ABSTRACT
Background and Aims:
Our aim was to assess the efficacy of analgesia using ilioinguinal–iliohypogastric (IIIH) nerve block, transversus abdominis plane (TAP) block and diclofenac after caesarean delivery (CD) under spinal anaesthesia (SA).]
Methods:
A total of 457 healthy parturients undergoing CD under SA were included in this prospective, observational study. Groups differed in the postoperative analgesic strategies received by the parturient at the end of surgery: group D (n = 148) received intramuscular diclofenac sodium, group I (n = 153) received bilateral IIIH block with bupivacaine plus clonidine and group T (n = 156) received bilateral TAP block with bupivacaine plus clonidine. Total duration of postoperative analgesia, numerical pain rating scale (NRS) scores, patient satisfaction score, rescue analgesics in the first 48 h postoperatively and adverse effects were observed. A value of P < 0.05 was taken as significant.
Results:
Total duration of analgesia was longest (18.2 ± 1.3 h) in group T and shortest in group D (6.3 ± 0.8 h) compared to group I (13.1 ± 1.2 h) (P < 0.001). Total analgesic requirement in postoperative 48 h was lowest in group T (152.1 ± 34.9 mg), highest in group D (355.0 ± 25.6 mg) and intermediate in group I (221.0 ± 30.0 mg) (P < 0.001). Mean NRS scores were lower in group T compared to those in groups D and I. The patients in group T were extremely satisfied, in group I were satisfied and in group D were dissatisfied (P < 0.001).
Conclusion:
Bilateral TAP block with bupivacaine and clonidine after CD under SA increases the duration of postoperative analgesia.
Keywords: Analgesic technique, bupivacaine, caesarean delivery, clonidine, diclofenac sodium, ilioinguinal–iliohypogastric nerve block, transversus abdominis plane block
INTRODUCTION
Caesarean delivery (CD) is commonly performed under spinal anaesthesia (SA) and is associated with moderate-to-severe postoperative pain. In the absence of adequate analgesia, maternal recovery, breast feeding initiation and bonding of mother with the baby can be affected. Hence, management of postoperative pain after CD is an area of concern for the obstetric anaesthesiologist.[1]
Multimodal analgesia is usually used for pain relief after CD. Several peripheral nerve blocks have been used to augment the systemic analgesics used for pain relief. The commonly performed nerve blocks include the transversus abdominis (TAP) block, ilioinguinal–iliohypogastric (IIIH) block, lumbar paravertebral block, quadratus lumborum block and erector spinae block. All these blocks have been employed with varying success in parturients undergoing CD under SA.
In this study, we compared intramuscular diclofenac sodium and two commonly used blocks (TAP block and IIIH block). The primary objective was the mean duration of postoperative analgesia. Secondary objectives were to compare the following parameters with the different analgesic techniques: total analgesic requirement (in mg) in the first 48 h postoperatively, pain scores at rest and on movement from supine to sitting position, haemodynamic parameters, difference in patient satisfaction scores and adverse effects.
METHODS
This study was conducted at the Department of Anaesthesiology at a tertiary care hospital in India from November 2015 to March 2017 after approval from the Ethics Committee for Human Research (vide letter no. LHMC/ECHR/2015/115 dated 30/10/2015). The trial was registered with Central Trial Registry - India (vide registration number CTRI/2018/01/011097, www.ctri.nic.in). Written informed consent was obtained for participation in the study and use of the patient data for research and educational purposes. The study was carried out in accordance with the principles of the Declaration of Helsinki, 2013.
Parturients aged 18–40 years who were scheduled to undergo elective/emergency CD under SA were eligible to participate in this study. The exclusion criteria were patients with American Society of Anesthesiologists (ASA) physical status III and IV, body weight >90 or <40 kg, history of drug allergy to drugs used in the study (diclofenac sodium, bupivacaine, clonidine or metoclopramide), contraindications to any of analgesic drugs, patients on chronic use of opioids, non-steroidal anti-inflammatory drugs (NSAIDs) or corticosteroids, and patients who were unable to understand numerical rating scale (NRS) score for pain or study protocol.
