Abstract
Background
The use of health surveys has been key in the scientific community to promptly communicate results about the health impact of COVID-19. But what information was collected, where, when and how, and who was the study population?
Objective
To describe the methodological characteristics used in large health surveys conducted in Spain early on in the COVID-19 pandemic.
Methods
Scoping review. Inclusion criteria: observational studies published between January 2020 and December 2021, with sample sizes of over 2,000 persons resident in Spain. Databases consulted: PubMed, CINAHL, Literatura Latinoamericana y del Caribe en CC de la Salud, Scopus, PsycINFO, Embase, Sociological Abstracts, Dialnet and Web of Science Core Collection. We analyzed the characteristics of the literature references, methodologies and information gathered in the surveys selected. Fifty five studies were included.
Results
Sixty percentage of the studies included had mental health as their main topic and 75% were conducted on the general adult population. Thirteen percentage had a longitudinal design, 93% used the internet to gather information and the same percentage used non-probability sampling. Thirty percentage made some type of sampling correction to reduce coverage or non-response biases, but not selection biases. Sixty seven percentage did not state the availability of their data.
Conclusions
Consistent with the extensive use of non-probability sampling without any bias correction in the extraordinary setting created by COVID-19, quality population frameworks are required so that probability and representative samples can be extracted quickly to promptly address other health crises, as well as to reduce potential coverage, non-response and particularly selection biases by utilizing reweighting techniques. The low data accessibility despite the huge opportunity that COVID-19 provided for Open Science-based research is striking.
Keywords: COVID-19, surveys and questionnaires, mental health, non-probability surveys, reweighting
Introduction
Health surveys are a fundamental support tool for decision-making in health planning. They provide information on magnitude, distribution and trends in health, the social factors that determine them and the use of social services from the population's perspective. They permit identification of the main challenges for prioritizing activity, designing and developing intervention strategies, evaluating and allocating resources, and the main risk groups in terms of health, lifestyles, and access to health services (1).
The highly significant role of surveys for Public Health was greater still with the COVID-19 pandemic due to the urgent requirement for its health impact outcomes to be conveyed (2). This context led the scientific community, regardless of location or area of expertise, to gather information about the pandemic quickly, and here surveys were the key tool. This resulted in the publication of an extremely large number of scientific articles mainly relating to population lockdown and restrictions on mobility (3–9); measures that brought changes and adaptations to the methods and techniques for collecting information through surveys.
In this respect, non-probability surveys conducted with volunteers via the internet proliferated: for example, via websites, mobile apps, and publicity on social media. These types of survey enable statistics to be accessed more rapidly and at the same time provide an inexpensive means of compiling data, although they are subject to selection and coverage biases. This does not happen with probability surveys, often used by health statistics services such as Gold Standard, since they enable valid inferences to be made about the population without having to include hypotheses in models (10, 11). Furthermore, sampling theory based on distribution of probability arising from sample design enables any potential sampling errors in the estimators concerned to be determined and controlled (11).
Prior statistical reweighting is therefore necessary in non-probability sampling in order to obtain valid and precise estimates that eliminate, or at last reduce, these biases (12, 13). In sum, the survey methodology used to compile and analyze information has a direct effect on the quality of the results obtained.
Finally, the use of health surveys has been key in the scientific community to promptly communicate results about the health impact of COVID-19. But what information was collected, where, when and how, and who was the study population? This research question justified the study objective of this work as the performance of a scoping review to describe the methodological characteristics of large health surveys conducted in Spain at the beginning of the COVID-19 pandemic.
Methods
We performed a scoping review (14) using the methodological framework developed by Arksey and O'Malley (15) and the Joanna Briggs Institute (16), and reported in line with PRISMA-ScR guidelines (17). We based our scoping review following the Population, Concept and Context (PCC) format as the research review question (18). Thus, the research review question for the Population was “Spanish surveys,” for the Context was “COVID-19,” and for the Concept was “Survey Methodology.”
The following databases were consulted: PubMed, CINAHL (Ebscohost), Literatura Latinoamericana y del Caribe en CC de la Salud (LILACS), Scopus, PsycINFO (Proquest), Embase (Elsevier), Sociological Abstracts (Proquest), Dialnet and Web of Science Core Collection. We selected biomedical and multidisciplinary databases because most of the surveys during the pandemic were related to social services and according to the following criteria:
Databases with large coverage and large numbers of journals included: Pubmed, Scopus, Embase.
Databases with Spanish journals and articles in Spanish included: LILACS, Scopus, Dialnet.
Databases specializing in health literature: Pubmed, CINAHL, Embase.
Databases specializing in socio-sanitary literature: PsyINFO, Sociological Abstract, WOS, Scopus.
This search was complemented with gray literature information sources: OpenGray (unpublished literature), Gray Literature Report, the University of Oxford Global Directory for COVID surveys (https://supertracker.spi.ox.ac.uk/surveys/) and open searches in Google. The searches were developed between January 2020 and December 2021. These coverage dates of the databases were given by the novelty of the subject, COVID-19. There were no language restrictions. The search strategy was conducted through a combination of controlled terminology (MeSH/Emtree) and free language representative of the concepts COVID-19, surveys, and Spain, and was adapted to the different databases consulted (Table 1).
Table 1.
Search terms (PubMed search strategy).
| 1. (“surveys and questionnaires” [MeSH Terms] OR “health surveys” [MeSH Terms] OR “healthcare survey” [Text Word] OR survey* [Text Word] OR questionnaire* [Text Word] OR interview* [Text Word]) |
| 2. (“COVID-19” [All Fields] OR “COVID-19” [MeSH Terms] OR “COVID-19 vaccines” [All Fields] OR “COVID-19 vaccines” [MeSH Terms] OR “COVID-19 serotherapy” [All Fields] OR “COVID-19 serotherapy” [Supplementary Concept] OR “COVID-19 nucleic acid testing” [All Fields] OR “COVID-19 nucleic acid testing” [MeSH Terms] OR “COVID-19 serological testing” [All Fields] OR “COVID-19 serological testing” [MeSH Terms] OR “COVID-19 testing” [All Fields] OR “COVID-19 testing” [MeSH Terms] OR “sars cov 2” [All Fields] OR “SARS-CoV-2” [MeSH Terms] OR “severe acute respiratory syndrome coronavirus 2” [All Fields] OR “ncov” [All Fields] OR “2019 ncov” [All Fields] OR ((“coronavirus” [MeSH Terms] OR “coronavirus” [All Fields] OR “cov” [All Fields]) AND 2019/11/01:3000/12/31[Date - Publication])) |
| 3. “Spain” [Text Word] |
| 4.1 AND 2 AND 3 |
The results were transferred to a Mendeley database, subsequent to which we identified and classified articles on the Rayyan web platform, eliminating duplicate references (19). Initial selection was performed by peers (ACL, EM, AO, CSC, and DY) through screening titles and abstracts for eligibility. In the event of disagreement, a third researcher was asked to arbitrate.
Inclusion criteria were observational studies published between January 2020 and December 2021, with a total effective sample of ≥2,000 persons resident in Spain, published in English and Spanish. Exclusion criteria were studies that did not collect any information on perception of physical or mental health, qualitative, intervention or experimental studies and studies based on records. In the event of several articles stemming from the same survey, the one providing the most information about the survey was selected.
