Abstract
With the incorporation of pass/fail outcomes into the curricula of many medical schools, a greater premium is being placed on leadership, research, and other extracurricular pursuits. These activities, as well as the cultivation of social capital, represent a “hidden curriculum” which offers significant benefits to career development that are not often explicitly stated. The hidden curriculum benefits students with generational knowledge of the medical school infrastructure and harms first-generation and/or low-income (FGLI) students, who take longer to integrate into the professional environment and experience more challenges along the way. FGLI students show increased persistence, and they offer diverse perspectives, but poor representation and lack of a clear pathway narrow their entry into several medical specialties, including neurology. As neurologists and educators, we play a role during a critical time of medical student professional development and can help bring the hidden curriculum into the light. Recognition of student backgrounds should guide policies to arm all students with knowledge to make the most of the limited timeframe of medical school. To reduce the lag phase of less enfranchised students, several effective practices can be instituted with minimal modification to existing medical school infrastructure. Efforts to support FGLI students by increasing transparency of the hidden curriculum, formalizing FGLI mentorship groups, and centralizing key information and resources will pay dividends with greater realization of promise and increased diversity and inclusion across more specialties.
Education, then, beyond all other divides of human origin, is a great equalizer of conditions of men—the balance wheel of the social machinery.
—Horace Mann
Introduction
In the United States, the share of the population with a complete college education has grown over the past few decades. Although this has been touted “the great equalizer,” the wealth gap has also continued to widen.1 In some families, a college education is the norm. In others, a new matriculant faces the uncertain pressures of a trailblazer. This dichotomy is particularly apparent in medical school, where parental education is heavily skewed toward graduate education and thus economically privileged backgrounds.2
Fortunately, trends of increased college education in the last decade have precipitated more awareness of the “first-generation” identity. In 2017, the Association of American Medical Colleges (AAMC) introduced the first-generation category into its application, allowing students who are the first in their family to receive a 4 year degree to identify themselves.3 Based on correlation with lower socioeconomic status, the AAMC also recognizes the broader category of “first-generation and/or low-income” or FGLI.4 FGLI status also intersects with race, gender, and sexual orientation, meaning that FGLI students are more likely to have multiple marginalized identities.5 To date, most research has centered on FGLI undergraduates, with little data pertaining to graduate students.6
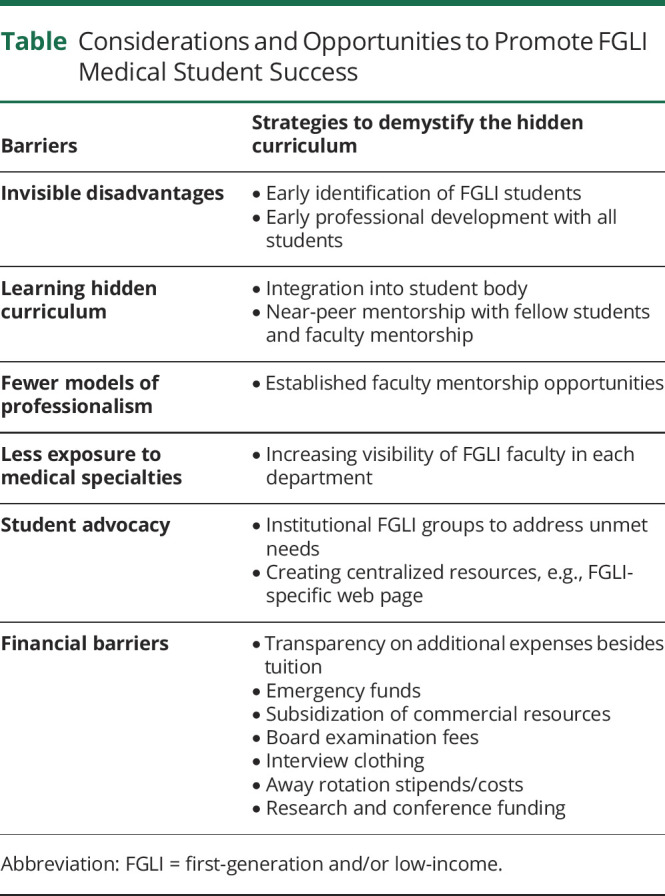
Medical schools have outlines for the competencies and knowledge they expect students to garner. However, there are other skills that must be cultivated to use the full resources of medical school and position oneself for residency. This “hidden curriculum” has previously been defined as the “unspoken or implicit values, behaviors, procedures, and norms that exist in the educational setting.”7 These factors help socialize students into medicine and build their professional identities, and they include but are not limited to fitting into clerkship teams, navigating the hierarchy of medicine, networking with faculty in specialties of interest, obtaining effective letters of recommendation, optimizing clinical/elective scheduling, balancing high-impact extracurriculars and research, seeking awards and leadership positions, and framing residency applications or interviews. These pursuits are not always promoted efficiently or explicitly. They are more readily visible to students with guidance from family that have completed higher education. Furthermore, there are financial barriers that create additional challenges for FGLI students. This commentary will discuss actions that medical schools and faculty can take to serve students of all backgrounds more equitably (Table). These recommendations are particularly relevant to the field of neurology because formal exposure to the field often occurs later in medical school, providing additional time for the advantages of more enfranchised students to accumulate.
