ABSTRACT
Background and Aims:
Pain associated with rib fractures is challenging to manage. This pilot trial aimed to assess the efficacy of erector spinae plane block (ESPB) compared with thoracic epidural analgesia (TEA) for controlling pain associated with multiple rib fractures.
Methods:
This randomised, single-blinded, controlled pilot study was conducted on trauma patients who had three or more rib fractures and had been admitted at a tertiary care centre. The study was conducted after receiving ethical approval and trial registration. Patients were randomised into two groups: TEA and ESPB, from February 2019 to February 2020. In the ESPB group, a unilateral or bilateral catheter was inserted in the erector spinae space, and an infusion of 0.125% bupivacaine was started. In the TEA group, the thoracic epidural catheter was inserted, and 0.125% bupivacaine infusion was started. Rescue analgesia using intravenous morphine (0.1 mg/kg) was administered if the Visual Analogue Scale (VAS) score was >3 for 48 hours postoperatively. The primary endpoint was total morphine consumption after administration of ESPB and TEA in patients with a rib fracture.
Results:
Forty patients completed the study, with 20 in each group. Total morphine consumption by patients in the ESPB group was 5.38 ± 2.6 mg per 48 hours, and by those in the TEA group was 5.22 ± 2.11 mg per 48 hours (P = 0.883). Thirty minutes after starting the infusion, mean arterial pressure (MAP) was 64.8 ± 2.1 mmHg in the ESPB group and 57.2 ± 1.3 mmHg in the TEA group (P = 0.00001).
Conclusion:
Total morphine consumption was not statistically different in this pilot trial among the two groups. ESP block may provide similar analgesia with better haemodynamic stability compared to TEA in patients with multiple traumatic rib fractures.
Keywords: Acute pain, epidural analgesia, erector spinae plane block, nerve block, rib fracture, thoracic epidural analgesia, trauma
INTRODUCTION
The pain associated with a rib fracture is challenging. If not treated promptly, the reduced tidal volume associated with it predisposes to significant atelectasis, retention of pulmonary secretions, and pneumonia. Apart from hypoventilation, the other cause of increased morbidity in rib fractures is an impaired gas exchange in the damaged lung underlying the fractures and an altered breathing mechanism.[1] Many analgesic techniques have been used to decrease the pain associated with rib fractures, including systemic opioids, thoracic epidural analgesia (TEA), paravertebral block, pectoralis blocks, intrapleural block, intercostal block, and, more recently, serratus anterior plane block.[2,3] Opioids were previously the mainstay of treatment but came with significant side effects, including respiratory depression, depressed cough reflex, and delirium.[4] TEA has become the most common modality, but a meta-analysis of randomised controlled trials (RCTs) found no benefits in developing pulmonary complications and length of stay.[5] Thoracic paravertebral blocks (TPVBs) have been used successfully, but this frequently utilises multiple catheters and requires proximity with pleura.
A recent addition to clinical practice is an ultrasound-guided erector spinae plane block (ESPB) that targets the space below the erector spinae muscle.[6] This pilot trial was conducted to assess the efficacy and safety of ESPB compared with TEA for relieving pain in patients with multiple traumatic rib fractures. The primary endpoint was total morphine consumption after administration of ESPB and TEA in patients with a rib fracture. Secondary endpoints were pain scores and mean arterial pressure (MAP) during the first 48 h.
METHODS
This randomised, single-blinded pilot study was conducted from February 2019 to January 2020 after receiving the approval of the institutional ethical committee (614/IEC/IGIMS/2018 dated 17 December 2018). The study was registered in the Clinical Trials Registry - India (vide registration number CTRI/2019/02/017503, www.ctri.nic.in). The study was carried out following the principles of the Declaration of Helsinki, 2013. The study included trauma patients with rib fractures admitted to a tertiary care hospital’s emergency department (ED). Every patient signed an informed and written consent (study protocol was explained in their native language) for participation in the study and use of patient data for research and educational purposes before enrolment. Patients 18 to 60 years of age, having rib fractures that induced any respiratory symptoms (pain in breathing, coughing, and moving, shortness of breath, or pain in taking a deep breath), and having a history of trauma not older than one week with multiple, unilateral, or bilateral rib fractures were included in the study. The presence and number of fractured ribs were confirmed through X-ray film and chest computed tomography (CT). Exclusion criteria were patients with long-standing analgesic therapy, opioid dependence, communication difficulty, or those on antiplatelets or anticoagulants (low molecular weight heparin or oral anticoagulant) or who were diagnosed with any bleeding disorder. Haemodynamically unstable patients (patients with systolic blood pressure below 90 mmHg or on any inotropic infusion), intubated patients (Glasgow Coma Scale <15), or those on mechanical ventilation were also excluded.
