ABSTRACT
Background and Aim:
This study evaluates the effectiveness of long-acting antihypertensive drugs (clonidine and enalaprilat) in blunting the intubation response. Also, the study seeks to determine how effectively clonidine and enalaprilat can maintain stable haemodynamics during a change in position.
Methods:
After ethical committee approval and trial registration, a double-blinded, randomised controlled trial was conducted with 71 consenting patients scheduled for elective spine surgery in a prone position under general anaesthesia. Group C received clonidine 2 μg/kg, and Group E received enalaprilat 1.25 mg diluted in normal saline as an intravenous infusion given over 10 min before induction of anaesthesia. The changes in heart rate (HR) and blood pressure (BP) in response to the infusion of the study drugs, induction, tracheal intubation and change in position were recorded. P value <0.05 was considered significant. Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) version 25.
Results:
Clonidine infusion caused a significant fall in heart rate post-infusion and post-induction with propofol (p value <0.05). Both clonidine and enalaprilat caused a significant fall in mean arterial pressure (MAP) post-infusion and post-induction (p value <0.05). Clonidine effectively blunted the intubation response with no increase in HR and MAP following intubation. Enalaprilat caused a significant rise in HR in response to intubation. On proning, there was a significant fall in MAP in both groups.
Conclusion:
Clonidine is effective in blunting the intubation response. Preoperative infusion of clonidine and enalaprilat causes hypotension during a change of position.
Keywords: Clonidine, enalaprilat, haemodynamics, intubation, prone position, spine surgery
INTRODUCTION
General anaesthesia with tracheal intubation is the most common mode of anaesthesia practised for lumbar spine surgeries.[1] Hypotensive drugs are often required during tracheal intubation to blunt the intubation response and during deliberate hypotension to maintain a bloodless surgical field.[2] Various pharmacological agents are used to alleviate the haemodynamic response to intubation, like fentanyl 2 μg/kg, sufentanil 1–2 μg/kg, clonidine 2 μg/kg, dexmedetomidine 0.5–1 μg/kg, and esmolol 1.5–2 mg/kg.[3,4] Clonidine is an α2-agonist that binds selectively to presynaptic α2-adrenergic receptors.[5,6] Of the many pharmaceutical agents used for alleviating intubation response, clonidine is unique as it has a long half-life. Another long-acting hypotensive agent is enalaprilat, an angiotensin-converting enzyme (ACE) inhibitor. Enalaprilat is the only ACE inhibitor that can be administered intravenously.
The main objective of the study was to analyse the efficacy of two long-acting hypotensive agents, intravenous (IV) clonidine (2 μg/kg) and enalaprilat (1.25 mg), in attenuating the increase in heart rate (HR) and blood pressure (BP) following intubation. In addition, the study aimed to analyse the changes in HR and BP following the administration of the study drug post-infusion, post-induction with propofol, during the shift from a supine to a prone position and in the intraoperative period.
METHODS
This double-blinded, randomised controlled trial was conducted from April to December 2019 in a tertiary care teaching hospital. The institutional ethics committee (IEC SRM MCH RC, No. 1417, dated 27th June 2018) approved the study, and it was registered under the Clinical Trial Registry - India (CTRI/2019/03/017893, https://ctri.nic.in/). The study was conducted in accordance with the ethical guidelines outlined in the Declaration of Helsinki, 2013. Patients of both sexes and of the American Society of Anesthesiologists (ASA) physical status I and II, aged 18–65 years, and scheduled for lumbar discectomy were recruited. Patients with body mass index (BMI) >30 kg/m2, those having diabetes mellitus with autonomic dysfunction, those with hypertensive, cardiopulmonary, hepatorenal, cerebrovascular, or psychiatric diseases, patients on tricyclic antidepressants, and patients with difficult airway were excluded from the study. On satisfying the inclusion and exclusion criteria, patients were informed about the anaesthetic techniques and the study methodology. A written informed consent was collected, granting permission for their involvement in the research and for utilisation of patient data for research and educational purposes.
Patients were randomly assigned into two groups using computer-generated random numbers. Group C received clonidine, while group E received enalaprilat. Allocation concealment was done using a serially numbered, opaque, sealed envelope technique. Patients, anaesthesiologists who administered the bolus infusion and those who recorded the observations for analysis were blinded.