Table.
Considerations and Opportunities to Promote FGLI Medical Student Success
Exposure to the Hidden Curriculum Varies Between Medical Students
Medical school is an environment where success begets more success over a finite course of time. Students who know how to make productive use of their time from the onset reap a tremendous and compounding advantage, frequently certified by acceptance into honors societies such as Alpha Omega Alpha or by recognition with school-specific awards. Underrepresented students, including FGLI students, may have less certainty choosing a specialty, less mentorship, and greater feelings of “imposter syndrome.”6 In addition, these students are likely to have increased financial stress, poorer mental health, more difficulty fitting in with their peers, and greater difficulty relating their experiences to friends and family. As such, they often experience more trial and error along the way. Some trials can be wonderfully instructive. Others are simply inefficient.
In medical school, the nonacademic pursuits of the hidden curriculum are required to build a compelling curriculum vitae. The exigency of these pursuits is often not as immediately apparent to FGLI students, who are frequently raised with the mentality that hard work and good grades are the only currency of success.8 In my case, a chance cultural connection before medical school gave me a mentor who introduced me to these additional pursuits. However, without institutional focus on preparing FGLI students, first exposure to the hidden curriculum will remain stochastic.
Early Mentorship Is the Best Way to Illuminate the Hidden Curriculum
Greater institutional acknowledgment and proactive measures are needed to clarify the hidden curriculum in the preclinical and clinical environments. Undergraduate FGLI students have been shown to have more difficulty accessing mentorship and finding research opportunities, which likely extends into medical school.9 The growth in pass/fail curricula may open doors to specialties that historically match or are pursued by fewer underrepresented students.10 However, without strong mentorship relationships, FGLI students may be less likely to consider these careers because of an incomplete sense of each specialty and/or wariness that they would be out of place.11
One of the most effective measures to demystify the path through medical school will be to establish robust peer and faculty mentorship structures for FGLI students at an early time point. At the most basic level, simple awareness of FGLI faculty can lower the activation energy to finding mentorship among less frequently pursued specialties such as neurology. Many neurologists also come from FGLI backgrounds, but this is an invisible identity not evident on faculty profiles. Recognition of FGLI faculty is an important action that departments can take to demonstrate representation, facilitate mentorship, and help recruit students into neurology. Identification as FGLI should be left to the individual discretion of faculty, but many would be eager to provide an approachable shared perspective.
Steps to Establish Mentorship at an Institutional Level
Beyond simple exposure, medical schools should consider a more concerted approach to connect FGLI students with faculty mentors and other support structures. Mentorship can be built into existing educational programs. Because student doctoring groups are some of the earliest experiences of medical school, these programs can be additionally used to pair FGLI students and faculty, providing an avenue for longitudinal and personalized guidance, support, and professional development.
Other steps can be taken to provide mentorship outside of the classroom. In recent years, many medical schools have developed FGLI student groups.3 These groups provide an additional opportunity for mentorship pairings and can help students leverage a multimentorship model. One such initiative is modeled by the STRIVE group at Northwestern, a near-peer program which pairs underrepresented medical students and residents.12 In this structure, the mentor has recently been in the shoes of the mentee, a simple but effective means for closely tailored guidance. Near-peer mentorship can improve student persistence, academic outcomes, and well-being, based on similar interventions in the undergraduate population.13,14
Steps to Connect Students With Additional Support
There are additional steps that institutions can take to improve outcomes for FGLI and underrepresented students beyond the realm of mentorship. Formalized FGLI groups constitute an organized front for student advocacy which can best represent needs that vary over time and with societal factors. For example, shortly after fellow students and I established the First in Family group at Michigan, the coronavirus disease 2019 pandemic began. Thus, our first actions were to conduct a student needs assessment, build an emergency fund, and share food pantry resources. Formalized groups can also keep track of the needs of their constituency and provide an avenue to access medical school leadership to address such concerns.
Many great resources already exist both within and external to medical institutions. The AAMC recently established a website for FGLI students and advisers focusing on professional development, emotional support, and financial support.4 Medical schools frequently have their own materials too. Simply consolidating these resources into a clear central location can dramatically improve the utilization of preexisting infrastructure. Institutions should consider creating FGLI-specific webpages dedicated to highlighting existing resources.
Steps to Address the Financial Component of FGLI Status
Finally, medical schools should examine their financial programs and commit to changes that improve access to the hidden curriculum. For example, many students use external subscription-based resources in their preclinical years. These resources focus on high-yield topics favored by board examinations and are used by students to optimize scores and free up time for nonacademic pursuits. However, the cost of these services can be a barrier.
