Abstract
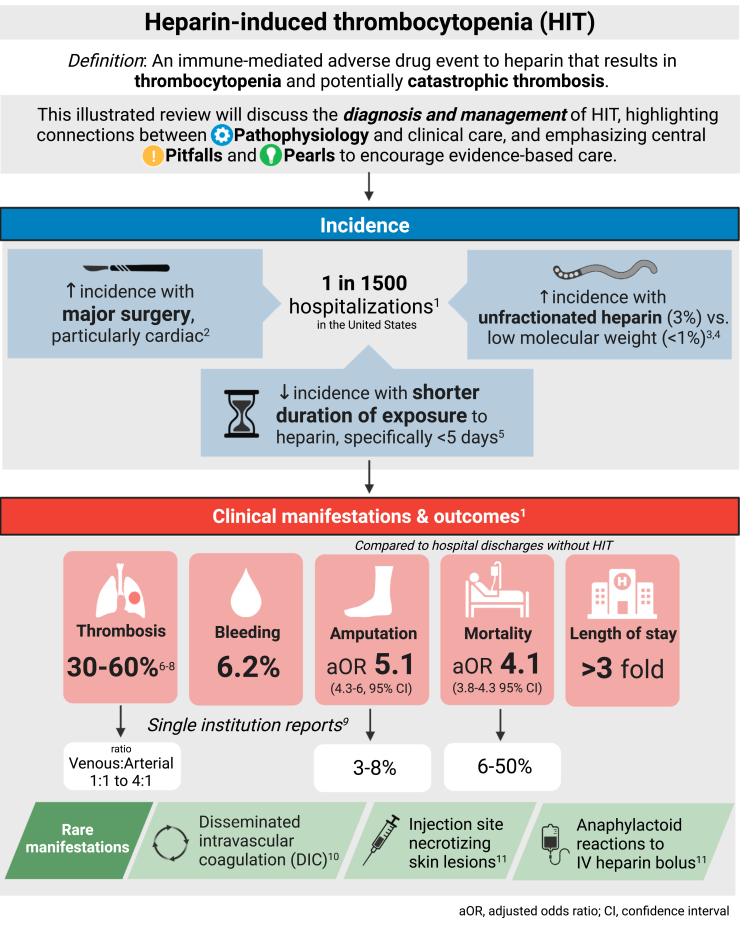
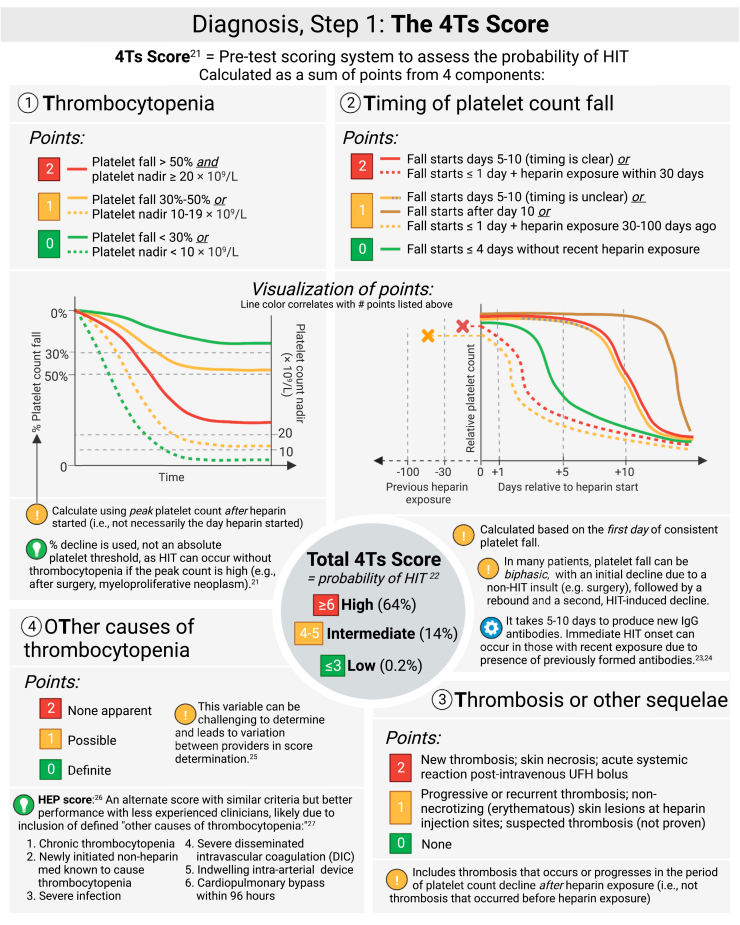
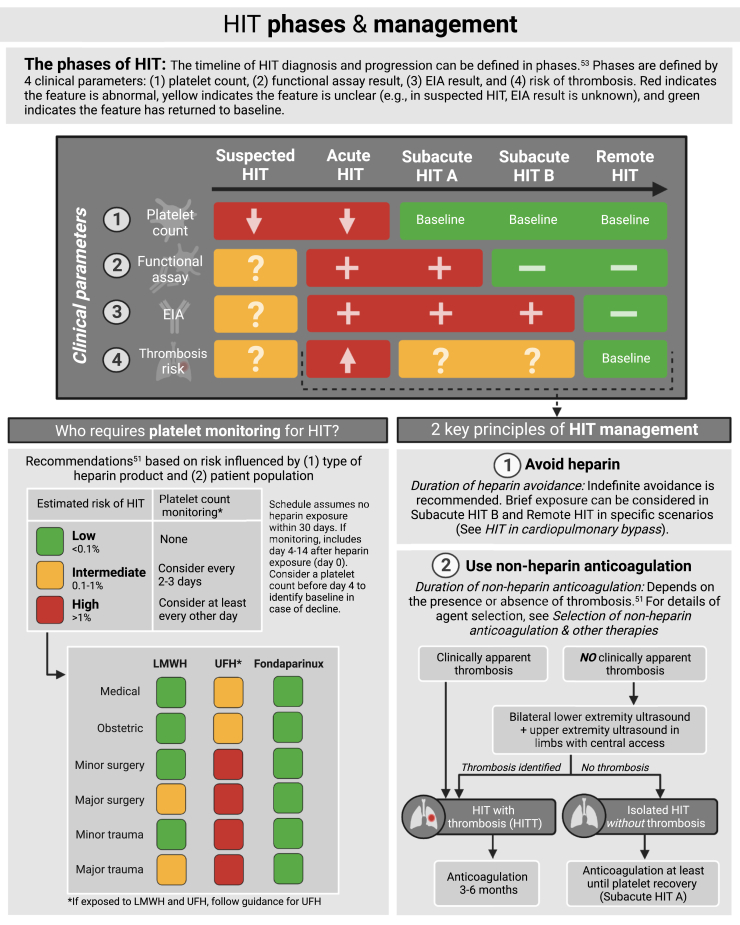
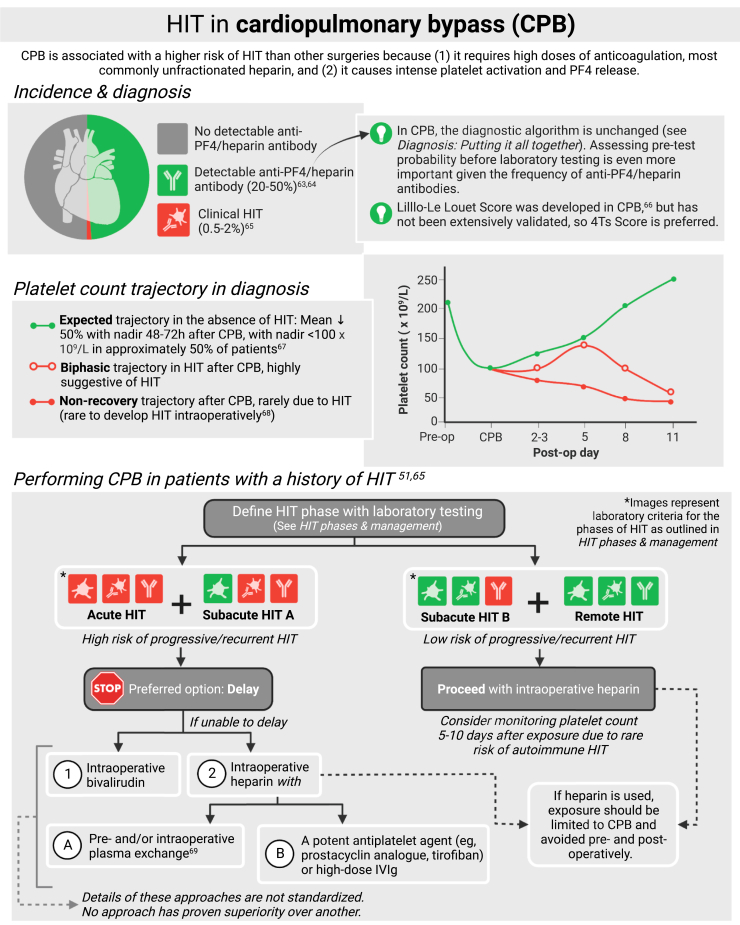
Heparin-induced thrombocytopenia (HIT) is an immune-mediated adverse drug effect from unfractionated or low-molecular-weight heparin that results in thrombocytopenia and potentially catastrophic thrombosis. HIT occurs due to the development of platelet-activating antibodies against multimolecular complexes of platelet factor 4 and heparin. Given the frequency of thrombocytopenia and heparin use among hospitalized patients, calculation of the 4Ts Score is recommended to identify patients at increased likelihood of HIT and direct further evaluation. In patients with an intermediate or high probability 4Ts Score, an immunoassay and functional assay are recommended to confirm or refute the diagnosis of HIT. Heparin avoidance and initiation of nonheparin anticoagulation are the mainstays of acute HIT management. In this illustrated review, we provide visual summaries of the diagnosis and management of HIT, highlighting connections between pathophysiology and clinical care as well as summarizing efforts in quality improvement in the field. We further emphasize common pitfalls and pearls in diagnosis and management to encourage evidence-based care. We include graphical representation of the unique challenges of HIT with cardiopulmonary bypass and also delineate autoimmune HIT and its subtypes.
Keywords: anticoagulants, drug-related side effects and adverse reactions, heparin, quality improvement, thrombosis
Essentials
-
•
Heparin-induced thrombocytopenia (HIT) is an immune adverse drug effect that results in low platelets and risk of thrombosis.
-
•
Use of the 4Ts Score is recommended to assess patient risk of HIT.
-
•
Sequential specialized testing is required to diagnose HIT.
-
•
Heparin avoidance and use of nonheparin anticoagulation are the mainstays of HIT management.
Acknowledgments
The authors thank Douglas Cines, MD, for his expert review of the manuscript. Illustrations created with BioRender.com.
Funding
The authors received no funding for this study.
Author contributions
J.M. conceptualized the manuscript and created the initial content and visualization. B.W. and A.C. provided critical review and revision.
Relationship disclosure
J.M. and B.W. report no relevant conflicts of interest. A.C. has served as a consultant for Synergy, MingSight, and the New York Blood Center and has received authorship royalties from UpToDate.
Footnotes
Handling Editor: Dr Michelle Sholzberg
References
