Abstract
The emergence of cases of so-called “chronic brain death” seems to undermine the biophilosophical justification of brain death as true death, which was grounded in the idea that death entails the loss of integration of the organism. Severely neurologically damaged patients who can persist for years with proper support seem to be integrated organisms, and common sense suggests that they are not dead. We argue, however, that mere integration is not enough for an organism to be alive, but that living beings must be substantially self-integrating (i.e., a living organism must itself be the primary source of its integration and not an external agent such as a scientist or physician). We propose that irreversible apnea and unresponsiveness are necessary but not sufficient to judge that a human being has lost enough capacity for self-integration to be considered dead. To be declared dead, the patient must also irrevocably have lost either (1) cardiac function or (2) cerebrosomatic homeostatic control. Even if such bodies can be maintained with sufficient technological support, one may reasonably judge that the locus of integration effectively has passed from the patient to the treatment team. While organs and cells may be alive, one may justifiably declare that there is no longer a substantially autonomous, whole, living human organism. This biophilosophical conception of death implies that the notion of brain death remains viable, but that additional testing will be required to ensure that the individual is truly brain dead by virtue of having irrevocably lost not only the capacity for spontaneous respiration and conscious responsiveness but also the capacity for cerebrosomatic homeostatic control.
The major reason for rethinking brain death is the phenomenon dubbed “chronic brain death” (CBD) prominently exemplified by Jahi McMath, who lived for more than 4 years after being declared brain dead.1-3 During this time, she underwent puberty. Insisting that such an individual was dead for 4 years seems unreasonable. The recognition of such cases has led to a variety of suggestions for revising the Uniform Determination of Death Act (UDDA), such as (1) tightening the criteria for diagnosis or (2) abandoning the idea of brain death.4
Some commentators have urged a third approach, changing the definition of brain death to fit current testing protocols.4-6 This seems unreasonable. Were a test for multiple sclerosis to give too many false positives, neurologists would not change the definition of multiple sclerosis; they would improve testing. Similarly, if our clinical tests for brain death result in too many false positives, we should improve our testing, not change the definition of death.
Death ought not to be something physicians define by consensus. Physicians can, and should, set testing standards, but these standards should be based on a biophilosophical conception of death—one that (1) encompasses ordinary cardiopulmonary death and neurologic death, (2) is widely accepted, (3) objective, and (4) works for any biological species.7,8 Such a conception was implicit in the work of the President's Commission9 and in the original UDDA.10 That standard was the loss of integration, founded on the belief that the brain was essential for the organismal unity of the body.11 The challenges raised by CBD, however, require refining that conception.
A Biophilosophically Informed Standard for Determining Organismal Death
We therefore propose a revised, biophilosophically informed standard for the determination of death, a conception that makes clear that living organisms are not just integrated, but self-integrating:
An organism that is judged to have irrevocably lost the fundamental capacity to be a substantially self-integrating individual member of its biological kind can be declared dead.
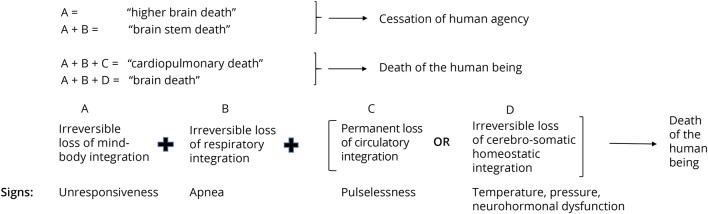
This organismal conception of death works for an ameba, a human being, and anything in between. Notably, however, the capacity for organismal self-integration becomes more complex up the evolutionary ladder. As shown in Figure 1, for human beings, we suggest that there are 4 fundamental functional sources of self-integration at the organismal level: mind-body integration, respiration, circulation, and cerebral homeostatic control.
Figure 1. Fundamental Spheres of Human Organismal Self-Integration.
