Abstract
Background
The prevalence of chemsex has been reported by multiple systematic reviews among men who have sex with men (MSM) focussing predominantly on the Global North. An Asian perspective with meta-analytical evidence is missing. This meta-analysis summarised the prevalence of substance use associated with chemsex, and chemsex activity among MSM and MSM sub-populations in Asia, as well as the likelihood for chemsex among MSM living with or without HIV.
Methods
We utilized PubMed, Web of Science and medRxiv to search for literature describing chemsex and its associated substance use among MSM and MSM sub-populations in Asia from January 1, 2010 to November 1, 2021 to conduct three meta-analyses with both frequentist and Bayesian approaches.
Results
We identified 219 studies and included 23 in the meta-analysis. Based on the frequentist models, methamphetamine was the default substance associated with chemsex among MSM in Asia (prevalence=0.16, 95%CI:0.09–0.22), followed by GHB/GBL (prevalence=0.15, 95%CI:0.03–0.27) and ketamine (prevalence=0.08, 95%CI:0.04–0.12), but hardly any cocaine (prevalence=0.01, 95%CI:0.00–0.03). Compared to a general MSM population (prevalence=0.19, 95%CI:0.15–0.23), MSM engaging in transactional sex showed a higher prevalence of chemsex (MSM sex work clients [prevalence=0.28, 95%CI:0.11–0.45]; MSM sex worker [prevalence=0.28, 95%CI:0.17–0.26]). MSM living with HIV also showed higher odds of chemsex activity (OR=3.35, 95%CI:1.57–7.10), compared to MSM living without HIV. Both meta-analytic models converged, indicating robust evidence.
Conclusions
Our meta-analyses showed that chemsex is not uncommon among MSM, and MSM engaging in transactional sex in Asia. We confirmed that MSM living with HIV have a higher likelihood of engaging in chemsex, too. Chemsex prevention and management strategies in Asia should be adjusted accordingly.
Keywords: chemsex, MSM, HIV, substance use, transactional sex, meta-analysis
1. Introduction
Chemsex, referring to the use of specific drugs before or during planned sexual activities to facilitate, initiate, prolong, sustain and intensify the encounter, usually includes using mephedrone, crystal methamphetamine, Gamma hydroxybutyrate/Gamma butyrolactone (GHB/GBL), cocaine and ketamine (Adam Bourne, Reid, Hickson, Torres Rueda, & Weatherburn, 2014; Maxwell, Shahmanesh, & Gafos, 2019), is reported as an emerging public health issue among men who have sex with men (MSM) (Hibbert, Brett, Porcellato, & Hope, 2019; Hibbert, Hillis, Brett, Porcellato, & Hope, 2021; Maxwell et al., 2019). Multiple health risks are associated with chemsex and are summarised in multiple studies and systematic reviews, which included a higher risk of sexual health consequences such as HIV infections and sexual transmitted infections (STIs); higher risk of sexual behaviours such as condomless anal intercourse (CAI), multiple partners and group sex; higher risk of mental health relevant consequences such as depression, anxiety and paranoia; and higher risk of poor general health such as malnutrition and dehydration (Herrijgers et al., 2020; Hibbert et al., 2021; Maxwell et al., 2019; Pichini, Di Trana, Torrens, Scherbaum, & Zaami, 2020; Schreck, Victorri-Vigneau, Guerlais, Laforgue, & Grall-Bronnec, 2021).
Most of the aforementioned evidence stems predominantly from Global North research contexts. To our knowledge, no systematic review on chemsex with a geographic focus on Asia exists. There is one scoping review which focuses on chemsex in Asia with Asian evidence but without peer review yet (Newland & Kelly-Hanku, 2021). This is a glaring reminder of the missing information from an Asian context. Secondly, systematic review data can often be rather unprecise, too. Summarised estimates range from 3% to 29% MSM for chemsex with non-injecting drug use, and from 1% to 50% MSM for chemsex with injecting drug use (based on studies from the Global North (mostly from United States and Western Europe (Maxwell et al., 2019)). Such summaries cannot be regarded as reliable epidemiological estimation and render a need for reliable meta-analytic evidence.
Furthermore, chemsex prevalence varies within the general MSM population. Chemsex activity is frequently observed and reported for specific MSM sub-populations, such as MSM who engage in transactional sex, for example sex workers and their clients (Brooks-Gordon & Ebbitt, 2021). One systematic review has summarized that persons in active use are more likely than persons not in active use to have received money for sex (Tomkins, George, & Kliner, 2019). Also, two systematic reviews have corroborated evidence for the association of chemsex and the HIV status of MSM (Lafortune et al., 2021; Maxwell et al., 2019). For all sub-groups, meta-analytic evidence is still missing in general, and for the Asian context in particular.
To bridge the literature and data gaps of chemsex and substance use associated with chemsex as defined by Maxwell et al. (2019, detailed definition see Section 2.3.1) among MSM, the meta-analyses reported here aim to investigate the prevalence of chemsex associated substances and chemsex activity among MSM, MSM engaging in transactional sex, and to clarify the risk/likelihood of chemsex activity between MSM living with and without HIV, in an Asian context. Also, to account for a biased estimation of the meta-analytic effect in frequentist meta-analytic models with low amounts of studies entered, we also conducted a Bayesian meta-analysis to compare parameters with the aim of improving the informational value of the analysis.
2. Material and methods
2.1. Selection Criteria and Search Strategy
This meta-analysis is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement (Hutton et al., 2015). The PRISMA statement checklist report can be found in the Appendix S1.
We selected relevant studies published between January 1, 2010 and November 1, 2021, by searching PubMed, Web of Science and medRxiv, using terms for chemsex, MSM population and Asian regions. Pertinent keywords and Medical Subject Headings (MeSH) terms related to these categories were used to maximize the output from the literature search (see Appendix S2 for full search terms). We also reviewed the references of included articles and relevant other systematic reviews and meta-analysis to ensure the comprehensiveness of the research presented.
The inclusion criteria for this meta-analysis included the following: 1) Having data on chemsex and any chemsex activities among adults who belong to the MSM population, including MSM in general, MSM sex work clients and MSM sex workers; 2) Having conducted and reported data from an specific Asian country/region (as defined by World Bank regions East Asia Pacific EAP and Japan, www.worldbank.org/en/region/eap); 3) Having published between January 1, 2010 and November 1, 2021 (data collection time must post to January 2010); 4) If possible, data on chemsex activities among MSM population based on HIV status was extracted to compare the chance of chemsex activity between MSM living with/without HIV. However, we did not exclude studies if they did not report HIV status or linked HIV status and chemsex engagement. Studies which 1) were conducted among MSM under 18 years; 2) did not report chemsex or any chemsex substance use; or 3) were case series, case reports, reviews or other systematic reviews/meta-analysis, letters to the editor, opinion pieces, conference abstracts, dissertations/thesis and articles without the outcomes of interest were excluded from the screening process.
2.2. Data Extraction and Quality Assessment
Data extraction and the evaluation of the literature quality were conducted by HW. Mendeley (version 1.19.4) was used to record all available information. The Newcastle-Ottawa Scale for nonrandomised studies was used to assess the methodological quality of the included studies with a cohort study design (Wells et al., 2000).
2.3. Statistical Analysis
2.3.1. Prevalence of chemsex, substance use associated with chemsex among MSM
Similar to the Global North focus of previous meta-analytic evidence, also the definition of chemsex is driven by a Global North perspective. Yet, substance prevalence has been shown to differ by global region (Hunter, Dargan, Benzie, White, & Wood, 2014; Liao et al., 2013; Lim, Akbar, Wickersham, Kamarulzaman, & Altice, 2018; Noor et al., 2021; Schmidt et al., 2016; Wei, Guadamuz, Lim, Huang, & Koe, 2012; White et al., 2014; Zaller et al., 2017) and likewise substance use associated with chemsex differs accordingly. First, we extracted the absolute number of MSM and MSM who had sex under the influence of various substances. We then grouped data by chemsex associated substances, namely cocaine, GHB/GBL, ketamine, mephedrone and methamphetamine, using the classification reported by Maxwell et al. (2019), for publications that did not report chemsex activity as such but listed specific substance use or used different abstract labels for the substance use. The lifetime engagement was collected as the default and the longest available timeframe was collected in case lifetime engagement data is missing. We re-calculated the prevalence of chemsex associated substance use among general MSM through our meta-analysis, instead of extracting the original proportion reported in the included studies.
We then extracted the absolute number of MSM reported by the selected studies for the quantitative synthesis and grouped data by MSM subgroups. This was coded as general MSM (without further information such as engaging in sex work or HIV status), MSM engaging in transactional sex (sex work clients and MSM sex workers). In addition, we conducted meta-analyses to measure the risk/likelihood of chemsex activity among MSM living with HIV. In this analysis, we extracted the absolute number of MSM and those engaged in chemsex in general and grouped data by HIV status (both self-reported and lab-confirmed). We re-calculated the odds ratio (OR) of the chemsex activity between MSM living with HIV and MSM not living with HIV through our meta-analysis, instead of extracting the original OR, relative risks (RR), or hazard ratios (HR) reported in the original studies.
We then extracted the absolute number of MSM engaged in chemsex activities in general, excluding specific substance use information. Due to the heterogenous reporting of chemsex, we coded chemsex activity as a fact, and included the following outcomes: having sex under the influence of new types of drugs, recreational drugs, illicit drugs, substances, chemsex, and sexualised drugs. We collected information on which outcome was included by the selected studies and included in the analysis as a note. Similar to the prevalence for substances associated with chemsex, the lifetime chemsex activities was collected as a default, and the longest timeframe available in the selected studies was collected instead when lifetime engagement information is missing. Lastly, we re-calculated the prevalence of chemsex engagement related to the respective MSM population.
2.3.2. Frequentist and Bayesian meta-analytical approaches
For all three meta-analyses described in section 2.3.1, we used a random-effects model and the DerSimonian-Laird method to estimate the model on proportion (Chemsex activities prevalence among MSM population and chemsex associated substances prevalence among MSM) or on a log-OR scale. The DerSimonian-Laird Q test and I2 values were used to assess heterogeneity, with low, moderate, and high heterogeneity corresponding to I2 values of 25%, 50%, and 75%. In addition, heterogeneity τ was assessed in this study. We investigated a publication bias by inspecting funnel plots. To test the funnel plot asymmetry, we used rank correction test. The Statistical analysis was carried out using R (version R 4.0.4) using the Metafor package v.2.4–0 (Viechtbauer, 2010).
