Abstract
Purpose
Although flatfoot is a widespread human condition, historical medical texts and ancient illustrations on this deformity are extremely rare. Nowadays, doubts regarding its management remain unsolved. This historical review aims to identify the presence of pes planus since the prehistoric era and examine the treatments proposed over the centuries up to the present.
Method
For this propose, we performed an extensive electronic search of the relevant literature, complemented by a manual search of additional sources from archaeological to artistic, literary, historical, and scientific accounts, describing flatfoot and its treatment in different eras.
Results
Flatfoot accompanied the evolutionary timeline of human species: from Lucy Australopithecus to Homo Sapiens. It was described among various diseases suffered by Tutankhamun (1343–1324 B.C.), while the first anatomical description dates to Emperor Trajan (53–117 A.D.) and the medical studies of Galen (129–201 A.D.). It was also represented in the anatomical drawings of Leonardo da Vinci (1452–1519) and Girolamo Fabrici d'Acquapendente (1533–1619). Historically, the conservative treatment by insoles was the only one proposed until the nineteenth century. Since then, the most popular surgical procedures performed for correction have been osteotomies, arthrodesis, arthrorisis, and tendon lengthening and transfer.
Conclusion
During the centuries, conservative therapeutic strategies have not radically changed in their substance, while operative ones have become the protagonists during the twentieth century up to the present. Nevertheless, after more than 2000 years of history, there is no consensus regarding the best indication for the flatfoot and if it really needs to be treated.
Keywords: Flatfoot; Pes planus; Insoles; Foot deformities; Arthrodesis, Arthrorisis; Osteotomies; Tendon lengthening; Tendon transfer
Introduction
Flatfoot or pes planus is a condition that has been defined in various ways over time. Most commonly, it has been simply described as a foot with the medial margin of its plantar aspect in complete contact with the ground. The aetiology of its most common forms has been ascribed to an atavism in the development of human being [1]. Krogman (Oak Park, Illinos 1903 - Litiz, Pennsylvania 1987) interestingly described the pes planus as a “scar” of human evolution, observing that “[…] Our fallen arch trouble, our bunions, our calluses, and our foot miseries generally hark back to the fact that our feet are not yet healed by adaptation and evolutionary selection into really efficient units” [1]. Other authors, Helfet and Lee, described the pes planus as a condition in which the medial longitudinal arch is lower than “normal” on weight-bearing [2]. Instead, the term “pes planovalgus” was introduced to describe a more complex form, where both the arch is flat in the sagittal plan and the heel is in a pronounced valgus position everted in the frontal plane [2].
Currently, normal adult feet are described as having a characteristic morphology with the presence of two arches that allow for the correct discharge of forces during standing, walking, running, and jumping. Essential for the stability of the plantar arches are the dynamic musculo-tendinous structures: the tibialis posterior tendon, tendons of the flexor hallucis longus and flexor digitorum longus muscles, the peroneus longus and brevis muscle, the plantar calcaneonavicular and the deltoid ligaments, and the plantar aponeurosis [3]. Although most forms of pes planus are a widespread condition across time periods, unlike clubfoot, historical medical texts and ancient illustrations on its evolution throughout history to contemporary scientific literature are extremely rare [4]. The goal of this historical review is to try to fill this gap.
The evolution of feet: from quadrupeds to bipeds
The foot is described as a part of the human body with an extraordinary number of anatomical evolutionary adaptations due to bipedalism and upright position. This is related to the disappearance of the opposability of the hallux in hominins and the consequent loss of the foot function as a grasping element [5].
In 1997, the orthopaedist Albert Isidro Llorens reported that in the primate evolution context, bipedalism is an anatomical adaptation to survive geo-climatic changes [6]. In 1809, Lamarck in his Philosophie zoologique [7] wrote that quadrupedal apes inhabited trees and only changed into pedals when they became fully terrestrial, probably because trees disappeared. In Darwin’s Descent of Man [8], it is argued that bipedalism emerged when an ancient primate became less arboreal conferring selective advantage because it freed hands from locomotion so they could be used to hold weapons and dominate other animals. Bipedal specialisation was found in ancient hominin such as Ardipithecus ramidus, lived about 4.4 million years (Myr) ago, and Austrolopithecus anamensis, lived about 4.2 Myr ago.
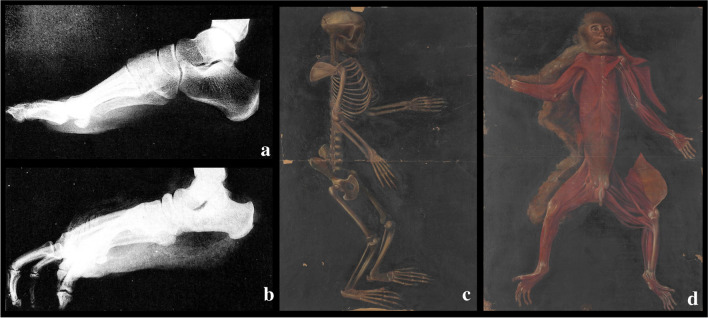
In 2016, Hatala and colleagues supposed that Pliocene hominin gained bipedal posture, conclusion based on studies conducted on the footprints discovered in 1977 at Laetoli, Tanzania. These trackways date back to around 3.66 Myr and are widely considered to have been made by Australopithecus afarensis [9]. In modern humans, foot bones are strong structures, able to hold the weight of the body to allow a walking bipedal gait [10]. It is recognised that all primates, such as chimpanzees, possess a transverse arch, but only humans have a longitudinal arch, making non-human primates anatomically and functionally flat-footed [11] (Fig. 1).
Fig. 1.
The evolution of foot in primates: a Lateral, not weightbearing, radiographic images of a human foot and b chimpanzee foot, modified from Donald Johanson, Blake Edgar, From Lucy to Language, s.l., Cassell & Co London, 2001; c and d anatomical images of the transverse arch in the monkey, from Theatrum totius animalis fabricae - De anatomia animalium, Rari 113, by Girolamo Fabrici d'Acquapendente, Marciana National Library in Venice
In the 1970s, mid-Pliocene hominin fossils were found at the site of Hadar in Ethiopia. The samples constituted the first substantial evidence for hominins older than three million years and were notable for some remarkable discoveries, such as the “Lucy” partial skeleton [12]. She was firstly described in 1978 by his discoverer D. Johanson in the manuscript “Kirtlandia” as a species of Australopithecus distinguished by a dentition with large upper central incisors with flexed roots, and asymmetric canines; a characteristic mandibular shape with an ascending ramus broad and post-canine teeth aligned in straight rows; a cranium featured by palate shallow, especially anteriorly; and dental arcade long, narrow, and straight-sided. Moreover, he described a high level of robusticity in all skeletal elements and pelvic region and lower limbs with bipedal locomotion adaptation [13]. By the studies conducted on bones of the famous 3.0–3.7-Myr-old hominin Australopithecus afarensis (this name derives from the Afar depression in Ethiopia where the largest portion of the paratype series was recovered [13]), it was found that “Lucy” had a flatfoot, although two other tibiae from Hadar suggest the presence of a rearfoot arch in the same species [14] (Fig. 2).
Fig. 2.