Further, patients requiring additional anaesthesia (due to prolonged duration of surgery) or those who were unable to communicate postoperatively due to postpartum obstetric or medical complications were excluded from the analysis as the study outcome could not be captured.
The study participants were divided into three groups as follows:
Group D: Diclofenac sodium 75 mg intramuscularly
Group I: Bilateral IIIH block with 10 ml of 0.25% bupivacaine along with 1 µg/kg clonidine on each side
Group T: Bilateral TAP block with 15 ml of 0.25% bupivacaine along with 1 µg/kg clonidine on each side.
The patients had the option to choose between intramuscular diclofenac sodium and nerve block. Those opting for nerve blocks were given either bilateral IIIH or bilateral TAP block on alternate basis.
A detailed pre-anaesthetic check-up and investigations were performed. Patients for elective CD were kept nil per oral (NPO) for 6 h, and pantoprazole 40 mg intravenously (IV) and metoclopramide 10 mg IV were given as aspiration prophylaxis. Patients were made familiar with 11-point, 10-cm NRS, with 0 representing no pain and 10 representing worst imaginable pain. On arrival in the operating room, pulse oximeter probe (SpO2), electrocardiography (ECG) leads and non-invasive blood pressure (NIBP) cuff were attached and the baseline readings were recorded. SA was performed at the L3–L4 or L2–L3 intervertebral space with hyperbaric 0.5% bupivacaine 1.8–2.0 ml with 25 μg fentanyl. At the end of the surgery, postoperative analgesia was administered as per the allocation made to the groups at the beginning of the study.
Patients allocated to group D were administered 75 g diclofenac sodium intramuscularly in the left buttock.
Group T received TAP block under aseptic conditions at the end of the surgery, when the sensory block had receded to T10 level by pin prick. The TAP block was performed under ultrasound (US) guidance (M-Turbo, SonoSite, USA) and a linear high-frequency (5–10 Hz) probe. Pajunk® SonoTAP 80-mm, 22-gauge cannula was used to give the block. The US probe was placed in a transverse plane on the lateral abdominal wall in the midaxillary line between the lower costal margin and the iliac crest. Two ml of saline was injected to confirm the correct needle position, followed by 15 ml of 0.25% bupivacaine along with 1 μg/kg clonidine. The TAP block was then performed on the opposite side using an identical technique.
Group I received the IIIH block in the supine position in aseptic conditions under US guidance. The inferior portion of the US probe was placed over the previously identified anterior superior iliac spine, with the superior margin of the probe pointed in an oblique plane at the umbilicus. Under continuous US guidance, an 80-mm, 22-gauge needle (SonoplexStim; Pajunk®, Germany) was advanced using an in-plane technique and 10 ml of 0.25% bupivacaine along with 1 μg/kg clonidine was injected on each side.
Both blocks were performed by an investigator who had an experience of giving at least 20 blocks before the study. The duration of postoperative analgesia in the three groups was recorded. Degree of pain was observed by using the NRS-11 score at rest and on movement from lying down to a sitting position, except when the patient was sleeping or sitting comfortably, then NRS score was considered ≤3. When the NRS score was ≥4 after wearing off of the study analgesia, systemic analgesic was administered in the form of diclofenac 1 mg/kg IV (to a maximum of 3 mg/kg/day). The amount of analgesic drug required in 48 h postoperatively was recorded. Sedation was evaluated using a 4-point ordinal scale (1 = wide awake and alert; 2 = awake but drowsy, responding to verbal stimulus; 3 = arousal, responding to physical stimulus; 4 = not arousal, not responding to physical stimulus). Post-operative nausea and vomiting (PONV) was assessed with a 4-point scale (0 = none, 1 = nausea, 2 = retching/dry vomiting, 3 = vomiting). Patients were asked to score their level of satisfaction with regards to postoperative pain relief on a 4-point patient satisfaction score (1 = extremely satisfied, 2 = satisfied, 3 = dissatisfied, 4 = extremely dissatisfied). Other associated side effects such as respiratory depression (respiratory rate [RR] <8 breaths/min or SpO2 <94%, dry mouth [on a binary scale, yes/no]) were also observed. All patients were monitored postoperatively using a non-invasive automated device and the readings were noted. Decreases in systolic blood pressure (SBP) to <90 mmHg or >20% below baseline (recorded on arrival in the operating room) were treated with IV ephedrine 6 mg as required. Bradycardia of <50 beats per min was treated with IV atropine 0.6 mg.