The patients were consecutively enrolled once they fulfilled the inclusion and exclusion criteria based on the screening log. General and systemic examination and scoring system [RibScore: the presence of six or more rib fractures, flail chest, three or more severely displaced fractures, first rib fracture, and at least one fracture in all three anatomical areas (anterior, lateral and posterior regions)] was done during screening.[7]
Simple randomisation was done in two groups using computer-generated random numbers (http://www.random.org) on the central computer. Group allocation was concealed in an opaque envelope with a sequence written on the top of the envelope. The envelopes were kept in a sequence and locked, accessible only to the trial coordinator. The trial coordinator was instructed to open the envelope and convey the group allocation once a patient was enrolled on the study. All patients underwent five-lead electrocardiogram (ECG), non-invasive blood pressure, and pulse oximetry monitoring. Furthermore, they were sensitised using the Visual Analogue Scale (VAS), in which 0 represented no pain, and ten represented the worst pain imaginable.
The patients in the control group (TEA group) were put on an epidural catheter, and in the intervention group (ESP group), a catheter was secured in the erector spinae plane. To blind the observer to the origin of the catheter, a sham dressing was put on the upper back.
In the TEA group, an 18-gauge Tuohy needle (Portex Epidural Minipack, SIMS Portex Ltd, Hythe, Kent, UK) was inserted using the midline approach until the operator felt the needle enter the interspinous ligament. The needle was advanced until the operator felt a loss of resistance using a syringe filled with air. The epidural catheter was threaded if no cerebrospinal fluid (CSF) leaked and no paraesthesia was noted. A 20-gauge multi-orifice epidural catheter (Portex Epidural Minipack, SIMS Portex Ltd, Hythe, Kent, UK) was inserted 4–5 cm into the epidural space. The tip of the catheter was inserted in the mid-fractured level of the rib from two levels below the last fractured rib. A test dose of 3 ml of 2% preservative-free lidocaine with 1:200000 epinephrine was administered into the thoracic epidural (TE) catheter to exclude intravascular or intrathecal insertion. Thirty minutes after drug delivery, sensory dermatomal testing was performed with an alcohol swab to assess the block level. The observer who collected the data was not aware of the intervention done.
In the ESP group, the patients were placed in a sitting or lateral decubitus position. The vertebrae corresponding to the centre of all affected ribs were selected. A high-frequency (10–15 MHz) linear array transducer was placed in a longitudinal parasagittal plane about 3 cm lateral to the spinous process. The transverse process was recognised as a hyperechoic curvilinear structure with a square contour. Muscles were identified from superficial to deep as the trapezius, rhomboideus major, and erector spinae muscles. An 18-gauge echogenic needle was inserted using an in-plane, cranial-to-caudal approach to contact the bony shadow of the transverse process (TP) with the tip deep into the fascial plane of the erector spinae muscle. The correct location of the needle tip was confirmed by injecting 0.5–1 ml of normal saline and observing linear fluid spread, lifting the erector spinae muscle off the tip of the TP. Once the fascial plane was recognised, a 20-gauge multi-orifice catheter (SIMS Portex Ltd, Hythe, Kent, UK) was secured. Correct catheter location was confirmed by 2–3 ml of 0.9% saline. The same was repeated on the other side for bilateral rib fractures. Thirty minutes after drug delivery, sensory dermatomal testing with an alcohol swab was performed to assess the block level. The same technique of observer blinding was practised in this group also. To blind the observer to the origin of the catheter, a sham dressing was put on the entire upper back.