Data were extracted independently (by CSC and DY) using a standardized, predefined form that included variables relating to characteristics:
Literature references: link to publication, first author institution of work, date of publication, language, name of journal, type of publication (scientific article, report, review, comment, letter), open access (yes/no), impact factor and position (highest quartile) (20).
Survey: geographical area, study population, study design, sampling design, effective sampling size, sample weighting and other corrections, survey type, date information collected, response rate, waves or measurements, analyses performed, availability of microdata (Tables 1, 2).
Information collected: objective of study, primary topic [defined as mental health (43), lifestyle habits (27), wellbeing (76), quality of life (29), life satisfaction (42), perceived risk of infection (56), resilience (45) and working conditions (22)], information blocks, scales/composite variables, conclusions, observations (Supplementary Tables 1, 2).
Table 2.
Methodological characteristics of the selected surveys.
| Reference | Geographic scope (number of countries) | Study population | Study design | Effective sampling size | Sampling adjustments | Field work (start date) | Analysis performed |
|---|---|---|---|---|---|---|---|
| Ahrendt et al. (21) | Countries (22) | General population (≥18) | Cross-sectional** | 2,000–5,000 | Correction factor | April 2020 | Descriptive |
| Ajanovic et al. (23) | Spain | General population ( ≤ 16) | Cross-sectional | 2,000–5,000 | N/A | July 2020 | Bivariate |
| Alonso et al. (24) | Region (6) | Healthcare professionals | Longitudinal | 5,000–10,000 | Calibration | May 2020 | Logistic models |
| Arpino et al. (25) | Countries (3) | General population (≥18) | Cross-sectional | 2,000–5,000 | Post-stratification | April 2020 | Descriptive |
| Carpintero-Rubio et al. (26) | Spain | General population (≥18) | Cross-sectional | 2,000–5,000 | N/A | May 2020 | Bivariate |
| Cervera-Martínez et al. (27) | Spain | General population (≥18) | Cross-sectional* | 5,000–10,000 | N/A | April 2020 | Linear models |
| Codagnone et al. (28) | Countries (3) | General population (≥18) | Cross-sectional*** | 2,000–5,000 | Post-stratification | April 2020 | Random forest models |
| Coronado et al. (29) | Spain | Women 40–70 | Cross-sectional | 2,000–5,000 | N/A | April 2020 | Linear models |
| de Pedraza and Vicente (30) | Spain | General population | Cross-sectional | 2,000–5,000 | Correction factor | March 2020 | Logistic models |
| Centre d'Estudis d'Opinió (CEO) (31) | Region | General population (≥16) | Cross-sectional | 10,000–50,000 | Correction factor | April 2020 | Descriptive |
| Faris et al. (32) | Spain | General population | Cross-sectional | 2,000–5,000 | Post-stratification | May 2020 | Tobit models |
| Farres et al. (33) | Region | General population (≥16) | Cross-sectional | >50,000 | N/A | April 2020 | Bivariate |
| Fernández-Prados et al. (34) | Spain | General population (≥18) | Cross-sectional | 2,000–5,000 | N/A | June 2020 | Logistic models |
| Garcia-Adasme et al. (35) | Region | General population ( ≤ 16) | Cross-sectional | 2,000–5,000 | N/A | April 2020 | Bivariate |
| García-Álvarez et al. (36) | Spain | General population (≥18) | Cross-sectional | 10,000–50,000 | N/A | March 2020 | Logistic models |
| García-Dantas et al. (37) | Spain | General population (≥18) | Cross-sectional | 2,000–5,000 | N/A | March 2020 | Bivariate |
| Garcia-Esquinas et al. (38) | Spain | General population (≥65) | Longitudinal** | 2,000–5,000 | N/A | April 2020 | Mixed models |
| Garrido-Cumbrera et al. (39) | Spain | General population (≥16) | Cross-sectional | 2,000–5,000 | N/A | April 2020 | Logistic models |
| Gómez-Salgado et al. (40) | Spain | General population (≥18) | Cross-sectional | 2,000–5,000 | N/A | March 2020 | Logistic models |
| Gonzalez et al. (41) | Spain | General population (≥18) | Cross-sectional | 2,000–5,000 | N/A | March 2020 | Bivariate |
| Gonzalez-Bernal et al. (42) | Spain | General population (≥18) | Cross-sectional | 2,000–5,000 | N/A | March 2020 | Linear models |
| Gonzalez-Sanguino et al. (43) | Spain | General population (≥18) | Longitudinal** | 5,000–10,000 | N/A | March 2020 | Linear models |
| Grané et al. (44) | Countries (45) | General population (≥50) | Longitudinal*,*** | 10,000–50,000 | Calibration | June 2020 | Cluster |
| Hidalgo et al. (46) | Spain | General population (≥18) | Cross-sectional*** | 5,000–10,000 | N/A | April 2020 | Bivariate |
| Jacques-Aviñó et al. (47) | Spain | General population | Cross-sectional | 5,000–10,000 | N/A | April 2020 | Logistic models |
| Jané-Llopis et al. (48) | Region | General population (≥16) | Cross-sectional | 10,000–50,000 | N/A | April 2020 | Linear models |
| Jones (49) | Countries (50) | General population | Longitudinal** | 10,000–50,000 | Correction factor | March 2020 | Descriptive |
| Justo-Alonso et al. (51) | Spain | General population (≥18) | Cross-sectional | 2,000–5,000 | N/A | March 2020 | Bivariate |
| Kim and Ryu (52) | Countries (25) | General population | Cross-sectional | 2,000–5,000 | N/A | March 2020 | Mixed models |
| Lázaro-Pérez et al. (53) | Spain | Armed forces professionals | Cross-sectional | 2,000–5,000 | N/A | August 2020 | Logistic models |
| López-Bueno et al. (54) | Spain | General population (≥18) | Cross-sectional | 2,000–5,000 | N/A | March 2020 | Logistic models |
| Maestro-Gonzalez et al. (55) | Spain | General population | Cross-sectional | 5,000–10,000 | N/A | March 2020 | Multivariate analysis (N/A) |
| Mansilla Domínguez et al. (56) | Spain | General population (≥18) | Cross-sectional | 10,000–50,000 | Post-stratification | March 2020 | Logistic models |
| Martin et al. (57) | Spain | Healthcare professionals | Cross-sectional | 2,000–5,000 | N/A | April 20 | Linear models |
| Martinez-Bravo and Sanz (58) | Spain | General population (≥18) | Cross-sectional* | 2,000–5,000 | Correction factor | May 2020 | Descriptive |