The primary outcome was the mean duration of postoperative analgesia, defined as the time in hours from the time of giving the analgesic technique to first analgesic administration in the postoperative period. Secondary outcomes were to compare the following parameters with the different analgesic techniques: total analgesic requirement (in mg) in the first 48 h postoperatively, pain scores at rest and on movement from supine to sitting position, haemodynamic parameters, difference in patient satisfaction scores and adverse effects.
Sample size calculated for this non-randomised clinical trial was 457. Power analysis based on the pilot cases indicated that at least 457 patients will be required to demonstrate an assumed clinically significant difference of 2 h in duration of postoperative analgesia with different techniques, taking an α of 0.01, a power of 95% and a standard deviation of 4 h based on data from the researcher experience. The formula used for sample size calculation is Cochran’s formula. To account for dropouts related to prolonged surgery or postoperative complications, we aimed to recruit at least 457 patients.
The data was compiled, tabulated and statistically analysed using Statistical Package for the Social Sciences (SPSS) version 20 (IBM Corp. Armonk, NY). The comparison of normally distributed continuous variables between the groups was performed using analysis of variance (ANOVA) with appropriate post hoc test. Chi-square test was used for categorical variables. For all statistical tests, P value less than 0.05 was considered significant.
RESULTS
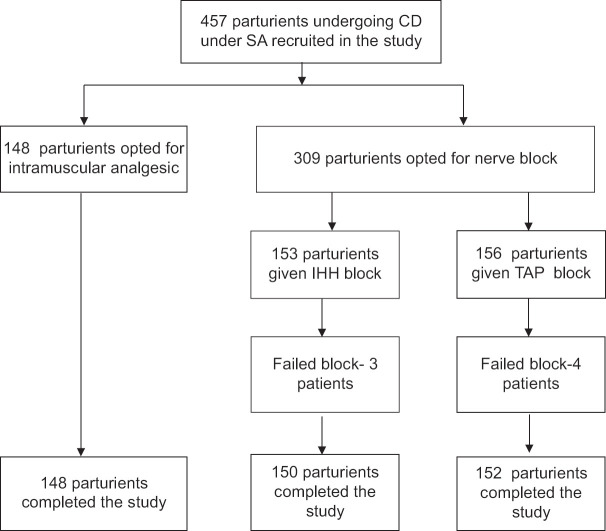
A total of 457 patients were analysed in this study [Figure 1]. The baseline age and weight of the study subjects are shown in Table 1.
Figure 1.
Flow diagram of the study. CD = caesarean delivery, SA = spinal anaesthesia
Table 1.
Demographic profile in the two groups
| Group D (n=148) | Group I (n=150) | Group T (n=152) | P value | |
|---|---|---|---|---|
|
| ||||
| Mean±SD | Mean±SD | Mean±SD | ||
| Age (yrs) | 25.2±3.3 | 25.3±3.8 | 25.5±3.8 | 0.806 |
| Weight (kg) | 69.0±9.6 | 68.8±9.8 | 67.9±10.1 | 0.621 |
Total duration of analgesia was longest in group T and shortest in group D compared to group I [Table 2]. The difference in the total duration of analgesia between groups D and I (P < 0.001), groups D and T (P < 0.001) and between groups I and T (P < 0.001) was clinically and statistically significant.
Table 2.