Residents or consultants anaesthesiologists with sufficient experience (had done the procedure more than 50 times successfully) in inserting epidural catheters and performing ESP blocks completed the procedure. After placing the catheters in both groups, the patient was started on bupivacaine 0.125% infusion, and the infusion volume was decided by the number of segments to be covered. The infusion rate was calculated depending on the number of ribs fractured (2 ml/h for every segment). The maximum dose of local anaesthetic was kept below 400 mg for 24 h to keep the total dose of local anaesthesia (LA) within safe levels.[8] VAS pain scores on quiet breathing were recorded 20 minutes after starting the infusion, and then two-hourly for 48 hours in the TEA and ESP groups. Rescue analgesia was provided as intravenous (IV) morphine (0.1 mg/kg) to keep the VAS scores below or equal to 3. A total of 48 hours of morphine consumption was recorded for every patient. IV metoclopramide (10 mg) was given as treatment for nausea and vomiting. Any other complication, local anaesthetic toxicity, motor weakness, or injury to the vital organs was noted. An independent observer did all recordings, unaware of group allocation.
Immediately after starting the infusion, then at 15 minutes, 30 minutes, 2 h, and then every 4 h for 48 h, the heart rate and MAP were recorded. Hypotension (decrease in MAP by 20 mmHg from baseline) was treated with IV ephedrine, 5 mg aliquotes, and a reduction in local anaesthetic infusion rate. All patients also received IV ibuprofen (ibuprofen lysine, NeoProfen) 10 mg/kg, initiated as soon as possible after diagnosing rib fracture and after every six hours.
The study’s primary objective was to compare the total 48 h of IV morphine consumption in both groups in the postoperative period, which was used as rescue analgesia to keep the VAS scores less than or equal to 3. The secondary objectives were comparing VAS scores at different time intervals and the haemodynamics for 48 h in the postoperative period.
As we could not find any previous study that compared ESPB and thoracic epidural analgesia in trauma patients, we decided to conduct this pilot study. A benchmark study published by Whitehead et al.[9] states that in a pilot trial, the objective is not to prove the superiority of the treatment but to test trial procedures and processes and that to get estimates of parameters for the main trial, a rule of thumb can be followed for sample size calculation. Additionally, Browne[10] cites a general flat rule to ‘use at least 30 subjects or greater to estimate a parameter’. Keeping this in consideration, we conducted this pilot study on 40 patients.
Data was collected and compiled using Microsoft Excel 2010. Quantitative data were expressed as mean and standard deviation or median and range, as appropriate. Sex ratio, the number of fractured ribs, and chest tube insertion in patients were expressed as frequency and percentage. The Chi-squared test and Fisher’s exact test (as appropriate) were used to examine the relationship between these variables. The two groups were compared for quantitative data using the independent sample t-test or Mann–Whitney U test. Two-way analysis of variance revealed an interaction between groups and measures; thus, each group was tested separately for repeated measures. A comparison of repeated measures was performed using analysis of variance for repeated measures of the Friedman test, followed by a suitable post hoc test.
All statistical analyses were two-tailed and performed using the Statistical Package for the Social Sciences (SPSS) 20.0 evaluation version [IBM Corp, Armonk, NY, USA) Statistics software. A P value of less than 0.05 was considered statistically significant. This study’s design, conduct, and reporting were done in compliance with the Consolidated Standards of Reporting Trials guidelines.