| Méndez-Giménez et al. (59) | Spain | General population (≥16; < 92) | Cross-sectional | 2,000–5,000 | N/A | March 2020 | Logistic models |
| Miranda-Mendizabal et al. (60) | Spain | General population | Cross-sectional* | 2,000–5,000 | Correction factor | October 2020 | Logistic models |
| Morales-Vives et al. (61) | Spain | General population (≥18) | Cross-sectional | 2,000–5,000 | N/A | March 2020 | Bivariate |
| Oliver et al. (62) | Spain | General population | Cross-sectional | >50,000 | Correction factor | March 2020 | Logistic models |
| Viejo et al. (45) | Spain | General population | Cross-sectional | 2,000–5,000 | N/A | October 2020 | Mixed models |
| Pérez-Raya et al. (22) | Spain | Healthcare professionals | Cross-sectional | 10,000–50,000 | Correction factor | April 20 | Descriptive |
| Pinedo et al. (6) | Spain | General population | Cross-sectional | 2,000–5,000 | N/A | March 2020 | Structural Equation models |
| Planchuelo-Gómez et al. (63) | Spain | General population | Longitudinal* | 2,000–5,000 | N/A | April 2020 | Mixed models |
| Pouso et al. (64) | Countries (9) | General population | Longitudinal | 5,000–10,000 | N/A | April 2020 | Mixed models |
| Rodríguez-Barranco et al. (65) | Spain | General population | Cross-sectional | 2,000–5,000 | N/A | April 2020 | Logistic models |
| Rodríguez-Larrad et al. (66) | Spain | University students | Cross-sectional | 10,000–50,000 | N/A | April 2020 | Bivariate |
| Rodríguez-Pérez et al. (67) | Spain | General population | Cross-sectional | 5,000–10,000 | N/A | March 2020 | Multivariate analysis (N/A) |
| Rodriguez-Ruiz et al. (68) | Spain | Healthcare professionals | Cross-sectional* | 2,000–5,000 | N/A | October 2020 | Bivariate |
| Romero et al. (69) | Spain | Healthcare professionals | Cross-sectional | 2,000–5,000 | N/A | April 2020 | Bivariate |
| Salas-Nicás et al. (70) | Spain | General population | Cross-sectional | 10,000–50,000 | Correction factor | April 2020 | Bivariate |
| Sánchez-Cantalejo et al. (71) | Region | General population (≥16) | Longitudinal**,*** | 10,000–50,000 | Calibration, Propensity Score Matching, Machine Learning | April 2020 | Mixed models |
| Valiente et al. (72) | Spain | General population | Cross-sectional | 2,000–5,000 | N/A | April 2020 | Logistic models |
| Vall-Roqué et al. (73) | Spain | Women (14–35) | Cross-sectional | 2,000–5,000 | N/A | May 2020 | Hierarchical models |
| Villanueva et al. (74) | Spain | General population (≥18; < 65) | Cross-sectional | 2,000–5,000 | Correction factor | April 2020 | Bivariate |
| Yélamos Agua et al. (75) | Spain | Chronic patients | Cross-sectional | 2,000–5,000 | N/A | April 2020 | Logistic models |
*Survey with 2 measurements; **survey with 3 or more measurements (Jones, SP collects 29 measurements with COVID data); ***probabilistic sample; N/A, not available in the manuscript.
The variables of the second paragraph (survey characteristics) were selected from the STROBE (50) list, given that the studies in this review are observational.
Results
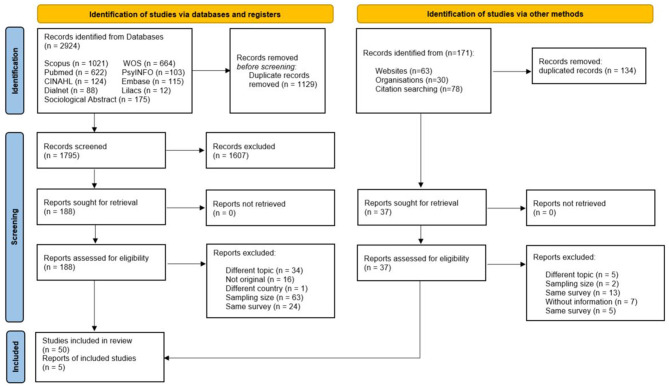
A total of 3,095 articles were identified following the search strategy described above. Two thousand nine hundred twenty-four articles were identified using scientific literature databases and 171 using gray literature. A full-text check was performed on 225 of them, i.e., 6.4 and 21.6%, respectively, for scientific literature databases and gray literature. Finally, 55 references were included for the analysis (Figure 1).
Figure 1.
PRISMA 2020 flow diagram for new systematic reviews which included searches of databases, registers, and other sources (77). For more information, visit: http://www.prisma-statement.org/.
Table 2 shows the methodological characteristics of each survey selected. The majority were signed by first authors from Spanish institutions (88%), 76.4% focused on Spain, 10.9% were conducted in smaller geographical units such as Autonomous Communities or municipalities, and 12.7% in various countries (in addition to Spain).
Almost half of the surveys selected published their results in 2020 (45%) and all of them began field work in 2020, one third of them in March (32.7%), 78.2% during the lockdown (March to April 2020) and 90.9% during the first state of emergency (March to June 2020). In addition, 80% of surveys collected information on one occasion or through one measurement. The YouGov bi-weekly information study (49) was found to have collected data on COVID-19 on 29 occasions.
As regards the study population of the 55 surveys selected for the analysis, 74.5% of them addressed the general adult population as their study population, while 9.1% considered the healthcare professionals (22, 24, 57, 68, 69). The same percentage of studies (3.6%, two surveys) considered as the study population the pediatric population (23, 35), women (29, 73) or people aged above 50 years old (38, 44). We also found one survey on chronic patients (75), on people aged over 50 or 65 years old, on the university community and on armed forces professionals.
The main topics among the selected surveys were mental health (60.0%), lifestyle habits (10.9%), wellbeing (7.3%), and quality of life, life satisfaction, perceived risk of infection, resilience and working conditions (3.6%). Information regarding the objectives, information blocks and scales or composite variables was also gathered and is available in Supplementary Tables 1, 2.
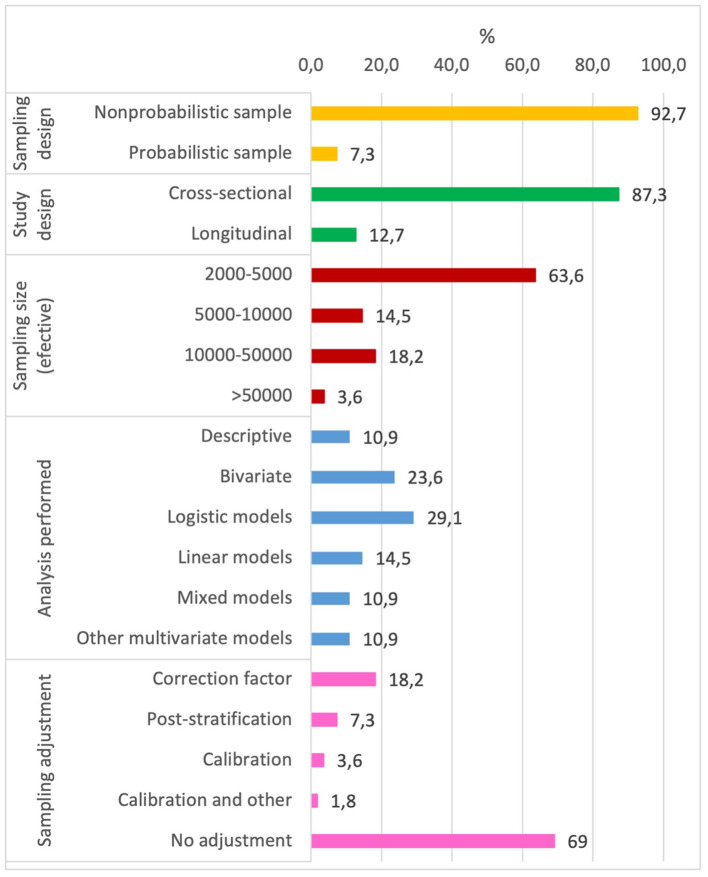
As regards sampling design, four of the fifty-five surveys selected (7.3%) had a probability design (28, 44, 46, 71) and seven (12.7%) were longitudinal surveys (Figure 2) (24, 38, 43, 44, 49, 63, 78), one on healthcare professionals (24) and the rest on the general population. Furthermore, three of these seven longitudinal surveys were cohort studies predating the pandemic (38, 44, 49). 92.7% of the surveys selected for the analysis gathered their data through online surveys, e.g., Qualtrics, Google forms, Lucid, SurveyGizmo or Surveymonkey, and 7.3% by telephone.