Study parameters in the two groups
| Observations | Group D (n=148) Mean±SD (95% CI) |
Group I (n=150) Mean±SD (95% CI) |
Group T (n=152) Mean±SD (95% CI) |
P | Group D versus group I | Group D versus group T | Group I versus group T |
|---|---|---|---|---|---|---|---|
| Total duration of analgesia (h) | 6.3±0.8 (4.7-7.9) | 13.1±1.2 (10.7-15.4) | 18.2±1.3 (15.5-20.6) | <0.001 | <0.001 | <0.001 | <0.001 |
| Rescue analgesic requirement (mg) | 355.0±25.6 (304.8-405.1) | 221.0±30.0 (162.2-279.8) | 152.1±34.9 (83.7-220.5) | <0.001 | <0.001 | <0.001 | <0.001 |
| Patient satisfaction score | 2.9±0.4 (2.1-3.6) | 2.0±0.1 (1.8-2.2) | 1.2±0.2 (0.8-1.6) | <0.001 | <0.001 | <0.001 | <0.001 |
| Dry mouth (n) | 19 | 25 | 26 | 0.284 | |||
| PONV (n) | 1.4 | 2.1 | 1.4 | 0.565 | |||
| Respiratory depression (n) | 0 | 0 | 0 | – |
h-Hour, mg-Milligram, PONV-Postoperative nausea and vomiting, SD-Standard Deviation, CI - Confidence Interval, n-number
The amount of systemic analgesic requirement in postoperative 48 h was lowest in group T, highest in group D and intermediate in group I [Table 2]. There was significant statistical difference in the requirement of rescue analgesics between groups D and I (P < 0.001), groups D and T (P < 0.001) and between groups I and T (P < 0.001).
The mean NRS scores at the time of first analgesic rescue were comparable in all the three groups (P > 0.02). The mean NRS was 4.33 ± 0.84 (95% confidence interval [CI], 2.68, 5.97) in group D, 4.66 ± 0.84 (95% CI, 3.01, 6.30) in group I and 4.55 ± 0.61 (95% CI, 3.35, 5.74) in group T.
There was no difference among the three groups in dry mouth and PONV scores [Table 2]. The mean RR was also comparable at all time points among the groups (P > 0.05).
The difference in the patient satisfaction scores was significant between groups D and I (P < 0.001), groups D and T (P < 0.001) and between groups I and T (P < 0.001). All the patients in group D were dissatisfied, in group I were satisfied and in group T were extremely satisfied [Table 2].
DISCUSSION
This study found that duration of postoperative analgesia after CD under SA was significantly more with TAP block compared to both bilateral IIIH and intramuscular diclofenac sodium. Bilateral IIIH, in turn, had greater duration of analgesia than intramuscular diclofenac sodium. Accordingly, the need for systemic analgesia in the 48-h postoperative period was the least in TAP block, which was followed by IIIH block and intramuscular diclofenac sodium. The adverse effects were comparable between the two groups.
The few studies available comparing the two blocks are for hernia repair surgery.[2] Modalities including bilateral IIIH as well as TAP block have been explored by various studies.[3-7] These studies report that bilateral IIIH block provided excellent postoperative pain control following CD and significantly reduced the amount of opioid used by patients following CD. In the present study, TAP block provided the longest duration of analgesia. The prolonged duration of analgesic effect after TAP blockade may relate to the fact that TAP is relatively poorly vascularised, and therefore drug clearance may be slow. Many previous investigators have reported the analgesic benefit of TAP block in patients undergoing a wide variety of lower abdominal surgeries including CD. Mc Donnell et al.[8] and Kanta et al.[6] investigated the effect of TAP block with 0.75% and 0.5% ropivacaine, respectively, and reported improved postoperative pain scores, reduced postoperative opioid consumption and higher patient satisfaction. Mankikar et al.[9] evaluated the efficacy of TAP block given with 0.5% ropivacaine in patients undergoing CD and concluded that the duration of postoperative analgesia was increased in TAP block. The mean duration of analgesia in our patients receiving TAP block was much longer than the said study since bupivacaine has a longer duration of action compared to ropivacaine and clonidine is known to further enhance the duration of local anaesthetics in peripheral nerve blocks.[10]
Eslamian et al.[11] also reported findings similar to ours. A meta-analysis by Abdallah et al.[12] concluded that TAP block can provide effective analgesia when spinal morphine is contraindicated or not used in patients undergoing CD under SA. In a recent similar study conducted by Jadon et al.,[13] TAP block, when given with 20 ml of 0.375% ropivacaine, provided 12 h of analgesia in the postoperative period.
