeholder presentation Written report |
Not mentioned | Positive reaction Insight Confidence in model Communication Consensus Systems thinking skills Further use of SD methods Efficiency |
| Chalise, 2018 (India) [55] | Build a valid model |
Environmental health | Community/ population | Management | Open source | Not mentioned | Insight Confidence in model Communication |
| Lembani et al., 2018 (South Africa) [56] | Build a valid model Build rapport across and among stakeholders |
Maternal and child health | Group/ organization | Demonstration | Open source Written report Stakeholder presentation |
Yes | Insight Commitment Consensus Shared language System changes Improved understanding of role or responsibility Efficiency |
| Reno, 2018 (United States) [57] | Build a valid model |
Maternal and child health | Community/ population | Demonstration | Non-open source | Not mentioned | Insight Communication Consensus |
| Brown et al., 2018 (Australia) [58] | Build a valid model Foster decision making |
Environmental health | Community/ population | Demonstration | Open source | Not mentioned | Insight |
| Atkinson et al., 2017 (Australia) [59] | Build a valid model Build rapport across and among stakeholders Foster decision making Design/improve implementation |
Mental health/addiction and substance abuse | Community/ population | Management | Open source | Not mentioned | Insight Consensus Further use of SD methods |
| Freebairn et al., 2017 (Australia) [60] | Build a valid model Build rapport across and among stakeholders Design/improve implementation |
Mental health/addiction and substance abuse | Community/ population | Management | Open source | Yes | Insight Confidence in model Communication Consensus Shared language Systems thinking skills |
| Kopainsky et al., 2017 (Zambia) [61] | Build a valid model Foster decision-making |
Nutrition | Individual | Demonstration | Non-open source Written report |
Yes | Positive reaction Insight Behavior Communication Consensus Improved understanding of role or responsibility Systems thinking skills |
| Morrow-Howell et al., 2017 (United States) [62] | Design/improve implementation | Social work and development | Community/ population | Demonstration | Open source | Not mentioned | Insight Further use of SD methods Efficiency |
| Macmillan et al., 2017 (United Kingdom, the Netherlands) [63] | Build a valid model Design/improve implementation |
Infrastructure | Community/ population | Demonstration | Open source Written report |
Not mentioned | Insight Communication |
| Mumba et al., 2017 (Zambia) [64] | Design/improve implementation Foster decision making |
Animal health | Community/ population | Demonstration | Open source | Not mentioned | Positive reaction Insight Consensus Systems thinking skills |
| Waqa et al., 2017 (Fiji) [20] | Build a valid model Design/improve implementation |
Nutrition | Community/ population | Demonstration | Open source | Yes | Insight Commitment Consensus System changes Improved understanding of role or responsibility Positive results of system changes |
| Jetha et al., 2017 (United States) [65] | Build a valid model |
Mental health/addiction and substance abuse | Group/ organization | Management | Open source | Not mentioned | Insight Consensus Improved understanding of role or responsibility Efficiency |
| Trani et al., 2016 (Afghanistan) [66] | Foster decision making Design/improve implementation |
Mental health/addiction and substance abuse | Community/ population | Demonstration | Open source | Not mentioned | Positive reaction Insight Commitment Communication Consensus Shared language Improved understanding of role or responsibility Efficiency |
| Jetha et al., 2016 (United States) [67] | Build a valid model | Occupational health | Group/ organization | Management | Open source | Insight | |
| Frerichs et al., 2016 (United States) [68] | Build a valid model |
Crime/violence | Community/ population | Demonstration | Open source Stakeholder presentation |
Not mentioned | Positive reaction Insight Commitment Confidence in model Communication Systems thinking skills Further use of SD methods |
| Zimmerman et al., 2016 (United States) [69] | Build a valid model Design/improve implementation |
Health care/Hospital administration and management | Group/ organization | Management | Non-open source | Yes | Positive reaction Insight Consensus Shared language System change Systems thinking skills Positive results of system changes Further use of SD methods Efficiency |
| Macmillan et al., 2016 (United Kingdom) [70] | Build a valid model Foster decision making Design/improve implementation |
Environmental health | Community/ population | Demonstration | Open source Website File copy |
Not mentioned | Insight Commitment Consensus Systems thinking skills |
| Brownson et al., 2015 (United States) [71] | Build rapport across and among stakeholders | Health care/Hospital administration and management | Group/ organization, Community/ population | Demonstration | Open source | Yes | Positive reaction Insight Commitment Confidence in model Behavior change Communication Shared language System changes Improved understanding of role or responsibility Systems thinking skills Positive results of system changes Efficiency |
| Homa, 2015 (United States) [72] | Build a valid model Foster decision-making |
Health care/Hospital administration and management | Community/ population | Research | Open source Website, blog, or social media post |
Not mentioned | Insight Efficiency |
| Thomas et al., 2015 (United States) [73] | Foster decision-making Design/improve implementation |
Nutrition | Community/ population | Demonstration | Non-open source | Yes | Positive reaction Insight Commitment Confidence in model Communication Consensus Shared language Systems change Efficiency |
| Brennan et al., 2015 (United States) [74] | Foster decision-making Design/improve implementation |
Nutrition | Community/ population | Demonstration | Non-open source | Not mentioned | Insight Commitment Communication Consensus Shared language Improved understanding of role or responsibility Efficiency |
| Munar et al., 2015 (Honduras) [75] | Foster decision-making | Maternal and child health | Community/ population | Research | Non-open source | Yes | Insight Systems thinking skills Further use of SD methods |
| Keane et al., 2015 (United States) [76] | Build a valid model Design/improve implementation |
Nutrition | Community/ population | Demonstration | Non-open source | Yes | Insight Commitment Confidence in model Behavior change Communication Shared language Systems change Positive results of system change Further use of SD methods |
| Moreland, 2015 (United States) [77] | Build a valid model |
Nutrition | Community/ population | Demonstration | Non-open source | Yes | Insight Behavior change Systems thinking skills Efficiency |
| Skouteris et al., 2015 (Australia) [78] | Build a valid model Design/improve implementation |
Nutrition | Community/ population | Demonstration | Non-open source | Yes | Insight Consensus |
| Esensoy et al., 2015 (Canada) [79] | Build a valid model Foster decision making Design/improve implementation |
Health care/Hospital administration and management | Group/ organization Community/ population |
Demonstration | Open source Panel presentations |
Not mentioned | Positive reaction Insight Commitment Confidence in model Communication Consensus Shared language Systems change Improved understanding of role or responsibility Positive results of systems change Efficiency |
| Ager et al., 2015 (Nigeria) [80] | Build a valid model |
Health care/Hospital administration and management | Group/ organization | Demonstration | Open source Stakeholder presentation |
Not mentioned | Insight |
| Van Nistelrooij et al., 2015 (Netherlands) [81] | Build a valid model | Health care/Hospital administration and management | Community/ population | Research | Non-open source | Not mentioned | Insight Confidence in model Consensus Further use of SD methods |
| Macmillan et al., 2014 (New Zealand) [82] | Foster decision making Design/improve implementation |
Infrastructure | Community/ population | Management | Open source | Not mentioned | Insight Communication Consensus |
