Abstract
PURPOSE:
To evaluate physician-reported assessments of an established faculty orientation program for new radiation oncology physicians at a large academic center and to prospectively analyze the effects of an onboarding improvement program based on those assessments.
MATERIALS AND METHODS:
An anonymous survey was designed and distributed to physicians new to the department who received onboarding orientation between 2013 and 2017. Survey questions addressed the comprehensiveness, effectiveness, and utility of various orientation activities. On the basis of the survey results, an improved onboarding program was designed and implemented for nine new faculty members between May 2018 and November 2018. A post-intervention survey querying topics similar to those in the pre-intervention survey was distributed to the new faculty members. Descriptive statistics were generated to compare the pre-intervention and post-intervention groups.
RESULTS:
The overall rate of survey completion was 85% (17 of 20). The intervention program markedly improved physician assessment of comprehensiveness and effectiveness of the onboarding process. Physicians strongly and consistently identified mentor shadowing, on-the-job training, and other faculty mentorship activities as the most important components of an effective onboarding experience.
CONCLUSION:
An enhanced, tailored, person-oriented, formal onboarding improvement program significantly increased physician assessment scores of comprehensiveness and effectiveness of the faculty onboarding process. This model can serve as a framework for increasing physician preparedness, encouraging early physician mentorship, and ensuring a universal standard of quality across large practices.
INTRODUCTION
The processes of orientation and onboarding are important yet separate facets of physician development. Many departments have established an orientation that includes didactic information about institutional policies and benefits, instruction about where to find various clinic and personal spaces, and printed or electronic material about software programs and applications. But while that type of knowledge is necessary, it is generally not sufficient. Often excluded in orientation programs are hands-on components such as demonstrations of physician-centered processes and decision-making, identification of relationships and collaborations between members of the department, mentorship, and ongoing assessment to ensure that physicians have gained the knowledge and skills necessary to function in their new roles and become organizational insiders.1 The process of imparting this person-centered knowledge to new physician members of a department can be broadly defined as onboarding.
Current onboarding programs for new medical staff often assume that residency and fellowship training provide the knowledge needed to become a fully operational member of the medical care team. Specific policies, institutional practices, and organizational structures are left to be navigated until after the physician has become clinically active. Within radiation oncology specifically, residents are rarely able to independently perform certain duties of an attending physician because of billing requirements. Furthermore, with the expansion of cancer care networks, new physicians are often expected to see patients in several different clinical locations, which can further increase the complexity of the onboarding process.
Efforts to optimize our onboarding process have recently been prioritized at Memorial Sloan Kettering Cancer Center because our department and institution have expanded outpatient services beyond our primary campus to facilities in the broader regional network of the New York tri-state area. These efforts are consistent with our mission to provide clinical excellence and uniformity between our tertiary hospital and our regional sites nearer to patients’ homes, which minimizes the social and financial burden that this care places on patients and their families. To support this initiative, many faculty now practice at more than one campus within the network. Within radiation oncology, all cases are reviewed centrally and prospectively. Furthermore, departmental policies, practice patterns, and access to and ability to enroll on institutional and national research studies need to be consistent across all of the regional network sites to ensure consistency of clinical capability, physician expertise, and patient experience. To continue to support this consistency throughout our network and in preparation for continued sustainable growth of our department, the leadership team in the Department of Radiation Oncology at our institution convened to investigate our current practices and improve upon our current onboarding experience.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board as a quality improvement project and not as research on human subjects. A radiation oncology faculty member (J.J.C.) was identified to lead onboarding implementation and was recognized as the Onboarding Director.
The established orientation program generally consisted of 1 to 2 weeks of departmental, information technology, and human resources orientation before new physicians were scheduled to see patients. To gain insight into the established program, an anonymous pre-intervention survey was conducted among radiation oncology physicians who had joined the faculty from another institution between 2013 and 2017. The survey was designed and distributed by the Onboarding Director to expand upon and gain insight from discussions and feedback from the recent faculty who had gone through the orientation program. Physicians who had trained at the study institution were excluded. The complete survey questionnaire is included in Appendix Figure A1 (online only). On the basis of pre-intervention survey results, the existing orientation program was modified to address common deficiencies and expand on the high-yield elements. The product was a comprehensive preclinical and clinical onboarding program approximately 4 weeks long (Fig 1).