- 1.Dhakal B., Kreuziger L.B., Rein L., Kleman A., Fraser R., Aster R.H., et al. Disease burden, complication rates, and health-care costs of heparin-induced thrombocytopenia in the USA: a population-based study. Lancet Haematol. 2018;5:e220–e231. doi: 10.1016/S2352-3026(18)30046-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pishko A.M., Cuker A. Heparin-induced thrombocytopenia in cardiac surgery patients. Semin Thromb Hemost. 2017;43:691–698. doi: 10.1055/s-0037-1602664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Warkentin T.E., Levine M.N., Hirsh J., Horsewood P., Roberts R.S., Gent M., et al. Heparin-induced thrombocytopenia in patients treated with low-molecular-weight heparin or unfractionated heparin. N Engl J Med. 1995;332:1330–1335. doi: 10.1056/NEJM199505183322003. [DOI] [PubMed] [Google Scholar]
- 4.Martel N., Lee J., Wells P.S. Risk for heparin-induced thrombocytopenia with unfractionated and low-molecular-weight heparin thromboprophylaxis: a meta-analysis. Blood. 2005;106:2710–2715. doi: 10.1182/blood-2005-04-1546. [DOI] [PubMed] [Google Scholar]
- 5.Smythe M.A., Koerber J.M., Mattson J.C. The incidence of recognized heparin-induced thrombocytopenia in a large, tertiary care teaching hospital. Chest. 2007;131:1644–1649. doi: 10.1378/chest.06-2109. [DOI] [PubMed] [Google Scholar]
- 6.Warkentin T.E., Sheppard J-A.I., Whitlock R.P. Temporal presentations of heparin-induced thrombocytopenia following cardiac surgery: a single-center, retrospective cohort study. J Thromb Haemost. 2022;20:2601–2616. doi: 10.1111/jth.15826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Warkentin T.E., Sheppard J.-A.I., Heels-Ansdell D., Marshall J.C., McIntyre L., Rocha M.G., et al. Heparin-induced thrombocytopenia in medical surgical critical illness. Chest. 2013;144:848–858. doi: 10.1378/chest.13-0057. [DOI] [PubMed] [Google Scholar]
- 8.Gruel Y., Vayne C., Rollin J., Weber P., Faille D., Bauters A., et al. Comparative analysis of a French prospective series of 144 patients with heparin-induced thrombocytopenia (FRIGTIH) and the literature. Thromb Haemost. 2020;120:1096–1107. doi: 10.1055/s-0040-1712957. [DOI] [PubMed] [Google Scholar]
- 9.Arepally G.M., Padmanabhan A. Heparin-induced thrombocytopenia: a focus on thrombosis. Arterioscler Thromb Vasc Biol. 2021;41:141–152. doi: 10.1161/ATVBAHA.120.315445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Warkentin T.E. Heparin-induced thrombocytopenia. Curr Opin Crit Care. 2015;21:576–585. doi: 10.1097/MCC.0000000000000259. [DOI] [PubMed] [Google Scholar]
- 11.Warkentin T.E., Roberts R.S., Hirsh J., Kelton J.G. Heparin-induced skin lesions and other unusual sequelae of the heparin-induced thrombocytopenia syndrome: a nested cohort study. Chest. 2005;127:1857–1861. doi: 10.1378/chest.127.5.1857. [DOI] [PubMed] [Google Scholar]
- 12.Bock P.E., Luscombe M., Marshall S.E., Pepper D.S., Holbrook J.J. The multiple complexes formed by the interaction of platelet factor 4 with heparin. Biochem J. 1980;191:769–776. doi: 10.1042/bj1910769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chong B.H., Fawaz I., Chesterman C.N., Berndt M.C. Heparin-induced thrombocytopenia: mechanism of interaction of the heparin-dependent antibody with platelets. Br J Haematol. 1989;73:235–240. doi: 10.1111/j.1365-2141.1989.tb00258.x. [DOI] [PubMed] [Google Scholar]