| Narayana et al., 2014 (India) [83] | Build a valid model |
Pharmaceuticals | Community/ population | Demonstration | Non-open source Written report |
Not mentioned | Insight Consensus Further use of SD methods |
| Biroscak et al., 2014 (United States) [84] | Build a valid model |
Health care/Hospital administration and management | Group/ organization | Demonstration | Non-open source | Not mentioned | Insight |
| Rouwette et al., 2014 (Netherlands) [85] | Build a valid model Build rapport across and among stakeholders |
Crime/violence | Community/ population | Demonstration | Open source Written report |
Yes | Positive reaction Insight Confidence in model Communication Consensus Shared language System change Improved understanding of role or responsibility Positive results of system changes |
| Merrill et al., 2013 (United States) [86] | Build a valid model Foster decision-making Design/improve implementation |
Health care/hospital administration and management | Group/ organization | Demonstration | Open source | Yes | Insight Confidence in model Consensus Efficiency |
| Hernantes et al., 2012 (Spain) [87] | Build a valid model Foster decision making |
Crisis and emergencies Infrastructure |
Community/ population | Management | Open source Website |
Not mentioned | Positive reaction Insight Confidence in model Communication Consensus Systems thinking skills |
| Goh et al., 2012 (Australia) [88] | Build a valid model |
Occupational health | Group/ organization | Demonstration | Non-open source | Yes | Insight Commitment Confidence in model Systems thinking skills Further use of SD methods Efficiency |
| Bridgewater et al., 2010 (United States) [89] | Build rapport across and among stakeholders Foster decision-making Design/improve implementation |
Crime/violence | Community/ population | Research | Open source | Not mentioned | Positive reaction Insight Communication Consensus Shared language Systems thinking skills Efficiency |
| Thompson et al., 2010 (United States) [90] | Build a valid model Foster decision making |
Environmental health | Community/ population | Research | Non-open source File copy |
Not mentioned | Positive reaction Insight Commitmet Confidence in model Behavior change Communication Improved understanding of role or responsibility Systems thinking skills |
| Stave, 2010 (United States) [91] | Build a valid model Design/improve implementation |
Environmental health | Community/ population | Management | Open source Written report Conference presentation Oral presentation File copy |
Not mentioned | Positive reaction Insight Commitment Confidence in model Behavior change Communication Consensus Shared language Systems thinking skills Further use of SD methods |
| Cavana et al., 2006 (New Zealand) [92] | Build a valid model |
Health care/Hospital administration and management | Community/ population | Management modeling | Non-open source Conference presentation |
Not mentioned | Positive reaction Insight Confidence in model Behavior change Consensus Shared language System change Improved understanding of role or responsibility Further use of SD methods Efficiency |
| Stave, 2002 (United States) [93] | Build a valid model Build rapport across and among stakeholders Foster decision-making Design/improve implementation |
Environmental health | Community/ population | Management | Non-open source Stakeholder presentation |
Yes | Positive reaction Insight Behavior change Communication Consensus Shared language Systems thinking skills Efficiency |
Study information
More than half of the documented studies on public health applications of GMB were published in the last five years from 2017–2022 (n = 42, 58.3%). Most of the studies were conducted in high-income countries, particularly the United States (n = 29, 40.3%) and Australia (n = 7, 9.7%), although studies were found across six continents and across the different country-level income classifications as defined by the World Bank [94]. GMB methods were most heavily utilized in the domains of nutrition (n = 19, 26.4%), health care/hospital administration (n = 15, 20.8%), and environmental health (n = 12, 16.7%). GMB was conducted for the following purposes: to build a valid model (n = 59, 81.9%), to design/improve implementation (n = 34, 47.2%), to foster decision-making (n = 29, 40.3%), and to build rapport among stakeholders (n = 16, 22.2%).
Session characteristics
The characteristics of the GMB sessions varied widely across studies. The number of participants in the sessions ranged from as few as five people to as many as 50 people in one session, with 15 as the median number of participants. Most of the studies required two to three sessions; however, some only had one session while one study required 22. Each session lasted about 1.5 hours to a full day, with a mean duration of four hours.
GMB relies on participants who represent relevant, diverse stakeholder groups and experts [9]. Among all the participant types in this review, community coalition members/advocacy groups (n = 39, 54.2%) were the most often engaged in GMB projects, followed by government officials (n = 38, 52.8%) and domain experts (n = 34, 47.2%). The correctional or justice system (n = 4, 5.6%) and funding agencies (n = 2, 2.8%) were the least commonly represented.
GMB sessions were typically directed by a school- or university-based team with training in SD modeling. Actual facilitation of the sessions was conducted by a GMB team of, on average, seven persons who took on roles such as conveners, community facilitators, modelers, recorders, note-takers, and observers [8]. The most common GMB scripts mentioned in the literature were causal loop diagramming (n = 46, 63.9%; convergent thinking), variable elicitation (n = 39, 54.2%; divergent thinking), concept models (n = 29, 40.3%; presentation), graphs over time (n = 21, 29.2%; divergent thinking), and action ideas (n = 21, 29.2%; divergent thinking, evaluation).
Process evaluations determine whether workshops are implemented as intended and resulted in meaningful outputs. Only 11 of the 72 studies (15.3%) reported conducting a process evaluation to assess the implementation of the workshops and their fidelity to stated objectives of the GMB sessions.
Model attributes
The majority of the modelers and system dynamicists reported utilizing Vensim (Ventana Systems, Harvard, MA) (n = 36, 50.0%) and Stella Architect (ISEE Systems) (n = 7, 9.7%) to create and refine the models that emerged from the GMB workshops. The models mostly included qualitative (CLDs and stock-and-flow figures) in nature (n = 45, 62.5%), but 26 studies (36.1%) involved quantitative or simulation modeling. Most of the models and simulations modeled the overall dynamics of a community (n = 54, 75.0%), 19 (26.4%) modeled the dynamics of a group or organization, while three (4.2%) centered only on individual factors and behaviors. Majority of the models created by stakeholder groups reached only the demonstration phase of modeling (n = 44, 61.1%), while 18 (25.0%) studies reached the management modeling phase.
GMB outcomes
Twenty-three (31.9%) studies reported that the findings and models from the GMB workshops influenced implementation through policy change, intervention development, and/or community action plans. These models were used to develop local action plans, revise intervention approaches in grant applications, guide strategic planning and agendas, publish guidelines and communication messages, develop new partnerships, and activate policy leverage points. The remaining studies (n = 49, 68.1%) did not report whether GMB influenced or contributed to implementation.
Insight, consensus, and communication were the most commonly reported outcomes of the papers reviewed (Fig 3). Insight is defined by Rouwette et al. as individual-level learning [16]. We documented that all studies (n = 72, 100%) in our review generated useful insights among participants. In studies that apply GMB, greater insights among participants are produced if the problem to be modeled aligns with their interests and priorities, and if modeling efforts are sufficient to support the aims of the study [16].
Fig 3. Outcomes identified in the GMB studies.