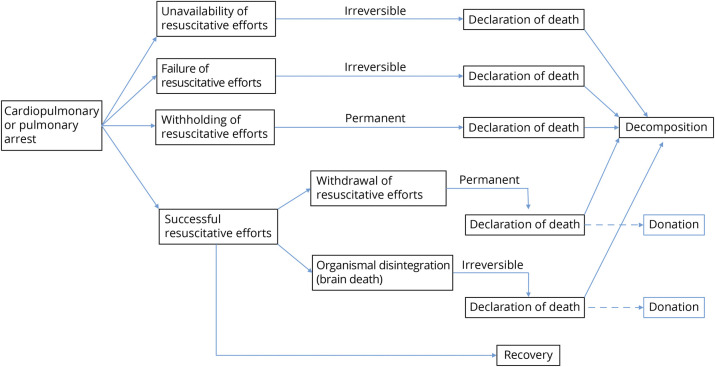
Given this conception of organismal death and the delineation of these 4 fundamental sources of human capacity for organismal self-integration, we submit the determination of death is a threshold concept12 that can be met when 2 necessary conditions plus 1 additional condition are satisfied (Figure 2).
Necessary conditions: (A) the irrevocable loss of conscious responsiveness and (B) the irrevocable loss of respiratory drive.
Additional conditions: either (C) the permanent cessation of circulation or (D) the irrevocable loss of cerebral homeostatic control.
Figure 2. Proposed Criteria for Death Regarding Fundamental Human Capacities for Organismal Self-Integration.
A + B + C maps to the cardiopulmonary death—an unresponsive, breathless, and pulseless patient. A + B + D maps to what was originally intended by whole brain death8—an unresponsive, centrally apneic patient with sufficient destruction of the brain such that cerebral homeostasis has been disrupted. Patients meeting either conditions A + B + C or A + B + D can be judged to have lost the fundamental capacity to be substantially self-integrating individual members of the human natural kind.
In an Aristotelian sense, human beings are rational animals.13 Loss of mind-body integration entails the loss of the rational, yet this loss alone only renders the patient damaged, not dead. Proponents of a “higher brain” standard of death would say that such individuals have died as persons.14 Yet they have not died as substantially self-integrating organisms. What additional functions must be lost before a human being can be declared dead? Certainly the loss of respiration seems necessary. Respiration is an animal's fundamental mode of interaction with its environment. Respiration, obtaining oxygen and dispelling carbon dioxide, is what permits metabolism. Respiration is also steeped in human symbolic history as a cardinal sign of life.
How Much Self-Integration Must Be Lost?
Yet, is the irrevocable loss of both conscious responsiveness and the ability to breathe sufficient to declare someone dead? Some observers, including some who agree that death entails the loss of the capacity for self-integration have asserted that that these conditions suffice,15 but it does not seem reasonable to say so. Common sense suggests that Jahi McMath was not dead. Likewise, a patient with postcoma wakeful unresponsiveness and a phrenic nerve injury is not dead. Both are cases of severely brain injured patients who irreversibly lack conscious responsiveness and cannot breathe independently. Yet such patients retain sufficient capacity for organismal self-integration that they could persist for prolonged periods with little support. Something more must be lost before one could reasonably declare a human being dead. We suggest that the threshold for having lost sufficient organismal self-integrative capacity to be declared dead is crossed by the additional loss of either cardiac function or cerebral homeostatic control.