Figure 2.
Sample design and statistical analysis of the selected surveys.
In respect of sampling size, 35 surveys had between 2,000 and 5,000 participants (effective sample), two being found with over 50,000 participants (33, 62), both of which were online cross-sectional surveys. Additionally, 92.7% of the surveys included did not report the response rate.
As regards the statistical analysis conducted, thirty-six surveys developed a multivariate model, the most frequent being binary logistic (16), linear (eight surveys) and mixed (six surveys). Other multivariate models used were multi-level (73), cluster (44), principal components (32), random forest (28) and structural equations (6).
The distribution of groups of observations in the health surveys usually differs from the distribution in the survey population due to several reasons (coverage of the sampling frame, sample design, or patterns of unit non-response). Weighting is one of the best ways to reduce variances and to correct for frame deficiencies. In that sense, 30% implemented some type of sampling adjustment (Figure 2). The most frequent correction was of sample representativeness in view of sociodemographic variables using records or reference surveys (ten surveys). Post-stratification and calibration were applied only in four and two surveys, respectively. These methods are usually considered in official governmental surveys to minimize errors associated with incomplete sampling frames and with sampling non-response (79–81). Of note is the Health and Social Survey (71) which, in addition to calibration to reduce potential coverage or representativeness biases, implemented other methods based on Propensity Score Matching and Machine Learning to reduce biases due to lack of response in longitudinal samples. No voluntary or non-probability surveys were identified that used correction to reduce the selection bias concerned.
Lastly, most of the surveys included (67.2%) did not report on the availability of microdata.
Discussion
As far as we are aware, this is the first scoping review on health surveys relating to COVID-19 and their main methodological characteristics; actually, we found only one similar study dating from 2013 (82), albeit based on population health surveys conducted at Autonomous Community level in Spain and, most relevantly, without the extraordinary context provided by the pandemic, in which there was an urgent need to gather data to support timely evidence-based decisions. Moreover, searching in so many bibliographic resources is a strength of this scoping review.
Our main purpose with this review was to describe the methodological characteristics of surveys conducted early on in the pandemic, hence the search was focused on 2020 and 2021, noting that all surveys started during the first year of COVID-19. In fact, four out of every five surveys (78.2%) were conducted during the 2 months of the first lockdown period (March and April 2020). This demonstrates the rapid response by and considerable effort that the scientific community invested in attempting to provide information about the impact of COVID-19 on the population's health, with particular emphasis on mental health evidenced by the fact that more than half of the surveys (60%) focused on this as their main topic. This response was possible thanks to the internet: nine out of every ten surveys (92.7%) used social media, media sampling to recruit participants, or online subscription panels via this channel. The use of these types of survey expanded to such an extent during COVID-19 lockdowns that, along with more social considerations such as increasingly widespread internet access and use, they took over from traditional survey methods. In this regard, our study found that only four of the fifty-five surveys reviewed were conducted over the phone (7.3%) and, as was to be expected, no face-to-face surveys were identified.
However, despite the efforts made by official statistical institutions, for example the European Statistical System through its Quality Assurance Framework (83), the scientific community faced the difficulty of obtaining quality population frameworks from which quickly to extract probability samples representative of the study populations concerned. As our review shows, 92.7% of the surveys were based on non-probability sampling, which confirms their extensive use in the extraordinary setting created by COVID-19. Given the rapid inclusion of these types of study, we could ask ourselves the following question in relation to official health statistics: are probability surveys destined to disappear? In Beaumont's opinion (84), this moment has not yet arrived because the alternatives are not reliable and general enough to eradicate the use of probability surveys without having a deleterious effect on the quality of estimates.
Non-probability surveys present two advantages: they can collect large samples and they can do this in a short period of time. This is evidenced in our review, which shows that one out of every five surveys (21.8%) had a sample size of over 10,000 people, bearing in mind that one of the inclusion criteria was having an effective sample size of over 2,000. By contrast, the main drawback of non-probability surveys is that they present significant issues in terms of selection and coverage biases, thus compromising the generalization of results to the study population (85). Our review found that 30.9% of the surveys conducted implemented some type of sampling adjustment by means of correction factors, post-stratification sampling weighting, or calibration with sociodemographic variables such as sex, age or geographical area based on records or reference surveys. However, these adjustments do not correct volunteer bias (86), shown by the fact that we did not find any surveys that included non-probability selection of the people surveyed in their estimates. In this respect, different reweighting techniques have been developed in recent years using Propensity Score Adjustment, Statistical Matching, Kernel Weighting and combinations of these techniques (13, 79, 87–89) that have shown themselves to be highly effective for eliminating biases and increasing representativeness in non-probability surveys.
Despite these limitations, non-probability sampling can complement probability sampling if it is designed as a means to offset known biases in probability sampling by focusing on survey participant profiles that tend to be under-represented in such surveys (90). This notwithstanding, we did not find it being used in our review. Furthermore, non-probability surveys can be useful in some cases for providing relevant information that would not otherwise be available, for example in studies on small sub-populations where probabilistic sampling will encounter problems in fulfilling sample size requirements, good access to the study population or a suitable population framework for sample selection (91). However, here again we did not find it being used in our review, because the majority of surveys in Spain on the health impact of COVID-19 were conducted on the general adult population (74.5%). Nor did we identify any studies on more potentially vulnerable populations such as ethnic minorities, residents in care homes for the older adult or in deprived areas, other than the Health and Social Survey which, in addition to conducting surveys on the general population, also collects data on populations living in deprived areas (71). This percentage of general population surveys could be even larger, given that we eliminated forty-two studies stemming from the same survey. It must be noted that this probability survey was able to be conducted through the construction of a population framework during COVID-19 based on linking population records (92) and social records (93). In addition, the interviews in it were conducted not via the internet but rather by telephone, a more suitable channel for reaching these types of population given the continuing digital gap. So population frameworks such as this one provide opportunities for conducting other probability surveys (by telephone or in person) on these types of population.