Consensus or mental model alignment is a group-level outcome defined as a shared view of the problem or actions among GMB participants. It is considered a prerequisite for shared action [16]. Forty-three (59.7%) of the articles in this review indicated that consensus was achieved after the workshops. A common strategy mentioned in the literature to achieve consensus was the use of CLDs as boundary objects [36]. Boundary objects are representations, such as a diagram, sketch, or prototype, that help individuals collaborate effectively across a boundary such as a difference in knowledge, training, or objective [95]. Other strategies to build consensus that were mentioned in the literature were voting [60, 64] and continued discussion until all concerns were addressed [86].
A change in the quality of communication among GMB participants is necessary for consensus to emerge [16]. Thirty-nine (54.2%) of the articles in this review explicitly mentioned that an improvement in communication among stakeholders occurred during the GMB workshops. Participatory methods such as GMB generally imply the presence of communication; it is possible that this outcome actually occurred more than was reported and was just not explicitly documented as it was thought to be obvious.
Model dissemination
Model dissemination was high, with 70 (97.2%) of the studies publishing the CLDs or the full models developed through GMB. However, while the workshop activities and resultant were disseminated actively to the academic community through peer-reviewed publications in open-source journals (n = 43, 59.7%), information on whether the models were shared back to stakeholders or the non-academic community was limited. Studies that reported doing so (n = 20, 27.8%) utilized formats such as oral presentations to stakeholders and planning committees or written reports. Four recent studies published from 2016–2022 also reported utilizing cloud-based interfaces such as Forio, Dropbox or Runthemodel.com to disseminate the model, with one study uploading the model onto a web-based, user-friendly interface that allowed stakeholders to easily experiment with the model parameters online and generate corresponding charts and graphs.
Discussion
To our knowledge, this is the first comprehensive review of public health or health care applications of GMB using well established systems science frameworks to assess the studies. Our review found that the application of GMB in public health and health care settings has increased steadily in recent years, with more than half of the papers published from 2017 to 2022. The application of GMB was most prevalent in the domains of nutrition, health care and hospital administration, and environmental health. In particular, our findings showed relatively robust work in obesity research, health care service planning, and air and water quality research. Vensim® was most commonly referenced as the software of choice, which may be attributed to its policy of making available a free version to the public and its inclusion of a feature that facilitates quick and easy causal loop diagramming, which is a core activity in most GMB projects.
Of the 72 papers in this review, 23 (31.9%) reported that the resultant models created via GMB had an eventual influence on the design and implementation of policies and programs, resulting in revisions of local action plans and strategic planning, development of new partnerships, and activation of policy leverage points [75]. The studies we reviewed revealed how SD models developed through GMB asserted their impact on policy through various mechanisms, such as by challenging pre-conceived notions of policy-makers and protecting against overconfidence by exposing potential weaknesses and unintended consequences in the system [96]. For example, a GMB session in Fiji involving officials from two government ministries led to a shared endorsement of a data sharing policy when the discussion uncovered that lack of access to evidence was a cause of poor food-related policymaking (Table 4). Another study reported how the identification of clear causal relationships between their non-profit organization’s performance indicators led to a direct revision of their budget [41]. As GMB offers a process for making these causal influences explicit while allowing for a nuanced discussion of their impacts, useful insights and opportunities for organizational or community action are able to emerge.
Table 4. GMB case highlights.
| Exploring the dynamics of food-related policymaking processes and evidence use in Fiji using systems thinking (Waqa et al., 2017) |
| This study used GMB to gain insights on the factors influencing the use of evidence in food-related policy-making in Fiji, where food items associated with non-communicable diseases are produced in cheap and abundant amounts. Eighteen middle and senior managers from the country’s Ministry of Health and Medical Services (MoHMS) and Ministry of Agriculture (MOA) participated in three GMB sessions where they engaged in activities such as variable elicitation, graphs over time, connection circles, CLDs, and action ideas. |
| The CLD generated through the sessions revealed the following barriers to the use of evidence in food-related policy making: consultation issues, lack of engagement with stakeholders, and delays due to politics vested interests. Recognizing their unique access to the food sector, the MOA resolved to influence the consultation loop by publishing guidelines on consultation with partners. The MoHMS sought to address the issues surrounding delays by publishing strategic health communication messages to counteract the food industry’s influence on consumers choices. Both ministries agreed to endorse a government policy for data sharing to improve access to evidence and strengthen engagement among stakeholders. A guide to integrate multi-sectoral consultation and stakeholder engagement in developing policies is also currently being developed by the organizations. |
| Because the participants were senior staff who had organizational expertise in the policymaking process, they were able to successfully influence change within the government system. More importantly, their participation in GMB facilitated a sense of ownership over the action plans and increased coordination between the two separate ministries. |
| Community needs assessment among Latino families in an urban public housing development (Escobedo et al., 2019) |
| The Partners for Strong Healthy Families (PSHF) is a community-campus partnership that aims to improve the health and well-being of Latino families living within and around a public housing community in Los Angeles. In 2018, the organization initiated a three-hour GMB workshop with resident parents and youth to gain insight on issues surrounding parent-youth relationships and design more effective interventions to improve family wellbeing. |
| The graphs over time created through the GMB session highlighted differences in perspectives. The youth identified increasing household responsibilities and police presence as priority issues while the parents focused on declining respect and differences in spoken languages. Creating the CLDs allowed both perspectives to be reconciled as the participants worked together to identify the interrelationships between the different variables. |
| The insights gained from the GMB session had a direct impact on intervention development. The funded grant had originally planned to focus on substance use and sexual risk behaviors; however, as those weren’t identified as concerns by both parents or youth during the GMB, the intervention shifted to a bilingual, family-based meditation intervention that would improve trust, respect, and communication between families. As negative police interaction with men in the community was also characterized during the GMB, a separate intervention program to address the impact of policing tactics on the health and wellbeing of male community members was also designed. Evaluation of these programs are planned in the future to determine their effectiveness in building family and community strengths. |
In addition to insight which was identified as an outcome in all the studies, consensus and communication were the most reported outcomes of GMB. A unique aspect of GMB is its flexibility in accommodating multiple worldviews and experiences from a wide range of stakeholders. The studies in this review described how GMB created an environment for diverse participants to express individual experiences and then build a collective model and action plan to address the shared problem. While disagreements regarding the relationships between variables were common in the initial phases of the process as participants made their mental models explicit, the participatory nature of the method allowed for productive conversations that eventually negotiated and reconciled viewpoints [36, 48, 60]. For example, a graphs-over-time exercise in one GMB session revealed differing answers among parents and youth regarding factors that affect familial relationships [37]. However, the subsequent CLD exercise allowed the two groups to bring those different variables together and explore how they interact in the system, resulting in the development of an intervention that addressed both groups’ concerns (Table 4).
Our study also underlines how GMB can be applied as a strategy for community participation and engagement [97]. Not only does the collaborative process foster a greater sense of ownership over the findings, GMB scripts such as Dots and Graphs Over Time [45, 49] also offer a unique method of eliciting information from stakeholders that traditional approaches such as interviews or surveys may not be able to draw out. Further, the outputs created such as graphs, CLDs, and simulation models can be used as springboards for future engagement with the community, with one study mentioning a plan to follow-up their GMB sessions with a community co-design workshop to develop an intervention for the identified issues [98].