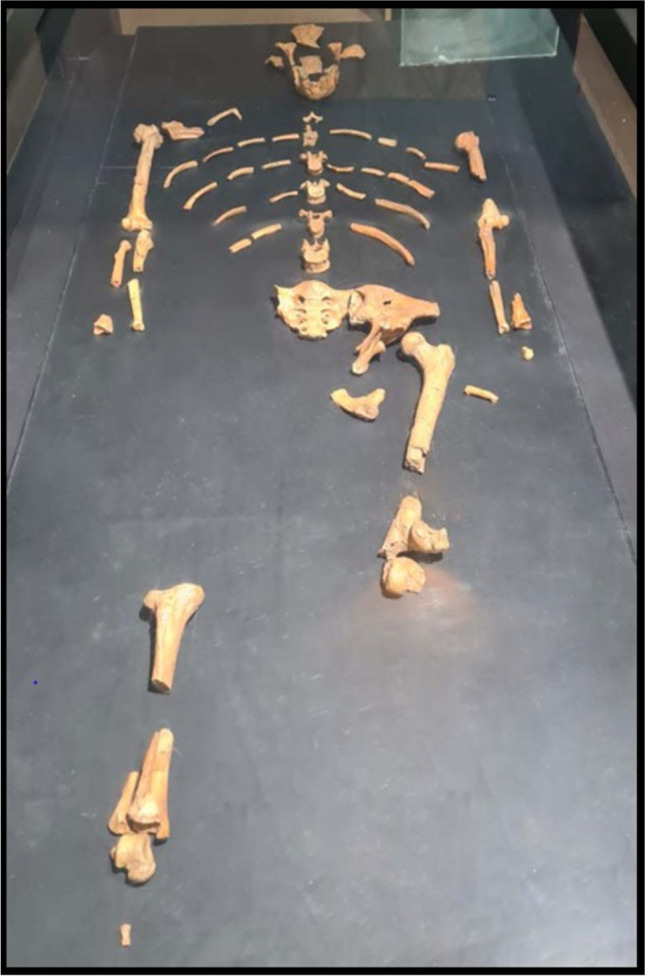
“Lucy” partial skeleton found at the sites of Hadar in Ethiopia in 1974 by Donald Johanson. The skeleton is dated to about 3.2 million years ago, and it has a small skull, 1.07 m high, and probably weighed between 29 and 45 kg. This original fossil of Lucy is kept at the National Museum of Ethiopia in Addis-Ababa
However, hominids, known as Archaic Primates, Prosimians, and Plesiadapiforms from the Paleocene and Eocene, show a traverse arch as reported by Conroy in his paper [15]. Considering the research in the fore/midfoot, the Kromdraai talar remains (Paranthropus robustus) exhibit similar features to those of Olduvai Hominid 8 (OH8), with its horizontal angle being more in line with apes (Gorilla gorilla, Pan troglodytes) than humans (continental Europeans, Bushmen, Anglo-Saxon/Romano-British). On the other hand, other studies proposed that the locomotion of Australopithecus sediba shows a unique form of bipedalism and a minor degree of arboreality, derived from its primitive and hominin foot. Its feet show a cuboid facet at a similar angle in line with humans, suggesting foot arching and a smooth calcaneal tuber surface.
Moreover, research conducted on the remains of the Homo floresiensis concluded that its feet show primitive features for the genus Homo, such as long lateral toes, a short first metatarsal, re-evolving short hind limbs, and flatfoot, among others [16].
The available evidence implies that there were several stages in the evolution of the arch of the human foot. First, apes such as chimpanzees and presumably the last common ancestor of apes and hominins lacked both a longitudinal and transverse arch. By 3.4 million years ago, though possibly earlier, a human-like transverse arch had evolved in A. afarensis, which however lacked a fully developed longitudinal arch [17]. Finally, in the genus Homo, we see a full longitudinal and transverse arch, enabling both effective walking and running [11]. The evolution of medial longitudinal arch can be dated to the attachment of the spring ligament in the talus found in individual OH 8 of Homo habilis (2.4–1.4 Myr) [18].
Since the Neanderthals to the first pair of shoes
The proportions and bone morphology of the Neanderthal foot are similar to those of Homo sapiens, with the exception of the talus. Neanderthals external talus morphology reflects the various adaptations associated with their presumably hunter-gatherer, shoeless lifestyle unlike Homo sapiens who began wearing footwear. Studies suggest that higher human body mass of Neanderthals and/or higher mechanical stress led to their habitually pronated foot posture [19]. Neanderthals apparently did not wear hard-soled shoes, but covered their feet with skins to keep warm. Archaeological evidence suggests that footwear was in use from at least the Middle Upper Paleolithic (Gravettian) in parts of Europe. A comparative biomechanical analysis of the proximal phalanges of the foot of Western Middle Paleolithic and Middle Upper Paleolithic Eurasian humans indicates that supportive footwear was rare in the Middle Paleolithic, but became frequent in the Middle Upper Paleolithic [20]. According to anthropologist Erik Trinkaus, the smallest toes on our extremities weakened during that time, an anatomical change that the expert attributes to the invention of rudimentary shoes. These, in fact, reduced the need for strong and flexible fingers to grip the ground and balance the step. Ancestors who lived in cold climates may have started covering their feet to insulate them from the cold as early as 500,000 years ago. Until now, it has been difficult for archaeologists to determine exactly when humans stopped walking barefoot, not least because the plant and animal materials used for prehistoric shoes were highly perishable. Notably, Neanderthals and early Homo sapiens of the Middle Paleolithic (100,000 to 40,000 years ago) still had much stronger and more agile fingers than the Upper Paleolithic peoples, who inhabited the earth 26,000 years ago [20].
The myth of Tutankhamun
It is necessary to fast forward to the Egyptian era to find the most famous ancient case of flatfoot: the Theban boy-king Tutankhamun. He was a scion of the 18th dynasty of the New Kingdom, the most powerful period of ancient Egypt (circa 1550–1070 B.C.). Nowadays, Tutankhamun is the most worldwide known pharaoh, although his tenure was brief because he died in the ninth year of his reign, about 1324 B.C., at 19 years of age [21].
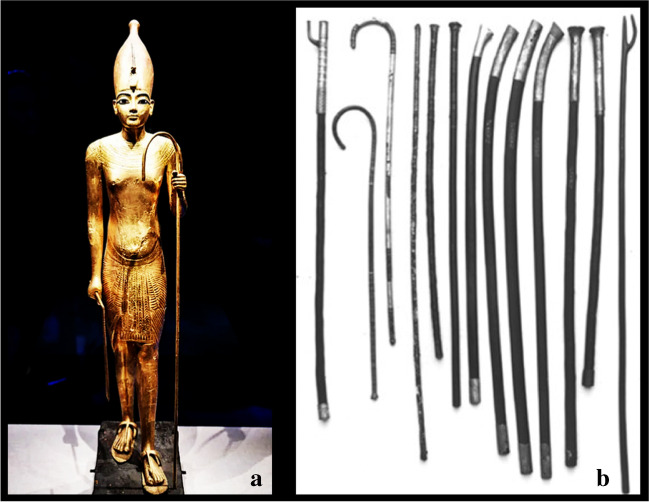
The weak pharaoh suffered from foot pathologies as supported by the King’s grave goods present in tomb KV62, discovered in the valley of kings by the British archaeologist and Egyptologist Howard Carter (London 1874–London 1939) [22] in November 1922. Although the pharaoh led a physically active life and had a normal body height for adolescence (1.67 m) [23], about 130 walking sticks were found in his tomb. Further, several images show the King with a long stick or a long sceptre; some suggest that the pharaoh may have used them to support himself (Fig. 3).
Fig. 3.