Some authors have opinioned that TAP block does not improve the quality of postoperative CD analgesia. Costello et al.,[14] Kwikiriza et al.[15] and Sultan et al.[16] concluded that in the setting of multimodal analgesia, spinal morphine reduces early pain after CD and TAP block does not provide comparable analgesia or any additional benefit to spinal morphine.
Majority of studies have administered bupivacaine alone for TAP block. Our group has earlier demonstrated the utility of clonidine in combination with bupivacaine.[17] The duration of analgesia provided by IIIH block in our study was less than that produced by TAP block. IIIH block produces very specific and limited dermatomal analgesia (L1, L2). TAP block, on the other hand, provides more widespread analgesia. The minimum analgesic requirement in TAP group is a reflection of the potency and long duration of action of TAP block given with bupivacaine and clonidine.
The incidence of adverse effects of clonidine like dry mouth was comparable among the three groups. Practice of long hours of fasting during labour may have also contributed to dryness of mouth in the non-clonidine group. Sedation levels were also comparable. Quite a few patients had been given a trial of labour and had prolonged labour pains. Also, many were delivered at odd hours in the night, probably contributing to their drowsiness. Although the patients were sedated, they were responding to verbal commands and were able to breastfeed the babies; also, drowsiness did not interfere with measurement of pain.
Regarding patient satisfaction, majority of the patients in group D were dissatisfied, in group I were satisfied and in group T were extremely satisfied. This reflects the long duration of analgesia provided by TAP block and IIIH block compared to diclofenac, with the incidence of adverse effects not being very different among the three groups.
The major limitation of our study is that it is not a randomised trial, and hence, a possibility of selection bias exists.
CONCLUSION
The bilateral TAP block with bupivacaine plus clonidine on each side for CD under SA significantly increases the duration of postoperative analgesia compared to bilateral IIIH block with bupivacaine plus clonidine on each side or intramuscular diclofenac sodium.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Elahwal L, Elrahwan S, Elbadry AA. Ilioinguinal and iliohypogastric nerve block for acute and chronic pain relief after caesarean section: A randomized controlled trial. Anesth Pain Med. 2022;12:e121837. doi: 10.5812/aapm.121837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kamal K, Jain P, Bansal T, Ahlawat G. A comparative study to evaluate ultrasound-guided transversus abdominis plane block versus ilioinguinal iliohypogastric nerve block for post-operative analgesia in adult patients undergoing inguinal hernia repair. Indian J Anaesth. 2018;62:292–7. doi: 10.4103/ija.IJA_548_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bell EA, Jones BP, Olufolabi AJ, Dexter F, Phillips-Bute B, Roy A, et al. Iliohypogastric-ilioinguinal peripheral nerve block for post-cesarean delivery analgesia decreases morphine use opioid-related side effects. Can J Anesth. 2002;49:694–700. doi: 10.1007/BF03017448. [DOI] [PubMed] [Google Scholar]
- 4.Gucev G, Yasui GM, Chang TY, Lee J. Bilateral ultrasound guided continuous ilioinguinal-iliohypogastric block for pain relief after cesarean delivery. Anesth Analg. 2008;106:1220–2. doi: 10.1213/ane.0b013e3181683821. [DOI] [PubMed] [Google Scholar]
- 5.Sakalli M, Ceyhan A, Uysal HY, Yazici I, Başar H. The efficacy of ilioinguinal and iliohypogastric nerve block for postoperative pain after caesarean section. J Res Med Sci. 2010;15:6–13. [PMC free article] [PubMed] [Google Scholar]