Before arrival in the operating room (OR), no preoperative sedatives were administered to the patients. Patients were shifted to the preoperative holding area, where an intravenous line was secured. Three-lead electrocardiogram (ECG), pulse oximetry and non-invasive blood pressure (NIBP) were applied to assess the physiological parameters. Baseline values were recorded. Strip for assessing bispectral index (BIS) monitoring was attached to the forehead. While waiting in the preoperative holding area, patients received IV 10 ml/kg lactated Ringer’s solution. Patients in group C were administered IV clonidine 2 μg/kg, diluted in 50 ml of normal saline and infused over 10 min. On the other hand, patients in group E received IV enalaprilat at a dosage of 1.25 mg, also diluted in 50 ml of normal saline and administered over 10 min.
Continuous monitoring was maintained throughout the patients’ transfer to the OR. In the OR, ECG, NIBP, pulse oximetry and end-tidal carbon dioxide (EtCO2) were attached. After adequate preoxygenation, general anaesthesia was induced using IV fentanyl 2 μg/kg, propofol 2 mg/kg and vecuronium 0.1 mg/kg. Trachea was intubated with a flexometallic endotracheal tube of appropriate size, which was performed by the same investigator each time. Haemodynamic responses to induction with an anaesthetic agent and intubation were recorded. A positive intubation response was defined as an increase in HR or mean arterial pressure (MAP) of more than 20% above the baseline values.
Ventilation was sustained utilising an anaesthesia workstation, Carestation 660 (General Electric company, Chicago, IL, USA), with sevoflurane, oxygen and nitrous oxide (30:70 ratio) at a fresh gas flow of 1 l/min. Ventilation parameters were adjusted to target EtCO2 levels between 35 and 45 mmHg. IV fentanyl infusion (1–2 μg/kg/h) was used for analgesia, and IV vecuronium (0.01–0.015 mg/kg) was supplemented every 15–20 min as and when needed. Patients were placed in a prone position. Haemodynamic variables upon changing to the prone position were recorded for evaluation. The minimum alveolar concentration (MAC) of sevoflurane was adjusted from 0.5 and 2 MAC to maintain a BIS value between 40 and 50 during the surgery. Fluids were administered according to the Holliday–Segar rule, with a 5 ml/kg/h allowance for third space loss. Blood loss was replaced with crystalloids or blood as appropriate, with the decision left to the physician’s discretion. Volatiles were stopped at the end of the procedure. After confirming spontaneous breathing, reversal of the residual neuromuscular block was achieved by administering neostigmine 2.5 mg and glycopyrrolate 0.5 mg. A sustained 5-s head lift and a train-of-four (TOF) ratio of 0.9 were confirmed before extubation. Patients were transferred to the recovery room for continuous monitoring.
A systolic BP of ≥160 mmHg, diastolic BP of ≥100 mmHg or two consecutive BP values greater than 20% above baseline were defined as hypertensive responses. Hypertensive episodes were treated initially by increasing the MAC of sevoflurane to a maximum of two. If the high BP was not controlled by increasing the MAC of sevoflurane, nitroglycerin infusion was started. Hypotension or haemodynamic instability was defined as an MAP ≤60 mmHg or two consecutive systolic or diastolic BP values ≤20% of the baseline. A hypotensive episode was initially treated with a 5 ml/kg fluid bolus; if the response was not adequate, then IV ephedrine 6 mg bolus was given.
Baseline HR and BP and variation in HR and BP between groups post-infusion of clonidine 2 μg/kg and enalaprilat 1.25 mg, post-induction, postintubation, and pre- and post-proning were recorded in both the groups. The primary outcome was to determine the change in HR and BP in response to intubation. The secondary outcomes were the changes in HR in response to the infusion of study drugs during induction, proning and surgery. The surgical field was graded on a 5-point Likert scale, with 1 indicating a bloody field with severe bleeding and 5 an excellent field with no bleeding.