Another outcome of our review worth noting is the low proportion of longitudinal surveys identified (12.7%). Surveys repeated over time are more difficult to conduct and analyze, but they do permit evaluation of changes in study variables in the same population, a key area for being able to obtain an overview of the pandemic and not just of its characteristics at a given moment in time (94). A sampling design that has proved useful in social research is rotating panel surveys where there is partial renewal of units (to mitigate panelist fatigue), the main advantage of which is that both cross-sectional and longitudinal estimates can be made (71), overcoming the potential limitation of many longitudinal studies in terms of needing to have rapidly available information on the state of the population. However, none of the surveys identified in our review used this design, other than the Health and Social Survey set up at the beginning of the COVID-19 state of emergency (71). This means that many of the surveys identified do not permit the changing effect of the pandemic on health in a single population to be known. Moreover, they were conducted at a very specific moment in time in highly exceptional circumstances, which must also be taken into account when extrapolating their results.
Lastly, this review is in line with other studies that show the high volume of scientific output related to COVID-19 (95). In our case, we identified more than 3,000 studies performed in Spain over 2 years, of which we selected 1.8% (55 surveys) for our review. Additionally, although our review centers on Spain, the studies it includes have a large international component given that 12.7% of them looked at other countries (some more than 27) (21, 25, 52, 64, 96) and 58.2% of them were published in journals situated in the first quartile (Journal Citation Reports).
As regards the search and the record created, they enable other analyses to be performed in subsequent years on specific topics such as mental health, and studies without a given exclusion criterion to be easily retrieved (thus enabling the analysis performed in this review to be repeated in other studies). For example, we considered as the last exclusion criteria surveys with a sample size of < 2,000 individuals. Our objective was to select large health surveys in terms of guaranteeing that sampling errors in overall estimates were below three percentage points assuming p = q = 0.5, 95% confidence level (power level did not apply because we considered observational studies), 0% sample loss because we refer to effective sample (not the theoretical one), and design effect two. If a lower sample size were required, it would be very easy to retrieve those studies through Rayyan and repeat the analysis. However, although our record facilitates identifying these studies through Rayyan, it is worth pointing out that barely one third of the surveys reviewed make their data openly available, and this hinders performing these studies or other analyses such as, for example, reweighting techniques which would provide more reliable estimates. This clearly reflects the ongoing lack of research based on Open Science (97), despite the major opportunity provided by COVID-19 to reverse this situation (98).
Author contributions
Conceptualization and funding acquisition: AC-L, MR, and CS-C. Methodology: AC-L, CS-C, AO-d-L-L, EM-R, and CH-C. Data curation and analysis: AC-L, CS-C, DY, AO-d-L-L, and EM-R. Writing—original draft preparation: AC-L, CS-C, and DY. Writing—review and editing: MR, AC-L, CS-C, AO-d-L-L, EM-R, and CH-C. Project administration: AC-L. All authors have read and agreed to the published version of the manuscript.
Funding Statement
This work was partially supported by Ministerio de Economía y Competitividad and Ministerio de Ciencia e Innovación of Spain (Grants PID2019-106861RB-I00, PI20/00855, and PI22/00512, respectively) and CIBER of Epidemiology and Public Health (CIBERESP).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1217519/full#supplementary-material
References
- 1.Andersen RM. National health surveys and the behavioral model of health services use. Med Care. (2008) 46:647–53. 10.1097/MLR.0b013e31817a835d [DOI] [PubMed] [Google Scholar]
- 2.Ministerio de la Presidencia Relaciones con las Cortes y Memoria Democrática,. Real Decreto 463/2020. BOE. (2020). Available online at: https://www.boe.es/buscar/pdf/2020/BOE-A-2020-3692-consolidado.pdf (accessed March 14, 2021).
- 3.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Serrano-Ripoll MJ, Meneses-Echavez JF, Ricci-Cabello I, Fraile-Navarro D, Fiol-deRoque MA, Pastor-Moreno G, et al. Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review and meta-analysis. J Affect Disord. (2020) 277:347. 10.1016/j.jad.2020.08.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. (2020) 5:e256. 10.1016/S2468-2667(20)30061-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pinedo R, Vicario-Molina I, González Ortega E, Palacios Picos A. Factors related to mental health during the COVID-19 lockdown in Spain. Front Psychol. (2021) 12:715792. 10.3389/fpsyg.2021.715792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodríguez-Rey R, Garrido-Hernansaiz H, Collado S. Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Front Psychol. (2020) 11:1540. 10.3389/fpsyg.2020.01540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mehra A, Rani S, Sahoo S, Parveen S, Singh AP, Chakrabarti S, et al. A crisis for elderly with mental disorders: relapse of symptoms due to heightened anxiety due to COVID-19. Asian J Psychiatr. (2020) 51:102114. 10.1016/j.ajp.2020.102114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tascon MG, Cuervo CM, Pinto CS, Gonzalez AM. Repercusión en la calidad de vida, salud y práctica de actividad física del confinamiento por Covid-19 en España (Effects on quality of life, health and practice of physical activity of Covid-19 confinement in Spain). Retos. (2021) 42:684–95. 10.47197/retos.v42i0.88098 [DOI] [Google Scholar]
- 10.Neyman J. On the two different aspects of the representative method: the method of stratified sampling and the method of purposive selection. J R Stat Soc. (1934) 97:558. 10.2307/2342192 [DOI] [Google Scholar]
- 11.Särndal C-E, Swensson B, Wretman J. Model Assisted Survey Sampling. (1992). Available online at: http://link.springer.com/10.1007/978-1-4612-4378-6 (accessed September 24, 2022).
- 12.Schonlau M, Couper MP. Options for conducting web surveys. Statist Sci. (2017) 32:279–92. 10.1214/16-STS597 [DOI] [Google Scholar]
- 13.Castro-Martín L, Rueda MDM, Ferri-García R. Estimating general parameters from non-probability surveys using propensity score adjustment. Math. (2020) 8:2096. 10.3390/math8112096 [DOI] [Google Scholar]
- 14.Sistemáticas R, Rocío E, Garabito M, Tamames Gómez S, López González M, Macías LM, et al. Revisiones sistemáticas exploratorias scoping review. Med Segur Trab. (2009) 55:12–9. 10.4321/S0465-546X2009000300002 [DOI] [Google Scholar]
- 15.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2007) 8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 16.Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. (2015) 13:141–6. 10.1097/XEB.0000000000000050 [DOI] [PubMed] [Google Scholar]
- 17.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 18.Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H. Chapter 11: scoping reviews (2020 version). In:Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis, JBI (2020). 10.46658/JBIMES-20-1234606196 [DOI] [Google Scholar]
- 19.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. (2016) 5:210. 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gisbert JP, Panés J. Publicación científica, indicadores bibliométricos e índice h de Hirsch. Gastroenterol Hepatol. (2009) 32:140–9. 10.1016/j.gastrohep.2008.09.024 [DOI] [PubMed] [Google Scholar]
- 21.Ahrendt D, Mascherini M, Nivakoski S, Sándor E. Living, working COVID-19 (Update April 2021): Mental Health Eurofound. (2020). Available online at: https://www.eurofound.europa.eu/publications/report/2021/living-working-and-covid-19-update-april-2021-mental-health-and-trust-decline-across-eu-as-pandemic (accessed September 24, 2022).