Our review also showed that systems change (n = 14, 19.4%), behavior change (n = 11, 15.3%), and positive results of system change (n = 9, 12.5%), were the least observed outcomes of GMB. As these three outcomes usually take time and may require considerable resources to realize, they may have just not yet been evident in the rest of the studies at the time of publication. This has been documented as a continuing challenge in the community-based SD field, as the delay between participation in GMB and the development of institutional initiatives has been found to reach up to several years or more [3]. Indeed, the papers in this review that reported the positive occurrence of these outcomes were those that had considerable project duration and follow-up periods of up to five years, supporting suggestions in the field to consider the use of longitudinal designs when evaluating participatory modeling activities.
Given our findings, our review has identified several recommendations for future applications of GMB in public health and health care settings. First, transdisciplinary stakeholder involvement is a key contributor to success [36, 56, 76, 99]. A closer evaluation of the 23 papers that reported an influence on implementation revealed that bringing in multiple perspectives was crucial to creating rich discussions and achieving acceptance of the model, with one study noting that diverse stakeholder participation led to lower rates of model rejection [99]. Studies that were unable to schedule single sessions with their desired stakeholders maximized participation by implementing strategies such as creating multiple expert panel sessions or conducting lunch-and-learn sessions during convenient times [79, 100]. It should be noted that in these papers, program implementers (n = 14, 60.9%), coalition members and advocacy groups (n = 11, 47.8%), and government officials (n = 10, 43.5%) were the most widely represented stakeholder groups in the sessions.
Second, while 43 of the 72 papers (59.7%) were published in open-source journals, only a third reported dissemination of the findings back to the stakeholders and the community through other means. As with any method involving the community and the practice of translational, participatory research, the dissemination of findings beyond scientific publication should be a fundamental activity, as journal audiences do not usually include non-academic stakeholders and the general public [101]. Dissemination of GMB findings to participants will provide a tangible deliverable, facilitate decision-making, and sustain implementation impact [36]. In addition to more traditional means of dissemination such as presentations to stakeholders and distribution of reports [36, 56, 85], the more recent published literature showed an increasing trend towards cloud-based model publication [52, 102]. Using cloud-based software expands a model’s reach, as it will allow the public, not just the modeling team, to interact with the product and run simulations from anywhere. Other software such as Stella Architect’s ISEE Exchange also allows modelers to present the structure and behavior of their models in a piece-by-piece, sequential manner, making the narrative more understandable and interesting even to those with limited modeling background.
Third, there is both a gap and inconsistency in how outcomes of GMB are reported in the public health literature. Reporting is focused on the developed CLDs, models, and simulations, but other effectiveness outcomes such as those proposed by Rouwette et al. [16] are not explicitly or consistently documented. Furthermore, only 11 (15.3%) papers indicated that they had conducted process evaluations of the sessions. More rigorous and standardized reporting on the characteristics and effectiveness of GMB are needed to advance the field scientifically and refine its application in public health and health care. For this, we propose using the guidelines and scoresheet created by Rouwette et al., which outlines the recommended context, mechanism, and outcome variables that can be used as standard measurements for assessing GMB activities [16].
Fourth, previous studies have pointed out GMB as a resource-intensive approach that requires extensive technical knowledge, suggesting that its application in public health might be restricted in settings with limited access to modeling tools or training [14, 103]. However, our review of GMB applications across multiple contexts illustrates how the methodology can be tailored to varying resource constraints and participant educational levels. For instance, a participatory modeling exercise in Zambia with small-scale farmers demonstrated how GMB could be adapted to participants with low or no formal educational background and in settings without computers or electricity. The workshop used white boards and images of harvested maize and coins to illustrate variables in the model. Regular drinking glasses filled with water were used to illustrate stock and flow and feedback loops. Evaluations of these sessions a year later showed that participants found these tools to be salient in allowing them to see the interconnected nature of the system and its behavior [61]. Given the growing expansion of GMB across various settings, more research is needed on how the methodology can further be adapted for different population groups and for low resource environments. We recommend that modelers and facilitators in these settings take on an implementation science lens and formally document and evaluate any adaptations in their approach.
Finally, system dynamics practitioners have documented that the reliability, validity and the utility of system dynamics models are associated with the quality of stakeholder engagement, which is, in turn, related to the quality of GMB session facilitation [9, 104]. Although our review describes outcomes of GMB, further evaluation on fostering and sustaining high quality participation among an appropriate mix of stakeholders is warranted. Additionally, evaluation that examines how GMB can establish and strengthen multi-stakeholder research teams, working groups, and/or coalitions should be conducted.
Our study has several limitations. First, our search may not have captured the whole breadth of the public health literature on GMB as GMB may not be properly coded as a keyword in all publications. We mitigated this by consulting seven databases and checking the reference lists of eligible articles to identify any missing studies. We also utilized different variations of GMB terminology in our keywords and tested them across the different databases to ensure that we were capturing core articles in our search. Second, our findings were dependent on the availability of the data reported in the papers. As our selected outcomes were not consistently reported across all papers, it is possible that some outcome characteristics had occurred in real life but were not documented in these publications. Finally, the application of GMB in public health may be underreported in the literature, as some GMB activities may not have been documented, especially those that were conducted by public health practitioners rather than researchers.
Conclusion
GMB is used in system dynamics projects to convene diverse stakeholders in a facilitated, deliberative scientific process that aims to specify, test and validate models that aim to further understanding of, and action to address, complex systems problems [1, 2, 11–13]. This paper demonstrates the growing breadth of GMB activities in public health and health care, with an emphasis on informing interventions for complex health challenges and enhancing the implementation of such interventions. Our findings suggest that effective GMB is associated with higher impact models as well as tangible benefits to participants, including opportunities to learn and apply new systems thinking. While the quality of the studies varies, reflecting a longstanding need to provide more training and capacity building in this method, it is evident that GMB will become increasingly more prevalent and potent as a tool for facilitating stakeholder involvement, advancing implementation science, and ultimately, developing systems solutions in the future.
Supporting information
(DOCX)
(XLSX)
Data Availability
All data files are available from the Github repository (https://github.com/weannemyrrh/Group-Model-Building-Data).