- 14.Gollomp K., Kim M., Johnston I., Hayes V., Welsh J., Arepally G.M., et al. Neutrophil accumulation and NET release contribute to thrombosis in HIT. JCI Insight. 2018;3 doi: 10.1172/jci.insight.99445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khandelwal S., Barnes A., Rauova L., Sarkar A., Rux A.H., Yarovoi S.V., et al. Complement mediates binding and procoagulant effects of ultralarge HIT immune complexes. Blood. 2021;138:2106–2116. doi: 10.1182/blood.2020009487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Suh J.S., Malik M.I., Aster R.H., Visentin G.P. Characterization of the humoral immune response in heparin-induced thrombocytopenia. Am J Hematol. 1997;54:196–201. doi: 10.1002/(sici)1096-8652(199703)54:3<196::aid-ajh4>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 17.Lindhoff-Last E., Gerdsen F., Ackermann H., Bauersachs R. Determination of heparin-platelet factor 4-IgG antibodies improves diagnosis of heparin-induced thrombocytopenia. Br J Haematol. 2001;113:886–890. doi: 10.1046/j.1365-2141.2001.02869.x. [DOI] [PubMed] [Google Scholar]
- 18.Greinacher A., Alban S., Omer-Adam M.A., Weitschies W., Warkentin T.E. Heparin-induced thrombocytopenia: a stoichiometry-based model to explain the differing immunogenicities of unfractionated heparin, low-molecular-weight heparin, and fondaparinux in different clinical settings. Thromb Res. 2008;122:211–220. doi: 10.1016/j.thromres.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 19.Cines D.B., Rauova L., Arepally G., Reilly M.P., McKenzie S.E., Sachais B.S., et al. Heparin-induced thrombocytopenia: an autoimmune disorder regulated through dynamic autoantigen assembly/disassembly. J Clin Apher. 2007;22:31–36. doi: 10.1002/jca.20109. [DOI] [PubMed] [Google Scholar]
- 20.Suvarna S., Espinasse B., Qi R., Lubica R., Poncz M., Cines D.B., et al. Determinants of PF4/heparin immunogenicity. Blood. 2007;110:4253–4260. doi: 10.1182/blood-2007-08-105098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lo G.K., Juhl D., Warkentin T.E., Sigouin C.S., Eichler P., Greinacher A. Evaluation of pretest clinical score (4 T's) for the diagnosis of heparin-induced thrombocytopenia in two clinical settings. J Thromb Haemost. 2006;4:759–765. doi: 10.1111/j.1538-7836.2006.01787.x. [DOI] [PubMed] [Google Scholar]
- 22.Cuker A., Gimotty P.A., Crowther M.A., Warkentin T.E. Predictive value of the 4Ts scoring system for heparin-induced thrombocytopenia: a systematic review and meta-analysis. Blood. 2012;120:4160–4167. doi: 10.1182/blood-2012-07-443051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Warkentin T.E., Kelton J.G. Temporal aspects of heparin-induced thrombocytopenia. N Engl J Med. 2001;344:1286–1292. doi: 10.1056/NEJM200104263441704. [DOI] [PubMed] [Google Scholar]