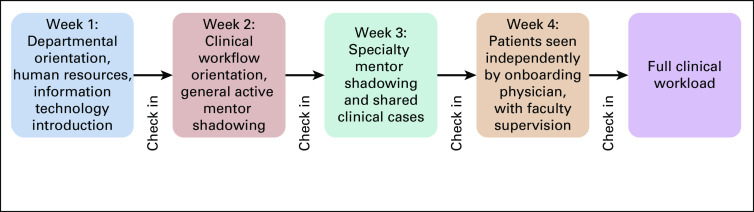
Fig 1.
Schedule and elements of improved onboarding program.
During the period when physicians shadowed their mentors (weeks 2 to 3 in Fig 1), site-specific checklists of must-know topics were distributed to both the onboarding faculty member and the mentor. At the end of each week, onboarding faculty members had a conference with the Onboarding Director to review the previous week’s activities and experiences, assess progress, and adjust the next week’s agenda if objectives of the previous week were not met.
In addition, a comprehensive Faculty Orientation Guide outlining common workflows, departmental practices, and specific disease-site treatment guidelines was compiled by the Onboarding Director with input from faculty leaders of disease teams, nursing staff, radiation therapy supervisors, and medical physics faculty. The guide was distributed to all new faculty members for reference and use during and after the orientation period.
After the program redesign, an anonymous post-intervention survey, designed and implemented by the Onboarding Director, was distributed to all radiation oncology faculty physicians undergoing the new onboarding program in 2018. Question #3 from the pre-intervention survey was omitted from the post-intervention survey because the intended time point of Question #3 was at least 1 year after completion of the onboarding program. The post-intervention survey is provided in Appendix Figure A2 (online only). Descriptive statistics were used to compare survey results before and after the intervention. A summary of the methods is provided in Figure 2.
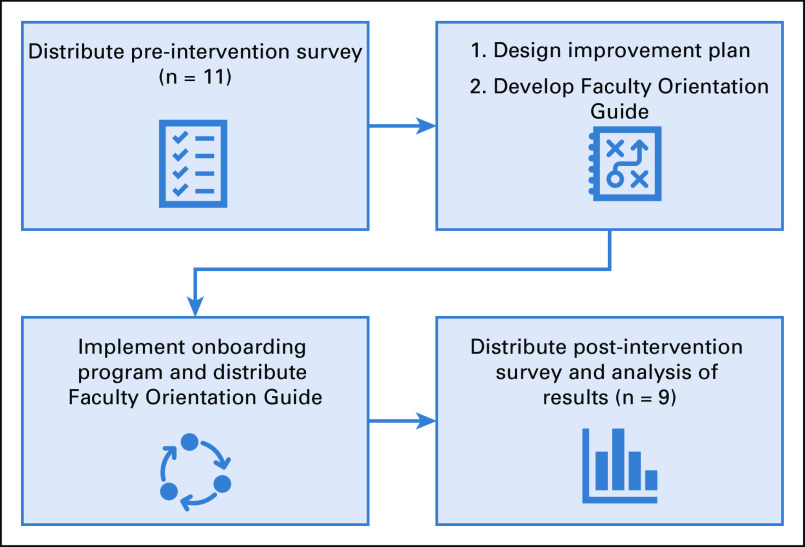
Fig 2.
Outline of method used to investigate the onboarding process, including administering a pre-intervention survey, designing an improvement plan, implementing an onboarding program, and conducting a post-intervention survey.
RESULTS
Pre-Intervention Survey
We identified 11 radiation oncology faculty physicians who came from outside institutions between 2013 and 2017 and had been previously oriented at the time of the study. E-mail invitations were sent to each eligible physician, and a total of eight faculty members submitted completed surveys, for a response rate of 72.7%. Results of the pre-intervention survey are presented in Appendix Figure A3 (online only).
Post-Intervention Survey
Between May 2018 and November 2018, a total of nine faculty members from outside institutions were hired and brought onboard with the enhanced onboarding program. After they completed the program, e-mail invitations were sent to faculty members and a total of 9 submitted completed surveys for a response rate of 100%. Results of the post-intervention survey are presented in Appendix Figure A4 (online only). A comparison of pre- and post-intervention assessments of the onboarding experience is shown in Figure 3.