Pharaoh Tutankhamun (1343–1324 B.C.): a wooden statue of the Pharaoh Tutankhamun and his stick, Saatchi Gallery (London, UK), suggesting that the pharaoh may have used it to support himself; b walking sticks found in his tomb, Burton photograph, kept in the Griffith Institute Archive, University of Oxford
Tutankhamun’s father, Akhenaton (Tebe 1375 B.C. circa–Akhetaton 1334 B.C. circa), with the same A + blood group [24], and his mother (perhaps Kiya or Nefertiti), were probably brother and sister, passing on genetic defects to their children. All findings collected between 1922 and 2020, including computed tomography (CT) and genetic disease analysis, showed that the King suffered from several diseases in his lower limbs: pes planus, painful Kohler’s disease and oligodactyly of the right foot, and club foot and bone necrosis of metatarsal bones II–III of the left one [24].
In 2010, the Egyptologist Zahi Abass Hawass reported the detailed examination of the King’s right foot, proving the presence of a low longitudinal arch with Rocher angle of 132° (normal value, 126°) [23]. Hawass demonstrated that Tutankhamun had juvenile aseptic bone necrosis of the left 2nd and 3rd metatarsals, also involving the 2nd metatarso-phalangeal joint, due to an ulcerative osteoarthritis, probably the final outcome of osteochondral lesions. The malformed 2nd toe of the left foot together with the congenital equinovarus deformity of the left foot transferred the additional joint load to the right foot, probably causing the flattening of the foot arch [23].
In 1971, Helck [25] proposed that the most probable cause of death of King Tutankhamun, as well as that of his possible relative Smenkhare, could be connected to a sort of plague [26], as advocated by other authors [27–29]. Although the latest evidence indicates that the young king suffered from malaria [23], these authors believe that drepanocytosis and malaria may not have been the only cause of death, rather a contributing factor, combined with an infection after a complex fracture of the distal right femur (the fracture type corresponds to 33C3 of the AO classification) [23, 24, 30]. In relation to whether malaria was the primary cause of death, Timmann and Meyer suggested that these findings seem to be related to Gaucher disease rather than to anaemia falciparum [31]. For these reasons, the actual cause of death remains debated [32, 33].
The most ancient image and the first description of flatfoot
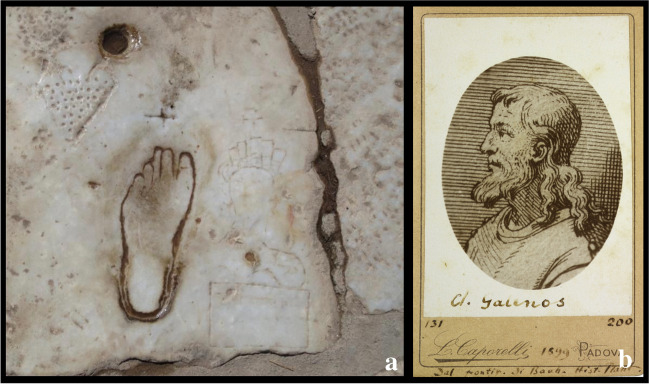
Another interesting finding regarding flatfoot dates to the first century A.D. during the reign of the emperor Trajan (Italica 53 A.D.–Selinunte 117 A.D.) in the town of Ephesus, where an engraved pictogram footprint of a flatfoot on the Marble Road was found [4]. This road led to the great theatre and to the Celsus Library, as a portion of the sacred way that led to the Temple of Artemis [34].
To our knowledge, this engraved pictogram is probably among the oldest representations of a flatfoot in history [4]. It consists of three symbols: the foot, a female head with a bust, and a pierced heart opposite the female figure, symbolising the woman waiting in a brothel and her eagerness for love. It was thus believed to represent an advertisement for a brothel, and it is a realistic illustration of a flat left foot. By the studies of Wokaunn, Ferenčić, and Mikolaučić in 2013, the flatfoot diagnosis has been confirmed by arch index calculation [4].
Probably the foot belongs to an adult man with a foot that was size 39/40 by current standards (EU sizing). He could have been a worker deployed to road construction or perhaps an artist expressing his inspiration or a seafarer who came from the port in search of some pleasure or simply a local passer-by.
In the same era, Galen (Pergamum, 129 AD–Rome 201 AD), the most famous Greek physician of antiquity after Hippocrates, was the first author to describe the pes planus as a deviation from normal foot anatomy, characterising the patients as “λειοποδες” (liopothes), which means people with smooth feet [35]. This can be considered the first historical definition of the pes planus in the second century A.D. Galen deals with the bony anatomy of the foot in his book On Bones for Beginners in chapter 24 dedicated to the tarsus and in chapter 25 describing the metatarsus (pethion) and the toes (Fig. 4).
Fig. 4.
Galen and Ephesus: a the imprint of the left foot in the ancient city of Ephesus; b portrait of Galen from The Botanical Garden Library, University of Padova
The anatomical studies of Leonardo Da Vinci and Girolamo Fabrici d’Acquapendente
No significant advances or developments in medical practices occurred after the fall of the Roman Empire until the Renaissance, a period of progress in European medical knowledge with renewed interest in the ideas of the ancient Greek and Roman civilisations.
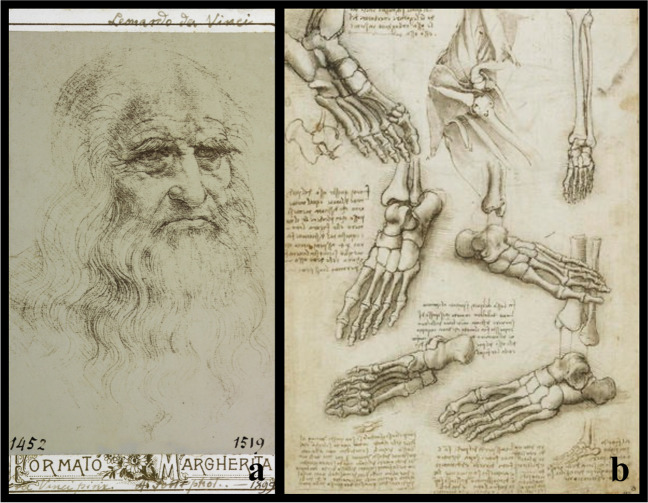
Leonardo da Vinci (Anchiano 1452–Amboise 1519) became the unassailable icon of this era with his contributions in the fields of science, anatomy, and technology [36]. Evidenced mostly in his over 13,000 pages of drawings and notebooks, his interests in anatomy and mechanics were well documented, including an understanding of how he believed the foot and ankle worked, stating: “The human foot is a masterpiece of engineering and a work of art”. Most of these drawings were created between 1510 and 1511 and gathered in Anatomic Manuscripts A, B, and C, now preserved in Windsor Castle as part of the Royal Collection [37]. He performed about 30 cadaver dissections at Santa Maria Nuova Hospital in Florence and the Santo Spirito Hospital in Rome. In Anatomic Manuscript A, some drawings of dissected and prepared specimens with soft tissues stripped off of a pes planus deformity are shown. Leonardo intended to publish this material as an illustrated treatise, but at his death on 2 May 1519, the drawings remained among his private papers and were bequeathed to his young disciple, Francesco Melzi (Milano, 1491–Vaprio d'Adda, 1570) [38] (Fig. 5).
Fig. 5.