RESULTS
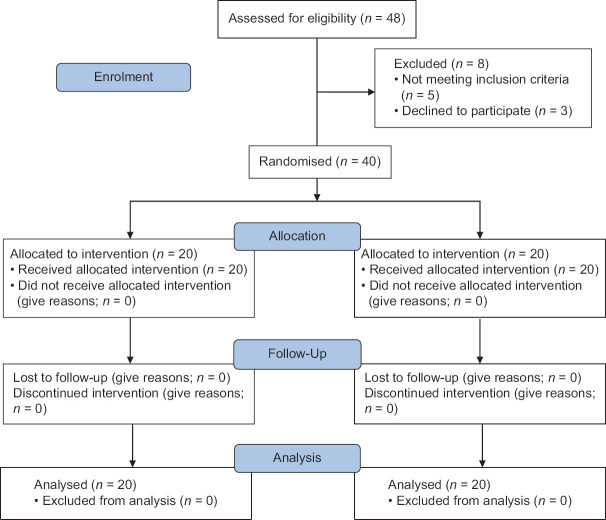
Forty patients received the allocated intervention and completed the final analysis [Figure 1]. The two groups were comparable in demography and baseline parameters [Table 1]. All patients received opioids for pain (IV fentanyl 2 μg/kg) before the intervention.
Figure 1.
Consolidated Standards of Reporting Trials (CONSORT) flow chart
Table 1.
Demographic and clinical characteristics
| TEA group (n=20) | ESPB group (n=20) | P | |
|---|---|---|---|
| Age (years) | 34.9±9.5 | 35.4±10.1 | 0.84 |
| Sex (M/F) | 15/5 | 14/6 | 0.73 |
| BMI (kg/m2) | 26.7±1.5 | 25.2±1.8 | 0.53 |
| Rib fracture (unilateral/bilateral) | 18/2 | 16/4 | 0.52 |
| Number of fractured ribs (3/4/5) | 14/4/2 | 16/2/2 | 0.34 |
| Chest tube insertion (right/left/none) | 3/5/12 | 5/3/12 | 0.45 |
| Associated injury | 18 | 17 | 0.75 |
| Lower limb injury | 10 | 11 | |
| Upper limb surgery | 5 | 6 | |
| Solid organ injury | 3 | 0 | |
| Radiographic scoring system | 3 (3, 3) | 3 (3, 3) | 0.88 |
Data are presented as mean±SD, median (interquartile range), and number. TEA=Thoracic epidural analgesia, ESPB=Erector spinae plane block, BMI=Body mass index
The total 48-h IV morphine consumption by patients in the ESPB group was 5.38 ± 2.6 mg and by those in the TEA group was 5.22 ± 2.11 mg (P = 0.88, t = −0.12; 95% confidence interval (CI) mean difference − 1.35–1.67). The median (IQR) baseline pre-block pain VAS score in the ESPB and TEA groups was 8 (8, 9) and 9 (8, 9), respectively. The post-block pain VAS scores were also comparable between the two groups, except at the 12th, 14th, and 22nd hour time points, during which the pain scores were higher in the ESPB group and were statistically significant [Figure 2]. The baseline heart rate and MAP were comparable between the two groups (P = 0.317). MAP was significantly lower in the TEA group than in the ESPB group during the whole study period except at 42 h [Figure 3]. The MAP decreased from 65.05 ± 0.39 mmHg to 57.2 ± 1.32 mmHg within 15 min of starting the infusion in the TEA group. In the ESPB group, MAP was 64.85 ± 2.10 mmHg at 15 min, comparable to the baseline value. The difference between groups was statistically significant [Figure 3]. The heart rate did not show significant changes over time in either group.
Figure 2.
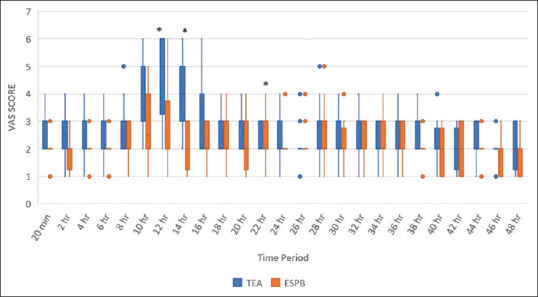
Comparison of VAS score of both groups in 48 hours. Values are represented in the median and interquartile range. VAS = Visual analogue score. TEA = Thoracic epidural analgesia. ESP = Erector spinae plane block. P value < 0.05 is considered statistically significant. *P-value showing a significant difference
Figure 3.