- 22.Pérez Raya F, Cobos Serrano JL, Ayuso Murillo D, Fernández Fernández P, Rodríguez Gómez JA, Almeida Souza AM de. Impacto del COVID-19 en las enfermeras en España: una encuesta. Int Nurs Rev. (2021) 68:248–55. 10.1111/inr.12682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ajanovic S, Garrido-Aguirre J, Baro B, Al E. How Did the COVID-19 Lockdown Affect Children and Adolescent's Well-Being: Spanish Parents, Children, and Adolescents Respond. Available online at: www.frontiersin.org (accessed September 24, 2022). [DOI] [PMC free article] [PubMed]
- 24.Alonso J, Vilagut G, Mortier P, Ferrer M, Alayo I, Aragón-Peña A, et al. Mental health impact of the first wave of COVID-19 pandemic on Spanish healthcare workers: a large cross-sectional survey. Rev Psiquiatr Salud Ment. (2021) 14:90–105. 10.1016/j.rpsm.2020.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arpino B, Pasqualini M, Bordone V, Solé-Auró A. Older people's nonphysical contacts and depression during the COVID-19 lockdown. Gerontologist. (2021) 61:176–86. 10.1093/geront/gnaa144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carpintero-Rubio C, Torres-Chica B, Guadrón-Romero MA, Visiers-Jiménez L, Peña-Otero D. Perception of musculoskeletal pain in the state of confinement: associated factors. Rev Lat Am Enfermagem. (2021) 29:e3454. 10.1590/1518-8345.4894.3454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cervera-Martínez J, Atienza-Carbonell B, Mota JC, Bobes-Bascarán T, Crespo-Facorro B, Esteban C, et al. Lifestyle changes and mental health during the COVID-19 pandemic: a repeated, cross-sectional web survey. J Affect Disord. (2021) 295:173–82. 10.1016/j.jad.2021.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Codagnone C, Bogliacino F, Gomez C, Charris R, Montealegre F, Liva G, et al. Assessing concerns for the economic consequence of the COVID-19 response and mental health problems associated with economic vulnerability and negative economic shock in Italy, Spain, and the United Kingdom. PLoS ONE. (2020) 15:e0240876. 10.1371/journal.pone.0240876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coronado PJ, Fasero M, Otero B, Sanchez S, de la Viuda E, Ramirez-Polo I, et al. Health-related quality of life and resilience in peri- and postmenopausal women during Covid-19 confinement. Maturitas. (2021) 144:4–10. 10.1016/j.maturitas.2020.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.de Pedraza P, Vicente MR. Are spaniards happier when the bars are open? using life satisfaction to evaluate COVID-19 non-pharmaceutical interventions (NPIs). Int J Environ Res Public Health. (2021) 18:10056. 10.3390/ijerph181910056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Societat . Centre d'Estudis d'Opinió. Available online at: https://ceo.gencat.cat/ca/estudis/registre-estudis-dopinio/estudis-dopinio-ceo/societat/detall/index.html?id=7588 (accessed September 24, 2022).
- 32.Faris LH, Gabarrell-Pascuet A, Felez-Nobrega M, Cristóbal-Narváez P, Mortier P, Vilagut G, et al. The association between substance use disorder and depression during the COVID-19 lockdown in Spain and the moderating role of social support: a cross-sectional study. Int J Ment Health Addict. (2021) 21:1–11. 10.1007/s11469-021-00651-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Farrés J, Ruiz JL, Mas JM, Arias L, Sarrias M-R, Armengol C, et al. Identification of the most vulnerable populations in the psychosocial sphere: a cross-sectional study conducted in Catalonia during the strict lockdown imposed against the COVID-19 pandemic. BMJ Open. (2021) 11:52140. 10.1136/bmjopen-2021-052140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fernández-Prados JS, Lozano-Díaz A, Muyor-Rodríguez J. Factors explaining social resilience against COVID-19: the case of Spain. Eur Soc. (2021) 23:S111–21. 10.1080/14616696.2020.1818113 [DOI] [Google Scholar]
- 35.Garcia-Adasme SI, Cárdenas-Rebollo JM, Jimenez-Perianes A, Lalinde M, Jimeno S, Ventura PS, et al. Pediatric home confinement due to COVID-19: somatic and anxiety spectrum consequences. J Clin Nurs. (2021) 30:3238–48. 10.1111/jocn.15829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.García-Álvarez L, de la Fuente-Tomás L, García-Portilla MP, Sáiz PA, Lacasa CM, Santo FD, et al. Early psychological impact of the 2019 Coronavirus disease (COVID-19) pandemic and lockdown in a large Spanish sample. J Glob Health. (2020) 10:020505. 10.7189/jogh.10.020505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.García-Dantas A, Justo-Alonso A, González-Vázquez A, Sánchez-Martín M, Del Río-Casanova L. Immediate psychological response during the very early stage of the coronavirus pandemic (COVID-19) in a spanish community sample. Actas Espanolas de Psiquiatria. (2021) 49:180–93. [PubMed] [Google Scholar]
- 38.García-Esquinas E, Ortolá R, Gine-Vázquez I, Carnicero JA, Mañas A, Lara E, et al. Changes in health behaviors, mental and physical health among older adults under severe lockdown restrictions during the COVID-19 pandemic in Spain. Int J Environ Res Public Health. (2021) 18:7067. 10.3390/ijerph18137067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Garrido-Cumbrera M, Foley R, Braçe O, Correa-Fernández J, López-Lara E, Guzman V, et al. Perceptions of change in the natural environment produced by the first wave of the COVID-19 pandemic across three European countries. results from the GreenCOVID study. Urban For Urban Green. (2021) 64:127260. 10.1016/j.ufug.2021.127260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gómez-Salgado J, Andrés-Villas M, Domínguez-Salas S, Díaz-Milanés D, Ruiz-Frutos C. Related Health Factors of Psychological Distress During the COVID-19. Available online at: www.mdpi.com/journal/ijerph (accessed November 6, 2020). [DOI] [PMC free article] [PubMed]
- 41.González Casas D, Mercado García E, Corchado Castillo AI, De la Paz Elez P. COVID-19 y su asociación con síntomas depresivos en población española. Rev habanera cienc méd. (2020) 19:e3631. Available online at: http://www.revhabanera.sld.cu/index.php/rhab/article/view/3631 [Google Scholar]
- 42.Gonzalez-Bernal JJ, Rodríguez-Fernández P, Santamaría-Peláez M, González-Santos J, León-Del-barco B, Minguez LA, et al. Life satisfaction during forced social distancing and home confinement derived from the COVID-19 pandemic in Spain. Int J Environ Res Public Health. (2021) 18:1474. 10.3390/ijerph18041474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.González-Sanguino C, Ausín B, Castellanos MÁ, Saiz J, López-Gómez A, Ugidos C, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. (2020) 87:172–6. 10.1016/j.bbi.2020.05.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Grané A, Albarrán I, Merchán DE. Impact of pandemic on european well-being: visualizing scenarios from the SHARE database. Int J Environ Res Public Health. (2021) 18:4620. 10.3390/ijerph18094620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Viejo P, Barbé D, Pérez R-B, del Mar M, Pérez L. Resiliencia para la promoción de la salud en la crisis Covid-19 en España. Rev ciencias Soc. (2020) 26:52–63. 10.31876/rcs.v26i4.34649 [DOI] [Google Scholar]
- 46.Hidalgo MD, Balluerka N, Gorostiaga A, Espada JP, Santed MÁ, Padilla JL, et al. The psychological consequences of COVID-19 and lockdown in the Spanish population: an exploratory sequential design. Int J Environ Res Public Health. (2020) 17:8578. 10.3390/ijerph17228578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jacques-Avinõ C, López-Jiménez T, Medina-Perucha L, De Bont J, Goncalves AQ, Duarte-Salles T, et al. Gender-based approach on the social impact and mental health in Spain during COVID-19 lockdown: a cross-sectional study. BMJ Open. (2020) 10:e044617. 10.1136/bmjopen-2020-044617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jané-Llopis E, Anderson P, Segura L, Zabaleta E, Muñoz R, Ruiz G, et al. Mental ill-health during COVID-19 confinement. BMC Psychiatry. (2021) 21:1–12. 10.1186/s12888-021-03191-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jones S. GitHub - YouGov-Data/covid-19-Tracker: This is the Data Repository for the Imperial College London YouGov Covid 19 Behaviour Tracker Data Hub. Available online at: https://github.com/YouGov-Data/covid-19-tracker (accessed September 24, 2022).