- 24.Lefler D.S., Cuker A., Linkins L.A., Warkentin T.E., Pishko A.M. Maximum 24-hour platelet count fall: metric for improving the diagnosis of heparin-induced thrombocytopenia among patients with intermediate probability 4Ts scores. J Thromb Haemost. 2020;18:2018–2024. doi: 10.1111/jth.14897. [DOI] [PubMed] [Google Scholar]
- 25.Crowther M., Cook D., Guyatt G., Zytaruk N., McDonald E., Williamson D., et al. Heparin-induced thrombocytopenia in the critically ill: interpreting the 4Ts test in a randomized trial. J Crit Care. 2014;29:470.e7. doi: 10.1016/j.jcrc.2014.02.004. 15. [DOI] [PubMed] [Google Scholar]
- 26.Cuker A., Arepally G., Crowther M.A., Rice L., Datko F., Hook K., et al. The HIT Expert Probability (HEP) Score: a novel pre-test probability model for heparin-induced thrombocytopenia based on broad expert opinion. J Thromb Haemost. 2010;8:2642–2650. doi: 10.1111/j.1538-7836.2010.04059.x. [DOI] [PubMed] [Google Scholar]
- 27.Pishko A.M., Fardin S., Lefler D.S., Paydary K., Vega R., Arepally G.M., et al. Prospective comparison of the HEP score and 4Ts score for the diagnosis of heparin-induced thrombocytopenia. Blood Adv. 2018;2:3155–3162. doi: 10.1182/bloodadvances.2018023077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Husseinzadeh H.D., Gimotty P.A., Pishko A.M., Buckley M., Warkentin T.E., Cuker A. Diagnostic accuracy of IgG-specific versus polyspecific enzyme-linked immunoassays in heparin-induced thrombocytopenia: a systematic review and meta-analysis. J Thromb Haemost. 2017;15:1203–1212. doi: 10.1111/jth.13692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cuker A., Ortel T.L. ASH evidence-based guidelines: is the IgG-specific anti-PF4/heparin ELISA superior to the polyspecific ELISA in the laboratory diagnosis of HIT? Hematology Am Soc Hematol Educ Program. 2009:250. doi: 10.1182/asheducation-2009.1.250. 2. [DOI] [PubMed] [Google Scholar]
- 30.Warkentin T.E., Sheppard J.I., Moore J.C., Sigouin C.S., Kelton J.G. Quantitative interpretation of optical density measurements using PF4-dependent enzyme-immunoassays. J Thromb Haemost. 2008;6:1304–1312. doi: 10.1111/j.1538-7836.2008.03025.x. [DOI] [PubMed] [Google Scholar]
- 31.Zwicker J.I., Uhl L., Huang W.Y., Shaz B.H., Bauer K.A. Thrombosis and ELISA optical density values in hospitalized patients with heparin-induced thrombocytopenia. J Thromb Haemost. 2004;2:2133–2137. doi: 10.1111/j.1538-7836.2004.01039.x. [DOI] [PubMed] [Google Scholar]
- 32.Sun L., Gimotty P.A., Lakshmanan S., Cuker A. Diagnostic accuracy of rapid immunoassays for heparin-induced thrombocytopenia. A systematic review and meta-analysis. Thromb Haemost. 2016;115:1044–1055. doi: 10.1160/TH15-06-0523. [DOI] [PubMed] [Google Scholar]