In the analysis of the risk/likelihood of chemsex activity among MSM living with HIV, to better estimate the between-study variance given the limited number of studies to be included in the meta-analysis, we conducted an additional Bayesian random-effects meta-analysis, which allows for all sources of uncertainty and incorporate external evidence on heterogeneity (Rhodes, Turner, & Higgins, 2014). The Bayesian framework introduces a formal combination of a prior probability distribution to obtain a posterior probability distribution of the pooled effect (Rhodes et al., 2014). Choosing an informative prior is necessary to precisely estimate heterogeneity (Rhodes et al., 2014). Following the recommendation of the log-OR endpoints for the simulation (Friede, Röver, Wandel, & Neuenschwander, 2017; Röver, 2017), and the application by Wang and Jonas (2021), we appointed the half-normal distribution with scale 0.5 as a prior for our Bayesian meta-analysis (H. Wang & Jonas, 2021). Results were shown as the posterior distribution of the fixed effect µ on a log-OR scale, heterogeneity τ and posterior knowledge of a “future” observation (prediction distribution). Both estimated fixed effects and random effects with 95% credible interval (CrI) were compared with the estimates from the classical frequentist approach. The Bayesian meta-analysis was carried out by using the Bayesmeta package v.2.6 (Röver, 2017).
3. Results
3.1. Research Selection and Characteristics
The search strategy identified 112 studies after removing duplicates. We excluded 64 studies after screening the titles and abstracts. Forty-eight studies remained for full-text screening, and 25 studies were excluded, leaving 23 studies to be included in the meta-analyses. Figure 1 shows the selection procedure in this study. Quality assessments were summarised in Table 1.
Figure 1.
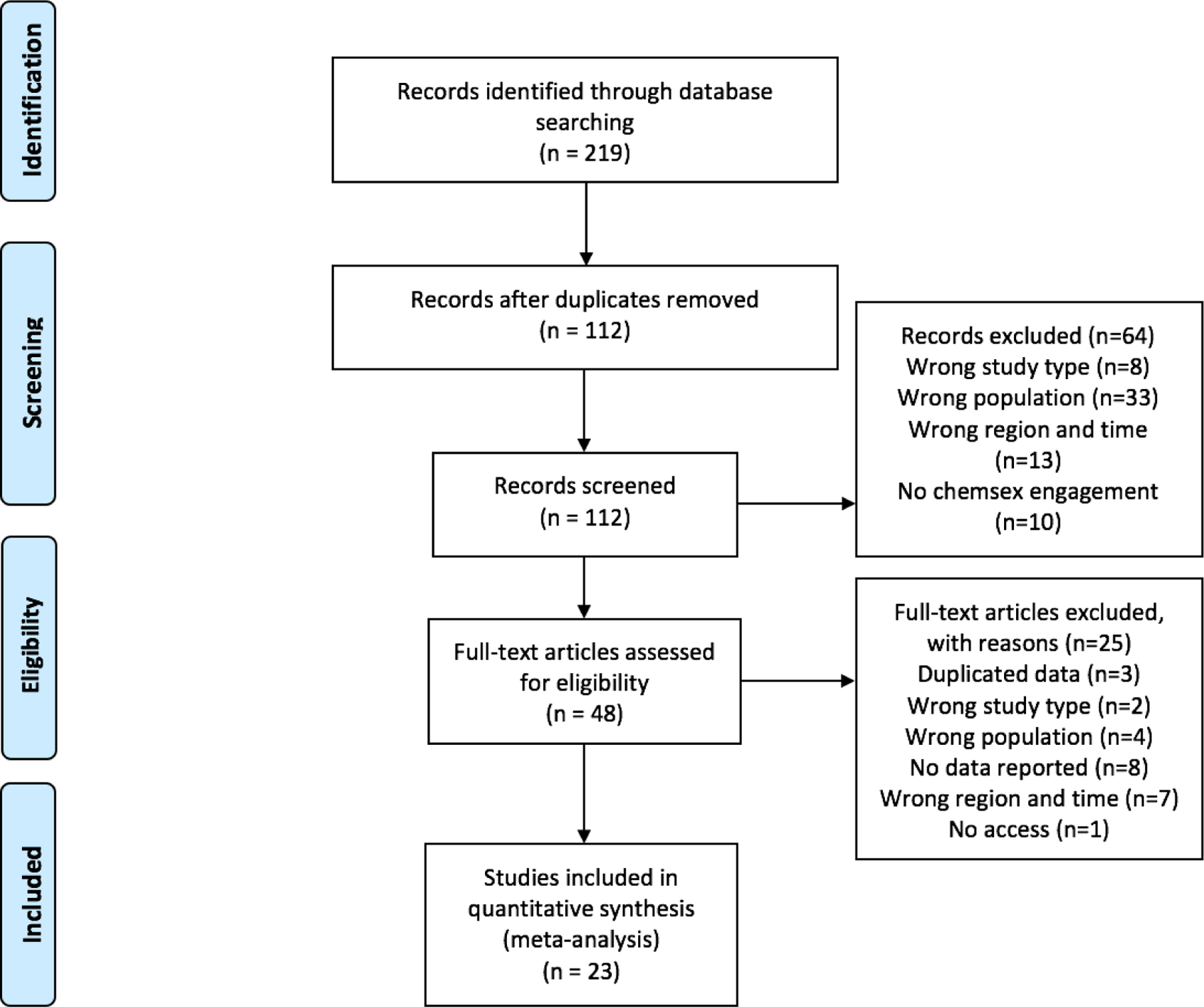
PRISMA Flow diagram of the study selection process.
Table 1.
Newcastle-Ottawa quality assessment of non-randomised studies
| Study, Year | Country/region | Study design | Selection | Comparability | Outcome | Total score | Result |
|---|---|---|---|---|---|---|---|
| (Duong et al., 2018) | Vietnam | Cross-sectional | *** | ** | ** | 7 | Good |
| (Han et al., 2020) | Thailand | Cross-sectional | *** | ** | ** | 7 | Good |
| (He et al., 2018) | China | Cross-sectional | *** | ** | ** | 7 | Good |
| (Hidaka et al., 2014) | Japan | Cross-sectional | *** | ** | ** | 7 | Good |
| (Ko et al., 2012) | Taiwan, China | Cross-sectional | *** | ** | ** | 7 | Good |
| (Lim et al., 2015) | Malaysia | Cross-sectional | *** | ** | ** | 7 | Good |
| (Liu & Detels, 2012) | China | Cross-sectional | *** | ** | ** | 7 | Good |
| (Mao et al., 2021) | China | Cross-sectional | *** | ** | ** | 7 | Good |
| (Nemoto et al., 2012) | Thailand | Cross-sectional | *** | ** | ** | 7 | Good |
| (Nishijima et al., 2013) | Japan | Cross-sectional | *** | ** | ** | 7 | Good |
| (Pattanasin et al., 2016) | Thailand | Cohort study | *** | ** | *** | 8 | Good |
| (Piyaraj et al., 2018) | Thailand | Cohort study | *** | ** | *** | 8 | Good |
| (Sapsirisavat et al., 2016) | Thailand | Cross-sectional | *** | ** | ** | 7 | Good |
| (Sze et al., 2020) | Hong Kong SAR | Cross-sectional | *** | ** | ** | 7 | Good |
| (Tan et al., 2021) | Singapore | Cross-sectional | *** | ** | ** | 7 | Good |
| (N. T. T. Vu et al., 2017) | Vietnam | Cross-sectional | *** | ** | ** | 7 | Good |
| (N. T. Vu et al., 2017) | Vietnam | Cross-sectional | *** | ** | ** | 7 | Good |
| (Z. Wang et al., 2020) | China | Cohort study | *** | ** | ** | 7 | Good |
| (Wansom et al., 2020) | Thailand | Cohort study | ** | ** | ** | 6 | Fair |
| (Wu, Shen, Chiou, Fang, & Lo, 2019) | Taiwan, China | Case-control | *** | ** | *** | 8 | Good |
| (Xu, Qian, et al., 2014) | China | Cross-sectional | *** | ** | ** | 7 | Good |
| (Xu, Zhang, et al., 2014) | China | Cross-sectional | *** | ** | ** | 7 | Good |
| (Yang et al., 2016) | China | Cross-sectional | *** | ** | ** | 7 | Good |
The selection, comparability, and exposure of each study were broadly assessed. Studies with 3 or 4 stars in selection domain AND 1 or 2 stars in comparability domain AND 2 or 3 stars in outcome/exposure domain were considered of good quality; studies with 2 stars in selection domain AND 1 or 2 stars in comparability domain AND 2 or 3 stars in outcome/exposure domain were considered of fair quality; or were considered as poor quality (Wells et al., 2000).
Of the selected studies (four cohort studies, one case-control studies and 18 cross-sectional studies), 14 of them reported chemsex activity among MSM general population, four of them reported chemsex activity among MSM sex work clients, and three of them reported chemsex activity among MSM sex workers. For the chemsex associated substances, six of them reported using cocaine, six of them reported using GHB/GBL, eight of them reported using ketamine, 15 of them reported using methamphetamine and only one of them reported using mephedrone (removed from the subgroup meta-analysis). Only eight of the selected studies reported links between the chemsex activity and HIV status (See Table 2, Table 3, and Table 4 for more detailed study characteristics).
Table 2.