- 50.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. (2008) 61:344–9. 10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 51.Justo-Alonso A, García-Dantas A, González-Vázquez AI, Sánchez-Martín M, del Río-Casanova L. How did different generations cope with the COVID-19 pandemic? early stages of the pandemic in Spain. Psicothema. (2020) 32:490–500. 10.7334/psicothema2020.168 [DOI] [PubMed] [Google Scholar]
- 52.Kim H-HS, Ryu J. Social distancing attitudes, national context, and health outcomes during the COVID-19 pandemic: findings from a global survey. Prev Med. (2021) 148:106544. 10.1016/j.ypmed.2021.106544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lázaro-Pérez C, Martínez-López JÁ, Gómez-Galán J, Fernández-Martínez MDM. COVID-19 pandemic and death anxiety in security forces in Spain. Int J Environ Res Public Health. (2020) 17:1–16. 10.3390/ijerph17217760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.López-Bueno R, Calatayud J, Casaña J, Casajús JA, Smith L, Tully MA, et al. COVID-19 confinement and health risk behaviors in Spain. Front Psychol. (2020) 11:1426. 10.3389/fpsyg.2020.01426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Maestro-Gonzalez A, Sánchez-Zaballos M, Mosteiro-Díaz MP, Zuazua-Rico D. Quality of sleep among social media users during the lockdown period due to COVID-19 in Spain. Sleep Med. (2021) 80:210–5. 10.1016/j.sleep.2021.01.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mansilla Domínguez JM, Font Jiménez I, Belzunegui Eraso A, Peña Otero D, Díaz Pérez D, Recio Vivas AM. Risk perception of COVID−19 community transmission among the Spanish population. Int J Environ Res Public Health. (2020) 17:8967. 10.3390/ijerph17238967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Martín J, Padierna Á, Villanueva A, Quintana JM. Evaluation of the mental health of health professionals in the COVID-19 era. what mental health conditions are our health care workers facing in the new wave of coronavirus? Int J Clin Pract. (2021) 75:e14607. 10.1111/ijcp.14607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Martinez-Bravo M, Sanz C. Inequality and psychological well-being in times of COVID-19: evidence from Spain. Ser J Spanish Econ Assoc. (2021) 12:489–548. 10.1007/s13209-021-00255-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Méndez-Giménez A, Cecchini JA, Fernández-Río J, Carriedo A. Physical activity and prevention of depressive symptoms in the Spanish population during confinement due to COVID-19. Psicothema. (2021) 33:111–7. 10.7334/psicothema2020.294 [DOI] [PubMed] [Google Scholar]
- 60.Miranda-Mendizabal A, Recoder S, Sebastian EC, Casajuana Closas M, Leiva Ureña D, Manolov R, et al. Socio-economic and psychological impact of COVID-19 pandemic in a Spanish cohort BIOVAL-D-COVID-19 study protocol. Gac Sanit. (2022) 36:70–3. 10.1016/j.gaceta.2021.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Morales-Vives F, Dueñas JM, Vigil-Colet A, Camarero-Figuerola M. Psychological variables related to adaptation to the COVID-19 lockdown in Spain. Front Psychol. (2020) 11:565634. 10.3389/fpsyg.2020.565634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Oliver N, Barber X, Roomp K, Roomp K. Assessing the impact of the COVID-19 pandemic in Spain: large-scale, online, self-reported population survey. J Med Internet Res. (2020) 22:e21319. 10.2196/21319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Planchuelo-Gómez Á, Odriozola-González P, Irurtia MJ, de Luis-García R. Longitudinal evaluation of the psychological impact of the COVID-19 crisis in Spain. J Affect Disord. (2020) 277:842. 10.1016/j.jad.2020.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pouso S, Borja Á, Fleming LE, Gómez-Baggethun E, White MP, Uyarra MC. Contact with blue-green spaces during the COVID-19 pandemic lockdown beneficial for mental health. Sci Total Environ. (2021) 756:143984. 10.1016/j.scitotenv.2020.143984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rodríguez-Barranco M, Rivas-García L, Quiles JL, Redondo-Sánchez D, Aranda-Ramírez P, Llopis-González J, et al. The spread of SARS-CoV-2 in Spain: hygiene habits, sociodemographic profile, mobility patterns and comorbidities. Environ Res. (2021) 1:192. 10.1016/j.envres.2020.110223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rodríguez-Larrad A, Mañas A, Labayen I, González-Gross M, Espin A, Aznar S, et al. Impact of COVID-19 confinement on physical activity and sedentary behaviour in Spanish university students: role of gender. Int J Environ Res Public Health. (2021) 18:1–14. 10.3390/ijerph18020369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rodríguez-Pérez C, Molina-Montes E, Verardo V, Artacho R, García-Villanova B, Guerra-Hernández EJ, et al. Changes in dietary behaviours during the COVID-19 outbreak confinement in the Spanish COVIDiet study. Nutrients. (2020) 12:1–19. 10.3390/nu12061730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rodriguez-Ruiz E, Campelo-Izquierdo M, Boga Veiras P, Mansilla Rodríguez M, Estany-Gestal A, Blanco Hortas A, et al. Impact of the coronavirus disease 2019 pandemic on moral distress among nurses and physicians in spanish ICUs. Crit Care Med. (2022) 50:E487–97. 10.1097/CCM.0000000000005434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Romero CS, Delgado C, Catalá J, Ferrer C, Errando C, Iftimi A, et al. COVID-19 psychological impact in 3109 healthcare workers in Spain: the PSIMCOV group. Psychol Med. (2022) 52:1. 10.1017/S0033291720001671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Salas-Nicás S, Moncada S, Llorens C, Navarro A. Working conditions and health in Spain during the COVID-19 pandemic: minding the gap. Saf Sci. (2021) 134:105064. 10.1016/j.ssci.2020.105064 [DOI] [Google Scholar]
- 71.Sánchez-Cantalejo C, Rueda MdM, Saez M, Enrique I, Ferri R, De M, et al. Impact of COVID-19 on the health of the general and more vulnerable population and its determinants: health care and social survey-ESSOC, study protocol. Int J Environ Res Public Health. (2021) 18:8120. 10.3390/ijerph18158120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Valiente C, Contreras A, Peinado V, Trucharte A, Martínez AP, Vázquez C. Psychological adjustment in Spain during the COVID-19 pandemic: positive and negative mental health outcomes in the general population. Span J Psychol. (2021) 24:e8. 10.1017/SJP.2021.7 [DOI] [PubMed] [Google Scholar]
- 73.Vall-Roqué H, Andrés A, Saldaña C. The impact of COVID-19 lockdown on social network sites use, body image disturbances and self-esteem among adolescent and young women. Prog Neuro-Psychopharmacology Biol Psychiatry. (2021) 110:110293. 10.1016/j.pnpbp.2021.110293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Villanueva VJ, Motos P, Isorna M, Villanueva V, Blay P, Vázquez-Martínez A. Impacto de las medidas de confinamiento durante la pandemia de Covid-19 en el consumo de riesgo de alcohol. Rev Esp Salud Pública. (2021). 95:20 deenero e202101015. [PubMed] [Google Scholar]
- 75.Yélamos Agua C, Berzal Pérez E, de Haro Gázquez D, Fernández Sánchez B, Navarro Jiménez JM. Psychosocial impact of the COVID-19 outbreak and lockdown on Spanish oncological patients: a quantitative approach. J Psychosoc Oncol. (2021) 39:385–98. 10.1080/07347332.2021.1880523 [DOI] [PubMed] [Google Scholar]
- 76.Sánchez-Cantalejo C, Rueda M, Saez M, Enrique I, Ferri-García R, De la Fuente M, et al. Impact of COVID-19 on the health of the general and more vulnerable population and its determinants: health care and social survey-ESSOC, study protocol. (2021). 10.21203/rs.3.rs-505722/v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cabrera-León A, Sánchez-Cantalejo C. Características y resultados de encuestas sobre el impacto de la enfermedad COVID-19. Comprender el COVID-19 desde una perspectiva de salud pública (2020). Available online at: https://www.easp.es/web/coronavirusysaludpublica/caracteristicas-y-resultados-de-encuestas-sobre-el-impacto-de-la-enfermedad-covid-19/ (accessed March 15, 2021).