Funding Statement
This study was funded through a grant awarded to NE by the NIH National Institute on Drug Abuse, Grant Number 450 UM1DA049415 (https://www.drugabuse.gov/funding/nida-funding-opportunities) and a grant awarded to TH by the Centers for Disease Control and Prevention through the NYU-CUNY Prevention Research Center, Grant Number 451 U48DP00639 (https://www.cdc.gov/grants/index.html). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Andersen D, Vennix J, Richardson G, Rouwette E. Group model building: problem structing, policy simulation and decision support. The Journals of the Operational Research Society. 2007;58(5):691–4. [Google Scholar]
- 2.Andersen DF, Richardson GP, Vennix JAM. Group model building: Adding more science to the craft. System Dynamics Review. 1997;13(2):187–201. [Google Scholar]
- 3.Hovmand PS. Community based system dynamics [Internet]. Vol. 9781461487630. 2014. 1 p. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84929907458&doi=10.1007%2f978-1-4614-8763-0&partnerID=40&md5=3ed840c2546d53297dd69b9fc46f1c43 [Google Scholar]
- 4.Sterman J. System dynamics: systems thinking and modeling for a complex world. In: ESD Working Papers. Cambridge, Massachusetts: Masachusetts Institute of Technology; 2002. [Google Scholar]
- 5.Kalk NJ, Robertson JR, Kidd B, Day E, Kelleher MJ, Gilvarry E, et al. Treatment and Intervention for Opiate Dependence in the United Kingdom: Lessons from Triumph and Failure. European Journal on Criminal Policy and Research. 2018. Jun 1;24(2):183–200. [Google Scholar]
- 6.Fischer B, Rehm J, Tyndall M. Effective Canadian policy to reduce harms from prescription opioids: learning from past failures. CMAJ. 2016. Dec 6;188(17–18):1240. doi: 10.1503/cmaj.160356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Forrester JW. System dynamics—the next fifty years. System Dynamics Review. 2007. Jun 1;23(2‐3):359–70. [Google Scholar]
- 8.Andersen D, Calhoun A, Hovmand P, Hower T, Rouwette E, Steins E, et al. Scriptapedia. 2016. Roles in Group Model Building. Available from: https://en.wikibooks.org/wiki/Scriptapedia/Roles_in_Group_Model_Building [Google Scholar]
- 9.Hovmand PS, Andersen DF, Rouwette E, Richardson GP, Rux K, Calhoun A. Group Model-Building Scripts’ as a Collaborative Planning Tool. Systems Research and Behavioral Science. 2012;29(2):179–93. [Google Scholar]
- 10.Andersen D, Calhoun A, Hovmand P, Hower T, Rouwette E, Steins E, et al. Scriptapedia. 2020. Scriptapedia. Available from: https://en.wikibooks.org/wiki/Scriptapedia [Google Scholar]
- 11.Klaus H, Ravera F, Tarrason D, Prell C. Participatory Modeling. In: International Encyclopedia fo Geography: People, the Earth, Environment, and Technology. Hoboken, NJ: John Wiley & Sons; 2017. [Google Scholar]
- 12.Richardson G, Andersen D. Teamwork in group model building. System Dynamics Review. 1994;11(2):113–37. [Google Scholar]
- 13.Andersen DF, Richardson GP. Scripts for group model building. System Dynamics Review. 1997;13(2):107–29. [Google Scholar]
- 14.Siokou C, Morgan R, Shiell A. Group model building: a participatory approach to understanding and acting on systems. Public Health Research and Practice. 2014;25(1). doi: 10.17061/phrp2511404 [DOI] [PubMed] [Google Scholar]
- 15.Costanza R, Ruth M. Using Dynamic Modeling to Scope Environmental Problems and Build Consensus. Environmental Management. 1998;22(2):183–95. doi: 10.1007/s002679900095 [DOI] [PubMed] [Google Scholar]
- 16.Rouwette E, Vennix J, Van Mullekom T. Group model building effectiveness: a review of assessment studies. System Dynamics Review. 2002;18(1):5–45. [Google Scholar]
- 17.Scott RJ. Explaining how group model building supports enduring agreement. Journal of Management & Organization. 2019;25(6):783–806. [Google Scholar]
- 18.Scott RJ. Outcomes of Group Model Building. In: Group Model Building Using System Dynamics to Achive Enduring Agreement. 2018. p. 29–44. [Google Scholar]
- 19.Rouwette E, Vennix J. System Dynamics and Organizational Intervention. Systems Research and Behavioral Science. 2006;23:451–66. [Google Scholar]
- 20.Waqa G, Moodie M, Snowdon W, Latu C, Coriakula J, Allender S, et al. Exploring the dynamics of food-related policymaking processes and evidence use in Fiji using systems thinking. Health Res Policy Syst. 2017. Aug 29;15(1):74. doi: 10.1186/s12961-017-0240-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gullett HL, Brown GL, Collins D, Halko M, Gotler RS, Stange KC, et al. Using Community-Based System Dynamics to Address Structural Racism in Community Health Improvement. Journal of Public Health Management and Practice [Internet]. 2022;28(Supplement 4). Available from: https://journals.lww.com/jphmp/Fulltext/2022/07001/Using_Community_Based_System_Dynamics_to_Address.6.aspx doi: 10.1097/PHH.0000000000001492 [DOI] [PubMed] [Google Scholar]
- 22.Hendricks G, Savona N, Aguiar A, Alaba O, Booley S, Malczyk S, et al. Adolescents’ Perspectives on the Drivers of Obesity Using a Group Model Building Approach: A South African Perspective . Int J Environ Res Public Health. 2022. Feb 14;19(4). doi: 10.3390/ijerph19042160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Broekhuizen H, Ifeanyichi M, Cheelo M, Drury G, Pittalis C, Rouwette E, et al. Policy options for surgical mentoring: Lessons from Zambia based on stakeholder consultation and systems science. PLOS ONE. 2021. Sep 29;16(9):e0257597. doi: 10.1371/journal.pone.0257597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Broekhuizen H, Ifeanyichi M, Mwapasa G, Pittalis C, Noah P, Mkandawire N, et al. Improving Access to Surgery Through Surgical Team Mentoring–Policy Lessons From Group Model Building With Local Stakeholders in Malawi. International Journal of Health Policy and Management [Internet]. 2021; Available from: https://www.ijhpm.com/article_4088.html doi: 10.34172/ijhpm.2021.78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sušnik J, Masia S, Indriksone D, Brēmere I, Vamvakeridou-Lydroudia L. System dynamics modelling to explore the impacts of policies on the water-energy-food-land-climate nexus in Latvia. Science of The Total Environment. 2021. Jun 25;775:145827. doi: 10.1016/j.scitotenv.2021.145827 [DOI] [PubMed] [Google Scholar]
- 26.Ibrahim Shire M, Jun GT, Robinson S. Healthcare workers’ perspectives on participatory system dynamics modelling and simulation: designing safe and efficient hospital pharmacy dispensing systems together. Ergonomics. 2020. Aug;63(8):1044–56. doi: 10.1080/00140139.2020.1783459 [DOI] [PubMed] [Google Scholar]