Model summary for chemsex associated substances use among MSM
| Substance | Study | Substance use | Total sample size | Prevalence | Pooled effect (95%CI) | τ | Notes |
|---|---|---|---|---|---|---|---|
| Cocaine | (Ko et al., 2012) | 12 | 1645 | 0.01 (0.00, 0.01) | 0.01 (0.00, 0.03) | 0.01 | In the past 6 months |
| (Lim et al., 2015) | 15 | 1235 | 0.01 (0.01, 0.02) | In the past 6 months | |||
| (Sapsirisavat et al., 2016) | 3 | 499 | 0.01 (0.00, 0.01) | Categorised to rare/regular | |||
| (Sze et al., 2020) | 29 | 569 | 0.05 (0.03, 0.07) | In the past 6 months | |||
| (Z. Wang et al., 2020) | 0 | 88 | 0.01 (0.00, 0.01) | In the past year | |||
| (Yang et al., 2016) | 1 | 205 | 0.00 (0.00, 0.01) | MSMLHIV | |||
|
| |||||||
| GHB/GBL | (Ko et al., 2012) | 33 | 1645 | 0.02 (0.01, 0.03) | 0.15 (0.03, 0.27) | 0.15 | In the past 6 months |
| (Lim et al., 2015) | 34 | 1235 | 0.03 (0.02,0.04) | In the past 6 months | |||
| (Sze et al., 2020) | 200 | 569 | 0.35 (0.31, 0.39) | In the past 6 months | |||
| (Tan et al., 2021) | 27 | 570 | 0.05 (0.03, 0.06) | - | |||
| (Z. Wang et al., 2020) | 29 | 88 | 0.33 (0.23, 0.43) | in the past year | |||
| (Wu et al., 2019) | 10 | 79 | 0.13 (0.05, 0.20) | MSMLHIV | |||
|
| |||||||
| Ketamine | (Ko et al., 2012) | 204 | 1645 | 0.12 (0.11, 0.14) | 0.08 (0.04,0.12) | 0.05 | In the past 6 months |
| (Lim et al., 2015) | 76 | 1235 | 0.06 (0.05, 0.07) | In the past 6 months | |||
| (Nemoto et al., 2012) | 22 | 112 | 0.20 (0.12, 0.27) | Kathoey | |||
| (Sze et al., 2020) | 63 | 569 | 0.11 (0.08, 0.14) | In the past 6 months | |||
| (N. T. Vu et al., 2017) | 8 | 622 | 0.01 (0.00, 0.02) | - | |||
| (Z. Wang et al., 2020) | 2 | 88 | 0.02 (−0.01, 0.05) | In the past year | |||
| (Wu et al., 2019) | 6 | 79 | 0.08 (0.02, 0.13) | MSMLHIV | |||
| (Yang et al., 2016) | 12 | 205 | 0.06 (0.03, 0.09) | MSMLHIV | |||
|
| |||||||
| Methamphet amine | (Duong et al., 2018) | 15 | 45 | 0.33 (0.20, 0.47) | 0.16 (0.09, 0.22) | 0.13 | - |
| (Han et al., 2020) | 16 | 48 | 0.33 (0.20, 0.47) | MSMLHIV | |||
| (Hidaka et al., 2014) | 211 | 5731 | 0.04 (0.03, 0.04) | - | |||
| (Ko et al., 2012) | 25 | 1645 | 0.02 (0.01, 0.02) | In the past 6 months | |||
| (Lim et al., 2015) | 87 | 1235 | 0.07 (0.06, 0.08) | In the past 6 months | |||
| (Nishijima et al., 2013) | 57 | 973 | 0.06 (0.04, 0.07) | History of illicit drug use among HIV positive samples | |||
| (Piyaraj et al., 2018) | 128 | 1372 | 0.09 (0.08, 0.11) | - | |||
| (Sapsirisavat et al., 2016) | 18 | 499 | 0.04 (0.02, 0.05) | Categorised to rare/regular | |||
| (Sze et al., 2020) | 222 | 569 | 0.39 (0.35, 0.43) | In the past 6 months | |||
| (Tan et al., 2021) | 27 | 570 | 0.05 (0.03, 0.06) | - | |||
| (N. T. Vu et al., 2017; N. T. T. Vu et al., 2017) | 89 | 622 | 0.14 (0.12, 0.17) | - | |||
| (Z. Wang et al., 2020) | 32 | 88 | 0.36 (0.26, 0.46) | In the past year | |||
| (Wansom et al., 2020) | 98 | 563 | 0.17 (0.14, 0.21) | MSMLHIV | |||
| (Wu et al., 2019) | 21 | 79 | 0.27 (0.17, 0,36) | MSMLHIV | |||
| (Yang et al., 2016) | 26 | 205 | 0.13 (0.08, 0.17) | MSMLHIV | |||
Notes: - refers to information not applicable. 95% CI = 95% confident interval. MSMLHIV = men have sex with men living with HIV. The scale on the effects is prevalence.
Table 3.
Model summary for chemsex activity among MSM population
| Subgroup | Study, Year | Chemsex activity | Total sample size | Prevalence | Pooled effect (95% CI) | τ | Notes |
|---|---|---|---|---|---|---|---|
| MSM general | (He et al., 2018) | 101 | 555 | 0.18 (0.15, 0.21) | 0.19 (0.15, 0.23) | 0.08 | New types drugs |
| (Ko et al., 2012) | 264 | 1645 | 0.16 (0.14, 0.18) | Recreational drugs within 6 months | |||
| Lim et al., 2015) | 169 | 1235 | 0.14 (0.12, 0.16) | Recreational drugs within 6 month | |||
| (Liu & Detels, 2012) | 83 | 418 | 0.20 (0.16, 0.24) | Recreational drugs | |||
| (Mao et al., 2021) | 275 | 4496 | 0.06 (0.05, 0.19) | Recreational drugs | |||
| (Nishijima et al., 2013) | 392 | 973 | 0.40 (0.37, 0.43) | History of illicit drug use among HIV positive samples | |||
| (Pattanasin et al., 2016) | 299 | 1744 | 0.17 (0.15, 0.19) | Recreational drugs | |||
| (Sapsirisavat et al.,2016) | 53 | 499 | 0.11 (0.08, 0.13) | Use of substance in the past 3 months | |||
| (Sze et al., 2020) | 356 | 2687 | 0.13 (0.12, 0.15) | Chemsex | |||
| (N. T. T. Vu et al., 2017) | 98 | 622 | 0.16 (0.13, 0.19) | Recent ATS use before or during sex | |||
| (Z. Wang et al., 2020) | 116 | 600 | 0.19 (0.16, 0.22) | Sexualised drug use in lifetime | |||
| (Wu et al., 2019) | 21 | 79 | 0.27 (0.17, 0.36) | MSMLHIV | |||
| (Xu, Qian, et al., 2014) | 145 | 625 | 0.23 (0.20, 0.27) | Recreational drugs | |||
| (Xu, Zhang, et al., 2014) | 1072 | 3830 | 0.28 (0.27, 0.29) | Recreational drugs | |||
|
| |||||||
| MSM sex work clients | (Mao et al., 2021) | 201 | 459 | 0.44 (0.39, 0.48) | 0.28 (0.11, 0.45) | 0.17 | Recreational drugs |
| (Nemoto et al., 2012) | 48 | 112 | 0.43 (0.34, 0.52) | Having sex under the influence of substances in the past six months | |||
| (Piyaraj et al., 2018) | 27 | 239 | 0.11 (0.07, 0.15) | Methamphetamine only | |||
| (Sze et al., 2020) | 72 | 492 | 0.15 (0.12, 0.18) | Chemsex | |||
|
| |||||||
| MSM sex workers | (Sze et al., 2020) | 60 | 373 | 0.16 (0.12, 0.20) | 0.28 (0.17, 0.26) | 0.12 | Chemsex |
| (Xu, Qian, et al., 2014) | 6 | 20 | 0.30 (0.10, 0.50) | Recreational drugs | |||
| (Yang et al., 2016) | 80 | 205 | 0.39 (0.13, 0.43) | Used drugs in the past 3 months | |||
Notes: MSM general refer to MSM without further information in transactional sex. 95% CI = 95% confident interval. MSMLHIV = men have sex with men living with HIV. The scale on the effects is prevalence.
Table 4.
Model summary for the risk/likelihood of chemsex activity among MSM living with HIV
| HIV negative |
HIV positive |
Frequentist approach |
Bayesian approach with half normal distribution prior† |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Year | Chemsex activity | Total Sample size | Chemsex activity | Total Sample size | Log Odds ratio (95%CI) | Pooled effect 95% CI) | τ | Fixed effect (95% CrI) | Random effect τ (95%CrI) | Predictive distribution (95% CrI) |
| (He et al., 2018) | 2018 | 85 | 473 | 16 | 82 | 0.10 (−0.49, 0.70) | 1.21 (0.45, 1.96) | 1.04 | 1.22 (0.52, 1.90) | 0.90 (0.57, 1.31) | 1.22 (−0.79, 3.21) |
| (Liu & Detels, 2012) | 2012 | 80 | 404 | 3 | 14 | 0.10 (−1.20, 1.40) | |||||
| (Mao et al., 2021) | 2021 | 113 | 4052 | 162 | 444 | 3.00 (2.73, 3.27) | |||||
| (Pattanasin et al., 2016) | 2016 | 215 | 1372 | 84 | 372 | 0.45 (0.17, 0.73) | |||||
| (Sapsirisavat et al., 2016) | 2016 | 38 | 387 | 15 | 112 | 0.35 (−0.29, 0.99) | |||||
| (Sze et al., 2020) | 2020 | 278 | 2514 | 78 | 173 | 1.89 (1.56, 2.21) | |||||
| (Xu, Qian, et al., 2014) | 2014 | 116 | 565 | 29 | 60 | 1.29 (0.74, 1.83) | |||||
| (Xu, Zhang, et al., 2014) | 2014 | 229 | 3476 | 125 | 354 | 2.05 (1.79, 2.30) | |||||
Half-normal distributions with scale 0.5. 95% CI = 95% confident interval. 95% CrI = 95% credible interval. The scale on the effects is log odds ratio.
3.2. Chemsex associated substance use prevalence among MSM
Four chemsex associated substances (cocaine, GHB/GBL, ketamine and methamphetamine) were grouped for the meta-analysis, with the exclusion of mephedrone (only one selected study reported mephedrone use (Z. Wang et al., 2020)). Figure 2 presents the pooled prevalence of these chemsex associated substance prevalence among MSM. Among the substances associated with chemsex, methamphetamine has the highest estimated pooled prevalence (pooled prevalence=0.16, 95%CI 0.09–0.22, τ=0.13, I2=99.66%), following by GHB/GBL (pooled prevalence=0.15, 95%CI 0.03–0.12, τ=0.15, I2=99.73%) and ketamine (pooled prevalence=0.08, 95%CI 0.04–0.22, τ=0.05, I2=96.29%). Cocaine use was estimated with a very small pooled proportion of 0.01 (95%CI 0.00–0.03, τ=0.17, I2=98.30%).
Figure 2. Forest plot of the chemsex associated substances prevalence among MSM with classic frequentist approach.