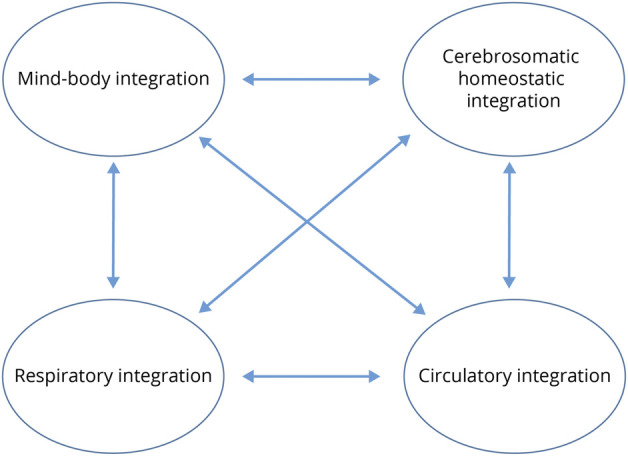
The disruptive technology that initially provoked questions about the declaration of death was mechanical ventilation. Ventilators gave physicians the ability to resuscitate individuals who otherwise would have been declared dead very quickly after a pulmonary or cardiopulmonary arrest.16 As shown in Figure 3, most humans still die without resuscitation. Where advanced resuscitation is available, humans may also now die by the failure of resuscitative efforts, or, given the proper justifying conditions, by forgoing resuscitation. The notion of brain death arose in response to a related question: could some patients also be declared dead despite resuscitation?
Figure 3. Paths to Death in Light of the Technical Medical Capacity for Resuscitation.
This was the question of the late 1950s, the one that led to the idea of brain death. Are there individuals who persist on ventilators but are so damaged and require so much support that they are no longer self-integrating human organisms? When the locus of organismal integration becomes not the individual, but the treatment team, it would seem that such a threshold has been crossed. An individual who is unresponsive and apneic but has also lost cerebral homeostatic control, as manifested by blood pressure and temperature instability, diabetes insipidus, lack of cerebral control over the hormones responsible for growth, metabolism, and sexual development and function, is no longer reasonably considered to be self-integrating.8 The locus of integration has become the health care team that supplies all these functions artificially. Notably, current scientific understanding associates most of these functions with the hypothalamus. Moreover, because thalamic function supports at least rudimentary consciousness, and cannot be tested directly, one can be more confident that the potential for consciousness has been lost if the functions of the adjacent hypothalamus have been disrupted. Thus, by the organismal standard we are proposing, an individual who has lost these functions in addition to having lost conscious responsiveness and respiratory drive can be declared dead.
This is not to say that all integrative functions of the body have ceased but rather that fundamental self-integration at the level of the organism has ceased. Cells continue to metabolize. Individual organs and organ subsystems continue to function. Some hormonal, spinal cord, and peripheral autonomic functions persist.17 But these do not suffice for declaring the patient alive as a substantially self-integrating individual organism. The distinction between organismal death and organ/cellular death is what makes transplantation possible.
Practically, this analysis would require either adding a direct assessment of cerebral homeostatic control to the clinical criteria used to determine brain death or additional testing to ensure that the all the critical integrative functions of the brain, including those of the hypothalamus, have been irrevocably damaged.8 Whether this includes physiologic assessment, endocrinologic testing, and/or improved evaluation of cerebral circulation are matters for scientific debate.18-22 Absent evidence of the loss of cerebral homeostatic control of the body, however, the individual could not be declared dead by neurologic criteria.
Because the early cases of brain death all exhibited very severe damage, explicit hypothalamic testing was superfluous: apnea and the absence of consciousness and brain stem reflexes were assumed to be sufficient to diagnose death of the entire brain, including the hypothalamus. These individuals all displayed signs of neurohormonal and autonomic instability, and thus it became the common understanding that none could persist long even with maximal support.23-29 Cases of CBD only emerged later because the scope of cases widened and the capabilities of intensive care units increased. Current diagnostic testing standards do not rule out persistent hypothalamic function.
Potential Counterarguments
What are the counterarguments against requiring evidence of cerebral homeostatic dysfunction before the declaration of brain death? One is that neurologists have arrived at a consensus on standards for determining brain death and simply to assert, “that's not how we do it.”5,6 Such an assertion, however, is neither biomedically satisfying nor philosophically adequate. Praxis ought to follow a definition; praxis does not constitute the definition. No one is dead simply because someone has decided to call them dead.