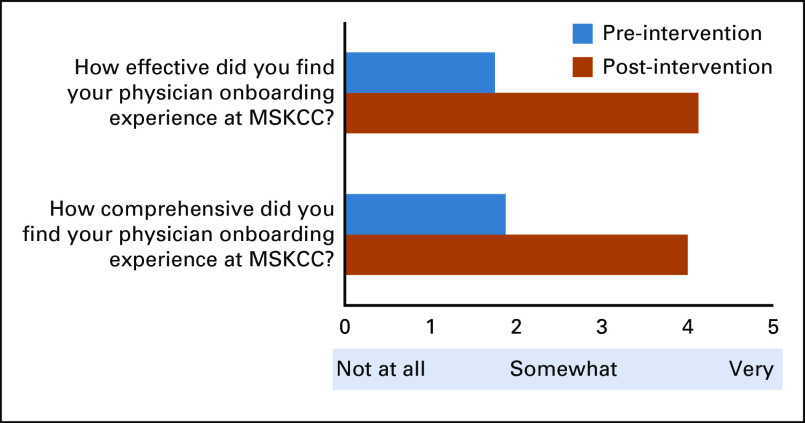
Fig 3.
Comparison of effectiveness and comprehensiveness of physician onboarding experience pre- and post-intervention of onboarding improvement program. MSKCC, Memorial Sloan Kettering Cancer Center.
Post-Intervention Qualitative Feedback
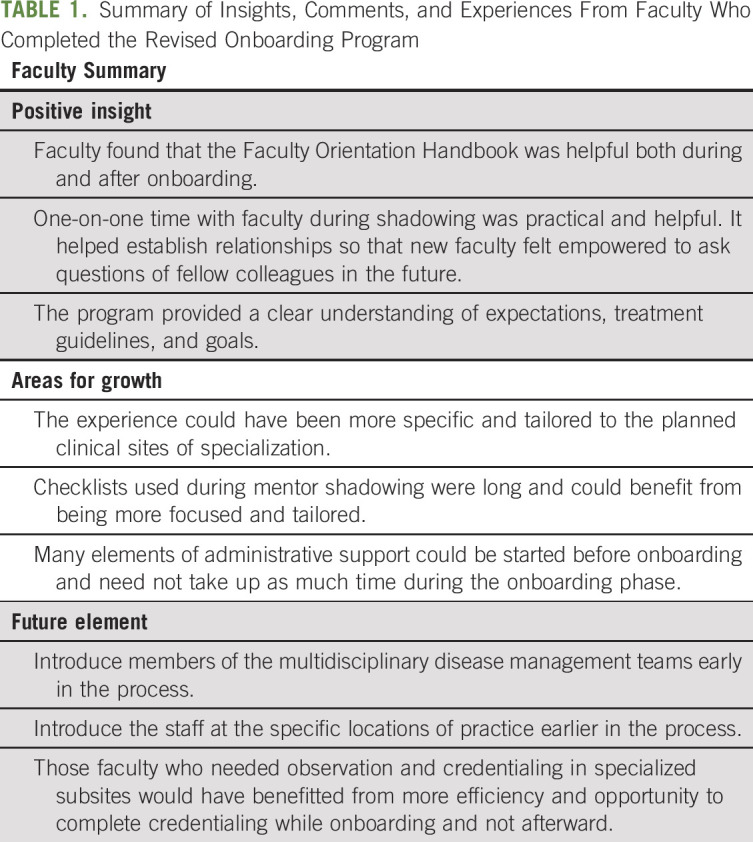
Physicians who completed the redesigned program were asked to summarize their insights and experiences and provide suggestions for other elements that could be integrated into future programs (see summary of comments in Table 1).
TABLE 1.