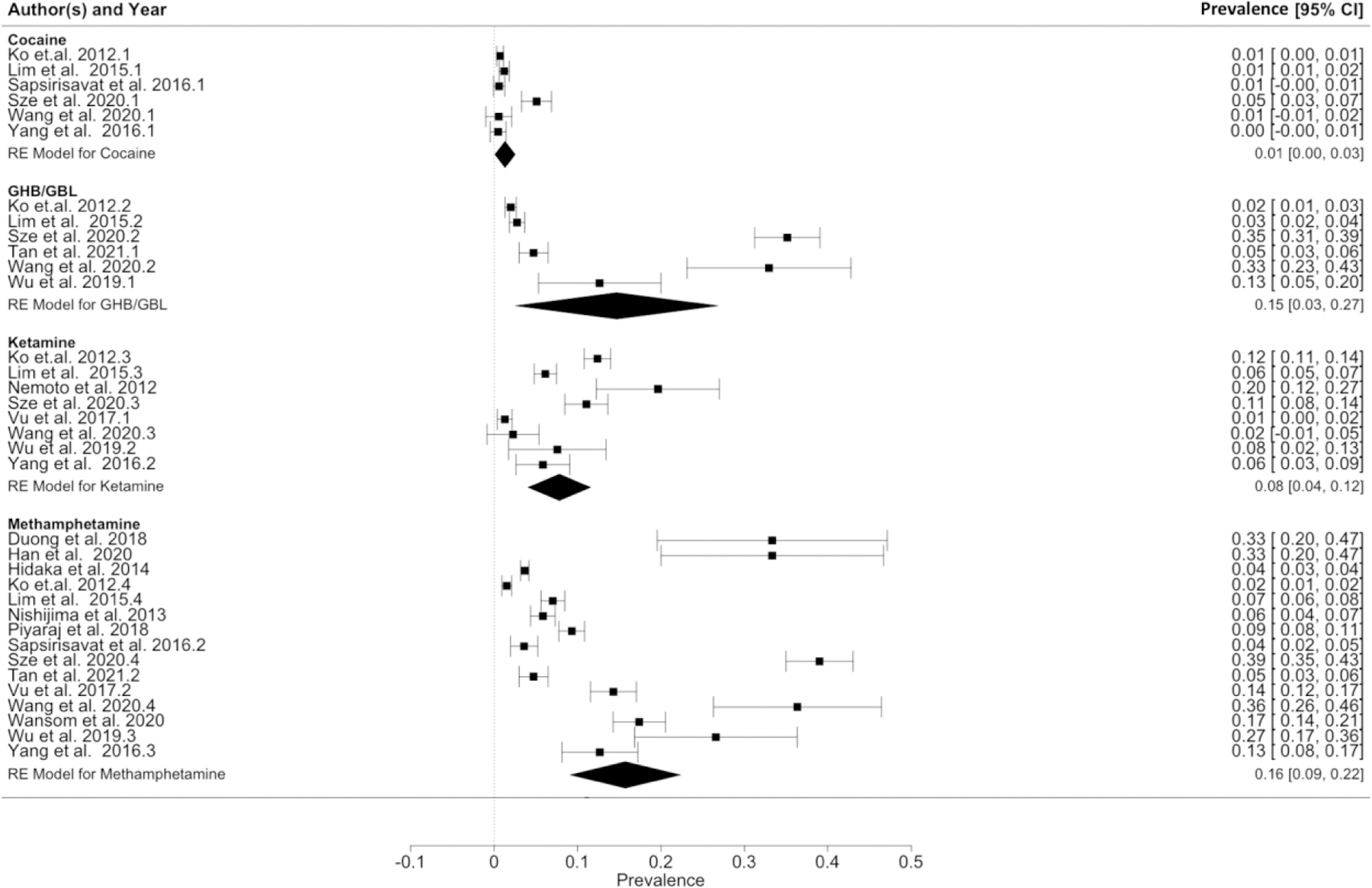
Note. Cocaine: Heterogeneity: Q=24.04, df=5, p=0.0002, I2=93.16%; GHB/GBL: Heterogeneity: Q=312.29, df=5, p<0.0001, I2=99.73%; Ketamine: Heterogeneity: Q=193.84, df=7, p<0.0001, I2=96.29%; Methamphetamine: Heterogeneity: Q=665.30, df=14, p<0.0001, I2=99.66%. 95%CI=95% confident interval.
3.3. Chemsex activity prevalence among different MSM population
Our meta-analysis estimated the pooled prevalence for chemsex activity among MSM general population as 0.19 (95% confidence interval [CI] 0.15–0.23, τ=0.08, I2=98.70%, Table 3, Figure 3). The pooled prevalence for chemsex activity among MSM sex work clients was higher than in the MSM general population (pooled prevalence=0.28, 95%CI 0.11–0.45, τ=0.17, I2=98.30%, Table 3, Figure 3). The pooled prevalence for chemsex activity for MSM sex workers is as same as for the MSM sex work clients, but with a narrower 95%CI (pooled prevalence=0.28, 95%CI 0.13–0.43, τ=0.12, I2=91.85%, Table 3, Figure 3).
Figure 3. Forest plot of the chemsex activity prevalence among different MSM population with classic frequentist approach.
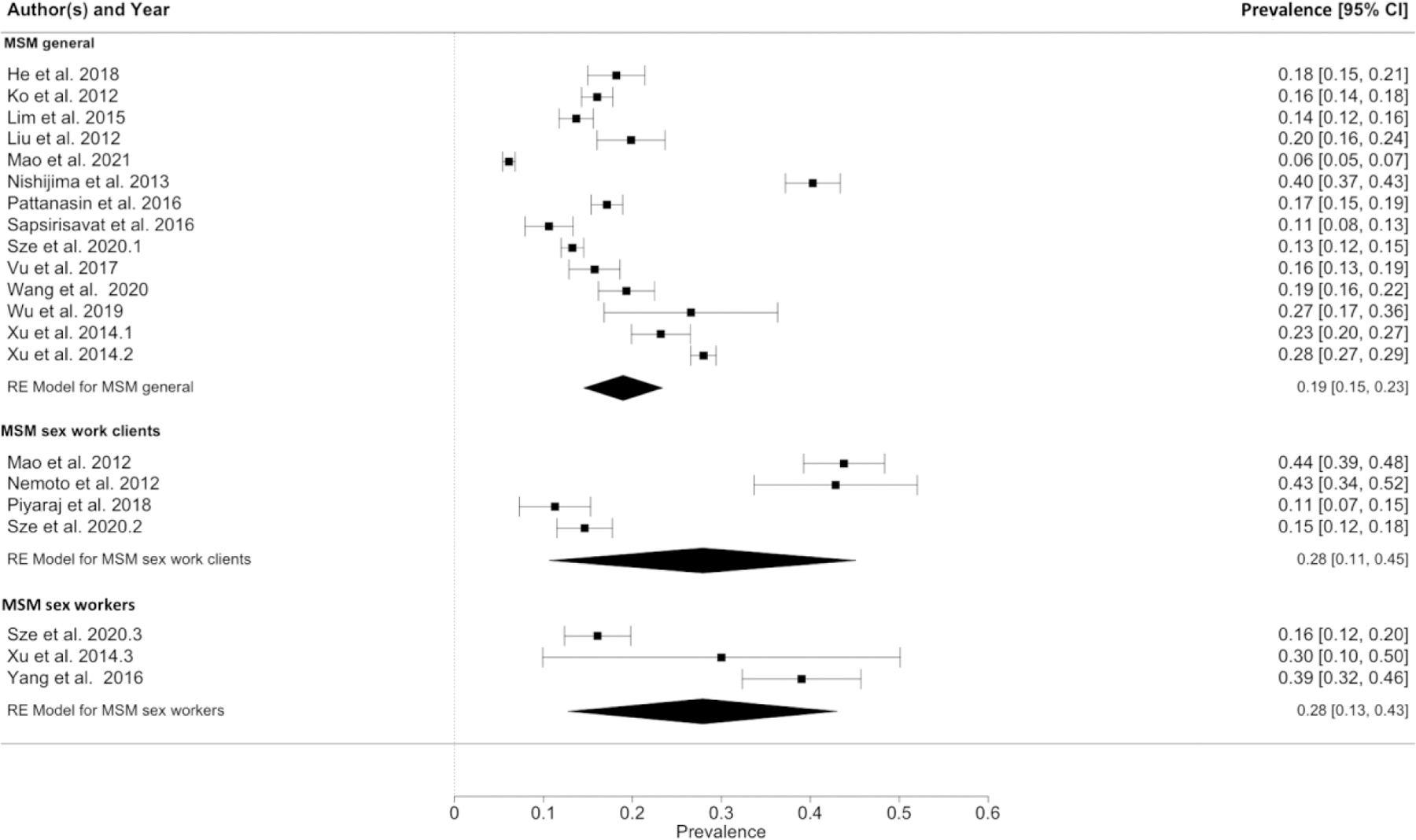
Note. MSM general: Heterogeneity: Q=1218.51, df=13, p<0.0001, I2=98.70%; MSM sex work clients: Heterogeneity: Q=156.91, df=3, p<0.0001, I2=98.30%; MSM sex workers: Heterogeneity: Q=35.22, df=2, p<0.0001, I2=91.58%. 95%CI=95% confident interval.
3.4. The risk/likelihood of chemsex activity among MSM living with HIV
3.4.1. Frequentist meta-analytical approach
Compared to MSM living without HIV, the pooled odds estimate for MSM living with HIV engaging in chemsex activity was higher when computed with the classical frequentist approach (OR=3.35, 95%CI= 1.57–7.10, τ=1.04, I2=96.68%, Figure 4).
Figure 4. Forest plot of the association of MSM living with HIV in comparison to MSM living without HIV in chemsex activity computed with classic frequentist approach.