Leonardo Da Vinci (1452-1519): a portrait of the Italian artist and anatomist, from The Botanical Garden Library, University of Padova; b drawing of the foot bones from Anatomic Manuscript A, from The Royal British Library
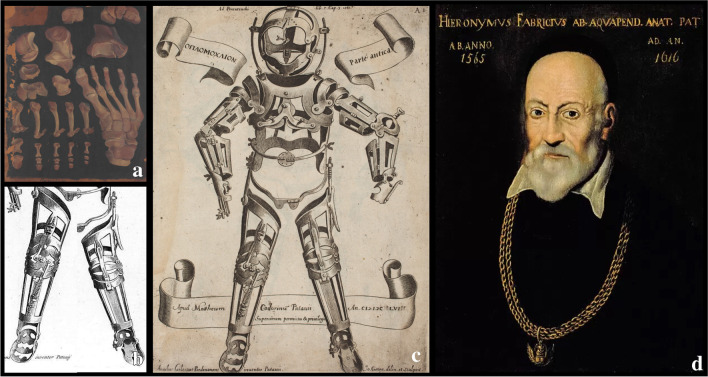
In the same era, Girolamo Fabrici d’Acquapendente (Acquapendente 1533–Padova 1619), an Italian anatomist, surgeon, and physiologist from Padua University, considered a precursor of modern orthopaedics, invented an external corrective device for the treatment of congenital and acquired deformities, the Oplomochlion. In 1594, he founded the first permanent anatomical theatre, still preserved in the Palazzo del Bo in Padua, in which he could study and teach anatomy based on cadaveric dissections.
The Oplomochlion consisted of a collection of very diverse orthotic, prosthetic, and surgical metal instruments arranged with a demonstrative purpose and a topographic criterion. In its distal part, it has an apparatus for correcting various deformities of the feet, in particular valgus deformity of the hindfoot and congenital talipes equinovarus. He understood that the bone tissue, together with the tendons and ligaments, is only pliant and malleable in children and adolescents. For this reason, Acquapendente stated that malformations such as those mentioned previously and pes planus could only be corrected in very young individuals by using specific parts of his Oplomochlion [39] (Fig. 6).
Fig. 6.
a Italian representation of right foot from dorsal view, 1575–1625, paint by G. F. d’Acquapendente, from “Theatrum totius animalis fabricae – De anatomia ossium”. Rari 111.21; Marciana National Library in Venice; b inferior part (legs) and c complete anterior view (pars antica) of the Oplomochlion form Fabrici’s Operationes chirurgicae (1647); d anonymous, Portrait of Girolamo Fabrici d'Acquapendente (Insignia of the Order of St. Mark of the Republic of Venice)
Conservative treatments: from antiquity to the twenty-first century
From ancient Egypt (3900 B.C.–342 A.D.) to the medieval period (500 A.D.–1400 A.D.), wood orthosis was the only treatment for Hugh Owen Thomas (Anglesey 1834–Liverpool 1891) and the management of pes planus. The first orthosis discovered throughout history is reported to come from the 5th Egyptian Dynasty, which is equivalent to 2750 B.C.–2625 B.C., and is a wood splint made for a fractured limb [40].
In the following periods, nothing can be found about the exact development of orthoses for flat feet in the literature. What we know is that materials have evolved and were later replaced with metal and leather which are either heavy, bulky, or thick, making them uncomfortable for the wearers. After the renaissance era (1400–1600) and the age of revolution (1700 –1850), the development of orthoses and prostheses showed a rapid change in shapes, structure, and composition [40].
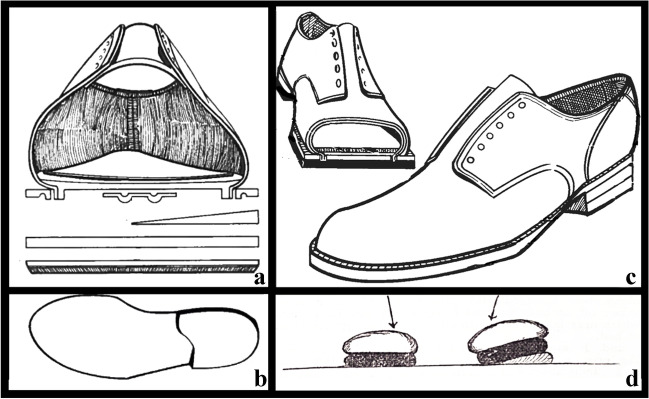
In 1876, Thomas invented a splint, which was used to treat deformities of the lower limb, including flatfoot. It was simple in design with the main objective of immobilising the lower limb. The splint was made from a padded metal ring attached to leather that was attached to an angled bar extending from the groin to below the foot on both sides of the leg. Basically, this device was a heel with an antero-medial extension [41] (longer than the standard) to add support to the medial arch of the midfoot [42] (Fig. 7).
Fig. 7.
Early conservative treatments (nineteenth century): a anterior section of the Thomas heel; b isolated Thomas heel; c complete shoe with the Thomas heel; d) stylized representation of an early orthesis used for the varus/valgus correction
In 1884, Alexander Ogston (Aberdeen 1844–Aberdeen 1929), an English surgeon remembered for being the first to describe Staphylococcus aureus, published an article in The Bristol Medico-Chirurgical Journal titled “On flatfoot, and its cure by operation” [43]. He wrote: “it is true that by rest and time the pain that accompanies the deformity becomes ameliorated or disappears, […] but the deformity does not disappear or even become materially diminished”. The therapy was therefore based on prolonged rest, with or without rigid bandages, and on the use of orthoses and braces. In particular, what was used was: “Boots with the inner margins of the soles raised, arched steel supports under the inner side of the sole, well moulded pads of cork and other materials, or hollow cushions of caoutchouc […]. Lateral supports to counteract the valgus position […]”. Another option was the so-called Langenbeck method, for child flatfoot: forced manual reduction of plantar flatness and subsequent immobilisation of the foot in plaster bandages for about three months [43–45].
Improvement in orthosis materials for flatfoot management occurred only after 100 years. During this period, the second industrial revolution (1870–1914) led to the discovery of plastic. In the 1960s, Yates and Lehneis wrote the first article about replacing metal orthoses with thermoformed plastics. It was a matter of discussion at first; however, after some investigation, it was found that plastic has more advantages than metal. It is light, hygienic, form-fitting, and noise-free. Unlike metal orthoses, plastic orthoses are thin enough to be worn under the user’s clothes, thus increasing the cosmetic value. Since then, thermoformed plastics have started to dominate the orthotic and prosthetic fields [46].
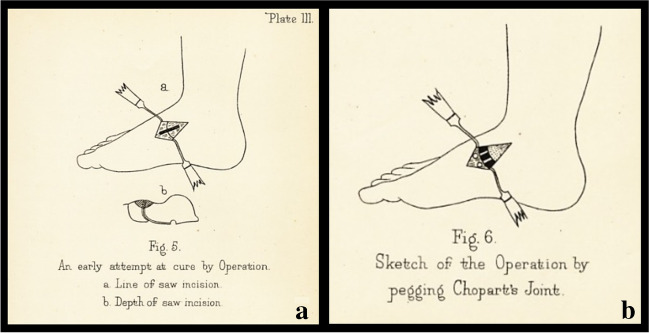
First surgical proposals for flatfoot correction
The surgical technique, described by Ogston in 1884, for flatfoot correction consisted of a medial incision below the ankle, joint exposure, removal of articular parts of the scaphoid and talus, reduction of the deformity, and subsequent stabilisation with an ivory block placed between the two bones. In the post-operative period, plaster casts were applied and then removed after four days to four weeks with discharge (bed rest) for two to three months. The results were reported as excellent, as the deformity remained reduced over time [43] (Fig. 8).
Fig. 8.