Summary of Insights, Comments, and Experiences From Faculty Who Completed the Revised Onboarding Program
DISCUSSION
We conducted a survey-based analysis of our faculty onboarding process at a large academic center and prospectively analyzed interventions designed to improve the process. Our primary findings were the following. First, an orientation that was not iterative or tailored to physicians new to the institution was of limited utility. Second, by collecting feedback and focusing on the onboarding components that established faculty found to be most informative, the onboarding process was perceived to be more comprehensive and applicable to clinical practice. Finally, although small numbers of participants precluded statistical testing, we were able to identify and prioritize individual components of the program that were the most useful to physicians at our institution, while minimizing time on those activities that were of limited use. On the basis of the post-intervention results, we have continued to implement the improved onboarding program with subsequent new faculty. We also continue to collect feedback from faculty about how to further improve and enhance the program.
A critical finding in this study that likely contributed to overall effectiveness of the new onboarding program was the importance of integrating opportunities for faculty mentorship, including clinical mentor shadowing and elbow-to-elbow interactions (compared with didactic or online course activities). Faculty mentorship was identified as high yield in the pre-intervention survey, so it was prioritized in the redesigned onboarding program and became the most important element in the post-intervention assessment by new physicians. Onboarding that involves one-on-one faculty mentorship helps establish and facilitate mentor relationships for junior faculty, which are critical for physicians’ success and well-being. Without proper professional preparation and investment in mentoring, new physicians are at high risk for exhaustion, detachment, and professional burnout.2 Burnout can have many negative effects on a health care system, including a high physician turnover rate, subsequent impaired access to care for patients, and compromised patient safety. Organizational-directed interventions such as more comprehensive onboarding programs that emphasize an early investment in mentoring can help increase physician satisfaction, provide a more favorable environment for clinical and research mentorship, and reduce the risk of professional burnout.3,4
In addition to identifying a need for physicians who were coming onboard to shadow their faculty mentors in the clinical setting, we also identified a need for a ramp-up period of independent clinical activity with truncated patient volume (see question 3 in Appendix Fig A4), which helped create opportunities for them to consult with and have longitudinal interactions with physician mentors. The ramp-up period also helped physicians become familiar with workflow and workplace culture and organization, and helped them troubleshoot issues before being required to handle a full clinical load of patients. In addition, preparing physicians to practice in several different clinical locations has highlighted the benefit of consistent workflows and expectations across the institution. In response, the department developed the Faculty Orientation Guide to use in conjunction with the onboarding process, which includes processes and procedures as well as disease-specific treatment guidelines for reference. The guide provided to faculty is published in electronic format, which allows for periodic updates and revisions to keep material up to date. Each radiation disease-site team now convenes a retreat at least once a year to review and update the clinical guidelines for ongoing use.
Finally, the now-active onboarding program outlined in this study allows for those undergoing the program to have protected time to learn, demonstrate proficiency, and independently execute a comprehensive body of activities and processes. Written site-specific checklists have been previously described as an effective tool for tracking and ensuring competency in navigating the work environment and gaining knowledge of resources within a large medical group.5 The use of site-specific checklists in clinical observation and mentor shadowing environments ensures that all predetermined topics are covered and that knowledge is converted to performance and action. Weekly check-ins serve as a type of formative assessment to allow subsequent activities and experiences to be modified as necessary.6 Although centralized expert review of all cases treated in the regional network was not directly assessed in this study, that type of review is perceived to be a useful ongoing measure of progress and competency that allows for ongoing engagement between attending physicians in the regional network and disease team leaders at the central campus. Centralized review has been recognized as a critical component of the ongoing unification of quality7 and plays a crucial role in ensuring a high level of quality and expertise among all faculty.
Over the last decade, there has been an increase in consolidation of independent practices into larger hospital systems, most pronounced in oncology.8 There is also a trend toward larger, multicenter oncology practice settings.9 As these trends continue, adequate onboarding of physicians and the development of an environment that supports meaningful faculty mentorship are paramount to ensure increased access to a universal standard of quality. The framework discussed in this study provides insights into our institution’s attempt to unify clinical quality across a large department with a range of practice locations, beginning with onboarding. Although the process of conducting assessment surveys before and after the onboarding program is most applicable to larger, multicenter practices and may not be possible in smaller practices, this study outlines thematic elements of onboarding that can be integrated into a variety of practice settings to ensure well-prepared and well-supported physicians.