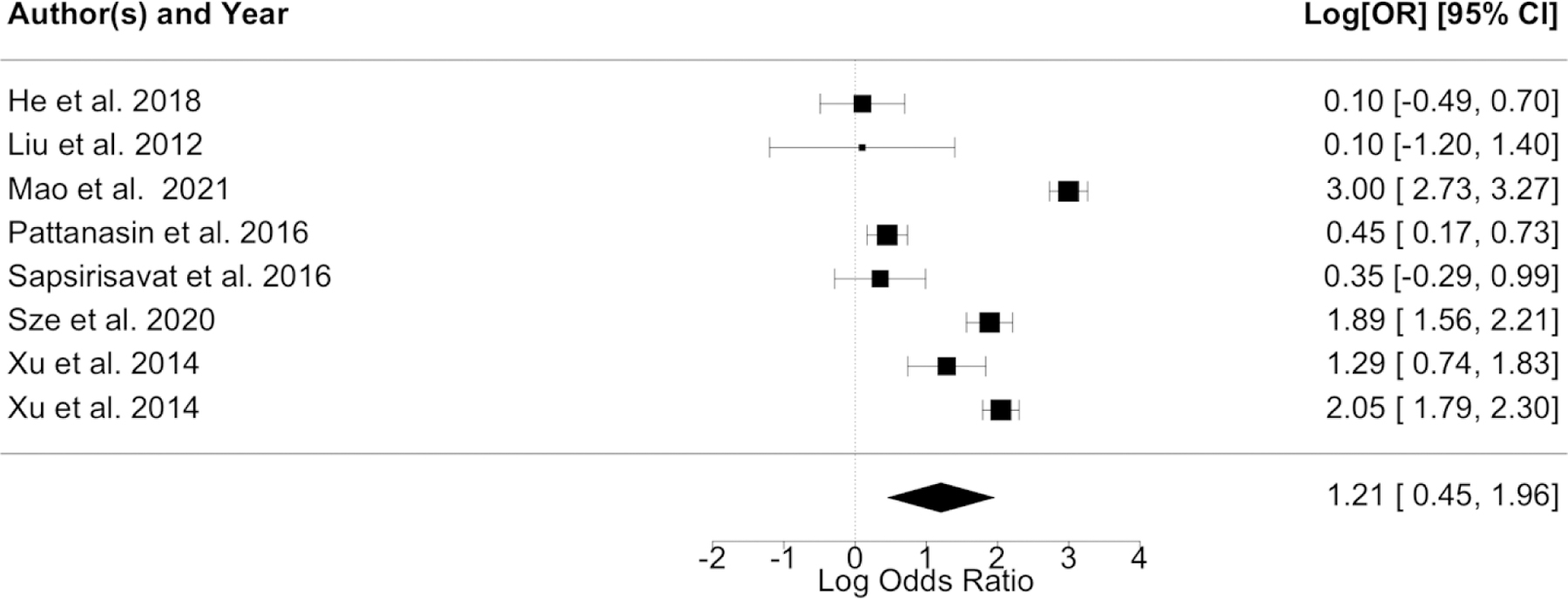
Note. Heterogeneity: Q=225.31, df=7, p<0.0001, I2=96.68%. 95%CI=95% confident interval.
3.4.2. Bayesian random-effects meta-analytical approach
A similar but slightly larger fixed effect of MSM living with HIV compared to MSM living without HIV was estimated by the Bayesian approach with an OR of 3.39 (95%CrI 1.68–6.69, Figure 5). The random effect τ was estimated at 0.90 (95%CrI 0.57–1.31). The prediction of the likelihood was estimated at a similar value of 3.39 but with a statistically insignificant prediction distribution (95%CrI 0.45–24.78). All comparisons between the two approaches are summarised in Table 4. Detailed information for the posterior distributions can be found in Appendix S4.
Figure 5. Forest plot of the association of MSM living with HIV in comparison to MSM living without HIV in chemsex activity computed with Bayesian approach with half normal distribution prior (scale of 0.5).
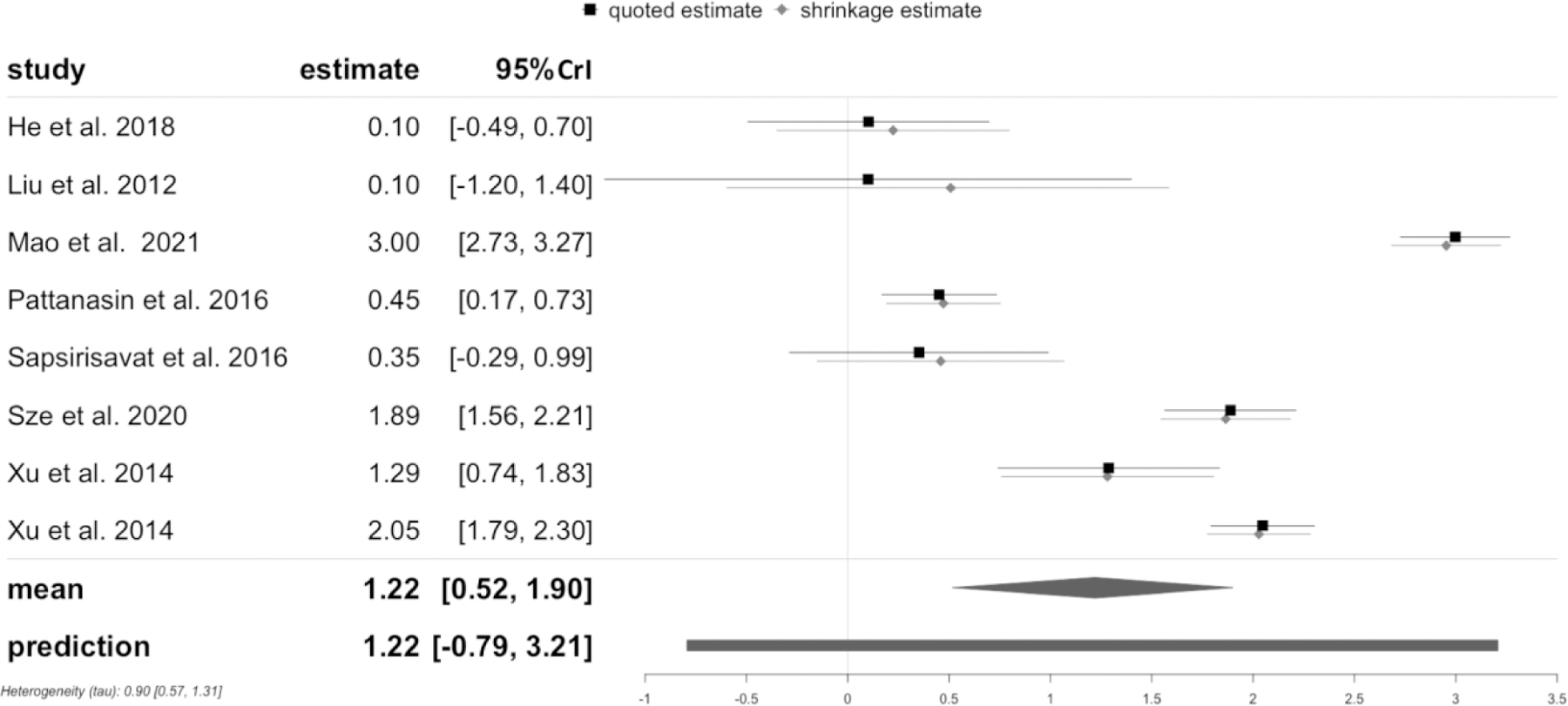
Note. 95% CrI = 95% credible interval. The black line indicates the quoted estimates specified through effect from individual study and its σi as same as in the frequentist approach. The grey line presents the shrinkage intervals which illustrate the posterior of each studyʼs true effect. The black diamond presents the posterior distribution of the pooled effect while the black bar shows the prediction distribution. The scale on the x-axis is log odds ratio.
3.5. Publication bias
There was no evidence of a publication bias for all meta-analyses in this study based on the funnel plots and the rank correction test. The publication bias assessment can be found in Appendix S3.
4. Discussion
To our knowledge, this is the first study to investigate the prevalence of chemsex and chemsex associated substances among MSM and different MSM sub-populations, together with the likelihood of chemsex activity in Asian region with meta-analytical evidence. Additionally, we applied a Bayesian meta-analysis to explore the influence from between-studies variance on the pooled results when the number of primary data available is limited following the suggestion from Wang and Jonas (2021) to increase the robustness of the estimates (H. Wang & Jonas, 2021). This meta-analysis of 23 studies showed a differential prevalence by chemsex related substances in Asia. While crystal methamphetamine is the most prevalent, cocaine is the least. GHB/GBL and ketamine showed more variability. Furthermore, this meta-analysis not only revealed a high prevalence of chemsex and chemsex associated substance use among MSM, especially those who engage transactional sex (both sex workers and clients) in Asia, but also summarised evidence that MSM living with HIV had a higher risk, respectively likelihood, to engage in chemsex compared to MSM living without HIV. These findings were confirmed by both meta-analytical approaches.
4.1. Chemsex associated substance use among MSM in Asia
Our pooled prevalence findings on the substances associated with chemsex revealed very little cocaine use among MSM in Asian contexts from 2010 onwards. This finding corroborated the findings from Wei et al. (2012) of 1.8% prevalence, using data from Asian Internet MSM Sex Survey 2010 (AIMSS-2010) for the Asian region (Wei et al., 2012), and is much lower than the reported cocaine use as a chemsex associated substance usually found in other regions (Hunter et al., 2014; Noor et al., 2021; Schmidt et al., 2016; White et al., 2014; Zaller et al., 2017). Within our expectations, methamphetamine is the chemsex associated substance of choice among MSM in Asia. This finding corroborated Asia-specific studies (Liao et al., 2013; Lim et al., 2018; Wei et al., 2012), but is different from the report from Amsterdam where GHB/GBL is the most common substance among MSM (Drückler, van Rooijen, & de Vries, 2018). However, our pooled estimate is much higher than the findings from Wei et al. (2012) of 4.0% prevalence based AIMSS-2010 data and similar but slightly lower than the estimation from Europe (Schmidt et al., 2016). This may suggest an increase of methamphetamine use in the Asian setting, however, evidence from a longitudinal cohort study is needed to confirm this assumption. Following methamphetamine, GHB/GBL and ketamine were used as frequently as well. Both substances were estimated with a higher pooled prevalence among MSM than the reported estimates from Wei et al. (2012), but much lower than the estimates from the European context (Drückler et al., 2018; Schmidt et al., 2016; Wei et al., 2012). However, the large variabilities for these two substances based on the included studies in our meta-analytical analysis should not be ignored (Table 2, Figure 2). More comprehensive data is thus needed in terms of accuracy. Furthermore, the fact that only one selected study reported mephedrone use can be interpreted that mephedrone, as a substance usually associated with chemsex in other regions, is yet to be emergent in Asia. This substance should be monitored, given that existing reports have confirmed the popularity of mephedrone among MSM elsewhere (Drückler et al., 2018; Schmidt et al., 2016). Our meta-analytic findings showed that substances associated with chemsex, especially methamphetamine, are not uncommon among MSM in Asia. Even though this use is less prevalent than in the Global North, attention, public health implications, and harm reduction interventions should be given to MSM populations in Asia to prevent additional harms due to the use of these substances for sexualized purposes.