- 27.Guariguata L, Rouwette EA, Murphy MM, Saint Ville A, Dunn LL, Hickey GM, et al. Using Group Model Building to Describe the System Driving Unhealthy Eating and Identify Intervention Points: A Participatory, Stakeholder Engagement Approach in the Caribbean. Nutrients. 2020. Jan 31;12(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sarmiento OL, Higuera-Mendieta D, Wilches-Mogollon MA, Guzman LA, Rodríguez DA, Morales R, et al. Urban Transformations and Health: Methods for TrUST—a Natural Experiment Evaluating the Impacts of a Mass Transit Cable Car in Bogotá, Colombia. Frontiers in Public Health [Internet]. 2020;8. Available from: https://www.frontiersin.org/articles/10.3389/fpubh.2020.00064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Weeks MR, Li J, Lounsbury D, Green HD, Abbott M, Berman M, et al. Using Participatory System Dynamics Modeling to Examine the Local HIV Test and Treatment Care Continuum in Order to Reduce Community Viral Load. Am J Community Psychol. 2017. Dec;60(3–4):584–98. doi: 10.1002/ajcp.12204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weeks MR, Lounsbury DW, Li J, Hirsch G, Berman M, Green HD, et al. Simulating system dynamics of the HIV care continuum to achieve treatment as prevention. PLOS ONE. 2020. Mar 19;15(3):e0230568. doi: 10.1371/journal.pone.0230568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Appel JM, Fullerton K, Hennessy E, Korn AR, Tovar A, Allender S, et al. Design and methods of Shape Up Under 5: Integration of systems science and community-engaged research to prevent early childhood obesity. PLoS One. 2019;14(8):e0220169. doi: 10.1371/journal.pone.0220169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hennessy E, Economos CD, Hammond RA. Integrating Complex Systems Methods to Advance Obesity Prevention Intervention Research. Health Educ Behav. 2020. Apr;47(2):213–23. doi: 10.1177/1090198119898649 [DOI] [PubMed] [Google Scholar]
- 33.Naumann RB, Kuhlberg J, Sandt L, Heiny S, Kumfer W, Marshall SW, et al. Integrating complex systems science into road safety research and practice, Part 2: applying systems tools to the problem of increasing pedestrian death rates. Inj Prev. 2020. Oct;26(5):424–31. doi: 10.1136/injuryprev-2019-043316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Allender S, Owen B, Kuhlberg J, Lowe J, Nagorcka-Smith P, Whelan J, et al. A Community Based Systems Diagram of Obesity Causes. PLOS ONE. 2015. Jul 8;10(7):e0129683. doi: 10.1371/journal.pone.0129683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McGlashan J, Hayward J, Brown A, Owen B, Millar L, Johnstone M, et al. Comparing complex perspectives on obesity drivers: action-driven communities and evidence-oriented experts. Obesity Science & Practice. 2018. Dec 1;4(6):575–81. doi: 10.1002/osp4.306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Langellier B.A., Kuhlberg J.A., Ballard E.A., Slesinski S.C., Stankov I., Gouveia N., et al. Using community-based system dynamics modeling to understand the complex systems that influence health in cities: The SALURBAL study. Health and Place [Internet]. 2019;60(()). Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L2003134782 doi: 10.1016/j.healthplace.2019.102215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Escobedo P, Gonzalez KD, Kuhlberg J, Calanche M, Baezconde-Garbanati L, Contreras R, et al. Community Needs Assessment among Latino Families in an Urban Public Housing Development. Hispanic Journal of Behavioral Sciences. 2019;41(3):344–62. [Google Scholar]
- 38.Fowler PJ, Wright K, Marcal KE, Ballard E, Hovmand PS. Capability Traps Impeding Homeless Services: A Community-Based System Dynamics Evaluation. J Soc Serv Res. 2019;45(3):348–59. doi: 10.1080/01488376.2018.1480560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dianati K, Zimmermann N, Milner J, Muindi K, Ezeh A, Chege M, et al. Household air pollution in Nairobi’s slums: A long-term policy evaluation using participatory system dynamics. Sci Total Environ. 2019. Apr 10;660:1108–34. doi: 10.1016/j.scitotenv.2018.12.430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ansah JP, Islam AM, Koh V, Ly V, Kol H, Matchar DB, et al. Systems modelling as an approach for understanding and building consensus on non-communicable diseases (NCD) management in Cambodia. BMC Health Services Research. 2019. Jan 3;19(1):2. doi: 10.1186/s12913-018-3830-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gamble E, Thorsen A, Black L. Expanding Strategic Opportunities in Nonprofits: Mapping the Interdependencies of Critical Performance Variables. Nonprofit Volunt Sect Q. 2019. Jun;48(3):616–32. doi: 10.1177/0899764019837599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Qayoom A H.W. Hadikusumo B. Multilevel safety culture affecting organization safety performance: a system dynamic approach. Engineering, Construction and Architectural Management. 2019. Jan 1;26(10):2326–46. [Google Scholar]
- 43.Hosseinichimeh N, Kim H, Ebrahimvandi A, Iams J, Andersen D. Using a Stakeholder Analysis to Improve Systems Modelling of Health Issues: The Impact of Progesterone Therapy on Infant Mortality in Ohio. Systems Research and Behavioral Science. 2019. Jul 1;36(4):476–93. [Google Scholar]
- 44.Baker P, Brown AD, Wingrove K, Allender S, Walls H, Cullerton K, et al. Generating political commitment for ending malnutrition in all its forms: A system dynamics approach for strengthening nutrition actor networks. Obes Rev. 2019. Nov;20 Suppl 2:30–44. doi: 10.1111/obr.12871 [DOI] [PubMed] [Google Scholar]
- 45.Gerritsen S, Renker-Darby A, Harré S, Rees D, Raroa DA, Eickstaedt M, et al. Improving low fruit and vegetable intake in children: Findings from a system dynamics, community group model building study. PLoS One. 2019;14(8):e0221107. doi: 10.1371/journal.pone.0221107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Urwannachotima N, Hanvoravongchai P, Ansah JP. Sugar-sweetened Beverage Tax and Potential Impact on Dental Caries in Thai Adults: An Evaluation Using the Group Model Building Approach. Systems Research and Behavioral Science. 2019. Feb 1;36(1):87–99. [Google Scholar]
- 47.Purwanto A, Sušnik J, Suryadi FX, de Fraiture C. Using group model building to develop a causal loop mapping of the water-energy-food security nexus in Karawang Regency, Indonesia. Journal of Cleaner Production. 2019. Dec 10;240:118170. [Google Scholar]
- 48.Roberts N, Li V, Atkinson JA, Heffernan M, McDonnell G, Prodan A, et al. Can the Target Set for Reducing Childhood Overweight and Obesity Be Met? A System Dynamics Modelling Study in New South Wales, Australia. Systems Research and Behavioral Science. 2019. Feb 1;36(1):36–52. [Google Scholar]
- 49.Mui Y, Ballard E, Lopatin E, Thornton RLJ, Pollack Porter KM, Gittelsohn J. A community-based system dynamics approach suggests solutions for improving healthy food access in a low-income urban environment. PLOS ONE. 2019. May 14;14(5):e0216985. doi: 10.1371/journal.pone.0216985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pagano A, Pluchinotta I, Pengal P, Cokan B, Giordano R. Engaging stakeholders in the assessment of NBS effectiveness in flood risk reduction: A participatory System Dynamics Model for benefits and co-benefits evaluation. The Science of the total environment. 2019;690:543–55. doi: 10.1016/j.scitotenv.2019.07.059 [DOI] [PubMed] [Google Scholar]