Surgical approach described by Ogston in Bristol Med Chir J (1884): a skin incision; b Chopart’s joint
In 1885, William Stokes (Dublin 1804–Dublin 1878), in his article “Astragaloid Osteotomy in the Treatment of Flat-Foot”, advised practicing the same incision without opening the ankle joint, modifying Ogston’s technique. He recommended performing an osteotomy to remove a wedge-shaped part of the head of the talus with an inferior base to restore the foot arch by abduction and supination. He expressed his scepticism about the flatfoot conservative treatment writing: “noticing how uniformly unsuccessful the attempts are to permanently remedy the deformity by any of the routine lines of practice, pushing up the arch of the foot and keeping it in that position by any of the various mechanical adjustments designed for this purpose” [44].
After this period, nothing can be found in the scientific literature over the subsequent 50 years regarding new deformity correction techniques until the second World War. In 1940, A.S. Blundell Bankart (Exter 1879–Northwood 1951) published a paper in The British Medical Journal titled “The treatment of flatfoot” in which he described six different types of flatfeet: the “congenital flatfoot”, presented at birth; the “Mobile flatfoot”, a deformity due to an incorrect posture typical of children and adolescents; the “Stiff flatfoot”, caused by fibrous adhesions, by tarsal coalition (fusion of two or more of the tarsal bones) [47], or by an increase in ligamentous thickness due to pre-existing reducible flatfoot or to outcomes of trauma or rheumatism; the “Contracted flatfoot”, fibrous flatfoot associated with claw toes and hallux valgus; the “Rigid (osseous) flatfoot”, caused by conditions of generalised arthrosis or outcomes of foot trauma; and finally the “Spasmodic flatfoot”, a typical condition of male adolescents between 13 and 18 years characterised by abduction and eversion of the foot, of unknown aetiology [48].
In the same article, Bankart gave useful indications for child flatfoot: “the treatment […] is uncertain and often disappointing. The most common method is manipulation under anaesthesia and fixation of the foot in plaster in the inverted position. […] Afterwards, he should wear an outside steel with a valgus T-strap to prevent passive eversion of the foot. In some very resistant cases, arthrodesis of the astragalo-scaphoid joint has been done” [48].
About 40 years later, in 1979, Douglas C. S. Brown wrote in the article titled “The Pediatric Foot”: “since many infant feet improve with arch supports, and many with flat feet do not have problems, it is hard to justify treating them. […] Certainly, the little scaphoid pads and 4 mm wedges do not harm, but combined with expensive shoes help perpetuate the myth that all this is necessary” [49].
Modern and current operative procedures for flatfoot (20th–21st centuries)
It is now known that foot deformity differs in aetiology and treatment between children and adults. In most cases and when the patient is asymptomatic, it does not need therapy even if it is a severe form [50]. On the contrary, in symptomatic cases, most of the authors agree on surgical therapy because of the low efficacy of conservative treatment (corrective shoes, custom-made arch supports, custom-made insoles, among others) [51–53].
Until now, the most popular corrective procedures described have been osteotomies, arthrodesis of one or more foot and ankle joints, arthrorisis, tendon lengthening and transfers, and hindfoot correction surgery. Combinations of these procedures have also been reported.
Osteotomies
Over time, the most widespread osteotomies and their variants have been numerous: the medial heel bone osteotomy; elongation of the lateral column through the calcaneus or cuboid; and osteotomy of the medial cuneiform, of the first metatarsal, and of the calcaneus.
Among the first described, Trendelenburg (1889) proposed a supramalleolar varising osteotomy of the fibula and tibia; Garrè and Kuttner (1914) recommend a personalised wedge resection of the talo-navicular joint; Perthes (1985) instead devised the “shaping double osteotomy”, an osteotomy with medial subtraction and lateral addition; Wilms (1919) recommended talonavicular arthrodesis and insertion of a bone wedge (taken from the head of the talus) into the calcaneocuboid joint.
The following are among the modern ones: Chambres (1946), Baker and Hill (1964), and Selakovich (1973) proposed additional subthalamic osteotomies; Baker and Hill recommended surgery for spastic neurologic flatfoot (1964); Regnauld (1974) performed an extra-articular osteotomy of the neck of the talus and the body of the scaphoid, lengthening the Achilles tendon [54]; the Evans calcaneal osteotomy, first described by Dillwyn Evans (Cardiff 1910–Cardiff 1974) in a post-mortem article published in 1975, resumed Perthes’ osteotomy, routinely used by foot and ankle surgeons to correct both paediatric and adult pes planovalgus deformities by performing an osteotomy in the neck of the calcaneus where a trapezoidal wedge of tricortical bone is placed [55].
Calcaneal osteotomy has become a reliable and widely used technique in the operative correction of hindfoot deformity [56]. The lateral approach originally described by Atkins in 1992 [57] has now been developed through anatomical cadaveric and clinical studies to improve wound healing and minimise the disruption to neighbouring neurovascular structures (sural nerve and branches of the peroneal artery). To reduce the rate of complications, a minimally invasive surgical (MIS) technique based on a low-speed, high-torque burr has been adopted in the last 20 years [56, 58, 59].
Arthrodesis
The origins of the triple arthrodesis date back to the early 1900s when the procedure was aimed to treat different conditions: idiopathic pes cavus and planus, deformities related to paralytic conditions of the foot [60]. In 1908, Royal Whitman (Portland 1857–New York 1946) devised a surgical treatment to address calcaneovalgus deformity due to neuromuscular abnormalities. He described the removal of the talus and backward displacement of the foot, though it was not successful for calcaneovalgus deformity [61]. In 1921, Hoke (Lincolnton 1874–USA 1944) proposed a triple arthrodesis where a portion of the talus was resected and the residual part remodelled with the fusion of the subtalar and calcaneocuboid joints [62]. This technique was in use for about 50 years. In 1978, J. W. Duncan published an article in which he found a 6.5% rate of osteonecrosis of the talus when the talar head resection was performed proximal to the origin of the artery of the tarsal canal [63]. Hoke’s technique was successfully modified by performing the resection distal to the artery. This technique is no longer used as it has been seen to lead to degenerative changes in the nearby joints over time [64].
Arthrorisis
The arthrorisis techniques involve the placement of an implant or bone graft within the tarsal sinus to limit subtalar joint movement, to improve the longitudinal arch, and to reduce the valgus of the subtalar joint. Arthrorisis procedures were originally designed for paediatric treatment and generally involve joint-sparing techniques that correct the flatfoot deformity while preserving foot function. This approach stems from extraarticular subtalar arthrodesis, first described by Grice in 1952, grafting a block of corticocancellous bone harvested from the tibia or iliac crest [65]. Also Chambers, in 1946, proposed to fill the sinus tarsi with an autologous bone graft [66]. In 1962, Haraldsson wrote that the goal of the flatfoot correction procedure had not to be the block but the limitation of joint movement, a concept subsequently reaffirmed by LeLièvre in 1970 [67].
Carried out for the first time by Recaredo Alvarez [68, 69] in 1972, the calcaneostop technique was used by Burutaran [70] in 1979, he described the results achieved with this surgical method stabilizing the heel with astragalic rise, hindering the valgisation. Later, Pisani [71], by introducing some modifications on the positioning of the screw, obtained a double effect of remodulation of the foot with respect of the articular and sinus-tarsal structure, historically paving the way for new additional corrective solutions.