Strengths of this investigation include the high participation rates in both the pre- and post-intervention surveys and the inclusion of both quantitative and qualitative feedback. Direct costs of implementing this program were low. Indirect costs were related to a temporary decrease in expected clinical revenue because of the truncated clinical volume of physicians within their first 4 weeks of practicing. However, with this investment, physicians will ultimately consume less time and resources than they would with piecemeal onboarding over many months. Limitations of this study include the use of unvalidated pre- and post-intervention surveys among different groups of physicians. The lag time of up to 5 years in the pre-intervention survey increases the potential for recall bias. Therefore, quantifying the impact of the onboarding program should be done with caution. In addition, this study includes only short-term results that are self-reported. Physician satisfaction is not directly assessed in this study. We plan to enhance the cooperation between onboarding and the Quality Assurance/Quality Improvement teams to allow the Quality Assurance process to inform critical onboarding elements and vice versa.
In conclusion, we developed an enhanced comprehensive onboarding program for new faculty joining a radiation oncology department within a large and geographically diverse network, based on survey input of recent faculty who had undergone previous onboarding programs. The improved onboarding program provides a comprehensive educational experience that moves learning from the rote to the meaningful through increased access to faculty mentors in initial mentor shadowing and ongoing case-specific feedback. The program has been particularly effective in promoting unification of policies, procedures, and treatment approaches across multiple practice sites. This model could serve as a framework for other departments both within and outside radiation oncology.
Appendix
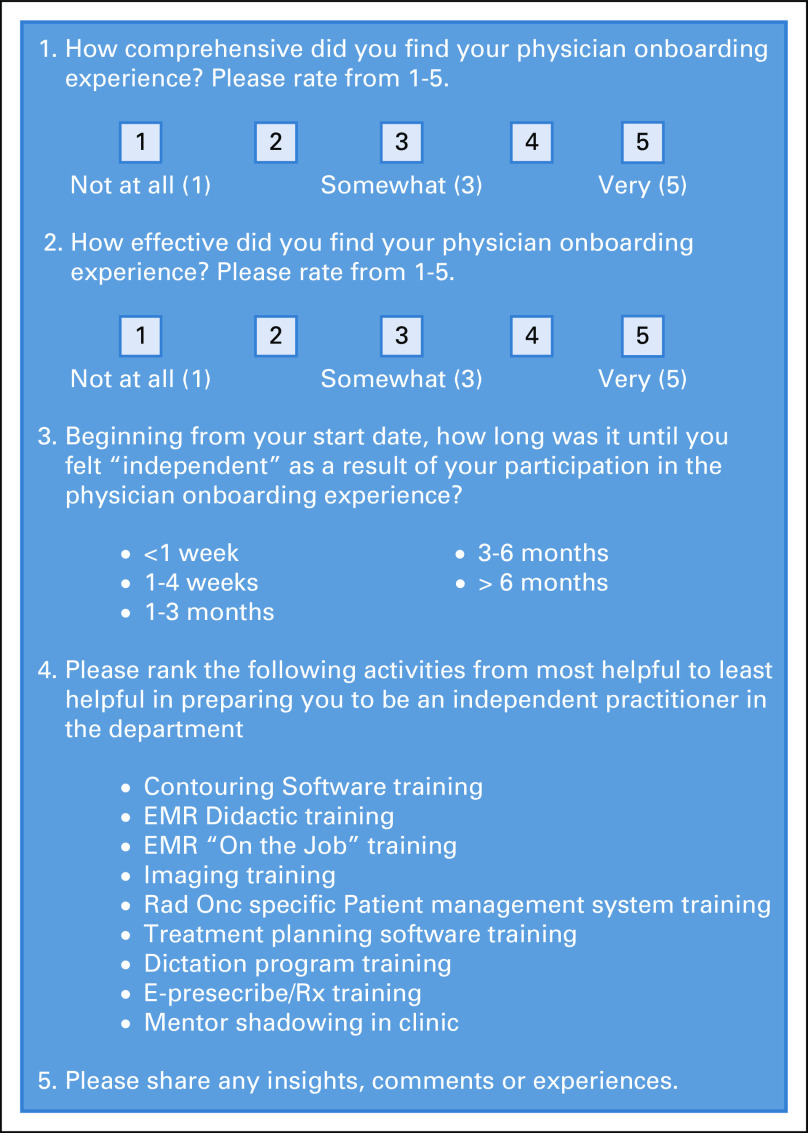
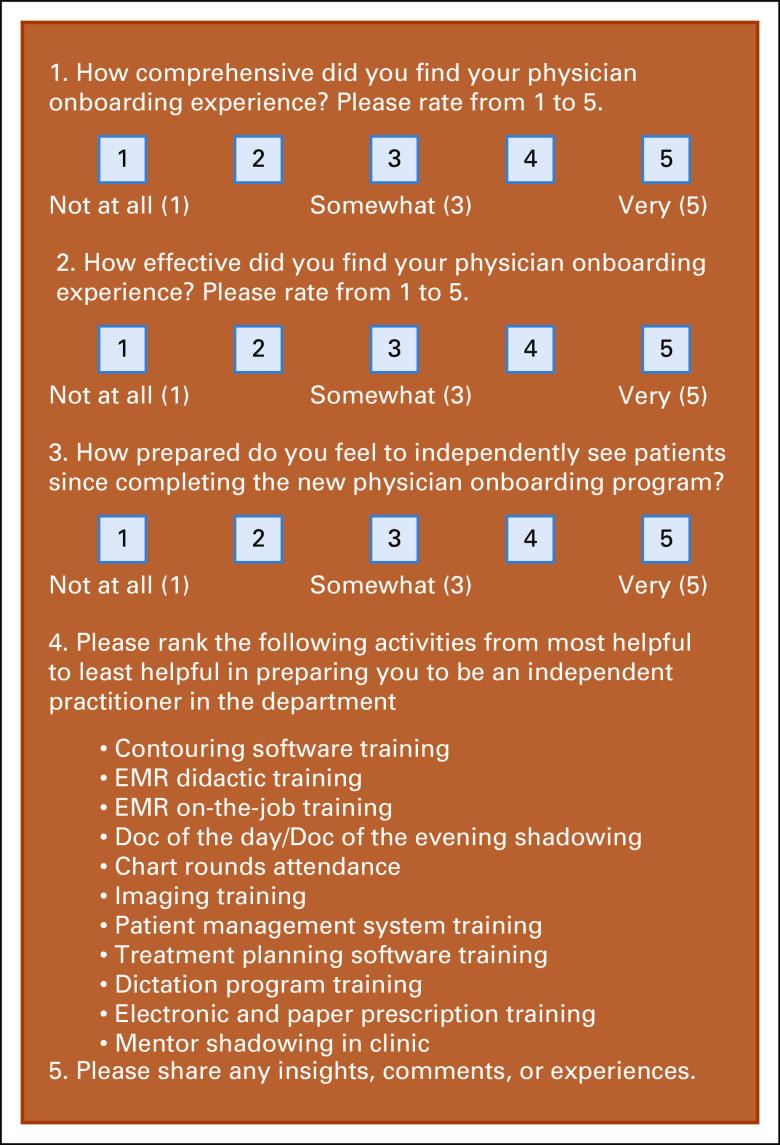
Fig A1.
Pre-intervention survey distributed to recently onboarded faculty members who came from outside institutions.