Medical schools and departments should consider establishing general funds to subsidize or reimburse FGLI students who seek opportunities that present unexpected or prohibitive costs. Some of these costs are mandatory, such as board examination fees, professional dress for clinical elective and interviews, and transportation to clinical sites. These costs add thousands of dollars in unanticipated expenses on top of medical school tuition. Other costs, such as those required for conference attendance, participation in away rotations, or research opportunities, may seem elective and thus disincentive FGLI student participation, but they are key aspects of the medical education. If medical schools are not transparent about these costs and do not consider internal funding opportunities to support these endeavors, it is likely that they will see unequal participation by FGLI students.
Within the neurology community, the American Academy of Neurology offers the Medical Student Diversity Program to support attendance at the national meeting.15 Many institutions offer away rotations for students interested in neurology, with stipends to cover expenses for underrepresented students. Away rotations are not required in neurology, but there are clear efforts underway to support students interested in neurology and increase diversity in the field. These opportunities should be further advertised and highlighted.
Conclusion
Residency programs are currently shifting toward a more holistic review, aiming to identify individuals who can enhance overall cultural competency.10 With the deemphasis of grades, social capital will play an increasing role. Working hard will always matter, but the efficiency of effort is modulated by connections and mentorship. Thus, it will become critically important to provide the script of the hidden curriculum to FGLI and underrepresented students at the earliest possible stages. Medical schools should aim to establish formalized mentorship, support, and resource infrastructure to pursue this goal. Students cannot find what they do not know to seek. As neurologists and educators, we have an opportunity to serve as mentors and advocates for students of all backgrounds because they will be our residents and peers of tomorrow.
Acknowledgment
The authors thank University of Michigan Office of Health Equity and Inclusion for recognizing and including First and Family (FGLI group) as a school sponsored organization.
Appendix. Authors

Study Funding
No targeted funding reported.
Disclosure
The authors report no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
References
- 1.U.S. Census Bureau. Releases New Educational Attainment Data. U.S. Census Bureau; 2020. Accessed November 4, 2022. census.gov/newsroom/press-releases/2020/educational-attainment.html. [Google Scholar]
- 2.Grbic D, Garrison G, Jolly P. Diversity of U.S. Medical School Students by Parental Education. Vol. 9. Analysis in Brief. 2010. Accessed November 4, 2022. aamc.org/media/5871/download. [Google Scholar]
- 3.Romero R, Miotto K, Casillas A, Sanford J. Understanding the experiences of first-generation medical students: implications for a diverse physician workforce. Acad Psychiatry. 2020;44(4):467-470. doi: 10.1007/s40596-020-01235-8. [DOI] [PubMed] [Google Scholar]
- 4.Tools and Resources for First-Generation Medical School Students. AAMC. Accessed November 4, 2022. aamc.org/professional-development/affinity-groups/gea/first-generation-students. [Google Scholar]
- 5.Christophers B, Macedo B, Nieblas-Bedolla E, Marr M, Andersen OS, Boothroyd C. First-generation physician-scientists are under-represented and need better support. Nat Med. 2021;27(5):752-755. doi: 10.1038/s41591-021-01352-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mason HRC, Ata A, Nguyen M, et al. First-generation and continuing-generation college graduates' application, acceptance, and matriculation to U.S. medical schools: a national cohort study. Med Educ Online. 2022;27(1):2010291. doi: 10.1080/10872981.2021.2010291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alsubaje MA. Hidden curriculum as one of current issue of curriculum. J Educ Pract. 2015;6(33):125-128. [Google Scholar]
- 8.Destin M. The double-edged consequences of beliefs about opportunity and economic mobility. Future Child. 2020;30(1):153-164. [Google Scholar]
- 9.Rondini AC. Healing the hidden injuries of class? Redemption narratives, aspirational proxies, and parents of low-income, first-generation college students. Sociological Forum. 2016;31(1):96-116. doi: 10.1111/socf.12228. [DOI] [Google Scholar]
- 10.Youmans QR, Essien UR, Capers Q. A test of diversity-what USMLE pass/fail scoring means for medicine. N Engl J Med. 2020;382(25):2393-2395. doi: 10.1056/NEJMp2004356. [DOI] [PubMed] [Google Scholar]
- 11.Robinson JA, Do-Nguyen CC. Increasing diversity in cardiothoracic surgery: first-generation medical students. JTCVS Open. 2021;7:289-293. doi: 10.1016/j.xjon.2021.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Youmans QR, Adrissi JA, Akhetuamhen A, et al. The STRIVE initiative: a resident-led mentorship framework for underrepresented minority medical students. J Grad Med Educ. 2020;12(1):74-79. doi: 10.4300/jgme-d-19-00461.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Destin M, Castillo C, Meissner L. A field experiment demonstrates near peer mentorship as an effective support for student persistence. Basic Appl Soc Psychol. 2018;40(5):269-278. doi: 10.1080/01973533.2018.1485101. [DOI] [Google Scholar]
- 14.Stephens NM, Hamedani MG, Destin M. Closing the social-class achievement gap: a difference-education intervention improves first-generation students' academic performance and all students' college transition. Psychol Sci. 2014;25(4):943-953. [DOI] [PubMed] [Google Scholar]
- 15.Medical Student Diversity. 2022. Accessed November 23, 2022. aan.com/education/medical-student-diversity. [Google Scholar]