Others have questioned whether the hypothalamus should be considered part of the brain,5,30 have downplayed the importance of hypothalamic function,6,31,32 or have admitted that those declared brain dead yet evidencing hypothalamic function are not really dead, but “dead enough” to be organ donors.33 Yet it seems wrongheaded to rewrite neuroanatomy to advance a definition of death. Moreover, denigrating the importance of the hypothalamus suggests an implicit commitment to a higher brain conception of death. The metabolic and autonomic integrative functions subserved by the hypothalamus are critical to life.
A third argument is to observe that the modification we suggest will result in fewer people being declared brain dead and therefore diminish the supply of organs.34 This not an adequate response. First, a good motive does not make an action right. Second, such arguments provide fodder for the deep and widely held (but historically questionable) public suspicion that brain death is not real death but something doctors “made up” to facilitate organ transplantation.35 Third, the impact on organ donation might not be as great as imagined. Profoundly neurologically injured individuals who are not brain dead could still be organ donors by donation after circulatory determination of death (DCDD). Success rates in heart transplantation after DCDD are improving rapidly.36
Last, one might suggest that our proposal is arbitrary. Why not just declare someone dead when they have permanently lost consciousness? Our proposal, however, is far from arbitrary. It comports with common sense. It includes as necessary the widely accepted conditions of apnea and loss of conscious responsiveness. Of importance, it grounds the judgment of sufficiency in a biophilosophical conception of death—that living organisms are substantially self-integrating. A human being who is irreversibly unconscious and dependent on a ventilator but can maintain her own blood pressure, thermoregulation, sodium balance, growth, and metabolism is still substantially self-integrating and therefore not dead.
Conclusion
Death is not a neurologic state of a living human being—it is the end of a human life. The emergence of cases of CBD therefore necessitates a re-examination of what is required to judge a human being to be dead by neurologic criteria. The original philosophical conception of death that was used to justify the notion of brain death, the loss of integration at the organismal level, still stands. The irrevocable loss of the critical organismically integrative functions of the brain meets that standard. What the cases of CBD demonstrate, however, is that certain functions that are fundamental to organismal integration persist in some patients diagnosed as brain dead by current clinical standards, allowing them to continue to live for long periods with minimal support. From this, it follows that additional testing will be required to assure that all the critical integrative functions of the brain have ceased if the determination of brain death is to be accurate. Against those who would argue that the emergence of cases of CBD refutes the notion that these patients have lost organismal integrative function, we have argued that that the mere passive persistence of integration is not sufficient for being a living organism. The cells of a tissue culture are alive in this sense and even communicate and exhibit rudimentary integration. But a tissue culture is not a living organism. The source of integration in a living organism should originate substantially within the organism itself, not in the acts of a scientist or a physician. One must then judge when the threshold has been reached for saying that the locus of organismal integration has substantially passed from the patient to the medical care team. We have argued that patients who have irrevocably lost the fundamental capacity for mind-body integration, respiratory drive, and cerebral homeostatic control have lost sufficient self-integration that they can be judged to have died. Thus, there is such a thing as brain death, but it requires more than apnea and the loss of conscious responsiveness to determine it. We do not need to abandon the concept of brain death—we just need to improve our testing.
Glossary
- CBD
chronic brain death
- DCDD
donation after circulatory determination of death
- UDDA
Uniform Determination of Death Act
Appendix. Authors
Study Funding
The authors report no targeted funding.
Disclosure
All authors report no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
References
- 1.Shewmon DA. Chronic “brain death”: meta-analysis and conceptual consequences. Neurology. 1998;51(6):1538-1545. doi: 10.1212/wnl.51.6.1538 [DOI] [PubMed] [Google Scholar]
- 2.Shewmon DA, Salamon N. The extraordinary case of Jahi McMath. Perspect Biol Med. 2021;64(4):457-478. doi: 10.1353/pbm.2021.0036 [DOI] [PubMed] [Google Scholar]
- 3.Aviv R. What does it mean to die? The New Yorker, February 5, 2018. Accessed May 24, 2023. newyorker.com/magazine/2018/02/05/what-does-it-mean-to-die.