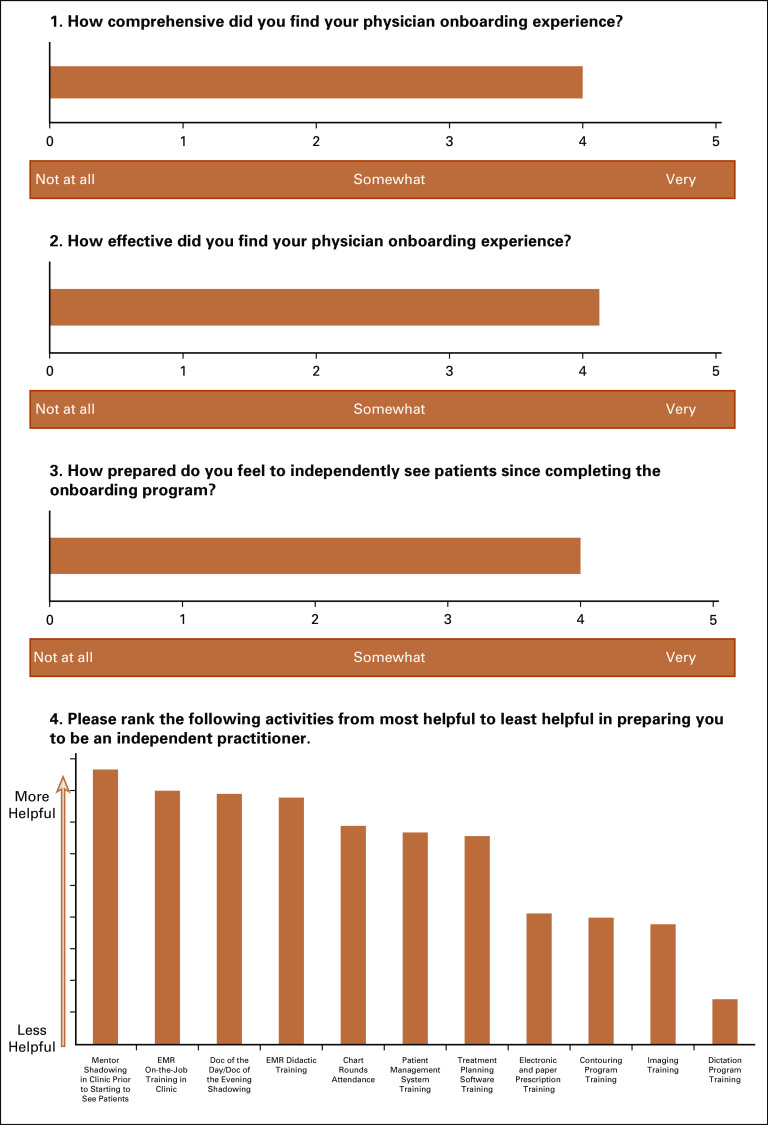
Fig A2.
Post-intervention survey distributed to onboarded faculty members who came from outside institutions. EMR, electronic medical record. Doc of the day/Doc of the evening, on-call physician for ad hoc clinical or treatment-related issues during scheduled radiation treatments.
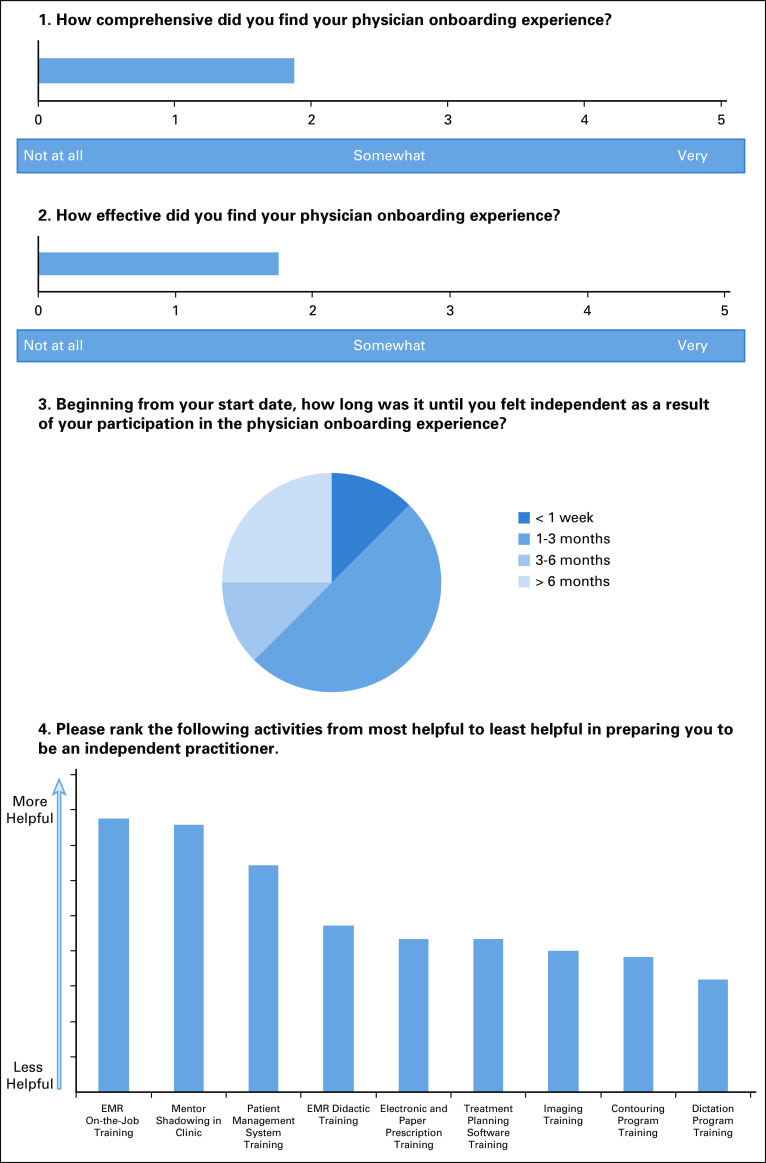
Fig A3.