- 51.Malard J, JF Adamowski, M Rojas D, Carrera J, J Gálvez, Monadres H, et al. Use of participatory system dynamics modelling to assess the sustainability of smallholder agriculture. In St. Joseph, MI: ASABE; 2015. p. 1. (ASABE Paper No. 152189490). Available from: https://elibrary.asabe.org/abstract.asp?aid=46322&t=5 [Google Scholar]
- 52.Koh K, Reno R, Hyder A. Designing an Agent-Based Model Using Group Model Building: Application to Food Insecurity Patterns in a U.S. Midwestern Metropolitan City. J Urban Health. 2018. Apr;95(2):278–89. doi: 10.1007/s11524-018-0230-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ansah JP, Matchar DB, Koh V, Schoenenberger L. Mapping the Dynamic Complexity of Chronic Disease Care in Singapore: Using Group Model Building in Knowledge Elicitation. Systems Research and Behavioral Science. 2018. Nov 1;35(6):759–75. [Google Scholar]
- 54.Eker S, Zimmermann N, Carnohan S, Davies M. Participatory system dynamics modelling for housing, energy and wellbeing interactions. Building Research & Information. 2018. Oct 3;46(7):738–54. [Google Scholar]
- 55.Chalise N, Kumar P, Priyadarshini P, Yadama GN. Dynamics of sustained use and abandonment of clean cooking systems: lessons from rural India. Environmental Research Letters. 2018. Mar;13(3):035010. [Google Scholar]
- 56.Lembani M, de Pinho H, Delobelle P, Zarowsky C, Mathole T, Ager A. Understanding key drivers of performance in the provision of maternal health services in eastern cape, South Africa: a systems analysis using group model building. BMC Health Services Research. 2018. Nov 29;18(1):912. doi: 10.1186/s12913-018-3726-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Reno R. Using group model building to develop a culturally grounded model of breastfeeding for low-income African American women in the USA. J Clin Nurs. 2018. Sep;27(17–18):3363–76. doi: 10.1111/jocn.13791 [DOI] [PubMed] [Google Scholar]
- 58.Brown H, Proust K, Newell B, Spickett J, Capon T, Bartholomew L. Cool Communities-Urban Density, Trees, and Health. Int J Environ Res Public Health. 2018. Jul 22;15(7). doi: 10.3390/ijerph15071547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Atkinson JA, O’Donnell E, Wiggers J, McDonnell G, Mitchell J, Freebairn L, et al. Dynamic simulation modelling of policy responses to reduce alcohol-related harms: rationale and procedure for a participatory approach. Public Health Research & Practice [Internet]. Available from: https://www.phrp.com.au/issues/february-2017-volume-27-issue-1-2/dynamic-simulation-modelling-of-policy-responses-to-reduce-alcohol-related-harms-rationale-and-procedure-for-a-participatory-approach/ doi: 10.17061/phrp2711707 [DOI] [PubMed] [Google Scholar]
- 60.Freebairn L, Rychetnik L, Atkinson JA, Kelly P, McDonnell G, Roberts N, et al. Knowledge mobilisation for policy development: implementing systems approaches through participatory dynamic simulation modelling. Health Res Policy Syst. 2017. Oct 2;15(1):83. doi: 10.1186/s12961-017-0245-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kopainsky B, Hager G, Herrera H, Nyanga PH. Transforming food systems at local levels: Using participatory system dynamics in an interactive manner to refine small-scale farmers’ mental models. Ecological Modelling. 2017;362:101–10. [Google Scholar]
- 62.Morrow-Howell N, Halvorsen CJ, Hovmand P, Lee C, Ballard E. Conceptualizing Productive Engagement in a System Dynamics Framework. Innov Aging. 2017. Mar 1;1(1):igx018. doi: 10.1093/geroni/igx018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Macmillan A, Woodcock J. Understanding bicycling in cities using system dynamics modelling. Journal of Transport & Health. 2017. Dec 1;7:269–79. doi: 10.1016/j.jth.2017.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mumba C, Skjerve E, Rich M, Rich KM. Application of system dynamics and participatory spatial group model building in animal health: A case study of East Coast Fever interventions in Lundazi and Monze districts of Zambia. PLoS One. 2017;12(12):e0189878. doi: 10.1371/journal.pone.0189878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jetha A, Kernan L, Kurowski A. Conceptualizing the dynamics of workplace stress: a systems-based study of nursing aides. BMC Health Serv Res. 2017. Jan 5;17(1):12. doi: 10.1186/s12913-016-1955-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Trani JF, Ballard E, Bakhshi P, Hovmand P. Community based system dynamic as an approach for understanding and acting on messy problems: a case study for global mental health intervention in Afghanistan. Confl Health. 2016;10:25. doi: 10.1186/s13031-016-0089-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jetha A, Pransky G, Fish J, Hettinger LJ. Return-to-Work Within a Complex and Dynamic Organizational Work Disability System. J Occup Rehabil. 2016. Sep;26(3):276–85. doi: 10.1007/s10926-015-9613-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Frerichs L, Lich KH, Funchess M, Burrell M, Cerulli C, Bedell P, et al. Applying Critical Race Theory to Group Model Building Methods to Address Community Violence. Prog Community Health Partnersh. 2016;10(3):443–59. doi: 10.1353/cpr.2016.0051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zimmerman L, Lounsbury DW, Rosen CS, Kimerling R, Trafton JA, Lindley SE. Participatory System Dynamics Modeling: Increasing Stakeholder Engagement and Precision to Improve Implementation Planning in Systems. Adm Policy Ment Health. 2016. Nov;43(6):834–49. doi: 10.1007/s10488-016-0754-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Macmillan A, Davies M, Shrubsole C, Luxford N, May N, Chiu LF, et al. Integrated decision-making about housing, energy and wellbeing: a qualitative system dynamics model. Environ Health. 2016. Mar 8;15 Suppl 1(Suppl 1):37. doi: 10.1186/s12940-016-0098-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Brownson RC, Kemner AL, Brennan LK. Applying a mixed-methods evaluation to Healthy Kids, Healthy Communities. J Public Health Manag Pract. 2015. Jun;21 Suppl 3(Suppl 3):S16–26. doi: 10.1097/PHH.0000000000000233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Homa L, Rose J, Hovmand PS, Cherng ST, Riolo RL, Kraus A, et al. A participatory model of the paradox of primary care. Ann Fam Med. 2015. Sep;13(5):456–65. doi: 10.1370/afm.1841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Thomas IM, Reilly SR. Group model building: a framework for organizing healthy community program and policy initiatives in Columbia, Missouri. J Public Health Manag Pract. 2015. Jun;21 Suppl 3:S79–83. doi: 10.1097/PHH.0000000000000209 [DOI] [PubMed] [Google Scholar]
- 74.Brennan LK, Sabounchi NS, Kemner AL, Hovmand P. Systems thinking in 49 communities related to healthy eating, active living, and childhood obesity. J Public Health Manag Pract. 2015. Jun;21 Suppl 3:S55–69. doi: 10.1097/PHH.0000000000000248 [DOI] [PubMed] [Google Scholar]
- 75.Munar W, Hovmand PS, Fleming C, Darmstadt GL. Scaling-up impact in perinatology through systems science: Bridging the collaboration and translational divides in cross-disciplinary research and public policy. Semin Perinatol. 2015. Aug;39(5):416–23. doi: 10.1053/j.semperi.2015.06.003 [DOI] [PubMed] [Google Scholar]