Four years later, Subotnick described the use of a silicone implant inserted into the sinus tarsi without being fixed [72], while in 1979, Lanham used the stem of a Swanson prosthesis. Later, Volger (1980) proposed to create housing in the calcaneus with a burr for the stem of the same implant to prevent its mobilisation. In 1983, Smith and Millar described the use of a polyethylene device (“STA-peg”) fixed in the heel [73, 74]. A few years later, Giannini et al. developed an expansive device to be inserted into the sinus tarsi, which they subsequently improved through the use of bioresorbable materials [75]. The Maxwell–Brancheau arthrorisis (MBA) implant, a large cylinder-shaped titanium screw, and the Giannini flatfoot expanding implant, a Teflon/stainless steel expansion drywall anchor design, are perhaps the most commonly used implants [75].
Tendon lengthening and transfer
In 1936, Kulowski reported an effusion into the tendon sheath of the tibialis posterior tendon for the first time [76]; then in 1950, Lapidus and Seidenstein reported two cases of tenosynovitis of the same structure [77]. Subsequently, Kettelkamp and Alexander published the results of surgical exploration in adult patients with a typical combination of painful flatfoot deformity with tenderness and swelling along the sheath of the tibialis posterior tendon. They found in two of them that the tendon had ruptured in the mid-portion, and in one of them, it had avulsed from the navicular insertion [78]. In 1974, Goldner was one of the first surgeons to perform a replacement of the tibialis posterior tendon using flexor digitorum longus and flexor hallucis longus [79]. This is a case series on 9 patients, treated using the advancement of the posterior tibial tendon and plication of the medial ligaments to decrease the flatfoot deformity. Among these patients, three were teenagers (11, 15, and 18 years old) with traumatic flatfoot. All the others were middle aged with chronic tenosynovitis [79].
Hindfoot correction surgery
The first technique of hindfoot correction surgery was described by Golding-Bird in 1888 and was based on scaphoid and/or astragalus head excision [80]. In 1927, Miller proposed a scaphoid-cuneiform and cuneiform-metatarsal arthrodesis with medial access to correct the deformity [81]. This procedure was modified by Hoke, introducing the first cuneiform osteotomy [82]. Meanwhile, Durham proposed a scapho-cuneiform arthrodesis stabilised with a K-wire or a screw [83]. In 1929, Kidner and Albanese reinserted plantarly and laterally the posterior tibial tendon with a medial resection of the scaphoid and the first cuneiform. Subsequently, Natiello came up with the tenodesis of the tibialis anterior and posterior, and Pisani described the removal of the calcaneal-scaphoid ligament tissue with a fixation of the tibialis posterior tendon.
Conclusions
During the centuries, some therapeutic strategies, especially conservative ones, have never radically changed in their substance, while the operative ones have become the protagonists of an extraordinary evolution during the twentieth century up to the present. Nevertheless, after more than 2000 years of history, there is no consensus regarding the best solution for the flatfoot. This lack of a gold standard treatment seems to be the result of multiple points of view about pes planus, and many authors, also quoted in the present study, seem to have spent more time trying to identify the best corrective method rather than to clearly answer a crucial question on this issue: is flatfoot a pathology, anatomical condition, or a mere phenotypic feature of the human body?
Author contribution
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Carlo Biz, Mariachiara Cerchiaro, Fabiana Mori, Alessandro Rossin, Mattia Ponticiello, Alberto Crimì, and Pietro Ruggieri. The first draft of the manuscript was written by Carlo Biz and Mariachiara Cerchiaro, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
Open access funding provided by Università degli Studi di Padova within the CRUI-CARE Agreement.
Data availability
Any research materials of this study are available at our institution and can be accessed.
Code availability
Not applicable.
Declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Carlo Biz, Email: carlo.biz@unipd.it.
Mariachiara Cerchiaro, Email: chiaracerchiaro@gmail.com.
Fabiana Mori, Email: fabiana.mori@studenti.unipd.it.
Alessandro Rossin, Email: alessandro.rossin.3@studenti.unipd.it.
Mattia Ponticiello, Email: mattia.ponticiello@studenti.unipd.it.
Alberto Crimì, Email: albe.crim@gmail.com.
Pietro Ruggieri, Email: pietro.ruggieri@unipd.it.
References
- 1.Krogman WM (1951) The scars of human evolution. Sci Am 185(6): 54–57. JSTOR. http://www.jstor.org/stable/24950554. Accessed 2 Sept 2022
- 2.Helfet AJ (1980) Disorders of the foot. Lippincott Williams & Wilkins, Philadelphia
- 3.Standring S (2017) Anatomia Del Gray 41 Ed.: 2 Volumi. Edra
- 4.Wokaunn M, Ferenčić SF, Mikolaučić M. The pictogram of the pes planus from the first century AD. Int Orthop. 2013;37(9):1871–3. doi: 10.1007/s00264-013-2020-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aiello L, Dean C (2002) Chapter twenty-three - the hominoid foot, Editor: Leslie Aiello, Christopher Dean, An Introduction to Human Evolutionary Anatomy, Academic Press, Pages 507–538, ISBN 9780120455911. 10.1016/B978-0-08-057100-3.50027-4
- 6.Isidro A. Comparative anatomy of the posterior foot, features derived from the type of locomotion. Biomecánica. 1997;9:137–147. [Google Scholar]
- 7.Lamarck JB (1809) Philosophie zoologique. Paris: Dentu. 1820. Système analytique des connaissances positives de l’homme, restreintes à celles qui proviennent directement ou indirectement de l’observation. Paris: Belin
- 8.Darwin C. Descent of man. London: Appleton; 1871. [Google Scholar]
- 9.Hatala KG, Demes B, Richmond BG. Laetoli footprints reveal bipedal gait biomechanics different from those of modern humans and chimpanzees. Proc Biol Sci. 2016;283(1836):20160235. doi: 10.1098/rspb.2016.0235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johanson DC, Edgar B (1996). From Lucy to language. Simon and Schuster
- 11.Venkadesan M, Yawar A, Eng CM, Dias MA, Singh DK, Tommasini SM, Haims AH, Bandi MM, Mandre S. Stiffness of the human foot and evolution of the transverse arch. Nature. 2020;579(7797):97–100. doi: 10.1038/s41586-020-2053-y. [DOI] [PubMed] [Google Scholar]
- 12.Kimbel WH, Delezene LK. “Lucy” redux: a review of research on Australopithecus afarensis. Am J Phys Anthropol. 2009;140(Suppl 49):2–48. doi: 10.1002/ajpa.21183. [DOI] [PubMed] [Google Scholar]