4.2. Chemsex among different MSM sub-populations
Chemsex among the general MSM population is not uncommon in Asia. According to our meta-analysis, one in five MSM ever engaged in the chemsex. However, an even higher prevalence was found in the context of sex work, for both clients and sex workers. Almost three in ten MSM engaging in transactional sex ever participated in chemsex. Our findings on MSM sex workers is comparable, but slightly lower to the Western setting, such as Amsterdam (Peters, Evers, Dukers-Muijrers, & Hoebe, 2020). Reasons for the higher prevalence of chemsex activity among MSM sex workers maybe the sense of “being control” and “making work easier” during the sex work (Brooks-Gordon & Ebbitt, 2021; Druckler et al., 2021), to be able to have transactional sex, or sex with the same gender in case of an own heterosexual orientation (Druckler et al., 2021), or to buffer sexual violence and discrimination shown by their clients (Wirtz, Peryshkina, Mogilniy, Beyrer, & Decker, 2015). Our meta-analytical evidence from Asia, again, stresses the needs for a regional and national public health approach for chemsex among MSM, especially for those who engaging in transactional sex such as MSM sex workers. In addition, in Asia, MSM sex workers often experience a greater distance to healthcare providers and counselling resources as they are also (illegal) migrants and may not have access to national health care programs (Guadamuz, Clatts, & Goldsamt, 2018). This should be taken into account for future investigations and interventions.
In addition, both of our frequentist and Bayesian meta-analysis confirmed the higher risk/likelihood of chemsex among MSM living with HIV compared to those who live without HIV, taking the limited data available into account. Even though in our Bayesian prediction model this higher likelihood is not statistically significant for the future estimate, the posterior estimation reflects a solid argument. Our findings are consistent with literature from Global North contexts (Colfax et al., 2005; Edmundson et al., 2018; Plankey et al., 2007), and Asia (Wei et al., 2012). While a systematic review also reported this association but with inconclusive findings (Maxwell et al., 2019), our study confirmed it with meta-analytical evidence. Given the established higher risk of acquiring HIV among MSM engaged in chemsex due to paying less attention on the health status with their partners (Kwan & Lee, 2019), we cannot point to the direction of the causal relationship between chemsex activity and HIV status in this meta-analysis. Qualitative studies and further causal relationship analysis are needed to reflect on this association. We seek to stress that MSM living with HIV should receive additional attention in terms of harm reduction.
4.3. Regional differences in Chemsex reporting and definition
We need to acknowledge that the definition of chemsex in our study is not as concise as one would like it to be due to the differences in definitions across the world, and the heterogenous terminologies used in publications from Asia. This heterogenous terminology use may also be influenced by local legal boundaries. We are aware that there are other commonly used definitions of chemsex different than the one we applied in our meta-analysis, such as by Bourne at al. (2015), which did not include ketamine and cocaine (A. Bourne, Reid, Hickson, Torres-Rueda, & Weatherburn, 2015), and Stuart (2013), which also included the injection drug use (Stuart, 2013). We chose to use both a labelling and substance based approach to be able to including articles that did not use a chemsex terminology but reported own terminologies but refer to similar substances. Other terminologies of chemsex in the selected studies are for example: recreational drugs (Ko et al., 2012; Lim et al., 2015; Liu & Detels, 2012; Mao et al., 2021; Pattanasin et al., 2016; Xu, Qian, et al., 2014; Xu, Zhang, et al., 2014), sexualised drugs (Z. Wang, Mo, Ip, Fang, & Lau, 2020), new type of drugs (He et al., 2018), illicit drugs for sexualised use (Nishijima et al., 2013) and substances for sexualised use (Nemoto et al., 2012; Sapsirisavat et al., 2016; Yang et al., 2016). The included studies using these terminologies thus do not always strictly follow the definition of chemsex we applied (Maxwell et al., 2019), and resulted in the inclusion of other substances, such as heroin, marijuana or ecstasy. The extracted number of substance use in our study would thus be higher and compared to following a stricter definition, in turn, our pooled prevalence would be overestimated. The slightly lower methamphetamine pooled prevalence among MSM may reflect this overestimation.
Furthermore, our data showed great variability between the substances which attests to the dynamic of substances used for chemsex. Novel substances, especially of the cathinone subtype are constantly being developed and pushed onto the market. Substances such as α-Pyrrolidinohexiophenone (α-php) need to be monitored in the future, as they make their entry on the chemsex circuit (Lagoutte-Renosi et al., 2021; Pieprzyca, Skowronek, Nižnanský, & Czekaj, 2020). We thus recommend that an Asian regional and global concise classification of chemsex should be developed and applied in the future to accelerate international cooperation and efforts of chemsex management and prevention.
4.4. Application of Bayesian meta-analysis
Following the recommendation by previous studies of applying Bayesian meta-analysis in the context of heterogenous data (Gronau et al., 2017; H. Wang & Jonas, 2021), we applied the Bayesian meta-analytical approach in this study, due to the limited number of the included studies and their heterogenous setting. With the consistent estimations by both frequentist and Bayesian approaches, we consider our findings on the risk/likelihood of chemsex activity among MSM living with/without HIV as solid and providing good evidence. Compared to the frequentist meta-analysis, our Bayesian estimates generated estimates with a narrower 95% credible interval and a smaller and more concise heterogeneity τ. We thus believe our estimates from the Bayesian meta-analysis to be more robust and closer to the true likelihood in reality. We, again, proved the feasibility and applicability of Bayesian meta-analytical approach in the field of HIV and substance use. Future synthesis studies in the field of substance and HIV, therefore, should not postpone the meta-analytic investigation due to the limited availability of studies, but should instead apply this approach for more robust estimates.
4.5. Study strengths and limitations
Our review has several strengths and limitations. The major strength being the specific focus on chemsex among MSM in Asia. To our knowledge, no systematic review of chemsex activity among MSM has a focus or sub-theme in the Asian region, and no meta-analytical evidence has been published for chemsex activity among MSM and the MSM sub-populations. Findings from our study can close this gap and can provide regional epidemiological information to public health authorities, non-governmental and community organizations in Asia. As the first regional meta-analysis of chemsex activity, we believe our methodology can be directly applied in other regions, too. Future studies should thus focus on other regions to provide a more comprehensive global picture of chemsex among MSM. The application of both the comparative frequentist and Bayesian meta-analysis approaches can be considered as another major strength. With the consistent estimated fixed effect, results from our meta-analysis can thus better inform subsequent decision making on chemsex harm reduction, and HIV prevention and management.
Other than the discussed methodological limitation in section 4.3, one major limitation in our review is the limited data from cohort studies. The majority of the included studies had a cross-sectional study design and only four of 23 studies had a cohort study design (Pattanasin et al., 2016; Piyaraj et al., 2018; Z. Wang et al., 2020; Wansom et al., 2020). As a result, a collection bias is possible in our included studies and could have biased our pooled estimates. We thus stress a need for conducting more cohort studies with a focus on chemsex, and we call for more cohort studies in Asia in particular in the future. In addition, one major limitation in our study can be the different time periods for chemsex and chemsex associated substance we exacted, as the included both lifetime activity and recent activity (three to six month prior). Given the lifetime prevalence can be higher than the recent prevalence, our pooled results can actually be underestimated. Another limitation in our study is the lack of other subgroups of MSM, such as MSM injecting drug users, heterosexual populations, female sex workers, or transgender individuals, and all of their intersectional interactions. There is already some evidence that members of these populations have been engaging in chemsex (Fan et al., 2021; Lawn, Aldridge, Xia, & Winstock, 2019; Xiong, Ong, Wang, Tang, & Wang, 2021). Based on our meta-analytical findings thus we cannot draw any conclusions on these populations. Future studies should thus focus on these populations, too. In sum, more detailed primary data reporting has the potential to improve the quality of future research syntheses and would allow to draw even more robust conclusions.
5. Conclusions
In conclusion, chemsex and chemsex associated substances are not uncommon among MSM in Asia. Crystal methamphetamine is the most prevalent substance, cocaine the least. Developments for ketamine and GHB/GBL should be monitored, there is insufficient data to estimate the prevalence of mephedrone. Higher prevalence of chemsex activity were found among MSM who engaged in transactional sex compared to the general MSM population. MSM living with HIV had an increased likelihood of engaging in chemsex events compared to MSM living without HIV. Healthcare providers, activists and substance management authorities should be aware of these characteristics in terms of improving preventive and harm reduction interventions. Chemsex classification, especially related to the inclusion of substances, should be further harmonised and regionally appropriately defined in the future.
Supplementary Material
Highlights.
This is the first meta-analysis of chemsex use among MSM in Asia.
Chemsex is not uncommon in Asia among MSMPLHIV, and MSM engaged in transactional sex.
Crystal meth is the most common substance, cocaine the least.
A regionally appropriate definition of chemsex should be developed.
More cohort studies on chemsex among MSM in Asia are warranted.