- 33.Warkentin T.E., Sheppard J.-A.I., Linkins L.-A., Arnold D.M., Nazy I. Performance characteristics of an automated latex immunoturbidimetricassay [HemosIL®HIT-Ab(PF4-H)] for the diagnosis of immune heparin-induced thrombocytopenia. Thromb Res. 2017;153:108–117. doi: 10.1016/j.thromres.2017.03.010. [DOI] [PubMed] [Google Scholar]
- 34.Sheridan D., Carter C., Kelton J.G. A diagnostic test for heparin-induced thrombocytopenia. Blood. 1986;67:27–30. [PubMed] [Google Scholar]
- 35.Warkentin T.E., Arnold D.M., Nazi I., Kelton J.G. The platelet serotonin-release assay. Am J Hematol. 2015;90:564–572. doi: 10.1002/ajh.24006. [DOI] [PubMed] [Google Scholar]
- 36.Price E.A., Hayward C.P., Moffat K.A., Moore J.C., Warkentin T.E., Zehnder J.L. Laboratory testing for heparin-induced thrombocytopenia is inconsistent in North America: a survey of North American specialized coagulation laboratories. Thromb Haemost. 2007;98:1357–1361. doi: 10.1160/th07-06-0401. [DOI] [PubMed] [Google Scholar]
- 37.Warkentin T.E., Hayward C.P., Smith C.A., Kelly P.M., Kelton J.G. Determinants of donor platelet variability when testing for heparin-induced thrombocytopenia. J Lab Clin Med. 1992;120:371–379. [PubMed] [Google Scholar]
- 38.Pötzsch B., Keller M., Madlener K., Müller-Berghaus G. The use of heparinase improves the specificity of crossreactivity testing in heparin-induced thrombocytopenia. Thromb Haemost. 1996;76:1121. [PubMed] [Google Scholar]
- 39.Greinacher A., Alban S., Dummel V., Franz G., Mueller-Eckhardt C. Characterization of the structural requirements for a carbohydrate based anticoagulant with a reduced risk of inducing the immunological type of heparin-associated thrombocytopenia. Thromb Haemost. 1995;74:886–892. [PubMed] [Google Scholar]
- 40.Greinacher A., Michels I., Kiefel V., Mueller-Eckhardt C. A rapid and sensitive test for diagnosing heparin-associated thrombocytopenia. Thromb Haemost. 1991;66:734–736. [PubMed] [Google Scholar]
- 41.Padmanabhan A., Jones C.G., Curtis B.R., Bougie D.W., Sullivan M.J., Peswani N., et al. A novel PF4-dependent platelet activation assay identifies patients likely to have heparin-induced thrombocytopenia/thrombosis. Chest. 2016;150:506–515. doi: 10.1016/j.chest.2016.02.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Padmanabhan A., Jones C.G., Bougie D.W., Curtis B.R., McFarland J.G., Wang D., et al. A modified PF4-dependent, CD62p expression assay selectively detects serotonin-releasing antibodies in patients suspected of HIT. Thromb Haemost. 2015;114:1322–1323. doi: 10.1160/TH15-02-0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Samuelson Bannow B., Warad D.M., Jones C.G., Pechauer S.M., Curtis B.R., Bougie D.W., et al. A prospective, blinded study of a PF4-dependent assay for HIT diagnosis. Blood. 