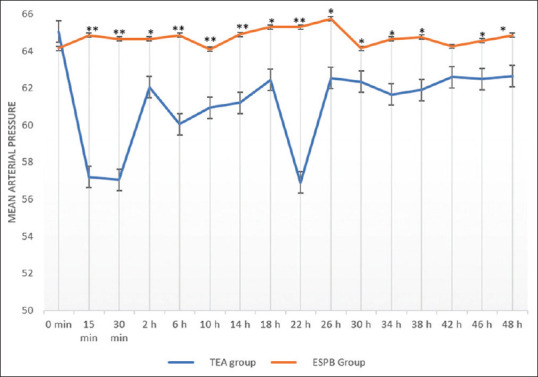
Comparison of mean arterial pressure in both groups throughout the first 48 hours. Values are expressed in mean ± SD. TEA = Thoracic epidural analgesia. ESPB = Erector spinae plane block. *significant P < 0.5, ** highly significant P < 0.001
A decrease in blood pressure was noted in five patients in the TEA group requiring ephedrine. In the ESPB group, no hypotension was reported. The incidence of nausea, vomiting, and oxygen saturation were comparable in the groups during the study period. No other complication was noted in either group.
DISCUSSION
In this pilot trial comparing ESPB with TEA for providing analgesia in trauma patients with rib fractures, we found that the morphine consumption was comparable in the two groups.
A retrospective cohort study on patients with multiple rib fractures receiving ESPB either by single-shot or continuous technique for analgesia also had encouraging results.[11] The primary outcomes were a change in incentive spirometry volume [improved from 784 (694) to 1375 (667) ml during the first 24 h; P < 0.01] and a change in pain scores [reduced from 7.7 (2.5) to 4.7 (3.2) in the first three hours; P < 0.01] following erector spinae plane blockade. Our results were even more encouraging. This is most probably due to the difference in the study’s design. The study, as mentioned earlier, included both single-shot ESPB and continuous ESPB, while the continuous technique was used in our research. Most of our patients had three fractured ribs, and none had more than five fractured ribs. The aforementioned retrospective study included patients with more than seven fractured ribs. The authors did a subgroup analysis based on the number of fractured ribs in patients and found no encouraging results in the group with patients with a higher number of fractured ribs. The reason could be inadequate coverage of all the segments through a single catheter or injection.[6] Although many cadaveric studies and radiological imaging studies investigating the spread in the thoracic ESPB have been published, we still could not define an accepted predictable spread for a wider area.[11,12] ESPB block has been useful in patients with rib fracture as reported in an retrospective study.[13]
TEA has traditionally been considered the gold standard for providing analgesia in rib fracture. Still, a trauma patient often has contraindications to epidural insertion, such as spinal or head injuries and anticoagulant therapy. Our study also found that MAP was significantly lower in the TEA group than in the ESPB group during the whole study period. Furthermore, patients with multiple rib fractures are often polytrauma patients with concomitant injuries, which also increases their susceptibility to hypotension. Studies report the association of morbidity and mortality with hypotension in these patients.[14,15] ESPB is a fascial plane block, and a advantage of the fascial plane block is haemodynamic stability. Coagulopathy or the use of anticoagulation is usually not an issue in ESPB since the theoretical risk of haemorrhage or haematoma is very low.
This pilot study has limitations: its sample size is small and needs to be powered to assess the treatment effect. Additionally, the contribution of associated injuries to overall pain scores could not be quantified, though associated injuries were comparable in the two groups. We could also have measured improvement in pulmonary spirometry as our secondary outcome for better block evaluation. Finally, since there was no previous prospective trial on this topic, our choice of anaesthetic dosage was based on our experience and a few published case reports. Future studies with a larger sample size are necessary to establish the efficacy of this block and the standard dose of anaesthetic required to achieve an adequate level of analgesia. Further trials are also warranted to determine the maximal spread of local anaesthetics by a single catheter.