- 6.Kanta B, Sonali D, Gazala P, Yunus K, Kiran K. A randomised comparative study of transversus abdominis plane block with or without intravenous diclofenac sodium as a component of multimodal regimen for post-operative analgesia following caesarean section. Indian J Anaesth. 2021;65:316–20. doi: 10.4103/ija.IJA_761_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baaj JM, Alsatali RA, Majaj HA, Babay ZA, Thallay AK. Efficacy of ultrasound guided transversus abdominis plane (TAP) block for post caesarean section delivery analgesia. Middle East J Anaesthesiol. 2010;20:821–6. [PubMed] [Google Scholar]
- 8.Mc Donnell JG, Curley G, Carney G, Benton A, Costello J, Maharaj CH, et al. The analgesic efficacy of transversus abdominis plane block after caesarean delivery: A randomized controlled trial. Anesth Analg. 2008;106:186–91. doi: 10.1213/01.ane.0000290294.64090.f3. [DOI] [PubMed] [Google Scholar]
- 9.Mankikar MG, Sardesai SP, Ghodki PS. Ultrasound-guided transversus abdominis plane block for post-operative analgesia in patients undergoing caesarean section. Indian J Anaesth. 2016;604:253–7. doi: 10.4103/0019-5049.179451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kohli S, Kaur M, Sahoo S, Vajifdar H, Kohli P. Brachial plexus block: Comparison of two different doses of clonidine added to bupivacaine. J Anaesthesiol Clin Pharmacol. 2013;29:491–5. doi: 10.4103/0970-9185.119147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eslamian L, Jalili Z, Jamal A, Marsoosi V, Movafegh A. Transversus abdominis plane block reduces postoperative pain intensity and analgesic consumption in elective cesarean delivery under general anesthesia. J Anesth. 2012;26:334–8. doi: 10.1007/s00540-012-1336-3. [DOI] [PubMed] [Google Scholar]
- 12.Abdallah FW, Halper SH, Margarido CB. Transversus abdominis plane block for postoperative analgesia after caesarean delivery under spinal anesthesia?A systematic review and meta-analysis. Br J Anaesth. 2012;109:679–87. doi: 10.1093/bja/aes279. [DOI] [PubMed] [Google Scholar]
- 13.Jadon A, Jain P, Chakraborty S, Motaka M, Parida SS, Sinha N, et al. Role of ultrasound guided transversus abdominis plane block as a component of multimodal analgesic regimen for lower segment caesarean section: A randomized double blind clinical study. BMC Anesthesiol. 2018;18:53. doi: 10.1186/s12871-018-0512-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Costello JF, Moore AR, Wieczorek PM, Macarthur AJ, Balki M, Carvalho JC. The transversus abdominis plane block, when used as part of a multimodal regimen inclusive of intrathecal morphine, does not improve analgesia after cesarean delivery. Reg Anesth Pain Med. 2009;34:586–9. doi: 10.1097/aap.0b013e3181b4c922. [DOI] [PubMed] [Google Scholar]
- 15.Kwikiriza A, Kiwanuka JK, Firth PG, Hoeft MA, Modest VE, Ttendo SS. The analgesic effects of intrathecal morphine in comparison with ultrasound-guided transversus abdominis plane block after caesarean section: A randomised controlled trial at a Ugandan regional referral hospital. Anaesthesia. 2019;74:167–73. doi: 10.1111/anae.14467. [DOI] [PubMed] [Google Scholar]
- 16.Sultan P, Halpern SH, Pushpanathan E, Patel S, Carvalho B. The effect of intrathecal morphine dose on outcomes after elective cesarean delivery: A meta-analysis. Anesth Analg. 2016;123:154–64. doi: 10.1213/ANE.0000000000001255. [DOI] [PubMed] [Google Scholar]
- 17.Singh R, Gupta D, Jain A. The effect of addition of intrathecal clonidine to hyperbaric bupivacaine on postoperative pain after lower segment caesarean section: A randomized control trial. Saudi J Anaesth. 2013;7:283–90. doi: 10.4103/1658-354X.115360. [DOI] [PMC free article] [PubMed] [Google Scholar]