Results of the pre-intervention survey of recently onboarded faculty members before the onboarding improvement program was implemented. EMR, electronic medical record.
Fig A4.
Results of the post-intervention survey of onboarded faculty members after the onboarding improvement program was implemented. EMR, electronic medical record.
AUTHOR CONTRIBUTIONS
Conception and design: John J. Cuaron
Collection and assembly of data: John J. Cuaron
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
From Orientation to Onboarding: A Survey-Based Departmental Improvement Program for New Radiation Oncology Faculty Physicians
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/site/ifc/journal-policies.html.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Erin F. Gillespie
Other Relationship: eContour.org
Daniel R. Gomez
Honoraria: Bristol-Myers Squibb, Merck, AstraZeneca, Varian Medical Systems, US Oncology, RefleXion Medical, Vindico Medical Education, WebMD, Medscape
Consulting or Advisory Role: AstraZeneca
Research Funding: AstraZeneca, Bristol-Myers Squibb, Merck
Travel, Accommodations, Expenses: AstraZeneca, Research to Practice, US Oncology, Vindico Medical Education, WebMD
Atif J. Khan
Employment: Memorial Sloan Kettering Cancer Center
Research Funding: Clovis Oncology
Borys Mychalczak
Consulting or Advisory Role: eviCore healthcare
No other potential conflicts of interest were reported.
REFERENCES
- 1.Bauer TN, Erdogan B: Organizational socialization: The effective onboarding of new employees, in Zedeck S. (ed): APA Handbook of Industrial and Organizational Psychology: Maintaining, Expanding, and Contracting the Organization, Volume 3. Washington, DC, American Psychological Association, 2011, pp 51-64 [Google Scholar]
- 2.Shanafelt TD, Boone S, Tan L, et al. : Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med 172:1377-1385, 2012 [DOI] [PubMed] [Google Scholar]
- 3.Swensen SJ, Shanafelt T: An organizational framework to reduce professional burnout and bring back joy in practice. Jt Comm J Qual Patient Saf 43:308-313, 2017 [DOI] [PubMed] [Google Scholar]
- 4.Fleig-Palmer MM, Rathert C: Interpersonal mentoring and its influence on retention of valued health care workers: The moderating role of affective commitment. Health Care Manage Rev 40:56-64, 2015 [DOI] [PubMed] [Google Scholar]
- 5.Tom W, Tom W, Albarran D, et al. : Ensuring mentorship of new physicians in their first year: Constructs for new mentoring processes. Perm J 23, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spolsky B, Hult FM: The Handbook of Educational Linguistics. Malden, MA, Blackwell Publishing, 2008 [Google Scholar]
- 7.Thaker NG, Sturdevant L, Jhingran A, et al. : Assessing the quality of a radiation oncology case-based, peer-review program in an integrated academic and community cancer center network. J Oncol Pract 12:e476-e486, 2016 [DOI] [PubMed] [Google Scholar]
- 8.Nikpay SS, Richards MR, Penson D: Hospital-physician consolidation accelerated in the past decade in cardiology, oncology. Health Aff (Millwood) 37:1123-1127, 2018 [DOI] [PubMed] [Google Scholar]
- 9.Kirkwood MK, Hanley A, Bruinooge SS, et al. : The state of oncology practice in America, 2018: Results of the ASCO Practice Census Survey. J Oncol Pract 14:e412-e420, 2018 [DOI] [PubMed] [Google Scholar]