The sample size was estimated using the mean HR recorded 3 min after intubation in the pilot study. The mean HR and standard deviation (SD) obtained 3 min after intubation in the clonidine and enalaprilat groups were μ1 = 77.10 and μ2 = 91.69 and s1 = 7.73 s2 = 8.57, respectively. With an α error of 0.05 and a β error of 0.8, a sample size (n) of 31 was determined for each group. With 10% non-response, a sample size of 35 participants was decided to be included in the study in each group. The statistical analysis was performed using the IBM Statistical Package for the Social Sciences (SPSS) statistics software (version 25.0; IBM Corp., Armonk, NY, USA). Continuous measurements were reported as mean ± SD, and categorical measurements were reported as number (%). No outliers were detected when testing the variances of the two samples. The normality of the data was assessed by conducting the Kolmogorov–Smirnov test. Intragroup comparisons were analysed using paired t-test, and intergroup comparisons were analysed using Student’s unpaired t-test. Categorical variables were tested using the Chi-squared test. A P value <0.05 was regarded as statistically significant.
RESULTS
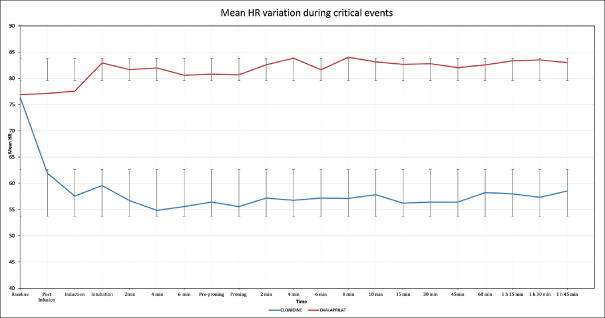
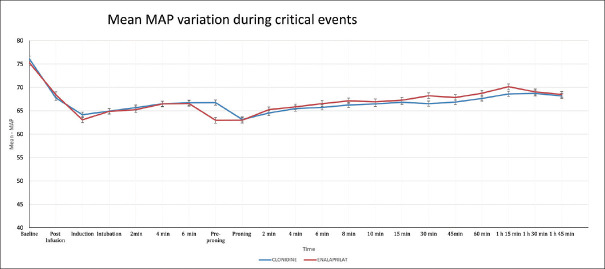
The distribution of patients in the two groups is shown in Figure 1. Both groups were comparable in their demographic data [Table 1]. The total duration of the surgery was comparable between the groups (P-Value >0.05). The patients who received clonidine infusion experienced a significant reduction in HR from baseline and after induction with propofol [Figure 2]. There was no significant alteration in HR from baseline or after induction in patients who received enalaprilat. A significant increase in HR was observed during tracheal intubation in patients who received enalaprilat. Patients in both groups had no significant change in HR on proning. Also, they experienced a significant reduction in MAP from baseline and on induction with propofol [Figure 3]. Both groups had no significant alteration in MAP in response to intubation. A significant fall in MAP on proning was noticed in both groups. Haemodynamics remained stable during the rest of the intraoperative period. The grading of the surgical field was found to be comparable between the groups (4.37 ± 0.48 in group C and 4.41 ± 0.49 in group E, P value 0.04, 95% confidence interval [CI] −0.90 to 0.27).
Figure 1.
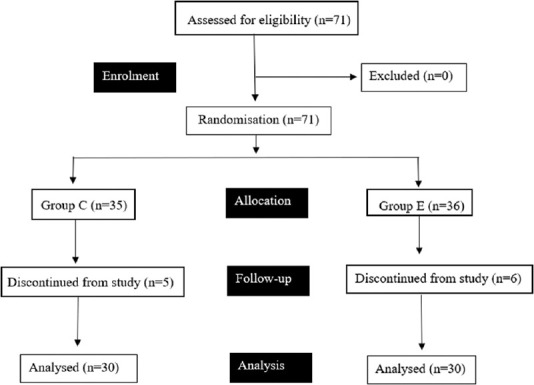
Flow of participants in the study
Table 1.
Demographic data for group C and group E
| Characteristics | Group C (n=35) | Group M (n=36) |
|---|---|---|
| Age (years) | 42.09±10 | 43.03±13.47 |
| Male/female (n) | 21/9 | 20/10 |
| BMI (kg/m2) | 23.34±2.34 | 24.07±3.78 |
| ASA I/II | 20/10 | 19/11 |
| Duration of surgery (min) | 95.5±7.9 | 94.5±8.1 |
Data presented as mean±standard deviation or number (n) or number. ASA=American Society of Anesthesiologists, BMI=body mass index
Figure 2.