- 4.Truog RD. The uncertain future of the determination of brain death. JAMA. 2023;329(12):971-972. doi: 10.1001/jama.2023.1472 [DOI] [PubMed] [Google Scholar]
- 5.Lewis A, Bonnie RJ, Pope T, et al. Determination of death by neurologic criteria in the United States: the case for revising the Uniform Determination of Death Act. J Law Med Ethic. 2019;47(4_suppl):9-24. doi: 10.1177/107311051989803 [DOI] [PubMed] [Google Scholar]
- 6.Omelianchuk A, Bernat J, Caplan A, et al. Revise the Uniform Determination of Death Act to align the law with practice through neurorespiratory criteria. Neurology. 2022;98(13):532-536. doi: 10.1212/WNL.0000000000200024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bernat JL. The biophilosophical basis of whole-brain death. Soc Philos Policy. 2002;19(2):324-342. doi: 10.1017/s0265052502192132 [DOI] [PubMed] [Google Scholar]
- 8.Sulmasy DP. Whole-brain death and integration: realigning the ontological concept with clinical diagnostic tests. Theor Med Bioeth. 2019;40(5):455-481. doi: 10.1007/s11017-019-09504-w [DOI] [PubMed] [Google Scholar]
- 9.President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Defining Death: A Report on the Medical, Legal, and Ethical Issues in the Determination of Death. U.S. Government Printing Office; 1981. [Google Scholar]
- 10.National Conference of Commissioners on Uniform State Laws. Uniform Determination of Death Act. Uniform Law Commission; 1980. [Google Scholar]
- 11.Bernat JL. The whole-brain concept of death remains optimum public policy. J Law Med Ethics. 2006;34(1):35-43, 3. doi: 10.1111/j.1748-720X.2006.00006.x [DOI] [PubMed] [Google Scholar]
- 12.Meier LJ. The demise of brain death. Br J Philos Sci. 2022;73:487-508. [Google Scholar]
- 13.Aristotle. De anima 414b18-19, 415a7-8; De partibus animalium 641b7f; Politica 1332b3-5. In: McKeown R, editor. The Basic Works of Aristotle. Random House; 1947. [Google Scholar]
- 14.Green MB, Wikler D. Brain death and personal identity. Philos Public Affair. 1980;9(2):105-133. [PubMed] [Google Scholar]
- 15.Moschella M. Deconstructing the brain disconnection-brain death analogy and clarifying the rationale for the neurological criterion of death. J Med Philos. 2016;41(3):279-299. doi: 10.1093/jmp/jhw006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Belkin GS. Death Before Dying: History, Medicine, and Brain Death. Oxford University Press; 2014. [Google Scholar]
- 17.Shewmon DA. The brain and somatic integration: insights into the standard biological rationale for equating “brain death” with death. J Med Philos. 2001;26(5):457-478. doi: 10.1076/jmep.26.5.457.3000 [DOI] [PubMed] [Google Scholar]
- 18.Halevy A. Beyond brain death? J Med Philos. 2001;26(5):493-501. doi: 10.1076/jmep.26.5.493.3004 [DOI] [PubMed] [Google Scholar]
- 19.Bioethicists of the Pellegrino Center for Clinical Bioethics. Proposal for revising the uniform definition of death act. Hastings Center Forum, February 18, 2022. Accessed May 24, 2023. thehastingscenter.org/defining-brain-death/.