- 79.Castro-Martín L, Rueda MdM, Ferri-García R. Inference from non-probability surveys with statistical matching and propensity score adjustment using modern prediction techniques. Math. (2020) 8:879. 10.3390/math8060879 [DOI] [Google Scholar]
- 80.Ranalli MG, Arcos Cebrián A, Rueda García MDM, Teodoro A. Calibration Estimation in Dual-Frame Surveys. (2015). Available online at: http://hdl.handle.net/10481/68532
- 81.Ferri-García R, Rueda MdM. Propensity score adjustment using machine learning classification algorithms to control selection bias in online surveys. PLoS ONE. (2020) 15:e0231500. 10.1371/journal.pone.0231500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Luisa Requena M, Suárez M, Pérez Ó, de los Santos Ichaso M, Sánchez JJ, Margolles M, et al. Encuestas de salud en españa: situación actual. Rev Esp Salud Publica. (2013) 87:549–73. 10.4321/S1135-57272013000600002 [DOI] [PubMed] [Google Scholar]
- 83.European Statisticals System,. Quality Assurance Framework of the European Statistical System. Version 2.0. (2019). Available online at: https://ec.europa.eu/eurostat/documents/64157/4392716/ESS-QAF-V1-2final.pdf/bbf5970c-1adf-46c8-afc3-58ce177a0646
- 84.Beaumont J,. Are Probability Surveys Bound to Disappear for the Production of Official Statistics?. Statistics Canada (2020). Available online at: https://www150.statcan.gc.ca/n1/pub/12-001-x/2020001/article/00001-eng.htm (accessed April 11, 2021).
- 85.Bethlehem J. Selection bias in web surveys. Int Stat Rev. (2010) 78:161–88. 10.1111/j.1751-5823.2010.00112.x [DOI] [Google Scholar]
- 86.Rao JNK. On making valid inferences by integrating data from surveys and other sources. Sankhya B Indian J Stat. (2021) 83:242–72. 10.1007/s13571-020-00227-w [DOI] [Google Scholar]
- 87.Castro-Martín L, Rueda MDM, Ferri-García R, Hernando-Tamayo C. On the use of gradient boosting methods to improve the estimation with data obtained with self-selection procedures. Math. (2021) 9:2991. 10.3390/math923299132357871 [DOI] [Google Scholar]
- 88.Valliant R. Comparing alternatives for estimation from nonprobability samples. J Surv Stat Methodol. (2020) 8:231–63. 10.1093/jssam/smz00325488851 [DOI] [Google Scholar]
- 89.Rueda MdM, Pasadas-del-Amo S, Rodríguez BC, Castro-Martín L, Ferri-García, R. Enhancing estimation methods for integrating probability and nonprobability survey samples with machine-learning techniques. an application to a survey on the impact of the COVID-19 pandemic in Spain. Biom J. (2023). 65: 2200035. 10.1002/bimj.202200035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Castro-Martín L, Rueda MdM, Ferri-García R. Combining statistical matching and propensity score adjustment for inference from non-probability surveys. J Comput Appl Math. (2022) 404:113414. 10.1016/j.cam.2021.113414 [DOI] [Google Scholar]
- 91.Wiśniowski A, Sakshaug JW, Perez Ruiz DA, Blom AG. Integrating probability and nonprobability samples for survey inference. J Surv Stat Methodol. (2020) 8:120–47. 10.1093/jssam/smz05137284419 [DOI] [Google Scholar]
- 92.Ieca I, de EyC A. Base de Datos Longitudinal de Población de Andalucía (2018). [Google Scholar]
- 93.Estrategia Regional Andaluza para la Cohesión e Inclusión Social. Intervención en Zonas desfavorecidas (ERACIS) - Junta de Andalucía. Available online at: https://juntadeandalucia.es/organismos/igualdadpoliticassocialesyconciliacion/areas/inclusion/zonas-transformacion/paginas/diseño-ejecucion-estrategias.html (accessed October 7, 2021).
- 94.Torres-Cantero AM, Álvarez León EE, Morán-Sánchez I, San Lázaro Campillo I, Bernal Morell E, Hernández Pereña M, et al. Health impact of COVID pandemic. SESPAS report 2022. Gac Sanit. (2022) 36 Suppl 1:S4–12. 10.1016/j.gaceta.2022.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Riccaboni M, Verginer L. The impact of the COVID-19 pandemic on scientific research in the life sciences. PLoS ONE. (2022) 17:e0263001. 10.1371/journal.pone.0263001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Jones SP. GitHub - YouGov-Data/covid-19-tracker: This is the data repository for the Imperial College London YouGov Covid 19 Behaviour Tracker Data Hub. Available online at: https://github.com/YouGov-Data/covid-19-tracker (accessed September 24, 2022).
- 97.Burgelman J-C, Pascu C, Szkuta K, Von Schomberg R, Karalopoulos A, Repanas K, et al. Open science, open data, and open scholarship: European policies to make science fit for the twenty-first century. Front Big Data. (2019) 2:43. 10.3389/fdata.2019.00043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Besançon Besançon L, Peiffer-Smadja N, Segalas C, Jiang H, Masuzzo P, Smout C, et al. Open science saves lives: lessons from the COVID-19 pandemic. BMC Med Res Methodol. (2021) 21:1–18. 10.1186/s12874-021-01304-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.