Heart rate variation between group C and group E. HR-Heart rate
Figure 3.
Mean arterial pressure variation between group C and group E. MAP-Mean arterial pressure
DISCUSSION
The study findings demonstrate that clonidine effectively attenuates the rise in HR and MAP upon tracheal intubation. On the other hand, enalaprilat is only partially effective as it causes an increase in HR, but no similar increase in BP. In addition, both drugs were found to cause a decrease in MAP when patients were prone.
Clonidine acts on the central α-receptors to decrease sympathetic flow, reducing peripheral vascular resistance, HR and BP. ACE inhibitors block the enzyme converting angiotensin I to angiotensin II, a potent vasoconstrictor.[7] Enalaprilat at a dose of 1.0–2.5 mg is used in high renin hypertensive emergencies, especially those associated with congestive cardiac failure.[8,9] Studies by Chatrapati and Shitole,[10] Aanchal et al.[11] and Acharya and Routray[12] also reported that infusion of clonidine is effective in blunting the intubation response, as seen by the absence of a significant increase in HR. Interestingly, when ACE inhibitors are used for treating hypertension, there is no associated reflex tachycardia. However, we found an increase in HR in response to intubation. This could be due to the increased level of bradykinin that is known to be induced by ACE inhibitors. Bradykinin can cause pain by directly stimulating pain neurons and releasing substance P.[13] We propose that the already painful intubation response would be further exacerbated by bradykinin, which could explain the increase in HR associated with enalaprilat.
Upon proning, both groups experienced a significant decrease in MAP. The incidence of hypotension was studied by Manohar et al.[14] in patients operated on for decompressive laminectomy in the prone position. Using a non-invasive cardiac output monitor, they found a 60% incidence of hypotension in patients with cervical myelopathy under anaesthesia. This was attributed to the combined effects of anaesthesia, cervical cord compression, prone positioning and autonomic nervous system dysfunction. In a systematic review on ‘prone position during surgery and its complications’ conducted by Kwee et al.,[15] cardiovascular compromise was reported upon shifting to the prone position in the form of decreased stroke volume, cardiac index and low BP. Patients in both groups had minimal blood loss. The surgeon’s assessment of the surgical fields was also comparable between the groups, with the responses showing very good or excellent fields. Our study results are similar to those of Jiwanmall et al.,[16] who assessed the surgical field and reported that clonidine is an excellent agent for hypotensive anaesthesia.
Our study has limitations that should be considered when interpreting the results. Firstly, we could not find any study that reported equipotent doses of the study drugs. Also, our study’s sample size was small, limiting our findings’ generalisability. Furthermore, a significant gap exists in the the literature regarding enalaprilat which necessiates further reasearch on enalaprilat as the only ACE inhibitor available for IV use in hypotensive anaesthesia. Overall, our study highlights the need for further research in this area to understand the optimal use of ACE inhibitors in hypotensive anaesthesia better.
CONCLUSION
Clonidine effectively blunts the rise in HR and BP, while enalaprilat is ineffective in blunting the increase in HR following tracheal intubation. In addition, although the infusion of clonidine or enalaprilat is effective in maintaining stable haemodynamics during the intraoperative period, both drugs produced significant falls in MAP on proning. Therefore, administering long-acting hypotensive medications such as clonidine and enalaprilat before surgery to mitigate intubation response is not recommended for patients in a prone position undergoing lumbar spine surgery, as it carries potential risks.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Pavithran P, Renuka S, Pramod SK, Salin E, Biju S, Kishore K. Comparison of the thoracolumbar interfascial plane block with local anaesthetic infiltration in lumbar spine surgeries –A prospective double-blinded randomised controlled trial. Indian J Anaesth. 