- 20.Bohatyrewicz R, Pastuszka J, Walas W, et al. Implementation of computed tomography angiography (CTA) and computed tomography perfusion (CTP) in Polish guidelines for determination of cerebral circulatory arrest (CCA) during brain death/death by neurological criteria (BD/DNC) diagnosis procedure. J Clin Med. 2021;10(18):4237. doi: 10.3390/jcm10184237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sawicki M, Sołek-Pastuszka J, Chamier-Ciemińska K, Walecka A, Walecki J, Bohatyrewicz R. Computed tomography perfusion is a useful adjunct to computed tomography angiography in the diagnosis of brain death. Clin Neuroradiol. 2019;29(1):101-108. doi: 10.1007/s00062-017-0631-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rady MY. Neuroimaging of intracranial perfusion and the clinical diagnosis of brain death: setting the gold standard in humans. Clin Neuroradiol. 2019;29(3):575-577. doi: 10.1007/s00062-019-00806-z [DOI] [PubMed] [Google Scholar]
- 23.Novitsky D, Wicomb WN, Cooper DK, Rose AG, Fraser RC, Barnard CN. Electrocardiographic, hemodynamic, and endocrine changes during experimental brain death in the Chacma baboon. J Transplant. 1984;4:63-69. [Google Scholar]
- 24.Mollaret P, Bertrand I, Mollaret H. Previous coma and necrosis of the central nervous system [in French]. Rev Neurol (Paris). 1959;101:116-139. [PubMed] [Google Scholar]
- 25.Murray JE. Organ transplantation: the practical possibilities. In: Gordon Wolstenholme G, O'Connor M, editors. Law and Ethics in Medical Progress. JA Churchill; 1968:54-77. [Google Scholar]
- 26.Drory Y, Ouaknine G, Kosary IZ, Kellermann JJ. Electrocardiographic findings in brain death; description and presumed mechanism. Chest. 1975;67(4):425-432. [DOI] [PubMed] [Google Scholar]
- 27.Jennett B, Gleave J, Wilson P. Brain death in three neurosurgical units. Br Med J (Clin Res Ed). 1981;282(6263):533-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bernat JL, Culver CM, Gert B. On the definition and criterion of death. Ann Intern Med. 1981;94(3):389-394. [DOI] [PubMed] [Google Scholar]
- 29.Power BM, Van Heerden PV. The physiological changes associated with brain death: current concepts and implications for treatment of the brain dead organ donor. Anaesth Intensive Care. 1995;23(1):26-36. doi: 10.1177/0310057X9502300107 [DOI] [PubMed] [Google Scholar]
- 30.Lewis A, Bonnie RJ, Pope T. It's time to revise the Uniform Determination of Death Act. Ann Intern Med. 2020;172(2):143-144. doi: 10.7326/M19-2731 [DOI] [PubMed] [Google Scholar]
- 31.Russell JA, Epstein LG, Greer DM, Kirschen M, Rubin MA, Lewis A; Brain Death Working Group. Brain death, the determination of brain death, and member guidance for brain death accommodation requests: AAN position statement. Neurology. 2019;92(5):228-232. doi: 10.1212/WNL.0000000000006750 [DOI] [PubMed] [Google Scholar]
- 32.Truog RD, Fackler JC. Rethinking brain death. Crit Care Med. 1992;20(12):1705-1713. doi: 10.1097/00003246-199212000-00018 [DOI] [PubMed] [Google Scholar]
- 33.Younger SJ. How to communicate clearly about brain death and first person consent to donate. AMA J Ethics. 2016;18(2):108-114. doi: 10.1001/journalofethics.2017.18.2.ecas2-1602 [DOI] [PubMed] [Google Scholar]
- 34.Marcus AD. Doctors and lawyers debate the meaning of “brain death.” Wall Street Journal, December 12, 2022:A3.
- 35.Machado C, Korein J, Ferrer Y, et al. The concept of brain death did not evolve to benefit organ transplants. J Med Ethics. 2007;33(4):197-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kwon JH, Ghannam AD, Shorbaji K, et al. Early outcomes of heart transplantation using donation after circulatory death donors in the United States. Circ Heart Fail. 2022;15(12):e009844. doi: 10.1161/CIRCHEARTFAILURE.122.009844 [DOI] [PubMed] [Google Scholar]