- 13.Johanson DC, White TD, Coppens Y (1978) A new species of the genus Australopithecus (Primates: Hominidae) from the Pliocene of eastern Africa. White & Coppens in Kirtlandia 28:1–14. https://biostor.org/reference/193077
- 14.DeSilva JM, Throckmorton ZJ (2010) Lucy’s flat feet: the relationship between the ankle and rearfoot arching in early hominins. PLoS One 5(12):e14432. 10.1371/journal.pone.0014432 [DOI] [PMC free article] [PubMed]
- 15.Conroy GC, Rose MD. The evolution of the primate foot from the earliest primates to the Miocene hominoids. Foot Ankle. 1983;3(6):342–364. doi: 10.1177/107110078300300604. [DOI] [PubMed] [Google Scholar]
- 16.Saldías E, Malgosa A, Jordana X, Martínez-Labarga C, Coppa A, Rubini M, Vila B, Isidro A (2021) A new methodology to estimate flat foot in skeletal remains: the example of Mediterranean collections. HOMO J Comp Hum Biol 2021. 10.1127/homo/2021/1320 [DOI] [PubMed]
- 17.Masao FT, Ichumbaki EB, Cherin M, Barili A, Boschian G, Iurino DA, Menconero S, Moggi-Cecchi J, Manzi G. New footprints from Laetoli (Tanzania) provide evidence for marked body size variation in early hominins. Elife. 2016;5:e19568. doi: 10.7554/eLife.19568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Day MH, Napier JR. Hominid fossils from Bed I, Olduvai Gorge, Tanganyika. Fossil foot bones. Nature. 1964;201:967–970. doi: 10.1038/201969a0. [DOI] [PubMed] [Google Scholar]
- 19.Sorrentino R, Stephens NB, Marchi D, DeMars LJ, Figus C, Bortolini E, ... Benazzi S (2021) Unique foot posture in Neanderthals reflects their body mass and high mechanical stress. J Hum Evol 161: 103093. 10.1016/j.jhevol.2021.103093 [DOI] [PubMed]
- 20.Trinkaus E. Anatomical evidence for the antiquity of human footwear use. J Archaeol Sci. 2005;32(10):1515–1526. doi: 10.1016/j.jas.2005.04.006. [DOI] [Google Scholar]
- 21.Glass N (2020) Inside the final resting place of Tutankhamun’s treasures, CNN travel destination Egypt, 8th August. https://edition.cnn.com/travel/article/tutankhamun-grand-egyptian-museum/index.html. Accessed 2 Sept 2022
- 22.Seshadri KG. The breasts of Tutankhamun. Indian J Endocrinol Metab. 2012;16(3):429–30. doi: 10.4103/2230-8210.95696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hawass Z, Gad YZ, Ismail S, Khairat R, Fathalla D, Hasan N, Ahmed A, Elleithy H, Ball M, Gaballah F, Wasef S, Fateen M, Amer H, Gostner P, Selim A, Zink A, Pusch CM. Ancestry and pathology in King Tutankhamun’s family. JAMA. 2010;303(7):638–47. doi: 10.1001/jama.2010.121. [DOI] [PubMed] [Google Scholar]
- 24.Hussein K, Matin E, Nerlich AG. Paleopathology of the juvenile pharaoh Tutankhamun-90th anniversary of discovery. Virchows Arch. 2013;463(3):475–479. doi: 10.1007/s00428-013-1441-1. [DOI] [PubMed] [Google Scholar]
- 25.Helck W (1971) Die Beziehungen Ägyptens zu Vorderasien im 3. und 2. Jahrtausend v. Chr. Harrassowitz, Wiesbaden
- 26.Martin GT (2012) A bibliography of the Amarna period and its aftermath: the reigns of Akhenaten, Smenkhkare, Tutankhamun and Ay (c. 1350–1321 BC). Routledge. 10.4324/9780203038284
- 27.Kozloff AP (2012) Amenhotep III: Egypt’s radiant pharaoh. Cambridge University Press, Cambridge
- 28.Moran ET, Volkwein JF. The cultural approach to the formation of organizational climate. Hum Relat. 1992;45(1):19–47. doi: 10.1177/001872679204500102. [DOI] [Google Scholar]
- 29.Redford DB. Akhenaten: the heretic king. Princeton: Princeton University Press; 1984. [Google Scholar]
- 30.Rühli FJ, Ikram S. Purported medical diagnoses of Pharaoh Tutankhamun, c. 1325 BC. Homo. 2014;65(1):51–63. doi: 10.1016/j.jchb.2013.08.006. [DOI] [PubMed] [Google Scholar]
- 31.Brandt G (2013) Did Tutankhamun suffer from hypophosphatasia? A hypothetical approach. Anthropologischer Anzeiger; Bericht uber die biologisch-anthropologische Literatur 70(3): 249–260. 10.1127/0003-5548/2013/0322 [DOI] [PubMed]
- 32.Tismmann C, Meyer CG. Malaria, mummies, mutations: Tutankhamun’s archaeological autopsy. Trop Med Int Health. 2010;15(11):1278–1280. doi: 10.1111/j.1365-3156.2010.02614.x. [DOI] [PubMed] [Google Scholar]
- 33.Lorenzen ED, Willerslev E. King Tutankhamun’s family and demise. Jama. 2010;303(24):2471–2475. doi: 10.1001/jama.2010.822. [DOI] [PubMed] [Google Scholar]
- 34.Encyclopædia Britannica (2013) Ephesus. http://www.britannica.com/EBchecked/topic/189556/Ephesus. Accessed 3 Sept 2022
- 35.Letters to author (2004) J Am Podiatric Med Assoc 94(5): September/October
- 36.Săceleanu MV, Mohan AG, Marinescu AA, Marinescu A, Ciurea AV. Leonardo da Vinci - ingenious anatomist: 500 years since the death of the famous erudite. Rom J Morphol Embryol. 2019;60(4):1391–1395. [PubMed] [Google Scholar]
- 37.Jones R. Leonardo da Vinci: anatomist. Br J Gen Pract. 2012;62(599):319–319. doi: 10.3399/bjgp12X649241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Clayton M, Philo R (2010) Leonardo daVinci: TheMechanicsofMan. Los Angeles: Getty
- 39.Biz C, Brunati A, Belluzzi E, Ruggieri P, Masiero S, Rippa Bonati M. Girolamo Fabrici d'Acquapendente and the Oplomochlion: the several applications of an effective rehabilitation tool. Am J Med Sci. 2020;359(1):1–7. doi: 10.1016/j.amjms.2019.10.007. [DOI] [PubMed] [Google Scholar]
- 40.Shahar FS, Hameed Sultan MT, Lee SH, Jawaid M, Md Shah AU, Safri SNA, Sivasankaran PN. A review on the orthotics and prosthetics and the potential of kenaf composites as alternative materials for ankle-foot orthosis. J Mech Behav Biomed Mater. 2019;99:169–185. doi: 10.1016/j.jmbbm.2019.07.020. [DOI] [PubMed] [Google Scholar]
- 41.Gray B, Santy-Tomlinson J. The Thomas’ splint: application and patient care. Int J Orthop Trauma Nurs. 2018;30:20–22. doi: 10.1016/j.ijotn.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 42.Inglis AM. Common foot problems in young children. Can Med Assoc J. 1961;84(7):363–70. [PMC free article] [PubMed] [Google Scholar]
- 43.Ogston A. On flat-foot and its cure by operation. Bristol Med Chir J. 1883;2(3):1–20. [PMC free article] [PubMed] [Google Scholar]
- 44.Stokes WI. Astragaloid osteotomy in the treatment of flat-foot. Ann Surg. 1885;2(10):279–85. doi: 10.1097/00000658-188507000-00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.The Treatment of Flat Foot (1892) The hospital 13(318):73 [PMC free article] [PubMed]
- 46.Shamp JAK. Ankle foot orthoses — metal vs. Plastic. Clin Prosthetics Orthot. 1983;7:1–3. [Google Scholar]
- 47.Denning JR. Tarsal coalition in children. Pediatr Ann. 2016;45(4):e139–43. doi: 10.3928/00904481-20160309-01. [DOI] [PubMed] [Google Scholar]