2021;137:1082–1089. doi: 10.1182/blood.2020008195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Crowther M.A., Cook D.J., Meade M.O., Griffith L.E., Guyatt G.H., Arnold D.M., et al. Thrombocytopenia in medical-surgical critically ill patients: prevalence, incidence, and risk factors. J Crit Care. 2005;20:348–353. doi: 10.1016/j.jcrc.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 45.Li A., Hicks L.K., Fan E. Things we do for no reason: HIT testing in low probability patients. J Hosp Med. 2019;14:374–381. doi: 10.12788/jhm.3165. [DOI] [PubMed] [Google Scholar]
- 46.American Society of Hematology ten things physicians and patients should question. Choosing wisely: an initiative of the ABIM Foundation. https://www.choosingwisely.org/societies/american-society-of-hematology/
- 47.Greinacher A., Eichler P., Lubenow N., Kwasny H., Luz M. Heparin-induced thrombocytopenia with thromboembolic complications: meta-analysis of 2 prospective trials to assess the value of parenteral treatment with lepirudin and its therapeutic aPTT range. Blood. 2000;96:846–851. [PubMed] [Google Scholar]
- 48.Warkentin T.E. How I diagnose and manage HIT. Hematology Am Soc Hematol Educ Program. 2011;2011:143–149. doi: 10.1182/asheducation-2011.1.143. [DOI] [PubMed] [Google Scholar]
- 49.Raschke R.A., Gallo T., Curry S.C., Whiting T., Padilla-Jones A., Warkentin T.E., et al. Clinical effectiveness of a Bayesian algorithm for the diagnosis and management of heparin-induced thrombocytopenia. J Thromb Haemost. 2017;15:1640–1645. doi: 10.1111/jth.13758. [DOI] [PubMed] [Google Scholar]
- 50.Cuker A. Clinical and laboratory diagnosis of heparin-induced thrombocytopenia: an integrated approach. Semin Thromb Hemost. 2014;40:106–114. doi: 10.1055/s-0033-1363461. [DOI] [PubMed] [Google Scholar]
- 51.Cuker A., Arepally G.M., Chong B.H., Cines D.B., Greinacher A., Gruel Y., et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: heparin-induced thrombocytopenia. Blood Adv. 2018;2:3360–3392. doi: 10.1182/bloodadvances.2018024489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Warkentin T.E., Nazy I., Sheppard J.-A.I., Smith J.W., Kelton J.G., Arnold D.M. Serotonin-release assay-negative heparin-induced thrombocytopenia. Am J Hematol. 2020;95:38–47. doi: 10.1002/ajh.25660. [DOI] [PubMed] [Google Scholar]
- 53.Cuker A. Management of the multiple phases of heparin-induced thrombocytopenia. Thromb Haemost. 2016;116:835–842. doi: 10.1160/TH16-02-0084. [DOI] [PubMed] [Google Scholar]
- 54.Warkentin T.E., Maurer B.T., Aster R.H. Heparin-induced thrombocytopenia associated with fondaparinux. N Engl J Med. 2007;356:2653–2655. doi: 10.1056/NEJMc070346. [DOI] [PubMed] [Google Scholar]
- 55.Kang M., Alahmadi M., Sawh S., Kovacs M.J., Lazo-Langner A. Fondaparinux for the treatment of suspected heparin-induced thrombocytopenia: a propensity score–matched study. Blood. 2015;125:924–929. doi: 10.1182/blood-2014-09-599498. [DOI] [PubMed] [Google Scholar]