- 76.Keane P, Ortega A, Linville J. Healthy Kids, Healthy Cuba: findings from a group model building process in the rural Southwest. J Public Health Manag Pract. 2015. Jun;21 Suppl 3:S70–73. doi: 10.1097/PHH.0000000000000250 [DOI] [PubMed] [Google Scholar]
- 77.Moreland JW. Improving Park Space Access for the Healthy Kids, Healthy Communities Partnership in Denver, Colorado. Journal of Public Health Management and Practice. 2015;21:S84–7. [DOI] [PubMed] [Google Scholar]
- 78.Skouteris H, Huang T, Millar L, Kuhlberg J, Dodd J, Callaway L, et al. A systems approach to reducing maternal obesity: The Health in Preconception, Pregnancy and Postbirth (HIPPP) Collaborative. Aust N Z J Obstet Gynaecol. 2015. Aug;55(4):397–400. doi: 10.1111/ajo.12341 [DOI] [PubMed] [Google Scholar]
- 79.Esensoy AV, Carter MW. Health system modelling for policy development and evaluation: Using qualitative methods to capture the whole-system perspective. Operations Research for Health Care. 2015;4:15–26. [Google Scholar]
- 80.Ager AK, Lembani M, Mohammed A, Mohammed Ashir G, Abdulwahab A, de Pinho H, et al. Health service resilience in Yobe state, Nigeria in the context of the Boko Haram insurgency: a systems dynamics analysis using group model building. Conflict and Health. 2015. Oct 5;9(1):30. doi: 10.1186/s13031-015-0056-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.van Nistelrooij LPJ, Rouwette EAJA, Verstijnen IM, Vennix JAM. The Eye of the Beholder: A Case Example of Changing Clients’ Perspectives Through Involvement in the Model Validation Process. Systems Research and Behavioral Science. 2015. Jul 1;32(4):437–49. [Google Scholar]
- 82.Macmillan A, Connor J, Witten K, Kearns R, Rees D, Woodward A. The societal costs and benefits of commuter bicycling: simulating the effects of specific policies using system dynamics modeling. Environ Health Perspect. 2014. Apr;122(4):335–44. doi: 10.1289/ehp.1307250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Narayana S A., Elias A A., Pati R K. Reverse logistics in the pharmaceuticals industry: a systemic analysis. The International Journal of Logistics Management. 2014. Jan 1;25(2):379–98. [Google Scholar]
- 84.Biroscak BJ, Schneider T, Panzera AD, Bryant CA, McDermott RJ, Mayer AB, et al. Applying Systems Science to Evaluate a Community-Based Social Marketing Innovation: A Case Study. Social Marketing Quarterly. 2014. Dec 1;20(4):247–67. [Google Scholar]
- 85.Rouwette E, Bleijenbergh I, Vennix J. Group Model-Building to Support Public Policy: Addressing a Conflicted Situation in a Problem Neighbourhood. Systems Research and Behavioral Science. 2014. Aug 1;33. [Google Scholar]
- 86.Merrill JA, Deegan M, Wilson RV, Kaushal R, Fredericks K. A system dynamics evaluation model: implementation of health information exchange for public health reporting. Journal of the American Medical Informatics Association. 2013. Jan;20(e1):e131–8. doi: 10.1136/amiajnl-2012-001289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hernantes J, Labaka L, Lauge A, Sarriegi J, Gonzalez J. Group model building: A collaborative modelling methodology applied to critical infrastructure protection. Int J of Organisational Design and Engineering. 2012. Jan 1;2:41–60. [Google Scholar]
- 88.Goh YM, Love PED, Stagbouer G, Annesley C. Dynamics of safety performance and culture: A group model building approach. Accident Analysis & Prevention. 2012. Sep 1;48:118–25. doi: 10.1016/j.aap.2011.05.010 [DOI] [PubMed] [Google Scholar]
- 89.Bridgewater K, Peterson S, McDevitt J, Hemenway D, Bass J, Bothwell P, et al. A Community-Based Systems Learning Approach to Understanding Youth Violence in Boston. Progress in community health partnerships: research, education, and action. 2011. Mar 1;5:67–75. doi: 10.1353/cpr.2011.0011 [DOI] [PubMed] [Google Scholar]
- 90.Thompson J, Forster C, Werner C, Peterson T. Mediated Modeling: Using Collaborative Processes to Integrate Scientist and Stakeholder Knowledge about Greenhouse Gas Emissions in an Urban Ecosystem. Society & Natural Resources. 2010. Aug 1;23:742−757. [Google Scholar]
- 91.Stave K. Participatory system dynamics modeling for sustainable environmental management: Observations from four cases. Sustainability. 2010;2:2762–84. [Google Scholar]
- 92.Cavana RY, Clifford LV. Demonstrating the utility of system dynamics for public policy analysis in New Zealand: the case of excise tax policy on tobacco. System Dynamics Review. 2006. Dec 1;22(4):321–48. [Google Scholar]
- 93.Stave KA. Using system dynamics to improve public participation in environmental decisions. System Dynamics Review. 2002. Jun 1;18(2):139–67. [Google Scholar]
- 94.World Bank. Data. 2021. World Bank Country and Lending Groups. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups [Google Scholar]
- 95.Black LJ. When visuals are boundary objects in system dynamics work. System Dynamics Review. 2013. Apr 1;29(2):70–86. [Google Scholar]
- 96.Ghaffarzadegan N, Lyneis J, Richardson G. How Small System Dynamics Models Can Help the Public Policy Process. System Dynamics Review. 2011;271(1):22–44. [Google Scholar]
- 97.Hovmand P. Group Model Building and Community-Based System Dynamics Process. In 2014. [Google Scholar]
- 98.Gerritsen S, Harré S, Rees D, Renker-Darby A, Bartos AE, Waterlander WE, et al. Community Group Model Building as a Method for Engaging Participants and Mobilising Action in Public Health. Int J Environ Res Public Health. 2020. May 15;17(10):3457. doi: 10.3390/ijerph17103457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Cassel MA, Hinsberger M. Flood partnerships: a participatory approach to develop and implement the Flood Risk Management Plans. Journal of Flood Risk Management. 2017;10(2):164–72. [Google Scholar]
- 100.Iturriza M, Hernantes J, Labaka L. Coming to Action: Operationalizing City Resilience. Sustainability. 2019;11(11):1–18. [Google Scholar]
- 101.Chen PG, Diaz N, Lucas G, Rosenthal MS. Dissemination of results in community-based participatory research. Am J Prev Med. 2010. Oct;39(4):372–8. doi: 10.1016/j.amepre.2010.05.021 [DOI] [PubMed] [Google Scholar]
- 102.Hosseinichimeh N, MacDonald R, Hyder A, Ebrahimvandi A, Porter L, Reno R, et al. Group Model Building Techniques for Rapid Elicitation of Parameter Values, Effect Sizes, and Data Sources. System Dynamics Review. 2017;33(1):71–84. [Google Scholar]
- 103.Vennix JAM. Group model-building: tackling messy problems. System Dynamics Review. 1999. Dec 1;15(4):379–401. [Google Scholar]
- 104.Bendoly E. System Dynamics Understanding in Projects: Information Sharing, Psychological Safety, and Performance Effects. Production and Operations Management. 2014. Aug 1;23(8):1352–69. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(XLSX)
Data Availability Statement
All data files are available from the Github repository (https://github.com/weannemyrrh/Group-Model-Building-Data).