- 48.Bankart AS. Treatment of flat-foot. Br Med J. 1940;1(4134):537–9. doi: 10.1136/bmj.1.4134.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brown DCS. The pediatric foot. Can Fam Physician. 1979;25:851–4. [Google Scholar]
- 50.Ueki Y, Sakuma E, Wada I. Pathology and management of flexible flat foot in children. J Orthop Sci. 2019;24(1):9–13. doi: 10.1016/j.jos.2018.09.018. [DOI] [PubMed] [Google Scholar]
- 51.Whitford D, Esterman A. A randomized controlled trial of two types of in-shoe orthoses in children with flexible excess pronation of the feet. Foot Ankle Int. 2007;28:715–723. doi: 10.3113/FAI.2007.0715. [DOI] [PubMed] [Google Scholar]
- 52.Wenger DR, Mauldin D, Speck G, et al. Corrective shoes and inserts as treatment for flexible flatfoot in infants and children. J Bone Joint Surg Am. 1989;71:800–810. doi: 10.2106/00004623-198971060-00002. [DOI] [PubMed] [Google Scholar]
- 53.Staheli LT. Planovalgus foot deformity. Current status. J Am Podiatr Med Assoc. 1999;89((2) (Feb)):94–99. doi: 10.7547/87507315-89-2-94. [DOI] [PubMed] [Google Scholar]
- 54.Cattaneo P, Fino G, Origo C, Rocca G, Rossi G, Bagliani GP. Revisione storica della chirurgia del piede piatto. Riv Ital Ort Trauma Ped. 1997;XIII(supplemento al fasc.1):129–144. [Google Scholar]
- 55.DeYoe BE, Wood J. The Evans calcaneal osteotomy. Clin Podiatr Med Surg. 2005;22(2):265–76. doi: 10.1016/j.cpm.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 56.Kendal AR, Khalid A, Ball T, Rogers M, Cooke P, Sharp R. Complications of minimally invasive calcaneal osteotomy versus open osteotomy. Foot Ankle Int. 2015;36(6):685–690. doi: 10.1177/1071100715571438. [DOI] [PubMed] [Google Scholar]
- 57.Eastwood DM, Irgau I, Atkins RM. The distal course of the sural nerve and its significance for incisions around the lateral hindfoot. Foot Ankle. 1992;13(4):199–202. doi: 10.1177/107110079201300406. [DOI] [PubMed] [Google Scholar]
- 58.Isidro Llorens A (2019) Pie egipcio. Los egipcios y sus pies. In: Notas con buen Pie y otros relatos. Punto Rojo Libros S., Sevilla, pp 161–176
- 59.Bernasconi A, Ray R. Role of minimally invasive surgery in adult flatfoot deformity. Foot Ankle Clin. 2020;25(3):479–491. doi: 10.1016/j.fcl.2020.05.007. [DOI] [PubMed] [Google Scholar]
- 60.Erard MUE, Sheean MAJ, Sangeorzan BJ. Triple arthrodesis for adult-acquired flatfoot deformity. Foot Ankle Orthop. 2019;4(3):2473011419849609. doi: 10.1177/2473011419849609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Whitman R. Further observations on the treatment of paralytic talipes calcaneus by astragalectomy and backward displacement of the foot. Ann Surg. 1908;47(2):264–273. doi: 10.1097/00000658-190802000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hoke M. An operation for stabilizing paralytic feet. Am J Orthop Surg. 1921;3:494–507. [Google Scholar]
- 63.Duncan JW, Lovell WW. Hoke triple arthrodesis. J Bone Joint Surg Am. 1978;60(6):795–798. doi: 10.2106/00004623-197860060-00012. [DOI] [PubMed] [Google Scholar]
- 64.Mosca VS. Flexible flatfoot in children and adolescents. J Child Orthop. 2010;4:107–121. doi: 10.1007/s11832-010-0239-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Grice DS. An extra-articular arthrodesis of the subastragalar joint for correction of paralytic flat feet in children. J Bone Joint Surg Am. 1952;34-A:927–56. doi: 10.2106/00004623-195234040-00020. [DOI] [PubMed] [Google Scholar]
- 66.Chambers EF. An operation for the correction of flexible flat feet of adolescents. West J Surg Obstet Gynecol. 1946;54:77–86. [PubMed] [Google Scholar]
- 67.LeLièvre J. Current concepts and correction in the valgus foot. Clin Orthop Relat Res. 1970;70:43–55. [PubMed] [Google Scholar]
- 68.Álvarez Rodríguez R. Calcáneo STOP. Rev Pie Tobillo. 2004;18(2):91–94. [Google Scholar]
- 69.Juanto MA, Fernandez EM, Mahfud M, Origo C. Nostra esperienza con la tecnica del calcaneo-stop secondo Recaredo Alvarez nel piede calcaneo-valgo. Riv It Orthop Traumatol Ped. 1998;14:35–42. [Google Scholar]
- 70.Burutaran JM. el Calcaneostop para lo tratamiento del valgo de talon infantile. Chir piede. 1979;4:319. [Google Scholar]
- 71.Pisani PC (2010) Il calcaneostop. Progressi in medicina e chirurgia vol. 19 pp 235–244. ed. Timeo, Bologna
- 72.Subotnick SI. The subtalar joint lateral extra-articular arthroereisis: a preliminary report. J Am Podiatry Assoc. 1974;64(9):701–11. doi: 10.7547/87507315-64-9-701. [DOI] [PubMed] [Google Scholar]
- 73.Viladot R, Torner CE, Rochera R. New surgical technique for the treatment of flat feet. Ann Med. 1976;6:80–87. [Google Scholar]
- 74.Smith SD, Millar EA (1983) Arthrorisis by means of a subtalar polyethylene peg implant for correction of hindfoot pronation in children. Clin Orthop Relat Res (181):15–23 [PubMed]
- 75.Giannini BS, Ceccarelli F, Benedetti MG, et al. Surgical treatment of flexible flatfoot in children a four-year follow-up study. J Bone Joint Surg Am. 2001;83-A(Suppl 2 Pt 2):73–79. doi: 10.2106/00004623-200100022-00003. [DOI] [PubMed] [Google Scholar]
- 76.Kulowski J. Tenosynovitis. General discussion and report of one case involving the posterior tibial tendon. J Wis State Med Assn. 1936;33:135–137. [Google Scholar]
- 77.Lapidus PW, Seidenstein H. Chronic non-specific tenosynovitis with effusion about ankle. J Bone Joint Surg. 1950;32-A:175–177. doi: 10.2106/00004623-195032010-00016. [DOI] [PubMed] [Google Scholar]
- 78.Kettelkamp DB, Alexander HH. Spontaneous rupture of the posterior tibial tendon. J Bone Joint Surg. 1969;51-A:759–764. doi: 10.2106/00004623-196951040-00014. [DOI] [PubMed] [Google Scholar]
- 79.Goldner JL, Keats PK, Bassett FH, Clippinger FW. Progressive talipes equinovalgus due to trauma or degeneration of the posterior tibial tendon and medial plantar ligaments. Orthop Clin North Am. 1974;5:39–51. doi: 10.1016/S0030-5898(20)31238-4. [DOI] [PubMed] [Google Scholar]
- 80.Golding-Bird CH. Operations on the tarsus in confirmed flat-foot. The Lancet. 1889;133(3423):677–678. doi: 10.1016/S0140-6736(01)90099-6. [DOI] [Google Scholar]
- 81.Miller OL. A plastic flat foot operation. JBJS. 1927;9(1):84–91. [Google Scholar]
- 82.Hoke Michael. An operation for the correction of extremely relaxed flat feet. J Bone Joint Surg. 1931;13(4):773–783. [Google Scholar]
- 83.Caldwell GD. Surgical correction of relaxed flatfoot by the Durham flatfoot plasty. Clin Orthop. 1953;2:221–226. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Any research materials of this study are available at our institution and can be accessed.
Not applicable.