2022;66:436–41. doi: 10.4103/ija.ija_1054_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rastogi B, Gupta K, Gupta PK, Agarwal S, Jain M, Chauhan H. Oral pregabalin premedication for attenuation of the haemodynamic pressor response of airway instrumentation during general anaesthesia: A dose-response study. Indian J Anesth. 2012;56:49–54. doi: 10.4103/0019-5049.93344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Savitha KS, Dhanpal R, Vikram MS. Haemodynamic responses at intubation, change of position, and skin incision: A comparison of multimodal analgesia with the conventional analgesic regime. Anesth Essays Res. 2017;11:314–20. doi: 10.4103/0259-1162.194556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bafna U, Sharma P, Singhal RK, Gurjar SS, Bhargava SK. Comparison of hypotensive properties of dexmedetomidine versus clonidine for induced hypotension during functional endoscopic sinus surgery: A randomised, double-blind interventional study. Indian J Anaesth. 2021;65:579–85. doi: 10.4103/ija.IJA_57_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rajaprabu T, Kumar V. Comparison between the haemodynamic stability of dexmedetomidine and clonidine infusions among patients undergoing laparoscopic cholecystectomy- A randomised controlled trial. Indian J Clin Anaesth. 2019;6:437–40. [Google Scholar]
- 6.Mahajan L, Kaur M, Gupta R, Aujla KS, Singh A, Kaur A. Attenuation of the pressor responses to laryngoscopy and endotracheal intubation with intravenous dexmedetomidine versus magnesium sulphate under bispectral index-controlled anaesthesia: A placebo-controlled prospective randomised trial. Indian J Anaesth. 2018;62:337–43. doi: 10.4103/ija.IJA_1_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oliveira-Paula GH, Lacchini R, Luizon MR, Fontana V, Silva PS, Biagi C, et al. Endothelial nitric oxide synthase tagSNPs influence the effects of enalapril in essential hypertension. Nitric Oxide. 2016;55-56:62–9. doi: 10.1016/j.niox.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 8.Faisal M, Cawello W, Laeer S LENA Consortium. Clinical pharmacokinetics of enalapril and enalaprilat in pediatric patients—A systematic review. Front Pediatr. 2021;9:611322. doi: 10.3389/fped.2021.611322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laeer S, Cawello W, Burckhardt BB, Ablonczy L, Bajcetic M, Breur JM, et al. Enalapril and enalaprilat pharmacokinetics in children with heart failure due to dilated cardiomyopathy and congestive heart failure after administration of an orodispersible enalapril minitablet (LENA-Studies) Pharmaceutics. 2022;14:1163. doi: 10.3390/pharmaceutics14061163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chatrapati S, Shitole AB. Efficacy of intravenous clonidine to attenuate cardiovascular stress response to laryngoscopy and tracheal intubation –A prospective randomised, double-blind study. Int J Contemp Med Res. 2016;3:1462–6. [Google Scholar]
- 11.Aanchal K, Asha T, Nabi N, Sethi AK. Comparison of clonidine and dexmedetomidine for attenuation of laryngoscopy and intubation response –A randomised controlled trial. J Clin Anesth. 2016;33:283–8. doi: 10.1016/j.jclinane.2016.04.026. [DOI] [PubMed] [Google Scholar]
- 12.Acharya N, Routray D. A prospective randomised study of efficacy of clonidine in attenuating haemodynamic response to laryngoscopy and tracheal intubation. Ann Int Med Dent Res. 2017;3:30–4. [Google Scholar]
- 13.Yagi A, Ichikawa S, Sakamaki T, Ono Z, Sato K, Nakamura T, et al. Role of norepinephrine in the lack of reflex tachycardia after angiotensin converting enzyme inhibitor treatment. Tohoku J Exp Med. 1992;166:429–37. doi: 10.1620/tjem.166.429. [DOI] [PubMed] [Google Scholar]
- 14.Manohar N, Ramesh VJ, Radhakrishnan M, Chakraborti D. Haemodynamic changes during prone positioning in anaesthetised chronic cervical myelopathy patients. Indian J Anaesth. 2019;63:212–7. doi: 10.4103/ija.IJA_810_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kwee MM, Ho YH, Rozen WM. The prone position during surgery and its complications: A systematic review and evidence-based guidelines. Int Surg. 2015;100:292–303. doi: 10.9738/INTSURG-D-13-00256.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jiwanmall M, Joselyn AS, Kandasamy S. Intravenous clonidine as a part of balanced anaesthesia for controlled hypotension in functional endoscopic sinus surgery: A randomised controlled trial. Indian J Anaesth. 2017;6:418–23. doi: 10.4103/ija.IJA_58_17. [DOI] [PMC free article] [PubMed] [Google Scholar]