CONCLUSION
ESPB provide similar analgesia with better haemodynamic stability than TEA in patients with multiple traumatic rib fractures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Dogrul BN, Kiliccalan I, Asci ES, Peker SC. Blunt trauma related chest wall and pulmonary injuries: An overview. Chin J Traumatol. 2020;23:125–38. doi: 10.1016/j.cjtee.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peek J, Smeeing DPJ, Hietbrink F, Houwert RM, Marsman M, de Jong MB. Comparison of analgesic interventions for traumatic rib fractures: A systematic review and meta-analysis. Eur J Trauma Emerg Surg. 2019;45:597–622. doi: 10.1007/s00068-018-0918-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nair A, Diwan S. Efficacy of ultrasound-guided serratus anterior plane block for managing pain due to multiple rib fractures: A scoping review. Cureus. 2022;14:e21322. doi: 10.7759/cureus.21322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim M, Moore JE. Chest trauma: Current recommendations for rib fractures, pneumothorax, and other injuries. Curr Anesthesiol Rep. 2020;10:61–8. doi: 10.1007/s40140-020-00374-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zaw AA, Murry J, Hoang D, Chen K, Louy C, Bloom MB, et al. Epidural analgesia after rib fractures. Am Surg. 2015;81:950–4. [PubMed] [Google Scholar]
- 6.Adhikary SD, Liu WM, Fuller E, Cruz-Eng H, Chin KJ. The effect of erector spinae plane block on respiratory and analgesic outcomes in multiple rib fractures: A retrospective cohort study. Anaesthesia. 2019;74:585–93. doi: 10.1111/anae.14579. [DOI] [PubMed] [Google Scholar]
- 7.Chapman BC, Herbert B, Rodil M, Salotto J, Stovall RT, Biffl W, et al. RibScore: A novel radiographic score based on fracture pattern that predicts pneumonia, respiratory failure, and tracheostomy. J Trauma Acute Care Surg. 2016;80:95–101. doi: 10.1097/TA.0000000000000867. [DOI] [PubMed] [Google Scholar]
- 8.Williams DJ, Walker JD. A nomogram for calculating the maximum dose of local anaesthetic. Anaesthesia. 2014;69:847–53. doi: 10.1111/anae.12679. [DOI] [PubMed] [Google Scholar]
- 9.Whitehead AL, Julious SA, Cooper CL, Campbell MJ. Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Stat Methods Med Res. 2016;25:1057–73. doi: 10.1177/0962280215588241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Browne RH. On the use of a pilot sample for sample size determination. Stat Med. 1995;14:1933–40. doi: 10.1002/sim.4780141709. [DOI] [PubMed] [Google Scholar]
- 11.Yang H-M, Choi YJ, Kwon H-J, O J, Cho TH, Kim SH. Comparison of injectate spread and nerve involvement between retrolaminar and erector spinae plane blocks in the thoracic region: A cadaveric study. Anaesthesia. 2018;73:1244–50. doi: 10.1111/anae.14408. [DOI] [PubMed] [Google Scholar]
- 12.Adhikary SD, Bernard S, Lopez H, Chin KJ. Erector spinae plane block versus retrolaminar block: A magnetic resonance imaging and anatomical study. Reg Anesth Pain Med. 2018;43:756–62. doi: 10.1097/AAP.0000000000000798. [DOI] [PubMed] [Google Scholar]
- 13.Riley B, Malla U, Snels N, Mitchell A, Abi-Fares C, Basson W, et al. Erector spinae nerve block for the management of rib fractures: A retrospective propensity-matched cohort study protocol. Anesth Crit Care. 2019;1:29–33. [Google Scholar]
- 14.Stroda A, Thelen S, M'Pembele R, Khademlou N, Jaekel C, Schiffner E, et al. Association between hypotension and myocardial injury in patients with severe trauma. Eur J Trauma Emerg Surg. 2023;49:217–25. doi: 10.1007/s00068-022-02051-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Durant E, Dixon B, Luftig J, Mantuani D, Herring AA. Ultrasound-guided serratus plane block for ED rib fracture pain control. Am J Emerg Med. 2017;35:197.e3–6. doi: 10.1016/j.ajem.2016.07.021. doi: 10.1016/j.ajem.2016.07.021. [DOI] [PubMed] [Google Scholar]