Funding:
This research project is supported by Mahidol University.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bourne A, Reid D, Hickson F, Torres Rueda S, & Weatherburn P (2014). The Chemsex study: drug use in sexual settings among gay and bisexual men in Lambeth, Southwark and Lewisham
- Bourne A, Reid D, Hickson F, Torres-Rueda S, & Weatherburn P (2015). Illicit drug use in sexual settings (‘chemsex’) and HIV/STI transmission risk behaviour among gay men in South London: findings from a qualitative study. Sex Transm Infect, 91(8), 564–568. doi: 10.1136/sextrans-2015-052052 [DOI] [PubMed] [Google Scholar]
- Brooks-Gordon B, & Ebbitt E (2021). The Chemsex ʻConsent Ladderʼ in Male Sex Work: Perspectives of Health Providers on Derailment and Empowerment. Social Sciences, 10, 69. doi: 10.3390/socsci10020069 [DOI] [Google Scholar]
- Colfax G, Coates TJ, Husnik MJ, Huang Y, Buchbinder S, Koblin B, … Vittinghoff E (2005). Longitudinal patterns of methamphetamine, popper (amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of San Francisco men who have sex with men. Journal of urban health, 82(1), i62–i70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drückler S, van Rooijen MS, & de Vries HJ (2018). Chemsex among men who have sex with men: a sexualized drug use survey among clients of the sexually transmitted infection outpatient clinic and users of a gay dating app in Amsterdam, the Netherlands. Sexually transmitted diseases, 45(5), 325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Druckler S, Zimmermann H, Eekman S, van Rooijen M, Davidovich U, de Vries H, & Heijman T (2021). P145 A qualitative study on sexualised drug use among male and transgender women sex workers in Amsterdam, the Netherlands. Sexually Transmitted Infections, 97(Suppl 1), A97. doi: 10.1136/sextrans-2021-sti.254 [DOI] [Google Scholar]
- Duong HT, Jarlais DD, Khuat OHT, Arasteh K, Feelemyer J, Khue PM, … Nagot, N. (2018). Risk Behaviors for HIV and HCV Infection Among People Who Inject Drugs in Hai Phong, Viet Nam, 2014. AIDS and behavior, 22(7), 2161–2171. doi: 10.1007/s10461-017-1814-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edmundson C, Heinsbroek E, Glass R, Hope V, Mohammed H, White M, & Desai M (2018). Sexualised drug use in the United Kingdom (UK): a review of the literature. International Journal of Drug Policy, 55, 131–148. [DOI] [PubMed] [Google Scholar]
- Fan X, Lau JTF, Cai Y, Li J, Ma T, Gu J, & Wang Z (2021). Prevalence and associated factors of sexualized drug use in sex work among transgender women sex workers in China. AIDS Care, 33(8), 1098–1106. doi: 10.1080/09540121.2020.1851017 [DOI] [PubMed] [Google Scholar]
- Friede T, Röver C, Wandel S, & Neuenschwander B (2017). Meta-analysis of few small studies in orphan diseases. Research Synthesis Methods, 8(1), 79–91. doi: 10.1002/jrsm.1217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gronau QF, Van Erp S, Heck DW, Cesario J, Jonas KJ, & Wagenmakers E-J (2017). A Bayesian model-averaged meta-analysis of the power pose effect with informed and default priors: the case of felt power. Comprehensive Results in Social Psychology, 2(1), 123–138. doi: 10.1080/23743603.2017.1326760 [DOI] [Google Scholar]
- Guadamuz TE, Clatts MC, & Goldsamt LA (2018). Heavy Alcohol Use Among Migrant and Non-Migrant Male Sex Workers in Thailand: A Neglected HIV/STI Vulnerability. Substance use & misuse, 53(11), 1907–1914. doi: 10.1080/10826084.2018.1436564 [DOI] [PubMed] [Google Scholar]
- Han WM, Colby DJ, Khlaiphuengsin A, Apornpong T, Kerr SJ, Ubolyam S, … Tangkijvanich, P. (2020). Large transmission cluster of acute hepatitis C identified among HIV-positive men who have sex with men in Bangkok, Thailand. Liver Int, 40(9), 2104–2109. doi: 10.1111/liv.14578 [DOI] [PubMed] [Google Scholar]
- He L, Pan X, Wang N, Yang J, Jiang J, Luo Y, Li X (2018). New types of drug use and risks of drug use among men who have sex with men: a cross-sectional study in Hangzhou, China. BMC Infect Dis, 18(1), 182–182. doi: 10.1186/s12879-018-3091-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrijgers C, Poels K, Vandebosch H, Platteau T, van Lankveld J, & Florence E (2020). Harm Reduction Practices and Needs in a Belgian Chemsex Context: Findings from a Qualitative Study. International journal of environmental research and public health, 17(23). doi: 10.3390/ijerph17239081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbert MP, Brett CE, Porcellato LA, & Hope VD (2019). Psychosocial and sexual characteristics associated with sexualised drug use and chemsex among men who have sex with men (MSM) in the UK. Sex Transm Infect, 95(5), 342–350. doi: 10.1136/sextrans-2018-053933 [DOI] [PubMed] [Google Scholar]
- Hibbert MP, Hillis A, Brett CE, Porcellato LA, & Hope VD (2021). A narrative systematic review of sexualised drug use and sexual health outcomes among LGBT people. Int J Drug Policy, 93, 103187. doi: 10.1016/j.drugpo.2021.103187 [DOI] [PubMed] [Google Scholar]
- Hidaka Y, Operario D, Tsuji H, Takenaka M, Kimura H, Kamakura M, & Ichikawa S (2014). Prevalence of sexual victimization and correlates of forced sex in Japanese men who have sex with men. PLoS One, 9(5), e95675–e95675. doi: 10.1371/journal.pone.0095675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter LJ, Dargan PI, Benzie A, White JA, & Wood DM (2014). Recreational drug use in men who have sex with men (MSM) attending UK sexual health services is significantly higher than in non-MSM. Postgraduate Medical Journal, 90(1061), 133. doi: 10.1136/postgradmedj-2012-131428 [DOI] [PubMed] [Google Scholar]
- Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, … Moher D (2015). The PRISMA Extension Statement for Reporting of Systematic Reviews Incorporating Network Meta-analyses of Health Care Interventions: Checklist and Explanations. Annals of Internal Medicine, 162(11), 777–784. doi: 10.7326/M14-2385 [DOI] [PubMed] [Google Scholar]
- Ko NY, Koe S, Lee HC, Yen CF, Ko WC, & Hsu ST (2012). Online Sex-Seeking, Substance Use, and Risky Behaviors in Taiwan: Results from the 2010 Asia Internet MSM Sex Survey. Archives of Sexual Behavior, 41(5), 1273–1282. doi: 10.1007/s10508-012-9908-8 [DOI] [PubMed] [Google Scholar]
- Kwan TH, & Lee SS (2019). Bridging Awareness and Acceptance of Pre-Exposure Prophylaxis Among Men Who Have Sex With Men and the Need for Targeting Chemsex and HIV Testing: Cross-Sectional Survey. JMIR public health and surveillance, 5(3), e13083. doi: 10.2196/13083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lafortune D, Blais M, Miller G, Dion L, Lalonde F, & Dargis L (2021). Psychological and Interpersonal Factors Associated with Sexualized Drug Use Among Men Who Have Sex with Men: A Mixed-Methods Systematic Review. Archives of Sexual Behavior, 50(2), 427–460. doi: 10.1007/s10508-020-01741-8 [DOI] [PubMed] [Google Scholar]
- Lagoutte-Renosi J, Richeval C, Phanithavong M, Wiart JF, Castex E, Vanhoy X, … Gaulier JM (2021). Hair analysis can support the follow-up addiction care after acute New Psychoactive Substances intoxication: Illustration by two cases. Drug Test Anal, 13(1), 227–234. doi: 10.1002/dta.2936 [DOI] [PubMed] [Google Scholar]
- Lawn W, Aldridge A, Xia R, & Winstock AR (2019). Substance-Linked Sex in Heterosexual, Homosexual, and Bisexual Men and Women: An Online, Cross-Sectional ʻGlobal Drug Surveyʼ Report. J Sex Med, 16(5), 721–732. doi: 10.1016/j.jsxm.2019.02.018 [DOI] [PubMed] [Google Scholar]
- Liao M, Kang D, Tao X, Li J, Qian Y, Wang G, … Jia Y (2013). Dual epidemics of syphilis and methamphetamine use among drug users in Shandong Province of China. AIDS Care, 25(10), 1236–1244. doi: 10.1080/09540121.2013.764384 [DOI] [PubMed] [Google Scholar]
- Lim SH, Akbar M, Wickersham JA, Kamarulzaman A, & Altice FL (2018). The management of methamphetamine use in sexual settings among men who have sex with men in Malaysia. International Journal of Drug Policy, 55, 256–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim SH, Cheung DH, Guadamuz TE, Wei C, Koe S, & Altice FL (2015). Latent class analysis of substance use among men who have sex with men in Malaysia: Findings from the Asian Internet MSM Sex Survey. Drug and Alcohol Dependence, 151, 31–37. doi: 10.1016/j.drugalcdep.2015.02.040 [DOI] [PubMed] [Google Scholar]
- Liu S, & Detels R (2012). Recreational drug use: an emerging concern among venue-based male sex workers in China. Sex Transm Dis, 39(4), 251–252. doi: 10.1097/OLQ.0b013e31824a0903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao X, Leuba SI, Hu Q, Yan H, Wang Z, Lu L, … Xu J (2021). Use of multiple recreational drugs is associated with new HIV infections among men who have sex with men in China: a multicenter cross-sectional survey. BMC public health, 21(1), 354–354. doi: 10.1186/s12889-021-10223-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell S, Shahmanesh M, & Gafos M (2019). Chemsex behaviours among men who have sex with men: A systematic review of the literature. Int J Drug Policy, 63, 74–89. doi: 10.1016/j.drugpo.2018.11.014 [DOI] [PubMed] [Google Scholar]
- Nemoto T, Iwamoto M, Perngparn U, Areesantichai C, Kamitani E, & Sakata M (2012). HIV-related risk behaviors among kathoey (male-to-female transgender) sex workers in Bangkok, Thailand. AIDS Care, 24(2), 210–219. doi: 10.1080/09540121.2011.597709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newland J, & Kelly-Hanku A (2021). A qualitative scoping review of sexualised drug use (including Chemsex) of men who have sex with men and transgender women in Asia Retrieved from https://www.aidsdatahub.org/resource/qualitative-scoping-review-sexualised-drug-use-including-chemsex-men-who-have-sex-men-and