- 56.Schindewolf M., Steindl J., Beyer-Westendorf J., Schellong S., Dohmen P.M., Brachmann J., et al. Use of fondaparinux off-label or approved anticoagulants for management of heparin-induced thrombocytopenia. J Am Coll Cardiol. 2017;70:2636–2648. doi: 10.1016/j.jacc.2017.09.1099. [DOI] [PubMed] [Google Scholar]
- 57.Mahieu E., Claes K., Jacquemin M., Evenepoel P., Op De Beek K., Bogaert A.M., et al. Anticoagulation with fondaparinux for hemodiafiltration in patients with heparin-induced thrombocytopenia: dose-finding study and safety evaluation. Artif Organs. 2013;37:482–487. doi: 10.1111/aor.12002. [DOI] [PubMed] [Google Scholar]
- 58.Ghaziri D., Dehaini H., Msheik M., Bahmad M., Zorkot M., Saad G.A. Novel fondaparinux protocol for anticoagulation therapy in adults with renal failure and suspected heparin-induced thrombocytopenia: a retrospective review of institutional protocol. BMC Pharmacol Toxicol. 2023;24:2. doi: 10.1186/s40360-023-00643-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Linkins L.-A., Dans A.L., Moores L.K., Bona R., Davidson B.L., Schulman S., et al. Treatment and prevention of heparin-induced thrombocytopenia: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e495S–e530S. doi: 10.1378/chest.11-2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Warkentin T.E., Elavathil L.J., Hayward C.P., Johnston M.A., Russett J.I., Kelton J.G. The pathogenesis of venous limb gangrene associated with heparin-induced thrombocytopenia. Ann Intern Med. 1997;127:804–812. doi: 10.7326/0003-4819-127-9-199711010-00005. [DOI] [PubMed] [Google Scholar]
- 61.Srinivasan A.F., Rice L., Bartholomew J.R., Rangaswamy C., La Perna L., Thompson J.E., et al. Warfarin-induced skin necrosis and venous limb gangrene in the setting of heparin-induced thrombocytopenia. Arch Intern Med. 2004;164:66–70. doi: 10.1001/archinte.164.1.66. [DOI] [PubMed] [Google Scholar]
- 62.Warkentin T.E. High-dose intravenous immunoglobulin for the treatment and prevention of heparin-induced thrombocytopenia: a review. Expert Rev Hematol. 2019;12:685–698. doi: 10.1080/17474086.2019.1636645. [DOI] [PubMed] [Google Scholar]
- 63.Welsby I.J., Krakow E.F., Heit J.A., Williams E.C., Arepally G.M., Bar-Yosef S., et al. The association of anti-platelet factor 4/heparin antibodies with early and delayed thromboembolism after cardiac surgery. J Thromb Haemost. 2017;15:57–65. doi: 10.1111/jth.13533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Warkentin T.E., Sheppard J.A., Horsewood P., Simpson P.J., Moore J.C., Kelton J.G. Impact of the patient population on the risk for heparin-induced thrombocytopenia. Blood. 2000;96:1703–1708. [PubMed] [Google Scholar]