- Nishijima T, Gatanaga H, Komatsu H, Takano M, Ogane M, Ikeda K, & Oka S (2013). High prevalence of illicit drug use in men who have sex with men with HIV-1 infection in Japan. PLoS One, 8(12), e81960–e81960. doi: 10.1371/journal.pone.0081960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noor SW, Hart TA, Okafor CN, Ware D, Chew KW, DʼSouza G, … Plankey M (2021). Staying or moving: Results of a latent transition analysis examining intra-individual stability of recreational substance use among MSM in the Multicenter AIDS Cohort Study from 2004 to 2016. Drug and Alcohol Dependence, 220, 108516. doi: 10.1016/j.drugalcdep.2021.108516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pattanasin S, Wimonsate W, Chonwattana W, Tongtoyai J, Chaikummao S, Sriporn A, … Holtz TH (2016). Loss to follow-up and bias assessment among a cohort of Thai men who have sex with men in Bangkok, Thailand. International journal of STD & AIDS, 27(3), 196–206. doi: 10.1177/0956462415578954 [DOI] [PubMed] [Google Scholar]
- Peters CMM, Evers YJ, Dukers-Muijrers NHTM, & Hoebe CJPA (2020). Sexually Transmitted Infection and Chemsex Also Highly Prevalent Among Male Sex Workers Outside Amsterdam, The Netherlands. Sexually transmitted diseases, 47(6). Retrieved from https://journals.lww.com/stdjournal/Fulltext/2020/06000/Sexually_Transmitted_Infection_and_Chemsex_Also.14.aspx [DOI] [PubMed] [Google Scholar]
- Pichini S, Di Trana A, Torrens M, Scherbaum N, & Zaami S (2020). Editorial: New Trends of Substance Abuse: Looking for New Psychotropic Effects of Chem Sex Drugs, Cognitive Enhancers, and New Psychoactive Substances. Frontiers in psychiatry, 11, 612192–612192. doi: 10.3389/fpsyt.2020.612192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieprzyca E, Skowronek R, Nižnanský Ľ, & Czekaj P (2020). Synthetic cathinones – From natural plant stimulant to new drug of abuse. European Journal of Pharmacology, 875, 173012. doi: 10.1016/j.ejphar.2020.173012 [DOI] [PubMed] [Google Scholar]
- Piyaraj P, van Griensven F, Holtz TH, Mock PA, Varangrat A, Wimonsate W, … Chonwattana W (2018). The finding of casual sex partners on the internet, methamphetamine use for sexual pleasure, and incidence of HIV infection among men who have sex with men in Bangkok, Thailand: an observational cohort study. The Lancet HIV, 5(7), e379–e389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plankey MW, Ostrow DG, Stall R, Cox C, Li X, Peck JA, & Jacobson LP (2007). The relationship between methamphetamine and popper use and risk of HIV seroconversion in the multicenter AIDS cohort study. Journal of acquired immune deficiency syndromes (1999), 45(1), 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes K, Turner R, & Higgins J (2014). Predictive distributions were developed for the extent of heterogeneity in meta-analyses of continuous outcome data. Journal of Clinical Epidemiology, 68. doi: 10.1016/j.jclinepi.2014.08.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Röver C (2017). Bayesian Random-Effects Meta-Analysis Using the bayesmeta R Package. Journal of Statistical Software, 93. doi: 10.18637/jss.v093.i06 [DOI] [Google Scholar]
- Sapsirisavat V, Phanuphak N, Keadpudsa S, Egan JE, Pussadee K, Klaytong P, … Stall R (2016). Psychosocial and Behavioral Characteristics of High-Risk Men Who Have Sex with Men (MSM) of Unknown HIV Positive Serostatus in Bangkok, Thailand. AIDS and behavior, 20(Suppl 3), 386–397. doi: 10.1007/s10461-016-1519-2 [DOI] [PubMed] [Google Scholar]
- Schmidt AJ, Bourne A, Weatherburn P, Reid D, Marcus U, & Hickson F (2016). Illicit drug use among gay and bisexual men in 44 cities: Findings from the European MSM Internet Survey (EMIS). International Journal of Drug Policy, 38, 4–12. doi: 10.1016/j.drugpo.2016.09.007 [DOI] [PubMed] [Google Scholar]
- Schreck B, Victorri-Vigneau C, Guerlais M, Laforgue E, & Grall-Bronnec M (2021). Slam Practice: A Review of the Literature. European Addiction Research, 27(3), 161–178. doi: 10.1159/000511897 [DOI] [PubMed] [Google Scholar]
- Stuart D (2013). Sexualised drug use by MSM: Background, current status and response. HIV Nurs, 13, 1–5. [Google Scholar]
- Sze WN, Kwan TH, Kei LKC, Chui LJY, Shan LS, Wong NS, … Lee SS (2020). Delineation of chemsex patterns of men who have sex with men in association with their sexual networks and linkage to HIV prevention. International Journal of Drug Policy, 75, 102591–102591. doi: 10.1016/j.drugpo.2019.10.015 [DOI] [PubMed] [Google Scholar]
- Tan RKJ, O’Hara CA, Koh WL, Le D, Tan A, Tyler A, … Wong ML (2021). Delineating patterns of sexualized substance use and its association with sexual and mental health outcomes among young gay, bisexual and other men who have sex with men in Singapore: a latent class analysis. BMC public health, 21(1), 1026–1026. doi: 10.1186/s12889-021-11056-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomkins A, George R, & Kliner M (2019). Sexualised drug taking among men who have sex with men: a systematic review. Perspectives in public health, 139(1), 23–33. [DOI] [PubMed] [Google Scholar]
- Viechtbauer W (2010). Conducting Meta-Analyses in R with the metafor Package 2010, 36(3), 48. doi: 10.18637/jss.v036.i03 [DOI] [Google Scholar]
- Vu NT, Holt M, Phan HT, La LT, Tran GM, Doan TT, … de Wit, J. (2017). The Relationship Between Methamphetamine Use, Sexual Sensation Seeking and Condomless Anal Intercourse Among Men Who Have Sex With Men in Vietnam: Results of a Community-Based, Cross-Sectional Study. AIDS and behavior, 21(4), 1105–1116. doi: 10.1007/s10461-016-1467-x [DOI] [PubMed] [Google Scholar]
- Vu NTT, Holt M, Phan HTT, La LT, Tran GM, Doan TT, … de Wit J (2017). Amphetamine-Type-Stimulants (ATS) Use and Homosexuality-Related Enacted Stigma Are Associated With Depression Among Men Who Have Sex With Men (MSM) in Two Major Cities in Vietnam in 2014. Subst Use Misuse, 52(11), 1411–1419. doi: 10.1080/10826084.2017.1284233 [DOI] [PubMed] [Google Scholar]
- Wang H, & Jonas KJ (2021). The likelihood of severe COVID-19 outcomes among PLHIV with various comorbidities: a comparative frequentist and Bayesian meta-analysis approach. Journal of the International AIDS Society, 24(11), e25841. doi: 10.1002/jia2.25841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z, Mo PKH, Ip M, Fang Y, & Lau JTF (2020). Uptake and willingness to use PrEP among Chinese gay, bisexual and other men who have sex with men with experience of sexualized drug use in the past year. BMC Infectious Diseases, 20(1), 299. doi: 10.1186/s12879-020-05024-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z, Yang X, Mo PKH, Fang Y, Ip TKM, & Lau JTF (2020). Influence of Social Media on Sexualized Drug Use and Chemsex Among Chinese Men Who Have Sex With Men: Observational Prospective Cohort Study. J Med Internet Res, 22(7), e17894–e17894. doi: 10.2196/17894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wansom T, Pinyakorn S, Kolsteeg CJ, Kroon E, Sacdalan CP, Chomchey N, … Colby DJ (2020). Brief Report: Group Sex and Methamphetamine Use Fuel an Explosive Epidemic of Hepatitis C Among HIV-Infected Men Who Have Sex With Men in Bangkok, Thailand. J Acquir Immune Defic Syndr, 84(4), 331–335. doi: 10.1097/qai.0000000000002356 [DOI] [PubMed] [Google Scholar]
- Wei C, Guadamuz TE, Lim SH, Huang Y, & Koe S (2012). Patterns and levels of illicit drug use among men who have sex with men in Asia. Drug and Alcohol Dependence, 120(1), 246–249. doi: 10.1016/j.drugalcdep.2011.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells G, Shea B, O’Connell D, Peterson j., Welch V, Losos M, & Tugwell P (2000). The Newcastle–Ottawa Scale (NOS) for Assessing the Quality of Non-Randomized Studies in Meta-Analysis
- White D, Rosenberg ES, Cooper HLF, del Rio C, Sanchez TH, Salazar LF, & Sullivan PS (2014). Racial differences in the validity of self-reported drug use among men who have sex with men in Atlanta, GA. Drug and Alcohol Dependence, 138, 146–153. doi: 10.1016/j.drugalcdep.2014.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wirtz AL, Peryshkina A, Mogilniy V, Beyrer C, & Decker MR (2015). Current and recent drug use intensifies sexual and structural HIV risk outcomes among female sex workers in the Russian Federation. Int J Drug Policy, 26(8), 755–763. doi: 10.1016/j.drugpo.2015.04.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu HH, Shen YT, Chiou CS, Fang CT, & Lo YC (2019). Shigellosis outbreak among MSM living with HIV: a case-control study in Taiwan, 2015–2016. Sex Transm Infect, 95(1), 67–70. doi: 10.1136/sextrans-2017-053410 [DOI] [PubMed] [Google Scholar]
- Xiong M, Ong J, Wang Y, Tang W, & Wang C (2021). P195 Sexualized drug use among female sex workers from eight cities in China. Sexually Transmitted Infections, 97(Suppl 1), A109. doi: 10.1136/sextrans-2021-sti.286 [DOI] [Google Scholar]
- Xu JJ, Qian HZ, Chu ZX, Zhang J, Hu QH, Jiang YJ, … Shang H (2014). Recreational drug use among Chinese men who have sex with men: a risky combination with unprotected sex for acquiring HIV infection. Biomed Res Int, 2014, 725361–725361. doi: 10.1155/2014/725361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu JJ, Zhang C, Hu QH, Chu ZX, Zhang J, Li YZ, … Qian HZ (2014). Recreational drug use and risks of HIV and sexually transmitted infections among Chinese men who have sex with men: Mediation through multiple sexual partnerships. BMC Infect Dis, 14, 642–642. doi: 10.1186/s12879-014-0642-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang GL, Zhang AD, Yu Y, Liu H, Long FY, & Yan J (2016). Drug use and its associated factors among money boys in Hunan Province, China. Public Health, 140, 213–220. doi: 10.1016/j.puhe.2016.06.005 [DOI] [PubMed] [Google Scholar]
- Zaller N, Yang C, Operario D, Latkin C, McKirnan D, O’Donnell L, … Spikes P (2017). Alcohol and cocaine use among Latino and African American MSM in 6 US cities. Journal of substance abuse treatment, 80, 26–32. doi: 10.1016/j.jsat.2017.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