- 65.Pishko A.M., Cuker A. Heparin-induced thrombocytopenia and cardiovascular surgery. Hematology Am Soc Hematol Educ Program. 2021;2021:536–544. doi: 10.1182/hematology.2021000289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lillo-Le Louët A., Boutouyrie P., Alhenc-Gelas M., Le Beller C., Gautier I., Aiach M., et al. Diagnostic score for heparin-induced thrombocytopenia after cardiopulmonary bypass. J Thromb Haemost. 2004;2:1882–1888. doi: 10.1111/j.1538-7836.2004.00949.x. [DOI] [PubMed] [Google Scholar]
- 67.Pouplard C., May M.A., Regina S., Marchand M., Fusciardi J., Gruel Y. Changes in platelet count after cardiac surgery can effectively predict the development of pathogenic heparin-dependent antibodies. Br J Haematol. 2005;128:837–841. doi: 10.1111/j.1365-2141.2005.05381.x. [DOI] [PubMed] [Google Scholar]
- 68.Warkentin T.E. Acute intraoperative HIT during heart surgery: why so rare? Thromb Res. 2016;146:110–112. doi: 10.1016/j.thromres.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 69.Padmanabhan A., Connelly-Smith L., Aqui N., Balogun R.A., Klingel R., Meyer E., et al. Guidelines on the use of therapeutic apheresis in clinical practice - evidence-based approach from the writing Committee of the American Society for Apheresis: the Eighth Special Issue. J Clin Apher. 2019;34:171–354. doi: 10.1002/jca.21705. [DOI] [PubMed] [Google Scholar]
- 70.Greinacher A., Selleng K., Warkentin T.E. Autoimmune heparin-induced thrombocytopenia. J Thromb Haemost. 2017;15:2099–2114. doi: 10.1111/jth.13813. [DOI] [PubMed] [Google Scholar]
- 71.Warkentin T.E., Greinacher A. Spontaneous HIT syndrome: knee replacement, infection, and parallels with vaccine-induced immune thrombotic thrombocytopenia. Thromb Res. 2021;204:40–51. doi: 10.1016/j.thromres.2021.05.018. [DOI] [PubMed] [Google Scholar]
- 72.McGowan K.E., Makari J., Diamantouros A., Bucci C., Rempel P., Selby R., et al. Reducing the hospital burden of heparin-induced thrombocytopenia: impact of an avoid-heparin program. Blood. 2016;127:1954–1959. doi: 10.1182/blood-2015-07-660001. [DOI] [PubMed] [Google Scholar]
- 73.Samuelson B.T., Glynn E., Holmes M., White A.A., Martin D.B., Garcia D. Use of a computer-based provider order entry (CPOE) intervention to optimize laboratory testing in patients with suspected heparin-induced thrombocytopenia. Thromb Res. 2015;136:928–931. doi: 10.1016/j.thromres.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 74.Lim M.Y., Foster J., Rourk A., Greenberg C.S. Initial and long term impact of a multi-disciplinary task force in the diagnosis and management of heparin-induced thrombocytopenia. J Thromb Thrombolysis. 2018;45:130–134. doi: 10.1007/s11239-017-1592-z. [DOI] [PubMed] [Google Scholar]
- 75.Lee J., Lindsley J., Chasler J., Streiff M.B., Naik R., Shanbhag S., et al. The impact of an antithrombotic stewardship program on heparin-induced thrombocytopenia management. J Pharm Pract. 2022 doi: 10.1177/08971900221116185. [DOI] [PubMed] [Google Scholar]